Abstract
Atherosclerosis is a pathology leading to cardiovascular diseases with high epidemiologic impact; thus, new therapies are required to fight this global health issue. Immunotherapy is a feasible approach to treat atherosclerosis and given that genetically engineered plants are attractive hosts for vaccine development; we previously proved that the plant cell is able to synthesize a chimeric protein called CTB:p210:CETPe, which is composed of the cholera toxin B subunit (CTB) as immunogenic carrier and target epitopes from the cholesteryl ester transfer protein (CETP461–476) and apolipoprotein B100 (p210). Since CTB:p210:CETPe was expressed in tobacco at sufficient levels to evoke humoral responses in mice, its expression in carrot was explored in the present study looking to develop a vaccine in a safe host amenable for oral delivery; avoiding the purification requirement. Carrot cell lines expressing CTB:p210:CETPe were developed, showing accumulation levels up to 6.1 µg/g dry weight. An immunoblot analysis revealed that the carrot-made protein is antigenic and an oral mice immunization scheme led to evidence on the immunogenic activity of this protein; revealing its capability of inducing serum IgG responses against p210 and CETP epitopes. This study represents a step forward in the development of an attractive oral low-cost vaccine to treat atherosclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atherosclerosis is a chronic inflammatory disease characterized by the deposition of cholesterol and fat in blood vessels with proliferation of inflammation-promoting cells, which results in the formation of an atheroma [1]. Given that the immune system is involved in the pathogenesis of atherosclerosis; immunotherapies to modulate or induce specific immune responses have been explored. One approach consists in the modulation of the inflammatory responses against self-antigens that contribute to atherosclerosis progression [2,3,4]. This approach has been explored for self-antigens derived from ApoB100, which is the main protein component of the low-density lipoproteins [5,6,7]. The protective effect of a prototype vaccine targeting p210 from ApoB100 was inhibited by administering anti-CD25 antibodies, suggesting that regulatory T cells (Tregs) mediate the protection provided by the vaccine [8]. It has also been shown that the administration of antibodies targeting p45 and p210 led to atheroprotective effects, indicating that activation of Th2 responses also plays an important therapeutic role [9, 10]. The cholesteryl ester transfer protein (CETP) has also been targeted through vaccines intended to induce humoral responses able to block this enzyme with the subsequent decrease in the HDL depletion it mediates [11,12,13].
Although the scenario on developing atherosclerosis vaccines is promising since it is expected that a number of atherosclerosis vaccine candidates will enter clinical trials in the following years; the cost of vaccination is an important factor to be considered to ensure proper vaccine coverage, especially in the developing world where access to vaccines is still limited. Plants offer an alternative to develop vaccine production platforms with singular advantages that not only comprise low cost but enhanced safety (plants do not replicate human pathogens), high biosynthetic capacity, the possibility of production in contained systems (bioreactors or greenhouses), and the possibility of using the plant cell itself as delivery vehicle of oral formulations based on freeze-dried plant biomass rendering easy to administer vaccines [14, 15].
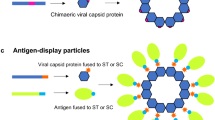
Our research group recently reported a plant-made vaccine candidate (CTB:p210:CETPe) targeting both ApoB100 and CETP using the cholera toxin B subunit (CTB) as the immunogenic carrier [16]. The vaccine candidate produced in tobacco plants elicited specific IgG responses against both epitopes when subcutaneous administration in mice was assessed. In this study we addressed the next step in the development of an attractive plant-made vaccine targeting atherosclerosis by expressing the CTB:p210:CETPe antigen in an edible crop, carrot, which opens the path for developing oral formulations. The oral immunogenicity of the carrot-made vaccine is reported.
