Abstract
Muscular dystrophies encompass a wide and heterogeneous subset of hereditary myopathies that manifest by the structural or functional abnormalities in the skeletal muscle. Some pathogenic mutations induce a dysfunction or loss of proteins that are critical for the stability of muscle cells, leading to progressive muscle degradation and weakening. Several studies have well-established cognitive deficits in muscular dystrophies which are mainly due to the disruption of brain-specific expression of affected muscle proteins. We provide a comprehensive overview of the types of muscular dystrophies that are accompanied by intellectual disability by detailed consulting of the main libraries. The current paper focuses on the clinical and molecular evidence about Duchenne, congenital, limb-girdle, and facioscapulohumeral muscular dystrophies as well as myotonic dystrophies. Because these syndromes impose a heavy burden of psychological and financial problems on patients, their families, and the health care community, a thorough examination is necessary to perform timely psychological and medical interventions and thus improve the quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuromuscular disorders (NMDs) encompass a broad group of progressive diseases affecting the nervous and muscular systems. NMDs are divided into several types according to the disease mechanism, incidence, inheritance pattern, and disease progression: myopathy, neuropathy, and neuromuscular junction (NMJ) disorders (Laing 2012). Encephalomyopathies refer to a hereditary and syndromic group of NMDs that mainly affect the muscular and central nervous system (CNS). The hallmark of them is myopathy with an altered mental state that can range from mild to severe (Darin and Tulinius 2000).
Generally, myopathies include various types that can be caused by inherited or metabolic disorders, endocrine disruption, infections, connective tissue diseases, toxic substances, or secondary to other agents (Peristeri et al. 2020). One of the most common hereditary myopathies is muscular dystrophy, determined by muscle tissue destruction and weakness, leading to different levels of dystrophy and fibrosis. Indeed, it is a group of hereditary diseases in which the voluntary muscles are gradually weakened and eventually lose the ability to performing activities such as sitting and walking. On the other hand, having such disabilities will impose the patients and their relatives on high costs and difficulties (Konstantelou et al. 2019).
Different types of muscular dystrophies are known, all of which have almost the same pathological findings. These types are distinguished from each other by the age of onset, the pattern of muscle infirmity, the grade of weakness, and their inheritance pattern. Nevertheless, due to the complexity of symptoms and the similarity of signs in the various types, a conclusive diagnosis is difficult (Zivkovic and Clemens 2015; Shieh 2013). Diagnosis of muscular dystrophies is possible through careful examination of clinical signs, family history for the disease and other muscle disorders, laboratory tests (such as serum creatine phosphokinase (CPK) measurement), electromyography, muscle biopsy, and genetic tests. Gene mutations and disturbances in proteins, mainly present in muscles, are the cause of the symptoms. The hereditary pattern varies from one type of disease to another and can be autosomal, X-linked, or mitochondrial. Therefore, a thorough examination of patients helps to understand the heredity as well as diagnosis of disease (Wicklund 2013; Rojas-Marcos 2019; Sewry 2010).
Thousands of proteins are required to maintain muscle cell function, and many genes are implicated in the production of these proteins. Muscular dystrophies are the consequences of genetic defects that lead to the loss or alteration of proteins vital to muscle function. Due to the different genetic backgrounds of muscular dystrophies, their clinical presentations are also different. There is a group of inherited and syndromic diseases characterized by muscular dystrophy concomitant with intellectual disability (ID) in the patient (Mohamadian et al. 2020). Intellectual disability, previously recognized as mental retardation, is characterized as having an IQ less than usual, onset age under 18 years, and impairment in adaptive skills where adaptive skills are behaviors that are usually expected from a person at any age. Based on the intelligence test and clinical examination, the severity of ID is ranged from mild to severe (Parsamanesh et al. 2019). Several studies have considered cognitive problems as a subset of CNS involvement in NMDs. It is well known that these syndromes enforced a heavy load of financial and psychological issues on the patients and their families and health care society. Therefore, early diagnosis of these patients is indispensable in applying psychological and medical interventions and subsequently modifying the quality of life. In this review, we have scrutinized the clinical and molecular evidence of these syndromes and summarized the assigned CNS involvements in Table 1.
CMD
The congenital muscular dystrophies consist a clinically and genetically heterogeneous group (Sanga et al. 2021). The incidence of Congenital muscular dystrophies (CMDs) is not well acknowledged, and it is approximately in the range of 1/100,000 individuals (Mercuri et al. 2009). CMD is characterized by the early onset of muscle weakness, hypotonia, and joint contractures appearing in infancy or before the first year after birth. CMD is one of the most common childhood dystrophies, discerned by autosomal recessive inheritance. Brain defects with or without mental retardation are seen in some cases (Butterfield 2019). Clinically, three types of CMD in combination with brain abnormalities have been identified. In all of them, a defect in O-glycosylation of α-dystroglycan leads to a reduction in binding of the α-dystroglycan-laminin complex to the extracellular matrix. Hence, these conditions are called muscular dystrophy-dystroglycanopathy (MDDG) syndromes. Moreover, new and lesser-known CMD forms including SYNE1-related CMDs and CHKB-related myopathies have been identified in association with severe mental disability (Mitsuhashi et al. 2011; Voit et al. 2007). Various forms of MDDG syndromes are created by the mutation in the DAG1 gene encoding α-dystroglycan and β-dystroglycan or 17 other genetic loci involved in the glycosylation pathway (Tonekaboni 2016; Paprocka et al. 2021). In the MDDG syndromes, the main cerebral pathological finding is neuronal migration anomalies, followed by a specific type of evolutionary monster known as the Cobblestone complex (Astrea et al. 2016). One multicentric research conducted by Mercuri et al. on 81 Italian patients with CMD as well as reduced level of alpha-DG in muscle biopsy found the prevalence rate of pathogenic variants in the following six genes; POMT1 (protein o-mannosyltransferase 1), POMT2 (protein O-mannosyltransferase 2), POMGnT1 (protein O-linked-mannose beta-1,2-N-acetylglucosaminyltransferase), FKRP (fukutin-related protein), FKTN (fukutin), and LARGE (acetylglucosaminyltransferase-like protein). POMT1 mutations were the most common in the study, followed by POMT2, POMGnT1, and FKRP. FUKUTIN and LARGE gene mutations were only found in one patient each. Moreover, a range of brain MRI findings is reported in the patients (Mercuri et al. 2009). Also, Messina et al. examined the ID and systemic brain involvements in CMD patients. The results indicated that cognitive impairment was not always dependent on the reduced α-DG or laminin α2 or structural brain changes (Messina et al. 2010). Evaluation of a large group of Chinese patients with MDDG syndrome showed that mutations in FKRP (the most common mutation) induce milder phenotypes while the POMGNT1 mutations are associated with severe phenotypes. The mental delay was a clinical manifestation related to mutations of the POMT1 gene (Song et al. 2020). On the other hand, Maroofian et al. stated that mutations in B3GALNT2 can cause a novel type of MDDG syndrome characterized by mental retardation and seizure, but without any evident muscular involvement (Maroofian et al. 2017). About two-thirds of congenital disorders of glycosylation are associated with intellectual disabilities (Wolfe and Krasnewich 2013). Generally, similar pathological evidence shared by animal models of dystroglycanopathy consisting of fukutin chimera, FKRP-NeoY307N, POMGnT1-null, LARGEmyd, and MORE-DG null mice suggests that appropriate α-DG glycosylation is indispensable for corticogenesis (Chan et al. 2010). Also, neurological phenotypes presented by LARGE knockout mice propose that a LARGE deficiency in the hippocampus leads to abnormal amplification of stimulatory synapses through AMPA-type glutamate receptor overload, thereby weakening hippocampal-dependent memory (Seo et al. 2018).
FCMD
Fukuyama congenital muscular dystrophy was first described in 1960 by Fukuyama (Fukuyama 1960). Fukuyama congenital muscular dystrophy (FCMD) is a rare inherited disease with an autosomal recessive inheritance pattern. After Duchenne muscular dystrophy (DMD), FCMD is the most prevalent CMD in Japan. Despite the incidence of 2–4 per 100,000 Japanese infants, Fukuyama is not common in other countries. Hypotonia and generalized muscle weakness occur before the age of 9 months (Reed 2009). In 50% of the affected infants, the power of crying and sucking has been severely reduced. Contracture in the hips, pelvic, knees, or interphalangeal joints is a decisive pathological finding. Although these children may have no problem sitting, they will never be able to walk. The most common complications of cortical dysplasia are seizures and epilepsy, which occur in 50–80% of children aged 1 to 6 years (Yoshioka and Higuchi 2005). After the age of 6, the children’s motor problems progress rapidly until they die in the early years of puberty. Progressive respiratory failure and cardiac dysfunction are the most common causes of death in FCMD patients and generally appear in the second decade of life (Ishigaki et al. 2018). The intense mental delay and speech disturbance are presented in all patients (IQ 30–60). Ocular abnormalities such as myopia, hypermetropia, cataracts, and retinal detachment are also seen in Fukuyama patients. Furthermore, almost 30% of the patients suffered from insomnia (Falsaperla et al. 2016; Mattos et al. 2021). In laboratory studies of the FCMD patients, an increase in the serum CK enzyme, as well as myopathic findings on electromyography, is noteworthy (Astrea et al. 2016). Given the poor prognosis as well as a higher prevalence of FCMD in Japan, prenatal diagnosis is performed in Japanese families by haplotype analysis using microsatellite markers (Saito 2006). Yang et al. reported three Chinese FCMD patients with mental retardation, motor developmental delay, muscle weakness, febrile convulsions, increased levels of serum CK, and a 3-kb insertion in the 3′ untranslated region of FKTN. Moreover, micropolygyria and extensive dysplasia in the white matter and brainstem were evident in brain MRI of the patients. Two heterozygous nonsense mutations in FKTN including c.139C > T (p.Arg47 ∗) and c.346C > T (p.Gln116 ∗) are also detected (Yang et al. 2015). Kobayashi and collaborators have also found the same 3-kb-retrotransposal insertion into the 3′ UTR of the FKTN gene (founder mutation) in the general Japanese population with a frequency of 1 in 88 (Kobayashi et al. 1998). However, Silan et al. have reported one Turkish individual with FCMD that had a homozygous mutation, 1-bp insertion mutation in exon 5 of the FKTN gene, other than the founder mutation that was reported previously (Silan et al. 2003).
