Abstract
The sudden global crisis of COVID-19, driven by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), demands swift containment measures due to its rapid spread and numerous problematic mutations, which complicate the establishment of herd immunity. With escalating fatalities across various nations no foreseeable end in sight, there is a pressing need to create swiftly deployable, rapid, cost-effective detection, and treatment methods. While various steps are taken to mitigate the transmission and severity of the disease, vaccination is proven throughout mankind history as the best method to acquire immunity and circumvent the spread of infectious diseases. Nonetheless, relying solely on vaccination might not be adequate to match the relentless viral mutations observed in emerging variants of SARS-CoV-2, including alterations to their RBD domain, acquisition of escape mutations, and potential resistance to antibody binding. Beyond the immune system activation achieved through vaccination, it is crucial to develop new medications or treatment methods to either impede the infection or enhance existing treatment modalities. This review emphasizes innovative treatment strategies that aim to directly disrupt the virus’s ability to replicate and spread, which could play a role in ending the SARS-CoV-2 pandemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The virus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is responsible for the onset of Coronavirus disease 2019 (COVID-19), significantly impacting the lives of millions. As of December 2023, Worldometer (https://www.worldometers.info/coronavirus/) reported that SARS-CoV-2 has infected over 700 million people and caused around 6.9 million casualties worldwide, therefore, making the current pandemic one of the deadliest in history. In order to deal with the pandemic, various steps have been implemented such as strict movement control protocols to mitigate social contact, mandatory use of personal protection equipment (PPE), unprecedentedly fast vaccine development, and approval for emergency use [1,2,3]. Despite significant efforts taken globally, the disease is still spreading persistently, causing major disruption to social and economic lives of millions every day.
SARS-CoV-2 is a single-stranded RNA virus which belongs to the coronavirus family. It carries genetic instructions for various proteins, including structural proteins like membrane protein, nucleocapsid protein, envelope protein, and spike glycoprotein. Additionally, it encodes non-structural proteins, the majority of which form the viral replication and transcription complex, along with accessory proteins [4]. The spike glycoprotein of SARS-CoV-2 can be cleaved by the host proteases such as the transmembrane protease, serine 2 (TMPRSS2) into 2 subunits: S1 and S2. Studies have found that there are specific furin cleavage sites between the S1 and S2 subunits which can be cleaved by furin-like proteases of the host for increased viral entry [5]. Within the S1 subunit, two domains are present: the N-terminal and the C-terminal. Either of these domains can serve as the receptor binding domain (RBD), responsible for binding to the host receptor angiotensin-converting enzyme 2 (ACE2) [6]. Upon successful cleaving and binding, the S2 subunit will then mediate endocytosis of the virion into the host cell through membrane fusion [6, 7]. As a result, the spike glycoprotein plays a crucial role in the viral transmission of SARS-CoV-2. Additionally, the RBD holds significant importance in antibody research, as the majority of antibodies utilized in therapeutics or currently under development target this specific domain [8, 9].
On the other hand, mutations in SARS-CoV-2 usually entail single-letter changes, involving substitutions or deletions of specific amino acids. For instance, the prevalent D614G mutation involves a substitution of aspartic acid (D) at position 614 with glycine (G), causing conformational changes in the spike protein and enhancing viral entry [10, 11]. The mutation of the SARS-CoV-2 virus is a significant cause for concern due to various factors. Some mutations may result in heightened transmissibility which translates to easier person-to-person spread [12]. Moreover, due to the importance of the spike protein and the RBD domain during virus-antibody interaction, mutation in the spike protein or other viral regions might impact its vulnerability to neutralization by antibodies or acquired immunity from previous infections. The most alarming aspect of mutation is that significant mutations in regions targeted by vaccines can diminish the efficacy of currently available vaccines [13,14,15,16].
To address the ongoing pandemic, substantial global efforts and resources are dedicated to the development of vaccine candidates to mitigate the COVID-19 pandemic [17]. Vaccines stand out as one of humanity’s most potent tools against infectious diseases. However, the relentless mutation of the virus is enabling the emergence of increasingly resistant variants, posing a challenge to the effectiveness of our current vaccines [18]. Nevertheless, researchers are also exploring therapeutic approaches apart from vaccination to address the ongoing pandemic. This includes exploring the use of antiviral compounds and agents that can directly disrupt the ability of the virus to infect and replicate within the host without relying on the host’s immune response.
The primary distinction between vaccines and other antiviral therapeutic strategies lies in their mechanisms of action. Vaccines function by triggering the immune system to generate antibodies and activate immune cells, including T cells. These components recognize and neutralize the virus upon future encounters. In contrast, antiviral therapeutics, such as antiviral drugs, operate by disrupting the virus’s ability to replicate and disseminate within the body. They achieve this by targeting specific viral enzymes, proteins, or processes crucial for viral replication [19, 20]. A variety of therapies and treatment strategies are under exploration to discover new avenues for providing additional treatment options.
In this review, we discuss the therapeutic approaches being devised in the global effort apart from immunization provided by vaccination to solve the ongoing SARS-CoV-2 pandemic.
Cocktail Therapy
To counter escape mutations, a primary strategy is employing monoclonal antibody cocktail, which is utilizing multiple antibodies targeting non-overlapping epitopes on the spike protein, rendering the commonly observed single-site mutation of SARS-CoV-2 ineffective [21]. However, due to the plasticity of the SARS-CoV-2, relying on cocktail therapy alone may be insufficient.
A well-known example of such therapy is REGEN-COV (formerly REGEN-COV2/REGN-COV2), a cocktail therapy which involves administration of casirivimab and imdevimab. In a study, REGEN-COV has shown success in reducing COVID-19 hospitalizations and severe cases by 56.4–59.2% respectively, while its efficacy in preventing COVID-19-related death was reported to be 93.5% [22]. In a similar study, REGEN-COV significantly reduced the need of additional medical intervention by 70% in COVID patients with high-risk factors [23].
Despite the multi epitope binding capabilities of REGEN-COV, the SARS-CoV-2 was still reported to be able to gain escape mutation to evade the said cocktail. In a study, the Delta variant in patients treated with casirivimab + imdevimab gained G446 and L455 mutations which significantly reduced the neutralizing activity of the cocktail [24]. Another study indicates that the spike protein can undergo a possible escape mutation at E406, which would maintain detectable binding to ACE2 while diminishing the potency of the casirivimab + imdevimab cocktail [21].
