Abstract
Concurrent chemoradiotherapy is the standard treatment for patients with locally advanced lung cancer. The most common dose-limiting adverse effect of thoracic radiotherapy (RT) is radiation pneumonia (RP). A randomized comparison study was designed to investigate targeted percutaneous microwave ablation at pulmonary lesion combined with mediastinal RT with or without chemotherapy (ablation group) in comparison with RT (target volume includes pulmonary tumor and mediastinal node) with or without chemotherapy (RT group) for the treatment of locally advanced non-small cell lung cancers (NSCLCs). From 2009 to 2012, patients with stage IIIA or IIIB NSCLCs who refused to undergo surgery or were not suitable for surgery were enrolled. Patients were randomly assigned to the RT group (n = 47) or ablation group (n = 51). Primary outcomes were the incidence of RP and curative effectiveness (complete response, partial response, and stable disease); secondary outcome was the 2-year overall survival (OS). Fifteen patients (31.9 %) in the RT and two (3.9 %) in the ablation group experienced RP (P < 0.001). The ratio of effective cases was 85.1 versus 80.4 % for mediastinal lymph node (P = 0.843) and 83.0 versus 100 % for pulmonary tumors (P = 0.503), respectively, for the RT and ablation groups. Kaplan–Meier analysis demonstrated 2-year OS rate of NSCLC patients in ablation group was higher than RT group, but no statistical difference (log-rank test, P = 0.297). Percutaneous microwave ablation followed by RT for inoperable stage III NSCLCs may result in a lower rate of RP and better local control than radical RT treatments.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the main cause of death due to cancer in both men and women worldwide accounting for 1.82 million cases and 1.6 million deaths in 2012 [1]. In 70 to 80 % of patients, the diagnosis is made at an advanced stage [2, 3]. A high proportion, 80 %, of lung cancer cases are classified as non-small cell lung cancer (NSCLC) [4]. Although the management of NSCLC has continued to improve over the past 5 years, due to late diagnosis the prognosis remains poor with a 5-year survival rate of about 16 % [5]. NSCLC can be classed according to its degree of invasiveness into four stages. Early stages I and II of NSCLC are generally treatable with surgical resection, but stage IIIA when the disease has spread to the lymph nodes in the middle of the chest is the point at which multimodal therapy needs to be considered [6]. Locally advanced NSCLC (LA-NSCLC) is a heterogeneous disease, encompassing stage IIIA. Many patients with LA-NSCLC are not suitable for surgery [6]. But therapy for stages IIIA and IIIB is associated with high rates of distant metastasis, local recurrence and toxicity [7]. The use of modern radiotherapy (RT) techniques has improved outcomes in some patients with limited metastatic disease [8].
Concurrent chemoradiotherapy is the recommended standard treatment modality for patients with locally advanced lung cancer [9]. However, RT risks adverse effects due to the sensitive nature of local tissues, commonly resulting in radiation pneumonia (RP) [10], and RP is the most common dose-limiting adverse effect of thoracic RT. Carefully targeted RT is intended to prevent RP by methods such as three-dimensional conformal radiotherapy (3DCRT), intensity-modulated radiotherapy (IMRT), and radiofrequency ablation minimizing the damage to normal tissue when a high dose is delivered to the tumor [11, 12], although RP is often inevitable especially in multiple mediastinal lymph nodes and/or larger pulmonary tumors, and sometimes, it is serious [13].
Another thermal ablative technique, involving microwaves, has also been considered recently in the treatment of lung tumors [14–16]. Although less studied than radiofrequency ablation, microwave ablation may have some advantages in that the microwave energy is deployed over a larger zone with higher temperatures produced faster [17]. This would allow larger tumors to be ablated with a higher degree of accuracy than with radiofrequency ablation, as shown in an animal model [18]. Thus, some studies have successfully used microwave ablation to treat unresectable NSCLC and found it to be a safe and reliable method [19–21]. However, it remains unclear whether microwave ablation provides significant benefits when compared to RT, in particular in terms of the incidence of RP resulting from treatment. Therefore, the aim of this study was to investigate targeted percutaneous microwave ablation at pulmonary lesions combined with mediastinal radiotherapy with or without chemotherapy in LA-NSCLC, in contrast to concurrent chemoradiotherapy or radiotherapy alone. The treatment methods were compared in terms of the ratio of RP and treatment effectiveness [complete response (CR), partial response (PR), and stable disease (SD) described as effectiveness] 3 months after RT. The secondary outcome was the 2-year overall survival (OS).
