Abstract
Psychosocial stress promotes cancer pathogenesis involving angiogenesis through alterations in neuroendocrine-immune functions that may involve adrenoceptor (AR)-dependent signaling mechanisms in the brain, lymphoid organs, and cancerous cells. Various concentrations of α1- and α2- AR-specific agonists and antagonists were incubated in vitro with estrogen receptor-positive (ER +) MCF-7, and ER (-) MDA MB-231 cells to examine the secretions of VEGF-A, VEGF-C, and nitric oxide (NO), and expression of signaling molecules- p-ERK, p-CREB, and p-Akt on the proliferation of breast cancer cell lines. Cellular proliferation, VEGF-A and NO secretion, expression of p-ERK, p-CREB, and p-Akt were enhanced in MCF-7 cells treated with α1-AR agonist while VEGF-C secretion alone was enhanced in MDA MB-231 cells. Treatment of MCF-7 and MDA MB-231 cells with α2- AR agonist similarly enhanced proliferation and decreased NO production and p-CREB expression while VEGF-C secretion was decreased in MCF-7 cells and p-Akt expression was decreased in MDA MB-231 cells. α1-AR inhibition reversed cellular proliferation and VEGF-A secretion by MCF-7 cells while α2-AR inhibition reversed the proliferation of MCF-7 and MDA MB-231 cells and VEGF-C secretion by MCF-7 cells. Taken together, breast cancer pathogenesis may be influenced by distinct α-AR-mediated signaling mechanisms on angiogenesis and lymphangiogenesis that are dependent on estrogen receptor status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine-immune network through the regulated release of neurotransmitters and neuropeptides, endocrine mediators, and immune effectors is crucial to the maintenance of cellular and systemic homeostasis [1, 2]. During young age, the neuroendocrine-immune network is functionally robust and the redundancy of several compensatory mechanisms confers the ability to overcome stressful stimuli and thus, maintains functional integrity. However, aging increases allostatic load with repeated exposure to stress and pathogens coupled with the general decline in the nervous, endocrine, and immune functions and loss of compensatory mechanisms and collectively contributes to the development of age-related diseases and cancer [1,2,3]. In addition to impaired functions of hypothalamic dopaminergic neurons, age-associated loss of cell-mediated immune functions and a decline in sympathetic neuronal activity in the secondary lymphoid organs can result in altered production of Th1 and Th2 cytokines and NO, and dysregulation of pro/anti-angiogenic factors that may contribute to mammary carcinogenesis [1, 4, 5].
Neural, endocrine, and immune effector molecules bind to specific receptors on tumor cells and mediate a multitude of cellular responses with implications at the local and systemic levels. Evidence of adrenergic stimulation and α2-ARs of the mammary gland were first reported in studies involved normal bovine mammary gland due to their effects on milk production [6,7,8]. α-AR actions are characterized in several breast tumor and non-tumor cell lines, which were associated with increased cell proliferation in vitro and with increased tumor growth in vivo [9,10,11]. Studies have reported α2-AR expression at the RNA and protein levels in estrogen-sensitive (IBH-6, IBH-7, MCF-7), estrogen-insensitive (MDA-MB-231, HS-578 T), HBL-100 and MCF-10A human breast cancer cell lines [10]. Adrenergic signaling influence breast cancer progression through increase in the tumor cell survival, and altering the tumor microenvironment in angiogenesis and inflammatory responses in in vitro breast cancer cell lines (MDA-MB-231, HS-578 T) [12]. In female, the neuroendocrine-immune milieu is influenced by rhythmic alterations in the levels of gonadal hormones especially estrogen and progesterone. The immunomodulatory role of estrogen has been widely shown in vivo although the direct effects of the hormone on cell-mediated immune functions in stimulated lymphocytes [13]. The distribution of α- and β-adrenergic receptors (AR) on bovine mammary cells, human breast cancers, and breast cancer cell lines indicate that norepinephrine (NE) released from several stress-associated signals can bind to specific adrenergic receptors on tumor cells with different affinities and mediate cellular responses [8, 10, 11, 14, 15]. One of the key pro-angiogenic molecules, vascular endothelial growth factor (VEGF), secreted by tumor cells in an autocrine manner is induced by norepinephrine to influence tumor growth [11, 16]. Similarly, estrogen released from mammary tumor cells and ovaries can stimulate cancer cells in an autocrine or paracrine manner and affect their growth and invasiveness depending on the presence or absence of ER [5, 17,18,19]. The expression of adrenergic receptors in the mammary gland may influence the response of the gland to sympathetic stimulation. Stress and sympathetic nervous system activation have been suggested to influence cancer progression, including breast cancer [20]. Chronic stress may contribute to an environment conducive to tumor growth and metastasis, although the mechanisms involved are complex [21]. Incubation of splenocytes of young male rats with estrogen altered the immunomodulatory effects of α1- and α2- adrenergic agonists in a receptor subtype-dependent manner suggesting that the receptor status determines cellular functions [22]. Although activation of α2-AR on the human breast cancer cells by agonists and catechol estrogens has been demonstrated to enhance proliferation and α2-blockade using yohimbine and rauwolscine prevented tumor growth in mice, the role of estrogen in modulating α-AR responses and their interactive effects on carcinogenesis involving angiogenesis and lymphangiogenesis have not been fully elucidated [11, 14]. The onset of age-associated loss of sympathetic noradrenergic fibers in rodents is much earlier in females compared with males implicating the degenerative effects of precluding exposure to estrogen throughout reproductive life and in the perimenopausal period [19, 23]. Estrogen responsiveness is a crucial discriminating factor in mammary tumorigenesis; hence, it is vital to understand the effects of adrenergic stimulation of estrogen receptor positive and negative tumor cells on angiogenic and intracellular signaling factors. Activation of the alpha-adrenergic receptors may stimulate downstream signaling molecules involved in various pathways such as the mitogen-activated protein kinase (MAPK) pathway, cyclic AMP signaling pathway. Signaling molecules such as p-ERK, p-CREB and p-Akt are part of a broader signaling cascade in regulating various downstream effectors involved in cell proliferation, survival, differentiation, metabolism, angiogenesis, and other cellular processes. Therefore, the present study was conducted to investigate the synergistic effects of ER- and AR-signaling in vitro to examine the role of adrenergic effectors such as α1- and α2- adrenergic agonists and antagonists on proliferation, VEGF A and C secretion, and nitric oxide production by ER ( +) and ER (−) breast cancer cell lines. In addition, the levels of molecular signaling factors such as p-ERK, p-CREB, and p-Akt were measured to understand the molecular actions of α1- and α2-AR agonists in ER ( +) and ER (−) breast cancer cell lines.
