Abstract
Objectives
To investigate the effect of left colonic artery (LCA) preservation on laparoscopic sigmoidectomy outcomes
Methods
We identified 447 consecutive patients who underwent laparoscopic sigmoidectomy at our hospital group between January 2010 and December 2016. We divided the patients into groups with and without LCA preservation and with and without anastomotic leakage (AL). We compared the patient age and gender, tumor location, stage, D2/D3 lymph node dissection, comorbidities, operating time, and blood loss between these groups. Univariate and multivariate analyses were performed to determine the risk factors for AL.
Results
There were significant differences in age, sex, tumor location, D2/D3 lymph node dissection, hypertension, operating time, blood loss, and AL for groups with and without LCA preservation. There were significant differences in sex, tumor location, and LCA preservation for groups with and without AL. Multivariate analysis showed male sex (hazard ratio (HR) = 6.37, 95% confidence interval (CI) 2.39–20.6; p < 0.0001), non-LCA preservation (HR = 5.01, 95% CI 1.41–31.8.0; p = 0.01), and rectosigmoidal tumor location (HR = 2.51, 95% CI 1.15–5.61; p = 0.01) as significant independent risk factors for AL.
Conclusions
Based on the results obtained by performing laparoscopic operation for sigmoid colon cancer and rectosigmoid cancer, the LCA preservative procedure is warranted for prevention of AL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sigmoidectomy and anterior resection are common surgical procedures for sigmoid colon cancer. Various patient characteristics (age, gender) and comorbidities (i.e., heart failure and renal failure, diabetes mellitus, hypertension, and chronic pulmonary disease) have been shown to affect postsurgical outcomes. Many surgeons prefer to perform a high tie (ligation by the root of the inferior mesenteric artery: IMA) during oncological sigmoid colon surgery. As a result, the left colic artery (LCA) must be sacrificed, making the blood supply to the anastomosis dependent on the superior mesenteric artery (SMA). Anastomotic leakage (AL) is a not-infrequent complication of this procedure, with an incidence ranging from 1.8 to 15.9% [1]. Consequently, a high tie might lead to an insufficient blood supply to the proximal anastomotic limb. In patients with rectal cancer, because a distal margin of ≥ 2 cm is recommended during sphincter-preserving surgery for rectal carcinoma, there is often no issue of selecting the distal margin [2]. However, in sigmoid colon cancer and rectosigmoid cancer, the surgeon must be entrusted with deciding on both the proximal and distal margins.
Anastomotic sealing using fibrin glue has been used as one approach to reducing AL, [3], and indocyanine green fluorescence imaging is useful for intra-operative monitoring [4]. As an alternative surgical approach, preservation of the left colonic artery (LCA) has been known to maintain blood flow to the anastomosis [5]. However, several studies have shown the importance of lymph node dissection up to the root of the IMA for better survival and precise staging [6]. There have been few studies comparing the outcomes of LCA-preserving and LCA-non-preserving colectomy in colon cancer patients [7, 8]. Recently, laparoscopic surgery has become as common as open surgery for sigmoid cancer [9, 10]. However, the technique of lymph node dissection around the IMA with preservation of the LCA technically demands a long time. Therefore, our objective was to evaluate the differences in patient characteristics and perioperative outcomes between LCA-preserving and LCA-non-preserving colectomy for sigmoid colon cancer and rectosigmoid cancer.
Methods
We reviewed the cases of 447 consecutive patients at our hospital group who underwent curative resection for the treatment of sigmoid colon cancer between January 2010 and December 2016. Rectosigmoid colon cancer was included in this analysis. All cases of emergency operations, stage IV cancer, stoma creation and double cancers were excluded from the analysis. We divided the patients into those with and without LCA preservation; we also analyzed those with and without AL. We compared the following factors between the LCA-preserving and LCA-non-preserving groups: patient age, gender, tumor location, and stage. This retrospective study was approved by our hospital’s Institutional Review Board, and the requirement for patient consent was waived.
Definitions
Most of the total and tumor-specific mesorectal excisions were performed by two teams of staff colorectal surgeons. LCA preservation was performed selectively based on the surgeon’s opinion on the situation. The method for D3 laparoscopic lymph node dissection was described previously [5]. The staging of all cancers was performed according to the TNM Classification of Malignant Tumors, seventh edition (TNM 7th).
Clinical anastomotic leakage was defined as the discharge of pus or feces along with fever and symptoms of infection, without communication between the pelvic fluid collection and the anastomotic site. Intra-abdominal abscess was not considered AL.
Statistical Analyses
Categorical variables were compared by the chi-square test when appropriate. Continuous variables are presented as median values and inter-quartile ranges, and comparison was made with the Mann–Whitney U test. Logistic regression analysis of postoperative AL complications was used for multivariate analysis.
