Abstract
Sepsis can induce acute and chronic changes in the central nervous system termed sepsis-associated encephalopathy (SAE). Not only cognitive deficits but also anxiety, depression, and post-traumatic stress disorder are common in severe sepsis survivors. In this study, we demonstrated that amitriptyline, a classic tricyclic antidepressant, reduced sepsis-induced brain damage through the tropomyosin receptor kinase A (TrkA) signaling pathway. Amitriptyline ameliorated neuronal loss assessed by Nissl staining in a mouse cecal ligation and puncture (CLP)–induced sepsis model. Furthermore, amitriptyline reduced early gliosis assessed by immunofluorescence and late cognitive deficits assessed by the Morris water maze (MWM) test. Moreover, amitriptyline treatment attenuated oxidative stress indicated by less superoxide dismutase (SOD) and catalase (CAT) activity consumption and malondialdehyde (MDA) accumulation. Interestingly, those protective effects of amitriptyline could be abolished by GW441756, a TrkA signaling pathway inhibitor. Immunoblot directly showed that TrkA signaling pathway–associated proteins, such as Akt and GSK3β, were involved in the neuroprotective effects of amitriptyline. Thus, amitriptyline appears to be an encouraging candidate to treat cognitive deficits and depression after severe sepsis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is an overwhelming systemic inflammatory course involving multiple organ systems that caused dysregulated host response to infection (Singer et al. 2016). Sepsis can generate acute and chronic changes in the central nervous system called sepsis-associated encephalopathy (SAE), which is clinically characterized by “altered mental status,” from mild inattentiveness and agitation to more severe disruption of consciousness, such as coma (Feng et al. 2017; Nwafor et al. 2019). More than that, rates of anxiety, depression, and post-traumatic stress disorder are higher in intensive care unit survivors than population norms (Calsavara et al. 2018; Davydow et al. 2009; Nikayin et al. 2016; Parker et al. 2015). Until now, SAE has no testified pharmacological therapy, except general sepsis treatments such as antibiotics and fluid resuscitation (Gofton and Young 2012).
Amitriptyline is a member of tricyclic antidepressants (TCAs) and is widely used to treat neuropathic pain (Mercadante 2015) and even irritable bowel syndrome (Chao and Zhang 2013) due to its anti-inflammatory effect. Recent studies demonstrated that amitriptyline might act as a small molecular tropomyosin receptor kinase A (TrkA) agonist and have potent protective effects in hypoxia-induced cardiomyocyte apoptosis and tumor necrosis factor-α (TNF-α)-induced neuronal damage in vitro (Dai et al. 2017; O’Neill et al. 2016). Interestingly, Xia et al. reported that amitriptyline could reduce inflammation and mortality in cecal ligation and puncture (CLP) and lipopolysaccharide-induced sepsis via mitigating pro-inflammatory response (Xia et al. 2019b). Furthermore, they have demonstrated that amitriptyline ameliorated sepsis-induced coagulopathy via decreasing TNF-α expression in macrophages (Xia et al. 2019a).
Considering the role of inflammatory response, cerebral hypoperfusion, and neuronal loss in SAE (Chaudhry and Duggal 2014), we hypothesize that amitriptyline may exert neuroprotection via TrkA signaling pathway. In this study, we tested the neuroprotective effects of amitriptyline in CLP-induced mice sepsis model. Morris water maze (MWM) test was used for cognitive dysfunction detection. Furthermore, GW441756, a TrkA pathway inhibitor, was used to explore the participation of Akt and glycogen synthase kinase 3β (GSK3β) in SAE.
Materials and Methods
Main Reagents and Animals
Amitriptyline (catalog no. S3183) and GW441756 (catalog no. S2891) were obtained from Selleck Chemicals (Houston, TX, USA). Amitriptyline was dissolved in normal saline, and GW441756 was dissolved in dimethyl sulfoxide (DMSO). Anti-GFAP mouse antibody was from Servicebio (Wuhan, Hubei, China). Rabbit antibody against Iba-1 was purchased from FUJIFILM Wako Chemicals (Osaka, Osaka Prefecture, Japan). Rabbit antibodies against phospho-Akt Ser473 (catalog no. 8200), total-Akt (catalog no. 4691), and phospho-GSK3β (catalog no. 9322) were purchased from Cell Signaling Technology (Boston, MA, USA). Rabbit anti-GSK3β (catalog no. 22104) was from ProteinTech (Wuhan, Hubei, China).
