Abstract
There is a high rate of misdiagnosis between major depressive disorder (MDD) and bipolar disorder (BD) in clinical practice. Our previous work provided suggestive evidence for brain-derived neurotrophic factor (BDNF) in differentiating BD from MDD. In this study, we aimed to investigate the role of mature BDNF (mBDNF) and its precursor (proBDNF) in distinguishing bipolar depression (BP) from MDD during acute depressive episode. A total of 105 participants, including 44 healthy controls, 37 MDD patients and 24 BP patients, were recruited. Enzyme-linked immunosorbent assay kits were applied to measure plasma mBDNF levels and proBDNF levels of all participants. Plasma mBDNF levels were significantly decreased in BP group than those in MDD group (P = 0.001) and healthy controls (P = 0.002). Significantly higher ratio of mBDNF to proBDNF (M/P) at baseline was showed in MDD group than those in BP group as well as in healthy controls (P = 0.000 and P = 0.000, respectively). The optimal model for discriminating BP was the M/P ratio (area under the ROC curve = 0.858, 95 % CI 0.753–0.963). Furthermore, the M/P ratio was restored to normal levels after antidepressants treatment in MDD group. In summary, our data demonstrated that both plasma mBDNF levels and M/P ratio were lower in BP compared with MDD. These findings further support M/P ratio as a potential differential diagnostic biomarker for BP among patients in depressive episodes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) and bipolar disorder (BD) are both common and severe psychiatric disorders with high misdiagnosis rate and heavy disease burden [1]. However, there is a high misdiagnosis rate of bipolar depression (BP) just based on symptomology in depressive patients whose previous manic or mixed episodes have not been well-recognized [2, 3]. In clinics, mood screening scales are commonly used as adjuvant tools to differentiate BP from MDD [4]. However, biomarkers in laboratory examination or neuroimaging for correctly diagnosis of BP may be more sensitive and objective. To develop specific biomarkers of BP would be a great help to correct treatment and rapid recovery for BP patients.
Brain-derived neurotrophic factor (BDNF) is an essential neurotrophic factor for neurogenesis and synaptic plasticity. There is accumulating evidence for its role in the pathophysiology of psychiatric disorders [5–7]. The association of BDNF and mood disorders has been widely explored in clinical studies and in animal models [8, 9]. Up to now, a number of clinical studies on different aspects of the association of BDNF and mood disorders, such as serum/plasma levels, mRNA levels and gene variations, have emerged in recent years [10–13]. BDNF protein levels in BD patients were reported to be decreased, regardless of depressive episodes, manic ones, or mixed ones [14–16]. Based on a meta-analysis of 52 clinical studies, peripheral BDNF has been suggested as a potential biomarker of disease activity in BD [11]. Meanwhile, a number of studies have reported decreased BDNF mRNA and protein levels in MDD patients [17–19]. Also, BDNF protein levels have been consistently reported to be associated with the prognosis of MDD and BD [20, 21].
Although plenty of evidences have demonstrated that BDNF levels were decreased during acute mood episodes both in BD and MDD [10, 11, 20, 22, 23], the same trajectory from acute episodes to remission did not necessarily indicated the same peripheral BDNF levels between MDD and BP. In 2009, Fernandes et al. [24] performed a study to investigate whether BDNF could be a differential diagnosis biomarker for depressive episodes and found decreased serum BDNF levels in BP compared with unipolar depression and controls with high accuracy. However, only protein levels of BDNF were not enough to be applied as a diagnostic tool due to its lack of specificity during acute episodes [14]. A 3-year prospective study pointed out that plasma BDNF levels alone on admission (only when combined with mRNA) did not properly discriminate bipolar from unipolar depression [25]. Thus, although some progress has been made in this area, the role of BDNF in differentiation between BP and MDD remains further investigation.
It is known that BDNF has two forms in blood: mature BDNF (mBDNF) and precursor BDNF (proBDNF) which elicits opposite effects in central nervous system [26, 27]. mBDNF is formed from the cleavage of proBDNF [28, 29], and therefore, the ratio of mBDNF to proBDNF (M/P) may reflect the metabolism of BDNF and serve as an index reflecting different biological function of mBDNF and proBDNF in brain [30]. It was shown that M/P ratio reduced in midbrain and hippocampus of aggressive rats [30]. Furthermore, the ratio of proBDNF/total BDNF was regarded as a highly predictive novel quantitative biomarker to detect stress in fishes [31]. Therefore, M/P ratio may be a more sensitive index than only BDNF (or proBDNF) in consideration of BDNF changes in central nervous system.
