Abstract
Background
Cholangiocarcinoma (CCA) is the second most frequent primary liver tumor and defined as the heterogeneous group of tumors derived from cells in the biliary tree.
Methods and Results
Based on the anatomical locations (intrahepatic, perihilar, and distal), there are various approaches to the diagnosis and treatment of CCA. Imaging modalities, staging classifications, understandings around natural behavior of CCA, and therapeutic strategies have had remarkable progress in recent years.
Conclusions
This article reviews and discusses the epidemiology, clinical presentation, diagnosis, and treatment modalities of CCA; determines the appropriate inclusion and exclusion criteria for liver transplantation (LT); and defines the risk of disease progression for patients in the waiting list of LT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cholangiocarcinoma (CCA) is the heterogeneous group of tumors derived from cells of the bile ducts and exhibit biliary epithelial differentiation [1]. Anatomically, the disease can be classified into three categories: intrahepatic cholangiocarcinoma (iCCA), hilar CCA, and distal CCA. iCCA arising from proximal to the second-degree bile ducts, hilar CCA is localized between the second-degree bile ducts and the cystic duct, and distal CCA originates distal to the cystic duct [1,2,3]. Although, no specific risk factor has been identified for development of CCA, most cases are sporadic and the underlying etiology is unknown. However, several studies have suggested that chronic biliary inflammation and increased cellular turnover, liver cirrhosis, chronic hepatitis B and C infection, diabetes, obesity, and excess use of alcohol have been linked to higher risks of developing CCA [4]. The diagnosis of CCA is mainly made by both clinical and imaging findings, and whenever the diagnosis of CCA is confirmed, staging of the disease severity is needed to assess the degree of extension of tumor outside the liver and biliary tree [1, 4]. Herein, we aimed to review the epidemiology, clinical presentation, and therapeutic strategies of CCA, and highlight the CCA in the liver transplantation (LT) setting.
Epidemiology of Cholangiocarcinoma
Approximately, 13% of overall cancer-related mortality is due to hepatobiliary malignancies. In this context, CCA accounts for about 15–20% of the primary hepatobiliary malignancies, which makes it the second most common primary liver tumor [5,6,7,8]. The incidence of CCA seems to be increasing, and it is the leading cause of nearly 20% of the deaths from hepatobiliary cancers [5]. The underlying reason for the increasing trend in CCA incidence has not been fully understood so far. Epidemiological studies showed that men have 1.5 fold increased risk of CCA development when compared with women. Moreover, the incidence of CCA is more commonly occurred after the fourth decade of life except for patients with primary sclerosing cholangitis which can present the disease earlier [7, 9, 10].
Classification of CCA
Most commonly, CCA is classified into three groups of intrahepatic (IH-CCA or iCCA), perihilar (pCCA), and distal (dCCA) subtypes which is based on the anatomical location of CCA. pCCA, which is also called Klatskin, and dCCA were previously grouped as extrahepatic CCA (EH-CCA) due to the differences in their tumor biology and management [7, 11].
Clinical Presentation and Diagnosis of Cholangiocarcinoma
The clinical presentation of CCA is often subtle and may manifest without any evident signs and symptoms. In some cases, the manifestation of CCA may cause jaundice as well as non-specific symptoms such as weight loss, night sweets, abdominal pain, emesis, vomiting, loss of appetite, and also the increase of cholestasis related parameters such as alanine transaminase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), alkaline phosphatase (ALP), and Bilirubin [12, 13]. Diagnosis of CCA is by the combination of the clinical presentation, imaging information, and biopsy modalities [7].
Diagnosing the Source of Jaundice
As stated above, jaundice and particularly painless jaundice is one the common presentations of CCA [4, 7]. Generally, the increase of the conjugated bilirubin can be due to the obstruction of biliary ducts that lead to the presence of acholia/pale stools, or it can have intrahepatic (i.e., hepatocellular damage) causes, which acholia does not usually develop (except in the first weeks of acute hepatitis) [14].
Initial Investigations
To determine the source of jaundice, physical examination and blood tests including full liver function should be performed prior to the imaging and other investigations. Generally, the increase of ALP, GGT, bile salts, 5’nucleotidase, or cholesterol is expected but hepatocyte enzymes such as AST are expected to be less elevated [4].
Diagnosis
Currently, there is no standard diagnostic tool for early detection of CCA and therefore could result in longer diagnostic delay and higher morbidity and mortality [15, 16]. Symptoms often developed at advanced stage disease and compared to nonsymptomatic patients; symptomatic patients have a lower chance of tumor resection [17, 18]. Less than half of CCA cases are diagnosed incidentally, for example, by cross-sectional imaging performed for other reasons [2, 17]. Imaging modalities such as ultrasound (US), contrast-enhanced ultrasound (CEUS), computed tomography (CT), magnetic resonance imaging (MRI) and Fludeoxyglucose-positron emission tomography (18FDG-PET) also play a crucial role in other stages of managing such as staging, follow-up, and monitoring the response to the therapy. Studies also show non-morphologic imaging as a potential tool for the prediction of the disease prognosis [19,20,21].
