Abstract
While many patients with hereditary optic neuropathies are caused by mitochondrial DNA (mtDNA) mutations of Leber’s hereditary optic neuropathy (LHON), a significant proportion of them does not have mtDNA mutation and is caused by mutations in genes of the nuclear genome. In this study, we investigated whether the OPA1 gene, which is a pathogenic gene for autosomal dominant optic atrophy (ADOA), is frequently mutated in these patients. We sequenced all 29 exons of the OPA1 gene in 105 Han Chinese patients with suspected LHON. mtDNA copy number was quantified in blood samples from patients with and without OPA1 mutation and compared to healthy controls. In silico program-affiliated prediction, evolutionary conservation analysis, and in vitro cellular assays were performed to show the potential pathogenicity of the mutations. We identified nine OPA1 mutations in eight patients; six of them are located in exons and three are located in splicing sites. Mutation c.1172T > G has not been reported before. When we combined our data with 193 reported Han Chinese patients with optic neuropathy and compared to the available data of 4327 East Asians by the Exome Aggregation Consortium (ExAC), we found a significant enrichment of potentially pathogenic OPA1 mutations in Chinese patients. Cellular assays for OPA1 mutants c.869G > A and c.2708_2711del showed abnormalities in OPA1 isoforms, mitochondrial morphology, and cellular reactive oxygen species (ROS) level. Our results indicated that screening OPA1 mutation is needed for clinical diagnosis of patients with suspected optic neuropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hereditary optic neuropathy is one of the most common genetic diseases, with typical symptom of progressive or acute loss of vision [1]. Primary mitochondrial DNA (mtDNA) mutations (for Leber hereditary optic neuropathy (LHON), OMIM535000) and the OPA gene mutations (for autosomal dominant optic atrophy (ADOA), OMIM165500) are two main causes for this disease. There are many patients suspected with optic neuropathy but without any known LHON primary mtDNA mutations. To characterize the pathogenic mutation and optimize a molecular screening method is very important for proper diagnosis of these patients.
The OPA1 gene is located in chromosome 3q28-29 and encodes a dynamin-related GTPase protein, which localizes to mitochondrial inner membrane and inter-membrane space [2]. The OPA1 is critical for mitochondrial function and morphology maintenance. First, OPA1 is a fusion protein that balances the fusion/fission process of mitochondrial inner membrane. OPA1 mutations could induce an overflow of cytochrome c from mitochondria and stimulate cellular apoptosis [3, 4]. Second, OPA1 is an essential component of mitochondrial cristae and inner membrane. Abnormal OPA1 protein impairs cellular function and causes mitochondrial respiratory chain dysfunction [4]. Finally, OPA1 protein regulates mitochondrial calcium (Ca2+) homeostasis and signaling, and mitochondrial Ca2+ retention capacity decreases in OPA1 knockdown cells [5].
The OPA1 gene was expressed in all tissues and had a high level in human retina and optic nerve [6]. Pathogenic OPA1 mutations could impair mitochondrial function in these tissues and caused a variety of mitochondrial disorders. The OPA1 gene mutations occurred in more than 60 % of ADOA patients [1], and mutations of the OPA3 gene could be also found in ADOA patients [7]. In this study, we screened all 29 exons of the OPA1 gene for mutations in 105 Han Chinese patients with suspected optic neuropathy. We observed an enrichment of OPA1 pathogenic mutations in these patients. Further functional assays showed that mutations c.869G > A and c.2708_2711del affected mitochondrial function.
Materials and Methods
Subjects
The patients were diagnosed as suspected optic neuropathy at the Pediatric and Genetic Clinic of the Eye Hospital, Zhongshan Ophthalmic Center, and/or local medical centers. All patients (n = 105) were sporadic cases without a family history of disease and were genetically unrelated. These patients had been analyzed for mtDNA sequence variations in our previous study [8] and were confirmed to have no LHON primary mtDNA mutations (m.11778G > A, m.14484T > C, m.3460G > A, and m.3635G > A).
