Abstract
Calcium phosphate cements (CPCs) are a new generation of bone repair materials with good biocompatibility for various stem cells. The minipig is a recommended large animal model for bone engineering research. This study aimed to evaluate the feasibility of utilizing CPC scaffolds for the adhesion, proliferation, and osteogenic differentiation of minipig’s bone marrow mesenchymal stem cells (pBMSCs). Passage 3 pBMSCs were seeded on the CPC scaffold and cultured with osteogenic culture medium (osteogenic group) or normal medium (control group). The density of viable cells increased in both groups, and pBMSCs firmly attached and spread well on the CPC scaffold. The alkaline phosphatase (ALP) activity in the osteogenic group had significantly increased on day 7 (D7) and peaked on D14. qRT-PCR revealed that mRNA levels of ALP and three osteogenic marker genes were significantly higher on D4, D7, and D14 in the osteogenic group. Alizarin Red S staining showed a significantly higher degree of bone mineralization from D7, D14 to D21 in the osteogenic group. These results indicated that pBMSCs can attach, proliferate well on CPC scaffold, and be successfully induced to differentiate into osteogenic cells. Our findings may be helpful for bone tissue engineering and the studies of bone regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone defects are commonly a secondary cause for osteoporosis, tumor, injury, or congenital malformation and can be treated with metal implants [1] and bone grafts [2]. About two million bone graft procedures are performed annually worldwide to repair bone defects in orthopedics and dentistry [3]. Although autograft and allograft bone are still largely utilized for bone graft procedures due to their natural characteristics, both the limited availability and risk of donor site morbidity still restrict their clinical applications [4]. Hence, development of an alternative source of bone grafts is still urgently required.
Hydroxyapatite (HA) and other calcium phosphate bioceramics are the key biomaterials used for bone repair and regeneration surgery due to their compositional resemblance to bone mineral [5, 6]. With a good osteoconductivity and bone-bonding ability, calcium phosphate materials have been successfully used in cranio-maxillofacial, dental, and orthopedic reconstruction during or after surgeries [7]. However, the clinical application of prefabricated bioceramics usually requires the reshaping of the graft or the surgical site or both, leading to increases in bone loss, trauma, and surgical times [8]. This limitation has been addressed by calcium phosphate cement [CPC), a new generation of bone repair material, which can self-harden in situ to form HA as an implant in the bone cavity [9]. In addition, CPC has been shown to possess three essential properties for biomaterials used in bone repair: good biocompatibility, good osteoconductivity, and a moderate bioresorbability [10].
CPC scaffolds have demonstrated a promising ability to enable cell attachment and proliferation of various stem cells. Human bone marrow mesenchymal stem cells (hBMSCs) seeded on various CPC scaffolds were successfully induced to undergo osteogenic differentiation [11, 12], and human umbilical cord mesenchymal stem cells (hUCMSCs) have provided similar results with CPC scaffolds [13]. In addition to hBMSCs and hUCMSCs, human embryonic stem cell-derived MSCs (hESC-MSCs) were also successfully differentiated into the osteogenic lineage after they were seeded onto CPC scaffolds [14]. Human-induced pluripotent stem cells derived MSCs (hiPSC-MSCs) with bone morphogenic protein 2 (BMP2) gene modification have also shown promising results for bone tissue engineering on CPC scaffolds. Furthermore, Xia et al., showed that dental pulp stem cells (DPSCs) and deciduous teeth stem cells (DTSCs) seeded onto CPC scaffolds were able to generate mineralized tissues [15]. These aforementioned studies demonstrate that CPCs are an ideal material for bone tissue engineering.
Furthermore, CPC has already been approved for repairing craniofacial defects by the Food and Drug Administration in 1996, thus becoming the first CPC for clinical application [16]. Nevertheless, clinical application of CPC is limited to the reconstruction of nonstress-bearing bone due to its brittle and weak native mechanical strength [16]. To improve its strength, we have previously developed a CPC composite with chitosan and polyglactin fibers: it was injectable, fast-setting in situ, and resistant to washout. The results demonstrated that the load-bearing properties of CPC composites have been significantly improved [17]. In addition, hUCMSCs showed excellent viability and osteogenic differentiation potential on CPC and CPC–chitosan–fiber scaffolds [17, 18].