Materials and Methods
Development of Transgenic Carrot Cell Lines
A synthetic gene, named CTB:p210:CETPe, was previously designed to encode a chimeric protein (CTB:p210:CETPe) and cloned in the pBI121 vector under control of the CaMV35S promoter [16]. Agrobacterium tumefaciens strain GV3101 containing the expression vector was used for carrot genetic transformation experiments. The recombinant Agrobacterium strain was grown in YM medium supplemented with 100 mg/L kanamycin at 28 °C. Carrot transformation was carried out following a previously described method [17]. Briefly, carrot (Daucus carota L.) seeds were surface-sterilized with 50% commercial Clorox bleach for 15 min and washed five times with sterilized water (5 min per rinse). Seeds were afterward treated with 0.01 M HCl in sterilized water for 15 min, washed five times with sterilized water, and germinated in 15 × 100 mm glass jars containing Murashige and Skoog (MS) medium. Cultures were maintained under a 16-h photoperiod (100 µmol/m2 s) at 25 °C for 4–5 weeks. Stems from carrot seedlings were cut into segments of 7–10 mm in length on a wet sterile filter paper. Explants were incubated in an overnight-grown culture of Agrobacterium carrying the pBI-CTB:p210:CETPe vector (OD600nm = 0.5) for 15 min, transferred onto the co-cultivation medium [MS basal medium supplemented with 1.33 µM 6-benzyladenine (BA) and 4.52 µM 2,4-dichlorophenoxyacetic acid (2,4-D)], and co-cultivated in the dark for 48 h. Explants were thoroughly washed with sterilized water and cultured on selection medium [MS basal medium supplemented with 1.33 µM BA and 4.52 µM 2,4-D along with 500 mg/L cefotaxime and 50 mg/L kanamycin]. Cultures were grown under a 16 h photoperiod (100 µmol/m2 s) at 25 °C and transferred once every 2 weeks onto a fresh selection medium. The rescued kanamycin resistant calli were propagated in selective media, and the biomass was freeze-dried in a LABCONCO equipment (conditions: −75 °C, 0.133 mBar for 36 h), and milled for further characterization.
Transgene Detection by PCR
Total DNA was isolated from carrot callus from putative transformed and wild-type lines according to Dellaporta et al. [18]. The pBI-CTB:p210:CETPe vector was used as positive control for this assay. A 25-µL PCR reaction mixture was set to amplify the CTB:p210:CETPe gene, which contained 1 × PCR buffer, 100 ng DNA, 1.5 mM magnesium chloride, 2.5 U Taq DNA polymerase (New England BioLabs, Ipswich, MA), 1 mM dNTPs, and 1 µM of primers (sense: 5′TACAGATTTGTGTGC; antisense: 5′GTGTTCAGGAAAACCG). Cycling conditions were: 95 °C for 5 min (initial denaturation), 35 cycles at 95 °C for 30 s, 50 °C for 30 s, 72 °C for 45 s, and a final extension at 72 °C for 10 min. This procedure was performed in a MultiGeneTM Mini Personal Thermal Cycler (Labnet). PCR products were analyzed by electrophoresis using 1% agarose gels.
CTB:p210:CETPe Detection by Western Blot and ELISA
Expression of CTB:p210:CETPe in the candidate carrot callus lines was assessed by Western blot assay. Protein extracts were obtained by milling in a mortar 50 mg of fresh callus in the presence of 200 µL of protein extraction buffer (750 mM Tris–HCl, pH 8, 15% sucrose, 100 mM β-mercaptoethanol, and 1 mM PMSF). The resulting extracts were clarified by centrifugation at 16,000×g for 15 min, and 50 µL aliquots were mixed with 50 µL of 1 × reducing loading buffer. The cholera toxin B subunit from Vibrio cholerae (Sigma, St. Louis, MO) was used as positive control. Samples were denatured by boiling for 5 min at 95 °C; SDS-PAGE was performed using 4–12% acrylamide gels under denaturing conditions. Gels were blotted onto BioTrace PVDF membranes (Pall Corporation, NY) using a TV100-EBK Electroblotter (AlphaMetrix Biotech, GER) for 1 h at 150 V in a methanol-based transfer buffer. After blocking with PBST plus 5% fat-free milk, the blots were incubated overnight with hyperimmune sera against either CT (1:500 dilution) or p210 (1:200 dilution). Horseradish peroxidase-conjugated secondary goat anti-mouse antibody (1:2000 dilution, Sigma, St. Louis, MO) was applied for 2 h at room temperature. Antibody binding was detected by incubation with the SuperSignal West Dura solution following instructions from the manufacturer (Thermo Scientific, Waltham, MA). Signal detection was performed by means of an X-ray film following standard procedures.