C57BL/6 mice (male, weight 20–25 g) were purchased from Hunan SJA Laboratory Animal Company (Changsha, China) and housed in an Experiment Animal Center (specific pathogen-free) of Central South University. All protocols were conducted in accordance with the Institutional Animal Care and Use Committee of Central South University.
Polymicrobial Sepsis Model and Drug Treatment
For cecal ligation and puncture (CLP) surgery, animals were anesthetized with a cocktail of ketamine (87.5 mg/kg) and xylazine (12.5 mg/kg). Sepsis was induced by CLP as Rittirsch et al. (2009) described. To mimic treatment in the clinic, mice were resuscitated with pre-warmed normal saline (37 °C, 700 μl, subcutaneously) and injected with antibiotics (imipenem in 700 μl normal saline, 25 mg/kg, IP) 6 h after surgery twice a day for 3 days (Coopersmith et al. 2003; Steele et al. 2017).
For pre-treatment, amitriptyline (8 or 16 mg/kg/day, dissolved in normal saline) was intraperitoneally injected twice daily for 2 days (Peng et al. 2015; Xia et al. 2019a). After surgery, amitriptyline was administrated until sacrifice. Since GW441756 could cross the blood-brain barrier, it was also intraperitoneally injected at 10 mg/kg/day (Bernard-Gauthier et al. 2015; Zhang et al. 2014).
Animal Experiment Design
One hundred eighty mice were randomly assigned to 5 groups: Sham group (n = 20), CLP group (n = 40), CLP + Amit8 group (n = 40), CLP + Amit16 group (n = 40), and CLP + Amit16 + GW group (n = 40). Mice in the Sham group received cecum isolation and exteriorization without ligation or puncture. Mice in the CLP group received CLP surgery. Furthermore, the CLP + Amit group received CLP surgery and amitriptyline pretreatment (8 or 16 mg/kg/day, IP, 2 days before CLP). Mice in the CLP + Amit16 + GW group received CLP surgery, amitriptyline (16 mg/kg/day, IP), and GW441756 (10 mg/kg/day, IP, 2 days before CLP). No mice died in the Sham group. For sacrifice, mice were anesthetized and decollated (Adams and Pacharinsak 2015). The left brains were used for Nissl and immunofluorescence staining, and the right hippocampi were homogenized for Western blot and biochemical analysis. The timeline of the study protocol is schematically illustrated in Fig. 1a.
Amitriptyline treatment mitigates neuronal loss in septic mice. a Schematic illustration of the study protocol. b Representative Nissl staining images in CA3 areas. Neuronal pyknosis is indicated by black arrows. Scale bar = 50 μm. c Neuronal pyknosis was calculated accordingly. Values are presented as mean ± standard deviation (SD). *p < 0.05, ***p < 0.001. CLP, cecal ligation and puncture; Amit8, amitriptyline 8 mg/kg; Amit16, amitriptyline 16 mg/kg; GW, GW441756
Brain Tissue for Nissl Staining and Immunofluorescence Labeling
Brain tissues were fixed and sectioned for Nissl staining as previously described (Deng et al. 2017a). Briefly, brain tissues were fixed in 4% paraformaldehyde at room temperature for 24 h and dehydrated in 70%, 80%, 90%, and 100% ethanol. After ethanol replacement by xylene, brain tissues were embedded in paraffin and sliced into 5-μm sections. When paraffin was removed thoroughly by xylene and ethanol, sections were stained with 0.1% cresyl violet acetate for 30 s and rinsed with distilled water. Samples were observed under a microscope, and neuronal pyknosis (shrunken and dense nucleus) was quantified by an expert who was blinded with grouping and treatments (Santos et al. 2013).
Immunofluorescence staining was carried out to detect both GFAP and Iba-1 expression in mice. For double immunofluorescent staining, 6-μm-thick coronal sections were cut. Antigen retrieval was performed by microwave irradiation in citrate buffer (pH = 6) for 8 min. After being blocked in 1.5% bovine serum albumin (BSA) for 1 h, brain sections were incubated with antibodies: rabbit anti-Iba1 (1:200), mouse anti-GFAP (1:200) at 4 °C overnight. After three thorough wash in phosphate-buffered saline (PBS), the sections were then incubated with secondary antibodies (goat anti-rabbit 594 Alexa Fluor and goat anti-mouse 488 Alexa Fluor, all in 1:500) for 1 h at room temperature. The sections were then counterstained with 1 μg/ml 4,6-diamidino-2-phenylindole (DAPI) for 5 min at room temperature in the dark. After being washed with PBS, sections were mounted for immunofluorescence microscopy observation.
