Abstract
Purpose
FOLFIRINOX (FFN), nab-paclitaxel plus gemcitabine (GN), and gemcitabine are three systemic therapies that provide clinically meaningful benefit to patients with unresectable pancreatic cancer (UPC). There are no clinical trials that directly compare the efficacy of all three regimens. In this study, we aim to examine and compare the real-world effectiveness of these treatments.
Methods
Patients diagnosed with UPC who initiated palliative chemotherapy from August 2014 to January 2016 at any one of six cancer centers in British Columbia were identified from the provincial pharmacy. Clinical, pathological, treatment, and outcome characteristics were compared.
Results
Two hundred twenty-five patients were included: 55% men, 68% Eastern Cooperative Oncology Group 0/1, 58% metastatic disease. Patients who received FFN were younger (p < 0.001) and in better performance status (p < 0.001). Patients treated with FFN or GN experienced significantly longer median overall survival (OS) when compared to those treated with gemcitabine (14.1 vs 10.5 vs 4.2 months, respectively, p < 0.001). Progression-free survival (PFS) was also longer among patients on FFN or GN in comparison to gemcitabine (FFN, HR 0.44, 95% CI 0.24 to 0.814, p = 0.008; GN, HR 0.30, 95% CI 0.19 to 0.47, p < 0.001). A significantly higher proportion of patients require two or more dose modifications on FFN (40%) compared to GN (14%) or gemcitabine (9%) (p < 0.001).
Conclusions
Receipt of modified FFN and GN portends a better prognosis than gemcitabine alone. In the absence of a randomized comparison of all three regimens, our population-based study reveals that the introduction of modified FFN and GN confers real-world effectiveness for UPC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic adenocarcinoma continues to portend a poor prognosis. It remains the fourth leading cause of cancer-related deaths in developed countries because the majority of patients still present with incurable disease at initial diagnosis [1]. The median overall survival (OS) for metastatic pancreatic adenocarcinoma is approximately 6 months without systemic therapy. While outcomes are better for locally advanced disease, median OS is estimated to be in the range of 12 months only [2]. Treatment of advanced pancreatic cancer is an evolving field with numerous studies being proposed and conducted in an effort to find more effective treatments.
Gemcitabine became the standard chemotherapy regimen for advanced pancreatic cancer in the late 1990s, after a randomized phase III trial showed a significant improvement in disease-related symptoms and median OS when compared to 5-fluorouracil alone (5.6 vs 4.4 months, p = 0.002) [3]. This remained the standard of care until 2011 when FOLFIRINOX (FFN) was introduced as a new first-line treatment for metastatic pancreatic cancer patients. Its use was limited to individuals with a good performance status because it posed significant toxicities and frequently required growth factor support [4]. This triplet regimen offered enhanced median OS as compared to gemcitabine monotherapy (11.1 vs 6.8 months, HR for death 0.57; 95% CI 0.45 to 0.73; p < 0.0001) [4]. Two years later, in 2013, gemcitabine plus nab-paclitaxel (GN) was evaluated against gemcitabine alone, which demonstrated superiority of the doublet over monotherapy in terms of median OS (8.5 vs 6.7 months; HR for death 0.72, 95% CI 0.62 to 0.83; p < 0.001) [5].
Currently, all three regimens are approved as first-line treatment for patients with advanced pancreatic cancer. While both FFN and GN confer a survival advantage over gemcitabine monotherapy, FFN and GN have not been examined directly in a head-to-head comparison. In the absence of a clinical trial, there is value in characterizing the utilization and outcomes of these regimens in the real world. Therefore, the primary objective of this study was to examine the OS in a population-based setting where advanced pancreatic cancer patients have access to FFN, GN, or gemcitabine as first-line treatment options. The secondary aim of the study was to analyze progression-free survival (PFS), patterns of utilization, and tolerability of these regimens.
Materials and Methods
Characteristics of the Study Setting
The British Columbia Cancer Agency is a provincial and population-based cancer control program that is responsible for funding and providing cancer treatment to approximately 4.5 million residents in the province of British Columbia, Canada. At the time of this study, the agency was comprised of six comprehensive cancer centers that were geographically distributed across different catchment areas of the province. All centers offer a full range of quality cancer programs including outpatient oncology clinics, chemotherapy suites, radiation facilities, surgical services, inpatient units, palliative and supportive care, and the opportunity to participate in clinical trials for the estimated 15,000 to 20,000 new patients referred to the British Columbia Cancer Agency annually.