Materials and methods
In vitro breast cancer cell culture
Both ER ( +) MCF-7 and ER (−) MDA MB 231 human breast cancer cell lines were obtained from the repository of the National Centre for Cell Science (NCCS), Pune, India. MCF-7 cells were maintained in DMEM medium, supplemented with 2 mM L-Glutamine, 100 units/ml Penicillin, 100 µg/ml Streptomycin, 1.5 g/l sodium bicarbonate, and 10% Fetal Bovine Serum and incubated at 37 °C in a humidified atmosphere with 5% CO2. MDA-MB-231 cell line was maintained in L15 medium, supplemented with 2 mM L-Glutamine,100 units /ml Penicillin, 100 μg/ml Streptomycin, 1.5 g/l sodium bicarbonate, and 10% Fetal Bovine Serum and incubated at 37 °C in a humidified atmosphere without CO2. Cells were cultured until they reached 70% confluence and such sub-confluent flasks were trypsinized and seeded in 96 well plates (5000 cells/ well) and incubated for 24 h until the monolayer was formed.
Treatment
Both MCF-7 and MDA-MB-231 cells were incubated with various concentrations of α1-AR agonist, phenylephrine (10–9 M and 10–6 M), or α2-AR agonist, clonidine (10–9 M and 10–6 M) with and without an α1-AR-specific antagonist, prazosin (10−5 M) or specific α2-AR antagonist, idazoxan (10–5 M) for 2, 4, and 6 days. The concentration of the agonist and antagonist were based on a preliminary study on splenic lymphocytes to mimic the physiological and pharmacological conditions, and also to understand the dose-dependent response, and time-dependent immediate and prolonged effects of the adrenergic agents [13, 22]. Plasma levels of epinephrine and norepinephrine ranges from 0–0.83 nmol/L and 0.41–10 nmol/L, respectively [24].Significant elevations were observed in acute anxiety, pheochromocytoma, ganglioblastoma, neuroblastoma, and severe stress [24].
Assessment of cell proliferation
MTT assay was performed to measure the proliferation of cancer cells. Briefly, the cells were treated with MTT reagent, incubated for 3 h, and read at 620 nm after completely solubilizing the formazan product formed in isopropanol containing 37% HCl. The proliferation of MCF-7 and MDA MB-231 cells were represented as column graphs in results section and as line graphs in the supplementary figures section for better visualization.
VEGF-A and VEGF-C secretion
Supernatants were collected and stored at −80 °C for VEGF-A and VEGF-C secretion using ELISA kits (R&D Systems, Minneapolis, Minn., USA).
Intracellular signaling pathway markers
Cell pellets were lysed in RIPA buffer containing phenylmethylsulfonyl fluoride (PMSF) and orthovanadate. Lysed samples were analyzed for ERK1/2, p-ERK1/2, CREB, p-CREB, Akt, and p-Akt using ELISA kits (R&D Systems, Minneapolis, Minn., USA).
Statistical analysis
Differences between groups were measured using ANOVA by the SPSS software package. Parameters that attained significance (p < 0.05) with ANOVA were further analyzed by Fisher’s least significant difference test. Agonist-treated groups were compared with the respective time-matched control groups after 2, 4 and 6 days of treatment for statistical significance. The agonist + antagonist-treated groups were compared with the respective time-matched agonist-treated groups for statistical significance. All values are expressed as mean ± S.E.M.
Results
Selective enhancement of proliferation of MCF-7 cells by α1-AR agonist
The proliferation of MCF-7 cells was significantly (p < 0.05) enhanced by phenylephrine treatment in day 2 (10–9 M and 10–6 M), day 4 and 6 (10–6 M) (Fig. 1A). This increase was reversed by co-treatment with the α1-AR-specific antagonist, prazosin, on day 2 (Phe 10–9 M + Pz 10–5 M) and day 4 (Phe 10–6 M + Pz 10–5 M) alone. Treatment with prazosin (10–5 M) alone for 2, 4, and 6 days significantly (p < 0.05) decreased the proliferation of MCF-7 cells. In ER (-) MDA MB-231 breast cancer cells, phenylephrine (10–9 M) significantly (p < 0.05) enhanced the proliferation, after 4 and 6 days of treatment, and the effects were not reversed by co-treatment with the antagonist (Fig. 1B).