Morris Water Maze Test
The spatial reference learning memory of mice was evaluated using the Morris water maze test 21 days after CLP. The apparatus has been previously described (Deng et al. 2017a). Briefly, in the training tests, mice were trained four times daily to locate an underwater hidden platform using several visual cues on the wall of the pool for 6 consecutive days. Each mouse was given 60 s maximum to swim per trial, with 30-s rest on the platform before the next trial. The escape latency was recorded as the average time that the animal spent in reaching the hidden platform. On the 7th day of the MWM test, a single 60-s probe test was performed. After the platform was removed, all the mice were forced to swim to find the original position of the platform. The time spent in the target quadrant was recorded.
Measurement of Superoxide Dismutase and Catalase Activities and Malondialdehyde Contents
Superoxide was generated in xanthine oxidase and hypoxanthine, and the superoxide scavenging effect of superoxide dismutase (SOD) was determined according to Oyanagui’s method (Oyanagui 1984). One unit of SOD activity was defined as the amount of enzyme required for inhibiting the superoxide-induced oxidation by 50%. Briefly, samples were thoroughly mixed with reagent nos. 1, 2, 3, and 4 and incubated at 37 °C for 50 min. The color-developing reagent was added into the mixture and incubated for 10 min at room temperature. The absorbance of the mixture at 550 nm was measured to calculate the SOD activity.
Catalase (CAT) activity was measured according to Goth (1991). One unit of CAT activity was defined as the amount catalyzing 1 μmol H2O2 per s at pH 7.0 and 37 °C. The reaction of H2O2 decomposition by CAT was terminated by adding ammonium molybdate, with the remaining H2O2 and ammonium molybdate producing a pale-yellow complex which was measured at 405 nm.
Malondialdehyde (MDA) was determined by measuring thiobarbituric acid–reactive substance (TBARS) described by Esterbauer and Cheeseman (1990). The method was used to obtain a spectrophotometric measurement of the color with an absorption maximum at 535 nm produced during the reaction of TBA with MDA at 90 °C. Briefly, samples were added to an equal volume of 1% thiobarbituric acid in a 90 °C water bath for 10 min. TBARS levels were estimated at 532 nm against a blank consisting of 5% cold trichloroacetic acid mixed with 1% thiobarbituric acid. Malondialdehyde bis acetal was used as a standard.
SOD and CAT activities and MDA contents were measured by commercially available kits (catalog nos. A001, A007, and A003) (Jiancheng Biotechnology, Nanjing, China). All results were normalized to protein concentrations according to the manufacturer’s instructions.
Immunoblot Analysis
Protein levels were detected by immunoblot as previously described (Mo et al. 2019). Antibodies were diluted in QuickBlock™ (Beyotime Biotech, Shanghai, China) primary antibody dilution buffer (p-Akt 1:1000, Akt 1:2000, p-GSK3β 1:1000, GSK3β 1:1000, GAPDH 1:3000).
Data Analysis
Standard deviation (SD) difference was verified with Brown-Forsythe test and Bartlett’s test. All data were shown as mean ± SD and analyzed by analysis of variance (ANOVA) using GraphPad Prism 7. Holm-Sidak’s multiple comparison tests were used for post hoc comparisons except separately declared. P < 0.05 was determined as statistically significant.
Results
Amitriptyline Treatment Mitigates Neuronal Loss in Septic Mice
A brief timeline of the study protocol is shown in Fig. 1a. The neuronal alterations were assessed by inspecting the numbers and morphology of neurons in CA3 regions of the hippocampus using Nissl staining. Neurons were uniform and intact in the Sham group, whereas the CLP group showed lower density with atrophied and disordered neurons, and some neuronal pyknosis. Interestingly, the neurons in the CA3 regions returned to a neat and dense arrangement after treatment with amitriptyline (8 or 16 mg/kg). Furthermore, blocking TrkA signaling pathway with GW441756 abolished the neuroprotective effects of amitriptyline (Fig. 1b and c). In general, these data suggested that amitriptyline mitigated sepsis-induced neuronal loss via TrkA pathway.
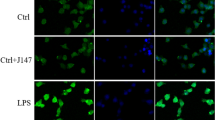
Amitriptyline-Treated Mice Are Protected from Early Sepsis-Induced Gliosis and Late Cognitive Dysfunction
Gliosis is crucial in the pathophysiology of sepsis-induced neuroinflammation and is believed to be highly associated with long-term cognitive deficits (Bi et al. 2019; Griton et al. 2019; Orhun et al. 2019). To determine the effect of amitriptyline on gliosis, immunofluorescence was performed to detect the activation of microglia and astrocytes. CLP surgery significantly increased protein levels of Iba-1 and GFAP (microglia and astrocytes marker, separately). Amitriptyline treatment suppressed both microglia (Fig. 2a and b) and astrocytes (Fig. 2a and c) activation in a dose-dependent manner.
