Abstract
Patients with huge hepatocellular carcinoma >10 cm in diameter represent a special subgroup for treatment. To date, there are few data and little consensus on treatment strategies for huge hepatocellular carcinoma. In this study, we summarized the effects and safety of transarterial chemoembolization for huge hepatocellular carcinoma. A retrospective study was performed based on a large cohort of patients (n = 511) with huge hepatocellular carcinoma who underwent serial transarterial chemoembolization between January 2008 to December 2011 and were followed up until March 2013. We found median survival time was 6.5 months. On multivariate analysis, Child-Pugh class (A versus B) (p < 0.0001), alpha-fetoprotein (≤400 µg/L) (p = 0.002), Barcelona Clinic Liver Cancer stage (B versus C) (p = 0.013), and other treatments after transarterial chemoembolization such as surgical resection (p = 0.008), radiation (p = 0.018), and local radiofrequency ablation (p = 0.002) were factors significantly associated with better overall patient survival after chemoembolization. Twenty-nine percent of these patients showed a tumor response after serial transarterial chemoembolization. Severe complications were few (4.9 %), including oncolytic syndrome (n = 3), tumor rupture (n = 3), gastrointestinal bleeding (n = 4), deep venous thrombosis (n = 3), acute cholecystitis (n = 4), femoral artery pseudoaneurysm (n = 1), acute pancreatitis (n = 1), and acute hepatic failure (n = 6). In conclusion, transarterial chemoembolization is a safe and effective treatment for selected patients with huge hepatocellular carcinoma and is recommended as a component of combination therapy. In addition, patients with good liver function and low alpha-fetoprotein levels may acquire greater survival benefits from transarterial chemoembolization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most deadly malignancies worldwide [1]. Tumor size is predictive of the stage of HCC progression [2, 3] and is one of the main critical factors used to determine the choice of treatment [3]. Small HCC, particularly <3 cm, typically receive radical treatment, including hepatic resection, radiofrequency ablation, or liver transplantation. Most research and clinical trials have investigated early-stage HCC, particularly those with tumors <3 cm, or even <2 cm. However, for large HCC with diameters >5 cm, or even >10 cm, data are limited. In general, for huge HCC with diameter >10 cm, treatment consists of surgical resection. However, this modality is not ideal because huge HCC are typically unresectable [4, 5].
Huge HCC has unique traits that accompany the large volume. Pathophysiologically, the huge HCC has prominent necrosis and inflammation, and the membrane surrounding the tumor is always not complete. Meanwhile, the tumors are prone to invade into the local vasculature to become emboli, which increase the possibility of metastasis. Therefore, portal vein (PV) invasion and satellite foci are commonly found upon diagnosis [6, 7]. In addition, the huge HCC has an increased risk of rupture, which in turn can accelerate local spread and deterioration of liver function. If therapy is ineffective, prognosis is poor [8]. Therefore, the management of huge HCC remains a major medical challenge.
To date, transarterial chemoembolization (TACE) is still the main therapy for unresectable HCC [9]. However, for huge HCC with diameter >10 cm, serial TACE becomes a challenge because of the large tumor burden and increased possibility of complications. Ke et al. [10] reported a successful treatment protocol combining TACE and radiofrequency ablation (RFA) for huge HCC based on a small sample of patients (n = 9). Another study reported the effect of TACE for huge HCC based on a small patient sample (n = 31) [11]. Herein, we performed a large-scale (n = 511) retrospective cohort study and summarized the effects and safety of TACE for patients with huge HCC in our institute.
Materials and methods
Patients
This study sample was derived from patients (n = 1,806) who underwent serial TACE between January 2008 to March 2011 and whose data were contained within a prospectively maintained database at the Liver Cancer Institute, Zhongshan Hospital, Fudan University. A diagnosis of HCC was made on the basis of pathology or the diagnostic criteria of the American Association of the Study of Liver Disease on the radiological evaluation or biopsy. For patients without typical contrast “wash-in” and “wash-out” upon radiological examination, the biopsy was performed.
The main inclusion criteria for the present study included patients with single or multiple HCC >10 cm in the largest diameter. Patients were excluded if they had previous treatment before the first TACE. We also excluded patients with severe impairment of liver function (Child-Pugh C). Meanwhile, patients who had received only intra-arterial chemotherapy without embolization were excluded. All patients gave informed consent before undergoing TACE. Approval was obtained from the Zhongshan Hospital review board to perform this study.