The expression levels of CTB:p210:CETPe and GM1 binding activity were analyzed by ganglioside-dependent ELISA (GM1-ELISA). Ninety-six-well polystyrene plates were individually coated overnight at 4 °C with Type III GM1 ganglioside at 1.5 µg/well dissolved in carbonate buffer (15 mM Na2CO3 and 35 mM NaHCO3). During the assay, three washes with PBST were performed between each step. The plates were blocked with 5% fat-free dry milk for 2 h at 25 °C. Protein extracts were obtained by milling in a mortar 25 mg of freeze-dried calluses in the presence of 500 µL of extraction buffer (750 mM Tris–HCl, pH 8, 15% sucrose, and 1 mM PMSF). The extracts were clarified by centrifugation at 16,000×g for 15 min at 4 °C and applied to blocked plates. After overnight incubation at 4 °C, anti-CT serum (1:500 dilution) was added and an incubation at 25 °C for 4 h was performed. A goat horseradish peroxidase-conjugated anti-mouse IgG (1:2000 dilution, Sigma, St. Louis, MO) was used for secondary labeling during 1 h at 25 °C. ABTS substrate solution [0.6 mM 2,2′-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS; Sigma, St. Louis, MO), 0.1 M citric acid, 1 mM of H2O2, pH 4.35] was added, and after an incubation for 30 min at 25 °C OD values at 405 nm were recorded in a Thermo Scientific Multiskan® FC microplate photometer (Thermo Scientific, Waltham, MA). A standard curve was included in the assay using known amounts of unmodified pure CTB to quantify the content of the recombinant protein in carrot calli.
Immunogenicity Assessment in Mice
Immunogenicity of the carrot-made CTB:p210:CETPe was assessed in 12-week-old female BALB/c mice with 25 g of body weight. Test animals were maintained under standard conditions with free access to food and water according to the procedures indicated by the Federal Regulations for Animal Experimentation and Care (SAGARPA, NOM-062-ZOO-1999, México). The protocol was approved by the Institutional Animal Care and Use Committee.
Four BALB/c mice groups were randomly established (n = 4) and the immunization schemes comprised four doses administered once a week by either oral or subcutaneous route. Doses were administered on days 1, 8, 15, and 22; consisting of 50 mg freeze-dried callus for oral administration (305 ng of CTB:p210:CETPe) or soluble protein extracted from 10 mg freeze-dried callus for subcutaneous administration (61 ng of CTB:p210:CETPe), from transgenic or WT lines. The doses were prepared milling freeze-dried leaf tissue in 100 μL of PBS. In the case of s.c. doses, extracts were clarified by centrifugation at 16,000×g for 15 min. Mice were bled on days 0 (preimmunization), 14, 21, and 28. Feces samples were collected from mice on day 35 and resuspended in 200 µL of ice-cold PBS supplemented with 5% fat-free milk and 1 mM of PMSF. Fecal extracts were clarified by centrifugation at 16,000×g for 15 min at 4 °C. Test animals were subsequently killed on day 35 by cervical dislocation, serum and fecal samples collected and stored at −80 °C until antibody content analysis. ELISA was performed to determine the presence of anti-p210 and anti-CETP IgG antibodies in serum and anti-p210 IgA antibodies in fecal samples. Ninety-six-well polystyrene plates were coated overnight at 4 °C with 1 µg/well of p210 synthetic peptide (sequence: KTTKQSFDLSVKAQYKKNKH; GenScript Co. USA) or 1 µg/well of CETPe synthetic peptide (sequence: FGFPEHLLVDFLQSLS; GenScript Co. USA). ELISA protocol comprised three washes with PBST between each step. Plates were blocked with 5% fat-free dry milk for 2 h at 25 °C. Serial dilutions of mice sera were added (1:20–1:80) and plates incubated at 4 °C overnight. A goat horseradish peroxidase-conjugated anti-mouse IgG was added as the secondary antibody (1:2000 dilution, Sigma, St. Louis, MO) and plates incubated for 2 h at 25 °C. Antibody binding detection was performed as described in the previous subheading.
Statistical Analysis
ELISA data from immunogenicity assays were analyzed by one-way ANOVA using Minitab 15 software. A p value less than 0.05 was considered statistically significant.
Results
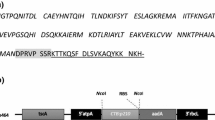
The CTB:p210:CETPe protein is an immunogen designed to induce humoral responses against epitopes from CETP and ApoB100 that contains CTB as a carrier to confer high immunogenicity in mucosal compartments. Carrot cell lines expressing CTB:p210:CETPe could serve as source of a bivalent low-cost vaccine against atherosclerosis. To express CTB:p210:CETPe in carrot cells a previously constructed vector was used (pBI-CTB:p210:CETPe), which mediates the constitutive expression of the antigen driven by the 35SCaMV promoter.
