Abstract
Schizophrenia is a serious psychotic disease. Recently, increasing evidences support that neurodegeneration occurs in the brain of schizophrenia patients with progressive morphological changes. Paliperidone, an atypical antipsychotic drug, could attenuate psychotic symptom and protect neurons from different stressors. However, the underlying mechanisms are largely unknown. In this study, we used SH-SY5Y cells to evaluate the neuroprotective capability of paliperidone against the neurotoxicity induced by N-methyl-d-aspartate receptor antagonist, MK-801. And, we also explored the possible molecular mechanism. Neurotoxicity of 100 μM MK-801, which reduced the cell viability, was diminished by 100 μM paliperidone using MTT and LDH assays (both p < 0.05). Analysis with Hoechst 33342/PI double staining demonstrated that exposure to MK-801 (100 μM) for 24 h led to the death of 30 % of cultured cells (p < 0.05). Moreover, the patch clamp technique was employed to detect voltage calcium channel changes; the results showed that paliperidone effectively blocked the Ca2+ influx through inhibiting the voltage-gated calcium channels (p < 0.05). Furthermore, paliperidone significantly reversed MK-801 induced increase of SIRT1 and decrease of miR-134 expression (both p < 0.05). Finally, SIRT1 inhibitor nicotinamide blocked MK-801 injury effects and suppressed miR-134 expression. Taken together, our results demonstrated that paliperidone could protect SH-SY5Y cells against MK-801 induced neurotoxicity via inhibition of Ca2+ influx and regulation of SIRT1/miR-134 pathway, providing a promising and potential therapeutic target for schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a serious psychotic disease which affects about 1 % of the world population [1]. Schizophrenia patients suffer from positive symptom (delusions, auditory hallucinations, and thought disorder) and negative symptom (blunted affect and emotion, alogia, anhedonia, and avolition) accompanying with deficit of cognition and these symptoms become apparently at late adolescent time or in early adulthood [2]. Recently, increasing studies demonstrated that progressive morphological alterations of brain occur in schizophrenia patients. Kempton MJ and his colleagues detects the progressive ventricular enlargement in schizophrenia [3]. More recently, researcher reports that reduction in cortical thickness and loss of synapse are identified in patients [4, 5]. Even in early-onset schizophrenia, temporal gray matter decreased obviously. These studies suggested that, during the pathogenesis of schizophrenia, neuronal damage or neurodegeneration possibly occur in the brain and then caused mental dysfunction.
Paliperidone, risperidone’s principal metabolite, is a second-generation atypical antipsychotics, which demonstrated to have superior antipsychotic effects on symptoms of schizophrenia [6]. Paliperidone is reported to be more effectively on managing the negative symptoms and cognitive disorder than typical antipsychotics with less side effects on patients [6–9]. Especially, paliperidone offered neuroprotective effects in recent studies. For example, paliperidone protected SH-SY5Y cells against cell death induced by β-amyloid peptide (25–35), N-methyl-4-phenylpyridinium ion [10]. In addition, paliperidone reduced the caspase-3 expression and protected SK-N-SH cells against neurotoxicity induced by dopamine [11]. Our previous study also suggested that paliperidone could protect primary cortical neurons against apoptosis induced by MK-801. However, the underlying physiological and molecular mechanisms underlying the protection are largely unclear.
Calcium is an important second messenger which generates diverse intracellular signals regulating various biological functions. Calcium influx results in varieties of physiological processes, including depolarization of membrane potential as well as death program in neurons [12–14]. Yan J et al. reported that CaV2.1 mediated by NCS-1 resulted in short-term synaptic facilitation [15]. Our research group found NMDA receptor antagonist MK-801, which is importantly involved in pathology of schizophrenia, increased the Ca2+ influx through time course of [Ca2+]i measurement, while paliperidone reversed Ca2+ influx in this process. Depolarization-induced calcium influx is mainly regulated by voltage-gated calcium channels in neurons. However, whether paliperidone could mediate voltage-gated calcium channels is unclear.
SIRT1 is a NAD+-dependent protein deacetylase, which regulates energy, longevity, and circadian clock rhythm [16, 17]. SIRT1 is closely related with nervous system [18, 19]. Recent studies demonstrates SIRT1 regulated memory and plasticity [20]. Especially, Kishi T et al. also suggests SIRT1 play an important role in the pathophysiology of schizophrenia in Japanese population [21]. MiR-134, a small noncoding RNA, also regulated neuroplasticity and neural development as a downstream molecule of SIRT1 [22]. One convincing evidence comes from postmortem analysis of schizophrenia patients, miR-134 expressed abnormally in prefrontal cortex Brodmann area 46, which suggested miR-134 participates in the pathogenic mechanism of schizophrenia [23]. Interestingly, a more recent study reported that SIRT1 is related with Ca2+/calmodulin-dependent protein kinase kinase (CaMKK) β in endothelium [24]. Based on these data, we hypothesized that paliperidone protects the neurons against cell damage possibly through regulating calcium channel and SIRT1/miR-134 expression.