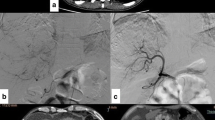
TACE procedure and follow-up
Superior mesenteric and celiac arteriography was performed initially to assess anatomy, tumor burden, and the tumor-feeding artery. The catheter was super-selectively inserted into the tumor-feeding artery. Chemotherapeutic agents such as 5-fluorouracil (1.0 g) and oxaliplatin (150 mg) were infused, and then an emulsion of 10 mg mitomycin C and 5–30 ml lipiodol was administrated (the amount of lipiodol chosen depended on tumor size and vasculature). For insufficient embolization with lipiodol in hypervascular tumors, gelatin sponge particles were used. After chemoembolization, patients were observed in case they experienced post-embolization syndrome (i.e., pain, nausea, and/or fever) or other adverse effects. Hydration, diuresis, and alkalinization of urine were performed for these patients post-TACE.
In our institute, tumor responses were mainly evaluated with regular computed tomography (CT) 1 month after TACE. For patients with residual disease, as shown by only partial lipiodol deposit in regular CT, or artery phase enhancement of contrast with dynamic enhanced CT or magnetic resonance imaging (MRI), TACE was repeated at an interval of 1.5–2.0 months. If the patients achieved complete tumor necrosis, follow-up with contrast-enhanced CT or MRI was performed, and alpha-fetoprotein (AFP) measurements were taken every 2–3 months. Treatment was terminated if a patient could not tolerate the procedure because of a decline in his/her clinical status or if a patient presented a complete response.
Measurements
The primary end point in this study was overall survival (OS). OS was defined as the time period between the first chemoembolization to the date of death regardless of reason for death. The second end point was objective response. Considering the short survival of patients with huge HCC, we evaluated the response 1 month after the second TACE in this study. Because part of patient cohort received only CT scan without enhancement during follow-up, we adopted the following strategy to consider the effect of necrosis in the evaluation: (1) For regular CT, we measured the longest diameter except the region with the lipiodol deposit. This method was based on the report of Okusaka et al. [12] whose research suggested good accordance between lipiodol imaging and pathology necrosis. (2) For contrast-enhanced CT/MRI, we evaluated the tumor response according to the modified response evaluation criteria in solid tumors (mRECIST) protocol [13].
For TACE-related complications, post-embolization syndrome consists of fever, abdominal pain, and a moderate degree of ileus. If the patient experienced high fever with chills, or elevated white blood cell counts and increased neutrophil/white blood cell ratio, the possibility of infection should be considered. TACE-related death was considered if the death occurred within 1 month post-TACE.
Statistical analyses
For survival analysis, patients lost to follow-up and patients who had not achieved a response at the end of this study were recognized as censored cases. Based on the definition of Barcelona Clinic Liver Cancer (BCLC) staging, in this study, we defined BCLC B stage where the tumor was >10 cm in diameter and without vessel invasion or metastasis. If the tumor concomitantly had PV invasion, multiple nodules, or remote metastasis, the tumor was classified as BCLC C stage. Cumulative survival curves were drawn according to the Kaplan–Meier method and were compared with the results of the log-rank test. Cox regression analysis was performed to assess the factors related to patient survival. Logistic regression analysis was used to identify the factors associated with tumor response. Stratification was used to control the potential confounders or effect modification in Cox and Logistic analyses. All p values were two-tailed, and the statistical significance was set at p < 0.05. Statistical analyses were performed using SPSS 18.0 software (SPSS Inc., Chicago, IL).
Results
Patients’ characteristics
Among 1,806 HCC patients potentially eligible for analysis, 511 (28.3 %) patients with huge HCC who met the aforementioned criteria were included in the study. The baseline characteristics of patients are summarized in Table 1. These patients had a median age of 53 (range 6–96) years. There were 450 male and 61 female patients, with a male–female ratio of 7:1. Most patients were hepatitis B surface antigen (HBsAg)-positive (79.3 %). There were 62.6 % (320 of 511) HCC patients classified as BCLC stage B and 37.4 % (191 of 511) patients classified as BCLC stage C. Of the 511 HCC patients, 478 (93.5 %) were of Child-Pugh stage A, and 33 were of (6.5 %) Child-Pugh stage B. The median tumor size was 12 cm (range 10–25 cm). One hundred and sixty-three patients (31.8 %) had PV invasion, and 48 patients (9.4 %) had metastasis based on image evaluation.
After chemoembolization, of the 511 patients, 18 underwent hepatic resection after TACE, and one patient underwent a partial pulmonary resection. Eighteen patients were treated with additional radiation therapy (RT). Twelve patients were treated with additional RFA, where nine patients underwent the procedure once, two patients twice, and one patient three times.