Similarly, AZD77442 (cocktail of monoclonal antibody composed of tixagevimab and cilgavimab) administration during the Omicron-dominated wave of COVID-19 (December 2021-April 2022) in Israel lowered the odds of hospitalization/death in immunocompromised persons by 92% [25]. A related study suggests that mutations G446 and Q493 observed in the SARS-CoV-2 Omicron variant make the virus susceptible to AZD7442. Additionally, the same study demonstrates that AZD7442 has the capability to neutralize all tested Omicron subvariants (BA.1, BA.1.1, BA.2, BA.2.12.1, BA.2.75, BA.4/BA.5) in vitro [26]. In spite of the effectiveness of AZD7742, the cocktail proved ineffective in neutralizing Omicron variants in individuals with hematologic malignancies [27] and B-cell malignancies [28].
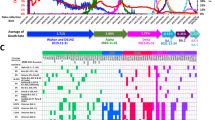
In the pursuit to enhance the effectiveness of antiviral treatments, researchers are exploring combinations of antiviral agents to assess their potential efficacy against SARS-CoV-2. Unlike monoclonal antibodies, antiviral agents do not necessarily rely on RBD binding to inhibit the virus, instead can directly interfere with the lifestyle or various aspects of the viral replication process (Fig. 1) [29, 30]. Though choosing the right combination of antiviral substances would not be an easy task as the selected combinates should not only inhibit the virus successfully but also should not exhibit any significant toxicity or side effects to the host.
Potential of innovative therapeutic strategies in combating SARS-CoV-2 entry into the host cell. A Monoclonal antibodies cocktail target multiple non-overlapping epitopes on the RBD. B Remdesivir, a well-known antiviral drug interferes with SARS-CoV-2 viral RNA replication by inhibiting RdRP. C TMPRSS2 inhibitor prevents viral interaction with host ACE2. D Use of heparan sulfate (HS) competitor to prevent viral adhesion by competing with HS binding sites
De Forni et al. (2022) proposed a broad-spectrum antiviral cocktail consisting of remdesivir (RDV) with either azithromycin (AZI) or ivermectin (IVM) which demonstrated synergistic increase in antiviral activity with no observed increase in cytotoxicity from their combined use. In the same trial, combining RDV with either AZI or IVM also significantly reduced the dosage ordinarily required from each individual drug to completely suppress SARS-CoV-2, thereby, lowering the risk of drug toxicity [31]. In a case report, a patient with compromised immunity due to follicular lymphoma and persistent SARS-CoV-2 infection exhibited successful treatment through the concurrent use of oral antiviral medications namely molnupiravir together with the combined protease inhibitors, nirmatrelvir/ritonavir. The administered therapy was well received, demonstrating both clinical and biochemical tolerance, without any observed signs of toxicity [32]. In a similar study, fourteen individuals with compromised adaptive humoral immunity and enduring SARS-CoV-2 infection underwent treatment with a combination of remdesivir and nirmatrelvir/ritonavir. All patients experienced resolution of COVID-19 symptoms within a median duration of 6 days and viral clearance was accomplished after median of 9 days [33]. In a parallel study, Wagoner et al. (2022) reported increased synergistic potential in suppressing SARS-CoV-2 when combining molnupiravir with two distinct categories of antivirals: those targeting SARS-CoV-2 entry (camostat, nafamostat, and avoralstat) and those focusing on SARS-CoV-2 replication (brequinar) [34]. Hence, research on drug cocktail comprising multiple antiviral agents holds promise for developing new therapeutic approaches that are more effective in addressing the emerging SARS-CoV-2 variants.
CAR-T Cell Therapy
Chimeric antigen receptor T cells (CAR-Ts) is a type of treatment which shows promise as an alternative therapeutic for treating SARS-CoV-2. In this strategy, T cells obtained from the patient’s blood are modified by adding a specific receptor that can bind to proteins present on the target cell (e.g., S protein). The addition of specific receptor transforms the modified T cells into living drugs which are able to elicit a greater and more specific immune response against the target in comparison to normal T cells [35] (Fig. 2). Guo et al. (2021) developed SARS-CoV-2 CAR-Ts which showed potent inhibitory activity against target cells expressing RBD, S1 peptide or S1 protein. These CAR-Ts were also successful in killing S1-expressing cells in vivo using mice. The cytolysis of targets were reported to be mainly mediated by the GZMB/perforin pathway [36]. In a similar work, Zhu et al. (2021) developed nanovesicles from bispecific CAR-T cells which express two single-chain fragment variables (scFv) named CR3022 and B38. The nanovesicles expressing both the single-chain fragment variables exhibit stronger inhibitory property against spike-pseudo-virus infectivity than nanovesicles that express either CR3022 or B38 alone. The co-expression of both CR3022 and B38 which target separate epitopes of spike protein may lessen the occurrence of viral resistance [37]. The successful development of SARS-CoV-2 CAR-Ts could lead to the next generation of SARS-CoV-2 vaccines where the T cells introduced into the host body are pre-equipped with receptors specific for SARS-CoV-2 binding.
Other Prospective Agents in Treating SARS-CoV-2
There are various other agents exhibiting diverse antiviral properties that have been identified and are currently undergoing research to assess their potential against SARS-CoV-2.
Chitosan Based Antiviral Agents
Chitosan is a naturally occurring compound that is valued in medical field for its antibacterial and antiviral activity [38, 39]. A study by Jang et al. (2022) showed chitooligosaccharide, a chitosan-based substance is able to inhibit SARS‐CoV‐2 in plaque assay and showed lower cytotoxicity than ivermectin [40]. In another report, chitosan and chitosan-derived substances namely chitobiose, chitotriose, and chitotetraose is shown to inhibit SARS-CoV-2 main protease (Mpro), a key enzyme vital for viral replication by combining hydrogen bonding and salt bridge interactions to create a stable complex [41]. Moreover, chitosan has demonstrated the ability to enhance the therapeutic properties of other antiviral compounds. Loutfy et al. (2022) combined silymarin (Sil) and chitosan nanoparticles (CNP) to create Sil-CNPs. The conjugation of these two compounds increased silymarin’s bioavailability and physicochemical qualities, allowing it to inhibit or compete with SARS-CoV-2 binding to the host cell [42]. In another study, the administration of N-dihydrogalactochitosan (GC) both before and after exposure to SARS-CoV-2 resulted in a notable decrease of up to 75% in morbidity and mortality among mice models expressing humanized ACE2 receptor. Furthermore, GC demonstrated the ability to lower infectious virus levels in the upper airway and did not induce histopathologic lesions in the lungs of the mice [43]. In a similar work, researchers investigated the effects of administering chitosan oligosaccharide, hydroxychloroquine, and a combination of both in Male Syrian hamsters. The combined use of intranasal chitosan oligosaccharide and hydroxychloroquine resulted in enhanced hydroxychloroquine absorption in the lungs, improved immune responses and did not elevate the risk of liver or heart injuries [44].