Tumor Markers
Carbohydrate antigen 19–9 (CA 19–9) is the most commonly used tumor marker for CCA and distinguishing CCA from HCC. Although CA 19–9 is more specific than other tumor markers such as CEA and CA-125, it is elevated in benign cholangiopathies or gastrointestinal, pancreatic, and gynecologic malignancies other than CCA. Also, Lewis antigen-negative patients do not express CA 19–9 [7].
Role of Ultrasound for CCA Detection
Although the unenhanced US lacks specific features, it is one of the primary diagnostic tools that shows a high detection rate. Also, CEUS, which is generally used in the setting of chronic liver disease, has a possibility of misclassification between iCCA and HCC in the use of unenhanced US [4, 22, 23] .On the other hand, dCCA is diagnosed with a high accuracy rate of 80–95%, but pCCA is more difficult to identify using the US. Generally, in patients with jaundice which the benign causes for the obstruction of the bile duct are excluded [24]. SpyGlass®, which is a novel endoscopic technique, is suggested as a more sensitive technique for the detection of CCA than other standard endoscopic techniques [25,26,27].
Role of Computed Tomography Imaging
Currently, the standard radiologic assessment for characterization and staging of CCA is CT [28]. The imaging patterns of iCCA in cirrhotic patients displayed as an arterial peripheral-rim enhancement with progressive homogeneous contrast uptake until the delayed or stable contrast uptake through the different dynamic phases [29]. Moreover, additional findings such as capsular retraction, delayed enhancement, satellite nodules, and vascular invasion are mainly supportive of iCCA diagnosis. In some cases that the tumor lesion is smaller than 1 cm, the characterization is challenging specially in in the presence of cirrhosis or atypical features [30]. Also, CT findings can be used in preoperative evaluation of patients’ prognosis, estimation of the resectability of pCCA, and assessment of the involvement of portal vein, hepatic artery, and bile ducts [31]. However, it is less accurate in the identification of lymph nodes and distant metastases [32].
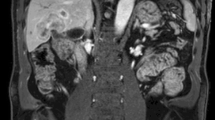
Role of Magnetic Resonance and Other Imaging
Similar to CT, MRI is used in the diagnosis and staging of CCA and could help clinicians in estimation of the respectability of pCCA, and evaluation of the involvement of portal vein and bile ducts [29, 32]. On the other hand, the use of hepato-specific contrast media and diffusion-weighted imaging (DWI) is one of the MRI advantages which are helpful in the discrimination of HCC and iCCA [33]. For the investigation of distant metastasis or nodal metastases, and completing the disease staging, the best modality is 18FDG-PET imagining [4].
Invasive Techniques for Confirmatory Tissue Diagnosis
A biopsy is required to confirm CCA diagnosis, which is minimally invasive in the diagnosis of iCCA and pCCA and mainly performed percutaneously with guiding of US imaging [4, 34]. Studies indicate that employing CEUS imaging increases the accuracy of the liver biopsy compared to the US [4]. The histological diagnosis of iCCA is according to the WHO classification of biliary tract cancer that could be differentiated into two main categories such as adenocarcinoma and mucinous carcinoma [35]. The tubular and/or papillary structures and a variable fibrous stroma are the most common histological findings of an iCCA [36].
Staging Systems of Cholangiocarcinoma
Staging is required to establish a systematic approach to prognostication, therapeutic stratification, and outcome comparison. So far, there are three major staging systems for iCCA including the American Joint Committee on Cancer/Union for International Cancer Control (AJCC/UICC), the National Cancer Center of Japan (NCCN) staging systems, and the Liver Cancer Study Group of Japan (LCSGJ). The AJCC/UICC has shown stage-survival correlation. Generally, cancer itself is staged as a primary tumor (T), regional lymph nodes metastasis (N), and the presence of distant metastases (M). This TNM classification is broadly used in oncology [37].
Therapeutic Strategies for Cholangiocarcinoma
Hepatic Surgery
Although the diagnosis of CCA is made at the late stages in the majority of the cases, the only possible curative option is surgical treatment [18, 38]. On the other hand, in cases with distant metastases, bilateral, multifocal disease, and comorbidities associated with operative risks, surgical resection is not recommended [7]. Also, studies showed that uncorrected preoperative jaundice can be associated with some of the postoperative complications. In the cases of CCA, major postoperative complications are intra-abdominal abscesses, biliary fistulae, sepsis, and bile duct leaks [7, 39, 40].
Nonsurgical Therapies
Various chemotherapy approaches have been proposed for the treatment of CCA patients. Two phase III randomized controlled trials have shown a better outcome and survival rate of CCA patients with combination of gemcitabine/cisplatin therapy when compared to gemcitabine monotherapy and also erlotinib plus gemcitabine/cisplatin compared to gemcitabine/cisplatin, respectively [41, 42]. Other therapeutic methods include radiofrequency ablation, hepatic arterial infusion chemotherapy (HAI), transarterial chemoembolization (TACE), drug-eluting bead-TACE, radioembolization, stereotactic radiotherapy, photodynamic therapy (PDT), and proton beam therapy (PBT) [7, 43,44,45].