Description of the Patient Population
Consecutive patients diagnosed with advanced pancreatic adenocarcinoma, defined as surgically unresectable disease, 18 years or older at diagnosis, and who initiated any palliative intent chemotherapy from August 2014 to January 2016 at any one of six cancer centers in British Columbia were identified from the provincial pharmacy database. Clinical, pathological, treatment, and outcome characteristics were extracted by comprehensive review of each patient’s electronic medical records. Ethics approval was obtained from the Institutional Review Board prior to the conduct of the study. In August 2014, all three regimens (FFN, GN, and gemcitabine) were funded for palliative intent therapy in both locally advanced and metastatic pancreatic cancer.
Definitions for Treatments and Outcomes
Palliative intent therapy with FFN, GN, and gemcitabine was administered based on treatment protocols as described in landmark clinical trials of these regimens by Conroy, Von Hoff, and Burris et al., respectively, with dose modifications at the treating clinician’s discretion [3,4,5]. At the British Columbia Cancer Agency, all of the systemic therapy protocols are coded with the treatment intent so it was possible to differentiate between gemcitabine given for adjuvant versus palliative purposes. Administration of at least one cycle of chemotherapy constituted receipt of the treatment. Patients were assigned to one of the three treatment groups in a mutually exclusive fashion based on the regimen they received as the first cycle. For purposes of our analyses, dose modifications were defined as any dose delays (or breaks from chemotherapy for 7 days or longer from the usual cycle length), dose reductions of one or more of the agents in the chemotherapy regimen, or omissions of one or more of the chemotherapy components in a treatment cycle, where applicable, relative to the patient’s initial dose level and regimen. Toxicities of interest (e.g., febrile neutropenia, neuropathy) were captured in a binary fashion (yes/no). OS was calculated as the time from pathologic diagnosis to death from any cause while PFS was characterized as the time from diagnosis to radiographic progression, clinical progression, or death, whichever occurred first.
Statistical Analyses
All data analyses were performed using R (version 3.3.0) [6] and GraphPad Prism software (version 4.0.3, GraphPad Software, La Jolla CA, USA). Comparisons of patient characteristics and treatment toxicities were performed with ANOVA for continuous variables, and Chi-squared tests for categorical variables. OS and PFS were assessed using the Kaplan-Meier method and comparisons between treatment groups were conducted in a pair-wise fashion using the log-rank test. Hazard ratios (HRs) for both OS and PFS were evaluated with Cox regression models that adjusted for age, Eastern Cooperative Oncology Group (ECOG) status, and disease extent. The significance level was set at p < 0.05.
Results
Clinical and Treatment Characteristics
A total of 225 patients were included in the study, of whom 92 (41%), 87 (39%), and 46 (20%) patients received FFN, GN, and gemcitabine, respectively. In this cohort, there were 123 (55%) men, 154 (68%) ECOG 0 or 1, and 154 (68%) cases of metastatic disease. In univariate analyses, patients treated with FFN were younger (p < 0.001), had better performance status (p < 0.001), and were more likely to have a primary tumor affecting the head of the pancreas (p = 0.048). The age ranges at diagnosis in the gemcitabine, GN, and FFN groups were 56 to 87, 42 to 86, and 34 to 82 years, respectively, and the interquartile ranges were 67 to 79, 61 to 73, and 56 to 67 years, respectively. Patients treated with gemcitabine had higher median bilirubin levels prior to starting treatment (p = 0.02). Ca19–9 level, use of biliary stents, and site(s) of metastasis were not statistically different between treatment groups (all p > 0.05). The median duration on treatment was 19 weeks in the FFN group, 21 weeks in the GN group, and 2.6 weeks in the gemcitabine group (p = 0.04). Additional clinical and treatment characteristics are summarized in Table 1.