In vitro addition of α1- AR agonist, phenylephrine (Phe), on the proliferation of ER (+) MCF-7 and ER (−) MDA MB-231 breast cancer cell lines. Coincubation of MCF-7 breast cancer cells with α1-AR agonist, phenylephrine, enhanced proliferation of cells on days 2, 4, and 6 while co-treatment with prazosin (Pz) decreased proliferation after 2 and 4 days of incubation (1A; S1A and S1B). Proliferation of MDA MB-231 cells was also enhanced by phenylephrine after 4 and 6 days although the effects were not reversed by cotreatment with the antagonist (1B; S2A and S2B). *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
Enhancement of VEGF-A and inhibition of VEGF-C in MCF-7 cells by α1-AR agonist
There was a significant (p < 0.05) increase, in the secretion of VEGF-A by ER ( +) MCF-7 cells upon stimulation with phenylephrine after 2 days (10–6 M), 4 days (10–6 M) and 6 days (10–9 M, 10–6 M) of treatment, and the effects were reversed upon co-incubation with prazosin 10–5 M (Fig. 2A). Interestingly, treatment with prazosin (10–5 M) alone significantly (p < 0.05) decreased VEGF-A secretion by MCF-7 cells, after 2, 4, and 6 days of treatment which was similar to its effects on proliferation.
Differential VEGF-A and VEGF-C secretion by AR agonist, phenylephrine (Phe), in ER (+) MCF-7 cells. VEGF-A secretion by MCF-7 cells was increased on days 2, 4, and 6 after phenylephrine treatment (2A). VEGF-C secretion was significantly decreased (2B) upon treatment with phenylephrine for 2 days. α1-AR antagonist, prazosin (Pz), reversed the effects on VEGF-A alone. *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
Treatment with phenylephrine (10–9 M, 10–6 M) significantly (p < 0.05) decreased the secretion of VEGF-C by MCF-7 cells, after 2 days of treatment, and the effect was reversed by co-treatment with the antagonist in day 2 (Phe: 10–6 M) and day 4 (Phe: 10–9 M and 10–6 M) (Fig. 2B).
Inhibition of VEGF-A and enhancement of VEGF-C in MDA MB-231 cells by α1-AR agonist
Stimulation of α1-AR in ER(−) MDA MB-231 cells with phenylephrine did not alter secretion of VEGF-A after 2, and 4 days of treatment (Fig. 3A). However, prolonged treatment with phenylephrine for 6 days significantly (p < 0.05) decreased the secretion of VEGF-A by MDA MB-231 cells; and the effects were reversed by co-treatment with prazosin (10–5 M).
Diverse secretion of VEGF-A and VEGF-C by α1- AR agonist, phenylephrine (Phe), in ER (−) MDA MB-231 cells. Treatment of MDA MB-231 cells with phenylephrine significantly decreased VEGF-A secretion (3A) and enhanced secretion of VEGF-C (3B) after 6 days of incubation. Phenylephrine-induced decrease in VEGF-A secretion alone was reversed by co-treatment with the antagonist, prazosin (Pz). *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
VEGF-C secretion was also not significantly altered after 2 and 4 days of treatment with phenylephrine (Fig. 3B). However, after 6 days of treatment, phenylephrine significantly (p < 0.05) enhanced the secretion of VEGF-C by MDA MB-231 cells in both 10–9 M and 10–6 M, although the effect was not reversed by co-treatment with prazosin.
Differential modulation of NO production in breast cancer cells by α1-AR agonist
α1-AR agonist treatment for 2 days did not affect NO production (Fig. 4A). However, phenylephrine (10–9 M and 10–6 M), treatment significantly (p < 0.05) enhanced the production of NO by MCF-7 cells after 4 and 6 days of treatment although co-treatment with the antagonist (Pz 10–5 M) reversed the agonist-mediated increase after 6 days (10–6 M).
α1-AR treatment differentially regulates NO production in ER (+) MCF-7 cells and ER (-) MDA MB-231 cells. Prolonged incubation with α1-AR agonist, phenylephrine (Phe) for 4 and 6 days enhanced the production of NO by MCF-7 cells (4A), while it did not alter NO production by MDA MB-231 cells (4B). *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
Stimulation of α1-AR on MDA MB-231 cells did not affect NO production after 2, 4, and 6 days of incubation (Fig. 4B).
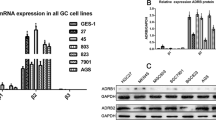
Enhancement of phosphorylation of ERK, CREB, and Akt in MCF-7 cells by α1-AR agonist
Expression of p-ERK was significantly (p < 0.05) enhanced in MCF-7 cells treated with phenylephrine for 4 days (10–9 M and 10–6 M) and 6 days (10–6 M), and reversed upon co-incubation with prazosin (10–5 M) (Fig. 5A). Interestingly, co-incubation of MCF-7 cells with prazosin (10–5 M) alone also significantly (p < 0.05) decreased p-ERK expression, after 6 days of treatment (Fig. 5A).
