Abstract
The Rho GTPase activating protein 26 (ARHGAP26) gene has been reported to be associated with neuropsychiatric diseases and neurodegenerative diseases including Parkinson’s disease. We examined whether the ARHGAP26 gene is associated with Alzheimer’s disease (AD) and/or cardiovascular disease (CVD). Multivariable logistic regression model was used to examine the associations of 154 single nucleotide polymorphisms (SNPs) within the ARHGAP26 gene with AD and CVD using the Alzheimer’s Disease Neuroimaging Initiative 1 (ADNI-1) cohort. Fourteen SNPs were associated with AD (top SNP rs3776362 with p = 3.43 × 10−3), while 37 SNPs revealed associations with CVD (top SNP rs415235 with p = 2.06 × 10−4). Interestingly, 13 SNPs were associated with both AD and CVD. SNP rs3776362 was associated with CVD, Functional Activities Questionnaire (FAQ), and Clinical Dementia Rating Sum of Boxes (CDR-SB). A replication study using a Caribbean Hispanics sample showed that 17 SNPs revealed associations with AD, and 12 SNPs were associated with CVD. The third sample using a family-based study design showed that 9 SNPs were associated with AD, and 3 SNPs were associated with CVD. SNP rs6836509 within the ARHGAP10 gene (an important paralogon of ARHGAP26) was associated with AD and cerebrospinal fluid total tau (t-tau) level in the ADNI sample. Several SNPs were functionally important using the RegulomeDB, while a number of SNPs were associated with significant expression quantitative trait loci (eQTLs) using Genotype-Tissue Expression (GTEx) databases. In conclusion, genetic variants within ARHGAP26 were associated with AD and CVD. These findings add important new insights into the potentially shared pathogenesis of AD and CVD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) and cardiovascular diseases (CVDs) including atherosclerosis, strokes, hypertension, myocardial infarction, coronary heart disease, and congestive heart failure, are common in aging, especially among adults aged 65 years and older, which constitute increasing public health problems (Carter et al. 2017; de la Torre 2012; Gong et al. 2018; Justin et al. 2013; Tini et al. 2020). AD, the most common form of neurodegenerative diseases and dementia, has a substantial genetic component with heritability of 58 to 79% (Gatz et al. 2006). Ninety-five percent of all people who have AD are late-onset AD with occurrence in the eighth or ninth decade of life (American Psychiatric Association 2013; Bettens et al. 2010; Guerreiro et al. 2010). As for CVD, the heritability ranges from 0.30 to 0.50 for various quantitative CVD measures (O'Donnell and Nabel 2008), and the narrow-sense heritability of CAD is estimated to be about 40% (McPherson and Tybjaerg-Hansen 2016; Peden and Farrall 2011).
The co-occurrence of AD and CVD has been suggested due to shared risk factors between AD and CVDs, as well as due to a direct causal association. For example, cardiac diseases cause hypoperfusion and microemboli, which have been implicated in the etiology of AD (Attems and Jellinger 2014; de Bruijn and Ikram 2014; de la Torre 2012; Justin et al. 2013; Tini et al. 2020). It has been reported that CVD and cardiovascular risk factors are associated with an increased risk of AD and mild cognitive impairment (MCI) (de Bruijn and Ikram 2014; Gorelick et al. 2011; Tini et al. 2020). Furthermore, AD and CVD share similar genetic and biochemical profiles and common triggers (Mur et al. 2020; Tini et al. 2020). Several genes have been linked to AD and CVD including apolipoprotein E (APOE), MTHFR, HFE, and FTO (Eriksson et al. 2010; Kotze and van Rensburg 2012; Mahley 2016; Mansoori et al. 2012; Mur et al. 2020; Ray et al. 2008). Individuals who carry AD-associated APOE-ε4 allele usually have higher cholesterol levels (de Bruijn and Ikram 2014) and display a more marked association between the extent of CVD and the density of cardinal neuropathological lesions of AD than subjects who do not carry this APOE-ε4 allele (Tini et al. 2020). Recently, one study identified 90 single nucleotide polymorphisms (SNPs) on 19 different chromosomes that jointly conferred increased risk for AD and cardiovascular outcomes (Broce et al. 2019).
Among the suggested candidate genes for AD and CVD, the Rho GTPase activating protein 26 (ARHGAP26) gene (also known GRAF, GRAF1, OPHN1L, OPHN1L1) is located at 5q31.3 (Borkhardt et al. 2000; Ishikawa et al. 1998). GAP (GTPase-activating protein), one of the modulators of Rho GTPase family, is involved in oxidative stress contributing to vascular disease (Strassheim et al. 2019) and neuroplasticity changes in AD and other brain diseases (Guiler et al. 2021; Lefort 2015). For example, the ARHGAP26 gene was reported to be associated with neuropsychiatric diseases (Dahm et al. 2014), while another study found that ARHGAP26 was significantly upregulated in Parkinson disease (PD), a neurodegenerative disorder, when compared with controls (Jiang et al. 2019). AD is the most common form of age-related neurodegenerative disorder with dementia featured by progressive memory loss and cognitive decline (Lane et al. 2018; Lipnicki et al. 2017). It has been demonstrated that AD shares genetic, epigenetic, and environmental risk factors with PD (Cacabelos 2020; Desikan et al. 2015; Kelly et al. 2020; Ramanan and Saykin 2013). However, no study has investigated the associations of the ARHGAP26 gene with AD and/or CVD. This study aimed to investigate the association of ARHGAP26 gene with the risk of AD and CVD by using a case–control sample, followed by a replication using additional case–control study. A third sample of a family-based study design was also used for replication and confirmation of the current findings in this study. In addition, the associations of ARHGAP10 gene (also known GRAF2; PSGAP; PS-GAP), an important paralogon of ARHGAP26 (Katoh and Katoh 2004), with AD and CVD were examined in the present study.