Mutation Screening for the OPA1 Gene
Genomic DNA was isolated from whole blood by using the AxyPrep™ Blood Genomic DNA Miniprep Kit (Axygen, USA) according to the manufacturer’s instruction. A total of 31 pairs of primers were designed to amplify and sequence all exons (including the 3′-UTR region) and the exon and intron boundary regions of the OPA1 gene (Table S1). In brief, PCR was performed in a total of 50-μL reaction volume containing 5-μL 10× PCR buffer (Mg2+ plus), 2.5 units of TaKaRa rTaq (TaKaRa Bio Inc., Dalian, China), 400 μM of each deoxynucleotide triphosphate (dNTP), 0.2 μM of each primer, and 50 ng DNA. We followed the standard nomenclature recommendations of the HGVS (http://www.HGVS.org/mutnomen/) to name the mutation(s), and mRNA sequence of OPA1 isoform 1 (NM_015560) was used as the reference sequence.
Quantification of mtDNA Copy Number
We quantified the mtDNA copy number in individuals of three groups (group no. 1: patient 1, suspected LHON patients with OPA1 mutations, n = 8; group no. 2: patient 2, suspected LHON patients without OPA1 mutations, n = 12; and group no. 3: control, healthy controls from the general populations reported in our previous study, n = 17 [9]) using the same method described in our previous study [10]. Real-time quantitative PCR with SYBR® Premix ExTaq TM II Kit (TaKaRa Biotechnology Co. Ltd., Dalian, China) was performed on the BioRad iQ5 Real-Time PCR System (Bio-Rad Laboratories Inc., USA). The single-copy nuclear β-globin gene was used as the reference gene. Primers and procedure were same to our previous study [10].
Plasmid Construction
Total RNA was extracted from whole blood of a healthy donor according to the manufacturer’s instructions using the TRIzol Reagent (Invitrogen, USA). Around 1 μg RNA was used to prepare complementary DNA (cDNA) by using the Transcriptor First-Strand cDNA Synthesis Kit (Roche, USA). The coding region of the wild-type OPA1 gene was amplified by primer pair OPA1-CDS-F (5′-CCGCTCGAGATGTGGCGACTACGTCGGG-3′)/OPA1-CDS-R (5′-CGCGGATCCTTTCTCCTGATGAAGAGCTT-3′), with cDNA as the template. The restriction endonuclease sites were designed in the 5′-end of each primer (Xho I site in OPA1-CDS-F and Bam HI site in OPA1-CDS-R are underlined). The amplicon was digested, purified, and cloned into plasmid pcDNA3.1. The flag tag was added to the C-terminal of the OPA1 protein for further detection. The OPA1 mutants identified in patients were generated by the site-directed mutagenesis PCR method. In brief, PCR was performed in a total of 50-μL reaction volume containing 5-μL 10× PCR buffer, 1 unit of KOD-Plus-Neo (TOYOBO, Japan), 1.5 mM Mg2+, 200 μM of each dNTP, 0.3 μM of each primer (Table S2), and 50-ng plasmid DNA. The following PCR condition was used: 1 cycle of 94 °C for 1 min, 30 cycles of 94 °C for 30 s and 65 °C for 7 min, and one extension cycle of 72 °C for 10 min.
Cell Culture and Transfection
HeLa cells were grown in Dulbecco’s modified Eagle’s medium (DMEM; Gibco, USA) supplemented with 100 u/mL penicillin, 100 μg/mL streptomycin, and 10 % FBS in a 12-well plate at 37 °C with 5 % CO2. A mixture of 2-μg plasmid DNA and 3 μL of FuGENE HD transfection reagent (Roche, USA) was transfected when cells were grown to 80 % confluence. Cells without any transfection or cells transfected with empty pcDNA3.1 vector were used as the controls. Cells were harvested at 48 h after the transfection.
