Abstract
Immune responses and inflammation play an important role in the pathogenesis of ischemic stroke. We therefore evaluated the 6-month prognostic value of early measurement of serum neopterin levels, a marker of inflammation and immune system activation, in Chinese patients with acute ischemic stroke (AIS). Consecutive AIS patients admitted to the emergency department were identified. Clinical information was collected. Serum concentration of neopterin and NIH stroke scale (NIHSS) were measured at the time of admission. Functional outcome was measured by modified Rankin scale (mRS) 6 months after admission. Multivariate analyses were performed using logistic regression models. During the inclusion period, 312 patients with first-ever AIS were included and 290 completed follow-up. The results indicated that the serum neopterin levels were significantly (P < 0.0001) higher in acutely ischemic stroke patients as compared to normal controls. Neopterin was an independent prognostic marker of 6-month functional outcome and death [odds ratio (OR) 4.33 (1.83–10.32) and 6.68 (2.44–12.13), respectively, P < 0.0001 for both, adjusted for NIHSS, other predictors and vascular risk factors] in patients with AIS. Neopterin improved the area under the receiver operating characteristic curve of the NHISS score for functional outcome from 0.75 (95 % CI 0.69–0.83) to 0.85 (95 % CI 0.79–0.91; P < 0.001) and for mortality from 0.76 (95 % CI 0.68–0.85) to 0.87 (95 % CI 0.81–0.94; P < 0.001). Serum neopterin is a useful, independent tool to predict functional outcome and mortality 6 months after stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is the second most common cause of death worldwide and a major cause of acquired disability in adults [1]. Similarly, stroke is the second most common cause of death and leading cause of adult disability in China. China has 2.5 million new stroke cases each year and 7.5 million stroke survivors [2]. Mortality after 1 year ranges between 21 and 27 %; 15 to 30 % of survivors are permanently disabled [3]. An early risk assessment with estimate of the severity of disease and prognosis is pivotal for optimized care and allocation of health care resources to improve outcome [4].
Systemic and local immune responses have important roles in causing stroke and are implicated in the primary and secondary progression of ischemic lesions, as well as in repair, recovery, and overall outcome after a stroke [1]. In addition, inflammation also plays an important role in the pathogenesis of ischemic stroke and other forms of ischemic brain injury [5]. Experimentally and clinically, the brain responds to ischemic injury with an acute and prolonged inflammatory process, characterized by rapid activation of resident cells (mainly microglia), production of proinflammatory mediators, and infiltration of various types of inflammatory cells (including neutrophils, different subtypes of T cells, monocyte/macrophages, and other cells) into the ischemic brain tissue [6].
Neopterin is a marker of peripheral immune system activation [7] and inflammation [8]. Neopterin is one of the important indicators for the cellular immune response, which is released by T cells in response to proinflammatory cytokines, such as IFNγ and IL-2 [9]. Thus, increased serum neopterin is a sensitive marker of activation of cell-mediated immunity and T cell activation [10]. Increased neopterin concentrations in body fluids of patients are observed during diseases with activated cellular (=TH1-type) immune response such as allograft rejection, virus infections, autoimmune disorders, or malignant tumors but also in neurodegenerative diseases or during pregnancy [11]. Similarly, measurement of neopterin levels may also help follow the evolution of specific inflammatory conditions (e.g., viral infection, renal transplant rejection, systemic inflammatory diseases, nephritic syndrome, and autoimmune diseases) [12].
In previous studies, increased plasma neopterin concentrations have been observed in patients with acute coronary disease (CAD) [13] and acute ischemic stroke (AIS) [14]. Ganz et al. [15] reported that in patients with recent stroke or TIA and no known coronary heart disease (CHD), neopterin predict the risk of future CHD events and improve risk prediction over traditional risk factors. Early increases in serum level of neopterin have recently been shown to predict 90-day unfavorable clinical outcome in patients after AIS [14]. However, the relationship between activation of neopterin and other markers with the long-term clinical outcome of stroke has not yet been studied. Thus, the primary aim of our prospective cohort study was to test the 6-month prognostic value of early measurement of serum neopterin levels in Chinese patients with AIS.