Effects of α1-AR signaling in ER (+) MCF-7 cells through p-ERK (5A), p-CREB (5B), and p-Akt (5C). Treatment of MCF-7 cells with phenylephrine (Phe) significantly enhanced p-ERK, p-CREB, and p-Akt expression, and the effects on p-ERK and p-Akt were reversed by co-treatment with the α1-AR antagonist, prazosin (Pz). *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
The expression of p-CREB was significantly (p < 0.05) increased in cells treated with 10–6 M of phenylephrine after 4 days of treatment, but was not reversed by co-treatment with antagonist. Treatment of MCF-7 cells with prazosin alone significantly (p < 0.05) decreased p-CREB expression after 4, and 6 days of co-incubation with prazosin (10–5 M) (Fig. 5B).
Phenylephrine (10–9 M) significantly (p < 0.05) enhanced p-Akt expression after 2 days (10–9 M) and 4 days (10–9 M, 10–6 M) of incubation (Fig. 5C). Co-incubation with prazosin, significantly (p < 0.05) decreased p-Akt expression after 2 days (10–6 M), 4 days (10–9 M), and 6 days (10–9 M, 10–6 M) of treatment. However, treatment with prazosin alone also significantly (p < 0.05) enhanced p-Akt expression after 2 and 4 days of incubation.
Suppression of p-Akt expression in MDA MB-231 cells by α1-AR agonist
Phenylephrine did not significantly alter p-ERK and p-CREB expression in the presence and absence of prazosin after 2, 4, and 6 days of treatment (Fig. 6A and B).
In vitro effects of α1-AR signaling in ER (−) MDA MB-231 cells are mediated through downregulation of p-Akt. p-ERK (6A) and p-CREB (6B) expression of MDA MB-231 cells were not altered by phenylephrine (Phe) treatment. However, p-Akt expression (6C) was significantly decreased by phenylephrine and the effect was not reversed after co-treatment with its antagonist, prazosin (Pz). *p < 0.05 compared to respective time-matched control group;#p < 0.05 compared to respective time-matched agonist-treated group.
The expression of p-Akt was significantly (p < 0.05) decreased following 2 days (10–9 M), 4 days (10–6 M) and 6 days (10–9 M, 10–6 M) of treatment of MDA MB-231 cells with phenylephrine although the effect was not reversed by co-treatment with the antagonist (Fig. 6C). Contrary to ER ( +) cell line MCF-7, co-incubation of ER (−) MDA MB-231 cells with the prazosin alone did not significantly affect p-ERK, p-CREB, or p-Akt expressions.
Enhancement of proliferation of MCF-7 and MDA MB-231 cells by α2- AR agonist
α2-AR agonist, clonidine (10–9 M), treatment of MCF-7 cells for 6 days significantly (p < 0.05) increased the proliferation of ER( +) MCF-7 cells that were not altered by the α2-AR antagonist, idazoxan (Fig. 7A). Co-treatment with idazoxan (10–5 M) significantly (p < 0.05) decreased the proliferation of clonidine-treated (10–6 M) cells after 2 and 4 days. Treatment of MCF-7 cells with idazoxan alone significantly (p < 0.05) decreased proliferation after 4 days of incubation.
α2-AR stimulation increases the proliferation of ER (+) MCF-7 and ER (−) MDA MB-231 cells. The proliferation of MCF-7 (6 days) (7A; S3A and S3B) and MDA MB-231 cells (2, 4, and 6 days) (7B; S4A and S4B) was increased by treatment with α2-AR agonist, clonidine (Clo) while co-treatment with the α2-AR-specific antagonist, idazoxan (Iz), decreased the proliferation in both the cell lines. *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
Similarly, clonidine significantly (p < 0.05) enhanced the proliferation of ER(-) MDA MB-231 cells after 2, 4, and 6 days (10–9 M, 10–6 M) of treatment (Fig. 7B). Co-incubation of cells with idazoxan significantly (p < 0.05) reversed the agonist-mediated increase in proliferation after 4 days.
Selective inhibition of VEGF-C secretion in MCF-7 cells by α2-AR agonist
There was no significant effect of clonidine treatment on VEGF-A secretion by MCF-7 cells after 2, 4, and 6 days of treatment (Fig. 8A). Co-treatment of clonidine-treated MCF-7 cells with idazoxan, and treatment with idazoxan alone significantly (p < 0.05) decreased the secretion of VEGF A after 2, 4, and 6 days.
Differential secretion of VEGF-A and VEGF-C by α2-AR agonist, clonidine (Clo), in ER (+) MCF-7 cells. VEGF-A secretion by MCF-7 cells was not altered after treatment with α2-AR agonist, clonidine (8A). In contrast, there was a decrease in VEGF-C secretion after incubation with clonidine (8B) and its specific antagonist, idazoxan (Iz). *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
However, VEGF-C secretion was significantly (p < 0.05) decreased after 2 days of incubation with clonidine, which was not reversed by co-treatment with idazoxan (Fig. 8B). Prolonged incubation of MCF-7 cells with clonidine (10–6 M) for 6 days did not significantly affect VEGF-C secretion. Interestingly, treatment of MCF-7 cells with idazoxan alone for 2 and 4 days significantly (p < 0.05) decreased VEGF-C secretion (Fig. 8B).
Enhancement of VEGF-A and VEGF-C secretion in MDA MB-231 cells by α2-AR agonist
Treatment with clonidine did not alter VEGF-A secretion after 2, 4, and 6 days of incubation in the MDA MB-231 cells (Fig. 9A).