First Line Medical Therapy
Most cases of cholangiocarcinoma are unresectable resulting in a poor prognosis. Historically, CCA is considered as chemotherapy-resistant cancer. However, clinical trials have shown that systemic chemotherapy greatly extended the survival of patients with advance CCA. Thus, systemic chemotherapy remains the cornerstone of palliative therapy for the majority of unresectable cholangiocarcinoma cases. Although it has been well-established that cancers arising from various anatomic sites of biliary tree have distinct histological phenotype, clinical trials have been grouped together all intrahepatic, perihilar, distal, gall bladder, and ampullary carcinoma and collectively referred them as biliary cancers. Therefore, it becomes difficult to interpret these findings and also limit the generalizability of the results.
Gemcitabine Plus Cisplatin
Currently, the first-line treatment for advanced unresectable cholangiocarcinoma is based on the combination of gemcitabine plus platinum. In a study done by Valle et al. in 2010 (also known as UK ABC-02 trial), they conducted a clinical trial of cisplatin and gemcitabine in patients with advanced CCA. This study included 241 CCA patients from a total of 410 patients who were randomly assigned to receive gemcitabine alone or in combination with cisplatin [46]. The survival rate of patients who received the doublet was significantly higher than gemcitabine alone (HR, 0.64; 95% CI, 0.52–0.80; P < 0.001). Results also showed that the combination of gemcitabine and cisplatin was well tolerated with similar adverse events between the two groups. These results were supported by a Japanese randomized trial (BT22 study) showing that gemcitabine plus cisplatin therapy was effective and well tolerated [47].
Other Gemcitabine-Based Regimens
Gemcitabine plus S-1 was compared to gemcitabine plus cisplatin in the Japanese phase III FUGA-BT trial [48]. In the preliminary reports, gemcitabine plus S-1 was non-inferior in terms of median overall survival (15.1 versus 13.4 months), median progression-free survival (6.8 versus 5.8 months), and objective response rate (30 versus 32%). Another non-randomized phase II study investigated the substitution of oxaliplatin (GEMOX) for cisplatin as an alternative for standard regiment in patients who are medically unfit to receive cisplatin-based therapy [49]. Findings presented in this study indicated promising results for combination of gemcitabine and oxaliplatin in terms of well tolerability and efficacy. It should be noted that evaluating prognostic factors including gender, disease status, liver metastasis, and number of metastatic sites along with biochemical parameters have been argued to be the most important factors than therapy itself in determining the overall survival outcome [50, 51]. Thus, GEMOX is considered as one of the standard first-line regimens for advanced biliary tract cancer. The combination of gemcitabine plus oxaliplatin (GEMOX) and bevacizumab was also evaluated in a phase II trial [52]. Whether this combination is superior to GEMOX alone or gemcitabine plus cisplatin should be further assessed in larger randomized clinical trials.
Gemcitabine (1000 mg/m2 on days 1 and 8) plus capecitabine (650 mg/m2 twice daily for 14 days of every 21-day cycle) is another gemcitabine base regimen for cholangiocarcinoma. In Knox et al. trial [53], the overall survival rate was reported to be 12.7 months. However, another study conducted by the Southwest Oncology Group (SWOG) reported that the median survival rate was to be only 7 months [54].
Weekly gemcitabine plus nab-paclitaxel combination has been evaluated in a phase II trial for metastatic cholangiocarcinoma with the median overall survival of 12.4 months [55]. Shroff et al.’s [56] phase II study of the combination of gemcitabine, cisplatin, and nab-paclitaxel reported a median progression-free and overall survival rate of 11.8 and 19.2 months, respectively.
Several new cytotoxic agents have also been proposed to possibly enhance the efficacy of chemotherapy treatment. In particular, docetaxel, paclitaxel, and irinotecan have been added to doublet reference chemotherapy regimen, but the results showed unfavorable outcomes such as lower response rate and disease control rate [57]. An ongoing phase II/III trial named AMEBICA are undertaken to determine whether FOLFIRINOX or in combination with gemcitabine/cisplatin could further improve the outcomes of patients with locally advanced non-resectable or metastatic biliary tract cancer [58].
Patients with Persistent Biliary Obstruction
For patients who have persistent hyperbilirubinemia despite stenting, a non-gemcitabine-based regimen, such as fluoropyrimidine plus oxaliplatin, is a good option. In recent studies, FU-based combination therapies may reach a longer overall survival rate but did not seen to be exceeded more than 1 year [59].