Subjects and Methods
Patients and Study Design
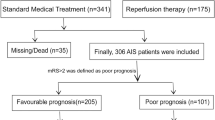
We conducted a prospective cohort study at the emergency department of the Affiliated Hospital of Weifang Medical College. From December 2011 to November 2013, all Chinese patients with first-ever AIS were included. Patients were eligible for inclusion if they were admitted to the emergency department with an AIS defined according to the World Health Organization criteria [16] and with symptom onset within 24 h. We excluded patients with intracranial hemorrhage, a history of recent surgery or trauma during the preceding 2 months, renal insufficiency (creatinine >1.5 mg/dl), malignancy, febrile disorders, acute or chronic inflammatory disease (assessed by history report and physical examination), febrile disorders, autoimmune diseases, severe edema or a prior myocardial infarction onset <3 months, as well as those with a history of valvular heart disease and/or intracardiac thrombus.
In our study, 200 age- and gender-matched healthy volunteers were assigned to the control group. The median age of normal included in this study was 71 years (IQR 64–79), and 47 % were women. A detailed medical history was taken, and clinical and laboratory examinations were performed on all participants in both groups. The study was approved by the ethics committee of the Affiliated Hospital of Weifang Medical College. The patients or their relatives gave written informed consent prior to entering the study.
Clinical Variables and Neuroimaging
The following clinical and demographical data were taken: age, gender, stroke etiology, blood pressure, leukocyte count, and presence of risk factors (i.e., smoking history; hypercholesterolemia; history of hypertension, diabetes mellitus, previous ischemic stroke, or transient ischemic attack, respectively; positive family history for myocardial infarction, stroke, or transient ischemic attack). Stroke cause was determined according to the criteria of the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification [17], which distinguishes large-artery arteriosclerosis, small-artery occlusion, cardioembolism, other causative factor, and undetermined causative factor. The clinical stroke syndrome was determined by applying the criteria of the Oxfordshire Community Stroke Project: total anterior circulation syndrome (TACS), partial anterior circulation syndrome (PACS), lacunar syndrome (LACS), and posterior circulation syndrome (POCS) [18]. The National Institutes of Health Stroke Scale (NIHSS) score was assessed on admission (with greater scores indicating increasing severity) [19].
Brain imaging (either CT or MRI) was performed routinely within 0 to 24 h after admission. Diagnosis of stroke was based on the results of strict neurological examination (CT, MRI, or both) according to the International Classification of Diseases, ninth revision. CCT was performed in all patients on admission mainly to exclude intracranial hemorrhage. Thereafter, MRI was performed using a stroke protocol, including T1-, T2-, and diffusion-weighted imaging (DWI) sequences, and a magnetic resonance angiography. In those patients, DWI lesion volumes were determined by one experienced neurologist unaware of the clinical and laboratory results. The infarct volume was calculated by using the formula 0.5 × a × b × c (where a is the maximal longitudinal diameter, b is the maximal transverse diameter perpendicular to a, and c is the number of 10-mm slices containing infarct) [20].
End Points and Follow-up
Functional outcome was obtained on 6 months according to the modified Rankin Scale (mRS) [21] blinded to neopterin levels. The primary end point of this study was favorable functional outcome of stroke patients after 6 months from baseline, defined as a mRS score of 0 to 2 points. Secondary end point in stroke patients was death or withdrawn from any cause within a 6-month follow-up. Outcome assessment was performed by one trained medical staff blinded to neopterin levels with a structured follow-up telephone interview with the patient or, if not possible, with the relative.
Blood Collection and Quantification
For the purpose of this study, blood samples of patients who were admitted to hospital were drawn from the antecubital vein at the first morning after admission (within 0–6 [n = 75], 6–12 [n = 90], 12–24 [n = 55], and 24–48 h [n = 70] from symptom onset). After centrifugation, serum of the samples were immediately stored at −80 °C before assay. Biomarker concentrations were measured in a central laboratory by investigators blinded to the clinical outcome and neuroimaging findings. Serum high-sensitivity C-reactive protein (Hs-CRP), homocysteine (HCY), white blood cells (WBC), and glucose levels were measured at admission using standard laboratory methods. Serum neopterin levels were measured using a human ELISA kit (Labor Diagnostika Nord GmbH & Co. KG). The results were expressed as nmol/L. The intra- and inter-assay coefficients of variation were 3.4–4.9 and 3.9–5.5 %, respectively. The median value of morning serum neopterin level in our normal cases is 4.6 nmol/L. The median in healthy individuals using this modification was in the range of the reported by another study (5.3 nmol/L in healthy Caucasians) [22]. For all measurements, levels that were not detectable were considered to have a value equal to the lower limit of detection of the assay.
