Abstract
Chronic systemic inflammatory response is proposed as an underlying mechanism for development of cancer cachexia. We conducted a prospective study to examine changes in inflammatory biomarkers during the disease course and the relationship between inflammatory biomarkers and cachexia in patients with inoperable pancreatic cancer. Twenty patients, median (range) age 67.5 (35–79) years, 5 females, were followed for median 5.5 (1–12) months. Cachexia was diagnosed according to the 2011 consensus-based classification system (weight loss >5 % past six months, BMI < 20 kg/m2 and weight loss >2 %, or sarcopenia) and the modified Glasgow Prognostic score (mGPS) that combines CRP and albumin levels. Inflammatory biomarkers were measured by enzyme immunoassays. The patients had increased levels of most inflammatory biomarkers, albeit not all statistically significant, both at study entry and close to death, indicating ongoing inflammation. According to the consensus-based classification system, eleven (55 %) patients were classified as cachectic upon inclusion. They did not differ from non-cachectic patients with regard to inflammatory biomarkers or energy intake. According to the mGPS, seven (35 %) were defined as cachectic and had a higher IL-6 (p < 0.001) than the non-cachectic patients. They also had a slightly, but insignificantly longer survival than non-cachectic patients (p = 0.08). The mGPS should be considered as an additional framework for identification of cancer cachexia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic adenocarcinoma is one of the most aggressive cancers often diagnosed at an advanced stage with a five-year survival rate less than 5 % [1, 2]. One factor related to the high mortality is cancer cachexia which is presumed to occur in a majority (>80 %) of these patients [3, 4]. Cancer cachexia is defined as a multifactorial syndrome accompanied by anorexia that cannot be fully reversed by nutritional support [5], and gradually leads to weight loss, muscular depletion, decreased physical function and psychological distress [6]. The most recent definition describes cachexia as a continuum with three stages of clinical relevance (pre-cachexia, cachexia and refractory cachexia) and associated with the underlying illness [5, 7]. Despite the efforts to establish a universally accepted cachexia definition and to develop classification criteria [5], routine standardized methods to describe the extent of cachexia and the impact on outcomes are still lacking [8]. One problem is that weight loss is used as a key criterion in the 2011 consensus-based classification system [5]. Since it is difficult to distinguish cachexia-related weight loss from weight loss caused by simple starvation, it is questionable how suitable this criterion is [4, 8].
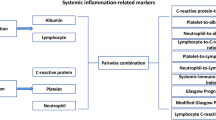
The exact mechanisms behind cancer cachexia remain unknown, but a variety of metabolic and endocrine changes which activate catabolic pathways are possibly involved [9]. Systemic inflammation seems to play an important role in the pathogenesis and is involved in weight loss and functional decline [10, 11]. The most widely used measure indicating systemic inflammation is an increase in C-reactive protein (CRP) level [5]. Elevated circulating concentrations of pro-inflammatory cytokines such as tumor necrosis factor α (TNF-α), interleukin (IL)-1, IL-6 and interferon (IFN)-γ are also responses to systemic inflammation and are postulated as mediators of the many catabolic signs associated with cancer cachexia [10]. TNF-α is among the first-line factors in promoting inflammation [12], and in experimental animal studies it causes both weight loss and anorexia [13]. TNF-α and in part IL-6 activate proteolysis, insulin resistance and apoptosis [14], while IL-1 and IFN-γ can cause hypercatabolism as well as anorexia and decreased survival in cachexia [13]. Furthermore, the various pro-inflammatory cytokines may upregulate leptin expression [10]. This hormone, secreted by the adipocytes, normally decreases food intake and increases energy consumption. It is also shown that IL-10 is an anti-inflammatory cytokine and acts by inhibiting the actions of, e.g., IL-6 in order to prevent and limit tissue damage by limiting overwhelming immune reactions [15]. Since systemic inflammation (i.e., cytokine release) seems to be the driving force behind cachexia, it is suggested that the modified Glasgow Prognostic score (mGPS) should be used to identify cancer cachexia [8]. The mGPS combines CRP and albumin and is shown to predict outcomes as well as reflect cachexia in cancer patients [8, 16].