Outcomes
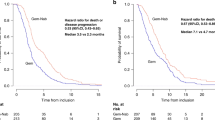
After a median observed follow-up of 8.5 months, 150 deaths have occurred at the time of analyses. The median OS was 14.1 months (95% CI, 9.7 to undefined) in the FFN group, compared to 10.5 months (95% CI, 9.5 to 14.1) in the GN group, and 4.2 months (95% CI, 3.6 to 5.7) in the gemcitabine group. Patients treated with FFN or GN experienced significantly longer median OS when compared to those treated with gemcitabine (p < 0.001) while median OS was not statistically significantly different between patients treated with FFN versus GN (p = 0.09) (Fig. 1A). Using gemcitabine as the reference group, the HR for death with FFN and GN treatment were both significantly lower when adjusted for age, ECOG, bilirubin level, and disease stage (FFN, HR 0.31, 95% CI, 0.16 to 0.59, p < 0.001; and GN, HR 0.26, 95% CI, 0.16 to 0.42, p < 0.001). In multivariate analysis, metastatic disease was identified as an independent adverse prognostic factor for OS (p < 0.001), but age and bilirubin were not (both p > 0.05).
a Observed overall survival (OS) in patients treated with gemcitabine (Gem, blue line), FOLFIRINOX (FFN, orange line), and gemcitabine and nab-paclitaxel (GN, gray line). b Observed progression-free survival (PFS) in patients treated with gemcitabine (Gem, blue line), FOLFIRINOX (FFN, orange line), and gemcitabine and nab-paclitaxel (GN, gray line)
Patients treated with FFN or GN also experienced significantly longer median PFS at 8.4 (95% CI 6.7 to 10.9) months and 8.5 (95% CI 8.0 to 10.2) months, respectively, when compared to those treated with gemcitabine alone at 3.7 (95% CI 3.0 to 4.9) months (all p < 0.001) (Fig. 1B). This observation persisted for FFN and GN after adjusting for confounders including age, ECOG, bilirubin level, and disease extent (FFN, HR 0.44, 95% CI 0.24 to 0.814, p = 0.008; GN, HR 0.30, 95% CI 0.19 to 0.47, p < 0.001). When the cohort was analyzed separately based on disease burden, FFN and GN resulted in significantly longer median OS when compared to gemcitabine alone in both locally advanced and metastatic diseases (all p < 0.001). For median PFS, FFN and GN were also superior to gemcitabine alone in metastatic disease (both p < 0.001) while there was a trend for superiority in the setting of locally advanced disease (FFN p = 0.053; GN p = 0.067). Additional details from the univariate and multivariate survival analyses are summarized in Tables 2 and 3, respectively.
Dose Adjustments, Adverse Events, and Subsequent Treatments
Tables 4 and 5 provide details regarding dosing, toxicities, and second-line treatment patterns. The median time to first dose modification (including any dose delays, reductions, or omissions of one or more of the therapeutic agents) was 7.3, 4.7, and 1.5 weeks into treatment for FFN, GN, and gemcitabine groups, respectively (p = 0.13). The most commonly observed clinically significant adverse events for FFN were neutropenia (16%), febrile neutropenia (8%), and neuropathy (21%), whereas these events were significantly less frequent for patients on GN and gemcitabine (p = 0.02 and p = 0.002, respectively). Of note, 37 (40%), 11 (13%), and 4 (9%) patients required two or more dose modifications during their course of treatment while on FFN, GN, and gemcitabine (p < 0.001).
At the time of analysis, first-line treatment was discontinued in 82, 86, and 100% patients receiving FFN, GN, and gemcitabine, respectively (p = 0.009). Although treatment discontinuation was due to progression in most cases, it was also attributable to toxicities in 28, 19, and 28% cases in the FFN, GN, and gemcitabine groups (p = 0.33). After first-line, 30% of patients who received FFN and 20% of patients who received GN proceeded to second-line chemotherapy (p < 0.001). Patients previously on FFN were subsequently treated with gemcitabine-based singlet or doublet therapy whereas patients on first-line GN tended to undergo 5-flurouracil-based therapy. None of the patients treated with gemcitabine monotherapy in the first-line setting proceeded to second-line therapy.
Discussion
Gemcitabine was at one time the only effective treatment available for advanced pancreatic adenocarcinoma, but recent studies have introduced FFN and GN as two additional first-line options for newly diagnosed patients [7, 8]. However, the lack of a randomized controlled trial directly comparing the efficacy of FFN and GN has generated some uncertainty about the best approach to treatment selection and underscores the value of a real-world study. To our knowledge, this is the first population-based comparison of all three available regimens where we found that FFN and GN provided similar survival advantages over gemcitabine monotherapy, particularly for metastatic disease. Importantly, we observed that patients receiving GN were more likely than those receiving FFN to be ECOG 2 or higher, suggesting that there is an inherent preference among physicians and patients to select treatment based on performance status and fitness to withstand toxicities.