Statistical Analysis
Results are expressed as percentages for categorical variables and as means (standard deviation (SD)) and medians (interquartile ranges (IQRs)) for the continuous variables, depending on the normal or nonnormal distribution of data. Shapiro–Wilk tests were used for normal distribution test. Proportions were compared using the chi-squared test. Two-group comparison of not normally distributed data was performed using Mann–Whitney U test, and a two-tailed Student’s unpaired t test was used for normally distributed continuous variables. Spearman’s rank correlation was used for bivariate correlations. In addition, associations between neopterin and NIHSS score and infarct volume were also assessed using ordered logistic regression models in multivariate adjustment with possible confounders.
To investigate whether neopterin allows predicting of both functional outcome and death in stroke, different statistical methods were used. First, the relation of neopterin with the two end points was investigated with the use of logistic regression models. Therefore, common logarithmic transformation (i.e., log) was performed to obtain normal distribution for skewed variables (i.e., neopterin concentrations). We used crude models and multivariate models adjusted for all significant outcome predictors and report odds ratios (ORs). For multivariate analysis, we included confounders, known risk factors, and other outcome predictors as assessed in univariate analysis. Note that the OR corresponds to a one-unit increase in the explanatory variable; for the log-transformed neopterin values, this corresponds to a tenfold increase.
Second, we compared different prognostic risk scores from different predictive models by calculating receiver operating characteristic curves (ROC) analysis. ROC was used to test the overall prognostic accuracy of neopterin, age, the NIHSS, HS-CRP, and HCY, and the results were reported as area under the curve (AUC). To test whether the neopterin levels improves score performance, we considered the nested models with NIHSS and neopterin as compared with those markers alone.
Finally, in order to study the ability of neopterin for mortality prediction, we calculated Kaplan–Meier survival curves and compared by the log-rank test. We reported hazard ratios (HRs). All statistical analyses were performed with SPSS for Windows, version 20.0 (SPSS Inc., Chicago, IL, USA) and STATA 9.2 (Stata Corp, College Station, TX), R version 2.8.1. Statistical significance was defined as P < 0.05.
Results
Patient Characteristics
From 463 screened patients, AIS was diagnosed in 312 patients (48 with transient ischemic attack, 39 with onset of symptoms >24 h, 19 with hemorrhagic stroke, 18 without informed consent, 10 with epileptic seizures, 10 with systemic infections, and 7 with malignant tumor were not analyzed) and 290 completed 6-month follow-up (14 lost to follow-up and 8 withdraw). The baseline characteristics of the 290 patients presenting with AIS are described in Table 1. The median age of patients included in this study was 71 years (IQR 64–79), and 46.6 % were women. The median NIHSS score on admission was 8 points (IQR 5–13). The median time from stroke onset to inclusion in the study was 7.2 h (IQR 3.8–16.6). In addition, the number of tissue plasminogen activator-treated patients was 70 (24.1 %).
Main Results
The results indicated that the neopterin serum levels were significantly (P < 0.0001) higher in AIS patients as compared to normal controls (17.6 nmol/L [IQR 13.3–22.5] vs 4.6 nmol/L [IQR 3.0–7.7]). There was a positive correlation between levels of neopterin and the NIHSS (r = 0.374, P < 0.0001). There was still a significant positive trend between serum neopterin levels and NIHSS scores (P = 0.006), using ordered logistic regression after multivariate adjustment for possible confounders. In addition, there was a significant, albeit weak, positive correlation between neopterin and Hs-CRP (r = 0.166, P = 0.011). In addition, in patients for whom MRI data were available (n = 183), there was a positive correlation between levels of neopterin and the infarct volume (r = 0.426, P < 0.0001). Statistical analysis revealed no influence of age, sex, BMI, time from stroke onset to blood sampling, etiological subtype, lesion location, WBC, and HCY on neopterin in stroke patients (P > 0.05, respectively).