Results
Patient Characteristics
Table 1 summarizes the clinicopathologic characteristics of the 447 patients who underwent surgical resection for sigmoid colon cancer. The study group comprised 262 males and 185 females aged 28–89 years (median 66 years). The tumor location was sigmoid (S) in 298 patients (66.6%) and rectosigmoid (RS) in 149 (33.3%). Regarding TNM staging, five patients (1.1%) were stage 0, 152 patients (34.0%) were stage I, 148 patients (33.1%) were stage II, and 142 patients (31.8%) were stage III. As for complications, 31 patients (6.9%) suffered ALs. Concomitant medical risk factors we examined were hypertension, diabetes, coronary heart disease, renal insufficiency, and chronic obstructive pulmonary disease.
Left Colonic Artery Preservation Prevented Anastomotic Leakage
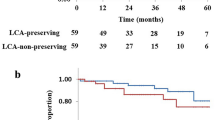
Left colonic artery preservation was performed in 129 patients (the LCA group), and high ligation without preservation was performed in 318 patients (the non-LCA group). Short-term outcomes are shown in Table 2. No significant differences in stage or comorbidities except for hypertension were found between patients who had received LCA preservation and those who had not received it. There was a significantly higher age (mean, 70 vs. 64; P < 0.0001), and larger percentage of hypertension patients (37.2 vs. 23.2%; p = 0.003) in the LCA group. D2 lymph node resection was preferred for the LCA group (p < 0.0001). The operating time differences of the LCA and non-LCA group were statistically significant (p = 0.04). Intra-operative blood loss was significantly lower for high-tie colectomies compared with low-tie laparoscopic procedures (mean, 78 vs. 48 g; P < 0.0001). The rate of AL was lower in the LCA group than in the non-LCA group (1.5 vs. 10.0%, P = 0.004).
High-Tie Ligation Is an Independent Risk Factor of Anastomotic Leakage
We next divided patients into AL (n = 31) and non-AL groups (n = 416). Univariate analysis of the whole data showed that AL was associated with male patients (p = 0.003), rectosigmoid tumor location (p < 0.0001), and non-LCA-preserving surgery (p = 0.004) (Table 3). Multivariate analysis demonstrated that all of these factors increased the risk of AL development: male gender (HR, 6.37; 95% CI, 2.39–20.6; P < 0.0001), rectosigmoid location (HR, 2.51; 95% CI, 1.15–5.61; P = 0.02), and high-tie resection (HR, 5.01; 95% CI, 1.41–31.8; P = 0.01) (Table 4).
Discussion
We found that high-tie surgery is a risk factor for AL in patients undergoing surgery for sigmoid and rectosigmoid colon cancer. A high tie for arterial ligation is known to decrease the blood flow to the anastomosis after rectal surgery [11]. When a high tie is performed, blood is supplied to the distal rectum only via the SMA pathway (the marginal artery and the arc of Riolan). The arc of Riolan is thought to be an enlargement of a normally existing collateral vessel. However, this artery is absent in about 5% of individuals, and only the marginal artery supplies blood from the SMA pathway to the IMA pathway. Moreover, Griffiths’ point is well-known as the critical point at the splenic flexure for collateral circulation between the SMA and the marginal artery branch of the IMA. Analysis of arteriographic studies shows that anastomosis at Griffiths’ point is present in 48% of patients, poor or tenuous in 9 %, and absent in 43% [12]. Thus, anatomic variations can also affect the colonic artery. It is generally difficult to diagnose such vascular variations on routine preoperative radiologic examinations.
Generally, in older patients with atherosclerotic vessels, ligation of IMA might result in hypoperfusion of the proximal limb [11]. Our analysis showed no significant effect of hypertension, diabetes, coronary heart disease, renal insufficiency, or chronic obstructive pulmonary disease. However, male sex, high-tie surgery, and rectosigmoidal tumor location were independent AL risk factors. Sex and tumor location are well-known risk factors from previous studies [1, 13]. As for blood supply, in the surgical community, many surgeons believe that IMA ligation necessitates a larger sigmoid resection. Consequently, mobilization of the splenic flexure would always be necessary. Previously published data showed that low tie is anatomically less invasive with respect to circulation in rectal cancer surgery [14]. However, little is known about the role of artery supply after sigmoidectomy and anterior resection. We should pay attention to both margins in cases with this location for prevention of AL. Some studies insisted high tie confers no increased risk of anastomotic leakage [15]. There is also a thought that high tie can also increase the length of the proximal limb and thereby decrease the tension on the anastomosis and thereby reduce anastomotic leaks [7]. However, Buunen et al. [16] insisted that it was not necessary to perform a high ligation to create a tension-free anastomosis and that low ligation could be safely applied in 80% of cases. Thus, it is controversy to keep the proximal colonic length by high ligation.
Recently, it was reported that the laparoscopic approach to Japanese D3 dissection has safety and clinical short-term benefits compared to open surgery [17]. However, just as previous studies have shown, our data indicated that laparoscopic D3 dissection of lymph nodes with preservation of the LCA was technically demanding and requires a long time [5].