Effects of α2-AR agonist, clonidine (Clo), on VEGF-A and VEGF-C secretion in ER (−) MDA MB-231 cells. Treatment with clonidine did not alter VEGF-A (9A) secretion in MDA MB-231 cells. However, treatment for 6 days increased VEGF-C (9B) secretion by clonidine while coincubation with α2-AR-antagonist, idazoxan (Iz), decreased it. *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
However, VEGF-C secretion was significantly (p < 0.05) enhanced upon treatment with α2-AR agonist, clonidine (10–6 M) for 6 days, and cells co-incubated with idazoxan showed a significant (p < 0.05) decrease in VEGF-C secretion after 2 and 6 days of treatment as compared with an agonist-treated group (Fig. 9B).
Suppression of NO production in MCF-7 and MDA MB-231 cells by α2-AR agonist
There was a significant (p < 0.05) decrease in NO production by ER ( +) MCF-7 cells upon treatment with clonidine (10–6 M) after 2 and 6 days of incubation (Fig. 10A). The effects of the agonist were reversed by co-treatment with idazoxan (10–5 M) after 2 and 4 days. Idazoxan alone significantly (p < 0.05) enhanced NO production after 2, 4, and 6 days of treatment.
Decline in NO production by treatment with α2-AR agonist, clonidine (Clo), in ER (+) MCF-7 and ER (−) MDA MB-231 cells. Clonidine treatment decreased NO production by ER (+) MCF-7 cells (10A) and ER (−) MDA MB-231 cells (10B). These effects were reversed by co-treatment with α2-AR- antagonist, idazoxan (Iz). *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
Treatment of ER(−) MDA MB-231 cells with clonidine significantly (p < 0.05) decreased NO production after 2 days (10–6 M) and 4 days (10–9 M and 10–6 M) (Fig. 10B). Co-treatment of clonidine-treated MDA MB-231 cells with idazoxan (10–5 M) significantly (p < 0.05) reversed the effects of the agonist on NO production after 2, 4, and 6 days. Interestingly, idazoxan alone significantly (p < 0.05) enhanced NO production in ER(-) MDA MB-231 cells after 2 and 4 days of treatment.
Selective inhibition of p-CREB expression in MCF-7 cells by α2-AR agonist
p-ERK and p-Akt expression by ER ( +) MCF-7 cells were not significantly altered by incubation with clonidine for 2, 4, and 6 days (Fig. 11A and C).
Selective downregulation of p-CREB signaling by α2-AR agonist, clonidine (Clo), in ER (+) MCF-7 cells. p-ERK (11A) and p-Akt (11C) expression by MCF-7 cells was not significantly altered by incubation with α2-AR agonist, clonidine. However, there was a decrease in p-CREB expression following treatment with clonidine and idazoxan (Iz; 11B) in MCF-7 cells. *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
However, p-CREB expression significantly (p < 0.05) declined upon incubation of MCF-7 cells with clonidine (10–9 M, 10–6 M) after 2, 4, and 6 days of treatment (Fig. 11B). Co-incubation with idazoxan did not reverse the clonidine-mediated decline in p-CREB expression. However, the co-treatment with idazoxan, has significantly (p < 0.05) decreased p-ERK expression (Clo: 10–6 M), and co-treatment of idazoxan alone has significantly (p < 0.05) lowered p-CREB expression. Co-treatment of agonist-treated MCF-7 cells with idazoxan has significantly (p < 0.05) enhanced p-Akt expression through incubation for all days.
Inhibition of p-CREB and p-Akt expression in MDA MB-231 cells by α2-AR agonist
There was no significant effect of clonidine on p-ERK expression by ER (-) MDA MB-231 cells after 2, 4, and 6 days of treatment (Fig. 12A).
Effects of α2- agonist, clonidine (Clo), on the expression of intracellular signaling molecules in ER (−) MDA MB-231 cells. Although α2-AR agonist, clonidine, did not alter p-ERK expression (12A), it significantly decreased p-CREB (12B) and p-Akt (12C) expression in MDA MB-231 cells. The clonidine-induced decline in p-CREB expression alone was reversed by co-treatment with idazoxan (Iz). α2-AR inhibition by idazoxan enhanced p-CREB expression alone. *p<0.05 compared to respective time-matched control group; #p<0.05 compared to respective time-matched agonist-treated group.
p-CREB expression was significantly (p < 0.05) decreased upon treatment with clonidine after 2 days (10–9 M, 10–6 M), 4 days (10–9 M), and 6 days (10–9 M) (Fig. 12B). The agonist-mediated decline was reversed by co-treatment with idazoxan (10–5 M) after 4 and 6 days of co-incubation. p-Akt expression was significantly (p < 0.05) decreased by treatment of ER(-) cells with clonidine for 2 and 4 days, and the effects were not reversed by co-treatment with the antagonist (Fig. 12C). Co-incubation of idazoxan alone has significantly (p < 0.05) decreased p-Akt expression in day 2 and 4.
Discussion
The cellular proliferation, secretion of pro-angiogenic factors, and activation of signaling molecules were differentially modulated by α1-AR and α2-AR agonists in ER ( +) MCF-7 and ER (−) MDA MB-231 cells in vitro in the present study. It also demonstrated that α1-AR agonist, phenylephrine, selectively enhanced the proliferation of ER( +) breast cancer cell line MCF-7, alone by enhancing the secretion of VEGF-A and NO, and activating p-ERK, p-CREB, and p-Akt signaling pathways. Although the direct effects of α1-AR stimulation on tumor cell proliferation and expression of pro-angiogenic factors have not been extensively studied, α1-expression was correlative with increased proliferation, decreased apoptosis, poor cancer-specific survival, and increased tumor recurrence [15]. The lack of α1-AR effects on ER(−) MDA MB-231 cells may, perhaps, be due to either differences in the distribution of receptor subtypes or the ER-induced signaling mechanisms on cell survival.