To our knowledge, the previous human BDNF enzyme-linked immunosorbent assay (ELISA) kits used in these studies had the limitation to distinguish mBDNF and proBDNF [32]. With the development of ELISA kits used to measure mBDNF and proBDNF separately, several studies have been carried out to explore the association between proBDNF and mood disorders as well as proBDNF and medication in recent years [33, 34]. Prior literatures reported higher serum mBDNF and lower proBDNF in BD patients [35], while lower serum mBDNF and higher serum proBDNF was reported in MDD patients [36, 37]. However, there is scarcity of data on the role of proBDNF and mBDNF in differential diagnosis of BP and MDD. In view of the inconsistent changes of mBDNF and proBDNF in peripheral blood in BD and MDD patients, we hypothesised that M/P ratio may have potential diagnostic values for distinguishing BP from MDD in the present study. A major objective of the present study was to determine whether plasma mBDNF levels, proBDNF levels and M/P ratio were different in BP and MDD. We also focused on the relationship of M/P ratio and antidepressants therapy in patients with MDD.
Materials and Methods
Participants
Participants aged from 18 to 50 years were recruited from Shanghai Mental Health Center from June 2014 to May 2015. The study was reviewed and approved by the Institutional Review Board of Shanghai Mental Health Centre, and all protocols related to human experiments were conducted in accordance with the Declaration of Helsinki. All participants received a detailed explanation of the study and written informed consent was obtained from all individuals prior to their inclusion. We made sure all of them knew the potential risks and benefits of our study before their participation.
All participants underwent the Structured Clinical Interview for DSM-IV-TR Axis I Disorders-Patient Edition (SCID-I/P) and patients were diagnosed according to DSM-IV-TR criteria for MDD and bipolar I disorder. Demographic data on age, gender, education, marriage and clinical characteristics, including age of the first onset, numbers of episodes, total duration of illness and family history of psychiatric disorders, were collected. MDD patients were treated with SSRIs and BP patients were treated with lithium monotherapy, quetipine monotherapy, or combination therapy of lithium and quetipine (see Supplementary Table S1). Only Benzodiazepines were allowed to improve insomnia for short-term use. Assessments of Hamilton Rating Scale for Depression-17 (HAMD), Hamilton Rating Scale for Anxiety (HAMA) and Young Mania Rating Scale (YMRS) were conducted independently by two experienced psychiatrists on admission and at weeks 2, 4, 6, 8 and 12, respectively. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS) was conducted by patients themselves. Drug-free patients who did not take any psychotropic medications during the period of 3 months before enrolment with HAMD score of >17 were recruited. Exclusion criteria included: comorbid other Axis I psychiatric disorders including those with anxiety disorder, schizophrenia, nicotine dependence and use, alcohol dependence and other substance abuse; severe medical illness (e.g. cancer and diabetes) and organic brain disease; and those who were pregnant or breastfeeding.
Healthy controls without any major Axis I disorders, positive family history of psychiatric disorders and severe physical diseases were recruited by advertisement and those whose scores of HAMD were less than 7 were enrolled. The QIDS was conducted by controls themselves.
Measurements
On admission, 10 ml peripheral venous blood of each fasting participant was collected in EDTA tubes between 7 a.m. and 9 a.m. In MDD group, we also intended to collect peripheral venous blood at week 12. Peripheral venous blood was centrifuged at 3000 rpm at 4 ˚C for 20 min and plasma samples were separated immediately. All plasma samples were then frozen to −80 ˚C for analysing simultaneously. ELISA kits (Code number: HEB005 and HEP142) were respectively applied to exam plasma levels of mBDNF and proBDNF. The reproducibility of the assay was tested prior to the measurement of the samples and the inter-assay coefficient of variation was 4.41 %. Each plasma sample was measured in duplicate by the ELISA assay according to the manufacturer’s introductions (Shanghai Bogoo Biotechnology Co., Ltd. Shanghai, China). The microplate reader (Mulltiskan MK3, Thermo Electron, USA) was set at 450 nm wave length and the optical density (OD) values were measured. Plasma levels of mBDNF and proBDNF in testing samples can be calculated based on standard curve thereby. The laboratory technicians who were responsible for analysing plasma mBDNF and proBDNF were masked to the status of all participants.
