Abstract
MMI-166 is a third-generation selective matrix metalloproteinase (MMP) inhibitor that prevents tumor invasion and metastasis by downregulating the activity of MMP-2 and MMP-9. However, MMI-166’s effect in pancreatic cancer cells has not been widely studied. Initially, we treated SW1990, human pancreatic cancer cells, with 0, 50 or 100 μg/ml of MMI-166 for 24 h. Apoptosis in the cells was then observed by inverted fluorescence microscope and flow cytometry; the apoptosis rate was dependent on MMI-166 concentration. We then injected nude mice with SW1990 cells. Volume of the resulting xenograft tumors in nude mice treated with MMI-166 was far less than that of the control group, whereas their apoptotic index was much greater. Expression of MMP-2, MMP-9, c-myc and survivin were markedly lower in tumors from the treated mice than in the control group. In cell experiments, MMP-2 and MMP-9 activities were downregulated by MMI-166 compared with controls, as were both mRNA and protein levels of MMP-2, MMP-9 and c-myc, although survivin expression did not differ. These results show that MMI-166 can induce apoptosis of pancreatic cancer cells in vitro and in vivo. The mechanism may be related to downregulation of c-myc by MMI-166.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of pancreatic cancer has increased globally year by year, and unless discovered at an early stage, has a very poor prognosis.
Matrix metalloproteinase (MMP) inhibitors are used to treat pancreatic cancer by inhibiting the activity of MMPs. As the first and second generations of MMP inhibitors had obvious side effects, a focus of research in this area was to find a high-efficient and low-toxic [1] MMPs inhibitor. MMI-166 is a third-generation MMP inhibitor, more selective than its predecessors, which can inhibit tumor invasion and metastasis by downregulating the activity of MMP-2 and MMP-9 [2]. MMI-166 has reportedly shown anti-invasion, anti-metastasis and anti-angiogenesis functions among animal models of lung cancer, colorectal cancer, pancreatic cancer, malignant glioma tumor and head and neck squamous cell carcinoma [1, 3–8]. Also, MMI-166 has been shown to inhibit the invasion ability of cervical cancer cells [9], malignant glioma cells and head and neck squamous cancer cells in vitro. However, whether MMI-166 could induce apoptosis in pancreatic cancer cells has not been widely studied. We observed the effect of MMI-166 on apoptosis of human pancreatic cancer cells SW1990, using fluorescence and flow cytometry, and expression of MMP-2, MMP-9, apoptosis-related proteins and apoptosis in a xenograft nude mouse model. We then explored dose–effect relationships between MMI-166 and activities of MMP-2 and MMP-9 and mRNA and protein expressions of MMP-2, MMP-9, c-myc and survivin, thus providing data to investigate resistance of pancreatic cancer for MMI-166.
Materials and methods
Cell morphology
We purchased SW1990 cells from the Shanghai Cell Bank of the Chinese Science Academy and cultured them in L-15 medium with 10 % fetal bovine serum. Cells were cultured to logarithmic phase in serum-free L-15 medium and inoculated into 24-well plates (5 × 104/well). When cells adhered, they were treated with 0, 50 or 100 μg/ml of MMI-166 (kindly donated by the Shionogi & Company, Ltd, Osaka, Japan) for 24 h. Cell morphology was viewed in an inverted-phase contrast microscope after cells were cultured for 24 h.
Apoptosis analysis by fluorescence and flow cytometry
Cells from the previous step were collected to form single cell suspensions by reaction buffer at the density of 1 × 105/ml. We added 10 μl Annexin V and 2 μl PI into 200-μl cell suspensions and incubated the samples for 15 min away from light at room temperature. Half of each mixture was stained into green by Annexin V and red by PI and observed under a fluorescence microscope. We selected five fields at 200× magnification of each concentration randomly and counted the apoptotic cells in each field. The least was added 400 μl buffer reaction and then oscillated gently for flow cytometry test of apoptotic rate.