To test our hypothesis, we examined the protective effect of paliperidone on a cell model with NMDA receptor antagonist MK-801 induced neuronal damage in SH-SY5Y cells. We used MTT and LDH assays to determine the cell viability. Hoechst 33342/PI double staining was employed to detect the cell death. Moreover, the patch clamp technique was used to explore whether paliperidone could regulate calcium channel and affect calcium influx. Furthermore, real-time quantitative PCR and Western blotting were performed to detect the expressions of SIRT1 and miR-134. Finally, nicotinamide, a SIRT1 inhibitor, was used to further reveal the roles of SIRT1 and miR-134 in paliperidone’s neuroprotection against MK-801-induced cell damage. This study would evaluate the pharmacological mechanism of paliperidone in schizophrenia.
Materials and Methods
Chemicals
DMEM/F12 (Hyclone) and fetal bovine serum (FBS, GIBCO) were mixed according to 9:1. Paliperidone was procured from Dalian Meilun Biotech Co., Ltd (Dalian, Jilin, China). Dizocilpine (MK-801) and DMSO were purchased from Sigma-Aldrich (St. Louis, MO, USA). LDH kit was purchased from Beyotime (Haimen, Jiangsu, China). SH-SY5Y cells were obtained from Shanghai Institute of cell library (Shanghai, China).
Paliperidone was dissolved in DMSO at a concentration of 50 mM and then diluted to 500 μM with phosphate buffer solution (PBS). Next, the solution was filtered using a 0.22-μm filter (Millipore, Billerica, MA, USA) and stored at 4 °C. MK-801 was also dissolved in PBS and filtered through a 0.22-μm filter. Before being used, stock solution was prepared with serum-free DMEM to 500 μM, and the working solution was diluted with serum-free medium to desired concentrations.
Cell Culture and Exposure to MK-801
SH-SY5Y cells were maintained in DMEM/ F12 medium with 10 % FBS (37 °C, 5 % CO2). And, the culture medium were refreshed every third day. The cells were seeded in 24-well plates at a density of 2 × 104 cells/cm2 before experiments. After cultured for 24 h in vitro, MK-801 solutions were added into culture medium with final concentrations of 25, 50, 100, and 200 μM, respectively. After treated with MK-801, SH-SY5Y cells were examined in the following experiments.
Exposure to Paliperidone and Experimental Groups
The cultured SH-SY5Y cells were divided into three groups as follows: (1) MK-801-treated group, cells were exposed in the medium at a concentration of 100 μM MK-801; (2) paliperidone protection group, which were further divided into three subgroups, cells were treated with 50, 100, and 200 μM paliperidone respectively in the presence of 100 μM MK-801; and (3) normal control group, cells were cultured in serum-free medium without MK-801 and paliperidone. The highest DMSO was 0.2 % in the experiments, and an equal concentration of DMSO was used in the MK-801 treated group and normal control group.
MTT Assay
In this study, MTT assay was employed to measure cell viability. SH-SY5Y cells were plated in 96-well plates and treated with different concentrations of drugs for 24 h in vitro culture. Then, we incubated cells with 100 μl MTT (5 mg/ml) solution for additional 4 h in the incubator (37 °C, 5 % CO2). Subsequently, MTT solution was removed and 100 μl DMSO was added into each of 96-well plate [24]. After shaking for 10 min at room temperature, the absorption value was detected at 490 nm with an ELISA reader (Thorm Multiskan Mk3, USA). The values were used to determine the cell viability.
LDH Assay
LDH assay was performed to further examine the cell viability by measuring the release of lactate dehydrogenase from damaged cells. The cytotoxicity of MK-801 and protection of paliperidone were examined in cultured SH-SY5Y cells. Cultured cells were exposed to different concentrations of drugs before detection. LDH cytotoxicity assay kit was used to measure cell activity according to previous reports with a modification [24, 25]. The optical density of samples was determined by an ELISA reader (Thorm Multiskan Mk3, PA, USA).
Hoest 3342 and PI Staining
Hoechst 33342 dye stains cellular with blue fluorescence, while propidium iodide dye only stains the nucleus of dead cells with red fluorescence. SH-SY5Y cells were treated with MK-801 or paliperidone for 24 h in vitro culture and washed with PBS for three times. Then, these cells were stained with Hoeshst33342 and PI simultaneously for 15 min at 37 °C. After the incubation, cells were rinsed with PBS. Morphological changes of cells were observed under fluorescence microscope (Carl Zeiss SAS, Jena, Germany). Five random views in different groups were selected to assess and quantify the living and dead cells as previously described in our laboratory [25].
Western Blotting
Cells were collected and lysed by RIPA buffer. Total proteins were extracted with its concentration checked by a NanoDrop® spectrophotometer (Molecular Devices), the proteins samples of different groups were separated by 10 % SDS-polyacrylamide gels, and then transferred to a PVDF membrane. Blots were blocked with TBST containing 10 % milk for 2 h and incubated in the primary antibodies against SIRT1 (1:1000, Santa Cruz Biotechnology, Inc., CA, USA) and β-actin (1:1000) at 4 °C overnight. Then, the blots were incubated in the secondary antibody (1:3000, ZSGB-BIO ORIGENE, Beijing, China) for 1 h at room temperature. Finally, the blots were detected with the Western detection reagents (Millipore Corporation, Billerica, MA, USA) and analyzed by Quantity One software (ImageJ, USA) according to a previous report [26].