Materials and Methods
Subjects
ADNI Sample
The Alzheimer’s Disease Neuroimaging Initiative (ADNI) (adni.loni.usc.edu) was launched in 2003 as a public–private partnership, led by Principal Investigator Michael W. Weiner, MD. The primary goal of ADNI has been to test whether serial magnetic resonance imaging (MRI), positron emission tomography (PET), other biological markers, and clinical and neuropsychological assessment can be combined to measure the progression of mild cognitive impairment (MCI) and early AD. The ADNI study began in 2004 as a multicenter that provides services in the United States and Canada. The ADNI is an ongoing, longitudinal, multicenter study designed to develop clinical, imaging, genetic, and biochemical biomarkers for the early detection and tracking of AD. In the present study, the merged data was used from several components of ADNI. There was an Institutional Review Board (IRB) exemption for the current study due to secondary data analysis.
Data of 800 individuals, 200 patients with early AD, 400 with MCI, and 200 with cognitive normal (CN) as controls were extracted from the ADNI cohort 1. Social-demographic factors included gender, age, race, and educational level. Gender was self-reported as either male or female. Age and years of education were considered as continuous variables. Race consisted of four subgroups: non-Hispanic White, non-Hispanic African American, Hispanic, and others. CVD was defined as Yes (with the cardiovascular disease history) or No (without cardiovascular disease history) with a total of 521 patients with CVD. Cerebrospinal fluid (CSF) biomarker included the total tau (t-tau). The Functional Activities Questionnaire (FAQ) was used to measure the activities of daily living, and the higher total scores represent increased disability (Pfeffer et al. 1982). The Clinical Dementia Rating Scale Sum of Boxes (CDR-SB) was utilized to examine the global cognition of participants. A higher CDR-SB score indicates a more severe degree of cognitive deficits (Morris 1993).
Genotyping was conducted using the Affymetrix technique. A total of 154 SNPs within the ARHGAP26 gene and 63 SNPs within the ARHGAP10 gene located at 4q31.23 were available in the ADNI sample. APOE-ε4 carriers were defined as individuals with at least one ε4 allele while non-carriers were defined as individuals with no ε4 allele (APOE-ε4-0) (Table 1).
The Caribbean Hispanics Sample
To validate the association of ARHGAP26 gene, we used data from The Columbia University Study of Caribbean Hispanics with Familial and Sporadic Late Onset Alzheimer’s disease-dbGaP Study Accession: phs000496.v1.p1 (Lee et al. 2011). Gender was self-reported as either male or female, while age and years of education were considered as continuous variables. All individuals are Hispanic. CVD was defined as Yes (with the history of heart disease) or No (without history of heart disease).
Genotyping was conducted using the Illumina technique. A total of 249 SNPs within the ARHGAP26 gene and 89 SNPs within the ARHGAP10 gene were available. APOE-ε4 carriers were defined as individuals with at least one ε4 allele while non-carriers were defined as individuals with no ε4 allele (APOE-ε4-0) (Table 1).
NIA-LOAD Family Study
Three thousand seven individuals were available from the National Institute on Aging-Late Onset Alzheimer's Disease (NIA-LOAD) Family Study: Genome-Wide Association Study for Susceptibility Loci–Study Accession: phs000168.v2.p2. The details about these subjects were described elsewhere (Lee et al. 2008). Genotyping was conducted by the Center for Inherited Disease Research (CIDR) using the Illumina Infinium II assay protocol. A total of 1266 AD cases and 1279 non-AD individuals from 1386 pedigree (including 589 nuclear families) (Table 1) were included. A total of 351 individuals with CVD and 1553 without CVD was available. A total of 155 SNPs within the ARHGAP26 gene and 62 SNPs within the ARHGAP10 gene were available.
Statistical Methods
Genotype Quality Control
The Golden Helix Software (https://www.goldenhelix.com/products/SNP_Variation/index.html) was used to assess control genotype data for conformity with Hardy–Weinberg equilibrium (HWE). To deal with population stratification, the principal-component analysis approach (Price et al. 2006) in HelixTree was used to obtain first three principal components (PCs) for both data. Call rate and minor allele frequency (MAF) was determined for each SNP using The Golden Helix Software. SNPs with MAF < 1%, and/or call rate < 95%, and/or HWE < 10−4 were removed for further association analyses.
Multivariable Logistic/Linear Regression Models in PLINK Software
For the case–control designs, the multivariable logistic regression analyses of risk of AD and CVD as binary traits, adjusted for gender, age, education, racial group, APOE-ε4 genotype, and first three PCs were performed. The asymptotic p-values for the logistic regression models were observed while the odds ratio (OR) and its 95% confidence interval were estimated. For continuous outcomes such as FAQ, CDR-SB, and t-tau, the multivariable linear regression analyses, adjusted for gender, age, education, racial group, APOE-ε4 genotype, and first three PCs, were performed. The multivariable logistic/linear regression models were performed using PLINKv1.9 (www.cog-genomics.org/plink/1.9/ (Chang et al. 2015). To deal with multiple testing, Bonferroni correction was used for statistical significance.
Haplotype Analysis in the ADNI Sample
Pairwise linkage disequilibrium (LD) statistics (D′) were assessed for controls, and haplotype blocks were constructed using HAPLOVIEW software (Barrett et al. 2005). Haplotype analysis of AD and CVD was performed using the multivariate logistic model using the PLINK v1.07 (Purcell et al. 2007). The asymptotic p-values for the logistic regression models were observed while the OR and its standard error were estimated using PLINK v1.07.
Family-Based Association Study
A family-based association analysis for AD and CVD was performed using the PLINK v1.07 (Purcell et al. 2007). The DFAM procedure in PLINK implements the sib-transmission disequilibrium test (TDT) and also allows for unrelated individuals to be included. This test can be used to combine discordant sibship data, parent–offspring trio data, and unrelated case/control data in a single analysis.
Functional Analysis In Silico
Functional annotation of SNPs was performed using three online functional prediction websites: SNPinfo (https://snpinfo.niehs.nih.gov/snpinfo/snpfunc.html), RegulomeDB (http://regulomedb.org/), and the Genotype-Tissue Expression (GTEx) (www.gtexportal.org). First, the associated SNPs were examined for microRNA binding sites, splicing sites, regulatory gene regions, and species-conserved regions using NIH-SNP Function Prediction (http://snpinfo.niehs.nih.gov/cgi-bin/snpinfo/snpfunc.cgi). Second, the potential functional consequences of associated SNPs were accessed using RegulomeDB (Boyle et al. 2012), which has a self-developed score system with a score ranging from 1 to 7, where a higher score indicates less functional significance. Third, the expression quantitative trait loci (eQTLs) of associated SNPs were assessed by the GTEx database.