Second Line Medical Therapy
Currently, there is no effective second-line treatment in regard to any advantages over best supportive care in a prospective RCT. Therefore, it is still unclear whether administering chemotherapy could benefit patients failing the standard first-line treatment [60,61,62]. In addition, the rapid deteriorating nature of CCA mostly precludes further evaluation of second-lines of treatment. It is noteworthy that based on small prospective phase II studies, approximately 20–40% of patients are offered an alternative chemotherapy regimen that can benefit highly selected patient populations [19, 63]. In terms of second-line treatment, a fluoropyrimidine-based schedule is considered as the most appropriate regimen in this setting [64]. However, the major limitations in proposing the best second-line treatment option are due to marked heterogeneity across studies as well as poor level of evidence. Thus, future well-designed prospective trials are warranted to elucidate these findings.
Phase III randomized ABC-06 study showed an overall better survival rate of FOLFOX chemotherapy when compared to BSC alone (6.2 vs. 5.3 months). However, although FOLFOX is considered as the standard of treatment following progression on cisplatin/gemcitabine (CisGem), the benefit was modest in Lamarca et al.’s study [65]. Moreover, in preliminary results presented at the 2019 annual American Society of Clinical Oncology (ASCO) meeting, FOLFOX has been shown to be significantly associated with better overall survival outcomes (26% vs 11% for 1 year).
Immunotherapy
One of the biggest breakthroughs in the last decade of cancer research was cancer immunotherapy. The growing body of evidence suggested that immune checkpoints and other T cell coinhibitory pathways could have a significant impact on anti-tumor immune response and increased overall survival rates in patients with various solid organ tumors. The anti-tumor activity of monoclonal antibodies is based on initiate or inhibit programmed cell death. There have been two major immunosuppressive pathways to operate against two distinct inhibitory receptors on T cells including programmed death-1 (PD1) and cytotoxic T lymphocyte antigen-4 (CTLA-4) and their specific ligands. These checkpoints are known as negative regulator of immune recognition to prevent excessive inflammation. Phase 1b trial of pembrolizumab monotherapy has been conducted on 89 patients with biliary tract cancer [66]. Thirty-seven patients (42%) who were assessed for PD-L1 expression had positive PD-L1. Twenty-four patients were received pembrolizumab in which 4 patients (17%) developed partial response and 4 (17%) were found to have stable disease. Other studies have shown similar responses in treatment with pembrolizumab among patients with biliary tract cancer and expressing PD-L1 [67, 68]. A phase II clinical trial (NCT03704480) is underway investigating durvalumab (anti-PD-L1) in combination with tremelimumab (anti- CTLA-4) with or without paclitaxel in patients with advanced CCA. The use of immunotherapy for treatment of advanced biliary cancer is on its early stages, and within the following years, our understanding regarding the administration of these agents will substantially increase our knowledge in the management of CCA.
Indication for Liver Transplantation
Liver Transplantation Alone
Orthotopic liver transplantation (OLT) is potentially a promising treatment modality due to its ability to achieve a tumor-free margin and perform a radical resection. In contrast, studies have reported that 5-year survival is only 28% in which the tumor recurs in nearly half of the patient, and the long-term survival is less than 20% [69,70,71]. The majority of recurrences develop within the first 2 years, and studies showed no association between adjuvant therapy and survival (Goldstein et al. 1993). Therefore, although OLT is an effective treatment for pCCA (with a recurrence-free 5-year survival 68%), OLT is not a recommended option in the treatment of CCA as a monotherapy [71].
Neoadjuvant Therapy and Liver Transplantation
Currently, the consideration for performing LT in patients with iCCA is not recommended mainly due to the lack of evidence and controversial reported outcomes [34]. The unsatisfactory long-term survival outcomes of patients who underwent LT made this procedure useless [72]. Patients who underwent LT alone have a 3-year survival of 50–65% [73]. The concomitant chemotherapies are an essential element in enhancing the survival rate with those who underwent neoadjuvant therapy in combination with LT often show better long-term survival outcome [74]. Although patients who underwent liver transplantation alone have overall poor results, those with absence of regional lymph node metastases showed better outcome following LT [75]. Despite promising results of local tumor control in the management of iCCA, the complications related to high-dose of brachytherapy are still challenging and attributed to high morbidity and mortality [76].
Prediction of Tumor Recurrence after Orthotopic Liver Transplantation
As mentioned previously, preoperative staging and neoadjuvant chemoradiation treatment in liver transplantation settings may result in an excellent long-term recurrence-free survival in early-stage cases with small hilar CCA [77]. Studies show aggressive tumor biology, perineural invasion, and including multifocality, but not tumor size can be independent predictors of tumor recurrence [74]. It seems a clinical model is still needed to guide the use of OLT and predict its outcomes.
Future Directions
Current clinical trials in the area of CCA are mainly limited by the sample size. Also, dissection of the molecular pathways causing CCA will help in the selection of an individualized medicine approach. On the other hand, there are few studies on evaluation of the therapeutic efficacy of targeted agents combined with retrospective analysis of transcriptomic data, but clinical trials are in favor of targeting EGFR combined with other molecular targets or chemotherapeutics [41]. Other promising approaches include Targeting JAK/STAT3 [78], Inhibition of IDH1/2-mutations [79], Targeting of cancer-associated fibroblasts (CAFs) [80], and targeting FGFR2 [81]. Identification of new and more specific tumor biomarkers is another important future direction [82]. Electrospray ionization tandem mass spectrometry (ESI-MS), surface-enhanced laser desorption, two-dimensional gel electrophoresis or ionization, protein chips, and proteome analysis are other technologies that can be used in the development of new specific diagnostic methods [83].