Materials and methods
Patients
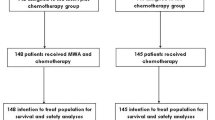
The study population was consecutively recruited from 132 patients with stage IIIA or IIIB NSCLCs who refused to undergo surgery or were not suitable for surgery at the Qilu Hospital from January 2009 to September 2012. The inclusion criteria were: (1) Karnofsky performance scale (KPS) score >60 points; (2) pulmonary reserve greater than severe obstructive or severe restrictive ventilatory dysfunction, and (3) cell pathology or histopathology confirmed the stage IIIA or IIIB NSCLC. The exclusion criteria were: (1) KPS score ≤60 points, (2) pulmonary reserve was severe obstructive or severe restrictive ventilatory dysfunction, (3) severe liver and kidney dysfunction, and (4) severe coagulopathy. According to the exclusion criteria, a total of 34 patients were excluded, so finally 98 patients with IIIA or IIIB NSCLC were finally enrolled (Fig. 1).
The diagnoses of all the patients were confirmed using the pathological results of bronchofibroscopy or percutaneous lung biopsy; in addition, the diagnoses in 54 patients were further confirmed using the pathological examinations of mediastinal lymph nodes obtained by mediastinoscopy or percutaneous biopsy [22].
The patients were randomly (simple randomization) assigned to the targeted percutaneous microwave ablation at pulmonary lesion combined with mediastinal radiotherapy with or without chemotherapy (ablation group n = 51) or radiotherapy (target volume includes pulmonary tumor and mediastinal node) with or without chemotherapy (radiotherapy group n = 47). This prospective cohort study was approved by the local ethics committee and institutional review board (Pingyi branch of Qilu Hospital affiliated to Shandong University, China). (Approval ID: 200901116), and all participants provided written informed consent.
Computed tomography guidance
A 16-slice spiral computed tomography (CT) machine (SOMATOM Emotion, Siemens, Germany) was used for imaging guidance. An outline of the positions of adjacent organs was made during conventional preoperative CT scanning. Based on the location of the lesion and its relationship with adjacent and vital structures, the optimal position of the patient and insertion sites of the required instrument were identified (Fig. 2a).
Computed tomography (CT) images of the microwave ablation procedure and follow-up. a CT guidance in microwave ablation; b puncture of the tumor; c ablation procedure; d enhanced CT scanning 1 month after ablation; e, f enhanced CT images 2 years after ablation e lung window; and f mediastinal window. Both e and f images are at the same CT level
Interventions for the ablation group
The patients in the ablation group all received targeted percutaneous microwave ablation at the pulmonary lesions combined with mediastinal radiotherapy with or without chemotherapy. The microwave ablation was performed either before or at 1 week after mediastinal RT. The microwave ablation system was a CO-100C Microwave System (Nanjing Eco Microwave System Co., Ltd., China) with a disposable microwave ablation probe: ECO-100AL8 (Nanjing Eco Microwave System Co., Ltd.). The puncture site for the ablation antenna was determined according to the size, shape, and adjacent relationships of the tumors; the pattern of ablation (single-point or multipoint ablation) was also determined accordingly. Reconstruction of the CT image was done to reassure the ablation site after the puncture (Fig. 2b), and then, the microwave device was turned on. The parameters were as follows: power of 60–75 W and time for a single-point ablation of 4–8 min. Bubble formation could be observed inside the tumor during the ablation (Fig. 2c). Enhanced CT scanning of the chest was performed in the patients 1 month later to exclude the existence of insufficient ablation regions; secondary ablation was performed if there were enhanced regions in the soft tissues (Fig. 2d).