Overall survival
During the follow-up period (mean, 15.0 months), 390 patients died and 52 survived, with the median patient survival period of 6.5 months. Some of the patients (n = 69) were lost during follow-up. Patient survival rates were 33 % at 1 year, 13 % at 3 years, and 10 % at 5 years after chemoembolization (Fig. 1). During the follow-up period, 160 (31.3 %) died from tumor progression, 59 (11.5 %) died from hepatic encephalopathy, 24 (5.8 %) died from gastrointestinal hemorrhage, and 4 (0.8 %) died from rupture of the tumor.
Univariate analysis indicated that Child-Pugh classification, cirrhosis, AFP, γ-glutamyl transferase, PV invasion, metastasis, BCLC stage, and additional treatments including hepatic resection, radiation therapy, or RFA were potential prognostic factors for OS (Table 2). On multivariate analysis, Child-Pugh class A (p < 0.0001), AFP (≤400 µg/L) (p = 0.002), BCLC B stage (p = 0.013), surgical resection after chemoembolization (p = 0.008), RT after chemoembolization (p = 0.018), and RFA after chemoembolization (p = 0.002) were independent prognostic factors for better patient survival after confounder adjustment (Table 3). In addition, tumor response was closely correlated with patient survival (Fig. 2).
Comparison of the survival curves between tumor responses by Kaplan–Meier method. a Comparison between complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD). b Comparison between patients with tumor response (CR + PR) and patients with stable disease or without response (SD + PD)
Tumor response
Two hundred and thirty-two patients (44.6 %) who had available images were evaluated for tumor response. After chemoembolization, ten patients (4.3 %) showed a complete response and 57 patients (24.6 %) showed a partial response, for a tumor response rate of 28.9 % (67 of 232). Despite therapy, 78 patients (33.6 %) showed stable disease and 87 patients (37.5 %) showed progressive disease. Age and serum AFP levels were variables with a p value <0.20 on univariate analysis that were entered into the multiple logistic regression model (ESM_1, Online Resource 1). On multivariate analysis, age (odds ratio 3.813; p = 0.014) was a significant factor in determining tumor response (ESM_2, Online Resource 2). Relatively, younger patients had more than twice the risk of progression than older patients undergoing chemoembolization.
Complications
Severe chemoembolization-related complications occurred in 25 patients (4.9 %). Four patients experienced gastrointestinal bleeding after TACE. Acute hepatic failure occurred in six patients. Acute cholecystitis occurred in four patients. Three patients had tumor rupture; three patients had deep venous thrombosis; one patient experience acute pancreatitis; and three patients experienced tumor lysis syndrome after chemoembolization. Femoral artery pseudoaneurysm occurred in one patient, who received the vascular repair. The procedure-related mortality was 0.6 %.
Discussion
For HCC of large size, available treatment options are becoming fewer and more difficult [8]. When HCC progresses to huge tumor size, the corresponding local invasion, spread, and metastasis increase concurrently; meanwhile, the risk of complications such as rupture and gastrointestinal bleeding also increases. For unresectable HCC, TACE is still the main treatment choice [14]. For huge HCC, however, doctors should consider the balance between the potential survival benefits and the treatment-related complications. In this large cohort, TACE was shown to be a safe and effective treatment for selected patients with huge HCC. Prior to our study, one study reported combined TACE and RFA to treat huge HCC in nine patients, which showed positive outcomes [10]. In addition, a recent report compared the efficacy between surgery and TACE for huge HCC [15]. The survival rates of patients who received TACE in our study (33 % at 1 year, 13 % at 3 years, and 10 % at 5 years) were similar to this recent report (37.8 % at 1 year, 16.3 % at 3 years, and 9.7 % at 5 years) [15]. However, the inclusion criteria in our study were different from that report where patients with huge HCC with metastasis were excluded.
In this study, some patients received additional treatments, either surgery, radiotherapy, or local RFA, after chemoembolization. Results showed that all of these additional treatments improved the survival of patients, which indicated that the combined treatments based on TACE can add survival benefits for patients with huge HCC. Although the evidence for the effectiveness of TACE treatment for huge HCC is lacking, the efficiency of TACE for large HCC with diameter ≥5 cm had been shown previously, particularly when combined with other local treatments [16], such as percutaneous microwave coagulation therapy [17], percutaneous ethanol ablation [18], or radiotherapy [19, 20]. Generally, surgery, percutaneous ethanol ablation, or RFA may help to promote local control, whereas radiotherapy is potentially more suitable for control of PV invasion or local lymph node invasion. Similar to our results, a cohort study based on TACE for large HCC (diameter >5 cm) indicated that additional treatments improved patient survival [16].