Statistical Methods
In our study, SPSS 18 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical computations. Data were examined for normality using the Kolmogorov-Smirnov test. Demographic data and clinical characteristics were analysed using chi-squared, Student’s t test or ANOVA (one way) as appropriate. The post hoc multiple comparisons were performed to identify the differences between groups and the significance level was set at <0.017 (Bonferroni correction, 0.05/3). Repeated measures in linear mixed models were conducted to assess effects of medications on scores of HAMD, HAMA and QIDS before and after treatment. Variables included in the linear mixed models were age, gender and time. Because the data of mBDNF, proBDNF and M/P ratio did not satisfy normal distribution, we performed comparisons using Kruskal-Wallis test for independent samples among three groups, Mann-Whitney U test for multiple comparisons and Wilcoxon test for two related samples to compare the changes before and after treatment. Spearman rank correlation analysis was also conducted among mBDNF, proBDNF, M/P ratio and clinical characteristics. To determine the best model for differentiating BP from MDD at depressive episode, the discriminatory capacity of each model (plasma mBDNF, plasma proBDNF and M/P ratio) was analysed by calculating the area under the receiver operating characteristic (ROC) curve using logistic regression. The optimal cut-off from ROC curve analysis was determined under the Youden index criterion. Significance was set at P < 0.05.
Results
Demographic Data of Participants
A total of 105 participants were recruited, including 44 healthy controls, 37 MDD patients and 24 BP patients. There was no significant difference of demographic data in terms of age (F = 0.202, P = 0.140), marriage (χ 2 = 2.227, P = 0.694) and gender (χ 2 = 0.184, P = 0.912), but education years (F = 6.524, P = 0.002; Table 1).
Clinical Characteristics and Scale Scores
Significant difference was found in the comparison between MDD group and BP group in terms of episode numbers and total duration except age of first episode (P = 0.010, P = 0.001 and P = 0.190, respectively). There was no significant difference in terms of QIDS, YMRS and HAMA except HAMD between MDD and BP at baseline (P = 0.921, P = 0.726, P = 0.961 and P = 0.008, respectively). The healthy controls showed significant lower QIDS (1.82 ± 1.67) compared with MDD group and BP group (P = 0.000 and P = 0.000; respectively). All the linear mixed models comparing HAMD, HAMA and QIDS scores before and after medications included time as fixed factors in MDD group (P = 0.000, P = 0.000 and P = 0.000, respectively) and BP group (P = 0.000, P = 0.000 and P = 0.001, respectively; Table 2 and Supplementary Table S2).
Plasma mBDNF Levels, proBDNF Levels and M/P Ratio
At baseline, there was significant difference in terms of mBDNF levels among MDD group, BP group and healthy controls (P = 0.000; Table 3). Multiple comparisons were performed to analyse the difference of mBDNF levels among BP group, MDD group and healthy controls. BP group had lower plasma mBDNF levels than those in MDD group (269.17 ± 159.23 vs. 397.30 ± 104.81, P = 0.000) as well as those in healthy controls (269.17 ± 159.23 vs. 353.80 ± 138.67, P = 0.002). There was no significant difference between MDD group and healthy controls (397.30 ± 104.81 vs. 353.80 ± 138.67, P = 0.034).
There was no difference in terms of proBDNF levels among MDD group, BP group and healthy controls (P = 0.185; Table 3). Additionally, no significant difference between groups was found when the post hoc multiple comparisons was performed (BP vs. MDD 91.55 ± 62.06 vs. 69.04 ± 22.15, P = 0.223; BP vs. healthy controls 91.55 ± 62.06 vs. 92.13 ± 55.44, P = 0.852; MDD vs. healthy controls 69.04 ± 22.15 vs. 92.13 ± 55.44, P = 0.073; respectively).
There was a significant difference among MDD group, BP group and healthy controls in terms of the baseline M/P ratio (P = 0.000; Table 3). MDD group had higher baseline M/P ratio than those in BP group and healthy controls (6.12 ± 1.86 vs. 3.43 ± 1.86, P = 0.000; 6.12 ± 1.86 vs. 4.63 ± 2.70, P = 0.000; respectively). BP group showed no significant difference in terms of the baseline M/P ratio compared with healthy controls (3.43 ± 1.86 vs. 4.63 ± 2.70, P = 0.026).