The overall OS and PFS outcomes seen among FFN and GN patients in our study were largely consistent with those observed in prior retrospective institutional series [9,10,11,12,13,14,15] as well as two meta-analyses [16, 17]. Because the ACCORD/PRODIGE and MPACT trials limited enrollment to metastatic disease only, our inclusion of locally advanced patients in the study cohort resulted in survival outcomes that were seemingly better. This is expected since locally advanced disease has a more favorable prognosis [2]. When we examined the subgroup with metastatic disease only, however, our median OS of 9.4 months for FFN more closely reflected findings of the ACCORD/PRODIGE trial [4]. A recent secondary analysis of the Canadian subset of patients enrolled in the MPACT trial also showed a better median OS of 11.9 months that corroborates the outcomes seen in the current analysis [18]. It is unclear why Canadian patients fared better than non-Canadian patients in the MPACT study, but universal healthcare through a single-payer system allowing for educational awareness programs and timely access to supportive care may be one potential reason. Another potential reason could be more familiarity with the treatment protocol, given a higher number of patients per treatment center enrolled in Canada compared to the rest of the study centers.
Interestingly, patients undergoing gemcitabine alone in our analysis appeared to have done worse than the expected 6 months that was seen in the trial conducted by Burris et al. A possible explanation for this includes selection bias whereby severely ill or frail patients in the real world who would otherwise be deemed ineligible for trial participation were still offered gemcitabine by physicians because of the clinical rather than the survival benefit associated with gemcitabine [19]. Another noteworthy finding is that metastatic patients receiving either combination regimen experienced similar OS even though FFN and GN are perceived to have different potency [20]. While cross-trial comparisons are fraught with limitations, FFN and GN are associated with numerical differences in OS according to the ACCORD/PRODIGE and MPACT trials [4, 5]. Since dose modifications were more prevalent among individuals receiving FFN in our study, the potentially lower dose intensity of chemotherapy may have modified its efficacy in the real world.
Another important feature of this study is our characterization of toxicity patterns. Overall, treatments appeared to be reasonably well tolerated in a population-based setting. During the study time period, growth factors were not routinely used at our institution because the cost was not reimbursed by most health insurance plans. Despite this, the rates of febrile neutropenia as well as rates of neutropenia were relatively infrequent (< 10%). It is possible that clinicians opted for more frequent dose modifications as a compensatory measure to minimize neutropenic risks to patients. Of note, neuropathy secondary to FFN also contributed to more dose modifications than neuropathy due to GN. The differences in neuropathy induced by oxaliplatin versus nab-paclitaxel are well described, with the latter being more transient and reversible and thus less debilitating [21, 22]. This may have implications during treatment selection, particularly for patients with preexisting neuropathy or conditions (e.g., diabetes) that may predispose to a higher risk for this side effect.
Finally, we explored patterns of second-line treatments. It is notable that only a minority of patients pursued further therapy after discontinuing first-line. Not surprisingly, patients receiving gemcitabine-based therapy proceeded to receive 5-fluorouracil-based therapy, and vice-versa. This type of treatment strategy is consistent with current evidence [7, 8]. A recent prospective multicenter cohort study by Portal et al. suggests that use of GN after FFN may be an effective approach to sequential therapy for patients. This produced a median OS of 18 months [23], although patient selection may have contributed to the apparent OS benefit. In a recent multicenter randomized trial, the use of 5-flurouacil and oxaliplatin versus infusional 5-flurouracil did not demonstrate a difference in PFS after treatment with gemcitabine. The study in fact demonstrated an inferior OS in the combination treatment arm, possibly due to poorer tolerance of combination treatment leading to less use of post-progression therapy [24, 25].