Data Availability Statement
The datasets used during the current study are available in the (Alzheimer’s Disease Neuroimaging Initiative (ADNI)) repository, (http://adni.loni.usc.edu/data-samples/access-data/), (dbGaP:phs000496.v1.p1 Columbia University Study of Caribbean Hispanics and Late Onset Alzheimer’s disease) repository, (https://www.ncbi.nlm.nih.gov/gap/?term=phs000496.v1.p1), and (National Institute on Aging—Late Onset Alzheimer's Disease Family Study: Genome-Wide Association Study for Susceptibility Loci dbGaP Study Accession: phs000168.v2.p2) repository, (https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000168.v2.p2).
Results
Genotype Quality Control and Descriptive Statistics
The characteristics of participants of the three samples are presented in Table 1. After merging SNPs and phenotypes, 755 individuals in the ADNI sample kept in the study include 173 individuals with AD, 368 with MCI, and 214 with CN, while 2307 individuals in the Caribbean Hispanics sample were remained including 864 individuals with AD and 1412 with CN. The mean ages were 75.20 years, 76.13 years, and 75.53 years for ADNI sample, Caribbean Hispanics sample, and NIA family-based study, respectively. There were slightly more males (59.2%) than females in the ADNI sample, and more females than males in the Caribbean Hispanics sample (67.6%) and the NIA family-based study (64.6%).
Single Marker Association Analysis in the ADNI Sample
A total of 14 SNPs within the ARHGAP26 gene were associated with AD (p < 0.05) in the ADNI sample, and the best associated SNP was rs3776362 (p = 3.43 × 10−3). Furthermore, 37 SNPs revealed associations with CVD (top SNP rs415235 with p = 2.06 × 10−4). Interestingly, 13 SNPs were associated with both AD and CVD (top 3 SNPs for AD rs3776362, rs245852, and rs35291 with p = 3.43 × 10−3, 9.47 × 10−3, and 9.996 × 10−3, respectively, and p = 8.66 × 10−3, 2.91 × 10−3, and 4.16 × 10−3 for CVD, respectively). The SNPs with p < 0.05 with AD or CVD are presented in Table S1. The top 10 SNPs associated with AD or CVD are presented in Table 2. The top two SNPs (rs415235 and rs1370982) showing significant associations with CVD remained significant after a Bonferroni correction (p < 0.05/137 = 3.65 × 10−4). The best AD-associated SNP, rs3776362, was further associated with FAQ, and CDR-SB (p = 0.0229 and 0.0411, respectively). Within the ARHGAP10 gene, four SNPs were associated with AD (top SNP rs6836509 with p = 0.0278), but no SNP was found to be associated with CVD. Interestingly, rs6836509 in the ADNI sample was associated with t-tau protein (p = 4.63 × 10−4), and rs17475681 was associated with FAQ and CRD-SB and FAQ (p = 0.0311 and 0.0152, respectively).
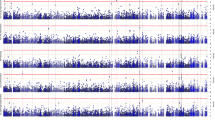
Haplotype Analyses in the ADNI Sample
Using HAPLOVIEW software, we identified three haplotype blocks including top AD-associated and CVD-associated SNPs within the ARHGAP26 gene in the ADNI sample. Figure 1 shows the LD (D′) structure. The G-C haplotype from rs13161500 and rs1370982 (D′ = 0.85) revealed significant associations with AD and CVD (p = 0.0126 and 1.27 × 10−4, respectively) (Table 3). The G-A haplotype from rs3776362 and rs1347813 (D′ = 1.00) revealed significant associations with AD and CVD (p = 3.42 × 10−3 and 8.43 × 10−3, respectively).
Association Analysis in Caribbean Hispanics Sample
Single marker analysis showed that 17 SNPs within the ARHGAP26 gene were associated with AD (p < 0.05) and the best associated SNP was rs2107622 with p = 5.59 × 10−4. Furthermore, 12 SNPs were associated with CVD (top SNP rs6580265 with p = 2.91 × 10−3). Interestingly, two SNPs (rs2107622 and rs245828) were associated with both AD and CVD (p = 5.59 × 10−4 and 2.50 × 10−2 for AD and p = 2.35 × 10−2 and 2.92 × 10−2 for CVD, respectively). The SNPs with p < 0.05 with AD or CVD in Caribbean Hispanics sample are presented in Table S2. The top 10 SNPs associated with AD or CVD are presented in Table 4. Within the ARHGAP10 gene, two SNPs (rs6845865 and rs10003349) were associated with AD, and several SNPs were associated with CVD.
Association Analysis in NIA Sample Using a Family-Based Study Design
A family-based study showed that nine SNPs within the ARHGAP26 gene were associated with AD and three SNPs were associated with CVD in the NIA sample (Table 5). Four AD-associated SNPs (rs245852, rs37212, rs3776362, and rs37210) within the ARHGAP26 gene from the NIA sample were also associated with AD and CVD in the ADNI sample (Table 2). Within the ARHGAP10 gene, four SNPs were associated with AD, but no SNP was associated with CVD.
In Silico Analysis
In the ADNI sample, rs3776362 associated with both AD and CVD was located at the gene regulatory region, and rs415235 associated with CVD was located at the species-conserved region. In the Caribbean Hispanics sample, rs7727006 associated with CVD was located at the gene regulatory region, and rs11167807 associated with AD was located at the species-conserved region.
RegulomeDB returned score of ≤ 3 is considered functionally important. Within the ARHGAP26 gene, three SNPs, rs3776362 (with 2b), rs463717 (3a), and rs1347813 (3a), associated with AD and CVD are functionally important in the ADNI sample (Table 2). Four SNPs, rs258764 (3a), rs11167807 (3a), and rs6894946 (2b) associated with AD, and rs17707291 (3a), associated with CVD are functionally important in the Caribbean Hispanics sample (Table 4). Two SNPs, rs3776362 (2b) and rs3776309 (2b), associated with AD are functionally important in the family-based study (Table 5).