Even if chronic ongoing systemic inflammation is present in a majority of patients with cancer, the role of inflammation and specific inflammatory biomarkers in cancer cachexia has not yet been clarified [9]. Due to the lack of longitudinal studies, it is not established whether inflammation simply is associated with the severity or progression of the cancer disease, or elicits symptoms by itself thereby representing a target for prevention or reduction of cachexia [17]. Lately, much effort has been put into measuring changes in body composition in cancer cachexia and recent studies support the value of determining muscle mass in the diagnosis [18]. However, knowledge about how inflammation and also energy intake vary during the disease trajectory is lacking. Hence, our aim was to study changes in inflammatory biomarkers and energy intake in an unselected cohort of pancreatic cancer patients with and without cachexia as they approached the terminal stage of disease. We also wanted to examine the relationship between inflammatory biomarkers and cachexia identified by two sets of classification systems, the 2011 consensus-based cachexia classification system [5] and mGPS [8]. Inflammatory biomarker levels from a cohort of healthy, normal weight individuals were included as a reference.
Patients and methods
Patients with pancreatic adenocarcinoma referred for palliative chemotherapy were included in this longitudinal pilot study at Oslo University Hospital (OUS) from March 2010 until January 2012. The patients were monitored every 4th week by two clinical nutritionists or a nurse, until death or up to one year. Eligibility criteria were histologically verified inoperable adenocarcinoma, age >18 years, understanding both verbal and written Norwegian and ability to respond to questionnaires. All eligible patients were formerly included in a pancreatic registry (a clinical interdepartmental database at OUS) including all patients referred for solid or cystic pancreatic or peri-ampullary neoplasms. The registry contained prospective data on demographic, anamnestic, diagnostic and treatment-related issues as well as patients’ self-reported symptoms collected monthly until death. Patients that reported symptoms affecting their dietary intake and/or weight loss received dietary counseling according to routine practice. Dietary advices included energy dense foods and oral nutritional supplements. Enteral or parenteral feeding was not initiated. Neither steroids nor appetite stimulants were used specifically to increase food intake, but pancreatic enzyme supplementation was prescribed when appropriate.
For most of the inflammatory biomarkers, there are no established reference values, thus we used data from a group of healthy, normal-weight adult volunteers to compare levels of cytokines and adipokines. These subjects were recruited in 2010 by advertisement in local newspapers for participation as a reference group in an intervention trial at Oslo and Akershus University College of Applied Sciences [19]. Inclusion criteria were age 18–70 years, body mass index (BMI) 17–25 kg/m2 and waist circumference ≤94 cm for men and ≤80 cm for women. Both studies were approved by the Regional Committee for Medical and Health Research Ethics South East. Patients and volunteers gave written informed consent before inclusion.
Energy intake
The 24-hour recall method was conducted as face-to-face interviews, and the patients were asked to recall food intake from the day before the interview. The quantities eaten were estimated by the patient and described in household measures as the number of units consumed (cups, glasses, spoons, number of slices, pieces, deciliters). A photographic booklet with portion sizes was used [20]. Tables of food portion sizes were used to translate household measures to weights [21].
Blood sampling and biochemistry
Non-fasting blood samples were collected from a cubital vein at the time of inclusion and then regularly every 4th week. Serum was obtained from silica gel tubes (Becton Dickinson vacutainer, Plymouth, UK) and kept on ice and centrifuged (1500g for 12 min) within one hour. Plasma was obtained from EDTA tubes (Becton Dickinson), kept on ice and centrifuged (2500g, 15 min) within 10 min. Serum and plasma samples were aliquoted and stored at −80 °C until further analyses. Serum levels of IL-10, INFγ, leptin, adiponectin, and TNF-α and plasma levels of IL-6 and insulin-like growth factor-1 (IGF-1) were measured by enzyme immunoassays from R&D Systems (Minneapolis, MN) according the manufacturer’s instructions. All analyses were performed in duplicates. The coefficients of variation for intra-assay and inter-assay variability were <5 % and <10 %, respectively, for all analyses. Results from standard blood chemistry and CRP were retrieved from the medical records.
Body composition
Muscle mass was determined by anthropometry of mid-upper-arm muscle area (MUAMA). Three trained persons performed the measurements. Triceps skin fold (TSF) was measured by using a Harpenden Skinfold Caliper and a standard, non-stretch tape on the non-dominant arm. The midpoint of the arm was measured, with the measuring tape between the shoulder (acromion) and the elbow (olecranon) while the person was bending the arm 90°. TSF and the mid-upper-arm circumference (MUAC) were measured at this midpoint. TSF was measured three times and the mean value was used. The mid-upper-arm muscle circumference (MUAMC) was calculated with the equation MUAC- (π × (TSF/10)) = MUAMC (cm) [22]. MUAMA (cm2) was derived from the MUAMC as (MUAMC)2/4π.