Agrobacterium tumefaciens-mediated transformation of carrot explants derived from in vitro germinated seedlings, allowed rescuing 20 putative transgenic carrot lines in kanamycin-containing media 2 months after co-culture. The candidate lines were propagated in selective media over a period of 6 months to obtain sufficient material for screening. Among the 20 rescued lines, four of them showed slow growth rates and eventually died. From the 16 lines that remained alive in selective media, seven were selected for further analysis based on their sustained growth under the selection pressure. The seven selected lines were first subjected to PCR analysis to detect the CTB:p210:CTPe transgene. Agarose gel analysis of PCR reactions revealed the presence of the expected CTB:p210:CETPe-derived amplicons (450 bp) in all tested lines (Fig. 1). No amplicons were detected for the PCR reaction loaded with DNA from the WT carrot line.
Detection of the CTB:p210:CETPe gene in transformed carrot callus lines. Genomic DNA samples from either putative transformed or wild-type carrot calli were assessed by PCR for the presence of the CTB:p210:CETPe gene using specific primers (PCR product: 450 bp). Lanes: MW, molecular weight marker; (+), positive control (pBI-CTB:p210:CETPe vector as template); 1, wild-type line; 2–8 candidate lines C5, C8, C15, C13, C3, C6, and C12; respectively
To explore the ability of carrot cells to synthesize the CTB:p210:CETPe protein, preliminary anti-CTB ELISA revealed that five lines possess the highest OD readings (data not shown); thus further analyses were focused on these lines (called C3, C5, C12, C13, and C15). Analysis by Western blot labeling was conducted to test the presence and integrity of the pBI-CTB:p210:CETPe fusion protein. Labeling with anti-CT serum revealed the presence of a ~13 kDa immunoreactive protein in samples from all the tested transgenic carrot lines (Fig. 2a). The positive control showed a ~12 kDa protein, which is in agreement with the theoretical molecular weight of CTB. Upon labeling with an anti-p210 serum, a 15-kDa immunoreactive protein was also detected; whereas the extract from the WT carrot showed no signal (Fig. 2b).
Immunodetection of the plant-made CTB:p210:CETPe antigen in callus carrot lines. a Western blot using an anti-CT antisera for labeling. Lanes: 1, positive control (250 ng of unmodified pure CTB); 2–8, protein extracts from lines C5, C15, C13, C6, C3, C12, and C8, respectively; line 9, protein extract from wild-type callus carrot line. b Western blot using an anti-p210 antisera for labeling. Lines: 1–5, protein extracts from lines C5, C15, C13, C3, and C12, respectively; line 6, protein extract from wild-type carrot callus line
To determine the accumulation levels and the in vitro GM1 binding activity of the carrot-made CTB:p210:CETPe protein, a GM1-ELISA was performed using an anti-CTB hyperimmune serum for labeling. Significantly higher signals were recorded for the transgenic lines when compared to those of the WT line (Fig. 3b), indicating a positive immunodetection of the CTB:p210:CETPe protein able to bind the GM1 ganglioside, which is an evidence on the ability of the plant-made chimeric antigen to form the pentameric structure. The standard curve made with unmodified pure CTB was used to estimate the reached levels of the CTB:p210:CETPe protein in the transformed lines. Transgenic carrot lines accumulated the CTB:p210:CETPe immunogen at up to 6.1 µg/g freeze-dried weight, with C15 as the most productive line.
Immunodetection of CTB:p210:CETPe produced in carrot callus lines. a Standard curve made with unmodified pure CTB protein solutions (0.8–50 ng/well) to estimate accumulation levels of CTB:p210:CETPe content in freeze-dried calli. b GM1-ELISA analysis to measure CTB:p210:CETPe content in carrot lines. An anti-CTB serum was used for labeling. Data represents mean values ± SD
The immunogenic potential of the carrot-made CTB:p210:CETPe vaccine was next assessed in BALB/c mice. After a scheme comprising four immunizations with material from the C15 carrot line, either by the oral or subcutaneous routes; ELISA revealed the presence of significant levels of IgG anti-CETP (Fig. 4a) and anti-p210 antibodies (Fig. 4b) in serum from mice groups immunized with the C15 line by either p.o. or s.c. routes. The levels of antibodies induced against the two target molecules (CETP and p210) were similar in magnitude for both administration routes. A significant IgA mucosal response against p210 was detected in feces from mice immunized by either oral or s.c. routes, with lower levels in the s.c. immunized group (p < 0.05, Fig. 5).