An appropriate animal model is crucial for the research on bone regeneration [19]. Because of the many similarities in bone composition [20], microstructure [21], and remodeling [22] with human, the minipig has been regarded as a recommended large animal model for preclinical orthopedic implant studies. The critical load-bearing bone defect created on the minipig’s long bone has been widely used for bone regeneration research [23, 24]. Although various types of MSCs have successfully produced bone on a CPC scaffold and shown the scaffold’s enhanced osteoinduction, the feasibility of minipig’s bone marrow mesenchymal stem cells (pBMSCs) as seed cells on a CPC scaffold for bone engineering has not been investigated. As the implant biomaterial was usually used for the delivery of cells to improve bone healing and osseointegration [25, 26], the scaffold material needs to show sufficient biocompatibility and ability to support cell attachment and differentiation. Therefore, the purpose of this study was to construct tissue engineering bone using minipig pBMSCs and CPC scaffold and to induce the pBMSCs to differentiate into the osteogenic lineage on the CPC scaffold. Our results showed that seeded pBMSCs attached, proliferated well, and could be successfully induced to osteogenic cells on the CPC scaffold.
Methods and Materials
CPC Scaffold Preparation
The CPC is comprised tetracalcium phosphate [TTCP: Ca4 (PO4)2O] and dicalcium phosphate anhydrous (DCPA: CaHPO4). TTCP was synthesized from equimolar amounts of DCPA and calcium carbonate (J. T. Baker, USA). The reactant was ground in a ball mill (Retsch PM4, USA) and sieved to obtain TTCP particles with a size range of 1–80 μm, with a median of 17 μm. DCPA was ground for 24 h to obtain particle sizes ranging from 0.4 to 3 μm, with a median of 1 μm. The TTCP and DCPA powders were mixed in a blender at a molar ratio of 1:1 to form the CPC powder. CPC powder was mixed with deionized water at a powder-to-liquid mass ratio of 4–1. The paste was placed into a circular mold of 12 mm diameter and 2 mm thickness. After setting at 100 % relative humidity for 4 h at 37 °C., the CPC disks were demolded and immersed in water at 37 °C for 20 h.
Isolation of pBMSCs
This study was approved by Guangdong Animal Research Management Center (No. 00049665). Five mL of bone marrow was aspirated from the posterior iliac crest of a Tibetan minipig (female, 10 months old) using a sterile bone marrow aspiration needle. The mononucleated cells were isolated by density gradient centrifugation method [25] with the Ficoll Paque Plus (BaiLu Biology Company, Guangzhou, China), and the cell pellet was resuspended in complete cell growth medium (Dulbecco’s modified Eagle medium (DMEM) (Invitrogen, USA) supplemented with 10 % fetal bovine serum (FBS, Invitrogen), 1 % nonessential amino acids (NEAA, Invitrogen), and 1 % penicillin/streptomycin (P/S, Hyclone, Logan, USA). The mononucleated cells were seeded into 6-wells plate with a density of 2 × 105/cm2 and cultured at 37 °C in a humidified incubator supplemented with 5 % CO2. After 24 h, nonadhesive cells were discarded; the culture medium was changed twice a week. At 80–90 % confluence, cells were harvested with trypsin/EDTA (Invitrogen) and re-plated at a splitting ratio of 1:3.
PBMSCs Seeding on CPC Scaffold
The CPC disks were sterilized by ethylene oxide and incubated overnight in culture medium for 24 h prior to seeding cells to improve cell attachment. A flask of confluent passage 2 pBMSCs was harvested. For the osteogenic group, the cell pellet was resuspended in the osteogenic media containing 50 μM ascorbate2-phosphate, 10 mM glycerol phosphate, 100 nM dexamethasone, and 10 nM Vitamin D3 (all purchased from Sigma, USA). A total of 3 × 105 pBMSCs in 2 mL osteogenic media was seeded onto a CPC disk into each of the 24 wells, as previously described [18]. For control group, pBMSCs were seeded on the CPC in the normal culture medium. The pBMSCs/CPC constructs were placed in the incubator, and the media was changed twice a week.