Neuroimaging and necropsy show brain abnormalities like pachygyria, polymicrogyria, and agyria in Fukuyama patients. Commonly, small amounts of normal brain tissue appear in the temporal-occipital regions of the patients (Reed 2009; Silfeler et al. 2012). The genetic basis of FCMD is established on mutation in the FKTN gene on chromosome locus 9q31-q33, affecting the fukutin protein of the basal membrane. Fukutin is mainly expressed in neurons and its deficiency prevents accurate glycosylation of α-dystroglycan, thereby disturbing the migration of neurons during brain development. Researchers believe that a defect in the migration of nerve cells causes a brain disorder called lissencephaly, in which the brain surface does not appear to have any groove (Saito and Matsumura 2011). Disturbances in cortical lamination and architecture can eventually lead to intellectual disability and severe learning disabilities. Moreover, Fukutin is also expressed in glial cells, suggesting a role in the integrity of the glial limitans (D’Angelo and Bresolin 2006). A fukutin-deficient chimeric mouse shows that despite the defects in the basal lamina of the cortex, no change in neuronal migration is observed (Takeda et al. 2003). It seems that the loss of interaction between hypoglycosylated α-dystroglycan and its ligand cause basal lamina dysfunction and subsequent cortical dysplasia in FCMD (Chiyonobu et al. 2005).
MEB
Muscle-eye-brain disease (OMIM no. 253280) or MDDG-3A is an autosomal recessive disorder that was first reported by Santavuori in 1978. The earlier clinical signs of muscle-eye-brain disease (MEB) include neonatal hypotonia and severe developmental delay which present at birth or in the first few months of life (Santavuori et al. 1977). In most cases, walking is delayed until the age of 4. In the second decade of life, muscle stiffness, joint freezing, and gait disturbance appear. Visual deterioration consists of severe myopia followed by retinal detachment, and cataracts are some complications of the MEB. Furthermore, a few patients have a neurological speech impairment (Taniguchi et al. 2003). CNS dysgenesis, including lissencephaly type II or pachygyria, and micropoligyria of occipital lobes, has been frequently observed in MEB patients (Falsaperla et al. 2016; Natarajan and Ionita 2018). Commonly, creatine kinase level elevates since the first year of life, and electromyography (EMG) shows myopathy. Autosomal recessive mutations in the POMGNT1 gene are involved in the development of the MEB condition, but over time, other reported dystroglycanopathies have been linked with MEB (Clement et al. 2008; Mercuri et al. 2006; Godfrey et al. 2007). POMGnT1 glycosyltransferase catalyzes the transfer of N-acetylglucosamine to O-linked mannose of α-dystroglycan. Twenty-four different mutations in the POMGnT1 gene have been identified in patients with MEB that the mutations did not occur at a hot spot (Diesen et al. 2004). Taniguchi et al. described the universal distribution and a broader phenotype range of MEB disease. They found that rather extreme brain signs, such as hydrocephalus, are seen in patients with mutations near the 5′end of the POMGnT1 gene, whereas patients with mutations near the 3′ end have slighter brain involvement (Taniguchi et al. 2003). Biancheri et al. demonstrated a genotype–phenotype correlation in MEB and increased our understanding of the clinical range associated with POMGnT1 mutations (Biancheri et al. 2006). Even in the same family, POMGnT1 mutations can cause MEB disease with various phenotypes (Teber et al. 2008).
The MEB has been considered to be confined to the Finnish population for several years. In Finland, The incidence of MEB is nearly 1/100,000 live birth while the carrier frequency of the founder mutation is anticipated to be 1/60 (Diesen et al. 2004; Kano et al. 2002). The Finnish founder mutation (c.1539 + 1G˃A (p.Leu472_His513del)) was introduced in 2004 as a causative variant of MEB. This splice site pathogenic variation induces premature stop codon (PTC) which leads to the deletion of 42 amino acids (De La Chapelle and Wright 1998). Arvio et al. described two middle-aged women carrying the Finnish variant of POMGnT1 with severe cognitive and motor disability, visual deficits, limited communication skills, epilepsy, recurrent bowel obstructions, and joint contracture (Arvio et al. 2019). Borizovna et al. reported compound heterozygous mutations in the POMGNT1 gene (c.1539 + 1G > A and c.385C > T) in a 6-year-old boy presenting MEB clinical characteristics by whole exome sequencing (WES) technique (Borisovna et al. 2019). The molecular diagnosis was still followed by clarifying new POMGnT1 mutations related to MEB in non-Finnish individuals as well as patients with new phenotypes, such as retained vision. An alternative study manifested a minor association between the position of the mutation and clinical significance. It highlighted the need to recognize POMGnT1 mutations of not just non-Finnish MEB-like individuals and in patients with Walker-Warburg syndrome (WWS) or even other CMDs worldwide (Taniguchi et al. 2003; Biancheri et al. 2006). All of the gene mutations reported in POMGnT1 result in a complete deficiency of enzyme function and are not associated with phenotype intensity (Hehr et al. 2007). De Bernabé described a patient with a phenotype of MEB disorder and a mutation in the FKRP gene. Mutations in the FKRP gene, which also occur in WWS, are likely to affect glycosyltransferase function (De Bernabé et al. 2004). As discussed in previous sections, O-mannosyl glycan is critical for the binding of α-dystroglycan and laminin. Hence, an inappropriate O-mannosylation resulted from defective POMGnT1 may disrupt the sarcolemmal linkage of skeletal muscle and migration of neuronal cells, as well (Yoshida et al. 2001). This could be a suggested pathophysiological pathway for the myopathic and cognitive manifestations assigned to MEB. Induction of dystrophic phenotype by an antibody blocking the interaction of α-dystroglycan and laminin (Brown et al. 1999), as well as weaker immunostaining of the laminin α2 chain in MEB muscles (Auranen et al. 2000), supports this.
WWS
The syndrome was first reported in 1942 by Walker, and years later in 1978, it was reported by Warburg as well (Walker 1942; Warburg 1978). The Walker-Warburg syndrome (OMIM no. 236670) is a rare disorder with a worldwide spread; the total prevalence is uncertain. A prevalence rate of 1.2 per 100,000 live births was recorded in a survey in northeastern Italy (Mostacciuolo et al. 1996). Unlike the FCMD and MEB, this syndrome is not limited to a specific race. The most frequent symptoms of WWS are severe cerebral abnormalities characterized by hydrocephalus, type II lissencephaly, occipital encephalocele, the fusion of two cerebral hemispheres, lack of corpus callosum, and cerebellar hypoplasia (Falsaperla et al. 2016). Children with WWS show different degrees of intellectual disability and often experience seizures. Ocular abnormalities consisting of congenital cataracts, microphthalmia, and buphthalmos have been observed in the patients. Affected children are blind at birth and suffer from severe hypotonia, a condition known as “floppy infant syndrome”(Barkovich 1998). Increased serum levels of CK and various abnormalities found in muscle biopsy indicate myopathy in these children. All patients suffer from severe mental and physical retardation and do not live for over 4 months (Suthar et al. 2018). WWS is highly heterogeneous, and so far, pathogenic changes in at least 14 genes have been attributed to its pathogenesis. At first, mutations in the most common genes including POMT1, POMT2, ISPD, FKTN, FKRP, and LARGE1 were discovered. Some of them are still unknown and are thought to be involved in the progression of the disease (Tuuli and Odibo 2017). de Bernabé et al. unraveled the WWS genetically by performing genome-wide linkage analysis followed by homozygosity mapping in 15 consanguineous families with WWS. Of thirty individuals examined, just six (20%) carried POMT1 mutations. In this study, a total of five POMT1 mutations in five families were identified (de Bernabé et al. 2002). Later, Currier et al. reported POMT1 mutations in only 2 of 30 patients with classic WWS. Linkage analysis in six consanguineous families exhibited 100% heterozygosity as well as negative LOD scores at the POMT1 region. So, the incidence of WWS-related POMT1 mutations can change in different populations (Currier et al. 2005). Van Reeuwijk registered a homozygous 63-kb intragenic deletion in the LARGE gene in a patient with familial WWS characterized by CMD, severe mental retardation, and eye abnormalities. Evidence suggests that mutations in the LARGE gene, like other genes involved in post-translational modification of α-dystroglycan, can lead to a broad clinical range (van Reeuwijk et al. 2007). Using the gene knockdown technique in zebrafish, Roscioli et al. identified WWS-causing mutations in the isoprenoid synthase domain-containing (ISPD) gene that are associated with faulty glycosylation of \(\alpha\)-dystroglycan (Roscioli et al. 2012) Although ISPD is the first WWS-related gene without any suggested glycosyltransferase activity, it is directly involved in the glycosylation pathway. Almost 32 CMD patients with severe CNS involvement carrying ISPD mutations have been reported in the literature (Gençpınar et al. 2019). Besides, de Bernabé et al. nominated the FKTN gene in the pathogenesis of WWS in one Turkish patient in whom a homozygous nonsense mutation of FKTN leads to a complete loss of protein function (de Bernabé et al. 2003). After that, Manzini et al. recorded novel mutations in POMT1, POMT2, FKTN (FCMD), and FKRP in 40% of WWS patients from different ethnicities. Among the patients participating in this cohort, mutations in the FKTN gene were more frequent in the European/American group compared to what was previously expected with the same founder mutation (Chiara Manzini et al. 2008). Besides this, uncommon genomic deletions or deletion/insertions in POMT2 were identified in other studies (Yanagisawa et al. 2009) . Van Reeuwijk et al. described a family with two siblings carrying a homozygous variation in the starting codon of the FKRP gene which is likely to cause protein loss, resulting in WWS (Van Reeuwijk et al. 2010). After that, a limited number of patients with the WWS phenotype carrying the FKRP mutations have been reported (de Bernabé et al. 2002).
All known genes involved in the pathogenesis of WWS are molecules modulating glycosylation and appear to be involved in the neural cell interactions (Spalice et al. 2009). Selective deletion of dystroglycan in the brain of mice is merely sufficient for the development of CMD-like brain abnormalities. In the mice, the high affinity to laminin-binding is also lost, and discontinuities are evident in the glia limitans. These events are thought to be a prelude to the onset of neural migration errors. Additionally, the mutant mice showed blunted hippocampal long-term potentiation (LTP) that suggests a possible postsynaptic mechanism of dystroglycan in learning and memory (Vajsar and Schachter 2006). In this regard, Moore et al. showed that some of the brain abnormalities observed in the WWS, such as excessive neural migration and fusion of the cerebral hemispheres, result from a brain-specific disturbance of α-dystroglycan glycosylation during mouse embryonic development (Moore et al. 2002). Therefore, dystroglycan complex defects are crucial to the pathogenesis of functional and structural brain abnormalities seen in WWS. Other possible targets of O-mannosylation in the brain are reelin and tenascin-J, which may be responsible for the development of WWS symptoms (Hirotsune et al. 1995; Lochter et al. 1991). These glycoproteins are influential factors in brain development. Reelin is secreted by Cajal-Retzius cells and other pioneer neurons and is involved in lissencephaly and cerebellar hypoplasia (Hong et al. 2000), while Tenascin-J1 plays an inhibitory role in neurite extension (Roll and Faissner 2019).