Interestingly, chitosan has also demonstrated promise for application in research related to vaccine development. In an investigation, an optimal oral COVID-19 vaccine candidate, rVSVΔG-Sdelta, was chosen from a range of vesicular stomatitis virus (VSV)-based constructs carrying spike proteins from various SARS-CoV-2 strains and modified with chitosan. Following chitosan modification, rVSVΔG-Sdelta triggered both local and systemic antibody responses, notably yielding broad-spectrum and enduring neutralizing antibodies against SARS-CoV-2 that persisted for up to 1 year. Golden hamsters vaccinated with this candidate demonstrated cross-protection against SARS-CoV-2 WT, Beta, Delta, BA.1, and BA.2 strains, resulting in significantly reduced viral replication in the respiratory tract and mitigated pulmonary pathology following SARS-CoV-2 challenge [45].
Similar results were achieved in another study which utilizes another chitosan derivative, namely dihydrogalactochitosan (GC). In the study, GC was utilized as an adjuvant by mixing it with recombinant SARS-CoV-2 trimeric spike (S) and nucleocapsid (NC) proteins to develop GC + S + NC for intranasal vaccination of K18-hACE2 transgenic mice, comparing its efficacy with Addavax (AV) prepared similarly. Unlike AV, intranasal administration of GC elicits a strong, systemic antibody response specific to the antigen and enhances the population of T cells in the cervical lymph nodes. Furthermore, animals vaccinated with GC + S + NC demonstrated substantial resistance to lethal SARS-CoV-2 challenge, exhibiting significantly reduced morbidity and mortality, with their weight and behavior returning to baseline levels 22 days post-infection. Conversely, animals intranasally vaccinated with AV + S + NC experienced severe weight loss, mortality, and respiratory distress, with none surviving beyond 6 days post-infection [46].
These findings suggest the possibility of employing chitosan derivatives in combination with other antiviral compounds or drugs to enhance the inhibition of SARS-CoV-2 or even for development of novel vaccines.
Antiviral Metal-Based Complexes
Several metal-based complexes have also demonstrated antiviral potential against SARS-CoV-2. In the study by R. Wang et al. (2022), the oral administration of combined bismuth drugs colloidal bismuth subcitrate (CBS) or bismuth subsalicylate (BSS) with N-acetyl-L-cysteine (NAC) significantly reduced viral lung loads and virus-associated pathology in a Syrian hamster infection model and exhibited broad-spectrum anti-CoV activity. The drug cocktail suppressed virus replication by targeting various conserved key cysteine proteases/enzymes in SARS-CoV-2 which includes papain-like protease (PLpro), main protease (Mpro), helicase (Hel), and angiotensin-converting enzyme 2 (ACE2). Despite being classified as a cocktail in the study, N-acetyl-L-cysteine was not reported to exhibit antiviral activity on its own, instead used in the cocktail to stabilize CBS in vitro and promotes its absorption during in vivo testing [47].
Some studies propose that gold metallodrugs, particularly auranofin, exhibit strong inhibitory activity against the interaction of SARS-CoV-2 spike protein and papain-like protease (PLpro). These metallodrugs have been shown to hinder viral entry and replication, even at low micromolar concentrations [48, 49].
In a similar work, auranofin is shown to be able to block SARS-CoV-2 in vitro by inhibiting a raft-dependent endocytic pathway involved in SARS-CoV-2 entry into host cells in addition to modifying ACE2 mobility at the plasma membrane. The same study also reported that auranofin enhanced cell viability in Vero E6 and Calu-3 cells within the micromolar range, prior to exhibiting toxicity beyond 2.5 μM [50]. Therefore, more research may be required on auranofin’s cytotoxicity so that it can be used on its own or in conjunction with other medications without fear of increased cytotoxicity.
In a separate study, Panchariya et al. (2021) demonstrated that zinc can effectively inhibit the SARS-CoV-2 main protease (Mpro) and impede viral replication in vitro. Furthermore, the inclusion of the natural ionophore, quercetin enhances the anti-viral potency of zinc [51]. In some related studies, selenocompounds have been suggested to inhibit main protease (Mpro) and papain-like protease (PLpro) of SARS-CoV-2 via in silico analyses which underscores their potential for development into antiviral drugs against SARS-CoV-2 [52, 53]. Another study revealed that a synthesized metal complex, rhenium(I) tricarbonyl picolinic acid, could effectively inhibit the 3CLpro of SARS-CoV-2 with IC50 values in the low micromolar range. Furthermore, this metal complex demonstrated selectivity for 3CLpro over various human proteases and other enzymes associated with SARS-CoV-2 [54].
In a parallel investigation, silver N-heterocyclic carbene (NHC) complexes exhibited potent enzymatic inhibition, demonstrating strong and selective inhibition of SARS-CoV-2 PLpro with IC50 values below 0.5 μM. Notably, their effectiveness against SARS-CoV PLpro was limited, and these complexes showed inactivity in experiments involving SARS-CoV-2 3CLpro. This confirms their preference or selectivity for PLpro from SARS-CoV-2 over other related proteases [55].