Within the ARHGAP26 gene, a total of 14 SNPs in Table 2, 9 SNPs in Table 4, and 4 SNPs in Table 5 had significant eQTLs. Within the ARHGAP10 gene, a total of 2 SNPs in Tables 2, 3 SNPs in Table 4, and 4 SNPs in Table 5 had significant eQTLs. A more comprehensive list of SNPs with eQTLs is presented in supplementary Table S3.
Discussion
The present study examined the associations of the ARHGAP26 gene polymorphisms with AD and CVD using three datasets. In the ADNI sample, there were 13 SNPs within the ARHGAP26 gene associated with both AD and CVD, while in the replication sample using a case–control sample, there were 2 SNPs associated with both AD and CVD. The results of an additional sample using a family-based study showed that nine SNPs were associated with AD, and three SNPs were associated with CVD. The top SNP rs3776362 associated with AD in the ADNI sample was associated with cognitive phenotypes (FAQ and CDR-SB). Haplotype analysis further supported the single marker of the ARHGAP26 gene in associations with AD and CVD in the ADNI sample. Several SNPs of this gene are functionally important using the RegulomeDB data. Within the ARHGAP10 gene, top SNP rs6836509 associated with AD and t-tau protein level in the ADNI sample. Additionally, over 20 SNPs of ARHGAP26 and ARHGAP10 genes had eQTLs using the GTEx database.
The ARHGAP26 (also known as GRAF) gene is a protein coding gene. Previous studies have shown that GRAF mRNA is expressed in a variety of avian tissues and is particularly abundant in brain and liver (Hildebrand et al. 1996; Lucken-Ardjomande Hasler et al. 2014). GRAF may be a regulator of the Rho family of small GTP-binding proteins that exhibit binding to a protein tyrosine kinase (Hildebrand et al. 1996; Shibata et al. 2001). Indeed, the GRAF gene is involved in leukemia (Bojesen et al. 2006; Borkhardt et al. 2000; Hildebrand et al. 1996), human brain cancer (Wang et al. 2013), gastric cancer (Wangxia et al. 2019), and ovarian cancer (Chen et al. 2019). ARHGAP26 is also critical for muscle development and may be involved in RhoA activity and progressive muscle degeneration (Doherty et al. 2011; Li et al. 2019). In addition, ARHGAP26 might be involved in the pathogenesis of mental retardation (Barresi et al. 2010) and neuropsychiatric diseases (Dahm et al. 2014). Interestingly, one recent study suggested that ARHGAP26 is involved in the development of dyslexia, a heritable neurodevelopmental disorder characterized by difficulties in reading and writing (Naskar et al. 2018). The patients with dyslexia are similar to patients with dementia who have language deficiencies with significantly lower results in the area of verbal expression, hearing comprehension, repetition, reading, and writing (Banovic et al. 2018). In the present study, we found ARHGAP26 gene polymorphisms were associated with AD and CVD. Especially, in the ADNI sample, there were 13 SNPs of the ARHGAP26 gene associated with both AD and CVD, while in the replication sample using a case–control sample, there were 2 SNPs associated with both AD and CVD. Additionally, four SNPs (rs245852, rs37212, rs3776362, and rs37210) were associated with AD both in ADNI and the family-based study. These findings suggest a shared genetic susceptibility among AD and CVD. To our knowledge, this is the first study that investigates the associations of ARHGAP26 gene polymorphisms with AD and CVD.
AD is the most common form of age-related neurodegenerative disorder with dementia (Lane et al. 2018; Lipnicki et al. 2017). Both AD and PD are neurodegenerative disorders and may share genetic, epigenetic, and environmental risk factors (Cacabelos 2020; Cifelli et al. 2019; Desikan et al. 2015; Jabir et al. 2015; Kelly et al. 2020; Ramanan and Saykin 2013; Ray et al. 2008). Although AD, vascular dementia (VD), and PD exert increasingly lethal or disabling effects, the associations among these diseases at the molecular level remain unclear (Chen et al. 2021). Interestingly, one recent study found that ARHGAP26 mRNA was significantly upregulated in PD, suggesting that the gene ARHGAP26 may be associated with PD (Jiang et al. 2019). Furthermore, it is suggested that common molecular mechanisms underlie the development of AD, PD, and cancer (Aliev et al. 2013; Driver et al. 2012; Forés-Martos et al. 2021; Jabir et al. 2015; Roe et al. 2010, Sharma et al. 2020). Previous findings and the current study suggest that ARHGAP26 may be one of the mechanisms to link AD, CVD, cancer, and PD; however, a confirmation study and a gene functional analysis are needed.
We also examined the association of the ARHGAP10 gene with AD and CVD. The ARHGAP10 gene, an important paralogon of ARHGAP26, is located at 4q31.23 (Katoh and Katoh 2004; Koeppel et al. 2004; Shibata et al. 2001). ARHGAP10 mRNA is expressed in the brain, heart, skeletal muscle, and testis (Ren et al. 2001; Shibata et al. 2001). Recently, ARHGAP10 gene mutations have been found to play a pathophysiologic and pathogenic role in schizophrenia (Hada et al. 2021; Sekiguchi et al. 2020). However, no study has focused on the effect of ARHGAP10 gene on AD and CVD. The present study showed that several SNPs in each of the three samples were associated with AD. Interestingly, rs6836509 in the ADNI sample was also associated with t-tau protein, and rs17475681 was associated with CRD-SB and FAQ. Additionally, several SNPs were found to be associated with CVD only in the Hispanic sample. These findings may suggest that ARHGAP10 gene may play a role in AD and related cognitive functions, but no SNPs on this gene have been found to be associated with both AD and CVD.
Previous studies have shown that the co-occurrence of AD and CVD might be due to shared risk factors between AD and CVDs, but there might also be a direct causal association of CVD and cardiovascular risk factors with AD (de la Torre 2012; Justin et al. 2013; Attems and Jellinger 2014; de Bruijn and Ikram 2014; Jabir et al. 2015; Monte and Vondriska 2014; Tini et al. 2020). AD and CVDs may also share genetic factors (Carter et al. 2017; Moreira et al. 2005; Mur et al. 2020; Nicot et al. 2007; Tan et al. 2013; Tini et al. 2020). Genome-wide association study also found that there may be a link between AD and CVDs using pathway analysis (Liu et al. 2014). A recent study identified 90 SNPs on 19 different chromosomes that jointly conferred increased risk for AD and cardiovascular outcomes (Broce et al. 2019). Our current findings and previous reports suggest three possible scenarios for genetic variants shared by AD and CVD: (1) genetic variants influence cardiovascular risk factors and AD independently, or (2) genetic variants influence AD through multiple cardiovascular risk factors (Broce et al. 2019), and/or (3) those disease-associated variants involved in common biology pathways result in the disease development. However, some genes could interact with cardiovascular risk factors in the development of AD (Bessi et al. 2020). Additionally, epigenetic influence at cellular and molecular levels in cancer, metabolic and cardiovascular complications are also involved in the development of neurological (psychosis) and neurodegenerative disorders such as AD and PD (Sharma et al. 2020).