Establishing human pancreatic cancer xenograft model
We purchased 20 male BALB/c nude mice from the Shanghai Laboratory Animal Center; they were 4–5 weeks old, weighed 18–22 g and were raised in a specific pathogen-free environment. We inoculated the back of each mouse subcutaneously with SW1990 cells in logarithmic phase, cultured in serum-free L-15 medium, at 1 × 107 per mouse. Seven days later, when the xenograft tumors had all formed, the mice were divided into control and experimental groups (n = 10 for both groups). The experimental groups were orally administered MMI-166 (200 mg/kg daily), and control groups were orally administered the same vehicle (saline containing 0.5 % carboxymethylcellulose-Na, 0.9 % benzyl alcohol, and 0.4 % Tween 80). Tumor volumes were measured by vernier caliper through long and short axes every 7 days. Mice were euthanized after 28 days, and their tumors were excised. Tumor volume was calculated as a × b 2 × π/6, where a and b are the long and short axes, respectively. Tumors were then fixed with 10 % neutral formalin, embedded in paraffin and sliced serially for TUNEL and immunohistochemical staining.
TUNEL
Sections were deparaffinized and dehydrated, and digested by Proteinase K solution (20 mg/l) at room temperature. Apoptotic cells were detected by TUNEL (Roche, Germany). Apoptotic cells, which had dark brown stained nuclei, were counted in five randomly selected fields at 400× magnification, using an inverted-phase contrast microscope. The average percentage of cells that were apoptotic was the apoptotic index (AI).
Immunohistochemistry
Immunohistochemical staining was used to detect MMP-2, MMP-9, p53, c-myc, bax, bcl-2, survivin, caspase-1 and fas. Primary antibodies to MMP-2 and MMP-9 were rabbit and rat antihuman polyclonal, respectively (Beijing Bioss Biological Technology Company). Primary antibodies to p53, c-myc, bax, bcl-2, were rat antihuman monoclonal and survivin, caspase-1 and fas were rabbit antihuman polyclonal which all came from Fuzhou Maxin Company; secondary antibodies were bought from Dako. Each antibody was tested three times and averaged, viewing ten fields at 100× magnification for positive cells. Integrated optical density (IOD) was calculated with Image-pro Plus 6.0 software.
Gelatin zymography
Activities of MMP-2 and MMP-9 from SW1990 cells were detected by gelatin zymography. Briefly, cells at logarithmic growth phase were inoculated into 6-well plates (5 × 105/ml) and cultured in serum-free L-15 medium with 0, 50 or 100 μg/m of MMI-166 for 24 h. Culture media were collected and centrifuged at 188×g for 5 min. Protein in culture media were quantified with bicinchoninic acid protein assay kits (Beyotime Institute of Biotechnology, China). We mixed 20-μg samples with 5 × sodium dodecyl sulfate (SDS) buffer and electrophoresed them in 10 % SDS-PAGE systems with 1 % gelatin. Gels were rinsed with eluent and detection buffer and then put in incubation liquid at 37 °C for 24 h. The eluent was subjected to constant mechanical stirring in 200 ml of 2.5 % Triton X-100. Detection buffers were buffer A (0.1 M glycine-NAOH) and optimized buffer B (50 mm Tris–HCL, 0.2 M NaCl, 5 mM CaCl2). Gels were then stained with Coomassie brilliant blue (Beyotime) and photographed with a gel imaging analyzer; images were analyzed with Image J software.
Reverse transcription-polymerase chain reaction (RT-PCR)
The mRNA expression of MMP-2, MMP-9, c-myc and survivin of SW1990 cells treated with MMI-166 was tested by RT-PCR. Briefly, total RNA was extracted by Trizol (Sigma, USA), and target genes were amplified with a RT-PCR kit (Takara). We electrophoresed 5-μl samples of PCR products in 3 % agarose gel systems containing ethidium bromide; results were analyzed with Image J software and standardized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH). Primers and amplification parameters were: (1) MMP-2 forward (F): 5′-GATACCCCTTTGACGGTAAGGA-3′, reverse (R):5′-CCTTCTCCCAAGGTCCATAGC-3′; MMP-9 F:5′-CAACTACGACACCGACGA-3′, R:5′-GCCTTGGAAGATGAATGGAA-3′; GAPDH F:5′-AGAAGGCTGGGGCTCATTTG-3′, R:5′-AGGGGCCATCCACAGTCTTC-3′; PCR conditions (for MMP-2 and MMP-9): 5 min at 95 °C, 40 cycles (94 °C for 30 s; 58 °C for 30 s; 72 °C for 1 min), 10 min at 72 °C, storage at 4 °C. (2) survivin F:5′-CACCGCATCTCTACATTCAAG-3′ and R:5′-GAAGCAGCCACTGTTACCAG-3′; PCR conditions: 2 min at 94 °C, 30 cycles (94 °C for 45 s; 55 °C for 45 s; 72 °C for 45 s), 5 min at 72 °C, storage at 4 °C. (3) c-myc F:5′-TCCAGCTTGTACCTGCAGGATCTGA-3′, R:5′-CCTCCAGCAGAAGGTGATCCAGACT-3′; PCR conditions: 12 min at 95 °C, 30 cycles (95 °C for 1 min; 65 °C for 1 min; 72 °C for 1 min), 10 min at 72 °C and storage at 4 °C.