Ablations were followed or preceded by 3DCRT standard fraction external beam RT, once per day, five times per week using a linear accelerator (BJ6B; Beijing Medical Apparatus and Instrument Institute, China) and treatment planning system (Topslane Venus, Shanghai, China). The RT covered the enlarged mediastinal lymph nodes but not the tumor in the lungs. Single RT was provided if the patient was older than 70 years, had a history of cardiopulmonary disease, a poor cardiopulmonary reserve, or was in a generally good condition but refused chemotherapy. Otherwise the patients underwent concurrent chemoradiotherapy. The chemotherapy administered included a schema of paclitaxel (Yangtze River Pharmaceutical Group, Jiangsu, China) plus cisplatin (Haosen Pharmaceutical Group, Jiangsu, China) for two cycles.
Interventions for the radiotherapy group
Patients in the radiotherapy group also received either single RT or concurrent chemoradiotherapy as for the ablation group. 3DCRT (conventional fractionated radiotherapy, once per day, five times per week) was provided for the enlarged mediastinal lymph nodes as well as the tumor in the lungs. Chemotherapy drugs included paclitaxel plus cisplatin (two cycles).
Outcomes
Primary outcomes were the incidence of RP and curative effectiveness. CT scanning of the chest was performed at 3 months after RT, and the Response Evaluation Criteria In Solid Tumors criteria were used for evaluating the treatment effects [23] [complete response (CR), partial response (PR), and stable disease (SD) were classified as effective, while progressive disease (PD) was classified as progression]. Remission of the tumor in the lungs and of mediastinal lymph nodes and the rate of incidence of RP (according to the Radiation Therapy Oncology Group/European Organization for Research and Treatment of Cancer evaluation criteria, namely Subjective, Objective, Management, Analytic Scales, acute RP ≥ 2 was included for the calculation) were evaluated [24].
Secondary outcome was the 2-year overall survival (OS). The patients were followed up by telephone once a month and every 3 months by imaging (chest abdomen enhanced CT, brain MRI) within 6 months after treatment. After 6 months, the patients were followed up once every 3 months. The rate of 2-year OS was calculated; the OS was measured from the time of diagnosis to death.
Statistical analysis
Statistical software SPSS version 13.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Data were expressed as median (min, max) and compared using Mann–Whitney U for independent samples. Categorical variables were compared using the Fisher’s exact test or Pearson Chi-square test, as appropriate. The Kaplan–Meier and log-rank tests were used for survival analysis. The threshold of statistical significant was P < 0.05.
Results
Baseline characteristics
Patients’ baseline characteristics are given in Table 1. There were 65 men and 33 women with an age range of 42–76 years recruited between January 2009 and September 2012. Among the 98 patients, 35, 42, 9, and 12 patients were diagnosed with squamous carcinoma, adenocarcinoma, adenosquamous carcinoma, and large cell carcinoma, respectively. Thirty-nine patients were diagnosed with stage IIIA carcinoma (including 12 with T1N2M0, 8 with T2N2M0, 7 with T3NIM0, and 12 with T3N2M0 carcinoma) and 59 patients were diagnosed with stage IIIB carcinoma (including 5 with T4N2M0, 11 with T4N3M0, 17 with T1N3M0, 14 with T2N3M0, and 12 with T3N3M0 carcinoma).
Fifty-one patients were assigned to the ablation group, 18 of those patients received single radiotherapy (DT5400-6000cGy/27-30f), while 33 patients received concurrent chemoradiotherapy (DT5600-6000cGy/28-30f). Forty-seven patients were included in the radiotherapy group. Fifteen patients received single radiotherapy (DT5400-6000cGy/27-30f over 6 weeks) due to their age and cardiopulmonary functions, and 32 patients received concurrent chemoradiotherapy (DT5600-6000cGy/28-30f over 6 weeks). There were no significant differences between the groups in terms of gender, TNM stage, histology or the number of patients receiving either radiotherapy alone or concurrent chemoradiotherapy (Table 1).