Neopterin and 6-Month Functional Outcome
In the 104 patients with an unfavorable functional outcome, serum neopterin levels were higher compared with those in patients with a favorable outcome [23.0 nmol/L (IQR 19.7–26.5) vs 14.6 nmol/L (IQR 12.4–19.1), P < 0.0001; Fig. 1). In univariate logistic regression analysis, we calculated the ORs of log-transformed neopterin levels as compared with the NIHSS score and other risk factors as presented in Table 2. With an unadjusted OR of 11.25 (95 % CI 2.33–28.77), neopterin had a strong association with unfavorable functional outcome. After adjusting for all other significant outcome predictors, neopterin remained an independent outcome predictor with an adjusted OR of 4.33 (95 % CI 1.53–10.32). In addition, age, the NIHSS score, glucose, Hs-CRP, and HCY remained significant outcome predictors, unlike all others assessed (Table 2). In the subgroup of patients (n = 183) in whom MRI evaluations were performed, neopterin was an independent unfavorable outcome indicator with an OR of 7.12 (95 % CI 3.34–13.13; P < 0.001) after adjustment for both lesion size (OR 1.07; 95 % CI 1.01–1.24; P = 0.012) and the NIHSS score (OR 1.17; 95 % CI 1.06–1.28; P = 0.006).
Distribution of serum neopterin levels in stroke patients with favorable outcomes and unfavorable outcomes. A favorable functional outcome was defined as a mRS score of 0 to 2 points, while unfavorable outcome was defined as 3–6 points. All data are medians and interquartile ranges (IQR). P values refer to Mann–Whitney U tests for differences between groups
Based on the ROC curve, the optimal cutoff value of serum neopterin levels as a mortality indicator was estimated to be 19.5 nmol/L, which yielded a sensitivity of 81.2 % and a specificity of 76.7 %, with the area under the curve at 0.85 (95 % CI 0.79–0.91). With an AUC of 0.85, neopterin showed a significantly greater discriminatory ability as compared with Hs-CRP (AUC 0.65; 95 % CI 0.57–0.73; P < 0.0001), age (AUC 0.64; 95 % CI 0.53–0.73; P < 0.0001), and NIHSS score (AUC 0.75; 95 % CI 0.69–0.83; P < 0.001) (Table 3). Interestingly, neopterin improved the NIHSS score (AUC of the combined model 0.90; 95 % CI 0.81–0.96; P < 0.001). This improvement was stable in an internal fivefold cross-validation that resulted in an average AUC (standard error) of 0.75 (0.036) for the NIHSS and 0.90 (0.021) for the combined model, corresponding to a difference of 0.15 (0.015). Moreover, a model combining neopterin level, age, Hs-CRP, HCY, and the NIHSS score showed an AUC of 0.94 (95 % CI 0.85–0.98), which was greater than all predictors alone (P < 0.001).
Neopterin and 6-Month Mortality
At 6 months, 47 patients (16.2 %) had died. Nonsurvivors had significantly higher neopterin levels than survivors [23.0 nmol/L (IQR 19.7–26.5) vs 14.6 nmol/L (IQR 12.4–19.1), P < 0.0001; Fig. 2]. In univariate logistic regression analysis, we calculated the ORs of log-transformed neopterin levels as compared with the NIHSS score and other risk factors as presented in Table 2. With an unadjusted OR of 13.22 (95 % CI 2.01–37.28), neopterin level was an independent predictor for mortality. After adjusting for all other significant outcome predictors, neopterin remained an independent mortality predictor with an adjusted OR of 6.68 (95 % CI 2.44–12.13). In addition, age, the NIHSS score, Hs-CRP, and HCY remained significant outcome predictors, unlike all others assessed (Table 2). In the subgroup of patients (n = 183) in whom MRI evaluations were performed, neopterin was an independent mortality predictor with an OR of 8.27 (95 % CI 2.02–18.27; P < 0.001) after adjustment for both lesion size (OR 1.03; 95 % CI 1.01–1.06; P = 0.006) and the NIHSS score (OR 1.15; 95 % CI 1.05–1.27; P = 0.008).
Similarly, based on the ROC curve, the optimal cutoff value of serum neopterin levels as an mortality indicator was estimated to be 20.0 nmol/L, which yielded a sensitivity of 84.3 % and a specificity of 81.8 %, with the area under the curve at 0.87 (95 % CI 0.81–0.94). The combination of neopterin level and the NIHSS score had a higher discriminatory accuracy (AUC 0.94; 95 % CI 0.87–0.98) than the NIHSS score alone (P < 0.001). Again, this improvement was stable in an internal fivefold cross-validation that resulted in an average AUC (standard error) of 0.76 (0.040) for the NIHSS and 0.94 (0.021) for the combined model, corresponding to a difference of 0.18 (0.019). In addition, the combination of neopterin level, age, Hs-CRP, HCY, and the NIHSS score showed the greatest accuracy (AUC 0.96; 95 % CI 0.92–0.99), greater than all individual parameters alone (P < 0.01) (17.6 (13.3–22.5)).