There are several strengths of this study. First, we used a total of three samples: a population-based case control (ADNI) sample, a case control Caribbean Hispanic sample, and a family-based sample. A family study offers several advantages and has long been the favored approach for genetic study because of (1) reducing the type 1 error rate arising from population stratification and the NIA family–based study confirmed the results of the ADNI sample; (2) possessing several advantageous features for linkage and association tests compared with using samples of related subjects; (3) remaining a powerful and advantageous approach in complex trait genetics; and (4) reducing heterogeneity for the study due to related family members who tend to share similar lifestyles and genetic factors for a trait. Second, three samples revealed that several common genetic variants were associated with both AD and CVD, while top AD-associated SNP rs3776362 in the ADNI sample was also associated with cognitive phenotypes such as FAQ and CDR-SB. In addition, we performed functional analyses and found several SNPs with eQTLs.
There are a number of limitations in this study. The three samples may have ethnic heterogeneity even though there is a small proportion of Hispanic population representation in the ADNI sample. The majority in the ADNI sample and the NIA-LOAD family-based sample are non-Hispanic White; however, the Caribbean Hispanic sample is a genetic heterogeneous population. Furthermore, different genotyping platforms may lead to a limited overlap of the SNPs in three sets of samples. Finally, the results in the present study might be spurious or subject to type I error due to the large number of analyses performed in this study.
Conclusion
ARHGAP26 genetic variants are significantly associated with the risks of AD and CVD in three independent samples. A number of SNPs within the ARHGAP26 gene associated AD and CVD are functionally important or have had significant eQTLs based on in silico analysis. Furthermore, one AD-associated SNP rs3776362 in the ADNI sample was also associated with cognitive phenotypes. In addition, several ARHGAP10 genetic variants are significantly associated with the risks of AD in these independent samples. Within the ARHGAP10 gene, top SNP rs6836509 associated with AD in the ADNI sample was associated with t-tau protein. These results suggest a potential role of ARHGAP26 and ARHGAP10 in the pathogenesis of AD and/or CVD. Future functional study of these two genes may help to better characterize the genetic architecture of AD and CVD.
Availability of Data and Materials
The datasets generated during and/or analyzed during the current study are available in the (Alzheimer’s Disease Neuroimaging Initiative (ADNI)) repository, (http://adni.loni.usc.edu/data-samples/access-data/), and (dbGaP:phs000496.v1.p1 Columbia University Study of Caribbean Hispanics and Late Onset Alzheimer’s disease) repository, (https://www.ncbi.nlm.nih.gov/gap/?term=phs000496.v1.p1).
References
Aliev G, Obrenovich ME, Tabrez S et al (2013) Link between cancer and Alzheimer disease via oxidative stress induced by nitric oxide-dependent mitochondrial DNA overproliferation and deletion. Oxid Med Cell Longev 2013:962984
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th ed. Author: Arlington, VA
Attems J, Jellinger KA (2014) The overlap between vascular disease and Alzheimer’s disease—lesson from pathology. BMC Med 12:206
Banovic S, Zunic LJ, Sinanovic O (2018) Communication difficulties as a result of dementia. Materia Socio-Medica 30(3):221–224. https://doi.org/10.5455/msm.2018.30.221-224
Barresi V, Ragusa A, Fichera M, Musso N, Castiglia L, Rappazzo G, Travali S, Mattina T, Romano C, Cocchi G et al (2010) Decreased expression of GRAF1/OPHN-1-L in the X-linked α thalassemia mental retardation syndrome. BMC Med Genomics 3:28
Barrett JC, Fry B, Maller J, Daly MJ (2005) Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21:263–265
Bessi V, Balestrini J, Bagnoli S, Mazzeo S, Giacomucci G, Padiglioni S, Piaceri I, Carraro M, Ferrari C, Bracco L, Sorbi S, Nacmias B (2020) Influence of ApoE genotype and clock T3111C interaction with cardiovascular risk factors on the progression to Alzheimer’s disease in subjective cognitive decline and mild cognitive impairment patients. J Pers Med 10(2):45. https://doi.org/10.3390/jpm10020045
Bettens K, Sleegers K, Van Broeckhoven C (2010) Current status on Alzheimer disease molecular genetics: from past, to present, to future. Hum Mol Genet 19(R1):R4–R11
Bojesen SE, Ammerpohl O, Weinhäusl A, Haas OA, Mettal H, Bohle RM, Borkhardt A, Fuchs U (2006) Characterisation of the GRAF gene promoter and its methylation in patients with acute myeloid leukaemia and myelodysplastic syndrome. Br J Cancer 94(2):323–332
Borkhardt A, Bojesen S, Haas OA, Fuchs U, Bartelheimer D, Loncarevic IF, Bohle RM, Harbott J, Repp R, Jaeger U, Viehmann S, Henn T, Korth P, Scharr D, Lampert F (2000) The human GRAF gene is fused to MLL in a unique t(5;11)(q31;q23) and both alleles are disrupted in three cases of myelodysplastic syndrome/acute myeloid leukemia with a deletion 5q. Proc Nat Acad Sci 97:9168–9173
Boyle AP, Hong EL, Hariharan M et al (2012) Annotation of functional variation in personal genomes using RegulomeDB. Genome Res 22:1790–1797
Broce IJ, Tan CH, Fan CC, Jansen I, Savage JE, Witoelar A, Wen N et al (2019) Dissecting the genetic relationship between cardiovascular risk factors and Alzheimer’s disease. Acta Neuropathol 137(2):209–226. https://doi.org/10.1007/s00401-018-1928-6