Weight was measured to the nearest 0.1 kg with the patient wearing light clothes and no shoes on the same scale at each visit. A correction factor of −1 kg was used to adjust for the weight of light clothing. Height was measured with a wall-mounted stadiometer to the nearest 0.1 cm. Waist and hip circumferences were measured with a standard, non-stretch tape to the nearest 0.1 cm while standing in a relaxed position with normal respiration. Waist circumference was measured at a point midway between the iliac crest and the lower rib margin. Hip circumference was measured as the maximum circumference of the posterior buttocks and the anterior symphysis.
Cachexia assessment
To be categorized as cachectic according to the consensus-based classification system, one of three criteria had to be fulfilled: weight loss >5 % during the past 6 months; or BMI < 20 kg/m2 and ongoing weight loss >2 %; or sarcopenia and ongoing weight loss >2 % [5]. Sarcopenia was determined by using MUAMA as a proxy (men <32 cm2, women <18 cm2). Furthermore, non-cachectic patients with unintentional weight loss ≤5 % during the last 6 months, anorexia (energy intake reported as <20 kcal/kg) and metabolic change (i.e., systemic inflammation with CRP > 8 mg/l) were classified as pre-cachectic [5, 23]. According to the mGPS, cachexia was classified as follows [8]:
-
CRP < 10 mg/l and albumin ≥35 g/l = 0 (no cachexia)
-
CRP < 10 mg/l and albumin <35 g/l = 0 (undernourished)
-
CRP > 10 mg/l and albumin ≥35 g/l = 0 (pre-cachexia)
-
CRP > 10 mg/l and albumin <35 g/l = 0 (refractory cachexia)
Statistics and strategy for data analysis
Because of the rapid decline in the number of participants, the data at study entry were compared with the last measurement and, when available, data collected three months or less before death. Survival was defined as time from the date of the histological diagnosis to the date of death. Data are presented as medians (range), and nonparametric tests were used. Comparison of groups was tested for significant differences with the Wilcoxon signed rank test for paired samples and the Mann-Whitney U test for unpaired samples. A comparison between the consensus classification and the mGPS was performed with a 2 × 2 contingency table and McNemar’s test with continuity correction. Missing values for concentrations of cytokines and adiponectine at baseline (three patients) were replaced with the first-observation carried-backward method [24] in all analyses. This alteration resulted in a small increase in the median value compared to the original data. A p value < 0.05 was considered statistically significant. Because of the explorative nature of this study, and the small number of patients, no multiple testing adjustments were performed. The data were analyzed with IBM SPSS Statistics v. 21 (IBM Corporation, Armonk, NY).
Results
Twenty patients (five females) with a median (range) age of 68 (35–79) years and adenocarcinoma of the pancreas (stage III and IV) were studied over a 12-month period. Six (30 %) patients had locally advanced cancer, 13 (65 %) had metastatic disease and one (5 %) had recurrent disease after an earlier pancreatic resection. The patients were treated at the discretion of the responsible physician. All patients received chemotherapy, gemcitabine (n = 17) and gemcitabine derivates (n = 3). One patient (recurrent disease) switched from chemotherapy to palliative radiotherapy (dose 8 Gy), due to severe side effects from chemotherapy. Median time from diagnosis to study entry was 7 (4–16) weeks. Overall median survival was 45.5 (14–111) weeks. At the time of censoring the data, all the patients had died.
Patient characteristics, clinical variables and body composition at study entry are shown in Table 1. The median BMI was 21.3 (15.2–30.9) kg/m2 and the daily median energy intake was 26.2 (8.6–79.7) kcal/kg. Total weight loss in the group was 6.4 (0.0–37.0) % of pre-morbid stable body weight, equivalent to a median weight loss of 3.1 (0.0–8.7) % per month. Sarcopenia was detected in two (10 %) patients.