Quantitative Real-Time PCR
The total RNA was extracted from cultured SH-SY5Y cells in different groups using TRIzol reagent, and its integrity was determined by a NanoDrop® spectrophotometer (Molecular Devices). The complementary DNA (cDNA) was synthesized from purified RNA using the First Stand cDNA Synthesis Kit (Fermentas) according to its instruction [27]. For miR-134, the reverse transcription synthesis was performed according to the instruction of commercial reagent Kit (RiboBio, miR10000447-1-5). The primers used for this study were listed as follows: SIRT1, forward primers: 5′-TAGACACGCTGGAACAGGTTGC-3′, reverse primers: 5′-CTCCTCGTACAGCTTCACAGTC-3′, Forward and reverse primers of miR-134 were purchased from Ribobio corporation (miR10000447-1-5). SYBR Green/ROX Master Mix was mixed with cDNA samples in a total volume of 10 μl. GAPDH and U6 were used as internal references. 2−ΔΔCt method was used to calculate fold change of SIRT1 and miR-134 expression.
Patch Clamp
Patch clamp technique was employed to record cell membrane potential and Ca2+ current by glass pipettes with a resistance of 8–10 MΩ. Current clamp and voltage clamp were used to record membrane potential and Ca2+ current, respectively. The membrane potential of cultured cells was recorded with standard extracellular solution containing (in mM/L): NaCl 130, KCl 3, MgCl2 1, CaCl2 2, HEPES 10, and glucose 25 at pH 7.3. The standard internal solution contained (in mM/L) KCl 145, NaCl 8, MgCl 1, Hepes-H 10, GTP 0.4, and Mg-ATP 2. When recording Ca2+ currents, TTX was dissolved in the standard extracellular solution and the internal solution contained (in mM/L) CsCl 145, NaCl 8, MgCl 1, Hepes-H 10, GTP 0.4, and Mg-ATP 2. The output signals were stored in an IBM-PC compatible computer and then analyzed with Igore Software. EPC-9 system was used in this experiment.
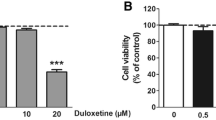
Effect of Nicotinamide on SH-SY5Y Cells Treated with MK-801
In order to further reveal the role of SIRT1 in paliperidone’s neuroprotection, SIRT1 inhibitor, nicotinamide was used in the experiment. Nicotinamide was diluted with PBS and stored at 4 °C. In this study, nicotinamide and MK-801 were synchronously added into the culture medium. The final concentration of nicotinamide was 5 mM. The cell viability and death rate affected by nicotinamide were analyzed by MTT and LDH assay. The mRNA expression level of miR-134 was also determined by real-time quantitatively PCR.
Statistical Analysis
All the data in this study were expressed as means ± SEM. Statistical analysis of the data were performed using by one-way analysis of variance (ANOVA) followed by post hoc Tukey’s multiple comparison test. p < 0.05 represented significant difference.
Results
MK-801 Induces Cytotoxicity in SH-SY5Y Cells
In control group, SH-SY5Y cells grew well with more neurites (Fig. 1a). When treated with MK-801, morphological alterations of cultured cells were visible under phase contrast microscope. Four different concentrations of MK-801 at 25, 50, 100, and 200 μM were added into culture medium for 24 h, and then a dose-dependent cytotoxic damage was evident (Fig. 1b–e). Twenty-five and 50 μM MK-801 resulted in a slightly damage of cells with neurites retracted and disappeared (Fig. 1b, c), while 100 and 200 μM MK-801 resulted in obvious cell damages including network collapsed and cell debris increased (Fig. 1d, e).
MK-801-induced neurotoxicity in SH-SY5Y cells. SH-SY5Y cells were treated with 25 (b), 50 (c), 100 (d), and 200 μM (e) MK-801 and observed under a phase contrast microscope and compared with the control (a). f The viability of SH-SY5Y cells, exposed to MK-801 for 24 h, was assessed by MTT assay (n = 14). g Extracellular LDH activity in MK-801-treated cells was assessed by LDH assay (n = 6, one-way ANOVA post hoc Tukey’s multiple comparison test, *p < 0.05 vs control group). Scale bars: a–e, 50 μm
MTT assay showed that cell viability decreased to 0.99 ± 0.01 and 0.97 ± 0.02 of the control when treated with 25 and 50 μM MK-801, respectively, for 24 h in vitro culture (Fig. 1f). While 100 and 200 μM MK-801 significantly decreased cell viability to 0.65 ± 0.03 and 0.54 ± 0.02 of the control, respectively (both p < 0.05, Fig. 1f). To further detect the changes of cell viability, we explored LDH release rates among different groups. The LDH release rates of cultured cells exposed to 100 and 200 μM MK-801 were elevated to 0.363 ± 0.041 and 0.395 ± 0.047, respectively, which were obviously both higher than the control (both p < 0.05). However, the LDH activity of 25 and 50 μM MK-801 showed no statistical difference compared with the control (both p > 0.05). Therefore, 100 μM was used in the following experiments.
Paliperidone Increases Cell Viability Against MK-801-Induced Damage
To examine whether paliperidone had a survival-potentiating effect, we evaluated MK-801 injured SH-SY5Y cells companied with or without paliperidone. In the presence of 100 μM MK-801, three different concentrations of paliperidone (50, 100, and 200 μM) were added into the medium. One hundred micromolars of paliperidone effectively rescued the injured SH-SY5Y cells with neurites visible, and the shapes of cell body changed from ellipse to rhombus (Fig. 2b, d). While in the groups of 50 and 200 μM paliperidone, less neurites were observed (Fig. 2c).