Cacabelos R (2020) Pharmacogenomics of Alzheimer’s and Parkinson’s diseases. Neurosci Lett 726:133807. https://doi.org/10.1016/j.neulet.2018.09.018
Carter CJ, France J, Crean S, Singhrao SK (2017) The Porphyromonas gingivalis/host interactome shows enrichment in GWASdb genes related to Alzheimer’s disease, diabetes and cardiovascular diseases. Front Aging Neurosci 9:408. https://doi.org/10.3389/fnagi.2017.00408
Chang CC, Chow CC, Tellier LCAM, Vattikuti S, Purcell SM, Lee JJ (2015) Second-generation PLINK: rising to the challenge of larger and richer datasets. GigaScience 4
Chen X, Chen S, Li Y, Gao Y, Huang S, Li H, Zhu Y (2019) SMURF1-mediated ubiquitination of ARHGAP26 promotes ovarian cancer cell invasion and migration. Exp Mol Med 51(4):1–12. https://doi.org/10.1038/s12276-019-0236-0
Chen Y, Liu Q, Liu J, Wei P, Li B, Wang N et al (2021) Revealing the modular similarities and differences among Alzheimer’s disease, vascular dementia, and Parkinson’s disease in genomic networks. Neuromol Med. https://doi.org/10.1007/s12017-021-08670-2
Cifelli JL, Capule CC, Yang J (2019) Noncovalent, electrostatic interactions induce positively cooperative binding of small molecules to Alzheimer’s and Parkinson’s disease-related amyloids. ACS Chem Neurosci 10(2):991–995. https://doi.org/10.1021/acschemneuro.8b00280
Dahm L, Ott C, Steiner J, Stepniak B, Teegen B, Saschenbrecker S, Hammer C, Borowski K, Begemann M, Lemke S et al (2014) Seroprevalence of autoantibodies against brain antigens in health and disease. Ann Neurol 76:82–94
de Bruijn RFAG, Ikram MA (2014) Cardiovascular risk factors and future risk of Alzheimer’s disease. BMC Med 12:1–130. https://doi.org/10.1186/s12916-014-0130-5
de la Torre JC (2012) Cardiovascular risk factors promote brain hypoperfusion leading to cognitive decline and dementia. Cardiovasc Psychiatry Neurol 2012:367516. https://doi.org/10.1155/2012/367516
Desikan RS, Schork AJ, Wang Y, Witoelar A, Sharma M, McEvoy LK, Holland D et al (2015) Genetic overlap between Alzheimer’s disease and Parkinson’s disease at the MAPT locus. Mol Psychiatry 20(12):1588–1595. https://doi.org/10.1038/mp.2015.6
Doherty JT, Lenhart KC, Cameronm MV, Mack CP, Conlon FL, Taylor JM (2011) Skeletal muscle differentiation and fusion are regulated by the BAR-containing Rho-GTPase-activating protein (Rho-GAP), GRAF1. J Biol Chem 286:25903–25921
Driver JA, Beiser A, Au R, Kreger BE, Splansky GL, Kurth T, Kiel DP, Lu KP, Seshadri S, Wolf PA (2012) Inverse association between cancer and Alzheimer’s disease: results from the Framingham Heart Study. BMJ 344:1442. https://doi.org/10.1136/bmj.e1442
Eriksson UK, Bennet AM, Gatz M, Dickman W, Pedersen NL (2010) Nonstroke cardiovascular disease and risk of Alzheimer disease and dementia. Alzheimer Dis Assoc Disord 24:213–219
Forés-Martos J, Boullosa C, Rodrigo-Domínguez D, Sánchez-Valle J, Suay-García B, Climent J, Falcó A, Valencia A, Puig-Butillé JA, Puig S, Tabarés-Seisdedos R (2021) Transcriptomic and genetic associations between Alzheimer’s disease, Parkinson’s disease, and cancer. Cancers (Basel) 13(12):2990. https://doi.org/10.3390/cancers13122990
Gatz M, Reynolds CA, Fratiglioni L, Johansson B et al (2006) Role of genes and environments for explaining Alzheimer disease. Arch Gen Psychiatry 63(2):168–174
Gong S, Su BB, Tovar H, Hinojosa P, Gonzalez V, Liu Y, Lu Y, Wang K, Xu C (2018) Polymorphisms within RYR3 gene are associated with risk and age at onset of hypertension, diabetes and Alzheimer’s disease. Am J Hypertens 31(7):818–826
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, Launer LJ et al (2011) Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42:2672–2713
Guerreiro RJ, Beck J, Gibbs JR, Santana I, Rossor MN, Schott JM et al (2010) Genetic variability in CLU and its association with Alzheimer’s disease. PLoS One 5(3):e9510
Guiler W, Koehler A, Boykin C, Lu Q (2021) Pharmacological modulators of small GTPases of Rho family in neurodegenerative diseases. Front Cell Neurosci 15:661612
Hada K, Wulaer B, Nagai T, Itoh N, Sawahata M, Sobue A, Mizoguchi H, Mori D, Kushima I, Nabeshima T, Ozaki N, Yamada K (2021) Mice carrying a schizophrenia-associated mutation of the Arhgap10 gene are vulnerable to the effects of methamphetamine treatment on cognitive function: association with morphological abnormalities in striatal neurons. Mol Brain 14(1):21. https://doi.org/10.1186/s13041-021-00735-4
Hildebrand JD, Taylor JM, Parsons TJ (1996) An SH3 domain-containing GTPase-activating protein for Rho and Cdc42 associates with focal adhesion kinase. Molec Cell Biol 16:3169–3178
Ishikawa K, Nagase T, Suyama M, Miyajima N, Tanaka A, Kotani H, Nomura N, Ohara O (1998) Prediction of the coding sequences of unidentified human genes. X. The complete sequences of 100 new cDNA clones from brain which can code for large proteins in vitro. DNA Res 5:169–176
Jabir NR, Firoz CK, Baeesa SS, Ashraf GM, Akhtar S, Kamal W, Kamal MA, Tabrez S (2015) Synopsis on the linkage of Alzheimer’s and Parkinson’s disease with chronic diseases. CNS Neurosci Ther 21(1):1–7. https://doi.org/10.1111/cns.12344
Jiang F, Wu Q, Sun S, Bi G, Guo L (2019) Identification of potential diagnostic biomarkers for Parkinson’s disease. FEBS Open Bio 9(8):1460–1468. https://doi.org/10.1002/2211-5463.12687