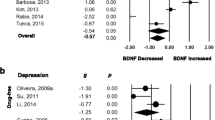
To determine the best model for discriminating BP in depressive episode, discriminatory capacity was analysed by calculating the area under the ROC curve using logistic regression. The areas of mBDNF, proBDNF and M/P ratio under the ROC curves were, respectively, 0.780 (95 % CI 0.638–0.922), 0.593 (95 % CI 0.434–0.752) and 0.858 (95 % CI 0.753–0.963; Fig. 1). Thus, the best model for discriminating BP was M/P ratio. The cut-point with optimal sensitivity and specificity for BP was then identified within the whole depressed patients. An optimal cut-off of M/P ratio was 4.316 which yielded sensitivity of 0.838 and specificity of 0.833.
Correlation Analysis
The results of Spearman rank correlation analysis showed negative association between proBDNF and age (r = −0.339, P = 0.040) as well as proBDNF and age of first onset (r = −0.524, P = 0.015) and positive association between M/P ratio and age of first onset(r = 0.556, P = 0.009) as well as M/P ratio and age(r = 0.360, P = 0.029) in MDD group. No other correlation was found among mBDNF, proBDNF, M/P ratio and clinical characteristics in MDD group and in BP group. (Table 4).
Changes After Antidepressants Treatment
Furthermore, we compared the alteration of mBDNF, proBDNF and M/P ratio after antidepressants treatment in 15 MDD patients. After treatment, plasma mBDNF levels (419.41 ± 129.71 vs. 213.96 ± 87.30, P = 0.001), plasma proBDNF levels (73.10 ± 17.32 vs. 66.56 ± 65.90, P = 0.023) and the M/P ratio (5.88 ± 1.78 vs. 4.26 ± 1.93, P = 0.041) were significantly changed (Fig. 2). In the comparison between healthy controls and MDD group after treatment, significant difference was found in terms of mBDNF, proBDNF but M/P ratio (P = 0.000, P = 0.008 and P = 0.889, respectively).
Plasma mBDNF, proBDNF and M/P changes during treatment in major depressive disorder. The plasma mBDNF levels were decreased (a Z = 3.181, P = 0.001). The plasma proBDNF levels were significantly changed (b Z = 2.272, P = 0.023). M/P ratio was decreased (c Z = 2.045, P = 0.041). mBDNF mature brain-derived neurotrophic factor, proBDNF precursor of brain-derived neurotrophic factor, M/P the ratio of mBDNF to proBDNF
Discussion
Recent meta-analyses demonstrated that BDNF is a biomarker for disease activity and successful treatment in mood disorders [11, 14, 20]. However, only few studies were performed to exam the diagnostic value of BDNF for BP and MDD. In our previous study, we found that BDNF was a biomarker for predicting BD in their first depressive episodes [25]. In the present study, we compared plasma mBDNF levels, plasma proBDNF levels and M/P ratio in both BP patients and MDD patients to further explore the diagnostic value of BDNF in mood disorders.
Some efforts have been done to explore the relationship of M/P ratio and BD, and the relationship of M/P ratio and MDD. Södersten et al. [35] observed that M/P ratio was significantly higher in mood stabilized BD patients. Yoshida et al. [36] found decreased serum levels of mBDNF and no difference of proBDNF in MDD patients, and Zhou et al. [37] reported higher serum proBDNF levels and lower mBDNF levels in MDD patients. However, it is still not known about the difference of M/P ratio between MDD patients and healthy controls as well as between MDD and BP. To the best of our knowledge, this is the first study to evaluate the diagnostic value of peripheral plasma mBDNF and proBDNF as well as M/P ratio as potential biomarkers for differentiating BP and MDD during acute depressive episode. The major findings of the present study indicated that M/P ratio compared with plasma mBDNF levels and plasma proBDNF levels was more sensitive for discriminating BP from acute depressive episode. M/P ratio was higher in MDD patients compared with BP patients at the acute phase. These results provided preliminary data for M/P ratio as a biomarker for differential diagnosis of BP.