Manipulation of Heparan Sulfate or Inhibition of Viral Adhesion by Exogenous Heparin
Several authors reported the essentiality of heparan sulfate (HS) as a co-factor in initiating the binding of SARS-CoV2 spike protein with ACE2 receptors, allowing for further viral infection and progression [56, 57]. Competitor of HS such as heparin when exogenously administered can effectively inhibit or block the open configurations of spike protein by competing with the HS binding sites, therefore, controlling their transmission. In the study by Nie et al. (2021), the negatively charged linear polyglycerol sulfate (LPGS) can competitively bind to the spike protein of SARS-CoV-2 which prevents viral binding to host HS that leads to infectivity. Compared to heparin, this synthetic polysulfate was reported to exhibit virus-inhibitory action that is more than 60-fold greater [58]. In another report, Zhang et al. (2022) demonstrated the anti-cancer drug, mitoxantrone, can modulate a heparan sulfate-spike complex during viral entry and inhibit the infection of SARS-CoV-2 strain in a cell-based model and in human lung EpiAirway 3D tissues [59]. In a parallel study, the synthetic polyanionic drug suramin demonstrated effective inhibition of SARS-CoV-2 infection by targeting both the ACE2 receptor and heparan sulfate binding sites on the RBDs of wild-type, Delta, and Omicron variants. Further analysis using surface plasmon resonance (SPR) experiments and docking studies suggests that suramin inhibits viral entry of the Omicron variant primarily by blocking both ACE2 and HS binding sites, whereas in the Delta and wild-type variants, the inhibition is attributed solely to ACE2 interactions [60].
These findings demonstrate that the development of inhibitory agents against HS sites can prove beneficial as therapeutic agents.
TMPRSS2 Inhibitor
Transmembrane protease, serine 2 (TMPRSS2) plays a crucial role in the pathogenicity of COVID-19 due to its involvement in the cleavage of the SARS-CoV-2 spike protein, which permits the virus to enter the host cell. Therefore, a theoretical therapeutic approach to preventing SARS-CoV-2 infection could involve the use of a TMPRSS2 inhibitor.
Shapira et al. (2022) reported the use of N-0385 as potent inhibitor of TMPRSS2. The ligand yielded beneficial outcomes such as improving weight loss and reducing clinical symptoms when tested with severe K18-human ACE2 transgenic mouse model of SARS-CoV-2 disease, suggesting a novel treatment option for COVID-19 patients [61]. In a similar study, K. Li et al. (2021) demonstrated that nafamostat can effectively inhibit SARS-CoV-2 infection in cultured human airway epithelia and Calu-3 2B4 cell lines in addition to improving disease outcomes in Ad5-hACE2 and K18-hACE2 mice models [62]. Another investigation unveiled that antithrombin (AT), an endogenous serine protease inhibitor involved in coagulation regulation, demonstrated binding and inhibitory effects on TMPRSS2 as evidenced by molecular docking and enzyme activity assays. As a result, AT impedes entry facilitated by the spikes of SARS‐CoV, MERS‐CoV, hCoV‐229E, SARS‐CoV‐2, and its concerning variants, including Omicron, while also suppressing lung cell infection caused by genuine SARS‐CoV‐2. Additionally, it was demonstrated that the activation of AT by anticoagulants like heparin or fondaparinux enhances its anti-TMPRSS2 and anti-SARS-CoV-2 capabilities, suggesting the potential repurposing of both native and activated AT for treating COVID-19. This study further highlights that the interaction between TMPRSS2 and the spike protein remains necessary for successful host infection even across different variants [63]. Consequently, these findings establish TMPRSS2 inhibitors as viable options for the treatment and management of COVID-19.
Conclusion
In this review, we discussed the approaches that have the potential to control the spread of COVID-19. The ability of SARS-CoV-2 variants to rapidly alter their RBD domain, acquiring escape mutations and potentially resisting antibody binding, suggests that vaccination alone might not be adequate to address emerging variations. While vaccination unquestionably provided humanity with a crucial defense against the ongoing pandemic, depending solely on immunization through vaccines would present a significant challenge in entirely eliminating the virus. Utilizing a combination of antiviral drugs or agents that target different mechanisms to hinder SARS-CoV-2, independent of the host’s immune response, can pose a significant challenge to the virus’s ability to mutate. For example, simultaneously blocking ACE-2 interaction to prevent viral entry and disrupting viral RNA replication would present a more formidable barrier to the virus’s mutation capability. Therefore, it is imperative for future studies to focus on the efficiency of combined strategies or approaches to impede the mutative capabilities of the SARS-CoV-2.
Data Availability
Not applicable.
References
Sun, C., & Zhai, Z. (2020). The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable Cities and Society, 62, 102390. https://doi.org/10.1016/j.scs.2020.102390
Zhao, C., Viana, A., Jr., Wang, Y., Wei, H. Q., Yan, A. H., & Capasso, R. (2020). Otolaryngology during COVID-19: Preventive care and precautionary measures. American Journal of Otolaryngology, 41(4), 102508. https://doi.org/10.1016/j.amjoto.2020.102508