LGMD
Limb-girdle muscular dystrophy (LGMD) is a term used to refer to a group of diseases that involve the proximal muscles, especially shoulder muscles, above the arm, the pelvic region, and the thighs. The general occurrence of LGMD worldwide has been 1 in 14,500–45,000 individuals (Murphy and Straub 2015; Norwood et al. 2009). The severity and age of onset are varied among subtypes and may be contradictory even among members of a family. Based on the new genetic criteria, LGMD is categorized as autosomal dominant (LGMD 1A-H) and autosomal recessive (LGMD 2A-Z). Recessive forms constitute almost 90% of LGMD cases, and among them, LGMD2A (Calpainopathies) is the most common. To date, about 50 genetic loci associated with LGMD forms have been identified. When ID accompanies LGMD, differential diagnosis of LGMD is more superficial because all conditions included in the subtype are dystroglycanopathy syndromes or MDDGs with autosomal recessive heredity (Wicklund 2019).
LGMD2K
LGMD2K (also known as MDDGC1) (OMIM no. 609308) is characterized by slow progression of the proximal muscle infirmity. Commonly, the onset age of LGMD2K is 1 to 6 years. CNS abnormalities appearing as microcephaly and/or mental delay (IQ 50 to 76) are reported in 60% of cases. Furthermore, the serum CK level is highly increased in these patients (Cirak et al. 2006). LGMD2K is allelic with WWS, and homozygous or compound heterozygous missense mutations in the POMT1 gene on 9q34.13 locus are known to cause the disease (Angelini 2017). The POMT1 protein has six loops, in which loops one, three, and five are located in the endoplasmic reticulum (ER) lumen, and the remaining loops are situated within the cytoplasm. Milder LGMD phenotypes are likely to be associated with mutations involving only the cytoplasmic loops. Conversely, the most severe clinical presentations of CMD are caused by pathogenic mutations in loop one and loop five inside the ER lumen (Wallace et al. 2014). Balci and colleagues reported five Turkish patients diagnosed with LGMD2K, mild intellectual disability, and normal brain MRI. Their findings showed that all patients carried p. Ala200Pro pathogenic variant in the POMT1 gene, an ancestral founder mutation affecting glycosylation of α-dystroglycan (Balci et al. 2005). Bello et al. described two patients affected by a novel phenotype of LGMD, one with a normal cognitive profile and the other with mild cognitive impairment. Both patients carried compound heterozygous POMT1 mutations and manifested dilated cardiomyopathy and reduced myocardial contractile force (Bello et al. 2012). Also, YİÇ and co-workers have studied the epidemiology of the genetic and clinical characteristics of childhood-initiated LGMDs in a part of the Turkish population. Out of 56 pediatric cases with LGMD, three patients (5%) suffered from generalized muscular hypertrophy, mild microcephaly, and intellectual disability. The whole-exome sequencing revealed two pathogenic missense variants (p.A647T, p.A647T) in the POMT1 gene of these patients (Yİş et al. 2018). POMT1 gene encoding O-mannosyltransferase 1 catalyzes the initial step in the O-mannosyl glycan synthesis. The highest tissue expression of POMT1 is in the adult testis, cardiac and skeletal muscles, and fetal brain (Jurado et al. 1999). POMT1is involved in the synthesis of the motif “Galb1 4GlcNAcb1 2Man-O-Ser/Thr” or O-mannose–linked core, which is present in all of the O-mannose–linked glycans. Furthermore, it seems that the phenotype associated with POMT1 mutations can be expected to be more severe than other glycosyltransferases. Neuromuscular phenotypes resulting from POMT1 mutations are likely to be mediated by the reduction or absence of O-mannosylation of target proteins that have basic functions in development (de Bernabé et al. 2002). Lack of O-mannosyl glycans is likely to prevent the natural interaction between a-dystroglycan and laminin-a2, thereby reducing the α-dystroglycan stability. Consequently, the binding of a-dystroglycan to the extracellular matrix is lost, paving the way for muscle weakness as well as neuronal migration disorders (Brown et al. 1999).
LGMD2N
LGMD type 2 N is an uncommon form of recessive LGMDs caused by pathogenic variants in the POMT2 gene. The causative gene is located on cytogenetic location 14q24.3 and contains 21 exons. POMT2 encodes another putative O-mannosyltransferase whose expression pattern overlaps with that described for POMT1 (Clement et al. 2008). So far, few patients with LGMD type 2 N (LGMD2N) are reported. Physical examination of the patients exhibits hypertrophy of calf muscles, mild-to-moderate proximal muscle weakness, and mild intellectual disability (Biancheri et al. 2007). In addition, delayed walking and increased serum creatine kinase level are the common features. Defects on echocardiograms have been seen in some cases (Angelini 2017). Biancheri et al. identified a missense mutation in the POMT2 gene in a 5-year-old Italian girl with a mild LGMD phenotype, increased CK serum levels, reduced muscle weakness, and lack of any brain involvement. The muscle biopsy showed an intense decrease in the α-dystroglycan (Biancheri et al. 2007). Saredi et al. reported two pathogenic mutations in the POMT2 gene, including a null and a missense, in a patient affected by a mild phenotype of LGMD with intellectual disability. The patient presents minor histopathological features and reduction of α-dystroglycan glycosylation, without any ocular or brain involvement (Saredi et al. 2014). Ostergaard and colleagues studied the specific clinical features in a cohort of LGMD2N patients. They found that all patients had mental retardation, unlike the other recessive LGMDs. Furthermore, the age of disease onset was in a wide range, and hamstring, paraspinal, and gluteal muscle involvement were found on MRI. The study found 11 novel POMT2 mutations associated with LGMD2N (Østergaard et al. 2018). Hu et al. induced a brain-specific deletion of POMT2 to investigate the role of O-mannosylation in brain development. POMT2 deficiency leads to the α-DG hypoglycosylation and loss of its binding to the pial basement membrane. This disruption underlies brain malformations such as overmigration of neocortical neurons as well as failure in the granule cell migration. The complications of POMT2 removal on brain development were time-dependent, meaning that earlier deletions led to more severe phenotypes (Hu et al. 2011). Since about one-third of the brain’s O-linked glycans are O-linked mannosyl glycans, POMT2 function in neural tissue is necessary for normal brain development (Kogelberg et al. 2001).
LGMD2T
LGMD type 2 T (OMIM no. 615352) is characterized by hypotonia, microcephaly, mild weakness of limb and proximal muscles followed by delayed gait. The onset age of the condition is from infancy to early childhood. Learning difficulties in the form of mild intellectual disability have been revealed in half of the patients. Additional manifestations consist of epilepsy, cardiomyopathy, cataracts, and respiratory defects exhibited in some patients (Topaloglu 2018). Carss et al. first reported mutations in guanosine diphosphate mannose (GDP-mannose) pyrophosphorylase B (GMPPB) resulting in decreased α-DG glycosylation in muscle biopsies of three unrelated LGMD patients from Indian, English, and Egyptian ethnicities. However, only the Indian and Egyptian patients showed mental retardation delay and epilepsy. Three patients had raised CK serum levels and dystrophic injuries on muscle biopsy (Carss et al. 2013). The GMPPB gene is located on 3p21 and comprises eight exons in the 1.7-kb mRNA (Tian et al. 2019; Angelini 2017). The clinical spectrum of the GMPPB mutations is extremely heterogeneous, ranges from LGMD type 2 T (LGMD2T) to congenital myasthenic syndromes (CMS), to severe CMD with ocular and brain involvement (WWS, MEB) (Montagnese et al. 2017). Sarkozy et al. reported eight patients presented with an LGMD phenotype and pathogenic variations assigned to GMPPB. Their findings expanded the phenotypic spectrum of GMPPB mutations by reporting a 13-year-old patient with impaired cognitive function and raised CK (Sarkozy et al. 2018). Jensen BS. et al. collected the clinical and pathological findings of nine unrelated patients with compound heterozygous variants in GMPPB ranging from LGMD to CMD. Five patients had clear evidence of LGMD, of which only one 20-year-old girl with moderate restrictive lung disease, sensorineural hearing loss, developed scoliosis, and muscle weakness has moderate to severe intellectual disability (Jensen et al. 2015). Oestergaard et al. found a preferential involvement of hamstring and paraspinal muscles in six patients with LGMD2T who carried GMPPB mutations. Variable loss of α-dystroglycan glycosylation was also seen in the patients. According to their study, the prevalence of LGMD2T in Denmark was estimated at 1.5% (Oestergaard et al. 2016). GMPPB enzyme provides GDP-mannose, a substrate for the N-glycosylation, O-mannosylation, and C-mannosylation pathways, as well as glycosylphosphatidylinositol (GPI)-anchor formation (Rodríguez Cruz et al. 2016). More than 50 mutations in the GMPPB gene have been reported till now, most of which are missense. Mutations in the catalytic domain of GMPPB are more destructive, and people carrying these variants present more severe phenotypes (Liu et al. 2021). Zheng et al. showed that knocking down of GMPPB in the zebrafish model resulted in scattered and irregular muscle fibers as well as shortening of caudal primary (CaP) motor neurons. They also found that both muscle and neuronal impairments could be efficiently recovered by the injection of wild-type GMPPB (Zheng et al. 2021). Recently, Wingo et al. conducted a proteome-wide association study of depression through integrating genome-wide association study (GWAS) findings with human brain proteomes. They identified GMPPB as one of 19 genes involved in depression pathogenesis through modulating the abundance of the brain protein (Wingo et al. 2021).
DMD
Duchenne muscular dystrophy (OMIM no. 310200) is a lethal recessive X linked (Xp21.2) disease and the most common subtype of childhood muscular dystrophies (MDs) (1/3500 live-born males) (Wicklund 2013). Dystrophin is a 427-kDa cytoskeletal protein, which along with its 11 binding partners is organized as a dystrophin-associated protein complex (DAPC) (Tadayoni et al. 2012). Dystrophin deficiency leads to the disassembly of DAPC and loss of interaction between F-actin and the extracellular matrix. Since the DAPC plays significant mechanical and signaling roles in strengthening and maintaining muscle fibers, detachment of DAPC components is followed by irreparable consequences on muscle cell function (Duan et al. 2021). Although dystrophin is found mainly in skeletal and cardiac muscles, it is also present in other tissues and the CNS, mostly in the cerebellum, hippocampus, and neocortex (Peristeri et al. 2020). In DMD, frameshifting or nonsense mutations in the dystrophin gene lead to the prematurely terminated protein, resulting in non-functional and unstable dystrophin (Crisafulli et al. 2020). DMD patients appear to be normal at birth; however, independent walking and difficulty standing on surfaces become apparent in early childhood (18 months). Afterward, at 4 years of age, proximal hip muscle weakness has emerged (Gowers’ sign). The notable clinical characteristics of DMD are motor delay and gait disturbances, including flat feet, deterioration of motor skills, a loss of physical endurance, and much more frequent falls. In the second decade, boys are often inbounded to wheelchairs. The intensity and onset-age of cardiomyopathy differ and are unrelated to the dystrophin gene mutations. Respiratory muscles are affected by fibrosis, which leads to respiratory failure (Bresolin et al. 1994; Waldrop and Flanigan 2019). Delays in language learning and cognitive function were also reported (Peristeri et al. 2020). Often, death is a consequence of cardiac or respiratory failure in DMD patients (Nardes et al. 2012; Rasic et al. 2014; Banihani et al. 2015a). Clinical characteristics and elevated plasma CPK are critical for the diagnosis (Anaya-Segura et al. 2015).