Western blot
Expression of MMP-2, MMP-9, c-myc and survivin proteins was detected by Western blot. Cells in serum-free L-15 medium were treated with 0, 50 or 100 μg/ml of MMI-166 for 24 h. Cells were harvested and washed twice with phosphate buffer saline and then incubated with radioimmunoprecipitation assay cell lysis liquid (RIPA, Beyotime) on ice for 30 min. The supernatants were collected and centrifuged at 12,000×g, 4 °C, for 10 min). The secreted protein was obtained from culture supernatants which were concentrated by using Microcon centrifugal filters (30-kDa Amicon Ultra, Millipore, USA). After quantifying the proteins, equal amounts of MMP-2, MMP-9, c-myc and survivin protein was separated using 6, 6, 10 and 12 % SDS-PAGE, respectively, with a Mini Protein System (Bio-Rad, France), and then transferred to polyvinylidene difluoride (PVDF) membranes. The membranes, after being blocked with blocking buffer (Beyotime), were incubated with primary antibodies (MMP-2, MMP-9 and c-myc—mouse monoclonal antibody; survivin—rabbit polyclonal antibody; 1:500 for all, Santa Cruz Biotechnology, Santa Cruz, CA, USA). After washing with TBST, membranes were incubated with goat anti-mouse (MMP-2, MMP-9 and c-myc) or anti-rabbit (survivin) secondary antibodies (1:1,000, Beyotime), respectively, and photographed by a gel imaging analyzer (Image J software). GAPDH was used as an internal reference.
Statistical analysis
Data are presented as mean ± SE. Data were first subjected to normality and homogeneity tests of variance; groups were then compared using ANOVA. Correlation of MMP-2, MMP-9, c-myc and survivin to apoptosis was analyzed with Pearson coefficient test. Student’s t test was used for statistical analysis; P < 0.05 was considered significant.
Results
MMI-166-treated cells showed morphological changes
The MMI-166-treated groups had significantly fewer cells, and the cells were smaller with poor refraction and contracted cell membranes; some cells floated in the culture. In contrast, the control group was well grown (Fig. 1A).
MMI-166 induces SW1990 cells apoptosis in vitro and vivo. Letters a, b and c indicate cells treated with 0, 50 and 100 μg/ml of MMI-166, respectively. A Morphological changes of SW1990 cells after MMI-166 treatment were observed under inverted-phase contrast microscope. B Apoptotic cells stained by Annexin V-PI were counted under inverted fluorescence microscope. C Representative results of apoptotic cells stained by Annexin V-PI. D Apoptosis was also analyzed by the Annexin V-FITC Apoptosis Detection Kit; apoptotic rate was tested by flow cytometry. E Representative dot-plots from flow cytometry illustrate apoptotic status in SW1990 cells. Data represent mean values ± SE *P < 0.05; **P < 0.01
MMI-166 induces apoptosis in vitro
Normal living cells were not stained, or only lightly stained, by both Annexin V and PI. Early apoptotic cells were deeply stained by Annexin V but not PI, whereas late apoptotic cells were deeply stained by both Annexin V and PI (showing red and green fluorescence). After treatment with 0, 50 or 100 μg/m of MMI-166 for 24 h, numbers of apoptotic cells were 17.0 ± 5.431, 72.4 ± 10.455 and 149.4 ± 11.127, respectively and differed significantly by dose (F = 252.551, P = 0.000; Fig. 1B, C) Apoptotic rates (which includes sums of late and early apoptotic rates) were detected by flow cytometry (Fig. 1E). Results were 8.880 ± 0.864 %, 16.333 ± 0.838 % and 20.990 ± 0.691 %, respectively, which also differed significantly by dose (F = 58.110, P < 0.001; Fig. 1D). These results show that apoptotic SW1990 cells increase as MMI-166 concentration rises, which indicates that MMI-166 can induce apoptosis in vitro.