Justin BN, Turek M, Hakim AM (2013) Heart disease as a risk factor for dementia. Clin Epidemiol 5:135–145
Katoh M, Katoh M (2004) Characterization of human ARHGAP10 gene in silico. Int J Oncol 25(4):1201–1206
Kelly J, Moyeed R, Carroll C, Luo S, Li X (2020) Genetic networks in Parkinson’s and Alzheimer’s disease. Aging (albany NY) 12(6):5221–5243. https://doi.org/10.18632/aging.102943
Koeppel MA, McCarthy CC, Moertl E, Jakobi R (2004) Identification and characterization of PS-GAP as a novel regulator of caspase-activated PAK-2. J Biol Chem 279:53653–53664
Kotze MJ, van Rensburg SJ (2012) Pathology supported genetic testing and treatment of cardiovascular disease in middle age for prevention of Alzheimer’s disease. Metab Brain Dis 27(3):255–266. https://doi.org/10.1007/s11011-012-9296-8
Lane CA, Hardy J, Schott JM (2018) Alzheimer’s disease. Eur J Neurol 25(1):59–70. https://doi.org/10.1111/ene.13439
Lee JH, Cheng R, Barral S, Reitz C, Medrano M, Lantigua R, Jiménez-Velazquez IZ, Rogaeva E, St George-Hyslop PH, Mayeux R (2011) Identification of novel loci for Alzheimer disease and replication of CLU, PICALM, and BIN1 in Caribbean Hispanic individuals. Arch Neurol 68(3):320–328
Lee JH, Cheng R, Graff-Radford N, Foroud T, Mayeux R, National Institute on Aging Late-Onset Alzheimer’s Disease Family Study Group (2008) Analyses of the National Institute on Aging Late-Onset Alzheimer’s Disease Family Study: implication of additional loci. Arch Neurol 65(11):1518–1526
Lefort R (2015) Reversing synapse loss in Alzheimer’s disease: Rho-guanosine triphosphatases and insights from other brain disorders. Neurotherapeutics 12(1):19–28. https://doi.org/10.1007/s13311-014-0328-4
Li M, Ye L, Ye X, Wang S, Zhang H, Liu J, Hong H (2019) Hypoxia-induced ARHGAP26 deficiency inhibits the proliferation and migration of human ductus arteriosus smooth muscle cell through activating RhoA-ROCK-PTEN pathway. J Cell Biochem 120(6):10106–10117. https://doi.org/10.1002/jcb.28294
Lipnicki DM, Crawford JD, Dutta R, Thalamuthu A, Kochan NA, Andrews G et al (2017) Age-related cognitive decline and associations with sex, education and apolipoprotein E genotype across ethnocultural groups and geographic regions: a collaborative cohort study. PLoS Med 14:e1002261
Liu G, Yao L, Liu J, Jiang Y, Ma G, Genetic and Environmental Risk for Alzheimer’s disease (GERAD1) Consortium, Chen Z, Zhao B, Li K (2014) Cardiovascular disease contributes to Alzheimer’s disease: evidence from large-scale genome-wide association studies. Neurobiol Aging 35(4):786–792
Lucken-Ardjomande Hasler S, Vallis Y, Jolin H, McKenzie A, McMahon H (2014) GRAF1a is a brain-specific protein that promotes lipid droplet clustering and growth, and is enriched at lipid droplet junctions. J Cell Sci 127(21):4602–4619
Mahley RW (2016) Apolipoprotein E: from cardiovascular disease to neurodegenerative disorders. J Mol Med 94:739–746
Mansoori N, Tripathi M, Luthra K, Alam R, Lakshmy R, Sharma S (2012) MTHFR (677 and 1298) and IL-6-174 G/C genes in pathogenesis of Alzheimer’s and vascular dementia and their epistatic interaction. Neurobiol Aging 33:1003.e1-1003.e8
McPherson R, Tybjaerg-Hansen A (2016) Genetics of coronary artery disease. Circ Res 118:564–578
Monte E, Vondriska TM (2014) Epigenomes: the missing heritability in human cardiovascular disease? Proteomics Clin Appl 8(7–8):480–487. https://doi.org/10.1002/prca.201400031
Moreira PI, Smith MA, Zhu X, Nunomura A, Castellani RJ, Perry G (2005) Oxidative stress and neurodegeneration. Ann N Y Acad Sci 1043(1):545–552. https://doi.org/10.1196/annals.1333.062
Morris JC (1993) Clinical dementia rating. Neurology 43:2412–2414
Mur J, McCartney DL, Walker RM, Campbell A, Bermingham ML, Morris SW, Porteous DJ, McIntosh AM, Deary IJ, Evans KL, Marioni RE (2020) DNA methylation in APOE: the relationship with Alzheimer’s and with cardiovascular health. Alzheimers Dement (N Y) 6(1):e12026. https://doi.org/10.1002/trc2.12026
Naskar T, Faruq M, Banerjee P, Khan M, Midha R, Kumari R, Devasenapathy S, Prajapati B, Sengupta S, Jain D, Mukerji M, Singh NC, Sinha S (2018) Ancestral variations of the PCDHG gene cluster predispose to dyslexia in a multiplex family. EBioMedicine 28:168–179. https://doi.org/10.1016/j.ebiom.2017.12.031
Nicot A-S, Toussaint A, Tosch V et al (2007) Mutations in amphiphysin 2 (BIN1) disrupt interaction with dynamin 2 and cause autosomal recessive centronuclear myopathy. Nat Genet 39(9):1134–1139. https://doi.org/10.1038/ng2086
O’Donnell CJ, Nabel EG (2008) Cardiovascular genomics, personalized medicine, and the National Heart, Lung, and Blood Institute: part I: the beginning of an era. Circ Cardiovasc Genet 1(1):51–57. https://doi.org/10.1161/CIRCGENETICS.108.813337
Peden JF, Farrall M (2011) Thirty-five common variants for coronary artery disease: the fruits of much collaborative labour. Hum Mol Genet 20:R198–R205
Pfeffer RI, Kurosaki TT, Harrah CH et al (1982) Measurement of functional activities of older adults in the community. J Gerontol 37:323–329
Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D (2006) Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet 38(8):904–909
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D et al (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81(3):559–575
Ramanan VK, Saykin AJ (2013) Pathways to neurodegeneration: mechanistic insights from GWAS in Alzheimer’s disease, Parkinson’s disease, and related disorders. Am J Neurodegener Dis 2(3):145–175