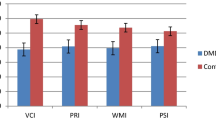
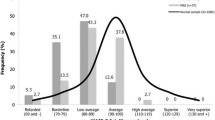
Although most boys with DMD are not intellectually disabled, non-progressive CNS manifestations are well described in some of them. A decrease in full-scale intelligence quotient (FSIQ) compared with the population’s mean is a consistent finding in DMD patients (Banihani et al. 2015b). In around 30.0% of patients with FSIQ less than 70, ID has been reported and approximately 3.0% of them are affected by severe impairment with FSIQ less than 50. Overall, 44% of DMD patients showed evidence of learning disabilities. Moreover, increased risk of neurobehavioral comorbidities like attention-deficit hyperactivity disorder (ADHD), epilepsy, anxiety, and autism spectrum disorders (ASD) have been reported in DMD patients (Parisi et al. 2018). It seems that a genotype–phenotype association provides a partial explanation for the cognitive differences between patients (Doorenweerd 2020). According to research by Ricotti et al., patients with distal mutations in the DMD gene were more likely to have neurodevelopmental problems, intellectual disability, memory deficits, and decreased gray matter volume and cerebral perfusion. However, emotional and behavioral problems were equally distributed in patients carrying proximal or distal mutations. There was no clear genotype–phenotype association between neuroimaging findings and learning/behavioral problems (Ricotti et al. 2016). Individuals with DMD mutations are indicated to have learning disabilities that are qualitatively similar to subjects with developmental dyslexia. In these patients, specific reading and writing problems and reducing the speed of rapid automated naming (RAN) have been found to cause phonological processing problems. About 40% of the patients have been identified as having difficulty reading, as well as deficiencies in phonological awareness/processing and short-term memory (Astrea et al. 2015). Mochizuki et al. evaluated intelligence quotient (IQ) in 74 Japanese DMD patients and followed them over a period of 12 years. The patients with an IQ below 70 (38%) were found to start walking later, need to ventilator and tube nutrition earlier, and died earlier than patients with normal intelligence (Mochizuki et al. 2008). The main pathophysiological mechanisms underlying cognitive deficits in DMD attributed to various dystrophin isoforms, the involvement of dystrophin in embryonic development, and the interaction between genes and non-genetic agents. Different transcripts of the dystrophin gene are expressed from three upstream and four internal promotors. Dystrophin protein 71 (Dp71) is an alternatively spliced transcript and the most predominant isoform in non-muscular tissues, especially the brain. In the brain, Dp71 is involved in neuronal differentiation, cell division, nuclear scaffolding, DNA repair, and organization of excitatory synapses (Naidoo and Anthony 2020). Previous studies on Dp71-null mice have revealed that Dp71 regulates the postsynaptic nerve terminal’s active zone morphology and glutamate receptor composition in the postsynaptic density (Banihani et al. 2014). According to recent evidence, it is likely that intellectual deficiency is the consequence of the combined loss of Dp71, Dp140, and Dp427, while the loss of Dp71 adds to the seriousness of cognitive impairment (Naidoo and Anthony 2020). Rasic et al. determined the frequency of cognitive impairment and its association with dystrophin mutations in Serbian DMD patients. About 40% of patients had some degrees of mental retardation, among those who had mutations affecting Dp140, Dp71, and Dp40 isoforms of dystrophin were associated with recurrent and more severe cognitive deficits (Rasic et al. 2014). Loss of Dp427 is potentially associated with emotional and behavioral problems that could be due to misplaced signaling receptors in neurons, preferably in the amygdala and hippocampus. In addition, the Dp140 isoform is highly expressed during development, and its essential role in neuronal differentiation has been suggested. On the other hand, evidence suggests that Dp140 and Dp71 are somehow involved in the cerebral vasculature. Although the exact relationship between this and the cognitive abilities of DMD patients is not yet known, the association of lower IQ with low cerebral perfusion in normally developing children has been established (Kilroy et al. 2011). Other studies have investigated the association between cerebellum involvement in DMD patients with speech and verbal functions. Metabolic examination of the cerebellum and the temporo-parietal region of the patients showed constant choline deficits and significant abnormalities in glutamate and N-acetyl compounds in these areas, which were related to verbal IQ and short-term verbal memory (Kreis et al. 2011). Elevated levels of choline-containing compounds are seen in several brain disorders and probably indicate an unstable increase in membrane turnover due to increased cell division or inflammation. However, there is a permanent increase in the choline compounds level in DMD, which may call into question the hypothesis of a change in membrane turnover (Anderson et al. 2002; Rae et al. 1998).
MD
Myotonic dystrophies are the most common subtype of muscular dystrophies with the onset age of adulthood. MDs are progressive and multisystemic genetic disorders that follow the autosomal dominant pattern of inheritance (Meola and Cardani 2015). Two subgroups are genetically identified: DM 1 (OMIM no. 160900) is more common and caused by an expansion of CTG trinucleotide repeat in 3′UTR of the dystrophia myotonica protein kinase (DMPK) gene where the number of repeats is greater than 50. DM 2 (OMIM no. 602668) is derived from the expansion of CCTG tetranucleotide repeat in the first intron of the nucleic acid-binding protein (CNBP) gene (formerly known as zinc finger 9 gene, ZNF9) where 75 or longer repeats have occurred (Johnson and Heatwole 2012). The number of repeats increases with age, thereby intensifying the disease over time. In DM1, the length of the CCTG expansion is directly correlated to clinical severity, while in DM2, no clear relationship was found between the two (Thornton 2014). The clinical presentation of DMs is diverse and contains myotonia, muscular dystrophy, cataracts, and cardiac conduction disorders. Additional manifestations include gastrointestinal, endocrine, respiratory, and CNS involvement. Despite the similarity of symptoms, the clinical phenotype is distinct for each subgroup (Udd and Krahe 2012). DM1 is characterized primarily by the weakness of the face and distal-predominant limb, grip myotonia without fluctuation, while DM2 is defined principally by progressive proximal and distal limb infirmity and variable mild grip myotonia. The incidence of DM is 1/3000 worldwide, while in some areas such as Quebec, it is 1/500 (Thornton 2014). The most severe form of DM1 is congenital myotonic dystrophy (CMD) which appears at birth or the first month of life and is often accompanied by evident developmental disabilities. Besides, all the patients suffer from intellectual disability along with serious learning difficulties (Zapata-Aldana et al. 2018; Stokes et al. 2019). Some studies on children with DM1 have linked the severity of cognitive dysfunctions (lower IQ score) to the number of triplet repeats tied to maternal inheritance. (Perini et al. 1999; Astrea et al. 2016). Stokes et al. evaluated 74 DM1 patients, 52 of whom had congenital form (CMD). Seventy-four percent of the cases had 143 to 2300 CTG repeats with maternal inheritance. Most patients had some form of developmental, cognitive, or behavioral problems. Cognitive impairments were evident in more than 50% of the DM1 patients, with higher occurrence in those with CMD. Speech/language delay, mood disorders, and ADHD also showed above-average rates (Stokes et al. 2019). Woo and colleagues. compared adult-onset and juvenile-onset DM1 in a cohort of 19 DM1 patients who underwent multiple neuropsychological studies. In the juvenile group, verbal intelligence and verbal memory were considerably impaired; however, in terms of performance intelligence and functional tasks, both groups were on the same level (Woo et al. 2019). In childhood-onset DM1, the first cognitive symptoms occasionally appear before the onset of muscle involvement. Additionally, these children tended to present psychopathological disorders, such as anxiety and ADHD (Udd and Krahe 2012). Structural and functional brain defects have been reported in adult-onset DM1. The most common neuropsychological symptom appears to be decreased perception skills which can be associated with some features of psychological disorders (Astrea et al. 2016). Structurally, brain MRI of DM1 patients shows different changes in white matter that are more prominent than atrophy (Goossens et al. 2000). One of the key distinctions between DM1 and DM2 seems to be CNS involvement. Cognitive deficiencies are rarely found in cases with DM2, although these are milder than in DM1(Peristeri et al. 2020; Goossens et al. 2000). The most common cognitive symptoms in DM2 include dysexecutive, visuospatial, and memory deficiencies. Additionally, sleep-related disorders, fatigue, and pain have also been reported frequently in DM2 (Peric et al. 2021). Meola et al. assessed the cognitive function of 21 DM1 and 19 DM2 patients. Cognitive deficiencies attributed to frontal lobe impairments as well as lower ID scores were noted in DM1 patients. Also, a decreased cerebral blood flow in the frontal, parietal, and temporal lobes was documented, which was related to cognitive disability (Meola et al. 1999, 2003). Since two replicate sequences in completely different genes produce largely similar traits, a common pathogenic mechanism may be involved. It is well established that the "gain-of-function RNA mechanism" is the main cause of DM pathogenesis (Lee and Cooper 2009). Intranuclear accumulation of mutant RNAs containing long repeats of (CUG)n or (CCUG)n disrupts the cellular function of two RNA-binding proteins: muscle blind like 1 (MBNL1) and CUGBP Elav-like family member 1 (CELF1), which are tissue-specific antagonist regulators of alternative splicing for hundreds of pre-mRNA targets, such as insulin receptor (INSR), troponin 2 (TNNT2), chloride channel 1 (CLCN1), ryanodine receptor (RyR1), dihydropyridine receptor (DHPR), sarco/endoplasmic reticulum Ca2 + -ATPase 1 (SERCA1), and MBNL2. So, the pathological repeats lead to downregulation of MBNL1 due to its sequestration into RNA forming ribonuclear foci as well as upregulation of CELF1 through its high stability. The main downstream effect of this deregulation is spliceopathy, which leads to the aberrant expression of embryonic isoforms in the adult tissues, underlying clinical manifestations of myotonic dystrophy (Meola 2020; López-Martínez et al. 2020). Apart from the missplicing, CELF1 and MBNL1 can also induce alterations in other processes including calcium regulation, proteostasis, non-coding RNA metabolism, and sarcomere protein localization (Ozimski et al. 2021). Another pathogenic mechanism attributed to the DM1 pathology is known as repeat-associated non-ATG (RAN) translation. RAN translation indicates AUG-independent translation of the mutant RNAs, thereby producing the expanded homopolymeric proteins (Cleary and Ranum 2013). Zu et al. observed positive immunostaining in DM1 myoblasts, skeletal muscle, and blood using antibodies against RAN poly-Gln protein. Similar staining is also shown in cardiomyocytes and leukocytes of a DM1 mouse model (Zu et al. 2011). In addition, in both humans and mice, caspases 8 and 10 are recruited into the nuclear aggregates of extended polyglutamine and provide the primary indicator of polyGln-induced apoptosis (Miyashita et al. 2001). There is strong evidence to support the importance of different signaling cascades in DM1 pathogenesis. Disruption of the protein kinase B/AKT signaling pathway in DM1 increases apoptosis, autophagy, and ubiquitin–proteasome activity. In addition, the interrupted nuclear factor κB (NFκB) pathway has been shown to be associated with inflammation in DM1(Ozimski et al. 2021).