The patients were followed for a median of 5.5 (1–12) months. The longitudinal data showed an insignificant decrease in energy intake from median 26.2 (8.6–79.7) kcal/kg at study entry to 23.7 (9.6–53.9) kcal/kg at the last measurement. Likewise, there was an insignificant decrease in weight from 63.4 (38.6–98.9) kg to 61.3 (40.1–75.0) kg. Albumin decreased significantly from a median of 43.0 mg/ml (29.0–46.0) to 39.0 (29.0–46.0) mg/ml (p = 0.01), whereas CRP increased insignificantly from median 5.8 mg/ml (0.0–51.9) to 14.1 mg/ml (4.5–69.0). Figure 1 summarizes changes in inflammatory biomarkers at study entry and three month before death. There was an increase in all inflammatory biomarkers, although statistically significant for adiponectin only (p = 0.04). IGF-1 decreased (p = 0.04) during the disease course, while INFγ remained at the same level.
Comparisons of the patients’ inflammatory biomarkers at study entry and ≤3 months before death with reference values from 40 healthy adults (14 females) are shown in Table 2. Median age of the healthy females was 47 (36–65) years and median BMI was 21.7 (17.4–25.2) kg/m2. Twenty-six healthy males had a median age of 51 (45–63) years and had a median BMI of 23.6 (20.5–25.4) kg/m2. Both at study entry and three months before death, the cancer patients had insignificantly higher median levels of IL-6, TNF-α and adiponectin, and insignificantly lower median levels of IL-10, leptin and IGF-1 than the reference group. However, the levels of IL-10 increased significantly from study entry until three months before death.
According to the 2011 consensus-based classification system, 11 (55 %) patients were classified as cachectic, one (5 %) as pre-cachectic and eight (40 %) as non-cachectic at study entry (Table 1). Since only one patient had pre-cachexia, this person was treated as non-cachectic in the analysis. No significant differences in inflammatory biomarkers or survival were found between cachectic and non-cachectic patients (Table 3). There was not difference in energy intake between the cachectic and the non-cachectic patients (p = 0.09) nor in weight change during the disease course (p = 0.26).
When using mGPS for classification, 12 (65 %) patients were non-cachectic, one (5 %) was undernourished, five (25 %) pre-cachectic and two (10 %) had refractory cachexia (Table 1). The last two groups were treated as cachectic and the undernourished as non-cachectic in the analysis. Cachectic patients had higher IL-6 (p < 0.001) and insignificantly shorter survival (p = 0.08) than non-cachectic patients (Table 4). There was no difference in energy intake between the cachectic and the non-cachectic patients (p = 0.21). One (14 %) cachectic patient gained weight during the disease course compared to five (38 %) non-cachectic (p = 0.22).
Although we found a moderate agreement between the 2011 consensus-based classification system and the mGPS regarding the number of cachectic and non-cachectic patients, namely 6/20 (30 %), the McNemar’s test failed to reject the null-hypothesis (p = 0.43) of a difference between the two classifications.
Discussion
Systemic inflammation driven by pro-inflammatory cytokines is assumed to play an important role in the development of cancer cachexia [5, 9, 11]. Production of pro-inflammatory cytokines triggers a systemic inflammation and causes an acute phase response with increased CRP and decreased albumin levels [11, 25]. In accordance with our findings, previous studies have reported increased levels of CRP, IL-6 and TNF-α in cachectic patients compared to controls [26–28]. However, when we used the 2011 consensus-based classification system to identify cancer cachexia [5], we found no differences in inflammatory biomarkers between cachectic and non-cachectic patients as reported by others [27]. We also found no significant difference in survival or energy intake between the two groups. When we used the mGPS [8], we found that cachectic patients had higher IL-6 levels than the non-cachectic patients which may be explained by using CRP as one of the criteria. The divergence between the two classifications systems may be related to the predominant focus on weight loss in the 2011 consensus-based classification system. Although sarcopenia is included as a criterion, the effect of this becomes small because anyone who has experienced weight loss >5 % will be categorized as cachectic. This emphasizes the need to rule out simple starvation before identifying cachexia [5, 29]. Patients with pancreatic cancer in particular, experience many symptoms and problems during the disease course that eventually may lead to diminished energy intake and weight loss [30, 31]. It is therefore a need for a uniform definition and objective consensus-based criteria that can exclude starvation, to improve understanding and management of cancer cachexia [5]. The mGPS excludes starvation and includes systemic inflammation by objective measures and should therefore be considered as a possible framework to supplement the 2011 consensus-based classification system [5, 8]. Furthermore, a recent study in a similar group of pancreatic patients revealed that a cachexia classification system including systemic inflammation as a criterion, was a better predictor of survival than the 2011 consensus-based classification system [32]. Interestingly, patients who had a combination of weight loss, reduced energy intake, sarcopenia and indications of metabolic change (i.e., CRP > 8 mg/l) had poorer survival than patients who did not have any of these risk factors.