Western Blot and Confocal Fluorescence Microscopy
Western blot was performed to show the expression of the OPA1 mutants following a similar procedure as described in our recent study [11]. In brief, HeLa cells were collected and lysed in lysis buffer (Beyotime, China) to extract total protein. About 20 μg protein was electrophoresed in 12 % SDS polyacrylamide gel and was transferred to a polyvinylidene difluoride membrane (Bio-Rad, USA). The membrane was blocked in 5 % (w/v) nonfat milk for 2 h at room temperature, then incubated with monoclonal mouse anti-FLAG antibody (Abmart, China) (1:5000) overnight at 4 °C. After three washes with TBST (each wash 5 min), the membrane was incubated with anti-mouse IgG peroxidase-conjugated secondary antibody (KPL, Gaithersburg, MD, USA) (1:10,000) for 1 h at room temperature. Immobilon Western Chemiluminescent HRP Substrate (Millipore, USA) was used to visualize the epitope.
Confocal fluorescence microscopy was used to investigate the localization of the OPA1 mutants and mitochondrial morphology. HeLa cells were co-transfected with pcDNA3.1-OPA1 fused with flag tag and DsRed-Mito. After transfection for 48 h, cells were fixed with paraformaldehyde (PFA; 4 % (w/v) in phosphate-buffered saline (PBS)) for 10 min and were permeabilized using 0.2 % (v/v) Triton X-100, followed by a block in 5 % (w/v) bovine serum albumin for 1 h at room temperature. Cells were incubated with primary antibody (anti-FLAG, Abmart, 1:5000) overnight at 4 °C, then with a FITC-conjugated secondary antibody (KPL, 1:50) for 1 h at room temperature after three washes with PBS. 4′,6-Diamidino-2-phenylindole (DAPI) (Roche) was used to color nucleus. Cells were imaged using the Olympus FluoView™ 1000 confocal microscope (Olympus, Melville, NY, USA) at 488 and 563 nm, respectively.
Measurement of Reactive Oxygen Species
Cellular reactive oxygen species (ROS) level was measured following the method described in our previous study [12]. In brief, cells were incubated in PBS containing 2-μM DCFH-DA probe (Sigma-Aldrich, USA, D6883) at 37 °C for 20 min. After three washes with PBS, cells were detected by flow cytometry (BD, Vantage SE, USA) at 535 nm.
Data Analysis
We searched the OPA1 mutations identified in patients in the available datasets, including dbSNP Short Genetic Variants (http://www.ncbi.nlm.nih.gov/projects/SNP); Exome Aggregation Consortium (ExAC), Cambridge, MA (http://exac.broadinstitute.org; accessed on December 16, 2015); and eOPA1 (http://mitodyn.org/home.php) [13, 14]. Evolutionary conservation of the OPA1 mutation was performed in the following eight species: Caenorhabditis elegans (CAA87771), Drosophila melanogaster (NP_610941), Danio rerio (NP_001007299), Gallus gallus (NP_001034398), Mus musculus (NP_001186106), Bos taurus (NP_001179890), Pan troglodytes (XP_003310226), and Homo sapiens (NP_056375). Five prediction algorithms (PolyPhen2 HumDiv and HumVar [15, 16], LRT [17], MutationTaster [18], and SIFT [19, 20]) were used to evaluate the potential pathogenicity of each mutation. We combined our data with 193 Chinese patients with optic neuropathy [21] and compared to 4327 East Asians by the ExAC. Fisher’s exact test was used to show the frequency difference of the OPA1 mutation between Chinese patients and the ExAC East Asians. Statistical difference of mtDNA copy number and cellular ROS levels between two groups was tested by two-tailed Student’s t test. A P value < 0.05 was considered as statistically significant.