Protective effects of paliperidone on MK-801-damaged cells. The SH-SY5Y cells were treated with 50 (b), 100 (c), and 200 μM (d) paliperidone in the presence of 100 μM MK-801. a MK-801-treated group. e Cell viability was assessed by MTT. The viability of SH-SY5Y cell significantly increased when adding paliperidone (n = 16). f The LDH release rate was further detected by LDH assay (n = 6), and the LDH release rate decreased. One-way ANOVA post hoc Tukey’s multiple comparison test, *p < 0.05 vs control group. Scale bars: a–d, 50 μm
The MTT metabolism assay and LDH release assay were further performed to explore the neuroprotective effect of paliperidone against MK-801 damage. In the MTT metabolism, only 100 μM paliperidone demonstrated neuroprotective effect in the presence of 100 μM MK-801 (Fig. 2e, p < 0.05). Compared with MK-801-treated group, the LDH activity of 100 and 200 μM paliperidone group decreased significantly, but not 50 μM paliperidone (p < 0.05, Fig. 2f). By combining Fig. 2e, f, it was shown the treatment of 100 μM paliperidone was more efficient. Therefore, 100 μM paliperidone was used in the subsequent examinations.
Paliperidone Decreases Cell Death Against MK-801-Induced Damage
Hoechst 33342/PI staining was used to access the living and dead cells. After stained with Hoechst 33342 and PI, the cultured SH-SY5Y cells were observed under microscope. In 100 μM MK-801-treated group, more dead cells were detected in red fluorescence compared with the control (Fig. 3a–f). However, in the presence of paliperidone, as shown in Fig. 3g–i, the dead cells decreased obviously. Thus, paliperidone effectively attenuated cell damages induced by MK-801. Statistical analysis also confirmed that paliperidone reduced SH-SY5Y cells death rate from 34 to 14 % (Fig. 3j, p < 0.05).
Cell death was assessed by Hoechst 33342/PI staining. Photographs of control group (a–c), MK-801-treated group (d–f), and paliperidone protective group (g–i) were examined. Dead cells were obviously increased after treated with MK-801 for 24 h, whereas paliperidone could attenuate cell damage and decreased the cell death rate (j). Cell death rate was computed from the ratio of dead SH-SY5Y cells to total cells. Arrows pointed to dead cells (n = 4). One-way ANOVA post hoc Tukey’s multiple comparison test, *p < 0.05 vs control group; #p < 0.05 vs MK-801-treated group
Paliperidone Hyperpolarizes the Membrane Potential and Inhibits Ca2+ Currents
In order to detect paliperidone’s effects on electrophysiological characteristic of SH-SY5Y cells, patch clamp was performed. Resting membrane potential of SH-SY5Y cells in control group was −61 ± 5 mV in the standard external solution, whereas it depolarized to −19 ± 3 mV after treated with MK-801 for 24 h (Fig. 4a, p < 0.05). The average reference amplitude of MK-801-induced depolarization was 42 mV. When exposed to 100 μM paliperidone, the membrane potential of SH-SY5Y cells hyperpolarized with the average amplitude of 5 mV (Fig. 4c, p < 0.05).
Paliperidone hyperpolarized membrane potential by inhibiting the voltage-gated Ca2+ channels. a, b Membrane potential of SH-SY5Y cells treated with or without MK-801 for 24 h (n = 4, t test, *p < 0.05 vs control group). c Paliperidone hyperpolarized the membrane potential of SH-SY5Y cells treated with MK-801 for 24 h in vitro. d Graphical representation of membrane potential in control, paliperidone-treated, and recovery group (n = 9, one-way ANOVA post hoc Tukey’s multiple comparison test, *p < 0.05 vs control group). e, f Voltage-gated calcium channels of cells were inhibited by paliperidone (n = 7, t test, *p < 0.05 vs control group)
According to our previous work that paliperidone affects the time course of Ca2+, so we investigated the Ca2+ currents exposed to paliperidone. These inward currents are generated by a depolarizing step drive from the holding potential of −80 mV. The Ca2+ currents obtained from a same SH-SY5Y cell in the standard external solution or adding paliperidone were recorded separately. When exposed to paliperidone, the amplitude of Ca2+ currents decreased to 61 ± 3 % of their original values (Fig. 4e, p < 0.05). The results indicated that MK-801 could lead to depolarization of SH-SY5Y cells, on the contrary, pailperidone could offset depolarization partly via inhibiting the Ca2+ currents.
Paliperidone Upregulates SIRT1 and Downregulates miR-134 Expression
To examine the underlying mechanism of paliperidone on SH-SY5Y cells against MK-801 neurotoxicity, SIRT1 and miR-134 expressions were accessed by quantitative real-time PCR and Western blotting. As shown in Fig. 5a, the application of MK-801 led to a significant increase in mRNA expression level of SIRT1 compared with the control (p < 0.05). We also observed paliperidone remarkably reduced SIRT1 level to around 0.7-fold of the control (Fig. 5b, p < 0.05). The protein expression of SIRT1 was analyzed by Western blotting. Compared with the MK-801-treated group, paliperidone also decreased SIRT1 protein level (Fig. 5c, d, p < 0.05). The expression of miR-134 was also examined by quantitative real-time PCR. The data showed that MK-801 suppressed miR-134 expression, and paliperidone effectively reversed this trend (Fig. 5e, f, p < 0.05).