This study has several limitations. First, this was a retrospective cohort study so it is subject to selection bias. In the absence of a three-arm clinical trial that compares FFN, GN, and gemcitabine, however, we must rely on observational studies to inform decision-making. In addition, we adjusted for measured confounders, such as age and ECOG, in order to better isolate the effect of treatment on outcomes. Second, there was no central or independent radiologic review of imaging studies, which were also conducted at the discretion of the treating physician rather than performed at regularly scheduled intervals, so our assessment of PFS may not be as robust as our measurement of OS. Third, we attempted to delineate dose modifications by examining delays, reductions, and omissions of agents, but this method is prone to misclassification bias since the reasons for dose adjustments are variable and can be based on physician, patient, and system factors that may be clinically warranted or not. In addition, dose modifications were only captured and compared to the initial dose administered due to limitations in the database. However, these limitations should be weighed against the study’s strengths which include its population-based nature and its description of patterns of use and outcomes in the real world. Moreover, our inclusion of locally advanced cases adds further insights into the utility of these regimens beyond metastatic disease.
In conclusion, our study supports the use of GN and FFN as first-line therapeutic options for advanced pancreatic cancer. When delivered to carefully selected patients with either locally advanced or metastatic disease, either regimen offers a survival advantage when compared to gemcitabine monotherapy. In this real-world comparison consisting of Canadian patients, outcomes achieved from the use of GN and FFN appear similar. All regimens are generally well tolerated, although FFN is associated with more toxicities that require more frequent dose modifications. Given these findings, current therapeutic decisions should be driven by individual patient preferences, performance status, and physician clinical judgment regarding a patient’s tolerance to specific side effects.
References
American Cancer Society. Cancer Facts and Figures 2016. 2016; Available at: http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2016/. Accessed 30 Jul 2016.
Peixoto RD, Speers C, McGahan CE, Renouf DJ, Schaeffer DF, Kennecke HF. Prognostic factors and sites of metastasis in unresectable locally advanced pancreatic cancer. Cancer Med. 2015;4(8):1171–7. https://doi.org/10.1002/cam4.459.
Burris HA 3rd, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15(6):2403–13. https://doi.org/10.1200/JCO.1997.15.6.2403.
Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817–25. https://doi.org/10.1056/NEJMoa1011923.
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691–703. https://doi.org/10.1056/NEJMoa1304369.
R Core Team. R. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. 2016; Available at: https://www.R-project.org/. Accessed 30 Jan 2016.
Ducreux M, Cuhna AS, Caramella C, Hollebecque A, Burtin P, Goere D, et al. Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v56–68. https://doi.org/10.1093/annonc/mdv295.
Sohal DP, Mangu PB, Khorana AA, Shah MA, Philip PA, O’Reilly EM, et al. Metastatic pancreatic cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2016;34(23):2784–96. https://doi.org/10.1200/JCO.2016.67.1412.
Chan K, Shah K, Lien K, Coyle D, Lam H, Ko YJA. Bayesian meta-analysis of multiple treatment comparisons of systemic regimens for advanced pancreatic cancer. PLoS One. 2014;9(10):e108749. https://doi.org/10.1371/journal.pone.0108749.
Chllamma MK, Cook N, Dhani NC, Giby K, Dodd A, Wang L, et al. FOLFIRINOX for advanced pancreatic cancer: the Princess Margaret Cancer Centre experience. Br J Cancer. 2016;115(6):649–54. https://doi.org/10.1038/bjc.2016.222.
De Vita F, Ventriglia J, Febbraro A, Laterza MM, Fabozzi A, Savastano B, et al. NAB-paclitaxel and gemcitabine in metastatic pancreatic ductal adenocarcinoma (PDAC): from clinical trials to clinical practice. BMC Cancer. 2016;16(1):709-016-2671-9. https://doi.org/10.1186/s12885-016-2671-9.
Kim GP, Parisi M, Patel M, Belk K. Real world hospital costs associated with nab-paclitaxel plus gemcitabine (nab-P+G) and FOLFIRINOX (FFX) as first line (1L) treatment (tx) for metastatic pancreatic adenocarcinoma (MPAC). J Clin Oncol. 2016;34(15_suppl):e15741.
Marthey L, Sa-Cunha A, Blanc JF, Gauthier M, Cueff A, Francois E, et al. FOLFIRINOX for locally advanced pancreatic adenocarcinoma: results of an AGEO multicenter prospective observational cohort. Ann Surg Oncol. 2015;22(1):295–301. https://doi.org/10.1245/s10434-014-3898-9.
Moorcraft SY, Khan K, Peckitt C, Watkins D, Rao S, Cunningham D, et al. FOLFIRINOX for locally advanced or metastatic pancreatic ductal adenocarcinoma: the Royal Marsden experience. Clin Colorectal Cancer. 2014;13(4):232–8. https://doi.org/10.1016/j.clcc.2014.09.005.