Kashte, S., Gulbake, A., El-Amin, S. F., III., & Gupta, A. (2021). COVID-19 vaccines: Rapid development, implications, challenges and future prospects. Human Cell, 34(3), 711–733. https://doi.org/10.1007/s13577-021-00512-4
Lamers, M. M., & Haagmans, B. L. (2022). SARS-CoV-2 pathogenesis. Nature Reviews Microbiology, 20(5), 270–284. https://doi.org/10.1038/s41579-022-00713-0
Hoffmann, M., Kleine-Weber, H., & Pöhlmann, S. (2020). A multibasic cleavage site in the spike protein of SARS-CoV-2 is essential for infection of human lung cells. Molecular Cell, 78(4), 779–784. https://doi.org/10.1016/j.molcel.2020.04.022
Wang, Q., Zhang, Y., Wu, L., Niu, S., Song, C., Zhang, Z., Lu, G., Qiao, C., Hu, Y., Yuen, K., Wang, Q., Zhou, H., Yan, J., & Qi, J. (2020). Structural and functional basis of SARS-COV-2 entry by using human ACE2. Cell, 181(4), 894-904.e9. https://doi.org/10.1016/j.cell.2020.03.045
Ou, X., Liu, Y., Lei, X., Li, P., Mi, D., Ren, L., Guo, L., Guo, R., Chen, T., Hu, J., Xiang, Z., Mu, Z., Chen, X., Chen, J., Hu, K., Jin, Q., Wang, J., & Qian, Z. (2020). Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nature Communications. https://doi.org/10.1038/s41467-020-15562-9
Piccoli, L., Park, Y. J., Tortorici, M. A., Czudnochowski, N., Walls, A. C., Beltramello, M., Silacci-Fregni, C., Pinto, D., Rosen, L. E., Bowen, J. E., Acton, O. J., Jaconi, S., Guarino, B., Minola, A., Zatta, F., Sprugasci, N., Bassi, J., Peter, A., De Marco, A., & Veesler, D. (2020). Mapping neutralizing and immunodominant sites on the SARS-COV-2 spike receptor-binding domain by structure-guided high-resolution serology. Cell, 183(4), 1024-1042.e21. https://doi.org/10.1016/j.cell.2020.09.037
Greaney, A. J., Starr, T. N., Gilchuk, P., Zost, S. J., Binshtein, E., Loes, A. N., Hilton, S. K., Huddleston, J., Eguia, R., Crawford, K. H., Dingens, A. S., Nargi, R. S., Sutton, R. E., Suryadevara, N., Rothlauf, P. W., Liu, Z., Whelan, S. P., Carnahan, R. H., Crowe, J. E., & Bloom, J. D. (2021). Complete mapping of mutations to the SARS-CoV-2 spike receptor-binding domain that escape antibody recognition. Cell Host & Microbe, 29(1), 44-57.e9. https://doi.org/10.1016/j.chom.2020.11.007
Hou, Y. J., Chiba, S., Halfmann, P., Ehre, C., Kuroda, M., Dinnon, K. H., Leist, S. R., Schäfer, A., Nakajima, N., Takahashi, K., Lee, R. E., Mascenik, T. M., Graham, R., Edwards, C. E., Tse, L. V., Okuda, K., Markmann, A. J., Bartelt, L., De Silva, A., … Baric, R. S. (2020). SARS-CoV-2 D614G variant exhibits efficient replication ex vivo and transmission in vivo. Science, 370(6523), 1464–1468. https://doi.org/10.1126/science.abe8499
Yurkovetskiy, L., Wang, X., Pascal, K. E., Tomkins-Tinch, C., Nyalile, T. P., Wang, Y., Baum, A., Diehl, W. E., Dauphin, A., Carbone, C., Veinotte, K., Egri, S. B., Schaffner, S. F., Lemieux, J. E., Munro, J. B., Rafique, A., Barve, A., Sabeti, P. C., Kyratsous, C. A., … Luban, J. (2020). Structural and functional analysis of the D614G SARS-COV-2 spike protein variant. Cell, 183(3), 739-751.e8. https://doi.org/10.1016/j.cell.2020.09.032
Chen, J., Wang, R., Wang, M., & Wei, G. W. (2020). Mutations strengthened SARS-CoV-2 infectivity. Journal of Molecular Biology, 432(19), 5212–5226. https://doi.org/10.1016/j.jmb.2020.07.009
Dhama, K., Nainu, F., Frediansyah, A., Yatoo, M. I., Mohapatra, R. K., Chakraborty, S., Zhou, H., Islam, M. R., Mamada, S. S., Kusuma, H. I., Rabaan, A. A., Alhumaid, S., Mutair, A. A., Iqhrammullah, M., Al-Tawfiq, J. A., Mohaini, M. A., Alsalman, A. J., Tuli, H. S., Chakraborty, C., & Harapan, H. (2023). Global emerging Omicron variant of SARS-CoV-2: Impacts, challenges and strategies. Journal of Infection and Public Health, 16(1), 4–14. https://doi.org/10.1016/j.jiph.2022.11.024
Nonaka, C. K. V., Franco, M. M., Gräf, T., de Lorenzo Barcia, C. A., de Ávila Mendonça, R. N., de Sousa, K. A. F., Neiva, L. M. C., Fosenca, V., Mendes, A. V. A., de Aguiar, R. S., Giovanetti, M., & de Freitas Souza, B. S. (2021). Genomic evidence of SARS-COV-2 reinfection involving E484K spike mutation. Brazil. Emerging Infectious Diseases, 27(5), 1522–1524. https://doi.org/10.3201/eid2705.210191
Motozono, C., Toyoda, M., Zahradnik, J., Saito, A., Nasser, H., Tan, T. S., Ngare, I., Kimura, I., Uriu, K., Kosugi, Y., Yue, Y., Shimizu, R., Ito, J., Torii, S., Yonekawa, A., Shimono, N., Nagasaki, Y., Minami, R., Toya, T., & Sato, K. (2021). SARS-CoV-2 spike L452R variant evades cellular immunity and increases infectivity. Cell Host & Microbe, 29(7), 1124-1136.e11. https://doi.org/10.1016/j.chom.2021.06.006
Malik, J. A., Ahmed, S., Mir, A., Shinde, M., Bender, O., Alshammari, F., Ansari, M., & Anwar, S. (2022). The SARS-CoV-2 mutations versus vaccine effectiveness: New opportunities to new challenges. Journal of Infection and Public Health, 15(2), 228–240. https://doi.org/10.1016/j.jiph.2021.12.014
Li, Y., Tenchov, R., Smoot, J., Liu, C., Watkins, S., & Zhou, Q. (2021). A comprehensive review of the global efforts on COVID-19 vaccine development. ACS Central Science, 7(4), 512–533. https://doi.org/10.1021/acscentsci.1c00120
Akash, K., Sharma, A., Kumar, D., Singh, S. K., Gupta, G., Chellappan, D. K., Dua, K., & Nagraik, R. (2022). Molecular aspects of Omicron, vaccine development, and recombinant strain XE: A review. Journal of Medical Virology, 94(10), 4628–4643. https://doi.org/10.1002/jmv.27936