Although BP and MDD share some similar symptom profiles, they are two distinct diseases [38]. Neuroimaging studies have shown that different activation of brain regions was found in BP and MDD [39]. Brain structural morphometry study showed distinct spatially distributed variations in cortical thickness and surface area in patients with BD and MDD [40]. And the dysfunctions in performing a moral valence decision task between MDD and BP were significantly different in left ventrolateral prefrontal cortex [41]. And the change of proBDNF and BDNF in different brain regions showed different directions at the same condition. Literature has reported that proBDNF levels in aggressive rats were increased in the midbrain and hippocampus but decreased in the frontal cortex [30]. Previous data have demonstrated different conversion rates of proBDNF to mBDNF in different regions of central nervous system. For example, Shirayama et al. [42] recently found that learned helplessness rats showed a reduction of BDNF and an increase of proBDNF in the medial prefrontal cortex; meanwhile, they also found an increase of BDNF and a reduction of proBDNF in the nucleus accumbens. Thus, in the present study, the different M/P ratio between MDD and BP demonstrated different conversion rates of proBDNF to mBDNF in peripheral blood plasma of these two psychiatric illnesses. Whether the variation of M/P ratio in BP and MDD was due to the activation of brain is still unknown.
It has been reported that proBDNF cleavage may be inhibited by some factors, such as early poor environment, PC7 (a member of the proprotein convertase family which are involved in the cleavage of secretory precursors) and acute stress [28, 31, 43]. MMP-9 as an important extracellular protease is also implicated in the conversion of proBDNF to mBDNF. MMP-9 was reported to correlate positively and significantly with mBDNF in BD patients [35]. However, there were also studies found no alteration of MMP-9 in BD and MDD [36, 44]. Thus, whether the difference of M/P ratio in BP and MDD was due to the influence of MMP-9 should be further investigated.
Fernandes et al. [24] have reported serum BDNF levels in depressive BD patients were lower compared to MDD patients and controls, but no difference between the MDD patients and controls. In this study, we found the mBDNF levels were lower in BP group compared with healthy controls and MDD and no differences between MDD and healthy controls. Up to now, only Södersten et al. [35] reported increased serum levels of mBDNF in mood-stabilized BD patients compared with healthy controls. One possible explanation for these inconsistent results is that most BD patients in their study have received medication, such as antidepressants, antipsychotics, lithium and antiepileptics. It has been reported that medication might enhance mBDNF levels by promoting the conversion of proBDNF to mBDNF [45]. Another possible reason is that the mood states of patients in their study were stabilized, but patients in the present study were in acute episodes. Furthermore, one important reason should be noticed is that the different results among the different studies of BDNF changes with pharmacological intervention can be due to differences of BDNF in serum and plasma. It has been reported that plasma appeared to be more sensitive to detect earlier changes in BDNF than serum [11, 14, 20]. In contrast to previous findings conducted by Yoshimura et al. in 2014 and 2012 [34, 36], we did not find any significant change of mBDNF in MDD patients compared with healthy controls, which probably would have occurred if we amplified the sample.
We found that plasma levels of proBDNF did not differ between any two groups. The differences of proBDNF in MDD and healthy controls were consistent with previous studies [34, 36]. In contrast to our results, significant difference was found between MDD patients and healthy controls in the study conducted by Zhou et al. [37]. And Södersten et al. [35] reported lower serum levels of proBDNF in mood-stabilized BD patients compared with controls. Consideration of these inconsistent findings leads to the further investigation of plasma proBDNF levels in BP patients and MDD patients.
Another important aim of this study is to evaluate the influence of antidepressant on mBDNF, proBDNF and M/P ratio. Our results have demonstrated that plasma mBDNF levels, plasma proBDNF levels and M/P ratio were significantly altered after a 12-week antidepressant therapy and M/P ratio was restored to normal levels. Yoshimura et al. [34] have reported that serum proBDNF/BDNF did not change after 4 weeks of treatment with fluvoxamine in MDD patients. It is important to note that serum and plasma levels are likely not comparable and the latter may be more potential [11]. Recently, Zhang et al. [46] found that electroconvulsive therapy (ECT) could upregulate proBDNF/mBDNF ratio in depressive rats. In consideration of anti-depression effects of ECT, our results may confirm this finding and provide further evidence for psychopharmacological mechanism of antidepressants. Taken together, these findings may suggest that the conversion of proBDNF to mBDNF may be influenced by antidepressant treatment, which may be manifested after 12 weeks of treatment. And these findings also suggested that M/P ratio like peripheral blood BDNF may be sensitive in the evaluation of treatment outcomes [47, 48].
The association of BDNF and recurrent MDD as well as suicide was reported in the previous study [17]. In the present study, we found the negative association between proBDNF and age of onset, and positive association between M/P ratio and age of onset. The present results meant the earlier onset, the higher plasma proBDNF levels and the lower M/P ratio. Further investigation will be needed to confirm these findings in future studies.