Systemic humoral responses induced in BALB/c mice upon oral or subcutaneous immunization with the carrot-made CTB:p210:CETPe antigen. Mice groups were subjected to a 4-week immunization scheme with biomass (oral) or tissue extract (subcutaneous) from wt or the C15 transgenic carrot callus line. a Anti-CETP or b anti-p210 antibody levels were determined by ELISA using the corresponding targets in the form of synthetic peptides. Mean OD405nm values ± SD from each experimental group (n = 4) are shown. The asterisks denote significant differences versus the group treated with the WT carrot (p < 0.05)
Mucosal humoral responses induced in BALB/c mice upon oral or subcutaneous immunization with the carrot-made CTB:p210:CETPe antigen. Mice groups were subjected to a 4-week immunization scheme with biomass (oral) or tissue extract (subcutaneous) from wt or the C15 transgenic carrot callus line. Anti-p210 IgA levels were determined by ELISA using the p210 peptide as target. Mean OD405nm values ± SD from each experimental group (n = 4) are shown. The asterisks denote significant differences versus the group treated with the WT carrot, whereas the double dagger denotes significant differences versus the group treated orally with the carrot-made CTB:p210:CETPe (p < 0.05)
Discussion
In the present study, a step forward in the development of an oral, low-cost vaccine against atherosclerosis was accomplished. Carrot callus lines were explored as biofactories of the CTB:p210:CETPe antigen to generate edible plant biomass amenable for the delivery of antigens by the oral route without the need of complex purification processes. The CTB:p210:CETPe encoding transgene was successfully transferred to the carrot genome by A. tumefaciens-mediated transformation. Lines were cultured during a long period in selective media, and the analyzed lines were positive for the presence of the transgene, indicating that stable transformation was achieved. In terms of yields, carrot lines accumulated the CTB:p210:CETPe antigen at levels up to 6.1 µg/g freeze-dried biomass; which is in the range of expression for other CTB-based antigens expressed in plants [19].
According to ELISA, the carrot-made CTB:p210:CETPe retained the antigenic determinants of the p210 and CETP target epitopes. Moreover, positive results from the GM1-ELISA also indicated that the carrot-made CTB:p210:CETPe chimera (comprising CTB as an immunogenic carrier) retained the GM1 binding activity of CTB, which is critical for the transmucosal transport of the antigen and uptake by antigen presenting cells [20]. The integrity of the CTB:p210:CETPe antigen was also evidenced by Western blot assays where it showed lower mobility than that of the unmodified pure CTB protein.
The achievement of immunogenic activity using orally administered antigens is a challenging goal: the vaccine must provide an efficient delivery of the vaccine antigens to the innate, local, and systemic immune systems and be able to break the tolerogenic environment. In our study we explored the potential of carrot cells to deliver the CTB:p210:CETPe antigen with the subsequent induction of humoral responses against the target epitopes from ApoB100 and CETP. Subcutaneous administration was also performed to compare the response attained through oral immunization. The carrot-made vaccine was capable of eliciting humoral responses against both p210 and CETP epitopes upon oral and subcutaneous immunization. Interestingly, the levels of antibodies attained by oral immunization with carrot-made CTB:p210:CETPe were similar to those raised by subcutaneous immunization. This is a relevant observation since oral immunization typically leads to modest responses that are lower than those attained through parenteral routes [21].
Thus, the carrot-made CTB:p210:CETPe possesses an attractive immunogenic potential that is attributed, in part, to the use of CTB as an immunomodulator carrier. This is in agreement with other studies that adopted CTB as an immunogenic carrier of human autoantigens leading to protective immune responses in mice [22, 23]. It is known that CTB pentamers bind to the GM1 ganglioside located at the gut epithelial cell surface, which results in the induction of both systemic and mucosal responses [24]. Another factor to consider is the role of the plant cell as a delivery vehicle that not only delays protein degradation but leads to a gradual antigen release that makes it bioavailable [25].