Results
High Frequency of OPA1 Mutations in Han Chinese Patients with Optic Neuropathy
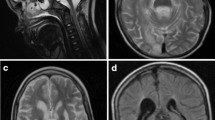
A total of nine mutations were identified in 8 out of 105 patients with suspected optic neuropathy. All mutations were heterozygous (Fig. 1). Among them, five (c.565G > A, p.E189K; c.575C > T, p.A192V; c.869G > A, p.R290L; c.1172T > G, p.L391R; and c.1465A > G, p.K489E) were missense mutations, three mutations (c.556 + 2T > G, c.2819 − 2A > G, and c.2614 − 2A > G) were located in the splice site of the intron and exon, and one mutation (c.2708_2711del) caused a truncated protein (Table 1). Mutations c.575C > T and c.1465A > G co-occurred in one patient. The web-based searches showed that mutation c.1172T > G (p.L391R) had not been reported previously. Mutations c.869G > A, c.1172T > G, and c.1465A > G were located in highly conserved domain of the GTPase and changed a highly conserved amino acid. Mutations c.565G > A and c.575C > T were not conserved in the eight species analyzed in this study (Fig. 2a). When we applied the five reported algorithms (PolyPhen2 HumDiv and HumVar [15, 16], LRT [17], MutationTaster [18], and SIFT [19, 20]) to predict the potential pathogenicity of these missense mutations, we found that mutation c.565G > A was predicted to be benign by all five algorithms; mutation c.575C > T was predicted to be possibly damaging by three of the five algorithms; and mutations c.869G > A, c.1172T > G, and c.1465A > G were predicted to be damaging by at least four algorithms, thus were highly possible to be pathogenic.
Sequencing electropherograms showing the OPA1 mutations in Han Chinese patients with optic neuropathy. Mutations c.565G > A, c.575C > T, c.869G > A, c.1172T > G, and c.1465A > G are missense mutations; mutations c.556 + 2T > G, c.2819 − 2A > G, and c.2614 − 2A > G are located in the splice site of the intron and exon; and mutation c.2708_2711del is a frame shift mutation. Mutations c.575C > T and c.1465A > G co-exist in patient Le1002
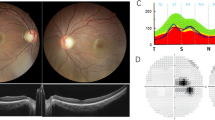
Evolutionary conservation analysis and isoform expression of the OPA1 mutants. a Eight species were used to analyze the evolutionary conservation of the OPA1 gene mutations. Sequences of Caenorhabditis elegans (CAA87771), Drosophila melanogaster (NP_610941), Danio rerio (NP_001007299), Gallus gallus (NP_001034398), Mus musculus (NP_001186106), Bos taurus (NP_001179890), Pan troglodytes (XP_003310226), and Homo sapiens (NP_056375) were retrieved from GenBank. b Western blot of the OPA1 isoforms in HeLa cells overexpressing different mutants. The two OPA1 isoforms were tagged by flag. A truncated protein (about 35 kDa) was observed in HeLa cells overexpressing mutant c.2708_2711del. The untransfected cells were as the control
We further combined our data with the reported OPA1 data in 193 Chinese patients [21], and compared to the East Asian population retrieved from the ExAC database (http://exac.broadinstitute.org), which contains the exome sequencing data of 4327 individuals. Mutation c.2708_2711del had a significantly higher frequency in Chinese patients with optic neuropathy than in the ExAC East Asians (P = 0.00002; Table 2). We retrieved all potentially pathogenic OPA1 mutations with a minor allele frequency (MAF) less than 0.01 in the East Asian population from the ExAC dataset (Supplementary Table 3) and grouped them into four categories (missense mutations, frame shift mutations, nonsense mutations, and splicing mutations; Table 3). Comparison of the four mutation categories between Han Chinese patients with optic neuropathy and the ExAC East Asian population revealed that these potentially pathogenic mutations are significantly enriched in Chinese patients (Table 3).
Altered Isoform Expression of OPA1 Mutants
Two OPA1 isoforms, long-OPA1 (l-OPA1) and short-OPA1 (s-OPA1), were recognized by Western blot in HeLa cells transfected with different OPA1 mutants (Fig. 2b). The s-OPA1 isoform in cells overexpressing mutant c.869G > A was somewhat larger than that of cells overexpressing with wild-type or other mutants. Cells that overexpressed OPA1 mutant with mutation c.2708_2711del showed no bands for l-OPA1 and s-OPA1, but a truncated protein with a size around 35 kDa was observed, which might be caused by the premature stop codon (Fig. 2b). These results suggested that the OPA1 gene mutations identified in Chinese patients affected the expression level of different isoforms, which might lead to further change of cellular function.