Paliperidone upregulated miR-134 level by inhibiting SIRT1 expression. a, b mRNA expression of SIRT1 of SH-SY5Y cells were detected by quantitative RT-PCR (n = 4). c, d Protein expression of SIRT1 was determined by Western blotting. Expressions of SIRT1 mRNA and protein were both raised by exposed to MK-801 for 24 h, and paliperidone reversed these changes (n = 5). e, f Quantitative RT-PCR was used to assess the expression level of miR-134. Paliperidone decreased the expression of miR-134 in MK-801-treated cells (n = 4). In the photographs a and e, control group, paliperidone protection group and MK-801-treated group were respectively represented by pound, triangle, and asterisk. One-way ANOVA post hoc Tukey’s multiple comparison test, *p < 0.05 vs control group; #p < 0.05 vs MK-801-treated group
SIRT1 Inhibitor Nicotinamide Attenuates MK-801-Induced Cell Damages
To explore if the MK-801 induced cytotoxicity was mediated by SIRT1, SH-SY5Y cells were treated simultaneously with MK-801 and SIRT1 inhibitor, nicotinamide. In MK-801-treated group, neurites shortened or disappeared. While application of nicotinamide obviously alleviated cell damages (Fig. 6a–c). The Hoechst 33342 and PI staining was used to distinguish dead cells with red fluorescence from cells with blue fluorescence. This double staining showed that nicotinamide could decrease dead cells caused by MK-801 (Fig. 6d–h). Moreover, MTT and LDH assay were performed to detect the cell viability. MTT assay revealed that nicotinamide increased cell viability of SH-SY5Y cells in the presence of MK-801 (Fig. 6g, p < 0.05). And, the data of LDH release assay was consistent with MTT assay (Fig. 6h, p < 0.05). Furthermore, real-time quantitative PCR revealed that nicotinamide upregulated expression of miR-134 compared with MK-801 treated group (Fig. 6i, p < 0.05), when was partly by inhibiting the function of SIRT1.
SIRT1 inhibitor nicotinamide blocked MK-801 induced cell damages. After treated with normal medium (a), MK-801 (b) and MK-801 + nicotinamide (c) for 24 h, SH-SY5Y cells were observed under a microscope. Hoechst 33342 and PI double staining were employed to detect cell death rate (d–f). Moreover, cell viability and LDH release rate were further assessed by MTT (g) and LDH assays (h). After nicotinamide was added and blocked SIRT1 activity, the cell viability increased (n = 13) and LDH release rate decreased (n = 9). j Expression level of miR-134 was detected by quantitative RT-PCR. Nicotinamide reversed MK-801 induced increased of miR-134 level. Control group: cells in normal medium; MK-801-treated group: cells in 100 μM MK-801; MK-801 + nicotinamide group: cells in 100 μM MK-801 and 5 mM nicotinamide (n = 8). One-way ANOVA post hoc Tukey’s multiple comparison test, *p < 0.05 vs control group; #p < 0.05 vs MK-801-treated group. Scale bars: a–c, 100 μm; d–f, 20 μm
Discussion
In this study, we established an in vitro damage model of SH-SY5Y cells using NMDA receptor antagonist MK-801, which can partly mimic neural injury model of psychosis as a previous report [26, 27]. Our data revealed the underlying mechanisms of paliperidone against MK-801-induced neuronal damages. Paliperidone inhibited voltage calcium channel and decreased calcium influx. Particularly, paliperidone reversed the process that MK-801 increased SIRT1 and decreased miR-134 levels. Possibly, it is a strategy to explore the mechanisms of paliperidone antipsychotic effects.
Calcium ion is a very important molecule which could regulate the functions of neurons such as transmitter release [28]. Previous studies demonstrate that calcium ions are transferred into cells major by voltage-gated calcium channels which participate in depolarizing signal [14, 29]. In this study, the SH-SY5Y cells were treated with MK-801 for 24 h in vitro, and the membrane potential depolarized from −60 to −20 mV. Therefore, MK-801 disturbed the homeostasis of intracellular calcium. Previous reports confirms that calcium dyshomeostasis caused abnormality of membrane potential, even hyperpolarize upon −40 mV, and then induced cell death [12, 30]. Interestingly, paliperidone inhibited the voltage-gated calcium channel and depolarized the membrane potential from −20 to −40 mV. Although cell membrane potential did not recover to normal level, paliperidone partly reversed this trend. In our previous study, palipridone effectively attenuated the elevation of intracellular calcium concentration through Ca2+ time course detection. This experiment further revealed that paliperidone inhibited voltage-gated calcium channel.
SIRT1, is a nicotinamide adenine dinucleotide-dependent histone deacetylase enzyme, which is essential in regulating cellular functions. Previous studies demonstrates that SIRT1 exerts a key role in neuroprotection and regulates metabolic activity [31, 32]. A growing body of evidences shows that SIRT1 are beneficial for several kinds of mental disorder, such as Alzheimer’s disease [20, 33, 34]. In this study, MK-801 upregulated SIRT1 expression, while treated with paliperidone, SIRT1 protein expression of SH-SY5Y cells even recovered to normal level. Therefore, paliperidone possibly protected SH-SY5Y cells through regulation SIRT1 expression. To further test our speculation, nicotinamide, an inhibitor of SIRT1, was used to block SIRT1’s activity. Cell viability of cultured cells were reversed to 69 % of the control group with MTT and LDH assays. It was interestingly expression of SIRT1 was downregulated by paliperidone in the MK-801-damaged cells. Several recent studies also revealed that SIRT1 inhibition could be neuroprotective. Li et al. declares that the inhibition of SIRT1 protected neurons through modulation IGF-I/IRS-2/Ras/ERK1/2 signaling pathway [35]. Sansone et al. demonstrates that SIRT1 silencing promoted neuron survival by inducing IGF-1 protein expression [36]. Slomka et al. also declares nicotinamide exerts neuroprotective role in cerebellar granule cells [37], which is consistent with our experiment.