Several efforts are ongoing to develop vaccines targeting CETP, which is intended to induce CETP blocking antibodies with the subsequent increase of HDL-C. Among the candidates, there is a version comprising a fusion of an epitope (aa 830–843) from the tetanus toxin and an epitope (aa 461–476) from human CETP; which led to positive outcomes in preclinical and phase I clinical trials [11, 26]. Another recently described vaccine candidate [27] consisted of a fusion protein comprising six tandem repeats of the CETP epitope (aa 461–476) and an IgG Fc domain (Fc-CETP6), which led to therapeutic effects in preclinical trials performed in rabbits. In the case of the p210 epitope from ApoB100, vaccines are intended to induce p210-specific antibodies and the expansion of Tregs that suppress the inflammatory response at the atherosclerotic lesions. For instance, a vaccine based on p210 fused to CTB-induced atheroprotective effects in a mouse model upon intranasal immunization; these effects are associated to IL-10+ regulatory Tr1 cells and p210-specific antibody responses [28]. A vaccine consisting of p2, p45, or p210 peptides from ApoB100 coupled to BSA has also shown atheroprotective effects in mice upon subcutaneous immunization, inducing IgG1-specific antibodies, Tregs (CD4+ and CD8+), and increased levels of IL-10 [29]. The above-mentioned vaccines are directed against a single target, imply high-cost production processes due to the employed expression/synthesis systems and the purification steps needed, and most of them were parenterally administered. Our CTB:p210:CETPe carrot-made vaccine constitutes the first atherosclerosis vaccine candidate produced in a generally recognized as safe (GRAS) host, opening the path for the development of oral vaccines not requiring complex processing [30]. In addition, since this vaccine targets both CETP and ApoB100, it is proposed as a vaccine with enhanced efficacy with respect to other candidates.
In the molecular pharming arena, the use of carrot cells offers substantial advantages over the tobacco model. Carrot is considered a safe material with GRAS status and thus will be used as a straightforward system for the formulation of oral vaccines avoiding the sophisticated downprocessing required for other hosts [31]. It is proposed that freeze-dried biomass can be encapsulated in gelatin capsules [32]. Moreover, carrot has been successfully applied in the production of biopharmaceuticals; in particular Protalix BioTherapeutics has achieved the commercialization of the glucocerebrosidase for enzyme replacement therapy in Gaucher’s disease patients [33]. In addition, several other products are under development, including products to be based on carrot cells as the delivery vehicles [34]. In vitro propagation of carrot callus or generation of suspension cultures offers enhanced biosafety since growing plants in greenhouses is avoided.
The immunogenicity proven in test BALB/c mice justifies further studies in atherosclerosis animal models to determine the atheroprotective effects. Ongoing experiments pursue determining the immunogenicity of the CTB:p210:CETPe carrot-made vaccine in rabbits to evaluate the potential of preventing or reducing atherosclerotic lesions once subjected to high cholesterol diet. In conclusion, the CTB:p210:CETPe carrot-made vaccine is a promising tool for the development of atherosclerosis oral vaccines, which are the ideal mode of immunization in terms of safety, costs, and patient’s comfort.
References
Sakakura, K., Nakano, M., Otsuka, F., Ladich, E., Kolodgi, F. D., & Virmani, R. (2013). Pathophysiology of atherosclerosis plaque progression. Heart, Lung and Circulation, 22, 399–411.
Shah, P. K., Chyu, K. Y., Dimayuga, P. C., & Nilsson, J. (2014). Vaccine for atherosclerosis. Journal of the American College of Cardiology, 64, 2779–2791.
Kimura, T., Tse, K., Sette, A., & Ley, K. (2015). Vaccination to modulate atherosclerosis. Autoimmunity, 48, 152–160.
Nilsson, J., Lichtman, A., & Tedgui, A. (2015). Atheroprotective immunity and cardiovascular disease: Therapeutic opportunities and challenges. Journal of Internal Medicine, 278, 507–519.
Fredrikson, G. N., Söderberg, I., Lindholm, M., Dimayuga, P., Chyu, K. Y., Shah, P. K., et al. (2003). Inhibition of atherosclerosis in ApoE-null mice by immunization with ApoB-100 peptide sequence. Arteriosclerosis, Thrombosis, and Vascular Biology, 23, 879–884.