FSHD
Facioscapulohumeral muscular dystrophy is a progressive muscular disorder with autosomal dominant inheritance. Landouzy and Dejerine first described facioscapulohumeral muscular dystrophy (FSHD) in 1884 (Landouzy and Dejerine 1884). FSHD is the third most prevalent muscular dystrophy after Duchenne and myotonic muscular dystrophy with an incidence rate of 1 in 15,000–20,000 birth (Tawil 2004). Typically, facial weakness manifests in the form of inability to completely close the eyes during sleep, transverse smile, and trouble whistling due to limited movements of the lips. Also, muscle weakness and atrophy are mainly seen as scapular winging, horizontal clavicles, and limitation in shoulder abduction and elbow flexion. The disorder develops or begins at a relatively early stage of life. Patients with a highly progressive phenotype can show rare characteristics, including a poly-hill sign, Beevor’s sign, extreme curvature, enhanced lumbar lordosis, and weakness of the hip girdle, foot extensor, and abdominal muscles (Mul et al. 2016; Mah and Chen 2018). CNS abnormalities such as cerebellar atrophy and intellectual impairments with an IQ of 25 to 50 have been reported in FSHD individuals (Zouvelou et al. 2008; Matsuzaka et al. 1986; Funakoshi et al. 1998). Grosso et al. noted that in some individuals with shorter 4q35 deletions, further muscular manifestations such as seizures, speech delay, and mental retardation may be seen. In these patients, there was no constant association between the size of the 4q35 fragment and the clinical severity of FSHD. Moreover, FSHD patients with a larger gene deletion appear to have a greater risk of displaying extreme clinical phenotypes with CNS disorders (Grosso et al. 2011). Saito et al. reported one 20-year-old girl with FSHD who had a facial muscle involvement since early childhood, but it remained hidden due to severe cognitive problems. The clinical manifestations consistent with the FSHD phenotype included an increased serum creatine kinase, a disrupted stapedial reflex, as well as hamstrings, scapular, and abdominal muscles involvements (Saito et al. 2007). Two biological forms of FSHD are FSHD type 1 (FSHD1) and type 2 (FSHD2). FSHD type 1 (OMIM no. 158900) is the most common subtype seen in approximately 95% of FSHD patients and is responsible for almost all early-onset cases (Mul et al. 2016). The phenotype of FSHD1 is associated with deletions in the subtelomeric region of chromosome 4q35 which consists of tandem repetitive units of 3.3 kb called D4Z4. Each D4Z4 unit is a copy of double homeobox 4 (DUX4) retrogene, which is expressed as a transcription factor in the germline, but is normally suppressed in somatic tissue. In normal people, the number of D4Z4 repetitions is 11 to more than 100 copies, while in FSHD patients, this number is reduced to 1 to 10 copies. The childhood-onset FSHD occurs when larger deletions are made in the D4Z4. Investigations revealed that the deletion leads to DNA hypomethylation of D4Z4 repeats and derepression of transcription in the region (Deutekom et al. 1993; van Overveld et al. 2003). Less than 5% of patients with FSHD phenotype have normal-size repeat arrays on 4q but show DNA hypomethylation of D4Z4 repeats. These patients are considered to have FSHD2 (OMIM no. 158901) correlated with mutations of the structural maintenance of chromosomes flexible hinge domain-containing protein 1 (SMCHD1 gene) or rarely DNA methyltransferase 3B (DNMT3B gene) in the presence of a disease-permissive 4qA haplotype. Haplotype 4qA contains the polymorphic polyadenylation signal (PAS), which is essential for the stabilization of DUX4 transcribed mRNA and thus the expression of the DUX4 protein in skeletal muscle (Hamel and Tawil 2018). Recently, Hamanaka et al. indicated some mutations in ligand-dependent nuclear receptor-interacting factor 1 (LRIF1), which is a facilitator of the interaction between SMCHD1 and chromatin, in FSHD2 pathogenesis (Hamanaka et al. 2020). SMCHD1, located at 18 p11 and containing 48 exons, encodes a protein belonging to the extremely conserved structural maintenance of chromosome (SMC) protein family as well as the human microrchidia (MORC) family. Both of the protein families are involved in the epigenetic regulation of chromatin status (Lemmers et al. 2012; van den Boogaard et al. 2016; Ruggiero et al. 2020). Contraction of number of D4Z4 repeats in FSHD1, as well as chromatin hypomethylation of D4Z4 repeats in FSHD2, reduces D4Z4 region suppressive heterochromatin. This chromatin relaxation leads to transcription of DUX4 mRNA and improper expression of DUX4 protein in myonuclei. It disrupts multiple signaling pathways that eventually lead to cell death in the muscles of infected individuals (Hamel and Tawil 2018; Schätzl et al. 2021).
Conclusion
Over the past two decades, substantial progress has been made in the field of decoding the cellular and molecular bases of neuromuscular disorders. Cognitive deficit is a general term used to describe impairments in the individual’s mental processes. Several cognitive function sub-domains, including memory, attention, problem-solving, and visual perception, have been considered in NMDs. Due to the diverse pathogenesis of muscular dystrophies and the influence of several systems, cognitive defects may also appear as a result of these conditions. Although there is a strong correlation between cognitive characteristics and brain protein expression or function, the direct link between tissue-specific protein expression and cognitive deficits in these NMDs is not yet clear. Cognitive deficits do not seem to be rare in muscular dystrophies. Some muscular dystrophies clearly present cognitive dysfunction, while others are often associated with neuropsychological problems, such as anxiety, ASD, and ADHD (Table 1). However, adequate studies on this topic have not yet been conducted. This is partly due to the low frequency of occurrence of these diseases and the intermittent lack of large cohorts of patients to provide robust and credible results. In summary, the most well-known pathomechanisms involved in the simultaneous progression of muscular dystrophy and intellectual disability include the following: defects in assembly and processing of DGC in both muscles and neurons in dystroglycanopathy syndromes (CMD. LGMD); loss of the brain and muscle dystrophin isoforms as well as choline and glutamate defects in DMD, spliceopathy arising from gain-of-function RNA mechanism in myotonic dystrophy; and DUX4 derepression due to the opening of the chromatin structure in FSHD. Given the effect that the simultaneous occurrence of cognitive impairment and muscle involvement has on the quality of life of these patients, a more accurate understanding of molecular mechanisms paves the way for the development of targeted therapeutic interventions and consequently improves their quality of life.