MiR-134 is a brain-specific microRNA. Recently, miR-134 is reported as a downstream molecule of SIRT1 in regulation memory and plasticity, and SIRT1 suppresses miR-134 expression through a repressor complex [38]. Is miR-134 involved in paliperidone’s neuroprotection against MK-801 induced damages of SH-SY5Y cells? We detected miR-134 expression using quantitatively RT-PCR. Our results showed that MK-801 upregulated miR-134 expression, while paliperidone decreased its expression. Importantly, when we blocked SIRT1 activity with nicotinamide, miR-134’s expression increased. It suggested that, at least partly, SIRT1/miR-134 signal pathway is involved in MK-801’s injury effects. A current report also declares that miR-134 regulates ischemia-induced neuronal cell death through inhibition CREB Signaling [39]. CREB and BDNF were important molecules and the downstream signals of SIRT1/miR-134. Although CREB decreased in some mental diseases, MK-801 increases CREB expression in rodent model and this was consistent with our speculation [40, 41]. Moreover, effects of MK-801 on BDNF mRNA level are multiple. MK-801 increases the BDNF mRNA in single cells in the limbic cortex [42]. Interestingly, paliperidone also increases BDNF level and the mechanism is unknown [43]. The molecular networks regulated by paliperidone are complex. As the network model shown in Fig. 7, SIRT1 performed a key role in this process and affected CREB and BDNF level indirectly. Besides inhibition of miR-134, SIRT1 also phosphorylated the IRS-2 and increased Ras/Erk activations, whereas we do not know whether paliperidone directly works on SIRT1 or not. This question needs to be investigated in the future.
The schematic diagram of paliperidone against MK-801-induced neurotoxicity to SH-SY5Y cells. Paliperidone blocks the calcium influx by antagonizing the 5-HT 2A receptor and reverses MK-801-induced increase on SIRT1 expression level. MK-801 directly antagonizes NMDA receptor and activates SIRT1 by unknown mechanisms. Consequently, SIRT1 may activate IRS-2 mediated signal transduction, such as Ras, MEK12, and ERK1/2. In particular, upregulation of SIRT1 suppresses the miR-134 expression which inhibits CREB and BDNF expression. Solid lines means a direct effect
MK-801, a noncompetitive NMDA receptor antagonist, can block glutamate receptors and induce neuronal degeneration [44]. For example, MK-801 induced neuronal apoptosis in the rat retrosplenial cortex and neuronal degeneration in several parts of rat brain; in vitro culture, MK-801 is demonstrated to cause the neuronal damage of cortical neurons, cerebellar granule cells, and neural stem cells [26, 45]. Our previous study also suggested that MK-801 insults primary cultured cortical neurons and suppresses Akt1/GSK3β expression. Here, we examined the effects of MK-801 on human neuroblastoma (SH-SY5Y) cells. Our data showed that MK-801 increased intracellular Ca2+ influx. Especially, MK-801 obviously upregulated SIRT1 and downregulated miR-134 expressions, which highlight a novel signal target for understanding the pathogenic mechanism of psychotic disease.
In conclusion, NMDA receptor antagonist MK-801 induced neuronal damage in SH-SY5Y cells, which upregulated SIRT1 and downregulated miR-134 expressions. Paliperidone effectively reversed this process. Moreover, patch clamp recording showed that paliperidone inhibited Ca2+ influx via inhibition voltage calcium channel. Our study revealed the underlying mechanism of paliperidone’s neuroprotection and provided a promising molecular target for treating psychotic disease.