Fredrikson, G. N., Andersson, L., Söderberg, I., Dimayuga, P., Chyu, K. Y., Shah, P. K., et al. (2005). Atheroprotective immunization with MDA-modified apo B-100 peptide sequences is associated with activation of Th2 specific antibody expression. Autoimmunity, 38, 171–179.
Fredrikson, G. N., Björkbacka, H., Söderberg, I., Ljungcrantz, I., & Nilsson, J. (2008). Treatment with apoB peptide vaccines inhibits atherosclerosis in human apo B-100 transgenic mice without inducing an increase in peptide-specific antibodies. Journal of Internal Medicine, 264, 563–570.
Wigren, M., Kolbus, D., Dunér, P., Ljungcrantz, I., Söderberg, I., Björkbacka, H., et al. (2011). Evidence for a role of regulatory T cells in mediating the atheroprotective effect of apolipoprotein B peptide vaccine. Journal of Internal Medicine, 269, 546–556.
Schiopu, A., Bengtsson, J., Söderberg, I., Janciauskiene, S., Lindgren, S., Ares, M. P., et al. (2004). Recombinant human antibodies against aldehyde-modified apolipoprotein B-100 peptide sequences inhibit atherosclerosis. Circulation, 110, 2047–2052.
Schiopu, A., Frendéus, B., Jansson, B., Söderberg, I., Ljungcrantz, I., Araya, Z., et al. (2007). Recombinant antibodies to an oxidized low-density lipoprotein epitope induce rapid regression of atherosclerosis in apobec-1(−/−)/low-density lipoprotein receptor(−/−) mice. Journal of the American College of Cardiology, 50, 2313–2318.
Rittershaus, C. W., Miller, D. P., Thomas, L. J., Picard, M. D., Honan, C. M., Emmett, C. D., et al. (2000). Vaccine-induced antibodies inhibit CETP activity in vivo and reduce aortic lesions in a rabbit model of atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 20, 2106–2112.
Gaofu, Q., Dan, M., Jie, W., Liao, Z., Li, Z., Roque, R. S., et al. (2004). Long-lasting specific antibodies against CETP induced by subcutaneous and mucosal administration of a 26-amino acid CETP epitope carried by heat shock protein 65 kDa in the absence of adjuvants. Vaccine, 22, 3187–3194.
Gaofu, Q., Jun, L., Xin, Y., Wentao, L., Jie, W., Xiuyun, Z., et al. (2005). Vaccinating rabbits with a cholesteryl ester transfer protein (CETP) B-Cell epitope carried by heat shock protein-65 (HSP65) for inducing anti-CETP antibodies and reducing aortic lesions in vivo. Journal of Cardiovascular Pharmacology, 45, 591–598.
Pniewski, T., Czyż, M., Wyrwa, K., Bociąg, P., Krajewski, P., & Kapusta, J. (2017). Micropropagation of transgenic lettuce containing HBsAg as a method of mass-scale production of standardised plant material for biofarming purposes. Plant Cell Reports, 36, 49–60.
Czyż, M., Dembczyński, R., Marecik, R., Wojas-Turek, J., Milczarek, M., Pajtasz-Piasecka, E., et al. (2014). Freeze-drying of plant tissue containing HBV surface antigen for the oral vaccine against hepatitis B. BioMed Research International, 2014, 485689.
Salazar-Gonzalez, J. A., Rosales-Mendoza, S., Romero-Maldonado, A., Monreal-Escalante, E., Uresti-Rivera, E. E., & Bañuelos-Hernández, B. (2014). Production of a plant-derived immunogenic protein targeting ApoB100 and CETP: Toward a plant-based atherosclerosis vaccine. Molecular Biotechnology, 56, 1133–1142.
Rosales-Mendoza, S., Soria-Guerra, R. E., de Jesús Olivera-Flores, M. T., López-Revilla, R., Argüello-Astorga, G. R., Jiménez-Bremont, J. F., et al. (2007). Expression of Escherichia coli heat-labile enterotoxin b subunit (LTB) in carrot (Daucus carota L.). Plant Cell Reports, 26, 969–976.
Dellaporta, S. L., Wood, J., & Hicks, J. B. (1983). A plant DNA mini preparation: Version II. Plant Molecular Biology Reporter, 1, 19–21.
Daniell, H., Singh, N. D., Mason, H., & Streatfield, S. J. (2009). Plant-made vaccine antigens and biopharmaceuticals. Trends in Plant Science, 14, 669–679.