Amitriptyline-treated mice are protected from early sepsis-induced gliosis and late cognitive dysfunction. a Representative immunofluorescence images illustrating Iba-1 (red) and GFAP (green) in the CA3 areas of hippocampi. Scale bar = 50 μm. b Quantitative results of Iba-1. c Quantitative results of GFAP. d Amitriptyline mitigated learning ability (escape latency) impairments during water maze training test from day 1 to day 6. Tukey’s multiple comparison test was used. n = 8 for each group. *p < 0.05, Sham vs CLP; &p < 0.05, CLP vs CLP + Amit8; ^p < 0.05, CLP vs CLP + Amit16; $p < 0.05, CLP + Amit8 vs CLP + Amit16; #p < 0.05, CLP + Amit16 vs CLP + Amit16 + GW. e Amitriptyline improved memory capacity shown by longer retention time in the target quadrant after the hidden platform was removed on day 7. *p < 0.05, **p < 0.01, ***p < 0.001. Iba-1, ionized calcium binding adaptor molecule 1; GFAP, glial fibrillary acidic protein; 4,6-diamidino-2-phenylindole, DAPI
To further determine the protective role of amitriptyline, the Morris water maze test was used to investigate cognitive dysfunction at a later stage of sepsis (21 days after CLP). During the 6 days of training tests, CLP group showed prolonged escape latency than the Sham group. Amitriptyline treatment mitigated learning ability impairments in a dose-dependent manner during day 4 to 6 (Fig. 2d). In the probed test at day 7, amitriptyline improved memory capacity shown by better retention time in the target quadrant after the hidden platform was removed (Fig. 2e). Interestingly, inhibition of TrkA pathway with GW441756 significantly abolished the protective effects of amitriptyline (Fig. 2 d and e). Thus, these data suggested that amitriptyline reduced gliosis and cognitive dysfunction via TrkA pathway.
Amitriptyline Treatment Mitigates Oxidative Stress in Hippocampi
Previously researches have demonstrated that gliosis usually resulted in significant oxidative stress (Bates et al. 2007). We have also revealed the role of oxidative stress in sepsis (Deng et al. 2017b; Huang et al. 2019; Mo et al. 2019); thus, we try to find out the effects of amitriptyline in a mouse sepsis model. Biochemical analysis indicated that CLP induced robust SOD and CAT activity consumption (Fig. 3a and c), and MDA content accumulation (Fig. 3b). Amitriptyline treatment attenuated oxidative stress, while GW441756 abolished those effects.
Amitriptyline Reduces Sepsis-Induced Brain Damage Through TrkA Signaling Pathway
To further investigate the mechanism, immunoblot was performed to detect TrkA signaling pathway–associated proteins (Fig. 4a). CLP robustly decreased the phosphorylation of Akt at Ser473 (Fig. 4b) and GSK3β at Ser9 (Fig. 4c). Furthermore, CLP increased cleaved caspase-3 significantly (Fig. 4d). Compared with the CLP group, amitriptyline markedly increased p-Akt and p-GSK3β and decreased cleaved caspase-3. Those protective effects were all inhibited when GW441756 was used. In general, the above data suggested that TrkA signaling pathway was involved in the protective effects of amitriptyline.
Amitriptyline reduces sepsis-induced brain damage through TrkA signaling pathway. a Immunoblots of hippocampal Akt, p-Akt, GSK3β, p-GSK3β, and cleaved caspase-3. GAPDH was used as a loading control. Images are representative of three experiments. b–d Semiquantitative results of immunoblot. Data represent mean ± SD, n = 3. Akt, serine/threonine-specific protein kinase; GSK3β, glycogen synthase kinase 3β; GAPDH, glyceraldehyde 3-phosphate dehydrogenase
Discussion
As a classic tricyclic antidepressant, amitriptyline has been used for over 50 years, while the exact mechanism is not acquainted entirely as far. More than increasing serotonin and norepinephrine levels, an early study suggested amitriptyline treatment significantly increased the secretion of interleukin-10 (IL-10) and enhanced IL-2 bioactivity (Kubera et al. 2000). Hutchinson et al. demonstrated that amitriptyline or its active metabolite might modulate Toll-like receptor 4 (TLR4) and TLR2 activities, and this may potentially contribute to its efficacy in treating chronic pain and enhancing the analgesic efficacy of opioids (Hutchinson et al. 2010). Kandil et al. demonstrated that amitriptyline ameliorated rotenone-induced neuronal degeneration and increased striatal dopamine level with motor recovery. Amitriptyline also reduced oxidative damage, microglia activation, and pro-inflammatory cytokines (Kandil et al. 2016). Furthermore, amitriptyline has been proved to be an inhibitor of acid sphingomyelinase, which could protect mice from sepsis-induced lung injury (Kornhuber et al. 2008; Peng et al. 2015). Our study demonstrates the protective effect of amitriptyline in sepsis-induced brain damage and cognitive deficits for the first time. Moreover, the mechanism may be associated with its activation of the TrkA signaling pathway.