Curative effectiveness and incidence of RP
Enhanced CT scanning of the chest was performed at 3 months after chemotherapy to evaluate the rate of remission of the pulmonary tumor and mediastinal lymph nodes as an indication of staging. In the mediastinal lymph node, curative effectiveness was found in 40 (85.1 %) patients in the radiotherapy group including 16, 19, and 5 patients who had CR, PR, and SD, respectively, while 41 (80.4 %) suggested curative effectiveness in the ablation group with 14, 22, and 5 patients who had CR, PR, and SD, respectively. PD was found in 7 (14.9 %) patients in the radiotherapy group and 10 (19.6 %) in the ablation group. Chi-square test was used to compare the differences between the two groups, and the results did not show any significant difference (P = 0.843; Table 2). In the pulmonary lesion, curative effectiveness was suggested in 39 (83.0 %) patients in the radiotherapy group with 6, 22, and 11 patients who had CR, PR, and SD, respectively. In the ablation group, curative effectiveness was suggested in 51 (100 %) patients and 12, 23, and 16 who had CR, PR, and SD, respectively. The differences between the two groups were not significant (P = 0.503). PD was found in 8 (17.0 %) patients in the radiotherapy group and 0 (0 %) in the ablation group (Table 2). In many patients, the tumor in the lungs disappeared completely, and the patients lived for a long time (Fig. 2e, f).
The rate of incidence of RP was 31.9 and 3.9 % in the radiotherapy group and the ablation group, respectively (Table 3), and the difference was statistically significant (P < 0.001).
Two-year OS
The patients were followed up for 2 years. No patients were lost to follow-up. Kaplan–Meier survival curves demonstrated 2-year OS rate of NSCLC patients in ablation group was higher than radiotherapy group, but no statistical difference (log-rank test, P = 0.297) (Fig. 3).
Kaplan–Meier curves showing the cumulative survival rate of patients with locally advanced non-small cell lung cancer (NSCLC) treated with radiotherapy concurrent chemotherapy (radiotherapy group) (blue curve) or targeted percutaneous microwave ablation at pulmonary lesion combined with mediastinal radiotherapy concurrent chemotherapy (ablation group) (green curve) (log-rank test, P = 0.297)
Adverse events in relation to microwave ablation
It was also found that the rate of incidence of pneumothorax was 17.6 % in the ablation group, and drainage was required for three cases. Nine patients had a small amount of hemoptysis during surgery or postoperatively in the ablation group, and symptomatic remission occurred after treatment. There were no severe or fatal cases.
Discussion
Concurrent chemoradiation is the method recommended by the National Comprehensive Cancer Network guideline for the treatment of stage III NSCLS [25, 26]. However, RP is often unavoidable using this method. Microwave ablation has shown some promise in treating lung cancer [19–21] and may result in lower rates of RP. The aim of this study was to directly compare, in terms of the incidence of RP and curative effectiveness, microwave ablation in combination with mediastinal RT and chemotherapy with the recommended method of radiotherapy and chemotherapy. The results show that the incidence of RP was lower in the ablation group compared with the radiotherapy group, and the results were statistically significant. However, curative effectiveness was similar in both groups, but no patients experienced PD in the ablation group and this was significantly different to the radiotherapy group. Two-year OS was also similar between groups.
It has previously been suggested that the major factor influencing the development of RP is the ratio of irradiated pulmonary volume to the overall pulmonary volume, namely the value of V20 [13]. Adjusting the target region, and the angle and direction of the x-ray could reduce the irradiated volume; however, in some cases where the mass is large, mass is located at the lung periphery, and multiple mediastinal lymph nodes are involved that need to be irradiated, the V20 could not be reduced and thus the risk of developing RP is very high.
Minimally invasive treatments have been introduced in recent years, and of these, percutaneous ablation seems to be an attractive option in lung cancer [27, 28]. Image-guided ablation has been recently introduced as a safe, alternative treatment of localized disease in selected patients. The three main ablative treatments currently used in the lung are radiofrequency ablation, microwave ablation, and percutaneous cryotherapy [29]. Yang et al. [20] found that percutaneous microwave ablation is safe and effective for the treatment of medically inoperable stage I peripheral NSCLC. Microwave ablation may be safely and effectively used as a therapeutic tool for the treatment of pulmonary metastases [30]. Several studies have used combined treatment of percutaneous image-guided microwave ablation and RT for patients with inoperable stage I/II NSCLC. With low rates of complication, combined treatment may result in an improved survival compared with either modality alone [31].