MMI-166 inhibits growth of SW1990 xenografts in a nude mouse model
We successfully established a xenograft model of human pancreatic cancer in nude mice. Differences in tumor volume between the control and experimental groups were not significant before taking MMI-166 (P = 0.495) or during the first week of treatment P = 0.444; Fig. 2A), but varied significantly in the second, third and fourth weeks (P = 9.03 × 10−6, P = 1.42 × 10−6, P = 2.92 × 10−7, respectively). Control group tumors were much bigger than in the experimental group, which suggest that MMI-166 inhibits growth of pancreatic cancer in vivo.
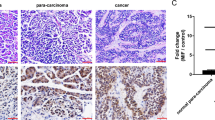
MMI-166 inhibits growth of human pancreatic cancer xenograft model of SW1990, induces apoptosis in vivo and downregulates expression of MMP-2, MMP-9, c-myc and survivin in a nude mice xenograft model. A Tumor volume of nude mice was measured by vernier caliper every 7 days. B Apoptosis index of human pancreatic cancer xenografts treated by MMI-166 was detected by TUNEL. C Representative results of TUNEL (a) and of immunohistochemical staining of MMP-2 (b), MMP-9 (c), c-myc (d), survivin (e), p53 (f), fas (g), bax (h), bcl-2 (i) and caspase-1 (j) (1: control group; 2: experimental group.) D IOD values of MMP-2, MMP-9, c-myc, survivin, p53, fas, bax, bcl-2 and caspase-1. MMI-166 could downregulate expression of MMP-2, MMP-9, c-myc and survivin in a xenograft model. Data represent mean values ± SE. *P < 0.05; **P < 0.01
MMI-166 induces apoptosis in vivo
Nuclei of apoptotic cells appeared dark brown through microscopic observation and showed typical apoptotic features, such as condensed, divided and/or marginalized chromatin, cracked nuclear membranes, etc. Apoptotic cells were scattered singly or in clusters. The AI of the experimental groups were significantly higher than for the control group (Fig. 2C). Differences were statistically significant (P = 0.000) and demonstrates that MMI-166 can induce apoptosis in vivo in these cells (Fig. 2B).
Effects of MMI-166 on expression of MMP-2, MMP-9, P53, c-myc, bax, bcl-2, survivin, caspase-1 and fas in nude mice xenografts
MMP-2, MMP-9, bax, bcl-2, survivin and caspase-1 are located in cytoplasm; p53 in the nucleus; fas in the cell membrane; and c-myc in both nucleus and cytoplasm. Expressions of MMP-2, MMP-9, c-myc and survivin in the experimental groups were significantly lower than the control group (P = 1.83 × 10−6; P = 1.52 × 10−5; P = 2.14 × 10−5; P = 1.42 × 10−4; Fig. 2C). However, the groups did not significantly differ in expressions of p53, bax, bcl-2, caspase-1 and fas (P = 0.943, P = 0.457, P = 0.834, P = 0.526 and P = 0.238, respectively). Expression of MMP-2 (r = −0.995, P = 3.14 × 10−5), MMP-9 (r = −0.995, P = 3.14 × 10−5), c-myc (r = −0.987, P = 2.52 × 10−4) and survivin (r = −0.988, P = 1.97 × 10−4) was inversely correlated with apoptosis in xenograft tissues (Fig. 2D). These results indicate that apoptosis increases in SW1990 cells, expressions of MMP-2, MMP-9, c-myc and survivin decrease.
MMI-166 inhibits activities of MMP-2 and MMP-9
The influence of MMI-166 on MMP-2 and MMP-9 activities in cells treated with 0, 50 or 100 μg/ml of MMI-166 for 24 h was detected by gelatin zymography (Fig. 3B). Relative activity of MMP-2 in the three dose groups (0.412 ± 0.044, 0.287 ± 0.018 and 0.181 ± 0.017, respectively) differed significantly (F = 46.95, P = 2.17 × 10−4), as did that of MMP-9 (F = 138.446, P = 9.54 × 10−6; 0.898 ± 0.049, 0.623 ± 0.049, 0.308 ± 0.0286, respectively, Fig. 3A).