Cell Viability
Cell viability was assessed by the live/dead Viability/Cytotoxicity Kit (Invitrogen). After culture for 1, 4, 7 and 14 days, the CPC disks were washed twice with phosphate-buffered saline. Each sample was incubated for 10 min at 37 °C with 2 mL culture media containing 2 mM calcein-AM and 2 mM ethidium homodimer-1. The stained cells were visualized by epifluorescence microscopy (Eclipse TE300; Nikon, Japan). Three randomly chosen fields of view were photographed for each disk. Five disks yielded 15 photos for each sample at each time point. The percentage of viable cells was measured as P viable = N viable/(N viable + N DEAD). The viable cell density was calculated from the following equation: D = N viable/area.
Scanning Electron Microscopy
The morphology of pBMSCs growth on the CPC scaffold was examined on day 1 and day 4 by scanning electron microscopy (SEM, XL-30, Philips, USA). Each sample was fixed for 24 h in 0.4 % glutaraldehyde and dehydrated in a series of graded ethanol solutions before coating with gold/palladium for 3 min and subsequent SEM observation.
Alkaline Phosphatase Assay
Alkaline phosphatase (ALP) activity of cells was measured by Alkaline Phosphatase Assay Kit (Beyotime, China) on Day 1 (D1), D4, D7, D14, and D21. The pBMSCs/CPC constructs were washed twice by PBS and transferred to 1.5 ml centrifuge tube. The 0.5 mL cell lysis buffer containing 0.2 % Triton X-100 (Sigma) with 10 mM Tris (pH 7.0) and 1 mM EDTA (Sigma) was added onto the CPC disks and pipetted for 30 times. The mixture was transferred to −80 °C freezer for 30 min and thawed at room temperature for 1 h. The freeze-thawing procedure was performed twice to lyse cells. The cell lysis buffer of each sample was transferred to 96-well plate, and the absorbance of 405 nm was measured by NanoDrop 2000c Spectrophotometer (Thermo Scientific, USA). Standard samples were made and assayed concurrently with test samples; a standard curve was constructed. The amount of p-nitrophenyl phosphate (pNpp) in each sample was calculated. The amount of protein in each sample was measured by a BCA Protein Assay Kit (Beyotime). The ALP activity was normalized to the amount of total protein and calculated by the following equation: [pNpp (μM/min)]/[Protein (mg)].
Real-Time PCR
The total RNA from the CPC/BMSCs constructs was extracted using Trizol (Invitrogen) on D1, D4, D7, and D14. cDNA was reverse transcribed by a Reverse Transcription Kit (RR036A,Takara, Japan). All target genes were searched on the NCBI gene bank, and the primers were obtained commercially (Takara). The target genes included ALP (Hs00758162_m1), bone gamma-carboxyglutamateprotein [osteocalcin (OC), Hs00609452_g1], collagen, type I, alpha 1 (Coll I, Hs00164004), runt-related transcription factor 2 (Runx2, NC_010449.4), and glyceraldehyde-3-phosphate dehydrogenase (GAPDH, Hs99999905). The SYBR® Premix Ex Taq™ II Kit (Takara) was used to measure the transcription level of the target genes. Quantitative real-time RT-PCR was performed in an Applied Biosystems® 7500 Real-Time PCR Systems. The mean fold changes from three separate experiments were analyzed using the 2−ΔΔCT method.