Availability of Data and Materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Anaya-Segura MA, García-Martínez FA, Montes-Almanza LÁ et al (2015) Non-invasive biomarkers for duchenne muscular dystrophy and carrier detection. Molecules 20:11154–11172
Anderson JL, Head SI, Rae C and Morley JW (2002) Brain function in Duchenne muscular dystrophy. Brain 125:4-13. https://doi.org/10.1093/brain/awf012
Angelini C (2017) Genetic neuromuscular disorders: a case-based approach. Springer
Arvio M, Määttänen L, Haanpää M, Lähdetie J (2019) Two middle-aged women with the Finnish variant of muscle-eye-brain disease (MEB). Am J Med Genet Part A. https://doi.org/10.1002/ajmg.a.61369
Astrea G, Battini R, Lenzi S, Frosini S, Bonetti S, Moretti E, Perazza S, Santorelli FM and Pecini C (2016) Learning disabilities in neuromuscular disorders: a springboard for adult life. Acta Myologica 35:90
Astrea G, Pecini C, Gasperini F et al (2015) Reading impairment in Duchenne muscular dystrophy: a pilot study to investigate similarities and differences with developmental dyslexia. Res Dev Disabil 45:168–177
Auranen M, Rapola J, Pihko H et al (2000) Muscle membrane-skeleton protein changes and histopathological characterization of muscle-eye-brain disease. Neuromuscul Disord 10:16–23. https://doi.org/10.1016/S0960-8966(99)00066-8
Balci B, Uyanik G, Dincer P et al (2005) An autosomal recessive limb girdle muscular dystrophy (LGMD2) with mild mental retardation is allelic to Walker-Warburg syndrome (WWS) caused by a mutation in the POMT1 gene. Neuromuscul Disord 15:271–275
Banihani R, Smile S, Yoon G, Mosleh M, Snider A and McAdam L (2014) GP 175: Cognitive and neurobehavioral profile and its relation with genotype mutation in boys with Duchenne muscular dystrophy. Neuromuscul Disord 24:858
Banihani R, Smile S, Yoon G et al (2015a) Cognitive and neurobehavioral profile in boys with Duchenne muscular dystrophy. J Child Neurol 30:1472–1482
Banihani R, Smile S, Yoon G et al (2015b) Cognitive and neurobehavioral profile in boys with duchenne muscular dystrophy. J Child Neurol. https://doi.org/10.1177/0883073815570154
Barkovich AJ (1998) Neuroimaging manifestations and classification of congenital muscular dystrophies. Am J Neuroradiol 19:1389-1396
Bello L, Melacini P, Pezzani R et al (2012) Cardiomyopathy in patients with POMT1-related congenital and limb-girdle muscular dystrophy. Eur J Hum Genet. https://doi.org/10.1038/ejhg.2012.71
Biancheri R, Bertini E, Falace A et al (2006) POMGnT1 mutations in congenital muscular dystrophy: genotype-phenotype correlation and expanded clinical spectrum. Arch Neurol 63:1491–1495
Biancheri R, Falace A, Tessa A et al (2007) POMT2 gene mutation in limb-girdle muscular dystrophy with inflammatory changes. Biochem Biophys Res Commun 363:1033–1037
Borisovna KO, Yurievna KA, Yurievich TK et al (2019) Compound heterozygous POMGNT1 mutations leading to muscular dystrophy-dystroglycanopathy type A3: a case report. BMC Pediatr. https://doi.org/10.1186/s12887-019-1470-2
Bresolin N, Castelli E, Comi GP et al (1994) Cognitive impairment in Duchenne muscular dystrophy. Neuromuscul Disord 4:359–369
Brown SC, Fassati A, Popplewell L et al (1999) Dystrophic phenotype induced in vitro by antibody blockade of muscle α-dystroglycan-laminin interaction. J Cell Sci 112:209–216. https://doi.org/10.1242/jcs.112.2.209
Butterfield RJ (2019) Congenital muscular dystrophy and congenital myopathy. Contin Lifelong Learn Neurol 25:1640-1661
Carss KJ, Stevens E, Foley AR et al (2013) Mutations in GDP-mannose pyrophosphorylase B cause congenital and limb-girdle muscular dystrophies associated with hypoglycosylation of α-dystroglycan. Am J Hum Genet 93:29–41
Chan YM, Keramaris-Vrantsis E, Lidov HG et al (2010) Fukutin-related protein is essential for mouse muscle, brain and eye development and mutation recapitulates the wide clinical spectrums of dystroglycanopathies. Hum Mol Genet. https://doi.org/10.1093/hmg/ddq314
Chiara Manzini M, Gleason D, Chang BS et al (2008) Ethnically diverse causes of Walker-Warburg syndrome (WWS): FCMD mutations are a more common cause of WWS outside of the Middle East. Hum Mutat 29:E231–E241
Chiyonobu T, Sasaki J, Nagai Y et al (2005) Effects of fukutin deficiency in the developing mouse brain. Neuromuscul Disord 15:416–426. https://doi.org/10.1016/j.nmd.2005.03.009
Cirak S, Herrmann R, Uyanik G et al (2006) Expanding the spectrum of POMT1 mutations: limb-girdle muscular dystrophy with mental retardation and microcephaly (LGMD2K). Neuropediatrics. https://doi.org/10.1055/s-2006-974138
Cleary JD, Ranum LPW (2013) Repeat-associated non-ATG (RAN) translation in neurological disease. Hum Mol Genet. https://doi.org/10.1093/hmg/ddt371
Clement E, Mercuri E, Godfrey C et al (2008) Brain involvement in muscular dystrophies with defective dystroglycan glycosylation. Ann Neurol. https://doi.org/10.1002/ana.21482
Crisafulli S, Sultana J, Fontana A, Salvo F, Messina S and Trifirò G (2020) Global epidemiology of Duchenne muscular dystrophy: an updated systematic review and meta-analysis. Orphanet J Rare Dis 15:1-20
Currier SC, Lee CK, Chang BS et al (2005) Mutations in POMT1 are found in a minority of patients with Walker-Warburg syndrome. Am J Med Genet Part A 133:53–57
D’Angelo MG, Bresolin N (2006) Cognitive impairment in neuromuscular disorders. Muscle Nerve 34:16–33. https://doi.org/10.1002/mus.20535
Darin N, Tulinius M (2000) Neuromuscular disorders in childhood: a descriptive epidemiological study from western Sweden. Neuromuscul Disord. https://doi.org/10.1016/S0960-8966(99)00055-3
de Bernabé DB-V, Currier S, Steinbrecher A et al (2002) Mutations in the O-mannosyltransferase gene POMT1 give rise to the severe neuronal migration disorder Walker-Warburg syndrome. Am J Hum Genet 71:1033–1043
de Bernabé DB-V, Van Bokhoven H, Van Beusekom E et al (2003) A homozygous nonsense mutation in the fukutin gene causes a Walker-Warburg syndrome phenotype. J Med Genet 40:845–848
De Bernabé DB-V, Voit T, Longman C et al (2004) Mutations in the FKRP gene can cause muscle-eye-brain disease and Walker-Warburg syndrome. J Med Genet 41:e61
De La Chapelle A, Wright FA (1998) Linkage disequilibrium mapping in isolated populations: the example of Finland revisited. Proc Natl Acad Sci 95:12416–12423
Deutekom JC, Wljmenga C, Tlenhoven EA, Gruter AM, Hewitt JE, Padberg GW, Ommen GJ, Hofker MH, Fronts RR et al (1993) FSHD associated DNA rearrangements are due to deletions of integral copies of a 3.2 kb tandemly repeated unit. Hum Mol Genet 2:2037–2042
Diesen C, Saarinen A, Pihko H et al (2004) POMGnT1 mutation and phenotypic spectrum in muscle-eye-brain disease. J Med Genet 41:e115
Doorenweerd N (2020) Combining genetics, neuropsychology and neuroimaging to improve understanding of brain involvement in Duchenne muscular dystrophy - a narrative review. Neuromuscul Disord 30:437-442
Duan D, Goemans N, Takeda Si, Mercuri E and Aartsma-Rus A (2021) Duchenne muscular dystrophy. Nat Rev Dis Prim 7:1-19
Falsaperla R, Praticò AD, Ruggieri M, Parano E, Rizzo R, Corsello G, Vitaliti G and Pavone P (2016) Congenital muscular dystrophy: From muscle to brain. Ital J Pediatr 42:1-11
Fukuyama Y (1960) A peculiar from of congenital progressive muscular dystrophy. Report of fifteen cases. Pediatr Univ Tokyo 4:5–8
Funakoshi M, Goto K, Arahata K (1998) Epilepsy and mental retardation in a subset of early onset 4q35-facioscapulohumeral muscular dystrophy. Neurology 50:1791–1794
Gençpınar P, Uyanık G, Haspolat Ş, Oygür N and Duman Ö (2019) Clinical and molecular manifestations of congenital muscular alpha-dystroglycanopathy due to an ISPD gene mutation. Neurophysiology 51:373-378. https://doi.org/10.1007/s11062-020-09831-y
Godfrey C, Clement E, Mein R et al (2007) Refining genotype-phenotype correlations in muscular dystrophies with defective glycosylation of dystroglycan. Brain. https://doi.org/10.1093/brain/awm212
Goossens E, Steyaert J, De Die-Smulders C, Willekens D and Fryns JP (2000) Emotional and behavioral profile and child psychiatric diagnosis in the childhood type of myotonic dystrophy. Genet Couns 11:317-327
Grosso S, Mostardini R, Di Bartolo RM et al (2011) Epilepsy, speech delay, and mental retardation in facioscapulohumeral muscular dystrophy. Eur J Paediatr Neurol 15:456–460
Hamanaka K, Šikrová D, Mitsuhashi S et al (2020) Homozygous nonsense variant in LRIF1 associated with facioscapulohumeral muscular dystrophy. Neurology. https://doi.org/10.1212/WNL.0000000000009617
Hamel J, Tawil R (2018) Facioscapulohumeral muscular dystrophy: update on pathogenesis and future treatments. Neurotherapeutics 15:863-871
Hehr U, Uyanik G, Gross C et al (2007) Novel POMGnT1 mutations define broader phenotypic spectrum of muscle–eye–brain disease. Neurogenetics 8:279–288
Hirotsune S, Takahara T, Sasaki N et al (1995) The reeler gene encodes a protein with an EGF–like motif expressed by pioneer neurons. Nat Genet. https://doi.org/10.1038/ng0595-77
Hong SE, Shugart YY, Huang DT et al (2000) Autosomal recessive lissencephaly with cerebellar hypoplasia is associated with human RELN mutations. Nat Genet. https://doi.org/10.1038/79246
Hu H, Li J, Gagen CS et al (2011) Conditional knockout of protein O-mannosyltransferase 2 reveals tissue-specific roles of O-mannosyl glycosylation in brain development. J Comp Neurol. https://doi.org/10.1002/cne.22572
Ishigaki K, Ihara C, Nakamura H et al (2018) National registry of patients with Fukuyama congenital muscular dystrophy in Japan. Neuromuscul Disord. https://doi.org/10.1016/j.nmd.2018.08.001
Jensen BS, Willer T, Saade DN et al (2015) GMPPB-associated dystroglycanopathy: emerging common variants with phenotype correlation. Hum Mutat. https://doi.org/10.1002/humu.22898
Johnson NE, Heatwole CR (2012) Myotonic dystrophy: from bench to bedside. Semin Neurol. https://doi.org/10.1055/s-0032-1329202
Jurado LAP, Coloma A, Cruces J (1999) Identification of a human homolog of the Drosophila rotated abdomen gene (POMT1) encoding a putative protein O-mannosyl-transferase, and assignment to human chromosome 9q34.1. Genomics 58:171-180 https://doi.org/10.1006/geno.1999.5819