The time to death was analyzed by Kaplan–Meier survival curves based on serum neopterin levels. Patients in the upper two quartiles (neopterin >22.5 nmol/L and between 17.6 and 22.5 nmol/L) had a higher risk of death compared to patients with neopterin levels in the lower two quartiles (neopterin <13.3 nmol/L and between 13.3 and17.6 nmol/L; P < 0.0001, log-rank test; Fig. 3). Patients with upper two quartiles’ serum neopterin levels (neopterin >22.5 nmol/L and between 17.6 and 22.5 nmol/L) had a significantly shorter mean survival time (5.01 vs 5.96 months; P < 0.0001) than those with lower two quartiles’ serum neopterin levels (neopterin <13.3 nmol/L and between 13.3 and 17.6 nmol/L).
Kaplan–Meier survival based on neopterin levels. Time to death was analyzed by Kaplan–Meier curves based on neopterin levels. Patients with upper two quartile serum neopterin levels had a significantly shorter mean survival time (5.01 vs 5.96 months; P < 0.0001) than those with lower two quartile serum neopterin levels
Discussion
Neopterin, a pteridine mainly synthesized by activated macrophages, is a marker of inflammation, immune system activation and an active participant in cardiovascular disease [23]. In this study, we firstly assessed the serum neopterin levels at admission with regard to their accuracy to predict functional outcome and mortality in patients with AIS within 6 months in Chinese sample. Our main finding was that neopterin is an independent prognostic marker of functional outcome and death in patients with AIS and adds significant additional predictive information to the clinical score of the NIHSS. We also demonstrated that neopterin levels increased with lesion size, neurological deficit (assessed by the NIHSS), and reflecting the severity of the stroke. The best validated clinical prognostic models are probably not accurate enough to predict outcome in individual patients with stroke. It seems that this combined model (neopterin and NIHSS score) may provide additional general prognostic information.
Serum inflammatory markers had been reported to be associated with short-tem outcomes [24] and long-term mortality [25] in patients with stroke. Whiteley et al. [26] reported that raised markers of the acute inflammatory response after stroke are associated with poor outcomes. However, the addition of these markers to a previously validated stroke prognostic model did not improve the prediction of poor outcome. In our study, we found that the serum level of neopterin, an inflammatory cytokine, was an independent prognostic marker of functional outcome in patients with AIS, which was supported by Lin et al. [14]. One study showed that the serum level of neopterin was positively correlated with the severity of coronary artery disease [27]. Kaski et al. [28] found that increased neopterin levels were an independent predictor of 180-day adverse cardiac events in Mediterranean patients with non-ST elevation acute coronary syndromes. Grammer et al. [29] found neopterin to be an independent predictor for both all-cause and cardiovascular mortality in patients with and without coronary artery disease.
Inflammation participates in the mechanisms of cerebral injury. In our study, we found a weak but significant positive correlation between neopterin and Hs-CRP. High Hs-CRP and neopterin levels could both be a sign of an inflammatory state. In epidemiological studies elevated Hs-CRP levels are consistently associated with atherosclerosis and vascular disease [30], and we did indeed observe significantly elevated Hs-CRP levels were corrected with unfavorable outcomes. However, the relationship between neopterin levels and function outcomes persisted on additional adjustment for Hs-CRP, which indicates that Hs-CRP and neopterin may carry different types of information as markers of inflammation.
Whether higher circulating neopterin level is an accelerator or only is a predictor marker of AIS remains uncertain. It is important to discuss whether neopterin in AIS patients have pathological roles or just was as indicator of oxidative stress or inflammation. Neopterin not only may be a marker for clinical outcome but could also play a pathogenic role in stroke. Firstly, this molecule is produced mainly by activated macrophages, which have been shown to play a key part in atheromatous plaque disruption. Inflammation plays an important role in atheromatous plaque vulnerability and disruption, and an association between high neopterin concentrations and the presence of vulnerable-complex plaques had previously been documented [31]. Secondly, neopterin not only is a biomarker of cell-mediated immunity but also serves as an indirect indicator of oxidative stress resulting from increased production of reactive oxygen and nitrogen intermediates secreted by activated macrophages [32]. Neopterin can interfere with intracellular signaling pathways known to be influenced by oxidative stress. It seems to be able to participate in several important molecular biological pathways that are regulated by redox balances. It stimulates nuclear factor-κB translocation to the nucleus, thus promoting the expression of proinflammatory genes and the production of adhesion molecules, tissue factor, and many other proteins implicated in atherogenesis, atheromatous plaque disruption, and disease progression [33]. Of importance, neopterin enhances apoptosis in different experimental settings [34].