Previous studies regarding cachexia and inflammation have mainly based their conclusions on results from cross-sectional studies, animal and experimental models [25, 28, 33], as opposed to the present study with a longitudinal design, relatively homogenous but small group of patients. We found that the levels of CRP and pro-inflammatory cytokines increased while that of albumin decreased during the disease course. The highest levels of pro-inflammatory cytokines were found three months or less before death. The progression of a neoplastic process probably results in an inflammatory response, characterized by production of cytokines such as IL-6 and TNF-α, and the induction of an acute phase response [34]. It is well established that serum levels of IL-6 generally are elevated in pancreatic cancer patients compared with healthy controls [35], and elevated circulating levels of IL-6 as well as IL-10 have been associated with weight loss, lipolysis and suppression of muscle synthesis [11, 33, 36]. The high levels of pro-inflammatory cytokines may therefore not be specific signs of cachexia, but rather a response of disease severity and progression [35]. Others have also questioned if IL-6 levels really capture the features of cachexia and have suggested that IL-1β better reflects the most prominent characteristics [37]. IL-1β was not measured in the present study, but we suggest including this biomarker in future studies. In the present study, IL-10 also increased during the disease course. Although IL-10 is considered anti-inflammatory, increased IL-10 is associated with worsened prognosis in chronic disease and may be a response to the increased cytokine production in cancer patients [36].
In the present study, adiponectin levels were also elevated compared with the reference values at study entry and increased toward death. This is in accordance with results obtained from a case–control study in patients with pancreatic cancer [38]. Adiponectin participates in body weight regulation with increasing levels as a response to weight loss [39]. Thus, elevated levels of adiponectin in pancreatic cancer may therefore be a response to the weight loss in the patients. Leptin plays an important role in the regulation of energy metabolism, and since the energy intake was low compared to daily needs one could expect elevated leptin levels as previously found in pulmonary cachexia [40]. We did not find this which is in accordance with results from other studies in advanced cancer [38, 39]. Plasma leptin levels are proportional to fat mass [41] and normally decrease when fat mass declines. In our study, this is reflected by a positive correlation between leptin and fat mass in our study (data not shown). Studies have also shown that leptin levels decrease with age in females [42]. Adiponectin levels normally increase with age in both genders [42]. Our patients had a median age of 67.5 years, while the reference subjects were about 17 years younger; thus, age may, at least in part, explain both the leptin and adipokines levels in the pancreatic patients.
Studies of IGF-1 levels in cancer cachexia are limited. Animal studies have shown that IGF-1 may be downregulated in models of cachexia [43]. A previous clinical study that defined cachexia by unintentional weight loss >5 % the previous 6 months, reported decreased levels of IGF-1 in cachectic patients compared with weight-stable patients and healthy controls [27]. IGF-1 reportedly predicts lean tissue mass in cancer [44]. In line with these studies, we found a decrease during the course of disease, possibly reflecting weight loss and/or loss of fat free mass. We also found lower IGF-1 levels in the pancreatic cancer patients than in the reference group, however not significantly. This may be explained with weight loss, but also the fact that IGF-1 levels can be influenced by the difference in age between the two groups. Age-related decline in the serum levels has been documented in earlier studies [45, 46].
The exact mechanisms of weight loss in cachexia are not fully understood, but both loss of appetite and hypermetabolism may play a role in wasting [9]. In this study, much of the weight loss could be explained by a low energy intake. A median intake of 26.2 kcal/kg at study entry is considered low and insufficient to maintain body weight [47]. An additional decrease in the energy intake and weight loss was seen during the disease course.
The main limitations of our study were the small sample size and the high attrition due to the disease severity and short survival in pancreatic cancer. However, the median survival (45.5 weeks) was in line with expected survival in pancreatic cancer [48]. This means that some patients can be followed for a relatively long period, with adequate nutritional interventions and symptomatic treatment to improve functional status and quality of life [49].