Conclusions
Therapeutic options for management of CCA are limited and associated with poor outcome and mortality. Despite recent advances in diagnostic modalities of CCA such as imaging and cytopathology techniques, early detection of CCA is still challenging. Clinical diagnosis of CCA is based on radiological evidence of malignant strictures of the common bile duct, increased serum levels of CA 19–9, malignant-looking appearance of a lesion during MRI, and normal serum levels of IgG4 level. Liver transplantation in combination with neoadjuvant chemotherapy has shown to improve overall survival rate among CCA patients.
References
Zamora-Valdes D, Heimbach JK. Liver transplant for cholangiocarcinoma. Gastroenterol Clin. 2018;47(2):267–80.
Banales JM, Cardinale V, Carpino G, Marzioni M, Andersen JB, Invernizzi P, et al. Expert consensus document: cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA). Nat Rev Gastroenterol Hepatol. 2016;13(5):261.
Rizvi S, Gores GJ. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology. 2013;145(6):1215–29.
Forner A, Da Fonseca LG, Díaz-González Á, Sanduzzi-Zamparelli M, Reig M, Bruix J. Controversies in the management of hepatocellular carcinoma. JHEP Reports. 2019.
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part III: liver, biliary tract, and pancreas. Gastroenterology. 2009;136(4):1134–44.
Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011;54(1):173–84.
Blechacz B. Cholangiocarcinoma: current knowledge and new developments. Gut Liver. 2017;11(1):13–26.
Kirstein MM, Vogel A. Epidemiology and risk factors of cholangiocarcinoma. Visc Med. 2016;32(6):395–400.
Rizvi S, Gores GJ. Current diagnostic and management options in perihilar cholangiocarcinoma. Digestion. 2014;89(3):216–24.
Qureshi K, Jesudoss R, Al-Osaimi AM. The treatment of cholangiocarcinoma: a hepatologist's perspective. Curr Gastroenterol Rep. 2014;16(10):412.
Welzel TM, McGlynn KA, Hsing AW, O'Brien TR, Pfeiffer RM. Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra-and extrahepatic cholangiocarcinoma in the United States. J Natl Cancer Inst. 2006;98(12):873–5.
DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245(5):755–62.
Bragazzi MC, Cardinale V, Carpino G, Venere R, Semeraro R, Gentile R, et al. Cholangiocarcinoma: epidemiology and risk factors. Transl Gastrointest Cancer. 2011;1(1):21–32.
Sullivan JI, Rockey DC. Diagnosis and evaluation of hyperbilirubinemia. Curr Opin Gastroenterol. 2017;33(3):164–70.
Blechacz B, Komuta M, Roskams T, Gores GJ. Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 2011;8(9):512–22.
Lozada ME, Chaiteerakij R, Roberts LR. Screening for hepatocellular carcinoma and cholangiocarcinoma: can biomarkers replace imaging? Curr Hepatol Rep. 2015;14(2):128–38.
Morimoto Y, Tanaka Y, Ito T, Nakahara M, Nakaba H, Nishida T, et al. Long-term survival and prognostic factors in the surgical treatment for intrahepatic cholangiocarcinoma. J Hepato-Biliary-Pancreat Surg. 2003;10(6):432–40.
Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008;248(1):84–96.
Lamarca A, Hubner RA, David Ryder W, Valle JW. Second-line chemotherapy in advanced biliary cancer: a systematic review. Ann Oncol. 2014;25(12):2328–38.
Joo I, Lee JM, Yoon JH. Imaging diagnosis of intrahepatic and perihilar cholangiocarcinoma: recent advances and challenges. Radiology. 2018;288(1):7–13.
Brungs D, Aghmesheh M, Sjoquist K, Goldstein D. Systemic treatment in advanced biliary cancers: a multicenter Australian analysis and review. Asia Pac J Clin Oncol. 2017;13(5):e291–e7.
Galassi M, Iavarone M, Rossi S, Bota S, Vavassori S, Rosa L, et al. Patterns of appearance and risk of misdiagnosis of intrahepatic cholangiocarcinoma in cirrhosis at contrast enhanced ultrasound. Liver Int. 2013;33(5):771–9.
Vidili G, Sio I, D’Onofrio M, Mirk P, Bertolotto M, Schiavone C. SIUMB guidelines and recommendations for the correct use of ultrasound in the management of patients with focal liver disease. 2018.
Hennedige TP, Neo WT, Venkatesh SK. Imaging of malignancies of the biliary tract-an update. Cancer Imaging. 2014;14(1):14.