Abbreviations
- MK-801:
-
Dizocilpine
- LDH:
-
Lactate dehydrogenase
- MTT:
-
3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl-2-H-tetrazolium bromide
- RT-PCR:
-
Real-time polymerase chain reaction
- CREB:
-
cAMP-response element binding protein
- miR-134:
-
MicroRNA-134
- SIRT1:
-
Sirtuin 1
- NMDA:
-
N-Methyl-d-aspartic acid
- NCS-1:
-
Neuronal calcium sensor-1
- CaV2.1:
-
Calcium channel, voltage-dependent, P/Q type, alpha 1A subunit
- TTX:
-
Tetrodotoxin
- IRS-2:
-
Insulin receptor substrates-2
- Erk:
-
Extracellular signal-regulated kinase 1/2
- MEK:
-
Mitogen-activated protein kinase/extracellular signal-regulated kinase kinase
- IGF-1:
-
Insulin-like growth factor 1
References
Rajji TK, Miranda D, Mulsant BH (2014) Cognition, function, and disability in patients with schizophrenia: a review of longitudinal studies. Can J Psychiatry 59(1):13–17
Sarkar S, Grover S (2013) Antipsychotics in children and adolescents with schizophrenia: a systematic review and meta-analysis. Indian J Pharmacol 45(5):439–446
Kempton MJ, Stahl D, Williams SC, DeLisi LE (2010) Progressive lateral ventricular enlargement in schizophrenia: a meta-analysis of longitudinal MRI studies. Schizophr Res 120(1–3):54–62
Vita A, De Peri L, Deste G, Sacchetti E (2012) Progressive loss of cortical gray matter in schizophrenia: a meta-analysis and meta-regression of longitudinal MRI studies. Transl Psychiatry 20(2):116
Cannon TD, Chung Y, He G, Sun D, Jacobson A, van Erp TG, McEwen S, Addington J et al (2015) Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk. Biol Psychiatry 77(2):147–157
Na KS, Kim CE, Kim YS, Lee JI, Han WS, Kang UG, Park DH, Kim B et al (2013) Effectiveness of paliperidone extended-release for patients with schizophrenia: focus on subjective improvement. Hum Psychopharmacol 28(2):107–116
Huang MW, Yang TT, Ten PR, Su PW, Wu BJ, Chan CH, Lan TH, Liu IC et al (2012) Effects of paliperidone extended release on the symptoms and functioning of schizophrenia. BMC Clin Pharmacol 12(1):1472–6904
Singh J, Robb A, Vijapurkar U, Nuamah I, Hough D (2011) A randomized, double-blind study of paliperidone extended-release in treatment of acute schizophrenia in adolescents. Biol Psychiatry 70(12):1179–1187
Sliwa JK, Bossie CA, Ma YW, Alphs L (2011) Effects of acute paliperidone palmitate treatment in subjects with schizophrenia recently treated with oral risperidone. Schizophr Res 132(1):28–34
Yang MC, Lung FW (2011) Neuroprotection of paliperidone on SH-SY5Y cells against beta-amyloid peptide(25–35), N-methyl-4-phenylpyridinium ion, and hydrogen peroxide-induced cell death. Psychopharmacology 217(3):397–410
Gasso P, Mas S, Molina O, Bernardo M, Lafuente A, Parellada E (2012) Neurotoxic/neuroprotective activity of haloperidol, risperidone and paliperidone in neuroblastoma cells. Prog Neuropsychopharmacol Biol Psychiatry 36(1):71–77
Berliocchi L, Bano D, Nicotera P (2005) Ca2+ signals and death programmes in neurons. Philos Trans R Soc Lond B Biol Sci 360(1464):2255–2258
Duchen MR (2012) Mitochondria, calcium-dependent neuronal death and neurodegenerative disease. Pflugers Arch 464(1):111–121
Simms BA, Zamponi GW (2014) Neuronal voltage-gated calcium channels: structure, function, and dysfunction. Neuron 82(1):24–45
Yan J, Leal K, Magupalli VG, Nanou E, Martinez GQ, Scheuer T, Catterall WA (2014) Modulation of CaV2.1 channels by neuronal calcium sensor-1 induces short-term synaptic facilitation. Mol Cell Neurosci 63:124–131
Hubbard BP, Sinclair DA (2014) Small molecule SIRT1 activators for the treatment of aging and age-related diseases. Trends Pharmacol Sci 35(3):146–154
Rehan L, Laszki-Szczachor K, Sobieszczanska M, Polak-Jonkisz D (2014) SIRT1 and NAD as regulators of ageing. Life Sci 105(1–2):1–6
Paraiso AF, Mendes KL, Santos SH (2013) Brain activation of SIRT1: role in neuropathology. Mol Neurobiol 48(3):681–689
Tang BL, Chua CE (2008) SIRT1 and neuronal diseases. Mol Aspects Med 29(3):187–200
Donmez G (2012) The effects of SIRT1 on Alzheimer’s disease models. Int J Alzheimers Dis 509529(10):3
Kishi T, Fukuo Y, Kitajima T, Okochi T, Yamanouchi Y, Kinoshita Y, Kawashima K, Inada T et al (2011) SIRT1 gene, schizophrenia and bipolar disorder in the Japanese population: an association study. Genes Brain Behav 10(3):257–263
Numakawa T, Richards M, Adachi N, Kishi S, Kunugi H, Hashido K (2011) MicroRNA function and neurotrophin BDNF. Neurochem Int 59(5):551–558
Santarelli DM, Beveridge NJ, Tooney PA, Cairns MJ (2011) Upregulation of dicer and microRNA expression in the dorsolateral prefrontal cortex Brodmann area 46 in schizophrenia. Biol Psychiatry 69(2):180–187
Wen L, Chen Z, Zhang F, Cui X, Sun W, Geary GG, Wang Y, Johnson DA et al (2013) Ca2+/calmodulin-dependent protein kinase kinase beta phosphorylation of Sirtuin 1 in endothelium is atheroprotective. Proc Natl Acad Sci U S A 110(26):10