Some limitations in this study should be considered. First, we did not explore the effect of medication on mBDNF and proBDNF in BP patients due to only a few participants in each treated subgroup. Further studies will be needed to describe mBDNF and proBDNF changes in BP patients after treatment. Second, due to the small size of this study, further investigation of large samples is needed to validate our results. Third, previous studies have found different BDNF levels in male and female [49, 50]. Tang et al. [51] reported that the M/P ratio differed in a sex-specific manner in zebra finches. In the present study, there was no gender stratification analysis due to small sample settings. Finally, in the present study, we did not consider the association of genetic variation in the gene encoding BDNF and mBDNF/proBDNF levels as well as the association of mBDNF/proBDNF levels and their respective receptors. Our previous studies have reported that genetic interactions between genetic variation in the gene encoding BDNF and its receptor in development of treatment-resistant depression [52].
In conclusion, we found lower plasma mBDNF levels and lower M/P ratio in BP compared with MDD. These findings further support the idea that BDNF has a potential role in differentiating BP from MDD. The contributions of our study are to provide preliminary data for M/P ratio as a potential biomarker for discriminating BP among patients in depressive episodes and to support that the M/P ratio may be a state marker of MDD which can be restored to normal levels by antidepressants treatment. In view of limitations in the present study, further investigation is required to make any definitive determination.
References
Organization WH (2001) The World Health Report 2001: Mental health: new understanding, new hope. World Health Organization,
Kamat SA, Rajagopalan K, Pethick N, et al. (2008) Prevalence and humanistic impact of potential misdiagnosis of bipolar disorder among patients with major depressive disorder in a commercially insured population. J Manag Care Pharm 14(7):631–642
Singh T, Rajput M (2006) Misdiagnosis of bipolar disorder. Psychiatry (Edgmont) 3(10):57–63
Hirschfeld RM (2014) Differential diagnosis of bipolar disorder and major depressive disorder. J Affect Disord 169(Suppl 1):S12–S16
Markham A, Bains R, Franklin P, et al. (2014) Changes in mitochondrial function are pivotal in neurodegenerative and psychiatric disorders: how important is BDNF? Br J Pharmacol 171(8):2206–2229
Lu B, Nagappan G, Lu Y (2014) BDNF and synaptic plasticity, cognitive function, and dysfunction. Handb Exp Pharmacol 220:223–250
Ikegame T, Bundo M, Murata Y, et al. (2013) DNA methylation of the BDNF gene and its relevance to psychiatric disorders. J Hum Genet 58(7):434–438
Valvassori SS, Arent CO, Steckert AV, et al. (2014) Intracerebral administration of BDNF protects rat brain against oxidative stress induced by Ouabain in an animal model of mania. Mol Neurobiol 52(1):353–362
Koike H, Fukumoto K, Iijima M, et al. (2013) Role of BDNF/TrkB signaling in antidepressant-like effects of a group II metabotropic glutamate receptor antagonist in animal models of depression. Behav Brain Res 238:48–52
Molendijk ML, Spinhoven P, Polak M, et al. (2014) Serum BDNF concentrations as peripheral manifestations of depression: evidence from a systematic review and meta-analyses on 179 associations (N = 9484). Mol Psychiatry 19(7):791–800
Fernandes BS, Molendijk ML, Kohler CA, et al. (2015) Peripheral brain-derived neurotrophic factor (BDNF) as a biomarker in bipolar disorder: a meta-analysis of 52 studies. BMC medicine 13:289
Gonzalez-Castro TB, Nicolini H, Lanzagorta N, et al. (2015) The role of brain-derived neurotrophic factor (BDNF) Val66Met genetic polymorphism in bipolar disorder: a case-control study, comorbidities, and meta-analysis of 16,786 subjects. Bipolar Disord 17(1):27–38
Verhagen M, van der Meij A, van Deurzen PA, et al. (2010) Meta-analysis of the BDNF Val66Met polymorphism in major depressive disorder: effects of gender and ethnicity. Mol Psychiatry 15(3):260–271