Williamson J, Draganov P. The usefulness of SpyGlass™ choledochoscopy in the diagnosis and treatment of biliary disorders. Curr Gastroenterol Rep. 2012;14(6):534–41.
Laleman W, Verraes K, Van Steenbergen W, Cassiman D, Nevens F, Van der Merwe S, et al. Usefulness of the single-operator cholangioscopy system SpyGlass in biliary disease: a single-center prospective cohort study and aggregated review. Surg Endosc. 2017;31(5):2223–32.
Labib PL, Davidson BR, Sharma RA, Pereira SP. Locoregional therapies in cholangiocarcinoma. Hepat Oncol. 2017;4(4):99–109.
Olthof SC, Othman A, Clasen S, Schraml C, Nikolaou K, Bongers M. Imaging of cholangiocarcinoma. Visc Med. 2016;32(6):402–10.
Abolhassani H, Kiaee F, Tavakol M, Chavoshzadeh Z, Mahdaviani SA, Momen T, et al. Fourth update on the Iranian National Registry of Primary Immunodeficiencies: integration of molecular diagnosis. J Clin Immunol. 2018;38(7):816–32.
Mar WA, Shon AM, Lu Y, Jonathan HY, Berggruen SM, Guzman G, et al. Imaging spectrum of cholangiocarcinoma: role in diagnosis, staging, and posttreatment evaluation. Abdom Radiol (NY). 2016;41(3):553–67.
Zhang H, Zhu J, Ke F, Weng M, Wu X, Li M, et al. Radiological imaging for assessing the respectability of hilar cholangiocarcinoma: a systematic review and meta-analysis. Biomed Res Int. 2015;2015.
Ruys A, Van Beem B, Engelbrecht M, Bipat S, Stoker J, Van Gulik T. Radiological staging in patients with hilar cholangiocarcinoma: a systematic review and meta-analysis. Br J Radiol. 2012;85(1017):1255–62.
Jhaveri KS, Hosseini-Nik H. MRI of cholangiocarcinoma. J Magn Reson Imaging. 2015;42(5):1165–79.
Bridgewater J, Galle PR, Khan SA, Llovet JM, Park J-W, Patel T, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60(6):1268–89.
Hamilton SR, Aaltonen LA. WHO classification of tumours. Pathology and genetics of tumours of the digestive system. Geneva: World health organization; 2000.
Goodman ZD. Neoplasms of the liver. Mod Pathol. 2007;20(1s):S49.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin. 2017;67(2):93–9.
Konstadoulakis MM, Roayaie S, Gomatos IP, Labow D, Fiel M-I, Miller CM, et al. Fifteen-year, single-center experience with the surgical management of intrahepatic cholangiocarcinoma: operative results and long-term outcome. Surgery. 2008;143(3):366–74.
Yoshida T, Matsumoto T, Sasaki A, Morii Y, Aramaki M, Kitano S. Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer. Arch Surg. 2002;137(1):69–73.
Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, et al. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 2005;137(4):396–402.
Lee HM, Jeong Y-I, Kim DH, Kwak TW, Chung C-W, Kim CH, et al. Ursodeoxycholic acid-conjugated chitosan for photodynamic treatment of HuCC-T1 human cholangiocarcinoma cells. Int J Pharm. 2013;454(1):74–81.
Valle JW, Wasan H, Johnson P, Jones E, Dixon L, Swindell R, et al. Gemcitabine alone or in combination with cisplatin in patients with advanced or metastatic cholangiocarcinomas or other biliary tract tumours: a multicentre randomised phase II study–the UK ABC-01 study. Br J Cancer. 2009;101(4):621–7.
Konstantinidis IT, Arkadopoulos N, Ferrone CR. Surgical management of intrahepatic cholangiocarcinoma in the modern era: advances and challenges. Chin Clin Oncol. 2016;5(1):9.
Ortner ME, Caca K, Berr F, Liebetruth J, Mansmann U, Huster D, et al. Successful photodynamic therapy for nonresectable cholangiocarcinoma: a randomized prospective study. Gastroenterology. 2003;125(5):1355–63.
Ibarra RA, Rojas D, Snyder L, Yao M, Fabien J, Milano M, et al. Multicenter results of stereotactic body radiotherapy (SBRT) for non-resectable primary liver tumors. Acta Oncol. 2012;51(5):575–83.
Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362(14):1273–81.
Okusaka T, Nakachi K, Fukutomi A, Mizuno N, Ohkawa S, Funakoshi A, et al. Gemcitabine alone or in combination with cisplatin in patients with biliary tract cancer: a comparative multicentre study in Japan. Br J Cancer. 2010;103(4):469–74.
Morizane C, Okusaka T, Mizusawa J, Katayama H, Ueno M, Ikeda M, et al. Randomized phase III study of gemcitabine plus S-1 combination therapy versus gemcitabine plus cisplatin combination therapy in advanced biliary tract cancer: a Japan Clinical Oncology Group study (JCOG1113, FUGA-BT). J Clin Oncol. 2018;36(4_suppl):205.