MMI-166 inhibits activities of MMP-2 and MMP-9 and downregulates mRNA and protein expressions of MMP-2, MMP-9 and c-myc. A Gelatin zymography was used to detect relative activities of MMP-2 and MMP-9. B Representative results of gelatin zymography. C Relative mRNA expressions of MMP-2, MMP-9, c-myc and survivin were detected by RT-PCR. GAPDH was used as internal control. D Representative figures and relative expression levels were analyzed by Image J software. E Western blotting analysis. Total extracts were prepared and subjected to western blot analysis to monitor expressions of MMP-2, MMP-9, c-myc and survivin. GAPDH was used as protein loading control. F Representative figures and relative expression levels were analyzed by Image J software
MMI-166 downregulates mRNA expression of MMP-2, MMP-9 and c-myc
After treatment with 0, 50 or 100 μg/ml of MMI-166 for 24 h, relative mRNA expression of MMP-2 significantly differed according to the three dose groups (F = 266.208, P = 1.38 × 10−6; 1.159 ± 0.052, 0.918 ± 0.019 and 0.55 ± 0.013, respectively); as did MMP-9 (F = 80.914, P = 4.57 × 10−5; 1.076 ± 0.026, 0.791 ± 0.077 and 0.59 ± 0.005, respectively); and c-myc (F = 70.761, P = 6.73 × 10−5; 0.669 ± 0.052, 0.507 ± 0.005 and 0.326 ± 0.031, respectively). However, relative mRNA expressions of survivin did not significantly vary (F = 4.479, P = 0.065; 0.346 ± 0.015, 0.367 ± 0.009 and 0.377 ± 0.015, respectively) (Fig. 3C, D).
MMI-166 downregulates protein expression of MMP-2, MMP-9 and c-myc
After treatment with 0, 50 or 100 μg/m of MMI-166 for 24 h, relative protein expressions of MMP-2 significantly varied in the three dose groups (F = 228.345, P = 2.18 × 10−6; 1.069 ± 0.016, 0.737 ± 0.049 and 0.545 ± 0.012, respectively); as did MMP-9 (F = 182.593, P = 4.22 × 10−6; 0.95 ± 0.025, 0.632 ± 0.043 and 0.425 ± 0.031, respectively); and c-myc (F = 451.102, P = 2.88 × 10−7; 1.367 ± 0.045, 0.56 ± 0.05 and 0.257 ± 0.045). However, relative protein expression of survivin did not significantly vary (F = 1.193, P = 0.366; 0.443 ± 0.072, 0.403 ± 0.081 and 0.487 ± 0.035, respectively) (Fig. 3E, F).
Discussion
For nearly half a century, the incidence of pancreatic cancer has risen steadily worldwide, although its prognosis has remained very poor, except for the relatively few cases discovered at early stages. The effect of pure surgical treatment on pancreatic cancer is very limited; however, current first-line chemotherapy drugs for pancreatic cancer are hindered by drug resistance [10]. Therefore, new effective treatments are desperately needed to improve the survival rates of patients with pancreatic cancer.
Matrix metalloproteinases are zinc-dependent secreted proteinases that can promote tumor cell invasion and metastasis and formation of new blood vessels in tumor tissues by degrading the extracellular matrix and basement membranes that help regulate intercellular adhesion. MMPs inhibitors can restrain MMP activity to block tumor invasion, metastasis and growth. The phase III trial of marimastat, a first-generation MMP inhibitor, found that when combined with gemcitabine its curative effect was not better than gemcitabine alone [11], and it could lead to adverse reactions such as inflammatory arthritis. The second-generation MMP inhibitor BAY12-9566 showed better tumor inhibition and less adverse reactions in initial and phase I testing, but gave significantly shorter progression-free survival and median survival than did single-agent gemcitabine and was abandoned during its phase II trial [12]. MMI-166, which selectively inhibits activities of MMP-2 and 9, is a third-generation MMP inhibitor [2] that reportedly decreases invasion, metastasis and growth of a variety of malignant tumor cells, including gastric cancer, lung cancer, colon cancer, head and neck squamous cell carcinoma and glioma [7, 8, 13].