In the present study, in the ablation group microwave ablation was used to treat the pulmonary tumors and 3DCRT plus concurrent chemotherapy was used to treat the mediastinal lymph nodes. The incidence of RP in the ablation group was lower than in the radiotherapy group. The reason for this might be the reduced radiation volume of the lungs. In contrast, the effectiveness of the treatment, which was evaluated at 3 months after RT, showed no significant difference in the mediastinal tumor between the two groups, while the remission rate of the pulmonary tumor was higher in the ablation group than in the radiotherapy group. The 2-year OS rate was also not significantly different between the two groups. These results were in accordance with previous findings [32].
Although the 2-year OS rate was not significantly different between the two groups, the lower rate of incidence of RP in the combination group suggested that the patients in the combination group had better quality of life. However to date, it is not clear whether the higher remission rate of the pulmonary tumor and the lower rate of incidence of RP could improve the survival rate, and further studies with longer-term follow-ups are needed to evaluate this hypothesis.
This study has some limitations. The sample size was quite small and was based in a single center so the results need to be confirmed in a larger study. Quality of life and other measures of patient experience of the treatment were not directly studied so should be considered in future to truly evaluate the value of microwave ablation for treatment of NSCLC. The follow-up period of 2 years was quite short. A longer follow-up period may provide some difference between the groups in terms of survival rates.
Percutaneous microwave ablation in combination with mediastinal radiotherapy, with or without chemotherapy, compared to radiotherapy of the pulmonary lesion and mediastinal region, with or without chemotherapy, suggests that both methods achieve similar outcomes in terms of curative effectiveness and two-year OS. However, there was a significantly lower incidence of RP in the patients treated with microwave ablation. These results suggest that microwave ablation should be considered for the treatment of inoperable stage III NSCLCs.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86.
Becker N, Motsch E, Gross ML, Eigentopf A, Heussel CP, Dienemann H, et al. Randomized study on early detection of lung cancer with MSCT in Germany: study design and results of the first screening round. J Cancer Res Clin Oncol. 2012;138:1475–86.
Shao Q, Li J, Li F, Wang S, Wang W, Liu S, et al. Clinical investigation into the initial diagnosis and treatment of 1168 lung cancer patients. Oncol Lett. 2015;9:563–8.
Shtivelman E, Hensing T, Simon GR, Dennis PA, Otterson GA, Bueno R, et al. Molecular pathways and therapeutic targets in lung cancer. Oncotarget. 2014;5:1392–433.
Chermiti Ben Abdallah F, Ben Ali G, Sadok Boudaya M, Mlika M, Chtourou A, Taktak S, et al. Treatment and prognosis of advanced stage non-small-cell lung cancer. Rev Mal Respir. 2014;31:214–20.
Al-Shahrabani F, Vallbohmer D, Angenendt S, Knoefel WT. Surgical strategies in the therapy of non-small cell lung cancer. World J Clin Oncol. 2014;5:595–603.
Chang JY, Kestin LL, Barriger RB, Chetty IJ, Ginsburg ME, Kumar S et al. ACR appropriateness criteria(R) nonsurgical treatment for locally advanced non-small-cell lung cancer: good performance status/definitive intent. Oncology (Williston Park). 2014; 28: 706–10, 12, 14 passim.
Laine AM, Westover KD, Choy H. Radiation therapy as a backbone of treatment of locally advanced non-small cell lung cancer. Semin Oncol. 2014;41:57–68.
Vansteenkiste J, De Ruysscher D, Eberhardt WE, Lim E, Senan S, Felip E et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24 Suppl 6: vi89–98.
Dang J, Li G, Zang S, Zhang S, Yao L. Comparison of risk and predictors for early radiation pneumonitis in patients with locally advanced non-small cell lung cancer treated with radiotherapy with or without surgery. Lung Cancer. 2014;86:329–33.
Selek U, Bolukbasi Y, Welsh JW, Topkan E. Intensity-modulated radiotherapy versus 3-dimensional conformal radiotherapy strategies for locally advanced non-small-cell lung cancer. Balkan Med J. 2014;31:286–94.
de Baere T, Farouil G, Deschamps F. Lung cancer ablation: what is the evidence? Semin Interv Radiol. 2013;30:151–6.
Yilmaz S, Adas YG, Hicsonmez A, Andrieu MN, Akyurek S, Gokce SC. Evaluation of the radiation pneumonia development risk in lung cancer cases. Asian Pac J Cancer Prev. 2014;15:7371–5.