In conclusion, we found that patients with advanced pancreatic cancer had increased, albeit insignificant, levels of most inflammatory biomarkers, both at study entry and close to death, indicating ongoing inflammation. Moreover, patients classified as cachectic by the 2011 consensus-based classification system did not have higher levels of inflammatory biomarkers than non-cachectic patients. When mGPS was used to identify and classify cachexia, the cachectic patients had higher levels of IL-6 and slightly lower survival than the non-cachectic patients, which is in line with the definition of cancer cachexia. The mGPS should be considered as an additional framework for identification of cancer cachexia to be validated in future longitudinal studies.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi:10.3322/CA.2007.0010.
Kneuertz PJ, Cunningham SC, Cameron JL, Torrez S, Tapazoglou N, Herman JM, et al. Palliative surgical management of patients with unresectable pancreatic adenocarcinoma: trends and lessons learned from a large, single institution experience. J Gastrointest Surg. 2011;15(11):1917–27. doi:10.1007/s11605-011-1665-9.
Wigmore SJ, Plester CE, Richardson RA, Fearon KC. Changes in nutritional status associated with unresectable pancreatic cancer. Br J Cancer. 1997;75(1):106–9.
Tisdale MJ. Cancer cachexia. Curr Opin Gastroenterol. 2010;26(2):146–51. doi:10.1097/MOG.0b013e3283347e77.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–95. doi:10.1016/S1470-2045(10)70218-7.
Hopkinson JB, Wright DN, McDonald JW, Corner JL. The prevalence of concern about weight loss and change in eating habits in people with advanced cancer. J Pain Symptom Manage. 2006;32(4):322–31. doi:10.1016/j.jpainsymman.2006.05.012.
Evans WJ, Morley JE, Argiles J, Bales C, Baracos V, Guttridge D, et al. Cachexia: a new definition. Clin Nutr. 2008;27(6):793–9. doi:10.1016/j.clnu.2008.06.013.
Douglas E, McMillan DC. Towards a simple objective framework for the investigation and treatment of cancer cachexia: the Glasgow Prognostic Score. Cancer Treat Rev. 2014;40(6):685–91.
Blum D, Omlin A, Baracos VE, Solheim TS, Tan BH, Stone P, et al. Cancer cachexia: a systematic literature review of items and domains associated with involuntary weight loss in cancer. Crit Rev Oncol Hematol. 2011;80(1):114–44. doi:10.1016/j.critrevonc.2010.10.004.
Gulen ST, Karadag F, Karul AB, Kilicarslan N, Ceylan E, Kuman NK, et al. Adipokines and systemic inflammation in weight-losing lung cancer patients. Lung. 2012;190(3):327–32.
Roxburgh CSD, McMillan DC. Cancer and systemic inflammation: treat the tumour and treat the host. Br J Cancer. 2014;110(6):1409–12. doi:10.1038/bjc.2014.90.
Cesari M, Penninx BWJH, Pahor M, Lauretani F, Corsi AM, Williams GR, et al. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol Ser A Biol Sci Med Sci. 2004;59(3):M242–8. doi:10.1093/gerona/59.3.M242.
Tuca A, Jimenez-Fonseca P, Gascon P. Clinical evaluation and optimal management of cancer cachexia. Crit Rev Oncol Hematol. 2013;88(3):625–36. doi:10.1016/j.critrevonc.2013.07.015.
Martignoni ME, Kunze P, Hildebrandt W, Kunzli B, Berberat P, Giese T, et al. Role of mononuclear cells and inflammatory cytokines in pancreatic cancer-related cachexia. Clin Cancer Res. 2005;11(16):5802–8. doi:10.1158/1078-0432.CCR-05-0185.
Sabat R, Grütz G, Warszawska K, Kirsch S, Witte E, Wolk K, et al. Biology of interleukin-10. Cytokine Growth Factor Rev. 2010;21(5):331–44.
Laird BJ, Kaasa S, McMillan DC, Fallon MT, Hjermstad MJ, Fayers P, et al. Prognostic factors in patients with advanced cancer: a comparison of clinicopathological factors and the development of an inflammation-based prognostic system. Clin Cancer Res. 2013;19(19):5456–64.
Klepstad P, Kaasa S. The importance and pitfalls of correlational science in palliative care research. Curr Opin Support Palliat Care. 2012;6(4):508–13. doi:10.1097/SPC.0b013e32835a0c70.
Prado CM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, et al. Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res. 2009;15(8):2920–6. doi:10.1158/1078-0432.CCR-08-2242.