OPA1 Mutants Impair Mitochondrial Function
Cellular localization of the ectopically expressed OPA1 mutant (marked by green fluorescence) was overlapped with mitochondria (red fluorescence), which was consistent with the notion that OPA1 is a mitochondrial protein and suggested that these mutants did not affect cellular localization of the OPA1 (Fig. 3). However, we found that mitochondrial morphology had a change from a network distribution to a dot distribution in the cells overexpressing mutant c.2708_2711del, which indicated the impairment of mitochondrial fusion (Fig. 3). No apparent change of mitochondrial morphology was observed in cells overexpressing the other mutants. We further quantified the cellular ROS level in all transfected cells and observed mild increase of ROS levels in cells overexpressing all mutants, albeit the difference was not significant (Fig. 4a).
Cellular ROS level in HeLa cells overexpressing OPA1 mutants and mtDNA copy number in patients with and without OPA1 mutations. a HeLa cells overexpressing OPA1 mutants (OPA1-mutation) had a relatively higher cellular ROS level than those cells overexpressing wild-type OPA1 (OPA1-WT) or empty expression vector pcDNA3.1. b mtDNA copy number in Han Chinese patients with optic neuropathy and normal controls. Patient 1—patients with optic neuropathy and OPA1 mutations, patient 2—patients with optic neuropathy but no OPA1 mutations, and control—healthy individuals reported in our previous study [9]
Decrease of mtDNA Copy Number in Patients with OPA1 Mutations
OPA1 plays an important role in mtDNA maintenance and distribution [22]. We measured the mtDNA copy number in patients with and without OPA1 mutations and healthy individuals. We found that the average mtDNA copy number was relatively decreased in the eight patients with OPA1 mutations in comparison to that of patients without mutation or normal controls, whereas the average mtDNA copy number was similar in the patients without OPA1 mutations and normal controls (Fig. 4b). Note that this pattern was based on limited number of individuals analyzed in this study and there was a large variance within each group.
Discussion
ADOA and LHON are two common ophthalmological diseases caused by gene mutations and can be diagnosed according to clinical symptoms and family history [23, 24]. There are many sporadic cases with symptoms similar to LHON but without any known LHON primary mtDNA mutations [7, 8, 25], and the exact etiological factor was unclear. The OPA1 gene was one of the most possible causal genes for this disease [7, 25]. Hitherto, many OPA1 gene mutations had been reported (cf. eOPA1 [http://mitodyn.org/home.php ]) and the mutation spectra were somewhat different among populations [7, 21, 26, 27]. The Chinese patients with optic neuropathy in this study expressed acute vision loss but had no known LHON primary mtDNA mutations [8]. Genetic analysis of the OPA1 gene mutations in these patients will undoubtedly help to make a proper diagnosis.
In this study, we identified an enrichment of potentially pathogenic OPA1 mutations in Chinese patients with optic neuropathy. The in silico program-affiliated prediction of the pathogenicity by using five algorithms showed that three mutations (c.869G > A, c.1172T > G, and c.1465A > G) might be damaging by changing the GTPase activity. Our current finding, together with the mutations reported in Han Chinese patients [21, 25], suggested that the mutation spectrum of the OPA1 gene in Chinese patients was different from that of populations of European ancestry. Mutation c.575C > T was previously reported in a glaucoma patient [28] and Chinese patients with suspected hereditary optic neuropathic [21] and had a relatively high frequency (2.5 %) in the ExAC East Asians (Table 2). Moreover, it caused no apparent mitochondrial morphology change in HeLa cells (Fig. 3). Therefore, variant c.575C > T may be regarded as a benign polymorphism. Mutation c.869G > A was previously reported in a French ADOA family and caused mitochondrial dysfunction [29]. Similar to mutations c.868C > T, c.808G > A, and c.869G > T [30], c.869G > A was located in highly conservative region of the GTPase and was predicted to be damaging (Table 1), which might influence the function of OPA1 by changing the expression of isoforms and its structure (Fig. 2). Mutant c.869G > A led to a larger s-OPA1 than that of wild type (Fig. 2); this result was consistent with a previous study that identified the isoform variation and function impairment in fibroblast cell of patients with c.869G > A [29]. Mutation c.2708_2711del was a hot spot mutation [21, 31, 32] and produced a truncated OPA1 protein of 35 KDa, which heavily affected the mitochondrial morphology (Fig. 3). However, mutation c.2708_2711del might not lead to seriously clinical symptoms according to previous study in ADOA patients [32]. Mutations c.556 + 2T > G, c.2819 − 2A > G, and c.2614 − 2A > G were located in splicing sites of exons and introns.