Kausar, S., Said Khan, F., Ishaq Mujeeb Ur Rehman, M., Akram, M., Riaz, M., Rasool, G., Hamid Khan, A., Saleem, I., Shamim, S., & Malik, A. (2021). A review: Mechanism of action of antiviral drugs. International Journal of Immunopathology and Pharmacology, 35, 20587384211002620. https://doi.org/10.1177/205873842110026
Mascellino, M. T., Di Timoteo, F., De Angelis, M., & Oliva, A. (2021). Overview of the main anti-SARS-CoV-2 vaccines: Mechanism of action, efficacy and safety. Infection and Drug Resistance. https://doi.org/10.2147/IDR.S315727
Addetia, A., Park, Y., Starr, T., Greaney, A. J., Sprouse, K. R., Bowen, J. E., Tiles, S. W., Van Voorhis, W. C., Bloom, J. D., Corti, D., Walls, A. C., & Veesler, D. (2023). Structural changes in the SARS-CoV-2 spike E406W mutant escaping a clinical monoclonal antibody cocktail. Cell Reports, 42(6), 112621. https://doi.org/10.1016/j.celrep.2023.112621
Hayek, S., Ben-Shlomo, Y., Dagan, N., Reis, B. Y., Barda, N., Kepten, E., Roitman, A., Shapira, S., Yaron, S., Balicer, R. D., Netzer, D., & Peretz, A. (2022). Effectiveness of REGEN-COV antibody combination in preventing severe COVID-19 outcomes. Nature Communications. https://doi.org/10.1038/s41467-022-32253-9
Kakinoki, Y., Yamada, K., Tanino, Y., Suzuki, K., Ichikawa, T., Suzuki, N., Asari, G., Nakamura, A., Kukita, S., Uehara, A., Saito, S., Kuroda, S., Sakagami, H., Nagashima, Y., Takahashi, K., & Suzuki, S. (2022). Impact of antibody cocktail therapy combined with casirivimab and imdevimab on clinical outcome for patients with COVID-19 in a real-life setting: A single institute analysis. International Journal of Infectious Diseases, 117, 189–194. https://doi.org/10.1016/j.ijid.2022.01.067
Ragonnet-Cronin, M., Nutalai, R., Huo, J., Dijokaite-Guraliuc, A., Das, R., Tuekprakhon, A., Supasa, P., Liu, C., Selvaraj, M., Groves, N., Hartman, H., Ellaby, N., Sutton, J. M., Bahar, M. W., Zhou, D., Fry, E., Ren, J., Brown, C., Klenerman, P., & Rokadiya, S. (2023). Generation of SARS-CoV-2 escape mutations by monoclonal antibody therapy. Nature Communications. https://doi.org/10.1038/s41467-023-37826-w
Kertes, J., David, S. S. B., Engel-Zohar, N., Rosen, K., Hemo, B., Kantor, A., Adler, L., Stein, N. S., Reuveni, M. M., & Shahar, A. (2022). Association between AZD7442 (Tixagevimab-Cilgavimab) administration and Severe Acute respiratory Syndrome Coronavirus 2 (SARS-COV-2) infection, hospitalization, and mortality. Clinical Infectious Diseases/Clinical Infectious Diseases, 76(3), e126–e132. https://doi.org/10.1093/cid/ciac625
Roe, T. L., Brady, T., Schuko, N., Nguyen, A., Beloor, J., Guest, J. D., Aksyuk, A. A., Tuffy, K. M., Zhang, T., Streicher, K., Kelly, E. J., & Kijak, G. H. (2023). Molecular characterization of AZD7442 (Tixagevimab-Cilgavimab) neutralization of SARS-COV-2 Omicron subvariants. Microbiology Spectrum. https://doi.org/10.1128/spectrum.00333-23
Stuver, R., Shah, G. L., Korde, N. S., Roeker, L. E., Mato, A. R., Batlevi, C. L., Chung, D. J., Doddi, S., Falchi, L., Gyurkocza, B., Hamilton, A., Lin, Y., Jakubowski, A. A., Joffe, E., Landau, H. L., Lin, R. J., Mailankody, S., Palomba, M. L., Park, J. H., & Vardhana, S. A. (2022). Activity of AZD7442 (tixagevimab-cilgavimab) against Omicron SARS-CoV-2 in patients with hematologic malignancies. Cancer Cell, 40(6), 590–591. https://doi.org/10.1016/j.ccell.2022.05.007
Chang, A., Koff, J. L., Lai, L., Orellana-Noia, V. M., Surati, M., Leal, A. M. K., Ellis, M. L., Wali, B., Moreno, A., Linderman, S. L., O’Leary, C. B., Allen, P. B., Churnetski, M. C., Dhodapkar, M. V., Suthar, M. S., Cohen, J. B., & Ahmed, R. (2023). Low neutralizing activity of AZD7442 against current SARS-CoV-2 Omicron variants in patients with B-cell malignancies. Blood Advances, 7(11), 2459–2462. https://doi.org/10.1182/bloodadvances.2022009475
Bibi, N., Gul, S., Ali, J., & Kamal, M. A. (2020). Viroinformatics approach to explore the inhibitory mechanism of existing drugs repurposed to fight against COVID-19. European Journal of Pharmacology, 885, 173496. https://doi.org/10.1016/j.ejphar.2020.173496
Frediansyah, A., Tiwari, R., Sharun, K., Dhama, K., & Harapan, H. (2021). Antivirals for COVID-19: A critical review. Clinical Epidemiology and Global Health, 9, 90–98. https://doi.org/10.1016/j.cegh.2020.07.006
De Forni, D., Poddesu, B., Cugia, G., Chafouleas, J., Lisziewicz, J., & Lori, F. (2022). Synergistic drug combinations designed to fully suppress SARS-CoV-2 in the lung of COVID-19 patients. PLoS ONE, 17(11), e0276751. https://doi.org/10.1371/journal.pone.0276751
Marangoni, D., Antonello, R. M., Coppi, M., Palazzo, M., Nassi, L., Streva, N., Povolo, L., Malentacchi, F., Zammarchi, L., Rossolini, G. M., Vannucchi, A. M., Bartoloni, A., & Spinicci, M. (2023). Combination regimen of nirmatrelvir/ritonavir and molnupiravir for the treatment of persistent SARS-CoV-2 infection: A case report and a scoping review of the literature. International Journal of Infectious Diseases, 133, 53–56. https://doi.org/10.1016/j.ijid.2023.04.412