Ray M, Ruan J, Zhang W (2008) Variations in the transcriptome of Alzheimer’s disease reveal molecular networks involved in cardiovascular diseases. Genome Biol 9(10):R148
Ren XR, Du QS, Huang YZ, Ao SZ, Mei L, Xiong WC (2001) Regulation of CDC42 GTPase by proline-rich tyrosine kinase 2 interacting with PSGAP, a novel pleckstrin homology and Src homology 3 domain containing rhoGAP protein. J Cell Biol 152(5):971–984
Roe CM, Fitzpatrick AL, Xiong C, Sieh W, Kuller L, Miller JP, Williams MM, Kopan R, Behrens MI, Morris JC (2010) Cancer linked to Alzheimer disease but not vascular dementia. Neurology 74(2):106–112. https://doi.org/10.1212/WNL.0b013e3181c91873
Sekiguchi M, Sobue A, Kushima I, Wang C, Arioka Y, Kato H, Kodama A, Kubo H, Ito N, Sawahata M, Hada K, Ikeda R, Shinno M, Mizukoshi C, Tsujimura K, Yoshimi A, Ishizuka K, Takasaki Y, Kimura H, Xing J, Yu Y, Yamamoto M, Okada T, Shishido E, Inada T, Nakatochi M, Takano T, Kuroda K, Amano M, Aleksic B, Yamomoto T, Sakuma T, Aida T, Tanaka K, Hashimoto R, Arai M, Ikeda M, Iwata N, Shimamura T, Nagai T, Nabeshima T, Kaibuchi K, Yamada K, Mori D, Ozaki N (2020) ARHGAP10, which encodes Rho GTPase-activating protein 10, is a novel gene for schizophrenia risk. Transl Psychiatry 10(1):247. https://doi.org/10.1038/s41398-020-00917-z.PMID:32699248;PMCID:PMC7376022
Sharma VK, Mehta V, Singh TG (2020) Alzheimer’s disorder: epigenetic connection and associated risk factors. Curr Neuropharmacol 18(8):740–753. https://doi.org/10.2174/1570159X18666200128125641
Shibata H, Oishi K, Yamagiwa A, Matsumoto M, Mukai H, Ono Y (2001) PKN-beta interacts with the SH3 domains of Graf and a novel Graf related protein, Graf2, which are GTPase activating proteins for Rho family. J Biochem 130:23–31
Strassheim D, Gerasimovskaya E, Irwin D, Dempsey EC, Stenmark K, Karoor V (2019) RhoGTPase in vascular disease. Cells 8(6):551. https://doi.org/10.3390/cells8060551
Tan M-S, Yu J-T, Tan L (2013) Bridging integrator 1 (BIN1): form, function, and Alzheimer’s disease. Trends Mol Med 19(10):594–603. https://doi.org/10.1016/j.molmed.2013.06.004
Tini G, Scagliola R, Monacelli F, La Malfa G, Porto I, Brunelli C, Rosa GM (2020) Alzheimer’s disease and cardiovascular disease: a particular association. Cardiol Res Pract 2020:2617970. https://doi.org/10.1155/2020/2617970
Wang Q, Hui H, Guo Z, Zhang W, Hu Y, He T, Tai Y, Peng P, Wang L (2013) ADAR1 regulates ARHGAP26 gene expression through RNA editing by disrupting miR-30b-3p and miR-573 binding. RNA 19(11):1525–1536. https://doi.org/10.1261/rna.041533.113
Wangxia LV, Fang Y, Liu Y, Zhao Y, Shi Z, Zhong H (2019) Circular RNA ARHGAP26 is over-expressed and its downregulation inhibits cell proliferation and promotes cell apoptosis in gastric cancer cells. Saudi J Gastroenterol 25(2):119–125. https://doi.org/10.4103/sjg.SJG_283_18
Acknowledgements
The present study is a secondary data analysis. The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. We acknowledge the NIH GWAS Data Repository, the Contributing Investigator(s) who contributed the phenotype data and DNA samples from his/her original study, and the primary funding organization that supported the contributing study “National Institute on Aging—Late Onset Alzheimer's Disease Family Study: Genome-Wide Association Study for Susceptibility Loci”. The case control data used for the validation analysis were obtained from dbGaP at http://www.ncbi.nlm.nih.gov/sites/entrez?Db=gap through dbGaP accession number: phs000496.v1.p1—The Columbia University Study of Caribbean Hispanics with Familial and Sporadic Late Onset Alzheimer's disease. Assistance with phenotype harmonization and genotype cleaning, as well as with general study coordination, was provided by Genetic Consortium for Late Onset Alzheimer’s Disease. The family-based dataset used for analyses described in this manuscript was obtained from dbGaP at http://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000168.v2.p2. The authors also thank the support of School of Nursing, West Virginia University.
Funding
The original study and ADNI was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12–2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). Funding support for the Genetic Consortium for Late Onset Alzheimer’s Disease was provided through the Division of Neuroscience, NIA. The Genetic Consortium for Late Onset Alzheimer’s Disease includes a genome-wide association study funded as part of the Division of Neuroscience, NIA.
Author information
Authors and Affiliations
Consortia
Contributions
KW and CX contributed to design, data management, and statistical analysis, drafted and reviewed statistical methods. YL, DFM, and DX managed the literature searches, added references, and drafted part of the manuscript. All authors were involved in a substantive review of the manuscript. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
All participants signed informed consent in the original studies. There was an Institutional Review Board exemption for current study due to secondary data analysis.
Consent for Publication
Consent for publication was obtained from the participants in the original studies.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, K., Lu, Y., Morrow, D.F. et al. Associations of ARHGAP26 Polymorphisms with Alzheimer’s Disease and Cardiovascular Disease. J Mol Neurosci 72, 1085–1097 (2022). https://doi.org/10.1007/s12031-022-01972-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-022-01972-5