Andre T, Reyes-Vidal JM, Fartoux L, Ross P, Leslie M, Rosmorduc O, et al. Gemcitabine and oxaliplatin in advanced biliary tract carcinoma: a phase II study. Br J Cancer. 2008;99(6):862–7.
Bridgewater J, Lopes A, Wasan H, Malka D, Jensen L, Okusaka T, et al. Prognostic factors for progression-free and overall survival in advanced biliary tract cancer. Ann Oncol. 2016;27(1):134–40.
Peixoto RD, Renouf D, Lim H. A population based analysis of prognostic factors in advanced biliary tract cancer. J Gastrointest Oncol. 2014;5(6):428–32.
Zhu AX, Meyerhardt JA, Blaszkowsky LS, Kambadakone AR, Muzikansky A, Zheng H, et al. Efficacy and safety of gemcitabine, oxaliplatin, and bevacizumab in advanced biliary-tract cancers and correlation of changes in 18-fluorodeoxyglucose PET with clinical outcome: a phase 2 study. Lancet Oncol. 2010;11(1):48–54.
Knox JJ, Hedley D, Oza A, Feld R, Siu LL, Chen E, et al. Combining gemcitabine and capecitabine in patients with advanced biliary cancer: a phase II trial. J Clin Oncol. 2005;23(10):2332–8.
Iqbal S, Rankin C, Lenz H-J, Gold PJ, Ahmad SA, El-Khoueiry AB, et al. A phase II trial of gemcitabine and capecitabine in patients with unresectable or metastatic gallbladder cancer or cholangiocarcinoma: southwest oncology group study S0202. Cancer Chemother Pharmacol. 2011;68(6):1595–602.
Sahai V, Catalano PJ, Zalupski MM, Lubner SJ, Menge MR, Nimeiri HS, et al. Nab-paclitaxel and gemcitabine as first-line treatment of advanced or metastatic cholangiocarcinoma: a phase 2 clinical trial. JAMA Oncol. 2018;4(12):1707–12.
Shroff RT, Javle MM, Xiao L, Kaseb AO, Varadhachary GR, Wolff RA, et al. Gemcitabine, cisplatin, and nab-paclitaxel for the treatment of advanced biliary tract cancers: a phase 2 clinical trial. JAMA Oncol. 2019;5(6):824–30.
Eckel F, Schmid RM. Chemotherapy in advanced biliary tract carcinoma: a pooled analysis of clinical trials. Br J Cancer. 2007;96(6):896–902.
Phelip J-M, Edeline J, Blanc J-F, Barbier E, Michel P, Bourgeois V, et al. Modified FOLFIRINOX versus CisGem first-line chemotherapy for locally advanced non resectable or metastatic biliary tract cancer (AMEBICA)-PRODIGE 38: study protocol for a randomized controlled multicenter phase II/III study. Dig Liver Dis. 2019;51(2):318–20.
Choi CW, Choi IK, Seo JH, Kim BS, Kim JS, Kim CD, et al. Effects of 5-fluorouracil and leucovorin in the treatment of pancreatic-biliary tract adenocarcinomas. Am J Clin Oncol. 2000;23(4):425–8.
Kobayashi S, Ueno M, Sugimori K, Morizane C, Kojima Y, Irie K, et al. Phase II study of fixed dose-rate gemcitabine plus S-1 as a second-line treatment for advanced biliary tract cancer. Cancer Chemother Pharmacol. 2017;80(6):1189–96.
Jung JH, Lee HS, Jo JH, Cho IR, Chung MJ, Bang S, et al. Combination therapy with capecitabine and cisplatin as second-line chemotherapy for advanced biliary tract cancer. Chemotherapy. 2017;62(6):361–6.
Kim R, Chiorean EG, Amin M, Rocha-Lima CMS, Gandhi J, Harris WP, et al. Phase 2 study of combination SPI-1620 with docetaxel as second-line advanced biliary tract cancer treatment. Br J Cancer. 2017;117(2):189–94.
Fornaro L, Cereda S, Aprile G, Di Girolamo S, Santini D, Silvestris N, et al. Multivariate prognostic factors analysis for second-line chemotherapy in advanced biliary tract cancer. Br J Cancer. 2014;110(9):2165–9.
Kim BJ, Yoo C, Kim KP, Hyung J, Park SJ, Ryoo BY, et al. Efficacy of fluoropyrimidine-based chemotherapy in patients with advanced biliary tract cancer after failure of gemcitabine plus cisplatin: retrospective analysis of 321 patients. Br J Cancer. 2017;116(5):561–7.
Lamarca A, Palmer DH, Wasan HS, Ross PJ, Ma YT, Arora A, et al. ABC-06 | A randomised phase III, multi-centre, open-label study of active symptom control (ASC) alone or ASC with oxaliplatin / 5-FU chemotherapy (ASC+mFOLFOX) for patients (pts) with locally advanced / metastatic biliary tract cancers (ABC) previously-treated with cisplatin/gemcitabine (CisGem) chemotherapy. J Clin Oncol. 2019;37(15_suppl):4003.