In this study, we determined that some prognostic factors were closely correlated with survival, which could potentially be useful predictors for the efficacy of TACE treatment. First, liver function was one of the main critical factors to affect the survival of patients with huge HCC. Secondly, based on BCLC stage, patients with huge HCC in this study included two subgroups, stage BCLC B and stage BCLC C. According to the guidelines, TACE is the standard treatment for BCLC B patients. Meanwhile, accumulating evidence has suggested that chemoembolization provides benefits to select patients with BCLC C stage HCC [21, 22]. In this study, the results suggested that patients with BCLC B stage disease had better survival after undergoing repeated TACE. Part of reason was that PV invasion and metastasis in patients with BCLC C stage were the independent prognostic factors for survival in this study.
Generally, the doses of chemotherapeutic agents and lipiodol used in chemoembolization are relatively large, which potentially increase the occurrence of treatment-related complications. In our cohort, the severe complications mainly included rupture, oncolytic syndrome, and gastrointestinal bleeding. For preventing tumor lysis syndrome, we regularly performed hydration. This type of complication was low [23]; however, when it occurred, mortality was high. Gastrointestinal bleeding always occurred in patients with PV invasion, particularly with a main PV embolus. Our recent meta-analysis indicated that TACE was also safe for HCC with PV invasion for selected patients [24]. For rupture, to date, tumor size did not appear to be predictive [25].
Although this study was based on a large sample population, there were still limitations. First, since we performed a retrospective cohort study, bias was possible because of the non-random selection of patients. Second, for BCLC C stage, sorafenib is the standard treatment, and TACE is not; therefore, we were not able to compare the efficacy of TACE against the standard of care. However, a recent study indicated that combined TACE and sorafenib showed no further survival benefits than TACE alone [26]. Third, as an end point, we selected the tumor response after the second TACE treatment in our patients because of their relatively short survival; this group likely does not represent or account for the whole therapeutic control effect. Recently, an analysis based on the apparent diffusion coefficient changes at diffusion-weighted MRI showed that the 1-month response was an independent predictor of outcome of HCC patients undergoing TACE [27].
In summary, our findings suggest that TACE is suitable and safe for huge HCC and is particularly suitable for patients with good liver function and BCLC B stage. For selected patients with huge HCC, additional treatments including surgical resection, radiotherapy, or RFA are strongly recommended post-TACE.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Earl TM, Chapman WC. Tumor size remains key for prediction of hepatocellular carcinoma recurrence after liver transplantation. Ann Surg Oncol. 2011;18:1217–8.
Kim SJ, Lee KK, Kim DG. Tumor size predicts the biological behavior and influence of operative modalities in hepatocellular carcinoma. Hepatogastroenterology. 2010;57:121–6.
Jin YJ, Lee JW, Choi YJ, Chung HJ, Kim YS, Lee KY et al. Surgery versus transarterial chemoembolization for solitary large hepatocellular carcinoma of BCLC stage A. J Gastrointest Surg. 2014;18:555–61.
Liang HY, Lu LG, Hu BS, Li Y, Shao PJ. Effects of sorafenib combined with chemoembolization and radiofrequency ablation for large, unresectable hepatocellular carcinomas. Chin Med J (Engl). 2013;126:4270–6.
Ariizumi S, Kotera Y, Takahashi Y, Katagiri S, Yamamoto M. Impact of hepatectomy for huge solitary hepatocellular carcinoma. J Surg Oncol. 2013;107:408–13.
Yamashita Y, Taketomi A, Shirabe K, Aishima S, Tsuijita E, Morita K, et al. Outcomes of hepatic resection for huge hepatocellular carcinoma (>/=10 cm in diameter). J Surg Oncol. 2011;104:292–8.
Poon RT, Fan ST, Wong J. Selection criteria for hepatic resection in patients with large hepatocellular carcinoma larger than 10 cm in diameter. J Am Coll Surg. 2002;194:592–602.
Lencioni R. Chemoembolization in patients with hepatocellular carcinoma. Liver Cancer. 2012;1:41–50.
Ke S, Ding X, Gao J, Gao K, Qian X, Cao B, et al. Solitary huge hepatocellular carcinomas 10 cm or larger may be completely ablated by repeated radiofrequency ablation combined with chemoembolization: initial experience with nine patients. Mol Med Rep. 2012;5:832–6.
Huang YH, Wu JC, Chen SC, Chen CH, Chiang JH, Huo TI, et al. Survival benefit of transcatheter arterial chemoembolization in patients with hepatocellular carcinoma larger than 10 cm in diameter. Aliment Pharmacol Ther. 2006;23:129–35.