Wesseltoft-Rao N, Holven KB, Telle-Hansen VH, Narverud I, Iversen PO, Hjermstad MJ, et al. Measurements of body fat is associated with markers of inflammation, insulin resistance and lipid levels in both overweight and in lean, healthy subjects. e-SPEN Journal. 2012;7(6):e234–40. doi:10.1016/j.clnme.2012.10.002.
Lillegaard IT, Andersen LF. Validation of a pre-coded food diary with energy expenditure, comparison of under-reporters v. acceptable reporters. Br J Nutr. 2005;94(6):998–1003.
Blaker B, Aarsland M. Mål og vekt for matvarer. Oslo: Landsforeningen for Kosthold & Helse; 1989. p. 6–41.
Thomas B. Manual of dietetic practice. 2nd ed. Oxford: Blacwell; 1994.
van der Meij BS, Schoonbeek CP, Smit EF, Muscaritoli M, van Leeuwen PA, Langius JA. Pre-cachexia and cachexia at diagnosis of stage III non-small-cell lung carcinoma: an exploratory study comparing two consensus-based frameworks. Br J Nutr. 2013;109(12):2231–9. doi:10.1017/S0007114512004527.
Engels JM, Diehr P. Imputation of missing longitudinal data: a comparison of methods. J Clin Epidemiol. 2003;56(10):968–76. doi:10.1016/S0895-4356(03)00170-7.
Seelaender M, Batista M Jr, Lira F, Silverio R, Rossi-Fanelli F. Inflammation in cancer cachexia: to resolve or not to resolve (is that the question?). Clin Nutr. 2012;31(4):562–6. doi:10.1016/j.clnu.2012.01.011.
Bilir C, Engin H, Can M, Temi Y, Demirtas D. The prognostic role of inflammation and hormones in patients with metastatic cancer with cachexia. Med Oncol. 2015;32(3):1–6. doi:10.1007/s12032-015-0497-y.
Garcia JM, Garcia-Touza M, Hijazi RA, Taffet G, Epner D, Mann D, et al. Active ghrelin levels and active to total ghrelin ratio in cancer-induced cachexia. J Clin Endocrinol Metab. 2005;90(5):2920–6. doi:10.1210/jc.2004-1788.
Kemik O, Sumer A, Kemik AS, Hasirci I, Purisa S, Dulger AC, et al. The relationship among acute-phase response proteins, cytokines and hormones in cachectic patients with colon cancer. World J Surg Oncol. 2010;8:85. doi:10.1186/1477-7819-8-85.
Khalid U, Spiro A, Baldwin C, Sharma B, McGough C, Norman AR, et al. Symptoms and weight loss in patients with gastrointestinal and lung cancer at presentation. Support Care Cancer. 2006;15(1):39–46. doi:10.1007/s00520-006-0091-0.
Bye A, Jordhoy MS, Skjegstad G, Ledsaak O, Iversen PO, Hjermstad MJ. Symptoms in advanced pancreatic cancer are of importance for energy intake. Support Care Cancer. 2013;21(1):219–27. doi:10.1007/s00520-012-1514-8.
Yavuzsen T, Walsh D, Davis MP, Kirkova J, Jin T, LeGrand S, et al. Components of the anorexia-cachexia syndrome: gastrointestinal symptom correlates of cancer anorexia. Support Care Cancer. 2009;17(12):1531–41. doi:10.1007/s00520-009-0623-5.
Wesseltoft-Rao N, Hjermstad MJ, Ikdahl T, Dajani O, Ulven SM, Iversen PO, et al. Comparing two classifications of cancer cachexia and their association with survival in patients with unresected pancreatic cancer. Nutr Cancer. 2015;67(3):472–80.
Kyrana E, Briggs S, Dhawan A. Molecular mechanisms of cachexia in chronic disease. Expert Rev Endocrinol Metab. 2012;7(1):73–90. doi:10.1586/eem.11.87.
Gordon JN, Green SR, Goggin PM. Cancer cachexia. Q J Med. 2005;98:779–88. doi:10.1093/qjmed/hci127.
Holmer R, Goumas FA, Waetzig GH, Rose-John S, Kalthoff H. Interleukin-6: a villain in the drama of pancreatic cancer development and progression. Hepatobiliary Pancreat Dis Int. 2014;13(4):371–80. doi:10.1016/S1499-3872(14)60259-9.