TrkA belongs to a family of tyrosine kinase receptors (TrkA, TrkB, and TrkC) that governs neural growth in the central nervous system. TrkA was triggered by nerve growth factor (NGF) and governs a number of physiological processes, such as cell survival, proliferation, neural development, and axon growth (Minnone et al. 2017). NGF bound to TrkA reduces inflammatory responses through increasing Akt phosphorylation. The inhibition of GSK3β induced by Akt further prevents NF-κB translocation, and the NF-κB-dependent transcription of pro-inflammatory cytokine genes is inhibited in the end (Prencipe et al. 2014). Akt, also referred to as protein kinase B (PKB), plays an essential role in controlling survival and apoptosis. It is activated by phosphorylation within the carboxy terminus at Ser473 (Sarbassov et al. 2005). Akt phosphorylates GSK3β at Ser9 results in the inactivation of GSK3β, which plays protective effects in chronic kidney diseases and myocardial infarction (Juhaszova et al. 2009; Zhang et al. 2019). Recently, Su et al. demonstrated GSK3β was also involved in high glucose-induced cardiomyocyte apoptosis (Su et al. 2019). Furthermore, the NGF/Akt/GSK3β pathway plays a crucial role in both peripheral and central neuropathy (Li et al. 2019; Liu et al. 2019). Although SAE has been considered a reversible syndrome in the clinic, recent studies using brain imaging or postmortem methods found that cognitive dysfunction was associated with neurodegenerative microglial activation and diffuse ischemic damage. A significant reduction of brain volume similar to neurodegenerative diseases was also observed (Gunther et al. 2012; Wang et al. 2018). In this study, Akt was activated and GSK3β was inactivated by amitriptyline treatment. Furthermore, through using GW441756, a TrkA antagonist, we revealed that TrkA signaling pathway was directly involved in the process of amitriptyline-exerted protection in sepsis-induced brain damage.
In conclusion, this study demonstrates amitriptyline protected mice from sepsis-induced brain damage via TrkA signaling pathway for the first time. Amitriptyline appears to be an encouraging candidate to treat cognitive deficits and depression after severe sepsis.
Data Availability
All datasets generated for this study are included in the manuscript.
Abbreviations
- SAE:
-
Sepsis-associated encephalopathy
- CLP:
-
Cecal ligation and puncture
- TrkA:
-
Tropomyosin receptor kinase A
- Akt:
-
Serine/threonine-specific protein kinase
- GSK3β:
-
Glycogen synthase kinase 3β
- GFAP:
-
Glial fibrillary acidic protein
- SOD:
-
Superoxide dismutase
- MDA:
-
Malondialdehyde
- CAT:
-
Catalase
- BBB:
-
Blood-brain barrier
References
Adams S, Pacharinsak C (2015) Mouse anesthesia and analgesia. Curr Protoc Mouse Biol 5:51–63. https://doi.org/10.1002/9780470942390.mo140179
Bates KA, Martins RN, Harvey AR (2007) Oxidative stress in a rat model of chronic gliosis. Neurobiol Aging 28:995–1008. https://doi.org/10.1016/j.neurobiolaging.2006.05.003
Bernard-Gauthier V, Aliaga A, Aliaga A, Boudjemeline M, Hopewell R, Kostikov A, Rosa-Neto P, Thiel A, Schirrmacher R (2015) Syntheses and evaluation of carbon-11- and fluorine-18-radiolabeled pan-tropomyosin receptor kinase (Trk) inhibitors: exploration of the 4-aza-2-oxindole scaffold as Trk PET imaging agents. ACS Chem Neurosci 6:260–276. https://doi.org/10.1021/cn500193f
Bi W, Lan X, Zhang JW, Xiao S, Cheng XF, Wang HD, Lu DX, Zhu L (2019) USP8 ameliorates cognitive and motor impairments via microglial inhibition in a mouse model of sepsis-associated encephalopathy. Brain Res 1719:40–48. https://doi.org/10.1016/j.brainres.2019.05.009
Calsavara AJC, Nobre V, Barichello T, Teixeira AL (2018) Post-sepsis cognitive impairment and associated risk factors: a systematic review. Aust Crit Care 31:242–253. https://doi.org/10.1016/j.aucc.2017.06.001