Mineral Synthesis
Bone mineralization was assessed by Alizarin RedS (ARS) staining method. Each sample on D1, D4, D7, and D14 was washed twice with PBS, fixed with 10 % formaldehyde, and stained with ARS (Millipore, USA). To quantify the ARS staining, an osteogenesis assay (Millipore) was used to extract the stained minerals and measure the concentration of Alizarin Red S at OD405 [27]. CPC specimens with the same compositions but without pBMSCs were used as a control to calculate the net Alizarin red amount of the CPC with pBMSCs.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Version 20 (SPSS Statistics V20, IBM Corporation, Somers, New York). Statistical significance was assessed using one- or two-way analyses of variance [ANOVA) and Tukey’s multiple comparison tests. A confidence level of 95 % (P < 0.05) was considered statistically significant. All data are presented as mean ± standard deviation (SD).
Results
pBMSCs Attached and Proliferated on CPC Scaffold
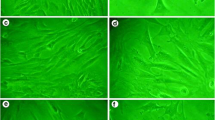
To address the feasibility of utilizing pBMSCs and CPC scaffold to construct tissue engineering bone, passage 2 pBMSCs were seeded onto the prepared CPC scaffold. Meanwhile, the seeded pBMSCs were induced to differentiate into osteogenic cells by osteogenic medium (osteogenic group), and the cells in the control group were cultured with normal DMEM medium. The viability of seeded cells was determined by LIVE/DEAD kit. Figure 1a shows that the pBMSCs in osteogenic group grew on the CPC disks at different time points after seeding. A trend was observed that the percentage of viable cells increased over time. The Pviable in osteogenic and control group on day 14 was 95 and 97 %, respectively (Fig. 1b). From D1 to D14, the density of seeded cells on CPC scaffold increased by 4- to 4.5-fold in both groups (Fig. 1c). A representative SEM micrograph of pBMSCs on CPC scaffold is shown in Fig. 2. After 4 days, the BMSCs in the osteogenic group had firmly attached and spread well on the scaffold, and the cytoplasmic extensions could be clearly observed. These results indicated that pBMSCs attached and proliferated well on the CPC disk.
pBMSCs attached and proliferated on CPC scaffolds. a Live/dead staining of pBMSCs cultured on CPC scaffold with osteogenic medium for 1 and 7 days. The viable pBMSCs were stained green and appeared to have adhered and attained a normal polygonal morphology. Dead cells were stained red (right lower panel). b The percentage of viable pBMSCs (P viable) (b) and viable cell density (c) are shown. In each plot, means not sharing a common superscript differ significantly according to Tukey’s multiple comparison test (P < 0.05). The value was presented as mean ± SD, n = 5 (Color figure online)
pBMSC-Induced Osteogenic Cells on CPC Scaffold Possessed Alkaline Phosphatase Activity
To determine if seeded pBMSCs could be induced to osteogenic cells on the CPC, we assessed the ALP activity among the two groups. The ALP activity of pBMSCs in the control group was maintained at a basal level during the whole period, while the ALP activity of the osteogenic group increased rapidly by D7 and reached the peak level on D14 of 1.550 ± 0.048 (μM pNPP/min)/(mgProtein). The ALP activity of the osteogenic group slightly decreased on D21. On D7, D14, and D21, there were significant differences in ALP activity between the two groups (P < 0.01, Fig. 3). The ALP mRNA expression levels between the two groups were determined by RT-PCR. Consistently, the ALP mRNA expression levels of the control groups stayed at a low level throughout the whole period, while those in the osteogenic group significantly increased from D4 to D14. The ALP mRNA peak in the osteogenic group was observed on D4: ALP mRNA levels were 11 fold higher than that on D1 (Fig. 4a).