Gelatin zymography, Western blot and RT-PCR, as used in our experiments, all showed MMI-166 to inhibit both activity and expression of MMP-2/9, in a dose-dependent manner in vitro. Expression of MMP-2/9 in cytoplasm of experimental groups was obviously lower than in controls. This study shows that MMI-166 inhibits expression of MMP-2/9 in pancreatic cancer tissues. MMP-2 and MMP-9 are MMP gelatin enzymes and can enhance tumor metastasis to surrounding and remote tissues by promoting extracellular matrix degradation and allowing tumors to break through the substrate membrane and extracellular matrix, thus affecting tumor invasion and metastasis.
Through fluorescence, we observed greater apoptosis in cells treated with MMI-166 in vitro. After that, we found apoptotic rate to increase dose dependently with MMI-166. We then analyzed apoptosis using xenografts in a nude mouse model by TUNEL. We found that AI of MMI-166-treated group was higher than that of controls. All the above experiments show that MMI-166 could promote apoptosis both in vitro and vivo. Pearson coefficient analyses showed that MMP-2 and MMP-9 are inversely correlated with apoptosis. As far as we know, many genes affect apoptosis regulation, including some genes related to cell proliferation and apoptosis such as p53, c-myc, bax, bcl-2, survivin, caspase-1, fas etc. Our experiment shows that expression of both c-myc and survivin in the MMI-166-treated groups is lower than in the control group. Reportedly, c-myc is a kind of intracellular “early rapid response” messenger and can induce cells into the cell cycle to promote proliferation when stimulated by some growth factors [14]. Li et al. [15] found that expression of c-myc in primary and metastatic pancreatic cancer tissue was obviously higher than pancreatic benign lesion tissue. Orian et al. [16] studied 62 cases of brain astrocytoma and found that protein expression rates for c-myc in low, medium and highly malignant tumor tissue varied significantly at 5, 33 and 76 %; they considered that the high c-myc expression indicates a high percentage of cells are in proliferation state. Apoptotic inhibition is an important indicator of tumor progression. Survivin is a member of the inhibitor of apoptosis protein family. Sarela et al. [17] reported positive survivin expression in 88 % of 52 cases. The apoptosis index is low when Survivin is positive; patients with low apoptosis indices have worse prognoses than those with high apoptosis indices. Thus, we speculated that increased apoptosis may be associated with decreased c-myc and survivin expression. Our in vitro experiments show c-myc expression in SW1990 cells was downregulated, whereas survivin expression showed no obvious change after treatment by MMI-166 for 24 h. We thus infer that the effect of MMI-166 on promoting apoptosis of pancreatic cancer is related to downregulated c-myc expression. Although survivin expression showed no obvious change, we could not eliminate the effects of sample size and protein concentration. The effect of MMI-166 on survivin expression should be further studied. Meyer et al. [18] reported that MMP-9 and MMP-10 could protect colon adenocarcinoma cells from apoptosis induced by PKC/p53. Chetty et al. [19] considered that MMP-2 could inhibit apoptosis by lung adenocarcinoma cancer cell through changes in bax/bcl-2 expression, inducing formation of Caspase-3, 8, 9 and PARP-1 and activation of fas/fasL.
In conclusion, we infer that MMI-166 promotes apoptosis of pancreatic cancer cells by inhibiting activities of MMP-2 and MMP-9 [2] to downregulate the c-myc pathway. However, the specific mechanism requires further study.
References
Maekawa R, Maki H, Wada T, Yoshida H, Nishida-Nishimoto K, Okamoto H, et al. Anti-metastatic efficacy and safety of MMI-166, a selective matrix metalloproteinase inhibitor. Clin Exp Metastasis. 2000;18(1):61–6.
Tamura Y, Watanabe F, Nakatani T, Yasui K, Fuji M, Komurasaki T, et al. Highly selective and orally active inhibitors of type IV collagenase (MMP-9 and MMP-2): N-sulfonylamino acid derivatives. J Med Chem. 1998;41:640–9.
Fujino H, Kondo K, Ishikura H, Maki H, Kinoshita H, Miyoshi T, et al. Matrix metalloproteinase inhibitor MMI-166 inhibits lymphogenous metastasis in an orthotopically implanted model of lung cancer. Mol Cancer Ther. 2005;4(9):1409–16.
Ohta M, Konno H, Tanaka T, Baba M, Kamiya K, Oba K, et al. Effect of combination therapy with matrix metalloproteinase inhibitor MMI-166 and mitomycin C on the growth and liver metastasis of human colon cancer. Jpn J Cancer Res. 2001;92(6):688–95.