Pasquini, Z., Toschi, A., Casadei, B., Pellegrini, C., D’Abramo, A., Vita, S., Beccacece, A., Bussini, L., Chionsini, M. C., Dentale, N., Cantiani, A., Lazzarotto, T., Bartoletti, M., Nicastri, E., Zinzani, P., Giannella, M., & Viale, P. (2023). Dual combined antiviral treatment with remdesivir and nirmatrelvir/ritonavir in patients with impaired humoral immunity and persistent SARS-CoV-2 infection. Hematological Oncology, 41(5), 904–911. https://doi.org/10.1002/hon.3206
Wagoner, J., Herring, S., Hsiang, T., Ianevski, A., Biering, S. B., Xu, S., Hoffmann, M., Pöhlmann, S., Gale, M., Aittokallio, T., Schiffer, J. T., White, J. M., & Polyak, S. J. (2022). Combinations of host- and virus-targeting antiviral drugs confer synergistic suppression of SARS-COV-2. Microbiology Spectrum. https://doi.org/10.1128/spectrum.03331-22
Milone, M. C., & Bhoj, V. G. (2018). The pharmacology of T cell therapies. Molecular Therapy Methods & Clinical Development, 8, 210–221. https://doi.org/10.1016/j.omtm.2018.01.010
Guo, X., Kazanova, A., Thurmond, S., Saragovi, H. U., & Rudd, C. E. (2021). Effective chimeric antigen receptor T cells against SARS-CoV-2. Iscience, 24(11), 103295. https://doi.org/10.1016/j.isci.2021.103295
Zhu, T., Xiao, Y., Meng, X., Tang, L., Li, B., Zhao, Z., Tan, Q., Shan, H., Liu, L., & Huang, X. (2021). Nanovesicles derived from bispecific CAR-T cells targeting the spike protein of SARS-CoV-2 for treating COVID-19. Journal of Nanobiotechnology. https://doi.org/10.1186/s12951-021-01148-0
Li, J., & Zhuang, S. (2020). Antibacterial activity of chitosan and its derivatives and their interaction mechanism with bacteria: Current state and perspectives. European Polymer Journal, 138, 109984. https://doi.org/10.1016/j.eurpolymj.2020.109984
Jaber, N., Al-Remawi, M., Al-Akayleh, F., Al-Muhtaseb, N., Al-Adham, I. S., & Collier, P. J. (2022). A review of the antiviral activity of Chitosan, including patented applications and its potential use against COVID-19. Journal of Applied Microbiology, 132(1), 41–58. https://doi.org/10.1111/jam.15202
Jang, D., Lee, D., Shin, Y. C., Lee, J. S., Jung, J., & Ryoo, S. (2022). Low molecular weight chitooligosaccharide inhibits infection of SARS-CoV-2 in vitro. Journal of Applied Microbiology, 133(2), 1089–1098. https://doi.org/10.1111/jam.15618
Wang, Q., Song, Y., Kim, M., Hahn, S. K., & Jiang, G. (2023). Effect of chitooligosaccharide on the inhibition of SARS-CoV-2 main protease. Biomaterials Research, 27(1), 13. https://doi.org/10.1186/s40824-023-00351-4
Loutfy, S. A., Abdel-Salam, A. I., Moatasim, Y., Gomaa, M. R., Fattah, N. F. A., Emam, M. H., Ali, F., ElShehaby, H. A., Ragab, E. A., El-Din, H. M. A., Mostafa, A., Ali, M. A., & Kasry, A. (2022). Antiviral activity of chitosan nanoparticles encapsulating silymarin (Sil–CNPs) against SARS-CoV-2 (in silico and in vitro study). RSC Advances, 12(25), 15775–15786. https://doi.org/10.1039/d2ra00905f
Weiss, C. M., Liu, H., Ball, E. E., Hoover, A. R., Wong, T. S., Wong, C. F., Lam, S., Hode, T., Keel, M. K., Levenson, R. M., Chen, W. R., & Coffey, L. L. (2023). N-dihydrogalactochitosan reduces mortality in a lethal mouse model of SARS-CoV-2. PLoS ONE, 18(8), e0289139. https://doi.org/10.1371/journal.pone.0289139
Lin, D. S., Tzeng, S. C., Cha, T., Hung, C., Lin, W., Yang, C., Lu, H., Chang, J., & Huang, S. (2023). Inhalable chitosan-based hydrogel as a mucosal adjuvant for hydroxychloroquine in the treatment for SARS-CoV-2 infection in a hamster model. Journal of Microbiology, Immunology and Infection, 56(5), 951–960. https://doi.org/10.1016/j.jmii.2023.08.001
Wang, S., Cui, H., Zhang, C., Li, W., Wang, W., He, W., Feng, N., Zhao, Y., Wang, T., Tang, X., Yan, F., & Xia, X. (2023). Oral delivery of a chitosan adjuvanted COVID-19 vaccine provides long-lasting and broad-spectrum protection against SARS-CoV-2 variants of concern in golden hamsters. Antiviral Research, 220, 105765. https://doi.org/10.1016/j.antiviral.2023.105765
Hoover, A. R., More, S., Liu, K., West, C. L., Valerio, T. I., Furrer, C. L., Adams, J. P., Yu, N., Villalva, C., Kumar, A., Alleruzzo, L., Lam, S. S., Hode, T., Papin, J. F., & Chen, W. R. (2024). N-dihydrogalactochitosan serves as an effective mucosal adjuvant for intranasal vaccine in combination with recombinant viral proteins against respiratory infection. Acta Biomaterialia, 175, 279–292. https://doi.org/10.1016/j.actbio.2023.12.039
Wang, R., Chan, J. F., Wang, S., Li, H., Zhao, J., Ip, T. K., Zuo, Z., Yuen, K., Yuan, S., & Sun, H. (2022). Orally administered bismuth drug together with N-acetyl cysteine as a broad-spectrum anti-coronavirus cocktail therapy. Chemical Science, 13(8), 2238–2248. https://doi.org/10.1039/d1sc04515f
Rothan, H. A., Stone, S., Natekar, J., Kumari, P., Arora, K., & Kumar, M. (2020). The FDA-approved gold drug auranofin inhibits novel coronavirus (SARS-COV-2) replication and attenuates inflammation in human cells. Virology, 547, 7–11. https://doi.org/10.1016/j.virol.2020.05.002
Gil-Moles, M., Basu, U., Büssing, R., Hoffmeister, H., Türck, S., Varchmin, A., & Ott, I. (2020). Gold metallodrugs to target coronavirus proteins: inhibitory effects on the spike-ACE2 interaction and on PLpro protease activity by auranofin and gold organometallics. Chemistry—A European Journal, 26(66), 15140–15144. https://doi.org/10.1002/chem.202004112
Laplantine, E., Chable-Bessia, C., Oudin, A., Swain, J., Soria, A., Merida, P., Gourdelier, M., Mestiri, S., Besseghe, I., Bremaud, E., Neyret, A., Lyonnais, S., Favard, C., Benaroch, P., Hubert, M., Schwartz, O., Guerin, M., Danckaert, A., Del Nery, E., … Weil, R. (2022). The FDA-approved drug Auranofin has a dual inhibitory effect on SARS-CoV-2 entry and NF-κB signaling. iScience, 25(10), 105066. https://doi.org/10.1016/j.isci.2022.105066