The main limitation of our study lies in its retrospective nature. We believe that future studies should focus on recurrence-free survival and overall survival by LCA preservation because Japanese D3 dissection is difficult in cases of LCA preservation.
In conclusion, laparoscopic colon resection in patients with LCA preservation is a safe and feasible option for AL prevention.
Abbreviations
- LCA:
-
Left colonic artery
- IMA:
-
Inferior mesenteric artery
- AL:
-
Anastomotic leakage
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- DM:
-
Diabetes mellitus
- HT:
-
Hypertension
References
Frasson M, Flor-Lorente B, Rodriguez JL, Granero-Castro P, Hervas D, et al. Risk factors for anastomotic leak after colon resection for cancer: multivariate analysis and nomogram from a multicentric, prospective, National Study with 3193 patients. Ann Surg. 2015;262:321–30.
Park IJ, Kim JC. Adequate length of the distal resection margin in rectal cancer: from the oncological point of view. J Gastrointest Surg. 2010;14:1331–7.
Kim HJ, Huh JW, Kim HR, Kim YJ. Oncologic impact of anastomotic leakage in rectal cancer surgery according to the use of fibrin glue: case-control study using propensity score matching method. Am J Surg. 2013.
Kawada K, Hasegawa S, Wada T, Takahashi R, Hisamori S, Hida K, et al. Evaluation of intestinal perfusion by ICG fluorescence imaging in laparoscopic colorectal surgery with DST anastomosis. Surg Endosc. 2017;31:1061–9.
Sekimoto M, Takemasa I, Mizushima T, Ikeda M, Yamamoto H, Doki Y, et al. Laparoscopic lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery. Surg Endosc. 2011;25:861–6.
Kanemitsu Y, Hirai T, Komori K, Kato T. Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery. Br J Surg. 2006;93:609–15.
Yasuda K, Kawai K, Ishihara S, Murono K, Otani K, Nishikawa T, et al. Level of arterial ligation in sigmoid colon and rectal cancer surgery. World J Surg Oncol. 2016;14:99.
Hinoi T, Okajima M, Shimomura M, Egi H, Ohdan H, Konishi F, et al. Effect of left colonic artery preservation on anastomotic leakage in laparoscopic anterior resection for middle and low rectal cancer. World J Surg. 2013;37:2935–43.
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372:1324–32.
Kitano S, Inomata M, Mizusawa J, Katayama H, Watanabe M, Yamamoto S, et al. Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. Lancet Gastroenterol Hepatol. 2017;2:261–8.
Seike K, Koda K, Saito N, Oda K, Kosugi C, Shimizu K, et al. Laser Doppler assessment of the influence of division at the root of the inferior mesenteric artery on anastomotic blood flow in rectosigmoid cancer surgery. Int J Color Dis. 2007;22:689–97.
Meyers MA. Griffiths’ point: critical anastomosis at the splenic flexure. Significance in ischemia of the colon. AJR Am J Roentgenol. 1976;126:77–94.
Park JS, Choi GS, Kim SH, Kim HR, Kim NK, Lee KY, et al. Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg. 2013;257:665–71.
Lange MM, Buunen M, van de Velde CJ, Lange JF. Level of arterial ligation in rectal cancer surgery: low tie preferred over high tie. A review. Dis Colon Rectum. 2008;51:1139–45.
Rutegard M, Hemmingsson O, Matthiessen P, Rutegard J. High tie in anterior resection for rectal cancer confers no increased risk of anastomotic leakage. Br J Surg. 2012;99:127–32.
Bonnet S, Berger A, Hentati N, Abid B, Chevallier JM, Wind P, et al. High tie versus low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery: impact on the gain in colon length and implications on the feasibility of anastomoses. Dis Colon Rectum. 2012;55:515–21.
Yamamoto S, Inomata M, Katayama H, Mizusawa J, Etoh T, Konishi F, et al. Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan clinical oncology group study JCOG 0404. Ann Surg. 2014;260:23–30.
Author information
Authors and Affiliations
Contributions
Study concept and design: SM; data acquisition: HK, SM, K. Sakamoto; analysis and interpretation of data: HK, SM, K. Sugimoto, YM, KS, RY, SU, ST, SS, TK, HO, MS, HM; drafting of the manuscript: SM; critical revision of the manuscript: K. Sato.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was performed in accordance with the ethical standards of the Committee on Human Experimentation of our institution.
Rights and permissions
About this article
Cite this article
Kato, H., Munakata, S., Sakamoto, K. et al. Impact of Left Colonic Artery Preservation on Anastomotic Leakage in Laparoscopic Sigmoid Resection and Anterior Resection for Sigmoid and Rectosigmoid Colon Cancer. J Gastrointest Canc 50, 723–727 (2019). https://doi.org/10.1007/s12029-018-0126-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-018-0126-z