Basu, I., & Mukhopadhyay, C. (2014). Insights into binding of cholera toxin to GM1 containing membrane. Langmuir, 30, 15244–15252.
Grassly, N. C., Kang, G., & Kampmann, B. (2015). Biological challenges to effective vaccines in the developing world. Philosophical Transactions of the Royal Society of London Series B Biological Sciences, 370, 20140138.
Herzog, R. W., Nichols, T. C., Su, J., Zhang, B., Sherman, A., Merricks, E. P., et al. (2017). Oral tolerance induction in hemophilia B dogs fed with transplastomic lettuce. Molecular Therapy, 25, 512–522.
Ruhlman, T., Ahangari, R., Devine, A., Samsam, M., & Daniell, H. (2007). Expression of cholera toxin B-proinsulin fusion protein in lettuce and tobacco chloroplasts–oral administration protects against development of insulitis in non-obese diabetic mice. Plant Biotechnology Journal, 5, 495–510.
Holmgren, J., Lycke, N., & Czerkinsky, C. (1993). Cholera toxin and cholera B subunit as oral–mucosal adjuvant and antigen vector systems. Vaccine, 11, 1179–1184.
Rosales-Mendoza, S., & Salazar-González, J. A. (2014). Immunological aspects of using plant cells as delivery vehicles for oral vaccines. Expert Review of Vaccines, 13, 737–749.
Davidson, M. H., Maki, K., Umporowicz, D., Wheeler, A., Rittershaus, C., & Ryan, U. (2003). The safety and immunogenicity of a CETP vaccine in healthy adults. Atherosclerosis, 169, 113–120.
Liaw, Y. W., Lin, C. Y., Lai, Y. S., Yang, T. C., Wang, C. J., Whang-Peng, J., et al. (2014). A vaccine targeted at CETP alleviates high fat and high cholesterol diet-induced atherosclerosis and nonalcoholic steatohepatitis in rabbit. PLoS ONE, 9, e111529.
Klingenberg, R., Lebens, M., Hermansson, A., Fredrikson, G. N., Strodthoff, D., Rudling, M., et al. (2010). Intranasal Immunization with an apolipoprotein B-100 fusion protein induces antigen-specific regulatory T cells and reduces atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology, 30, 946–952.
Pierides, C., Bermudez-Fajardo, A., Fredrikson, G. N., Nilsson, J., & Oviedo-Orta, E. (2013). Immune responses elicited by apoB-100-derived peptides in mice. Immunologic Research, 56, 96–108.
Govea-Alonso, D. O., Beltrán-López, J., Salazar-González, J. A., Vargas-Morales, J., & Rosales-Mendoza, S. (2017). Progress and future opportunities in the development of vaccines against atherosclerosis. Expert Review of Vaccines, 16, 337–350.
Rosales-Mendoza, S., Angulo, C., & Meza, B. (2016). Food-grade organisms as vaccine biofactories and oral delivery vehicles. Trends in Biotechnology, 34, 124–136.
Lakshmi, P. S., Verma, D., Yang, X., Lloyd, B., & Daniell, H. (2013). Low cost tuberculosis vaccine antigens in capsules: Expression in chloroplasts, bio-encapsulation, stability and functional evaluation in vitro. PLoS ONE, 8, e54708.
Rosales-Mendoza, S., & Tello-Olea, M. A. (2015). Carrot cells: A pioneering platform for biopharmaceuticals production. Molecular Biotechnology, 57, 219–232.
Shaaltiel, Y., Gingis-Velitski, S., Tzaban, S., Fiks, N., Tekoah, Y., & Aviezer, D. (2015). Plant-based oral delivery of β-glucocerebrosidase as an enzyme replacement therapy for Gaucher’s disease. Plant Biotechnology Journal, 13, 1033–1040.
Acknowledgements
We acknowledge Andrea Romero-Maldonado for helping on antisera production. Current investigations from the group are supported by CONACYT/México (Grant INFR-2016-271182 and CB-256063 to SRM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Govea-Alonso, D.O., Tello-Olea, M.A., Beltrán-López, J. et al. Assessment of Carrot Callus as Biofactories of an Atherosclerosis Oral Vaccine Prototype. Mol Biotechnol 59, 482–489 (2017). https://doi.org/10.1007/s12033-017-0036-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12033-017-0036-5