Cellular ROS level could affect many disorders, such as tumors and liver inflammation [33, 34]. It has been identified that the OPA1 gene mutations could increase ROS level, accelerate lattice cell apoptosis, and shorten the life span in Drosophila model [35, 36]. Chen et al. [37] identified that the heterozygous OPA1 mutation led to decreased mtDNA copy number, increased ROS level, and fragmented mitochondria in mouse model. Similar to these studies, we identified an increasing ROS level in HeLa cells overexpressing OPA1 mutants and a decreasing mtDNA copy number in patients with the OPA1 mutations, although the difference was not statistically significant (perhaps due to the relatively small number of patients under consideration). The increasing ROS could induce release of OPA1 and cytochrome c from mitochondria to cytosol, which would lead to mitochondrial fragmentation and cell death [38]. Our current results, together with others [36, 37], suggested that increasing ROS and mitochondrial dysfunction might be one of the causes for optic neuropathy.
In sum, the OPA1 gene mutations are frequent in Han Chinese patients with optic neuropathy. In silico prediction and functional assays indicated that some of these mutations are pathogenic and affect cellular ROS level, expression of OPA1 isoforms, and mitochondrial morphology. The significant enrichment of potentially pathogenic mutations in Han Chinese patients with suspected optic neuropathy indicated that screening the OPA1 gene mutations should be encouraged for precise diagnosis of patients.
References
Yu-Wai-Man P, Griffiths PG, Hudson G, Chinnery PF (2009) Inherited mitochondrial optic neuropathies. J Med Genet 46(3):145–158
Hoppins S, Lackner L, Nunnari J (2007) The machines that divide and fuse mitochondria. Annu Rev Biochem 76:751–780
Frezza C, Cipolat S, Martins de Brito O, Micaroni M, Beznoussenko GV, Rudka T, Bartoli D, Polishuck RS et al (2006) OPA1 controls apoptotic cristae remodeling independently from mitochondrial fusion. Cell 126(1):177–189
Olichon A, Baricault L, Gas N, Guillou E, Valette A, Belenguer P, Lenaers G (2003) Loss of OPA1 perturbates the mitochondrial inner membrane structure and integrity, leading to cytochrome c release and apoptosis. J Biol Chem 278(10):7743–7746
Kushnareva YE, Gerencser AA, Bossy B, Ju WK, White AD, Waggoner J, Ellisman MH, Perkins G et al (2013) Loss of OPA1 disturbs cellular calcium homeostasis and sensitizes for excitotoxicity. Cell Death Differ 20(2):353–365
Wang AG, Fann MJ, Yu HY, Yen MY (2006) OPA1 expression in the human retina and optic nerve. Exp Eye Res 83(5):1171–1178
Yu-Wai-Man P, Shankar SP, Biousse V, Miller NR, Bean LJ, Coffee B, Hegde M, Newman NJ (2011) Genetic screening for OPA1 and OPA3 mutations in patients with suspected inherited optic neuropathies. Ophthalmology 118(3):558–563
Zhang AM, Jia X, Bi R, Salas A, Li S, Xiao X, Wang P, Guo X et al (2011) Mitochondrial DNA haplogroup background affects LHON, but not suspected LHON, in Chinese patients. PLoS One 6(11), e27750
Feng YM, Jia YF, Su LY, Wang D, Lv L, Xu L, Yao YG (2013) Decreased mitochondrial DNA copy number in the hippocampus and peripheral blood during opiate addiction is mediated by autophagy and can be salvaged by melatonin. Autophagy 9(9):1395–1406