Panchariya, L., Khan, W. A., Kuila, S., Sonkar, K., Sahoo, S., Ghoshal, A., Kumar, A., Verma, D. K., Hasan, A., Khan, M. A., Jain, N., Mohapatra, A. K., Das, S., Thakur, J. K., Maiti, S., Nanda, R. K., Halder, R., Sunil, S., & Arockiasamy, A. (2021). Zinc2+ion inhibits SARS-CoV-2 main protease and viral replicationin vitro. Chemical Communications, 57(78), 10083–10086. https://doi.org/10.1039/d1cc03563k
Rakib, A., Nain, Z., Sami, S. A., Mahmud, S., Islam, A., Ahmed, S., Siddiqui, A. B. F., Babu, S. M. O. F., Hossain, P., Shahriar, A., Nainu, F., Emran, T. B., & Simal-Gandara, J. (2021). A molecular modelling approach for identifying antiviral selenium-containing heterocyclic compounds that inhibit the main protease of SARS-CoV-2: An in silico investigation. Briefings in Bioinformatics, 22(2), 1476–1498. https://doi.org/10.1093/bib/bbab045
Nogara, P. A., Omage, F. B., Bolzan, G. R., Delgado, C. P., Aschner, M., Orian, L., & Teixeira Rocha, J. B. (2021). In silico studies on the interaction between Mpro and PLpro From SARS-CoV-2 and Ebselen, its metabolites and derivatives. Molecular Informatics, 40(8), 2100028. https://doi.org/10.1002/minf.202100028
Karges, J., Giardini, M. A., Blacque, O., Woodworth, B., Siqueira-Neto, J. L., & Cohen, S. M. (2023). Enantioselective inhibition of the SARS-CoV-2 main protease with rhenium (I) picolinic acid complexes. Chemical Science, 14(3), 711–720. https://doi.org/10.1039/d2sc05473f
Gil-Moles, M., O’Beirne, C., Esarev, I. V., Lippmann, P., Tacke, M., Cinatl, J., Bojkova, D., & Ott, I. (2023). Silver N-heterocyclic carbene complexes are potent uncompetitive inhibitors of the papain-like protease with antiviral activity against SARS-CoV-2. RSC Medicinal Chemistry, 14(7), 1260–1271. https://doi.org/10.1039/d3md00067b
Clausen, T. M., Sandoval, D. R., Spliid, C. B., Pihl, J., Perrett, H. R., Painter, C. D., Narayanan, A., Majowicz, S. A., Kwong, E. M., McVicar, R. N., Thacker, B. E., Glass, C. A., Yang, Z., Torres, J. L., Golden, G. J., Bartels, P. L., Porell, R. N., Garretson, A. F., Laubach, L., & Esko, J. D. (2020). SARS-COV-2 infection depends on cellular heparan sulfate and ACE2. Cell, 183(4), 1043-1057.e15. https://doi.org/10.1016/j.cell.2020.09.033
Liu, L., Chopra, P., Li, X., Bouwman, K. M., Tompkins, S. M., Wolfert, M. A., De Vries, R. P., & Boons, G. (2021). Heparan sulfate proteoglycans as attachment factor for SARS-COV-2. ACS Central Science, 7(6), 1009–1018. https://doi.org/10.1021/acscentsci.1c00010
Nie, C., Pouyan, P., Lauster, D., Trimpert, J., Kerkhoff, Y., Szekeres, G. P., Wallert, M., Block, S., Sahoo, A. K., Dernedde, J., Pagel, K., Kaufer, B. B., Netz, R. R., Ballauff, M., & Haag, R. (2021). Polysulfates block SARS-CoV-2 uptake through electrostatic interactions. Angewandte Chemie, 60(29), 15870–15878. https://doi.org/10.1002/anie.202102717
Zhang, Q., Radvak, P., Lee, J., Xu, Y., Cao-Dao, V., Xu, M., Zheng, W., Chen, C. Z., Xie, H., & Ye, Y. (2022). Mitoxantrone modulates a heparan sulfate-spike complex to inhibit SARS-CoV-2 infection. Scientific Reports. https://doi.org/10.1038/s41598-022-10293-x
Kwon, P. S., Xu, S., Oh, H., Kwon, S., Rodrigues, A. L., Feroz, M., Fraser, K., He, P., Zhang, F., Hong, J. J., Linhardt, R. J., & Dordick, J. S. (2023). Suramin binds and inhibits infection of SARS-CoV-2 through both spike protein-heparan sulfate and ACE2 receptor interactions. Communications Biology. https://doi.org/10.1038/s42003-023-04789-z
Shapira, T., Monreal, I. A., Dion, S. P., Buchholz, D. W., Imbiakha, B., Olmstead, A. D., Jager, M., Désilets, A., Gao, G., Martins, M., Vandal, T., Thompson, C. A. H., Chin, A., Rees, W. D., Steiner, T., Nabi, I. R., Marsault, E., Sahler, J., Diel, D. G., & Jean, F. (2022). A TMPRSS2 inhibitor acts as a pan-SARS-CoV-2 prophylactic and therapeutic. Nature, 605(7909), 340–348. https://doi.org/10.1038/s41586-022-04661-w
Li, K., Meyerholz, D. K., Bartlett, J. A., & McCray, P. B., Jr. (2021). The TMPRSS2 inhibitor nafamostat reduces SARS-CoV-2 pulmonary infection in mouse models of COVID-19. MBio. https://doi.org/10.1128/mBio.00970-21
Wettstein, L., Immenschuh, P., Weil, T., Conzelmann, C., Almeida-Hernández, Y., Hoffmann, M., Kempf, A., Nehlmeier, I., Lotke, R., Petersen, M., Stenger, S., Kirchhoff, F., Sauter, D., Pöhlmann, S., Sanchez-Garcia, E., & Münch, J. (2022). Native and activated antithrombin inhibits TMPRSS2 activity and SARS-CoV-2 infection. Journal of Medical Virology. https://doi.org/10.1002/jmv.28124
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Thamby Rajah Mahendran devised the idea for the manuscript. Thamby Rajah Mahendran, Binsin Cynthia and Ramesh Thevendran performed literature search, and wrote the first draft. Thamby Rajah Mahendran and Binsin Cynthia designed the figures. Maheswaran Solayappan critically reviewed this manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mahendran, T.R., Cynthia, B., Thevendran, R. et al. Prospects of Innovative Therapeutics in Combating the COVID-19 Pandemic. Mol Biotechnol (2024). https://doi.org/10.1007/s12033-024-01240-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12033-024-01240-4