Chao GQ, Zhang S (2013) A meta-analysis of the therapeutic effects of amitriptyline for treating irritable bowel syndrome. Intern Med 52:419–424. https://doi.org/10.2169/internalmedicine.52.9147
Chaudhry N, Duggal AK (2014) Sepsis associated encephalopathy. Adv Med 2014:762320–762316. https://doi.org/10.1155/2014/762320
Coopersmith CM, Amiot DM II, Stromberg PE, Dunne WM, Davis CG, Osborne DF, Husain KD, Turnbull IR, Karl IE, Hotchkiss RS, Buchman TG (2003) Antibiotics improve survival and alter the inflammatory profile in a murine model of sepsis from Pseudomonas aeruginosa pneumonia. Shock. 19:408–414. https://doi.org/10.1097/01.shk.0000054370.24363.ee
Dai Y, Wang S, Li C, Chang S, Lu H, Huang Z, Zhang F, Yang H, Shen Y, Chen Z, Qian J, Ge J (2017) Small molecule antidepressant amitriptyline protects hypoxia/reoxygenation-induced cardiomyocyte apoptosis through TrkA signaling pathway. Eur J Pharmacol 798:9–15. https://doi.org/10.1016/j.ejphar.2017.01.029
Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM (2009) Depression in general intensive care unit survivors: a systematic review. Intensive Care Med 35:796–809. https://doi.org/10.1007/s00134-009-1396-5
Deng S, Ai Y, Gong H, Chen C, Peng Q, Huang L, Wu L, Zhang L, Zhang L (2017a) Neuroglobin protects rats from sepsis-associated encephalopathy via a PI3K/Akt/Bax-dependent mechanism. J Mol Neurosci 63:1–8. https://doi.org/10.1007/s12031-017-0933-x
Deng SY, Zhang LM, Ai YH, Pan PH, Zhao SP, Su XL, Wu DD, Tan HY, Zhang LN, Tsung A (2017b) Role of interferon regulatory factor-1 in lipopolysaccharide-induced mitochondrial damage and oxidative stress responses in macrophages. Int J Mol Med 40:1261–1269. https://doi.org/10.3892/ijmm.2017.3110
Esterbauer H, Cheeseman KH (1990) Determination of aldehydic lipid peroxidation products: malonaldehyde and 4-hydroxynonenal. Methods Enzymol 186:407–421. https://doi.org/10.1016/0076-6879(90)86134-h
Feng Q et al (2017) Characterization of sepsis and sepsis-associated encephalopathy. J Intensive Care Med:885066617719750. https://doi.org/10.1177/0885066617719750
Gofton TE, Young GB (2012) Sepsis-associated encephalopathy. Nat Rev Neurol 8:557–566. https://doi.org/10.1038/nrneurol.2012.183
Goth L (1991) A simple method for determination of serum catalase activity and revision of reference range. Clin Chim Acta 196:143–151. https://doi.org/10.1016/0009-8981(91)90067-m
Griton M, Dhaya I, Nicolas R, Raffard G, Periot O, Hiba B, Konsman JP (2019) Experimental sepsis-associated encephalopathy is accompanied by altered cerebral blood perfusion and water diffusion and related to changes in cyclooxygenase-2 expression and glial cell morphology but not to blood-brain barrier breakdown. Brain Behav Immun 83:200–213. https://doi.org/10.1016/j.bbi.2019.10.012
Gunther ML, Morandi A, Krauskopf E, Pandharipande P, Girard TD, Jackson JC, Thompson J, Shintani AK, Geevarghese S, Miller RR 3rd, Canonico A, Merkle K, Cannistraci CJ, Rogers BP, Gatenby JC, Heckers S, Gore JC, Hopkins RO, Ely EW, VISIONS Investigation, VISualizing Icu SurvivOrs Neuroradiological Sequelae (2012) The association between brain volumes, delirium duration, and cognitive outcomes in intensive care unit survivors: the VISIONS cohort magnetic resonance imaging study*. Crit Care Med 40:2022–2032. https://doi.org/10.1097/CCM.0b013e318250acc0
Huang L, Zhang L, Liu Z, Zhao S, Xu D, Li L, Peng Q, Ai Y (2019) Pentamidine protects mice from cecal ligation and puncture-induced brain damage via inhibiting S100B/RAGE/NF-kappaB. Biochem Biophys Res Commun 517:221–226. https://doi.org/10.1016/j.bbrc.2019.07.045
