Abstract
Background
This study aimed to analyze the current status of brain death/death by neurologic criteria (BD/DNC) determination in Korea over a decade, identifying key areas for improvement in the process.
Methods
We conducted a retrospective analysis of data from the Korea Organ Donation Agency spanning 2011 to 2021, focusing on donors whose donations were not completed. The study reviewed demographics, medical settings, diagnoses, and outcomes, with particular emphasis on cases classified as nonbrain death and those resulting in death by cardiac arrest during the BD/DNC assessment.
Results
Of the 5047 patients evaluated for potential brain death from 2011 to 2021, 361 were identified as noncompleted donors. The primary reasons for noncompletion included nonbrain death (n = 68, 18.8%), cardiac arrests during the BD/DNC assessment process (n = 80, 22.2%), organ ineligibility (n = 151, 41.8%), and logistical and legal challenges (n = 62, 17.2%). Notably, 25 (36.8%) of them failed to meet the minimum clinical criteria, and 7 of them were potential cases of disagreement between the two clinical examinations. Additionally, most cardiac arrests (n = 44, 55.0%) occurred between the first and second examinations, indicating management challenges in critically ill patients during the assessment period.
Conclusions
Our study highlights significant challenges in the BD/DNC determination process, including the need for improved consistency in neurologic examinations and the management of critically ill patients. The study underscores the importance of refining protocols and training to enhance the accuracy and reliability of brain death assessments, while also ensuring streamlined and effective organ donation practices.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The concept of brain death or death by neurologic criteria (BD/DNC) has been a subject of varying definitions across different countries, medical institutions, and religions, challenging its status as a mode of death [1,2,3]. Since the introduction of the concept of brain death in 1950s, several structured guides for determining BD/DNC have been released, emphasizing the importance of establishing prerequisites for BD/DNC and accurately assessing patients through a thorough neurologic examination to meet the minimum clinical criteria (MCC) [4,5,6]. Recent initiatives, such as the World Brain Death Project (WBDP) [6], have sought to address these discrepancies by standardizing the criteria for brain death determination globally. The WBDP represents a significant effort by an international panel of experts who have developed consensus-based recommendations to ensure the uniform application of brain death criteria. These guidelines emphasize the importance of confirming the irreversible cessation of all brain functions through a meticulous clinical assessment and the exclusion of any reversible conditions that could mimic brain death.
In South Korea, diagnosis of brain death is only allowed under specific requirements and procedures outlined in the Organ Transplantation Act (Amended by Act no. 17214, Apr 7, 2020) [7] and the Attached Table of the Enforcement Decree (Amended by Presidential Decree no. 33000, Nov 22, 2022) [8]. Thus, the diagnosis of BD/DNC in South Korea is specifically made within the context of cadaveric organ donation and is not used as a general diagnostic criterion for death. Although Korean law does not provide a legal definition of “death” per se, it does specify requirements as prerequisites for BD/DNC and outlines a detailed process for determining brain death. This process includes mandatory dual clinical examinations and the use of an electroencephalogram as a confirmatory test for BD/DNC.
The purpose of this study is to analyze a decade-long nationwide data set obtained from the Korea Organ Donation Agency (KODA) to examine the current landscape of BD/DNC determination in South Korea. We have focused our analysis on patients who, despite being potentially brain dead, did not complete the organ donation. This investigation includes cases of nonbrain death (NBD) declarations and deaths resulting from cardiac arrest.
Methods
Data Source and Patient Population
We conducted a retrospective study using nationwide records obtained from the KODA, an official institution in South Korea responsible for managing notifications of suspected patients with BD/DNC and coordinating organ donation. In South Korea, it is mandatory for physicians to report any patients suspected to be brain dead to KODA. Typically, physicians make these notifications when patients are in deep comatose states without self-triggered respirations, raising suspicion of brain death. From there, the actual determination process, including the dual clinical examinations, electroencephalogram (EEG) test, and the decision of whether the patient needs ancillary tests, is conducted by two independent board-certified neurologists or neurosurgeons who were not involved in the patient care.
For our study, we requested KODA a list of noncompleted donors between 2011 and 2021. These patients were reported as suspected BD/DNC and underwent the BD/DNC determination process, and by excluding all patients who successfully donated their organs, our final list of noncompleted donors was made. The data obtained from KODA comprised information such as the year of occurrence, patient’s age and sex, the medical setting where the brain injury occurred, the diagnosis, the specific time point when the BD/DNC declaration was halted, and a brief comment explaining the reasons for noncompleted donations. These records were collected by KODA’s organ transplant coordinators, the majority of whom are registered nurses.