Kano H, Kobayashi K, Tachikawa M et al (2002) Deficiency of α-dystroglycan in muscle-eye-brain disease. Biochem Biophys Res Commun. https://doi.org/10.1006/bbrc.2002.6608
Kilroy E, Liu CY, Yan L, Kim YC, Dapretto M, Mendez MF and Wang DJ (2011) Relationships between cerebral blood flow and IQ in typically developing children and adolescents. J Cogn Sci 12:151 https://doi.org/10.17791/jcs.2011.12.2.151
Kobayashi K, Nakahori Y, Miyake M et al (1998) An ancient retrotransposal insertion causes Fukuyama-type congenital muscular dystrophy. Nature 394:388–392
Kogelberg H, Chai W, Feizi T, Lawson AM (2001) NMR studies of mannitol-terminating oligosaccharides derived by reductive alkaline hydrolysis from brain glycoproteins. Carbohydr Res. https://doi.org/10.1016/S0008-6215(01)00051-9
Konstantelou E, Pasparaki E, Tzilas V et al (2019) Neuromuscular diseases. ERS Monogr. https://doi.org/10.1183/2312508X.10021519
Kreis R, Wingeier K, Vermathen P et al (2011) Brain metabolite composition in relation to cognitive function and dystrophin mutations in boys with Duchenne muscular dystrophy. NMR Biomed. https://doi.org/10.1002/nbm.1582
Laing NG (2012) Genetics of neuromuscular disorders. Crit Rev Clin Lab Sci 49:33-48
Landouzy M, Dejerine J. De la myopathie atrophique progressive (myopathie héréditaire, débutant dans l'enfance par la face, sans altération du système nerveux). Comptes Rendus de l'Académie des Sciences. 1884;98:53–55. Landouzy L, Dejerine J (1884) De la myopathie atrophique progressive (myopathie héréditaire débutant, dans l’enfance, par la face, sans altération du système nerveux. Comptes Rendus de l'Académie des Sciences 98:53–55
Lee JE, Cooper TA (2009) Pathogenic mechanisms of myotonic dystrophy. Biochem Soc Trans. https://doi.org/10.1042/BST0371281
Lemmers RJLF, Tawil R, Petek LM et al (2012) Digenic inheritance of an SMCHD1 mutation and an FSHD-permissive D4Z4 allele causes facioscapulohumeral muscular dystrophy type 2. Nat Genet 44:1370
Liu Z, Wang Y, Yang F et al (2021) GMPPB-congenital disorders of glycosylation associate with decreased enzymatic activity of GMPPB. Mol Biomed. https://doi.org/10.1186/s43556-021-00027-2
Lochter A, Vaughan L, Kaplony A et al (1991) J1/tenascin in substrate-bound and soluble form displays contrary effects on neurite outgrowth. J Cell Biol. https://doi.org/10.1083/jcb.113.5.1159
López-Martínez A, Soblechero-Martín P, de-la-Puente-Ovejero L, Nogales-Gadea G and Arechavala-Gomeza V (2020) An overview of alternative splicing defects implicated in myotonic dystrophy type i. Genes 11:1109
Mah JK, Chen Y-W (2018) A pediatric review of facioscapulohumeral muscular dystrophy. J Pediatr Neurol JPN 16:222
Maroofian R, Riemersma M, Jae LT et al (2017) B3GALNT2 mutations associated with non-syndromic autosomal recessive intellectual disability reveal a lack of genotype-phenotype associations in the muscular dystrophy-dystroglycanopathies. Genome Med. https://doi.org/10.1186/s13073-017-0505-2
Matsuzaka T, Sakuragawa N, Terasawa K, Kuwabara H (1986) Facioscapulohumeral dystrophy associated with mental retardation, hearing loss, and tortuosity of retinal arterioles. J Child Neurol 1:218–223
Mattos MK, Chang A, Pitcher K, Whitt C, Ritterband LM and Quigg MS (2021) A review of insomnia treatments for patients with mild cognitive impairment. Aging Dis
Meola G (2020) Myotonic dystrophy type 2: The 2020 update. Acta Myol 39:222
Meola G, Cardani R (2015) Myotonic dystrophy type 2: an update on clinical aspects, genetic and pathomolecular mechanism. J Neuromuscul Dis. https://doi.org/10.3233/JND-150088
Meola G, Sansone V, Perani D et al (1999) Reduced cerebral blood flow and impaired visual-spatial function in proximal myotonic myopathy. Neurology. https://doi.org/10.1212/wnl.53.5.1042
Meola G, Sansone V, Perani D et al (2003) Executive dysfunction and avoidant personality trait in myotonic dystrophy type 1 (DM-1) and in proximal myotonic myopathy (PROMM/DM-2). Neuromuscul Disord. https://doi.org/10.1016/S0960-8966(03)00137-8
Mercuri E, Messina S, Bruno C et al (2009) Congenital muscular dystrophies with defective glycosylation of dystroglycan: a population study. Neurology 72:1802–1809. https://doi.org/10.1212/01.wnl.0000346518.68110.60
Mercuri E, Topaloglu H, Brockington M et al (2006) Spectrum of brain changes in patients with congenital muscular dystrophy and FKRP gene mutations. Arch Neurol. https://doi.org/10.1001/archneur.63.2.251
Messina S, Bruno C, Moroni I et al (2010) Congenital muscular dystrophies with cognitive impairment: a population study. Neurology 75:898–903
Mitsuhashi S, Ohkuma A, Talim B et al (2011) A congenital muscular dystrophy with mitochondrial structural abnormalities caused by defective de novo phosphatidylcholine biosynthesis. Am J Hum Genet. https://doi.org/10.1016/j.ajhg.2011.05.010
Miyashita MUT, Ohtsuka Y, Okamura-Oho Y et al (2001) Extended polyglutamine selectively interacts with caspase-8 and -10 in nuclear aggregates. Cell Death Differ. https://doi.org/10.1038/sj.cdd.4400819
Mochizuki H, Miyatake S, Suzuki M et al (2008) Mental retardation and lifetime events of Duchenne muscular dystrophy in Japan. Intern Med. https://doi.org/10.2169/internalmedicine.47.0907
Mohamadian M, Naseri M, Ghandil P et al (2020) The first report of two homozygous sequence variants in FKRP and SELENON genes associated with syndromic congenital muscular dystrophy in Iran: Further expansion of the clinical phenotypes. J Gene Med. https://doi.org/10.1002/jgm.3265
Montagnese F, Klupp E, Karampinos DC et al (2017) Two patients with GMPPB mutation: the overlapping phenotypes of limb-girdle myasthenic syndrome and limb-girdle muscular dystrophy dystroglycanopathy. Muscle Nerve. https://doi.org/10.1002/mus.25485
Moore SA, Saito F, Chen J et al (2002) Deletion of brain dystroglycan recapitulates aspects of congenital muscular dystrophy. Nature. https://doi.org/10.1038/nature00838
Mostacciuolo ML, Miorin M, Martinello F et al (1996) Genetic epidemiology of congenital muscular dystrophy in a sample from north-east Italy. Hum Genet 97:277–279
Mul K, Lassche S, Voermans NC et al (2016) What’s in a name? The clinical features of facioscapulohumeral muscular dystrophy. Pract Neurol 16:201–207
Murphy AP, Straub V (2015) The classification, natural history and treatment of the limb girdle muscular dystrophies. J Neuromuscul Dis 2:S7-S19
Naidoo M, Anthony K (2020) Dystrophin Dp71 and the neuropathophysiology of Duchenne muscular dystrophy. Mol Neurobiol 57:1748-1767
Nardes F, Araújo APQC, Ribeiro MG (2012) O retardo mental na distrofia muscular de Duchenne. J Pediatr (rio j) 88:6–16
Natarajan N and Ionita C (2018) 64 - Neonatal Neuromuscular Disorders. In: Gleason CA and Juul SE (eds) Avery's Diseases of the Newborn (Tenth Edition), Elsevier, Philadelphia pp. 952-960.e2
Norwood FLM, Harling C, Chinnery PF, Eagle M, Bushby K, Straub V (2009) Prevalence of genetic muscle disease in Northern England: in-depth analysis of a muscle clinic population. Brain 132:3175–3186. https://doi.org/10.1093/brain/awp236
Oestergaard ST, Stojkovic T, Dahlqvist JR, Bouchet-Seraphin C, Nectoux J, Leturcq F, Cossée M, Solé G, Thomsen C, Krag TO and Vissing J (2016) Muscle involvement in limb-girdle muscular dystrophy with GMPPB deficiency (LGMD2T). Neurol Genet 2:e112. https://doi.org/10.1212/nxg.0000000000000112
Østergaard ST, Johnson K, Stojkovic T et al (2018) Limb girdle muscular dystrophy due to mutations in POMT2. J Neurol Neurosurg Psychiatry 89:506–512
Ozimski LL, Sabater-Arcis M, Bargiela A, Artero R (2021) The hallmarks of myotonic dystrophy type 1 muscle dysfunction. Biol Rev. https://doi.org/10.1111/brv.12674
Paprocka J, Jezela-Stanek A, Tylki-Szymańska A, Grunewald S (2021) Congenital disorders of glycosylation from a neurological perspective. Brain Sci 11:88
Parisi L, Di Filippo T, Glorioso P, La Grutta S, Epifanio MS and Roccella M (2018) Autism spectrum disorders in children affected by Duchenne muscular dystrophy. Minerva Pediatr.70:233-239. https://doi.org/10.23736/s0026-4946.16.04380-2
Parsamanesh N, Safarpour H, Etesam S et al (2019) Identification and in silico characterization of a novel point mutation within the phosphatidylinositol glycan anchor biosynthesis class G gene in an Iranian family with intellectual disability. J Mol Neurosci 69:538–545
Peric S, Rakocevic-Stojanovic V, Meola G (2021) Cerebral involvement and related aspects in myotonic dystrophy type 2. Neuromuscul Disord. https://doi.org/10.1016/j.nmd.2021.06.002
Perini GI, Menegazzo E, Ermani M et al (1999) Cognitive impairment and (CTG)n expansion in myotonic dystrophy patients. Biol Psychiatry. https://doi.org/10.1016/S0006-3223(99)00016-5
Peristeri E, Aloizou A-M, Keramida P, Tsouris Z, Siokas V, Mentis A-FA and Dardiotis E (2020) Cognitive deficits in myopathies. Int J Mol Sci 21:3795
Rae C, Scott RB, Thompson CH et al (1998) Brain biochemistry in Duchenne muscular dystrophy: A 1H magnetic resonance and neuropsychological study. J Neurol Sci. https://doi.org/10.1016/S0022-510X(98)00190-7
Rasic MV, Vojinovic D, Pesovic J et al (2014) Intellectual ability in the Duchenne muscular dystrophy and dystrophin gene mutation location. Balk J Med Genet 17:25–35
Reed UC (2009) Congenital muscular dystrophy - part II: a review of pathogenesis and therapeutic perspectives. Arq Neuropsiquiatr 67:343-362. https://doi.org/10.1590/S0004-282X2009000200035
Ricotti V, Mandy WPL, Scoto M et al (2016) Neurodevelopmental, emotional, and behavioural problems in Duchenne muscular dystrophy in relation to underlying dystrophin gene mutations. Dev Med Child Neurol. https://doi.org/10.1111/dmcn.12922
Rodríguez Cruz PM, Belaya K, Basiri K et al (2016) Clinical features of the myasthenic syndrome arising from mutations in GMPPB. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2016-313163
Rojas-Marcos I (2019) Muscular dystrophies. Med. https://doi.org/10.1016/j.med.2019.04.003