Alkaline phosphatase activity elevated in pBMSC-induced osteogenic cells on CPC scaffold. ALP activities of each group were determined as described in the “Materials and methods.” Means not sharing a common superscript differ significantly according to Tukey’s multiple comparison test (P < 0.05). The value was presented as mean ± SD, n = 5
mRNA expressions of osteogenic markers elevated in pBMSCs-induced osteogenic cells on CPC scaffold. The mRNA expressions of osteogenic makers were determined by RT-PCR. a Alkaline phosphatase (ALP), b Osteocalcin (OC), c Collagen type I (Coll I), and d Runx2 gene expression. The ALP peaked on day 4 (D4). The OC and Coll I peaked on D7. The expressions of ALP and the other three osteogenic marker genes were significantly greater in the osteogenic group than those in the control group. Means not sharing a common superscript differ significantly according to Tukey’s multiple comparison test (P < 0.05). The value was presented as mean ± SD, n = 5
mRNA Expression of Osteogenic Markers Elevated in pBMSC-Differentiated Osteogenic Cells on CPC Scaffold
Next, we further assessed the expressions of other osteogenic markers to confirm osteogenic differentiation. On D4, D7, and D14, the osteogenic group had significantly greater mRNA levels of OC, Coll I, and Runx2 than the control group (Fig. 4b, c). These data confirmed that pBMSCs cultured on CPC can be induced to osteogenic cells with osteogenic media.
Mineralization of the Tissue Engineering Bone
Bone mineralization was evaluated with Alizarin Red S staining. Because the CPC disk consisted of minerals, the blank disks (without pBMSCs) also stained. The staining color in the osteogenic groups became darker and thicker (Fig. 5a) than control groups. At D21, a dark red staining of minerals synthesized by the cells that cover the CPC disk became evident (Fig. 5a). In contrast, no obvious staining mineral on the CPC was observed at each time point in the control group. The quantitative results of the Alizarin Red S staining data are shown in Fig. 5b. The mineralization in osteogenic group was significantly higher than that of control group on D7 and D14. Taken together, these data further indicated that seeded pBMSCs can be successfully induced to osteogenic cells on the CPC scaffold.
Mineralization of the tissue engineering bone. a Alizarin Red S staining of cell mineralization on CPC constructs. The CPC disks without cells also stained red because CPC consisted of apatite minerals. b The quantitative results of mineralization were plotted. Means not sharing a common superscript differ significantly according to Tukey’s multiple comparison test (P < 0.05). The value was presented as mean ± SD, n = 5 (Color figure online)
Discussion
In this study, we utilized pBMSCs as seed cells and CPC as scaffolds to engineer bone tissue. After seeding on the CPC, the microscopic images showed that the pBMSCs attached to the CPC disk and proliferated well. Osteogenic medium successfully induced osteogenic differentiation of the seeded pBMSCs, as confirmed by elevated ALP activity, mRNA expression of osteogenic markers, and bone mineralization. Thus, we showed that pBMSCs attached and proliferated well on the CPC scaffold and successfully differentiated into osteogenic cells on the CPC scaffolds.
In bone engineering, one of the main functions of scaffold is to support cells for osteogenesis [28, 29]. An ideal biomaterial as a bone substitute is needed to provide a natural substrate for cell attachment, proliferation, and differentiation. CPCs are excellent biomaterials for bone engineering since previous studies have shown their promising ability for cell attachment and proliferation of various stem cells, including hBMSCs, hUCMSCs, hESC-MSCs, hiPSC-MSCs, DPSCs, DTSCs, and osteoblastic cells [30]. In the field of orthopedic and dental research, minipig models have been extensively used in preclinical research due to their many similarities in bone characteristics with humans. However, to our knowledge, pBMSCs cultured on CPC scaffolds have not been explored. In the present study, for the first time, we investigated the pBMSCs’ interactions with CPC scaffold for cell proliferation and differentiation with two different culture media.
The SEM images showed that the pBMSCs firmly attached and spread well on the scaffold on D4. The spreading and development of cytoplasmic extensions suggested good viability and attachment of pBMSCs on CPC. The percentage of the viable cells in both groups gradually increased over the cultured time and exceeded 95 % on D14. The cell density of viable cells also increased rapidly in both groups. Taken together, these results demonstrated that pBMSCs exhibited excellent viability as cultured on CPC scaffold, indicating that the CPC scaffold provided a suitable environment for attachment and proliferation of pBMSCs.