Hutchinson MR, Loram LC, Zhang Y, Shridhar M, Rezvani N, Berkelhammer D, Phipps S, Foster PS, Landgraf K, Falke JJ, Rice KC, Maier SF, Yin H, Watkins LR (2010) Evidence that tricyclic small molecules may possess toll-like receptor and myeloid differentiation protein 2 activity. Neuroscience. 168:551–563. https://doi.org/10.1016/j.neuroscience.2010.03.067
Juhaszova M, Zorov DB, Yaniv Y, Nuss HB, Wang S, Sollott SJ (2009) Role of glycogen synthase kinase-3beta in cardioprotection. Circ Res 104:1240–1252. https://doi.org/10.1161/CIRCRESAHA.109.197996
Kandil EA, Abdelkader NF, El-Sayeh BM, Saleh S (2016) Imipramine and amitriptyline ameliorate the rotenone model of Parkinson’s disease in rats. Neuroscience. 332:26–37. https://doi.org/10.1016/j.neuroscience.2016.06.040
Kornhuber J, Tripal P, Reichel M, Terfloth L, Bleich S, Wiltfang J, Gulbins E (2008) Identification of new functional inhibitors of acid sphingomyelinase using a structure-property-activity relation model. J Med Chem 51:219–237. https://doi.org/10.1021/jm070524a
Kubera M, Holan V, Mathison R, Maes M (2000) The effect of repeated amitriptyline and desipramine administration on cytokine release in C57BL/6 mice. Psychoneuroendocrinology. 25:785–797
Li K et al (2019) Taurine protects against myelin damage of sciatic nerve in diabetic peripheral neuropathy rats by controlling apoptosis of schwann cells via NGF/Akt/GSK3beta pathway. Exp Cell Res 383:111557. https://doi.org/10.1016/j.yexcr.2019.111557
Liu Y, Wang H, Liu N, du J, Lan X, Qi X, Zhuang C, Sun T, Li Y, Yu J (2019) Oxymatrine protects neonatal rat against hypoxic-ischemic brain damage via PI3K/Akt/GSK3beta pathway. Life Sci. https://doi.org/10.1016/j.lfs.2019.04.070
Mercadante S (2015) Topical amitriptyline and ketamine for the treatment of neuropathic pain. Expert Rev Neurother 15:1249–1253. https://doi.org/10.1586/14737175.2015.1101347
Minnone G, De Benedetti F, Bracci-Laudiero L (2017) NGF and its receptors in the regulation of inflammatory response. Int J Mol Sci 18. https://doi.org/10.3390/ijms18051028
Mo Y, Deng S, Zhang L, Huang Y, Li W, Peng Q, Liu Z, Ai Y (2019) SS-31 reduces inflammation and oxidative stress through the inhibition of Fis1 expression in lipopolysaccharide-stimulated microglia. Biochem Biophys Res Commun 520:171–178. https://doi.org/10.1016/j.bbrc.2019.09.077
Nikayin S, Rabiee A, Hashem MD, Huang M, Bienvenu OJ, Turnbull AE, Needham DM (2016) Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. Gen Hosp Psychiatry 43:23–29. https://doi.org/10.1016/j.genhosppsych.2016.08.005
Nwafor DC, Brichacek AL, Mohammad AS, Griffith J, Lucke-Wold BP, Benkovic SA, Geldenhuys WJ, Lockman PR, Brown CM (2019) Targeting the blood-brain barrier to prevent sepsis-associated cognitive impairment. J Cent Nerv Syst Dis 11:1–14. https://doi.org/10.1177/1179573519840652
O’Neill E, Kwok B, Day JS, Connor TJ, Harkin A (2016) Amitriptyline protects against TNF-alpha-induced atrophy and reduction in synaptic markers via a Trk-dependent mechanism. Pharmacol Res Perspect 4:e00195. https://doi.org/10.1002/prp2.195
Orhun G et al (2019) Association between inflammatory markers and cognitive outcome in patients with acute brain dysfunction due to Sepsis. Noro Psikiyatri Arsivi 56:63–70. https://doi.org/10.29399/npa.23212
Oyanagui Y (1984) Reevaluation of assay methods and establishment of kit for superoxide dismutase activity. Anal Biochem 142:290–296. https://doi.org/10.1016/0003-2697(84)90467-6
Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ, Needham DM (2015) Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med 43:1121–1129. https://doi.org/10.1097/CCM.0000000000000882