Ebrahimi B, Tucker SL, Li D, Abbruzzese JL, Kurzrock R. Cytokines in pancreatic carcinoma. Cancer. 2004;101(12):2727–36. doi:10.1002/cncr.20672.
Scheede-Bergdahl C, Watt HL, Trutschnigg B, Kilgour RD, Haggarty A, Lucar E, et al. Is IL-6 the best pro-inflammatory biomarker of clinical outcomes of cancer cachexia? Clin Nutr. 2012;31(1):85–8. doi:10.1016/j.clnu.2011.07.010.
Dalamaga M, Migdalis I, Fargnoli JL, Papadavid E, Bloom E, Mitsiades N, et al. Pancreatic cancer expresses adiponectin receptors and is associated with hypoleptinemia and hyperadiponectinemia: a case-control study. Cancer Causes Control. 2009;20(5):625–33. doi:10.2307/40272028.
Wolf I, Sadetzki S, Kanety H, Kundel Y, Pariente C, Epstein N, et al. Adiponectin, ghrelin, and leptin in cancer cachexia in breast and colon cancer patients. Cancer. 2006;106(4):966–73. doi:10.1002/cncr.21690.
Creutzberg EC, Wouters EFM, Vanderhoven-Augustin IML, Dentener MA, Schols AMWJ. Disturbances in leptin metabolism are related to energy imbalance during acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;162(4):1239–45. doi:10.1164/ajrccm.162.4.9912016.
Li M-D. Leptin and beyond: an odyssey to the central control of body weight. Yale J Biol Med. 2011;84(1):1–7.
Schautz B, Later W, Heller M, Peters A, Müller MJ, Bosy-Westphal A. Impact of age on leptin and adiponectin independent of adiposity. Br J Nutr. 2012;108(02):363–70. doi:10.1017/S0007114511005605.
Costelli P, Muscaritoli M, Bossola M, Penna F, Reffo P, Bonetto A, et al. IGF-1 is downregulated in experimental cancer cachexia. Am J Physiol Regul Integr Comp Physiol. 2006;291(3):R674–R83. doi:10.1152/ajpregu.00104.2006.
Fouladiun M, Korner U, Bosaeus I, Daneryd P, Hyltander A, Lundholm KG. Body composition and time course changes in regional distribution of fat and lean tissue in unselected cancer patients on palliative care–correlations with food intake, metabolism, exercise capacity, and hormones. Cancer. 2005;103(10):2189–98. doi:10.1002/cncr.21013.
Hall DT, Ma JF, Di Marco S, Gallouzi I-E. Inducible nitric oxide synthase (iNOS) in muscle wasting syndrome, sarcopenia, and cachexia. Aging (Albany NY). 2011;3(8):702–15.
Vlachostergios PJ, Gioulbasanis I, Kamposioras K, Georgoulias P, Baracos VE, Ghosh S, et al. Baseline insulin-like growth factor-I plasma levels, systemic inflammation, weight loss and clinical outcome in metastatic non-small cell lung cancer patients. Oncology. 2011;81(2):113–8. doi:10.1159/000331685.
Thoresen L, Fjeldstad I, Krogstad K, Kaasa S, Falkmer UG. Nutritional status of patients with advanced cancer: the value of using the subjective global assessment of nutritional status as a screening tool. Palliat Med. 2002;16(1):33–42.
Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic cancer. Lancet. 2004;363(9414):1049–57. doi:10.1016/S0140-6736(04)15841-8.
Labori KJ, Hjermstad MJ, Wester T, Buanes T, Loge JH. Symptom profiles and palliative care in advanced pancreatic cancer: a prospective study. Support Care Cancer. 2006;14(11):1126–33. doi:10.1007/s00520-006-0067-0.
Acknowledgments
The entire data collection was carried out at the Departments of Surgery, Oncology and Palliative Care at Oslo University Hospital. Appreciation is expressed to the staff of the study and to patients who participated.
Funding
This study was funded by Oslo and Akershus University College of Applied Sciences and Hole’s trust fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bye, A., Wesseltoft-Rao, N., Iversen, P.O. et al. Alterations in inflammatory biomarkers and energy intake in cancer cachexia: a prospective study in patients with inoperable pancreatic cancer. Med Oncol 33, 54 (2016). https://doi.org/10.1007/s12032-016-0768-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-016-0768-2