ALP, an enzyme, is a well-defined marker for osteogenic differentiation and can be expressed by stem cells during osteogenesis [31, 32]. In the present work, ALP activity of pBMSCs in the osteogenic group increased over the culture time and was seven times higher on D14 than on D1, indicating that pBMSCs seeded on the CPC were successfully differentiating into the osteogenic lineage. This observation was similar with previous studies [33–35]. A number of studies have described the elevation of ALP activity and then a decrease during the osteogenic differentiation process of BMSCs of multiple species [33–35].
ALP, OC, Col I, and Runx2 play key roles in osteogenic differentiation and are considered marker genes for osteogenic differentiation [32, 36]. The present study revealed an increased mRNA expression of these four osteogenic markers in the osteogenic group. The ALP expression peaked on D4 (4 times higher on D4 than on D1) and had decreased by D8. In agreement, Kim et al. [32] showed that the expression of ALP measured via RT-PCR was minimal on D1, peaked on D4, and then decreased on D8 [32]. Our study showed that the mRNA expression of OC and Col I peaked on D7, and Runx2 peaked on D14, which were consistent with Zhou et al. [37].
The osteogenic differentiation was further confirmed by evidence of mineralization of pBMSCs cultured on the CPC scaffold. A significantly higher degree of bone mineralization was observed in the osteogenic group. The mineralization increased as the cells proliferated and differentiated in the osteogenic medium from D7 and D14 to D21. However, there was no mineralization in the control group. Taken together, these results suggested that the seeded pBMSCs had successfully differentiated into osteogenic cells.
In conclusion, our in vitro study showed promising data that pBMSCs can grow and proliferate well on CPC scaffold. In addition, the seeded pBMSCs can be successfully induced to differentiate into the osteogenic lineage. Future work should be conducted to confirm that the developed pBMSCs/CPC construct can be effective in an in vivo preclinical study. Our findings may be helpful for the studies of bone regeneration in a wide range of dental, craniofacial, and orthopedic field.
References
Agarwal, R., & García, A. J. (2015). Biomaterial strategies for engineering implants for enhanced osseointegration and bone repair. Advanced Drug Delivery Reviews, 94, 53–62.
Gamie, Z., Tran, G. T., Vyzas, G., Korres, N., Heliotis, M., Mantalaris, A., et al. (2012). Stem cells combined with bone graft substitutes in skeletal tissue engineering. Expert Opinion on Biological Therapy, 12, 713–729.
Marino, J. T., & Ziran, B. H. (2010). Use of Solid and Cancellous Autologous Bone Graft for Fractures and Nonunions. Orthopedic Clinics of North America, 41, 15–26.
Low, K. L., Tan, S. H., Zein, S. H., Roether, J. A., Mouriño, V., & Boccaccini, A. R. (2010). Calcium phosphate-based composites as injectable bone substitute materials. Journal of Biomedical Materials Research. Part B, Applied Biomaterials, 94, 273–286.
Zhao, J., Zhang, Z., Wang, S., Sun, X., Zhang, X., Chen, J., et al. (2009). Apatite-coated silk fibroin scaffolds to healing mandibular border defects in canines. Bone, 45, 517–527.
Park, J. H., Lee, E. J., Knowles, J. C., & Kim, H. W. (2014). Preparation of in situ hardening composite microcarriers: calcium phosphate cement combined with alginate for bone regeneration. Journal of Biomaterials Applications, 28, 1079–1084.
Barrère, F., van Blitterswijk, C. A., & de Groot, K. (2006). Bone regeneration: molecular and cellular interactions with calcium phosphate ceramics. International Journal of Nanomedicine, 1, 317–332.
Laurencin, C. T., Ambrosio, A. M., Borden, M. D., & Cooper, J. A. (1999). Tissue engineering: orthopedic applications. Annual Review of Biomedical Engineering, 1, 19–46.
Yokoyama, A., Yamamoto, S., Kawasaki, T., Kohgo, T., & Nakasu, M. (2002). Development of calcium phosphate cement using chitosan and citric acid for bone substitute materials. Biomaterials, 23, 1091–1101.
Kinoshita, Y., & Maeda, H. (2013). Recent developments of functional scaffolds for craniomaxillofacial bone tissue engineering applications. Scientific World Journal, 2013, 863157.