Classifications and Brain Death Determination Protocol
We categorized the patients into four distinct groups based on the reasons for noncompleted donations: (1) NBD, which included patients declared nonbrain dead due to objective evidence contradicting BD/DNC. This evidence was obtained from clinical examinations, apnea tests, EEG tests, or other ancillary tests, and could involve the presence or reemergence of spontaneous movements, brainstem reflexes, spontaneous respiration, or apnea-triggered respiration, along with remaining electrical activity in EEG or detectable blood flow on ancillary tests. (2) Death due to cardiac arrest encompassed patients who sustained cardiac arrest during the BD/DNC assessment process and did not survive, excluding those who were successfully resuscitated and subsequently donated their organs. (3) Organ ineligibility, which referred to patients newly diagnosed with conditions that contraindicate donation during the evaluation process, such as active infections or malignancies, or those whose organs were found to be severely damaged on procurement surgery. (4) Logistical and legal challenges included cases in which donations were not completed because of the withdrawal of family consent, requirements for autopsy and legal proceedings, or cancellations of procurement surgeries because of the absence of suitable organ recipients.
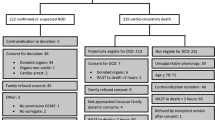
The data also included information on the specific stage, following the standard BD/DNC determination process in Korea, at which the process was halted. This process, mandated by Korean law, consists of several steps: the first clinical examination with an apnea test, then a minimum interval of 6 h, and then the second clinical examination with another apnea test, an EEG test (with or without ancillary tests), and the BD/DNC decision committee. The list of mandatory clinical examinations for brainstem reflexes includes light reflex, corneal reflex, oculo-cephalic reflex, vestibulo-ocular reflex, ciliospinal reflex, gag reflex, and cough reflex. The interruption could occur at any point between the initiation of the first clinical examination and the conclusion of the final procurement surgery. The brief summary of the BD/DNC determination process is depicted in Fig. 1.
The standard Korean brain death determination process with causes of interruption according to the protocol. The upper part of the figure illustrates the stages at which the brain death determination was halted for patients found to be nonbrain dead by the minimal clinical criteria. The lower part of the figure indicates the percentage of patients sustaining cardiac arrest at each stage during the brain death determination process, resulting in death due to cardiac arrest. BD/DNC, brain death/death by neurologic criteria, EEG, electroencephalogram
Additionally, the medical settings in which the neurologic injury occurred were classified as accident-related, illness-related, or unclassified. Accident-related injuries included traffic accidents, suicide attempts, and other accidents such as carbon monoxide intoxication, asphyxia, electrical burns, falls, and homicides. Illness-related injuries included cardiac arrest, hemorrhagic or ischemic strokes, brain tumors, and central nervous system infections. The etiological classification included asphyxia and hypoxia, cardiac arrest, ischemic stroke, hemorrhagic stroke, and traumatic brain injury.
Statistical Analysis
Continuous variables, which were checked for normality using the Shapiro − Wilk test, are reported as medians with interquartile ranges. Categorical variables are presented as numbers (percentages). Categorical variables were compared using χ2 tests or Fisher’s exact tests, whereas continuous variables were compared using the Mann − Whitney U-test. All statistical analyses were conducted using R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria), and a P value of less than 0.05 was considered statistically significant.
Ethics Statement and Data Availability
The study design was approved by the Institutional Review Board of Ajou University Medical Center (no. AJOUIRB-DB-2022-534), and the requirement to obtain informed consent was waived owing to the retrospective nature of the study. Anonymized data not published within this article will be made available by request from any qualified investigator.
Results
Patient Characteristics
Between 2011 and 2021, 5047 patients were reported to KODA as suspected of having BD/DNC, and 361 (7.2%) were classified as noncompleted donors. The median age of the noncompleted donors was 54 years (interquartile range 44–63 years), and 258 (71.5%) were male. The patients included in this analysis were from 80 hospitals nationwide. A summary of patient characteristics is presented in Table 1.
The medical settings in which neurologic injuries occurred among noncompleted donors included illness-related injuries in 196 cases (54.3%), accident-related injuries in 143 cases (39.6%), and unclassified medical settings in 22 cases (6.1%). Specific diagnoses for neurologic injuries comprised hemorrhagic stroke in 125 cases (34.6%), traumatic brain injury in 113 cases (31.3%), cardiac arrest in 63 cases (17.5%), injuries related to asphyxia and hypoxia in 38 cases (10.5%), ischemic stroke in 18 cases (5.0%), and other diagnoses in 4 cases (1.1%).
Regarding the reasons for noncompleted donations, 68 patients (18.8%) received a diagnosis of NBD despite initial impressions, 80 patients (22.2%) were classified as having died due to cardiac arrest during the BD/DNC assessment process, 151 patients (41.8%) were withdrawn from the process due to organ ineligibility, and 62 patients (17.2%) were withdrawn from the process due to logistical and legal challenges.
Reasons for NBD
Of the 68 patients classified as NBD, 25 (36.8%) failed to meet the MCC. Furthermore, 38 patients (55.9%) exhibited remaining electrical activity on the EEG test, whereas 5 patients (7.4%) showed remaining blood flow in ancillary tests. Among the patients who were rejected by MCC, 18 patients were declared NBD between the first and second examinations, 4 patients between the second examination and EEG, and 3 patients even after passing the EEG test (Fig. 1).