O'Neil BH, Wallmark J, Lorente D, Elez E, Raimbourg J, Gomez-Roca C, et al. 502 pembrolizumab (MK-3475) for patients (pts) with advanced colorectal carcinoma (CRC): preliminary results from KEYNOTE-028. Eur J Cancer. 2015;51:S103.
Meng X, Huang Z, Teng F, Xing L, Yu J. Predictive biomarkers in PD-1/PD-L1 checkpoint blockade immunotherapy. Cancer Treat Rev. 2015;41(10):868–76.
Gani F, Nagarajan N, Kim Y, Zhu Q, Luan L, Bhaijjee F, et al. Program death 1 immune checkpoint and tumor microenvironment: implications for patients with intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2016;23(8):2610–7.
Meyer CG, Penn I, James L. Liver transplantation for cholangiocarcinoma: results in 207 patients1. Transplantation. 2000;69(8):1633–7.
Rosen C, Heimbach J, Gores GJ. Surgery for cholangiocarcinoma: the role of liver transplantation. Hpb. 2008;10(3):186–9.
Murad SD, Kim WR, Therneau T, Gores GJ, Rosen CB, Martenson JA, et al. Predictors of pretransplant dropout and posttransplant recurrence in patients with perihilar cholangiocarcinoma. Hepatology. 2012;56(3):972–81.
Facciuto ME, Singh MK, Lubezky N, Selim MA, Robinson D, Kim-Schluger L, et al. Tumors with intrahepatic bile duct differentiation in cirrhosis: implications on outcomes after liver transplantation. Transplantation. 2015;99(1):151–7.
Fu Y, Yang W, Wu W, Yan K, Xing B-c, Chen M-h. Radiofrequency ablation for postoperative recurrences of intrahepatic cholangiocarcinoma. Chin J Cancer Res. 2011;23(4):295–300.
Hong JC, Jones CM, Duffy JP, Petrowsky H, Farmer DG, French S, et al. Comparative analysis of resection and liver transplantation for intrahepatic and hilar cholangiocarcinoma: a 24-year experience in a single center. Arch Surg. 2011;146(6):683–9.
Shimoda M, Farmer DG, Colquhoun SD, Rosove M, Ghobrial RM, Yersiz H, et al. Liver transplantation for cholangiocellular carcinoma: analysis of a single-center experience and review of the literature. Liver Transpl. 2001;7(12):1023–33.
De Vreede I, Steers JL, Burch PA, Rosen CB, Gunderson LL, Haddock MG, et al. Prolonged disease-free survival after orthotopic liver transplantation plus adjuvant chemoradiation for cholangiocarcinoma. Liver Transpl. 2000;6(3):309–16.
Heimbach JK, Gores GJ, Nagorney DM, Rosen CB. Liver transplantation for perihilar cholangiocarcinoma after aggressive neoadjuvant therapy: a new paradigm for liver and biliary malignancies? Surgery. 2006;140(3):331–4.
Sia D, Tovar V, Moeini A, Llovet J. Intrahepatic cholangiocarcinoma: pathogenesis and rationale for molecular therapies. Oncogene. 2013;32(41):4861–70.
Chng KR, Chan SH, Ng AHQ, Li C, Jusakul A, Bertrand D, et al. Tissue microbiome profiling identifies an enrichment of specific enteric bacteria in Opisthorchis viverrini associated cholangiocarcinoma. EBioMedicine. 2016;8:195–202.
Mertens JC, Fingas CD, Christensen JD, Smoot RL, Bronk SF, Werneburg NW, et al. Therapeutic effects of deleting cancer-associated fibroblasts in cholangiocarcinoma. Cancer Res. 2013;73(2):897–907.
Borad MJ, Champion MD, Egan JB, Liang WS, Fonseca R, Bryce AH, et al. Integrated genomic characterization reveals novel, therapeutically relevant drug targets in FGFR and EGFR pathways in sporadic intrahepatic cholangiocarcinoma. PLoS Genet. 2014;10(2):e1004135.
Kisiel JB, Dukek BA, V S R Kanipakam R, Ghoz HM, Yab TC, Berger CK, et al. Hepatocellular carcinoma detection by plasma methylated DNA: discovery, phase I pilot, and phase II clinical validation. Hepatology. 2019;69(3):1180–92.
Takahashi M, Wakabayashi G, Nitta H, Takeda D, Hasegawa Y, Takahara T, et al. Pure laparoscopic right hepatectomy by anterior approach with hanging maneuver for large intrahepatic cholangiocarcinoma. Surg Endosc. 2013;27(12):4732–3.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moazzami, B., Majidzadeh-A, K., Dooghaie-Moghadam, A. et al. Cholangiocarcinoma: State of the Art. J Gastrointest Canc 51, 774–781 (2020). https://doi.org/10.1007/s12029-020-00390-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-020-00390-3