Fernandes BS, Berk M, Turck CW, et al. (2014) Decreased peripheral brain-derived neurotrophic factor levels are a biomarker of disease activity in major psychiatric disorders: a comparative meta-analysis. Mol Psychiatry 19(7):750–751
Piccinni A, Veltri A, Costanzo D, et al. (2015) Decreased plasma levels of brain-derived neurotrophic factor (BDNF) during mixed episodes of bipolar disorder. J Affect Disord 171:167–170
Rabie MA, Mohsen M, Ibrahim M, et al. (2014) Serum level of brain derived neurotrophic factor (BDNF) among patients with bipolar disorder. J Affect Disord 162:67–72
Lee BH, Kim H, Park SH, et al. (2007) Decreased plasma BDNF level in depressive patients. J Affect Disord 101(1–3):239–244
Lee BH, Kim YK (2009) Reduced platelet BDNF level in patients with major depression. Prog Neuro-Psychopharmacol Biol Psychiatry 33(5):849–853
Hong W, Fan J, Yuan C, et al. (2014) Significantly decreased mRNA levels of BDNF and MEK1 genes in treatment-resistant depression. Neuroreport 25(10):753–755
Polyakova M, Stuke K, Schuemberg K, et al. (2015) BDNF as a biomarker for successful treatment of mood disorders: a systematic & quantitative meta-analysis. J Affect Disord 174:432–440
Fernandes BS, Gama CS, Cereser KM, et al. (2011) Brain-derived neurotrophic factor as a state-marker of mood episodes in bipolar disorders: a systematic review and meta-regression analysis. J Psychiatr Res 45(8):995–1004
Tunca Z, Ozerdem A, Ceylan D, et al. (2014) Alterations in BDNF (brain derived neurotrophic factor) and GDNF (glial cell line-derived neurotrophic factor) serum levels in bipolar disorder: the role of lithium. J Affect Disord 166:193–200
Sen S, Duman R, Sanacora G (2008) Serum brain-derived neurotrophic factor, depression, and antidepressant medications: meta-analyses and implications. Biol Psychiatry 64(6):527–532
Fernandes BS, Gama CS, Kauer-Sant’Anna M, et al. (2009) Serum brain-derived neurotrophic factor in bipolar and unipolar depression: a potential adjunctive tool for differential diagnosis. J Psychiatr Res 43(15):1200–1204
Li Z, Zhang C, Fan J, et al. (2014) Brain-derived neurotrophic factor levels and bipolar disorder in patients in their first depressive episode: 3-year prospective longitudinal study. Br J Psychiatry 205(1):29–35
Woo NH, Teng HK, Siao CJ, et al. (2005) Activation of p75NTR by proBDNF facilitates hippocampal long-term depression. Nat Neurosci 8(8):1069–1077
Koshimizu H, Kiyosue K, Hara T, et al. (2009) Multiple functions of precursor BDNF to CNS neurons: negative regulation of neurite growth, spine formation and cell survival. Molecular brain 2:27
Cao W, Duan J, Wang X, et al. (2014) Early enriched environment induces an increased conversion of proBDNF to BDNF in the adult rat’s hippocampus. Behav Brain Res 265:76–83
Ethell IM, Ethell DW (2007) Matrix metalloproteinases in brain development and remodeling: synaptic functions and targets. J Neurosci Res 85(13):2813–2823
Ilchibaeva TV, Kondaurova EM, Tsybko AS, et al. (2015) Brain-derived neurotrophic factor (BDNF) and its precursor (proBDNF) in genetically defined fear-induced aggression. Behav Brain Res 290:45–50
Tognoli C, Rossi F, Di Cola F, et al. (2010) Acute stress alters transcript expression pattern and reduces processing of proBDNF to mature BDNF in Dicentrarchus labrax. BMC Neurosci 11:4
Yoshida T, Ishikawa M, Iyo M, et al. (2012) Serum levels of mature brain-derived neurotrophic factor (BDNF) and its precursor proBDNF in healthy subjects. The Open Clinical Chemistry Journal 5:7–12
Lim Y, Zhong JH, Zhou XF (2015) Development of mature BDNF-specific sandwich ELISA. J Neurochem 134(1):75–85
Yoshimura R, Kishi T, Hori H, et al. (2014) Serum proBDNF/BDNF and response to fluvoxamine in drug-naive first-episode major depressive disorder patients. Ann General Psychiatry 13:19
Sodersten K, Palsson E, Ishima T, et al. (2014) Abnormality in serum levels of mature brain-derived neurotrophic factor (BDNF) and its precursor proBDNF in mood-stabilized patients with bipolar disorder: a study of two independent cohorts. J Affect Disord 160:1–9
Yoshida T, Ishikawa M, Niitsu T, et al. (2012) Decreased serum levels of mature brain-derived neurotrophic factor (BDNF), but not its precursor proBDNF, in patients with major depressive disorder. PLoS One 7(8):e42676