Oba K, Konno H, Tanaka T, Baba M, Kamiya K, Ohta M, et al. Prevention of liver metastasis of human colon cancer by selective matrix metalloproteinase inhibitor MMI-166. Cancer Lett. 2002;175(1):45–51.
Matsushita A, Onda M, Uchida E, Maekawa R, Yoshioka T. Antitumor effect of a new selective matrix metalloproteinase inhibitor, MMI-166, on experimental pancreatic cancer. Int J Cancer. 2001;92(3):434–40.
Nakabayashi H, Yawata T, Shimizu K. Anti-invasive and antiangiogenic effects of MMI-166 on malignant glioma cells. BMC Cancer. 2010;10:339.
Katori H, Baba Y, Imagawa Y, Nishimura G, Kagesato Y, Takagi E, et al. Reduction of in vivo tumor growth by MMI-166, a selective matrix metalloproteinase inhibitor, through inhibition of tumor angiogenesis in squamous cell carcinoma cell lines of head and neck. Cancer Lett. 2002;178(2):151–9.
Iwasaki M, Nishikawa A, Fujimoto T, Akutagawa N, Manase K, Endo T, et al. Anti-invasive effect of MMI-166, a new selective matrix metalloproteinase inhibitor, in cervical carcinoma cell lines. Gynecol Oncol. 2002;85(1):103–7.
Fazal S, Saif MW. Supportive and palliative care of pancreatic cancer. JOP. 2007;8(2):240–53.
Bramhall SR, Rosemurgy A, Brown PD, Bowry C, Buckels JA, Marimastat Pancreatic Cancer Study Group. Marimastat as first-line therapy for patients with unresectable pancreatic cancer: a randomized trial. J Clin Oncol. 2001;19(15):3447–55.
Moore MJ, Hamm J, Dancey J, Eisenberg PD, Dagenais M, Fields A, et al. Comparison of gemcitabine versus the matrix metalloproteinase inhibitor BAY 12-9566 in patients with advanced or metastatic adenocarcinoma of the pancreas: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2003;21(17):3296–302.
Maki H, Hojo K, Tanaka H, Sawada TY, Maekawa R, Yoshioka T, et al. Augmented anti-metastatic efficacy of a selective matrix metalloproteinase inhibitor, MMI-166, in combination with CPT-11. Clin Exp Metastasis. 2002;19(6):519–26.
Dang CV, Resar LM, Emison E, Kim S, Li Q, Prescott JE, et al. Function of the c-myc oncogenic transcription factor. Exp Cell Res. 1999;253(1):63–77.
Li S, Shi XT, Zhang X, Zhang Y, Yi LH. The relationship between bcl-2, apoptosis and c-myc in pancreatic cancer. J Hepatopancreatobiliary Surg. 2001;13(4):204–7.
Orian JM, Vasilopoulos K, Yoshida S, Kaye AH, Chow CW, Gonzales MF, et al. Overexpression of multiple oncogenes related to histological grade of astrocytic glioma. Br J Cancer. 1992;66(1):106–12.
Sarela AI, Verbeke CS, Ramsdale J, Davies CL, Markham AF, Guillou PJ. Expression of survivin, a novel inhibitor of apoptosis and cell cycle regulatory protein in pancreatic adenocarcinoma. Br J Cancer. 2002;86(6):886–92.
Meyer E, Vollmer JV, Bovey R, Stamenkovic I. Matrix metalloproteinases 9 and 10 inhibit protein kinase C-potentiated, p53-mediated apoptosis. Cancer Res. 2005;65(10):4261–72.
Chetty C, Bhoopathi P, Lakka SS, Rao JS. MMP-2 siRNA induced Fas/CD95-mediated extrinsic II apoptotic pathway in the A549 lung adenocarcinoma cell line. Oncogene. 2007;26(55):7675–83.
Acknowledgments
This works was supported by Science and Technology Development Plan Project of Shandong Province (2009GG20002096).
Conflict of interest
All authors have no conflict of interest to report.
Ethical standard
All applicable international, national and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of Capital Medical University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Chong-chong Gao and Ben-gang Gong have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Gao, Cc., Gong, Bg., Wu, Jb. et al. MMI-166, a selective matrix metalloproteinase inhibitor, promotes apoptosis in human pancreatic cancer. Med Oncol 32, 418 (2015). https://doi.org/10.1007/s12032-014-0418-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0418-5