Phenylephrine, α1-AR agonist, enhanced VEGF-A and NO in ER( +) MCF-7 cells that may have been the result of binding of VEGF-A to its high-affinity receptor, VEGF-R2, leading to an increase in NO production through the PI3K/p-Akt pathway and thereby, enhancing cellular survival by inhibiting pro-apoptotic pathways [25,26,27]. In addition to PI3K/Akt pathway. VEGF-A binding to VEGF-R2 in endothelial cells has been shown to trigger PKC-mediated phosphorylation of sphingosine, leading to activation of H-Ras, c-Raf-1, and ERK1/2 and inducing phosphorylation of CREB in human umbilical vein endothelial cells [28,29,30]. This is in agreement with our study where phenylephrine treatment of ER( +) MCF-7 cells enhanced VEGF-A and NO production through enhanced p-Akt, p-ERK, and p-CREB expression. Phenylephrine-induced increase in the secretion of VEGF-C in ER(−) MDA MB-231 cells may promote lymphangiogenesis through its binding to VEGF-R3 receptors and activate the adapter proteins Shc, Grb2-Sos, and mediate ER1/2 phosphorylation in a Ras-dependent and -independent mechanisms in lymphatic endothelial cells [31]. Also, MDA MB-231 cells transfected with the exon-deleted version of estrogen receptor (ER)-α enhanced the secretion of VEGF in MDA MB-231 cells, thereby indicating the role of ER in activating VEGF signaling in breast cancer cells [32]. Understanding the role of adrenergic receptors in angiogenesis is relevant in the context of diseases such as cancer where angiogenesis is a critical process for tumor growth and metastasis. In vitro studies have shown that alpha-adrenergic stimulation regulates neo-angiogenesis in the endothelial cells from Wistar-Kyoto rats [33].
In the present study, incubation of breast cancer cells with α2-AR agonist, clonidine, similarly enhanced the proliferation of ER( +) MCF-7 and ER(−) MDA MB-231 cells in vitro. The pro-proliferative effects of α2-AR agonist, clonidine, have been demonstrated in DMBA-induced mammary tumors in rats, mouse mammary tumors, and MCF-7 breast cancer cell lines [9, 11, 34]. However, in vivo treatment of mice with 4T1, metastatic adenocarcinoma cell line, with highly selective α2-AR agonist, dexmedetomidine, increased tumor growth and lung metastasis without altering VEGF or IL-6 levels in the tumor that may be related to the stromal factors in the tumor environment [35]. Also, clonidine has been shown to inhibit IL-1β-induced VEGF secretion in human retinal pigment epithelial cells by suppression of intracellular signaling cascades such as p38MAPK and MEK1/2 [36]. In agreement with these findings, activation of α2-AR signaling in MCF-7 cells did not alter VEGF-A secretion, decreased VEGF-C and NO production, down-regulated p-CREB expression, and did not alter p-ERK and p-Akt expression. Similar findings were observed in ER(-) MDA MB-231 cells where no significant change was observed in VEGF-A, VEGF-C, and p-ERK expression and decreased NO, p-CREB, and p-Akt expression. The decline in the expression of p-CREB by clonidine may be due to its distinctive inhibitory effects on cAMP levels [9].
α1-AR blockade using prazosin significantly decreased the proliferation and VEGF-A secretion by ER( +) MCF-7 cells, although it did not alter proliferation and VEGF secretion in ER(−) MDA MB-231 cells. These findings were supported by results from another study where treatment of MCF-7 cells with prazosin reversed epinephrine-mediated increase in proliferation [9]. Similarly, the α2-AR antagonist, idazoxan, significantly decreased the proliferation of MCF-7 and MDA MB-231 cells and VEGF-C secretion by MCF-7 cells in the present study. Such effects were found in experimentally induced mammary tumors in animals where α2- AR blocker, rauwolscine, significantly diminished tumor growth in vivo and in vitro [11, 37]. Another α2-AR blocker, yohimbine, also inhibited cellular proliferation of cancer cells by decreasing agonist-mediated increase in the intracellular levels of cAMP in MCF-7 cells and by inducing apoptosis in PC-2 and PC-3 pancreatic cancer cell lines [9, 38]. Interestingly, breast cancer cells (MCF-7, MDA MB-231, and MDA MB-453) co-cultured with endothelial cells and treated with norepinephrine showed enhanced VEGF-A expression through activation of Notch signaling pathway mediated by norepinephrine-activated β2-AR-PKA-mTOR pathway [39]. ARs have been shown to enhance tumor angiogenesis through peroxisome proliferator-activated receptor gamma (PPARγ) signaling mechanism in animal models of breast cancer. [40].