Roll L, Faissner A (2019) Tenascins in CNS lesions. Semin. Cell Dev Biol 89:118-124. https://doi.org/10.1016/j.semcdb.2018.09.012
Roscioli T, Kamsteeg E-J, Buysse K et al (2012) Mutations in ISPD cause Walker-Warburg syndrome and defective glycosylation of α-dystroglycan. Nat Genet 44:581–585
Ruggiero L, Mele F, Manganelli F et al (2020) Phenotypic variability among patients with D4Z4 reduced allele facioscapulohumeral muscular dystrophy. JAMA Netw Open 3:e204040
Saito F, Matsumura K (2011) Fukuyama-type congenital muscular dystrophy and defective glycosylation of α-dystroglycan. Skelet Muscle 1:22. https://doi.org/10.1186/2044-5040-1-22
Saito K (2006) Prenatal diagnosis of Fukuyama congenital muscular dystrophy. Prenat Diagnosis Publ Affil with Int Soc Prenat Diagnosis 26:415–417
Saito Y, Miyashita S, Yokoyama A et al (2007) Facioscapulohumeral muscular dystrophy with severe mental retardation and epilepsy. Brain Dev 29:231–233
Sanga S, Ghosh A, Kumar K et al (2021) Whole-exome analyses of congenital muscular dystrophy and congenital myopathy patients from India reveal a wide spectrum of known and novel mutations. Eur J Neurol. https://doi.org/10.1111/ene.14616
Santavuori P, Leisti J, Kruus S (1977) Muscle, eye and brain disease: a new syndrome. Neuropadiatrie 8:553
Saredi S, Gibertini S, Ardissone A et al (2014) A fourth case of POMT2-related limb girdle muscle dystrophy with mild reduction of α-dystroglycan glycosylation. Eur J Paediatr Neurol. https://doi.org/10.1016/j.ejpn.2013.10.005
Sarkozy A, Torelli S, Mein R et al (2018) Mobility shift of beta-dystroglycan as a marker of GMPPB gene-related muscular dystrophy. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2017-316956
Schätzl T, Kaiser L, Deigner HP (2021) Facioscapulohumeral muscular dystrophy: genetics, gene activation and downstream signalling with regard to recent therapeutic approaches: an update. Orphanet J Rare Dis 16:129. https://doi.org/10.1186/s13023-021-01760-1
Seo BA, Cho T, Lee DZ et al (2018) LARGE, an intellectual disability-associated protein, regulates AMPA-type glutamate receptor trafficking and memory. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.1805060115
Sewry CA (2010) Muscular dystrophies: an update on pathology and diagnosis. Acta Neuropathol 120:343-358. https://doi.org/10.1007/s00401-010-0727-5
Silan F, Yoshioka M, Kobayashi K et al (2003) A new mutation of the fukutin gene in a non-Japanese patient. Ann Neurol off J Am Neurol Assoc Child Neurol Soc 53:392–396
Silfeler I, Arica V, Davran R et al (2012) Fukuyama congenital muscular dystrophy. Pakistan J Med Sci. https://doi.org/10.1016/j.nmd.2019.06.457
Song D, Dai Y, Chen X et al (2020) Genetic variations and clinical spectrum of dystroglycanopathy in a large cohort of Chinese patients. Clin Genet. https://doi.org/10.1111/cge.13886
Spalice A, Parisi P, Nicita F et al (2009) Neuronal migration disorders: clinical, neuroradiologic and genetics aspects. Acta Paediatr Int J Paediatr 98:421–433. https://doi.org/10.1111/j.1651-2227.2008.01160.x
Stokes M, Varughese N, Iannaccone S, Castro D (2019) Clinical and genetic characteristics of childhood-onset myotonic dystrophy. Muscle Nerve. https://doi.org/10.1002/mus.26716
Suthar R, Angurana SK, Singh U, Singh P (2018) Walker-Warburg syndrome. Neurol India. https://doi.org/10.4103/0028-3886.246262
Tadayoni R, Rendon A, Soria-Jasso LE, Cisneros B (2012) Dystrophin Dp71: the smallest but multifunctional product of the duchenne muscular dystrophy gene. Mol Neurobiol 45:43-60. https://doi.org/10.1007/s12035-011-8218-9
Takeda S, Kondo M, Sasaki J et al (2003) Fukutin is required for maintenance of muscle integrity, cortical histiogenesis and normal eye development. Hum Mol Genet 12:1449–1459. https://doi.org/10.1093/hmg/ddg153
Taniguchi K, Kobayashi K, Saito K et al (2003) Worldwide distribution and broader clinical spectrum of muscle–eye–brain disease. Hum Mol Genet 12:527–534
Tawil R (2004) Facioscapulohumeral muscular dystrophy. Curr Neurol Neurosci Rep 4:51–54
Teber S, Sezer T, Kafalı M et al (2008) Severe muscle–eye–brain disease is associated with a homozygous mutation in the POMGnT1 gene. Eur J Paediatr Neurol 12:133–136
Thornton CA (2014) Myotonic dystrophy. Neurol Clin 32:705-719
Tian WT, Zhou HY, Zhan FX et al (2019) Lysosomal degradation of GMPPB is associated with limb-girdle muscular dystrophy type 2T. Ann Clin Transl Neurol. https://doi.org/10.1002/acn3.787
Tonekaboni SH (2016) Congenital muscular dystrophy: an overview. Genet Third Millenn 14:0-0
Topaloglu H (2018) Muscular dystrophies with mental retardation. Proceedings of the XIII Congress of mediterranean society of Myology: Avanos, Turkey June 27-29, 2018. Acta myologica 37:129-183
Tuuli MG and Odibo AO (2018) 38 - Walker-Warburg Syndrome. In: Copel JA, D'Alton ME, Feltovich H, Gratacós E, Krakow D, Odibo AO, Platt LD and Tutschek B (eds) Obstetric Imaging: Fetal Diagnosis and Care (Second Edition), Elsevier, pp. 189-190.e1. https://doi.org/10.1016/B978-0-323-44548-1.00038-3
Udd B, Krahe R (2012) The myotonic dystrophies: molecular, clinical, and therapeutic challenges. Lancet Neurol 11:891-905. https://doi.org/10.1016/S1474-4422(12)70204-1
Vajsar J, Schachter H (2006) Walker-Warburg syndrome. Orphanet J Rare Dis 1:1–5
van den Boogaard ML, Lemmers RJLF, Balog J et al (2016) Mutations in DNMT3B modify epigenetic repression of the D4Z4 repeat and the penetrance of facioscapulohumeral dystrophy. Am J Hum Genet 98:1020–1029
van Overveld PGM, Lemmers RJFL, Sandkuijl LA et al (2003) Hypomethylation of D4Z4 in 4q-linked and non-4q-linked facioscapulohumeral muscular dystrophy. Nat Genet 35:315–317
van Reeuwijk J, Grewal PK, Salih MAM et al (2007) Intragenic deletion in the LARGE gene causes Walker-Warburg syndrome. Hum Genet 121:685–690
Van Reeuwijk J, Olderode-Berends MJW, Van den Elzen C et al (2010) A homozygous FKRP start codon mutation is associated with Walker-Warburg syndrome, the severe end of the clinical spectrum. Clin Genet 78:275–281
Waldrop MA, Flanigan KM (2019) Update in Duchenne and Becker muscular dystrophy. Curr Opin Neurol 32:722–727
Walker EA (1942) Lissencephaly. Arch Neurol Psychiatry 48:13–29
Wallace SE, Conta JH, Winder TL et al (2014) A novel missense mutation in POMT1 modulates the severe congenital muscular dystrophy phenotype associated with POMT1 nonsense mutations. Neuromuscul Disord 24:312–320
Warburg M (1978) Hydrocephaly, congenital retinal nonattachment, and congenital falciform fold. Am J Ophthalmol 85:88–94
Wicklund MP (2013) The muscular dystrophies. Contin Lifelong Learn Neurol 19:1535-1570. https://doi.org/10.1212/01.CON.0000440659.41675.8b
Wicklund MP (2019) The limb-girdle muscular dystrophies. Contin Lifelong Learn Neurol 25:1599-1618. https://doi.org/10.1212/CON.0000000000000809
Wingo TS, Liu Y, Gerasimov ES et al (2021) Brain proteome-wide association study implicates novel proteins in depression pathogenesis. Nat Neurosci. https://doi.org/10.1038/s41593-021-00832-6
Wolfe LA, Krasnewich D (2013) Congenital disorders of glycosylation and intellectual disability. Dev Disabil Res Rev 17:211-225. https://doi.org/10.1002/ddrr.1115
Woo J, Lee HW, Park JS (2019) Differences in the pattern of cognitive impairments between juvenile and adult onset myotonic dystrophy type 1. J Clin Neurosci. https://doi.org/10.1016/j.jocn.2019.07.029
Yanagisawa A, Bouchet C, Quijano-Roy S et al (2009) POMT2 intragenic deletions and splicing abnormalities causing congenital muscular dystrophy with mental retardation. Eur J Med Genet 52:201–206
Yang H, Kobayashi K, Wang S et al (2015) Founder mutation causes classical Fukuyama congenital muscular dystrophy (FCMD) in Chinese patients. Brain Dev. https://doi.org/10.1016/j.braindev.2015.02.010
Yİş ULU, Di̇ni̇z G, Hazan F et al (2018) Childhood onset limb-girdle muscular dystrophies in the Aegean part of Turkey. Acta Myol 37:210
Yoshida A, Kobayashi K, Manya H et al (2001) Muscular dystrophy and neuronal migration disorder caused by mutations in a glycosyltransferase, POMGnT1. Dev Cell 1:717–724. https://doi.org/10.1016/S1534-5807(01)00070-3
Yoshioka M, Higuchi Y (2005) Long-term prognosis of epilepsies and related seizure disorders in Fukuyama-type congenital muscular dystrophy. J Child Neurol. https://doi.org/10.1177/08830738050200041901
Zapata-Aldana E, Ceballos-Sáenz D, Hicks R, Campbell C (2018) Prenatal, neonatal, and early childhood features in congenital myotonic dystrophy. J Neuromuscul Dis. https://doi.org/10.3233/JND-170277
Zheng L, Liu Z, Wang Y et al (2021) Cryo-EM structures of human GMPPA–GMPPB complex reveal how cells maintain GDP-mannose homeostasis. Nat Struct Mol Biol. https://doi.org/10.1038/s41594-021-00591-9
Zivkovic SA, Clemens PR (2015) Muscular dystrophy. In: Neurobiology of Brain Disorders: Biological Basis of Neurological and Psychiatric Disorders Elsevier, pp. 151-166. https://doi.org/10.1016/B978-0-12-398270-4.00011-2
Zouvelou V, Rentzos M, Zalonis I, Filippopolitis K, Manta P, Evdokimidis I (2008) Cognitive impairment and cerebellar atrophy in typical onset 4q35 fascioscapulohumeral dystrophy. Muscle and Nerve 38:1523-1524. https://doi.org/10.1002/mus.21100
Zu T, Gibbens B, Doty NS et al (2011) Non-ATG-initiated translation directed by microsatellite expansions. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.1013343108
Author information
Authors and Affiliations
Contributions
M. Mohamadian and P. Ghandil designed the article contents. M. Mohamadian, M. Rastegr, and N. Parsamanesh wrote the original manuscript. A. Ghadiri and M. Naseri made revisions to the manuscript. All the authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohamadian, M., Rastegar, M., Pasamanesh, N. et al. Clinical and Molecular Spectrum of Muscular Dystrophies (MDs) with Intellectual Disability (ID): a Comprehensive Overview. J Mol Neurosci 72, 9–23 (2022). https://doi.org/10.1007/s12031-021-01933-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-021-01933-4