He, F., Li, J., & Ye, J. (2013). Improvement of cell response of the poly(lactic-co-glycolic acid)/calcium phosphate cement composite scaffold with unidirectional pore structure by the surface immobilization of collagen via plasma treatment. Colloids Surfactants B Biointerfaces, 103, 209–216.
Vater, C., Lode, A., Bernhardt, A., Reinstorf, A., Heinemann, C., & Gelinsky, M. (2010). Influence of different modifications of a calcium phosphate bone cement on adhesion, proliferation, and osteogenic differentiation of human bone marrow stromal cells. Journal of Biomedical Materials Research Part A, 92, 1452–1460.
Chen, W., Liu, J., Manuchehrabadi, N., Weir, M. D., Zhu, Z., & Xu, H. H. K. (2013). Umbilical cord and bone marrow mesenchymal stem cell seeding on macroporous calcium phosphate for bone regeneration in rat cranial defects. Biomaterials, 34, 9917–9925.
Chen, W., Zhou, H., Weir, M. D., Tang, M., Bao, C., & Xu, H. H. (2013). Human embryonic stem cell-derived mesenchymal stem cell seeding on calcium phosphate cement-chitosan-RGD scaffold for bone repair. Tissue Engineering Part A, 19, 915–927.
Xia, L., Zhang, M., Chang, Q., Wang, L., Zeng, D., Zhang, X., et al. (2013). Enhanced dentin-like mineralized tissue formation by AdShh-transfected human dental pulp cells and porous calcium phosphate cement. PLoS One, 8, e62645.
Friedman, C. D., Costantino, P. D., Takagi, S., & Chow, L. C. (1998). Bonesource(TM) hydroxyapatite cement: A novel biomaterial for craniofacial skeletal tissue engineering and reconstruction. Journal of Biomedical Materials Research, 43, 428–432.
Zhao, L., Burguera, E. F., Xu, H. H., Amin, N., Ryou, H., & Arola, D. D. (2010). Fatigue and human umbilical cord stem cell seeding characteristics of calcium phosphate-chitosan-biodegradable fiber scaffolds. Biomaterials, 31, 840–847.
Zhao, L., Weir, M. D., & Xu, H. H. (2010). Human umbilical cord stem cell encapsulation in calcium phosphate scaffolds for bone engineering. Biomaterials, 31, 3848–3857.
Pearce, A. I., Richards, R. G., Milz, S., Schneider, E., & Pearce, S. G. (2007). Animal models for implant biomaterial research in bone: a review. Eur. Cell. Mater., 13, 1–10.
Aerssens, J., Boonen, S., Lowet, G., & Dequeker, J. (1998). Interspecies differences in bone composition, density, and quality: Potential implications for in vivo bone research. Endocrinology, 139, 663–670.
Martiniaková, M., Grosskopf, B., Omelka, R., Vondráková, M., & Bauerová, M. (2006). Differences among species in compact bone tissue microstructure of mammalian skeleton: Use of a discriminant function analysis for species identification. Journal of Forensic Sciences, 51, 1235–1239.
Martínez-González, J. M., Cano-Sánchez, J., Campo-Trapero, J., Gonzalo-Lafuente, J. C., Díaz-Regañón, J., & Vázquez-Piñeiro, M. T. (2005). Evaluation of minipigs as an animal model for alveolar distraction. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics, 99, 11–16.
Horner, E. A., Kirkham, J., Wood, D., Curran, S., Smith, M., Thomson, B., et al. (2010). Long bone defect models for tissue engineering applications: criteria for choice. Tissue Engineering Part B, 16, 263–271.
Hakimi, M., Jungbluth, P., Sager, M., Betsch, M., Herten, J., Becker, M., et al. (2010). Combined use of platelet-rich plasma and autologous bone grafts in the treatment of long bone defects in mini-pigs. Injury, 41, 717–723.