Zhou L, Xiong J, Lim Y, et al. (2013) Upregulation of blood proBDNF and its receptors in major depression. J Affect Disord 150(3):776–784
Cuellar AK, Johnson SL, Winters R (2005) Distinctions between bipolar and unipolar depression. Clin Psychol Rev 25(3):307–339
Redlich R, Dohm K, Grotegerd D, et al. (2015) Reward processing in unipolar and bipolar depression: a functional MRI study. Neuropsychopharmacology 40(11):2623–2631
Fung G, Deng Y, Zhao Q, et al. (2015) Distinguishing bipolar and major depressive disorders by brain structural morphometry: a pilot study. BMC psychiatry 15:298
Radaelli D, Dallaspezia S, Poletti S, et al. (2013) Different neural responses to a moral valence decision task in unipolar and bipolar depression. ISRN psychiatry 2013:568617
Shirayama Y, Yang C, Zhang JC, et al. (2015) Alterations in brain-derived neurotrophic factor (BDNF) and its precursor proBDNF in the brain regions of a learned helplessness rat model and the antidepressant effects of a TrkB agonist and antagonist. Eur Neuropsychopharmacol 25(12):2449–2458
Wetsel WC, Rodriguiz RM, Guillemot J, et al. (2013) Disruption of the expression of the proprotein convertase PC7 reduces BDNF production and affects learning and memory in mice. Proc Natl Acad Sci USA 110(43):17362–17367
Chiarani F, Fries GR, Stertz L, et al. (2013) Expression of matrix metalloproteinases in patients with bipolar disorder. Rev Bras Psiquiatr 35(4):375–379
Tang M, Jiang P, Li H, et al. (2015) Antidepressant-like effect of n-3 PUFAs in CUMS rats: role of tPA/PAI-1 system. Physiol Behav 139:210–215
Zhang F, Luo J, Min S, et al. (2016) Propofol alleviates electroconvulsive shock-induced memory impairment by modulating proBDNF/mBDNF ratio in depressive rats. Brain Res 1642:43–50
Fornaro M, Escelsior A, Rocchi G, et al. (2015) BDNF plasma levels variations in major depressed patients receiving duloxetine. Neurological sciences: official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology 36(5):729–734
Mikoteit T, Beck J, Eckert A, et al. (2014) High baseline BDNF serum levels and early psychopathological improvement are predictive of treatment outcome in major depression. Psychopharmacology 231(15):2955–2965
Kreinin A, Lisson S, Nesher E, et al. (2015) Blood BDNF level is gender specific in severe depression. PLoS One 10(5):e0127643
Choi S, Han KM, Won E, et al. (2014) Association of brain-derived neurotrophic factor DNA methylation and reduced white matter integrity in the anterior corona radiata in major depression. J Affect Disord 172:74–80
Tang YP, Wade J (2013) Developmental changes in BDNF protein in the song control nuclei of zebra finches. Neuroscience 250:578–587
Li Z, Zhang Y, Wang Z, et al. (2013) The role of BDNF, NTRK2 gene and their interaction in development of treatment-resistant depression: data from multicenter, prospective, longitudinal clinic practice. J Psychiatr Res 47(1):8–14
Acknowledgments
This work was supported by the National Natural Science Foundation of China (91232719, 81201056, 81301159), Shanghai Health Bureau Excellent Young Talents Program (XYQ2011014), Shanghai Committee of Science and Technology (12401906200), the National Key Clinical Disciplines at Shanghai Mental Health Centre (OMA-MH, 2011-873), Shanghai Clinical Centre for Mental Disorders (2014) and the “12th Five-year Plan” of National Key Technologies R&D Program (2012BAI01B04, Ministry of Science and Technology of China). We thank those who assisted with study recruitment: Ruizhi Mao, Lvchun Cui, Chenglei Wang and Jingjing Xu.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors of this paper do not have any commercial associations that might pose a conflict of interest in connection with this manuscript.
Electronic supplementary material
Supplementary Table S1
(DOCX 18 kb)
Supplementary Table S2
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Zhao, G., Zhang, C., Chen, J. et al. Ratio of mBDNF to proBDNF for Differential Diagnosis of Major Depressive Disorder and Bipolar Depression. Mol Neurobiol 54, 5573–5582 (2017). https://doi.org/10.1007/s12035-016-0098-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-0098-6