Collectively, α1-AR agonist enhanced the proliferation and expression of pro-angiogenic factors in vitro through ERK/CREB/Akt pathways in ER( +) breast cancer cells while only VEGF-C, a lymphangiogenic factor, was enhanced in ER(−) breast cancer cells. The findings are highly relevant in-context to the involvement of alpha-adrenergic receptor in the modulation of tumor angiogenesis. α2-AR agonist on the other hand similarly enhanced proliferation and inhibited expression of pro-angiogenic factors in ER( +) and ER(−) breast cancer cells possibly through specific intracellular signaling pathways. α1- and α2-AR antagonists had distinct effects on cancer cell proliferation, expression of pro-angiogenic factors, and intracellular targets suggesting specific receptor-mediated effects. These results imply a differential role for sympathetic interactions in influencing outcomes in hormone-responsive and non-responsive breast cancers from which parallels can be drawn to develop treatment strategies by targeting adrenergic modulation of angiogenic factors affecting tumor growth. Further studies are required to explore the use of adrenergic receptor agents either alone or as part of combination therapy in the prevention and treatment of breast cancer in women.
References
Meites J. Relation of the neuroendocrine system to the development and growth of experimental mammary tumors. J Neural Transm. 1980;48:25–42.
ThyagaRajan S, Felten DL. Modulation of neuroendocrine–immune signaling by L-deprenyl and L-desmethyldeprenyl in aging and mammary cancer. Mech Ageing Dev. 2002;123:1065–79.
Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39.
ThyagaRajan S, Madden KS, Teruya B, Stevens SY, Felten DL, Bellinger DL. Age-associated alterations in sympathetic noradrenergic innervation of primary and secondary lymphoid organs in female Fischer 344 rats. J Neuroimmunol. 2011;233:54–64.
ThyagaRajan S, Tran L, Molinaro CA, Gridley DS, Felten DL, Bellinger DL. Prevention of mammary tumor development through neuroimmunomodulation in the spleen and lymph nodes of old female sprague-dawley rats by L-deprenyl. NeuroImmunoModulation. 2013;20:141–51.
Roets E, Vandeputte-Van Messom G, Peeters G. Relationship between milkability and adrenoceptor concentrations in teat tissue in primiparous cows. J Dairy Sci. 1986;69:3120–30.
Hammon HM, Bruckmaier RM, Honegger UE, Blum JW. Distribution and density of alpha- and beta-adrenergic receptor binding sites in the bovine mammary gland. J Dairy Res. 1994;61:47–57.
Inderwies T, Pfaffl MW, Meyer HHD, Blum JW, Bruckmaier RM. Detection and quantification of mRNA expression of alpha- and beta-adrenergic receptor subtypes in the mammary gland of dairy cows. Domest Anim Endocrinol. 2003;24:123–35.
Vázquez SM, Pignataro O, Luthy IA. Alpha2-adrenergic effect on human breast cancer MCF-7 cells. Breast Cancer Res Treat. 1999;55:41–9.
Vázquez SM, Mladovan AG, Pérez C, Bruzzone A, Baldi A, Lüthy IA. Human breast cell lines exhibit functional alpha2-adrenoceptors. Cancer Chemother Pharmacol. 2006;58:50–61.
Bruzzone A, Piñero CP, Castillo LF, Sarappa MG, Rojas P, Lanari C, et al. Alpha2-adrenoceptor action on cell proliferation and mammary tumour growth in mice. Br J Pharmacol. 2008;155:494–504.
Obeid EI, Conzen SD. The role of adrenergic signaling in breast cancer biology. Cancer Biomark. 2013;13:161–9.
Priyanka HP, Singh RV, Pratap UP, ThyagaRajan S. Estrogen modulates β2-adrenoceptor-induced cell-mediated and inflammatory immune responses through ER-α involving distinct intracellular signaling pathways, antioxidant enzymes, and nitric oxide. Cell Immunol. 2014;292:1–8.
Chiesa IJ, Castillo LF, Lüthy IA. Contribution of alpha2-adrenoceptors to the mitogenic effect of catecholestrogen in human breast cancer MCF-7 cells. J Steroid Biochem Mol Biol. 2008;110:170–5.
Powe DG, Voss MJ, Habashy HO, Zänker KS, Green AR, Ellis IO, et al. Alpha- and beta-adrenergic receptor (AR) protein expression is associated with poor clinical outcome in breast cancer: an immunohistochemical study. Breast Cancer Res Treat. 2011;130:457–63.
Weil J, Benndorf R, Fredersdorf S, Griese DP, Eschenhagen T. Norepinephrine upregulates vascular endothelial growth factor in rat cardiac myocytes by a paracrine mechanism. Angiogenesis. 2003;6:303–9.
Maynadier M, Nirdé P, Ramirez J-M, Cathiard AM, Platet N, Chambon M, et al. Role of estrogens and their receptors in adhesion and invasiveness of breast cancer cells. Adv Exp Med Biol. 2008;617:485–91.
Razandi M, Pedram A, Levin ER. Plasma membrane estrogen receptors signal to antiapoptosis in breast cancer. Mol Endocrinol. 2000;14:1434–47.
P Priyanka H, S Nair R, 2020 Inspire Laboratory, Institute of Advanced Research in Health Sciences, Tamil Nadu Government Multi Super Speciality Hospital, Omandurar Government Estate, Chennai-600002. Neuroimmunomodulation by estrogen in health and disease. AIMS Neuroscience. 7: 401–17.
Armaiz-Pena GN, Cole SW, Lutgendorf SK, Sood AK. Neuroendocrine influences on cancer progression. Brain Behav Immun. 2013;30:S19-25.
Thaker PH, Han LY, Kamat AA, Arevalo JM, Takahashi R, Lu C, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med. 2006;12:939–44.
Priyanka HP, ThyagaRajan S. Selective modulation of lymphoproliferation and cytokine production via intracellular signaling targets by α1- and α2-adrenoceptors and estrogen in splenocytes. Int Immunopharmacol. 2013;17:774–84.