Pieri, F., Lucarelli, E., Corinaldesi, G., Fini, M., Aldini, N. N., Giardino, R., et al. (2009). Effect of mesenchymal stem cells and platelet-rich plasma on the healing of standardized bone defects in the alveolar ridge: a comparative histomorphometric study in minipigs. Journal of Oral and Maxillofacial Surgery, 67, 265–272.
Okabe, K., Yamada, Y., Ito, K., Kohgo, T., Yoshimi, R., & Ueda, M. (2009). Injectable soft-tissue augmentation by tissue engineering and regenerative medicine with human mesenchymal stromal cells, platelet-rich plasma and hyaluronic acid scaffolds. Cytotherapy, 11, 307–316.
Wang, Y. H., Liu, Y., Maye, P., & Rowe, D. W. (2006). Examination of Mineralized Nodule Formation in Living Osteoblastic Cultures Using Fluorescent Dyes. Biotechnology Progress, 22, 1697–1701.
Silva, G. A., Coutinho, O. P., Ducheyne, P., & Reis, R. L. (2007). Materials in particulate form for tissue engineering. 2. Applications in bone. Journal of Tissue Engineering Regenerative Medicine, 1, 97–109.
Kretlow, J. D., Young, S., Klouda, L., Wong, M., & Mikos, A. G. (2009). Injectable biomaterials for regenerating complex craniofacial tissues. Advanced Materials, 21, 3368–3393.
Hesaraki, S., & Nezafati, N. (2014). In vitro biocompatibility of chitosan/hyaluronic acid-containing calcium phosphate bone cements. Bioprocess and Biosystems Engineering, 37, 1507–1516.
Wang, J., de Boer, J., & de Groot, K. (2008). Proliferation and Differentiation of MC3T3-E1 Cells on Calcium Phosphate/Chitosan Coatings. Journal of Dental Research, 87, 650–654.
Kim, K., Dean, D., Mikos, A. G., & Fisher, J. P. (2009). Effect of initial cell seeding density on early osteogenic signal expression of rat bone marrow stromal cells cultured on cross-linked poly(propylene fumarate) disks. Biomacromolecules, 10, 1810–1817.
Moreau, J. L., & Xu, H. H. K. (2009). Mesenchymal stem cell proliferation and differentiation on an injectable calcium phosphate-chitosan composite scaffold. Biomaterials, 30, 2675–2682.
Hofmann, S., Hagenmüller, H., Koch, A. M., Müller, R., Vunjak-Novakovic, G., Kaplan, D. L., et al. (2007). Control of in vitro tissue-engineered bone-like structures using human mesenchymal stem cells and porous silk scaffolds. Biomaterials, 28, 1152–1162.
Leach, J. K., Kaigler, D., Wang, Z., Krebsbach, P. H., & Mooney, D. J. (2006). Coating of VEGF-releasing scaffolds with bioactive glass for angiogenesis and bone regeneration. Biomaterials, 27, 3249–3255.
Tang, M., Weir, M. D., & Xu, H. H. (2012). Mannitol-containing macroporous calcium phosphate cement encapsulating human umbilical cord stem cells. J. Tissue. Eng. Regen. Med., 6, 214–224.
Zhou, H., & Xu, H. H. K. (2011). The fast release of stem cells from alginate-fibrin microbeads in injectable scaffolds for bone tissue engineering. Biomaterials, 32, 7503–7513.
Acknowledgments
We gratefully acknowledge Prof. Zhengliang Zhao at the Southern Medical University for SEM assistance and useful discussions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by National Natural Science Foundation of China 31328008 (LZ), Natural Science Foundation of Guangdong s20130010014253 (LZ) and 2014A03031327 (LZ), Guangdong Provincial Science and Technology Project 2012B010200024 (LZ), and Guangzhou Science and Technology Project 2012027 (LZ).
Additional information
G. Qiu, P. Wang and G. Li have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Qiu, G., Wang, P., Li, G. et al. Minipig-BMSCs Combined with a Self-Setting Calcium Phosphate Paste for Bone Tissue Engineering. Mol Biotechnol 58, 748–756 (2016). https://doi.org/10.1007/s12033-016-9974-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12033-016-9974-6