Bi R, Zhang AM, Zhang W, Kong QP, Wu BL, Yang XH, Wang D, Zou Y et al (2010) The acquisition of an inheritable 50-bp deletion in the human mtDNA control region does not affect the mtDNA copy number in peripheral blood cells. Hum Mutat 31(5):538–543
Bi R, Zhang W, Yu D, Li X, Wang HZ, Hu QX, Zhang C, Lu W et al (2015) Mitochondrial DNA haplogroup B5 confers genetic susceptibility to Alzheimer’s disease in Han Chinese. Neurobiol Aging 36(3):1604. e7
Guo H, Zhuang XY, Zhang AM, Zhang W, Yuan Y, Guo L, Yu D, Liu J et al (2012) Presence of mutation m.14484T > C in a Chinese family with maternally inherited essential hypertension but no expression of LHON. Biochim Biophys Acta 1822(10):1535–1543
Ferre M, Amati-Bonneau P, Tourmen Y, Malthiery Y, Reynier P (2005) eOPA1: an online database for OPA1 mutations. Hum Mutat 25(5):423–428
Ferre M, Caignard A, Milea D, Leruez S, Cassereau J, Chevrollier A, Amati-Bonneau P, Verny C et al (2015) Improved locus-specific database for OPA1 mutations allows inclusion of advanced clinical data. Hum Mutat 36(1):20–25
Adzhubei I, Jordan DM, Sunyaev SR (2013) Predicting functional effect of human missense mutations using PolyPhen-2. Current protocols in human genetics/editorial board, Jonathan L Haines [et al.] Chapter 7:Unit7 20
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR (2010) A method and server for predicting damaging missense mutations. Nat Methods 7(4):248–249
Chun S, Fay JC (2009) Identification of deleterious mutations within three human genomes. Genome Res 19(9):1553–1561
Schwarz JM, Cooper DN, Schuelke M, Seelow D (2014) MutationTaster2: mutation prediction for the deep-sequencing age. Nat Methods 11(4):361–362
Kumar P, Henikoff S, Ng PC (2009) Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4(7):1073–1081
Ng PC, Henikoff S (2003) SIFT: predicting amino acid changes that affect protein function. Nucleic Acids Res 31(13):3812–3814
Chen Y, Jia X, Wang P, Xiao X, Li S, Guo X, Zhang Q (2013) Mutation survey of the optic atrophy 1 gene in 193 Chinese families with suspected hereditary optic neuropathy. Mol Vis 19:292–302
Elachouri G, Vidoni S, Zanna C, Pattyn A, Boukhaddaoui H, Gaget K, Yu-Wai-Man P, Gasparre G et al (2011) OPA1 links human mitochondrial genome maintenance to mtDNA replication and distribution. Genome Res 21(1):12–20
Delettre C, Lenaers G, Griffoin JM, Gigarel N, Lorenzo C, Belenguer P, Pelloquin L, Grosgeorge J et al (2000) Nuclear gene OPA1, encoding a mitochondrial dynamin-related protein, is mutated in dominant optic atrophy. Nat Genet 26(2):207–210
Tonska K, Kodron A, Bartnik E (2010) Genotype-phenotype correlations in Leber hereditary optic neuropathy. Biochim Biophys Acta 1797(6–7):1119–1123
Chen J, Xu K, Zhang X, Jiang F, Liu L, Dong B, Ren Y, Li Y (2014) Mutation screening of mitochondrial DNA as well as OPA1 and OPA3 in a Chinese cohort with suspected hereditary optic atrophy. Invest Ophthalmol Vis Sci 55(10):6987–6995
Kamakari S, Koutsodontis G, Tsilimbaris M, Fitsios A, Chrousos G (2014) First report of OPA1 screening in Greek patients with autosomal dominant optic atrophy and identification of a previously undescribed OPA1 mutation. Mol Vis 20:691–703
Liskova P, Ulmanova O, Tesina P, Melsova H, Diblik P, Hansikova H, Tesarova M, Votruba M (2013) Novel OPA1 missense mutation in a family with optic atrophy and severe widespread neurological disorder. Acta Ophthalmol (Copenh) 91(3):e225–e231