ThyagaRajan S, Hima L, Pratap UP, Priyanka HP, Vasantharekha R. Estrogen-induced neuroimmunomodulation as facilitator of and barrier to reproductive aging in brain and lymphoid organs. J Chem Neuroanat. 2019;95:6–12.
Young WF. Adrenal Medulla, Catecholamines, and Pheochromocytoma. Goldman’s Cecil Medicine [Internet]. Elsevier Inc.; 2011 [cited 2024 Jan 31]. p. 1470–5. Available from: http://www.scopus.com/inward/record.url?scp=84904370580&partnerID=8YFLogxK.
Dayanir V, Meyer RD, Lashkari K, Rahimi N. Identification of tyrosine residues in vascular endothelial growth factor receptor-2/FLK-1 involved in activation of phosphatidylinositol 3-kinase and cell proliferation. J Biol Chem. 2001;276:17686–92.
Dimmeler S, Fleming I, Fisslthaler B, Hermann C, Busse R, Zeiher AM. Activation of nitric oxide synthase in endothelial cells by Akt-dependent phosphorylation. Nature. 1999;399:601–5.
Fulton D, Gratton J-P, McCabe TJ, Fontana J, Fujio Y, Walsh K, et al. Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601.
Mayo LD, Kessler KM, Pincheira R, Warren RS, Donner DB. Vascular endothelial cell growth factor activates CRE-binding protein by signaling through the KDR receptor tyrosine kinase. J Biol Chem. 2001;276:25184–9.
X S, W W, Rd M, D B. Sphingosine kinase mediates vascular endothelial growth factor-induced activation of ras and mitogen-activated protein kinases. Molecular and cellular biology [Internet]. 2002 [cited 2024 Jan 18];22. Available from: https://pubmed.ncbi.nlm.nih.gov/12391145/.
Takahashi T, Ueno H, Shibuya M. VEGF activates protein kinase C-dependent, but Ras-independent Raf-MEK-MAP kinase pathway for DNA synthesis in primary endothelial cells. Oncogene. 1999;18:2221–30.
Fournier E, Blaikie P, Rosnet O, Margolis B, Birnbaum D, Borg JP. Role of tyrosine residues and protein interaction domains of SHC adaptor in VEGF receptor 3 signaling. Oncogene. 1999;18:507–14.
Koduri S, Goldhar AS, Vonderhaar BK. Activation of vascular endothelial growth factor (VEGF) by the ER-alpha variant, ERDelta3. Breast Cancer Res Treat. 2006;95:37–43.
Ciccarelli M, Santulli G, Campanile A, Galasso G, Cervèro P, Altobelli GG, et al. Endothelial α1-adrenoceptors regulate neo-angiogenesis. Br J Pharmacol. 2008;153:936–46.
Lüthy IA, Bruzzone A, Piñero CP, Castillo LF, Chiesa IJ, Vázquez SM, et al. Adrenoceptors: non conventional target for breast cancer? Curr Med Chem. 2009;16:1850–62.
Szpunar MJ, Burke KA, Dawes RP, Brown EB, Madden KS. The antidepressant desipramine and α2-adrenergic receptor activation promote breast tumor progression in association with altered collagen structure. Cancer Prev Res (Phila). 2013;6:1262–72.
Watanabe K, Zhang X-Y, Kitagawa K, Yunoki T, Hayashi A. The effect of clonidine on VEGF expression in human retinal pigment epithelial cells (ARPE-19). Graefes Arch Clin Exp Ophthalmol. 2009;247:207–13.
Pérez Piñero C, Bruzzone A, Sarappa MG, Castillo LF, Lüthy IA. Involvement of α2- and β2-adrenoceptors on breast cancer cell proliferation and tumour growth regulation. Br J Pharmacol. 2012;166:721–36.
Shen S-G, Zhang D, Hu H-T, Li J-H, Wang Z, Ma Q-Y. Effects of alpha-adrenoreceptor antagonists on apoptosis and proliferation of pancreatic cancer cells in vitro. World J Gastroenterol. 2008;14:2358–63.
Chen H, Liu D, Yang Z, Sun L, Deng Q, Yang S, et al. Adrenergic signaling promotes angiogenesis through endothelial cell-tumor cell crosstalk. Endocr Relat Cancer. 2014;21:783–95.
Zahalka AH, Arnal-Estapé A, Maryanovich M, Nakahara F, Cruz CD, Finley LWS, et al. Adrenergic nerves activate an angio-metabolic switch in prostate cancer. Science. 2017;358:321–6.
Funding
Supported by the Department of Bio-Technology (BT/PR9199/Med/30/12/2007), Government of India, New Delhi.
Author information
Authors and Affiliations
Contributions
Material preparation, data collection was performed by HPP and UPP. Data analysis was performed by HPP. The first manuscript draft was prepared by HPP and RV. The manuscript draft was edited, and revised critically by RSN, HPP, and RV. The figures were edited by RSN. Project supervision and acquisition of funds by STR and RV. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Priyanka, H.P., Pratap, U.P., Nair, R.S. et al. Estrogen-receptor status determines differential regulation of α1- and α2-adrenoceptor-mediated cell survival, angiogenesis, and intracellular signaling responses in breast cancer cell lines. Med Oncol 41, 92 (2024). https://doi.org/10.1007/s12032-024-02322-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-024-02322-8