The interpretation of the data must be done cautiously. The number of patients studied is still low considering the variability of stroke pathology. This would be worth considering in studies to follow. In addition, a group of stroke-mimics (epileptic, metabolic, tumor, etc.) will be the right comparison group and this should be investigated in further study. Second, our biochemical data are based on single time-point blood samplings, and, since blood samples were all obtained in a rested state in the morning, it is unknown whether similar relationships between neopterin and inflammation markers would be seen at other times in the day. In addition, this study yielded no data regarding when and how long neopterin are elevated in these patients. Third, although patients with significant acute medical illnesses known to be associated with an inflammatory burden were excluded from this study, included participants were likely experiencing some degree of systemic inflammation prior to the stroke. As a result, levels of the inflammatory markers detected here were not solely due to stroke. Fourth, our blood-based measurements of markers were taken peripherally, from which we cannot infer local tissue or CNS levels. Finally, only Chinese stroke patients and controls were included. Hence, it remains unclear whether the present findings also apply to other ethnic groups.
Conclusion
In this context, neopterin appears to have an interesting potential as a new prognostic biomarker and makes it a promising candidate also for a multimarker panel. This may allow targeted therapies for stroke patients in the future. However, further research is required to establish the true role of neopterin in clinical practice and whether this molecule plays any role in the pathogenesis of atherosclerosis and stroke progression.
References
Macrez R, Ali C, Toutirais O et al (2011) Stroke and the immune system: from pathophysiology to new therapeutic strategies. Lancet Neurol 10:471–480
Song FY, Wu MH, Zhu L et al (2014) Elevated serum mannose-binding lectin levels are associated with poor outcome after acute ischemic stroke in patients with type 2 diabetes. Mol Neurobiol. doi:10.1007/s12035-014-8941-0
Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P (2008) Impact of functional status at six months on long term survival in patients with ischaemic stroke: prospective cohort studies. BMJ 336:376–379
Tu WJ, Dong X, Zhao SJ, Yang DG, Chen H (2013) Prognostic value of plasma neuroendocrine biomarkers in patients with acute ischaemic stroke. J Neuroendocrinol 25:771–778
Jin R, Liu L, Zhang S et al (2013) Role of inflammation and its mediators in acute ischemic stroke. J Cardiovasc Transl Res 6:834–851
Jin R, Yang G, Li G (2010) Inflammatory mechanisms in ischemic stroke: role of inflammatory cells. J Leukoc Biol 87:779–789
Parker DC, Mielke MM, Yu Q et al (2013) Plasma neopterin level as a marker of peripheral immune activation in amnestic mild cognitive impairment and Alzheimer’s disease. Int J Geriatr Psychiatry 28:149–154
Alanbay I, Mutlu Ercan C, Coksuer H et al (2012) Neopterin: a promising marker for the inflammation in polycystic ovary syndrome. Gynecol Endocrinol 28:879–883
Celik C, Erdem M, Caycı T et al (2010) The association between serum levels of neopterin and number of depressive episodes of major depression. Prog Neuro-Psychopharmacol Biol Psychiatry 34:372–375
Fuchs D, Weiss G, Reibnegger G, Wachter H (1992) The role of neopterin as a monitor of cellular immune activation in transplantation, inflammatory, infectious, and malignant diseases. Crit Rev Clin Lab Sci 29(3–4):307–341
Widner B, Laich A, Sperner-Unterweger B et al (2002) Neopterin production, tryptophan degradation, and mental depression—what is the link? Brain Behav Immun 16:590–595
De Rosa S, Cirillo P, Pacileo M et al (2011) Neopterin: from forgotten biomarker to leading actor in cardiovascular pathophysiology. Curr Vasc Pharmacol 9:188–199
Pedersen ER, Midttun Ø, Ueland PM et al (2011) Systemic markers of interferon-γ–mediated immune activation and long-term prognosis in patients with stable coronary artery disease. Arterioscler Thromb Vasc Biol 31:698–704