Peng H, Li C, Kadow S, Henry BD, Steinmann J, Becker KA, Riehle A, Beckmann N, Wilker B, Li PL, Pritts T, Edwards MJ, Zhang Y, Gulbins E, Grassmé H (2015) Acid sphingomyelinase inhibition protects mice from lung edema and lethal Staphylococcus aureus sepsis. J Mol Med (Berl) 93:675–689. https://doi.org/10.1007/s00109-014-1246-y
Prencipe G et al (2014) Nerve growth factor downregulates inflammatory response in human monocytes through TrkA. J Immunol 192:3345–3354. https://doi.org/10.4049/jimmunol.1300825
Rittirsch D, Huber-Lang MS, Flierl MA, Ward PA (2009) Immunodesign of experimental sepsis by cecal ligation and puncture. Nat Protoc 4:31–36. https://doi.org/10.1038/nprot.2008.214
Santos LE et al (2013) Alcohol abuse promotes changes in non-synaptic epileptiform activity with concomitant expression changes in cotransporters and glial cells. PLoS One 8:e78854. https://doi.org/10.1371/journal.pone.0078854
Sarbassov DD, Guertin DA, Ali SM, Sabatini DM (2005) Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 307:1098–1101. https://doi.org/10.1126/science.1106148
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 315:801–810. https://doi.org/10.1001/jama.2016.0287
Steele AM, Starr ME, Saito H (2017) Late therapeutic intervention with antibiotics and fluid resuscitation allows for a prolonged disease course with high survival in a severe murine model of sepsis. Shock. 47:726–734. https://doi.org/10.1097/SHK.0000000000000799
Su D, Zhao J, Hu S, Guan L, Li Q, Shi C, Ma X, Gou J, Zhou Y (2019) GSK3beta and MCL-1 mediate cardiomyocyte apoptosis in response to high glucose. Histochem Cell Biol 152:217–225. https://doi.org/10.1007/s00418-019-01798-0
Wang LM, Wu Q, Kirk RA, Horn KP, Ebada Salem AH, Hoffman JM, Yap JT, Sonnen JA, Towner RA, Bozza FA, Rodrigues RS, Morton KA (2018) Lipopolysaccharide endotoxemia induces amyloid-beta and p-tau formation in the rat brain. Am J Nucl Med Mol Imaging 8:86–99
Xia BT, Beckmann N, Winer LK, Kim Y, Goetzman HS, Veile RE, Gulbins E, Goodman MD, Nomellini V, Caldwell CC (2019a) Amitriptyline treatment mitigates sepsis-induced tumor necrosis factor expression and coagulopathy. Shock. 51:356–363. https://doi.org/10.1097/SHK.0000000000001146
Xia BT et al (2019b) Amitriptyline reduces inflammation and mortality in a murine model of sepsis. Cell Physiol Biochem 52:565–579. https://doi.org/10.33594/000000040
Zhang Q, Descamps O, Hart MJ, Poksay KS, Spilman P, Kane DJ, Gorostiza O, John V, Bredesen DE (2014) Paradoxical effect of TrkA inhibition in Alzheimer’s disease models. J Alzheimers Dis 40:605–617. https://doi.org/10.3233/JAD-130017
Zhang HF, Wang JH, Wang YL, Gao C, Gu YT, Huang J, Wang JH, Zhang Z (2019) Salvianolic acid a protects the kidney against oxidative stress by activating the Akt/GSK-3beta/Nrf2 signaling pathway and inhibiting the NF-kappaB signaling pathway in 5/6 nephrectomized rats. Oxidative Med Cell Longev 2019:2853534–2853516. https://doi.org/10.1155/2019/2853534
Funding
This work was supported by the National Natural Science Foundation of China (nos. 81671960, 81873956, and 81974285).
Author information
Authors and Affiliations
Contributions
Lina Zhang, Xiaobei Peng, Yuhang Ai, and Li Huang conceived and designed the research; Li Li, Songyun Deng, Yan Huang, Yunan Mo, and Qianyi Peng performed the experiments; Shuangpin Zhao, Zhiyong Liu, Yunan Mo, and Qianyi Peng analyzed the data; Lina Zhang and Li Huang wrote the paper.
Corresponding author
Ethics declarations
All protocols were conducted in accordance with the Institutional Animal Care and Use Committee of Central South University.
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, L., Peng, X., Ai, Y. et al. Amitriptyline Reduces Sepsis-Induced Brain Damage Through TrkA Signaling Pathway. J Mol Neurosci 70, 2049–2057 (2020). https://doi.org/10.1007/s12031-020-01611-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-020-01611-x