Wei Z, Ye X, Yang X, Zheng A, Huang G, Li W, et al. Microwave ablation in combination with chemotherapy for the treatment of advanced non-small cell lung cancer. Cardiovasc Intervent Radiol. 2015;38:135–42.
Carrafiello G, Mangini M, Fontana F, Ierardi AM, De Marchi G, Rotolo N, et al. Microwave ablation of lung tumours: single-centre preliminary experience. Radiol Med. 2014;119:75–82.
Belfiore G, Ronza F, Belfiore MP, Serao N, di Ronza G, Grassi R, et al. Patients’ survival in lung malignancies treated by microwave ablation: our experience on 56 patients. Eur J Radiol. 2013;82:177–81.
Sonntag PD, Hinshaw JL, Lubner MG, Brace CL, Lee FT, Jr. Thermal ablation of lung tumors. Surg Oncol Clin N Am. 2011; 20: 369–87, ix.
Brace CL, Hinshaw JL, Laeseke PF, Sampson LA, Lee FT Jr. Pulmonary thermal ablation: comparison of radiofrequency and microwave devices by using gross pathologic and CT findings in a swine model. Radiology. 2009;251:705–11.
Acksteiner C, Steinke K. Percutaneous microwave ablation for early-stage non-small cell lung cancer (NSCLC) in the elderly: a promising outlook. J Med Imaging Radiat Oncol. 2015;59:82–90.
Yang X, Ye X, Zheng A, Huang G, Ni X, Wang J, et al. Percutaneous microwave ablation of stage I medically inoperable non-small cell lung cancer: clinical evaluation of 47 cases. J Surg Oncol. 2014;110:758–63.
Liu H, Steinke K. High-powered percutaneous microwave ablation of stage I medically inoperable non-small cell lung cancer: a preliminary study. J Med Imaging Radiat Oncol. 2013;57:466–74.
Rami-Porta R, Crowley JJ, Goldstraw P. The revised TNM staging system for lung cancer. Ann Thorac Cardiovasc Surg. 2009;15:4–9.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the radiation therapy oncology group (RTOG) and the European organization for research and treatment of cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31:1341–6.
Albain KS, Swann RS, Rusch VW, Turrisi AT 3rd, Shepherd FA, Smith C, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet. 2009;374:379–86.
Zarogoulidis K, Zarogoulidis P, Darwiche K, Boutsikou E, Machairiotis N, Tsakiridis K, et al. Treatment of non-small cell lung cancer (NSCLC). J Thorac Dis. 2013;5(Suppl 4):S389–96.
Ghaye B. Percutaneous ablation of malignant thoracic tumors. JBR-Btr. 2013;96:142–54.
Roberton BJ, Liu D, Power M, Wan JM, Stuart S, Klass D, et al. Pulmonary ablation: a primer. Can Assoc Radiol J. 2014;65:177–85.
Sharma A, Abtin F, Shepard JA. Image-guided ablative therapies for lung cancer. Radiol Clin North Am. 2012;50:975–99.
Vogl TJ, Naguib NN, Gruber-Rouh T, Koitka K, Lehnert T, Nour-Eldin NE. Microwave ablation therapy: clinical utility in treatment of pulmonary metastases. Radiology. 2011;261:643–51.
Grieco CA, Simon CJ, Mayo-Smith WW, DiPetrillo TA, Ready NE, Dupuy DE. Percutaneous image-guided thermal ablation and radiation therapy: outcomes of combined treatment for 41 patients with inoperable stage I/II non-small-cell lung cancer. J Vasc Interv Radiol. 2006;17:1117–24.
Zheng A, Wang X, Yang X, Wang W, Huang G, Gai Y, et al. Major complications after lung microwave ablation: a single-center experience on 204 sessions. Ann Thorac Surg. 2014;98:243–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Xu, X., Ye, X., Liu, G. et al. Targeted percutaneous microwave ablation at the pulmonary lesion combined with mediastinal radiotherapy with or without concurrent chemotherapy in locally advanced non-small cell lung cancer evaluation in a randomized comparison study. Med Oncol 32, 227 (2015). https://doi.org/10.1007/s12032-015-0672-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-015-0672-1