Rombouts SJ, Mungroop TH, Heilmann MN, van Laarhoven HW, Busch OR, Molenaar IQ, et al. FOLFIRINOX in locally advanced and metastatic pancreatic cancer: a single centre cohort study. J Cancer. 2016;7(13):1861–6. https://doi.org/10.7150/jca.16279.
Suker M, Beumer BR, Sadot E, Marthey L, Faris JE, Mellon EA, et al. FOLFIRINOX for locally advanced pancreatic cancer: a systematic review and patient-level meta-analysis. Lancet Oncol. 2016;17(6):801–10. https://doi.org/10.1016/S1470-2045(16)00172-8.
Gresham GK, Wells GA, Gill S, Cameron C, Jonker DJ. Chemotherapy regimens for advanced pancreatic cancer: a systematic review and network meta-analysis. BMC Cancer. 2014;14:471. 2407–14-471
Tehfe M, Dowden S, Kennecke H, El-Maraghi R, Lesperance B, Couture F, et al. Nab-paclitaxel plus gemcitabine versus gemcitabine in patients with metastatic pancreatic adenocarcinoma: Canadian subgroup analysis of the phase 3 MPACT trial. Adv Ther. 2016;33(5):747–59. https://doi.org/10.1007/s12325-016-0327-4.
Peixoto RD, Ho M, Renouf DJ, Lim HJ, Gill S, Ruan JY, et al. Eligibility of metastatic pancreatic cancer patients for first-line palliative intent nab-paclitaxel plus gemcitabine versus FOLFIRINOX. Am J Clin Oncol. 2017;40(5):507–11.
Conroy T, Bachet JB, Ayav A, Huguet F, Lambert A, Caramella C, et al. Current standards and new innovative approaches for treatment of pancreatic cancer. Eur J Cancer. 2016;57:10–22. https://doi.org/10.1016/j.ejca.2015.12.026.
Goldstein D, Von Hoff DD, Moore M, Greeno E, Tortora G, Ramanathan RK, et al. Development of peripheral neuropathy and its association with survival during treatment with nab-paclitaxel plus gemcitabine for patients with metastatic adenocarcinoma of the pancreas: a subset analysis from a randomised phase III trial (MPACT). Eur J Cancer. 2016;52:85–91. https://doi.org/10.1016/j.ejca.2015.10.017.
Park SB, Lin CS, Krishnan AV, Goldstein D, Friedlander ML, Kiernan MC. Long-term neuropathy after oxaliplatin treatment: challenging the dictum of reversibility. Oncologist. 2011;16(5):708–16. https://doi.org/10.1634/theoncologist.2010-0248.
Portal A, Pernot S, Tougeron D, Arbaud C, Bidault AT, de la Fouchardiere C, et al. Nab-paclitaxel plus gemcitabine for metastatic pancreatic adenocarcinoma after Folfirinox failure: an AGEO prospective multicentre cohort. Br J Cancer. 2015;113(7):989–95. https://doi.org/10.1038/bjc.2015.328.
Gill S, Ko YJ, Cripps C, Beaudoin A, Dhesy-Thind S, Zulfiqar M, et al. PANCREOX: a randomized phase III study of 5-fluorouracil/leucovorin with or without oxaliplatin for second-line advanced pancreatic cancer in patients who have received gemcitabine-based chemotherapy. J Clin Oncol. 2016;34(32):3914–20. https://doi.org/10.1200/JCO.2016.68.5776.
Vogel A, Ciardiello F, Hubner RA, Blanc JF, Carrato A, Yang Y, et al. Post-gemcitabine therapy for patients with advanced pancreatic cancer—a comparative review of randomized trials evaluating oxaliplatin- and/or irinotecan-containing regimens. Cancer Treat Rev. 2016;50:142–7. https://doi.org/10.1016/j.ctrv.2016.09.001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval was obtained from the Institutional Review Board prior to the conduct of the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, Y., Camateros, P. & Cheung, W.Y. A Real-World Comparison of FOLFIRINOX, Gemcitabine Plus nab-Paclitaxel, and Gemcitabine in Advanced Pancreatic Cancers. J Gastrointest Canc 50, 62–68 (2019). https://doi.org/10.1007/s12029-017-0028-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-017-0028-5