Lin HS, Tsai TH, Liu CF et al (2012) Serum level and prognostic value of neopterin in patients after ischemic stroke. Clin Biochem 45:1596–1601
Ganz P, Amarenco P, Goldstein LB et al (2013) Association of MCP-1, hsCRP, Neopterin, MMP-9 and NT-proBNP with coronary heart disease risk in patients with prior stroke or transient ischemic attack. Results of the analysis of 13 biomarkers from the SPARCL trial. Circulation 128:A14940
Hatano S (1976) Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 54:541–553
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Bamford J, Sandercock P, Dennis M et al (1991) Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 337:1521–1526
Brott T, Marler JR, Olinger CP, Adams HP Jr, Tomsick T, Barsan WG et al (1989) Measurements of acute cerebral infarction: lesion size by computed tomography. Stroke 20:871–875
Sims JR (2009) Gharai, L R, Schaefer, P.W, et al. ABC/2 for rapid clinical estimate of infarct, perfusion, and mismatch volumes. Neurology 72:2104–2110
Bonita RBR (1988) Modification of Rankin Scale: recovery of motor function after stroke. Stroke 19:1497–1500
Fuchs D, Avanzas P, Arroyo-Espliguero R et al (2009) The role of neopterin in atherogenesis and cardiovascular risk assessment. Curr Med Chem 16:4644–4653
Yan J, Tan C, Wu J et al (2013) Neopterin negatively regulates expression of ABCA1 and ABCG1 by the LXRα signaling pathway in THP-1 macrophage-derived foam cells. Mol Cell Biochem 379:123–131
Tu WJ, Zhao SJ, Liu TG, Yang DG, Chen H (2013) Combination of high-sensitivity C-reactive protein and homocysteine predicts the shortterm outcomes of Chinese patients with acute ischemic troke. Neurol Res 35:912–921
Markaki I, Franzén I, Talani C, Loizou L, Kostulas N (2013) Long-term survival of ischemic cerebrovascular disease in the acute inflammatory stroke study, a hospital-based cohort described by TOAST and ASCO. Cerebrovasc Dis 35:213–219
Whiteley W, Jackson C, Lewis S, Lowe G, Rumley A et al (2009) inflammatory markers and poor outcome after stroke: a prospective cohort study and systematic review of interleukin-6. PLoS Med 6(9):e1000145
Lyu Y, Jiang X, Dai W (2015) The roles of a novel inflammatory neopterin in subjects with coronary atherosclerotic heart disease. Int Immunopharmacol 24:169–172
Kaski JC, Consuegra-Sanchez L, Fernandez-Berges DJ et al (2008) Elevated serum neopterin levels and adverse cardiac events at 6 months follow-up in Mediterranean patients with non-ST-segment elevation acute coronary syndrome. Atherosclerosis 201(1):176–183
Grammer TB, Fuchs D, Boehm BO, Winkelmann BR, Maerz W (2009) Neopterin as a predictor of total and cardiovascular mortality in individuals undergoing angiography in the Ludwigshafen Risk and Cardiovascular Health Study. Clin Chem 55:1135–1146
Zacho J, Tybjærg-Hansen A, Jensen JS et al (2008) Genetically elevated C-reactive protein and ischemic vascular disease. N Engl J Med 359:1897–1908
Avanzas P, Arroyo-Espliguero R, Cosín-Sales J, Aldama G, Pizzi C, Quiles J et al (2004) Markers of inflammation and multiple complex stenoses (pancoronary plaque vulnerability) in patients with non-ST segment elevation acute coronary syndromes. Heart 90:847–852
Murr C, Widner B, Wirleitner B et al (2002) Neopterin as a marker for immune system activation. Curr Drug Metab 3:175–187
Avanzas P, Arroyo-Espliguero R, Kaski JC (2009) Neopterin and cardiovascular disease: growing evidence for a role in patient risk stratification. Clin Chem 55:1056–1057
Hoffmann G, Rieder J, Smolny M et al (1999) Neopterin-induced expression of intercellular adhesion molecule-1 (ICAM-1) in type II-like alveolar epithelial cells. Clin Exp Immunol 118:435–440
Acknowledgments
We also express our gratitude to all the patients who participated in this study and thereby made this work possible.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Zeng, X., Zhang, G., Yang, B. et al. Neopterin as a Predictor of Functional Outcome and Mortality in Chinese Patients with Acute Ischemic Stroke. Mol Neurobiol 53, 3939–3947 (2016). https://doi.org/10.1007/s12035-015-9310-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9310-3