Okusaka T, Okada S, Ueno H, Ikeda M, Yoshimori M, Shimada K, et al. Evaluation of the therapeutic effect of transcatheter arterial embolization for hepatocellular carcinoma. Oncology. 2000;58:293–9.
Lencioni R. New data supporting modified recist (mRECIST) for hepatocellular carcinoma. Clin Cancer Res. 2013;19:1312–4.
Lencioni R. Chemoembolization for hepatocellular carcinoma. Semin Oncol. 2012;39:503–9.
Min YW, Lee JH, Gwak GY, Paik YH, Rhee PL, Koh KC, et al. Long-term survival after surgical resection for huge hepatocellular carcinoma: comparison with transarterial chemoembolization after propensity score matching. J Gastroenterol Hepatol. 2014;29:1043–8.
Yoon HM, Kim JH, Kim EJ, Gwon DI, Ko GY, Ko HK. Modified cisplatin-based transcatheter arterial chemoembolization for large hepatocellular carcinoma: multivariate analysis of predictive factors for tumor response and survival in a 163-patient cohort. J Vasc Interv Radiol. 2013;24:1639–46.
Xu LF, Sun HL, Chen YT, Ni JY, Chen D, Luo JH, et al. Large primary hepatocellular carcinoma: transarterial chemoembolization monotherapy versus combined transarterial chemoembolization-percutaneous microwave coagulation therapy. J Gastroenterol Hepatol. 2013;28:456–63.
Gao F, Gu YK, Fan WJ, Zhang L, Huang JH. Evaluation of transarterial chemoembolization combined with percutaneous ethanol ablation for large hepatocellular carcinoma. World J Gastroenterol. 2011;17:3145–50.
Yasuda S, Ito H, Yoshikawa M, Shinozaki M, Goto N, Fujimoto H, et al. Radiotherapy for large hepatocellular carcinoma combined with transcatheter arterial embolization and percutaneous ethanol injection therapy. Int J Oncol. 1999;15:467–73.
Cho JY, Paik YH, Park HC, Yu JI, Sohn W, Gwak GY, et al. The feasibility of combined transcatheter arterial chemoembolization and radiotherapy for advanced hepatocellular carcinoma. Liver Int. 2014;34:795–801.
Pinter M, Hucke F, Graziadei I, Vogel W, Maieron A, Konigsberg R, et al. Advanced-stage hepatocellular carcinoma: transarterial chemoembolization versus sorafenib. Radiology. 2012;263:590–9.
Prajapati HJ, Dhanasekaran R, El-Rayes BF, Kauh JS, Maithel SK, Chen Z, et al. Safety and efficacy of doxorubicin drug-eluting bead transarterial chemoembolization in patients with advanced hepatocellular carcinoma. J Vasc Interv Radiol. 2013;24:307–15.
Hsieh PM, Hung KC, Chen YS. Tumor lysis syndrome after transarterial chemoembolization of hepatocellular carcinoma: case reports and literature review. World J Gastroenterol. 2009;15:4726–8.
Xue TC, Xie XY, Zhang L, Yin X, Zhang BH, Ren ZG. Transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus: a meta-analysis. BMC Gastroenterol. 2013;13:60.
Aoki T, Kokudo N, Matsuyama Y, Izumi N, Ichida T, Kudo M, et al. Prognostic impact of spontaneous tumor rupture in patients with hepatocellular carcinoma: an analysis of 1160 cases from a nationwide survey. Ann Surg. 2014;259:532–42.
Choi GH, Shim JH, Kim MJ, Ryu MH, Ryoo BY, Kang YK, et al. Sorafenib alone versus sorafenib combined with transarterial chemoembolization for advanced-stage hepatocellular carcinoma: results of propensity score analyses. Radiology. 2013;269:603–11.
Vandecaveye V, Michielsen K, De Keyzer F, Laleman W, Komuta M, Op de Beeck K et al. Chemoembolization for hepatocellular carcinoma: 1 month response determined with apparent diffusion coefficient is an independent predictor of outcome. Radiology. 2014;270:747–57.
Acknowledgments
This study was supported by the National Clinical Key Special Subject of China, the National Natural Science Foundation of China (81172275 and 21272565), and the National Basic Research Program of China (973 Program, 2009CB521700).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Tongchun Xue and Fan Le have contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xue, T., Le, F., Chen, R. et al. Transarterial chemoembolization for huge hepatocellular carcinoma with diameter over ten centimeters: a large cohort study. Med Oncol 32, 64 (2015). https://doi.org/10.1007/s12032-015-0504-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-015-0504-3