Peng L, Zhu D, Feng X, Dong H, Yue Q, Zhang J, Gao Q, Hao J et al (2013) Paliperidone protects prefrontal cortical neurons from damages caused by MK-801 via Akt1/GSK3beta signaling pathway. Schizophr Res 147(1):14–23
Ono T, Hashimoto E, Ukai W, Ishii T, Saito T (2010) The role of neural stem cells for in vitro models of schizophrenia: neuroprotection via Akt/ERK signal regulation. Schizophr Res 122(1–3):239–247
Klimaviciusa L, Safiulina D, Kaasik A, Klusa V, Zharkovsky A (2008) The effects of glutamate receptor antagonists on cerebellar granule cell survival and development. Neurotoxicology 29(1):101–108
Sheng L, Leshchyns’ka I, Sytnyk V (2013) Cell adhesion and intracellular calcium signaling in neurons. Cell Commun Sign 11(94):11–94
Frank CA (2014) How voltage-gated calcium channels gate forms of homeostatic synaptic plasticity. Front Cell Neurosci 8 (40)
Matute C (2010) Calcium dyshomeostasis in white matter pathology. Cell Calcium 47(2):150–157
Liu D, Gharavi R, Pitta M, Gleichmann M, Mattson MP (2009) Nicotinamide prevents NAD+ depletion and protects neurons against excitotoxicity and cerebral ischemia: NAD+ consumption by SIRT1 may endanger energetically compromised neurons. Neuromol Med 11(1):28–42
Wang J, Fivecoat H, Ho L, Pan Y, Ling E, Pasinetti GM (2010) The role of Sirt1: at the crossroad between promotion of longevity and protection against Alzheimer’s disease neuropathology. Biochim Biophys Acta 8(4):26
Jesus S, Gomez-Garre P, Carrillo F, Caceres-Redondo MT, Huertas-Fernandez I, Bernal-Bernal I, Bonilla-Toribio M, Vargas-Gonzalez L et al (2013) Genetic association of sirtuin genes and Parkinson’s disease. J Neurol 260(9):2237–2241
Lalla R, Donmez G (2013) The role of sirtuins in Alzheimer’s disease. Front Aging Neurosci 5 (16)
Li Y, Xu W, McBurney MW, Longo VD (2008) SirT1 inhibition reduces IGF-I/IRS-2/Ras/ERK1/2 signaling and protects neurons. Cell Metab 8(1):38–48
Sansone L, Reali V, Pellegrini L, Villanova L, Aventaggiato M, Marfe G, Rosa R, Nebbioso M et al (2013) SIRT1 silencing confers neuroprotection through IGF-1 pathway activation. J Cell Physiol 228(8):1754–1761
Slomka M, Zieminska E, Salinska E, Lazarewicz JW (2008) Neuroprotective effects of nicotinamide and 1-methylnicotinamide in acute excitotoxicity in vitro. Folia Neuropathol 46(1):69–80
Gao J, Wang WY, Mao YW, Graff J, Guan JS, Pan L, Mak G, Kim D et al (2010) A novel pathway regulates memory and plasticity via SIRT1 and miR-134. Nature 466(7310):1105–1109
Huang W, Liu X, Cao J, Meng F, Li M, Chen B, Zhang J (2015) miR-134 regulates ischemia/reperfusion injury-induced neuronal cell death by regulating CREB signaling. J Mol Neurosci 55(4):821–829
Guan L, Jia N, Zhao X, Zhang X, Tang G, Yang L, Sun H, Wang D et al (2013) The involvement of ERK/CREB/Bcl-2 in depression-like behavior in prenatally stressed offspring rats. Brain Res Bull 99:1–8
Ahn YM, Seo MS, Kim SH, Kim Y, Yoon SC, Juhnn YS, Kim YS (2005) Increased phosphorylation of Ser473-Akt, Ser9-GSK-3beta and Ser133-CREB in the rat frontal cortex after MK-801 intraperitoneal injection. Int J Neuropsychopharmacol 8(4):607–613
Castren E, da Penha BM, Lindholm D, Thoenen H (1993) Differential effects of MK-801 on brain-derived neurotrophic factor mRNA levels in different regions of the rat brain. Exp Neurol 122(2):244–252
Hanson ND, Nemeroff CB, Owens MJ (2011) Lithium, but not fluoxetine or the corticotropin-releasing factor receptor 1 receptor antagonist R121919, increases cell proliferation in the adult dentate gyrus. J Pharmacol Exp Ther 337(1):180–186
Wozniak DF, Dikranian K, Ishimaru MJ, Nardi A, Corso TD, Tenkova T, Olney JW, Fix AS (1998) Disseminated corticolimbic neuronal degeneration induced in rat brain by MK-801: potential relevance to Alzheimer’s disease. Neurobiol Dis 5(5):305–322
Hwang JY, Kim YH, Ahn YH, Wie MB, Koh JY (1999) N-Methyl-D-aspartate receptor blockade induces neuronal apoptosis in cortical culture. Exp Neurol 159(1):124–130
Acknowledgments
We thank Guibao Li for applying technical supports in the work. This experiment was supported by the following grants, a grant from the National Natural Science Foundation of China with no.81371471, grants from Natural Science Foundation of Shandong Province with no. ZR2010HM051 and no. ZR2012HM026, and a grant from Shandong Provincial Science and Technology Development Plan with no. 2011GSF11810.
Conflict of Interest
We, all authors, declare that we have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, D., Zhang, J., Wu, J. et al. Paliperidone Protects SH-SY5Y Cells Against MK-801-Induced Neuronal Damage Through Inhibition of Ca2+ Influx and Regulation of SIRT1/miR-134 Signal Pathway. Mol Neurobiol 53, 2498–2509 (2016). https://doi.org/10.1007/s12035-015-9217-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9217-z