Yu-Wai-Man P, Stewart JD, Hudson G, Andrews RM, Griffiths PG, Birch MK, Chinnery PF (2010) OPA1 increases the risk of normal but not high tension glaucoma. J Med Genet 47(2):120–125
Olichon A, Landes T, Arnaune-Pelloquin L, Emorine LJ, Mils V, Guichet A, Delettre C, Hamel C et al (2007) Effects of OPA1 mutations on mitochondrial morphology and apoptosis: relevance to ADOA pathogenesis. J Cell Physiol 211(2):423–430
Pesch UE, Leo-Kottler B, Mayer S, Jurklies B, Kellner U, Apfelstedt-Sylla E, Zrenner E, Alexander C et al (2001) OPA1 mutations in patients with autosomal dominant optic atrophy and evidence for semi-dominant inheritance. Hum Mol Genet 10(13):1359–1368
Lodi R, Tonon C, Valentino ML, Iotti S, Clementi V, Malucelli E, Barboni P, Longanesi L et al (2004) Deficit of in vivo mitochondrial ATP production in OPA1-related dominant optic atrophy. Ann Neurol 56(5):719–723
Yu-Wai-Man P, Griffiths PG, Gorman GS, Lourenco CM, Wright AF, Auer-Grumbach M, Toscano A, Musumeci O et al (2010) Multi-system neurological disease is common in patients with OPA1 mutations. Brain 133(Pt 3):771–786
Takahashi A, Ohtani N, Yamakoshi K, Iida S, Tahara H, Nakayama K, Nakayama KI, Ide T et al (2006) Mitogenic signalling and the p16INK4a-Rb pathway cooperate to enforce irreversible cellular senescence. Nat Cell Biol 8(11):1291–1297
Brenner C, Galluzzi L, Kepp O, Kroemer G (2013) Decoding cell death signals in liver inflammation. J Hepatol 59(3):583–594
Tang S, Le PK, Tse S, Wallace DC, Huang T (2009) Heterozygous mutation of Opa1 in Drosophila shortens lifespan mediated through increased reactive oxygen species production. PLoS One 4(2), e4492
Yarosh W, Monserrate J, Tong JJ, Tse S, Le PK, Nguyen K, Brachmann CB, Wallace DC et al (2008) The molecular mechanisms of OPA1-mediated optic atrophy in Drosophila model and prospects for antioxidant treatment. PLoS Genet 4(1), e6
Chen L, Liu T, Tran A, Lu X, Tomilov AA, Davies V, Cortopassi G, Chiamvimonvat N et al (2012) OPA1 mutation and late-onset cardiomyopathy: mitochondrial dysfunction and mtDNA instability. J Am Heart Assoc 1(5), e003012
Sanderson TH, Raghunayakula S, Kumar R (2015) Release of mitochondrial Opa1 following oxidative stress in HT22 cells. Mol Cell Neurosci 64:116–122
Acknowledgments
We thank all participants in this study. We thank Miss Dandan Yu and Dr. Deng-Feng Zhang for the technical assistance. This study was supported by National Natural Science Foundation of China (grant number 81200725) and the Strategic Priority Research Program (B) of the Chinese Academy of Sciences (XDB02020003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Written informed consents conforming to the tenets of the Declaration of Helsinki were obtained from each participant prior to the study. The Institutional Review Boards of the Zhongshan Ophthalmic Center and the Kunming Institute of Zoology approved this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOC 62 kb)
Supplementary Table 2
(DOC 35 kb)
Supplementary Table 3
(XLSX 26 kb)
Rights and permissions
About this article
Cite this article
Zhang, AM., Bi, R., Hu, QX. et al. The OPA1 Gene Mutations Are Frequent in Han Chinese Patients with Suspected Optic Neuropathy. Mol Neurobiol 54, 1622–1630 (2017). https://doi.org/10.1007/s12035-016-9771-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-9771-z