To understand the reasons behind MCC rejection, we conducted a detailed analysis because a notably high number of patients were rejected based on the MCC. Table 2 summarizes the characteristics of these patients. Among the 25 patients who failed to meet the MCC, 60% displayed evidence of brainstem activity, such as self-triggered respiration or definite brainstem reflexes (e.g., cough reflex). In two cases, nondilation of the pupils was cited as a reason for declaring NBD; however, the size of the pupils was not documented, with records only indicating that the pupils were not dilated. Moreover, a substantial portion (44%) were labeled as NBD due to observed movements during the determination process, although the exact nature of these movements was not documented. One patient was reported to have seizures, a manifestation of definite cortically mediated movement. However, another patient exhibited movement after successfully passing the first and second clinical examinations, even though electrocerebral silence was confirmed by the EEG test. This inconsistency raised concerns about the consistency and quality of the clinical examination process. Because the initiation of the second clinical examination implies that the first examiner confirmed that the patient met BD/DNC prerequisites and exhibited whole-brain inactivity, seven patients who were rejected after passing the second MCC were considered potential cases of disagreement by two independent neurologists.
For the patients who showed remaining blood flow on the ancillary tests, blood flow was detected by transcranial Doppler in four patients and by single-photon emission computed tomography in one patient. No significant differences were observed in the medical setting and etiological classification between patients with NBD and other reasons (Table 3).
Death by Cardiac Arrest
We further investigated the 80 patients who experienced cardiac arrest and subsequently passed away during the BD/DNC determination process, resulting in their failure to donate. Cardiac arrest predominantly occurred between the 1st and the 2nd examination in 55.0% of patients. Additionally, 23.8%, 7.5%, 11.3%, and 2.5% of patients experienced cardiac arrest between the second examination and EEG test, between the EEG test and BD/DNC committee evaluation, after confirmation by the BD/DNC committee but before procurement surgery, and during the actual procurement surgery, respectively (Fig. 1). To gain insight into the characteristics of patients who died of cardiac arrest, we compared them with those with noncompleted donations due to other issues. The proportions of patients’ medical settings and etiological classifications did not significantly differ between the two groups. However, a noticeable tendency toward a higher proportion of nonischemic mechanisms was observed in the cardiac arrest group (Table 3).
Discussion
Our study aimed to investigate the current status of the BD/DNC determination process in Korea. Our retrospective analysis revealed a substantial proportion (n = 68, 18.8%) of noncompleted donors ultimately classified as NBD during the determination process, and another significant portion (n = 80, 22.2%) of noncompleted donors who died before organ donation could occur due to cardiac arrest. Ensuring the accurate and reliable diagnosis of brain death is of utmost importance, given the critical medical condition of patients with brain death. Unfortunately, our data highlight concerns about the accuracy of the current BD/DNC determination process in South Korea and, at the same time, underscores missed opportunities for organ donation.
The process of declaring death should be approached with the utmost caution because the death is permanent. In our study, we observed a significantly large number of patients declared as NBD despite initial impressions of brain death, some of them even after two independent clinical examinations. This contrast to a previous study by Lustbader et al. [9], which found no reemergence or positive neurologic signs after the first BD/DNC examination among 1311 patients who underwent a second examination, raises concerns about the accuracy of the current BD/DNC determination process in South Korea. Similarly, Varelas et al. [10] found zero patients who had regained brain function during the periods following brain death declaration with single clinical examination among 266 patients, suggesting that a single well-performed examination may be more accurate than two examinations.
Several factors may contribute to the high rate of NBD, such as the lack of standardized protocols, variations in the interpretation of neurologic examinations, and potentially inadequate training of the examining physicians. Although it cannot be confirmed whether these patients were falsely classified as NBD, it is evident that the decision-making process should not rely on individual clinical experience or variations in interpretation, given the irreversible consequences of declaring brain death. To further refine the accuracy of brain death assessments, we must address specific clinical challenges highlighted from our study. For instance, the presence of nonreactive, nondilated pupils, which may result from pontine brainstem injuries, should not automatically negate the diagnosis of brain death. These findings underscore the necessity for clinicians to possess a thorough understanding of neuroanatomy to correctly interpret such signs. Additionally, the observation of movements deemed reflexive rather than indicative of cortical activity points to the critical need for distinguishing between spinal and cortical reflexes. Misinterpretations by clinicians, potentially due to a lack of experience, highlight an urgent need for enhanced neurologic training. In some cases in the United States, neurology residents may graduate without ever having the opportunity to examine a single patient with brain death, a situation that is not uncommon in Korea, as well [11, 12]. This lack of exposure to real-life patients can hinder their ability to assess brain death confidently and accurately. Implementing structured educational programs and providing opportunities for hands-on experience with patients with brain death can help equip neurologists and health care professionals with the necessary skills and expertise in this crucial area. Furthermore, ongoing education and continuous professional development should be emphasized to keep medical practitioners abreast of the latest guidelines and advancements in brain death determination. According to this context, the recent structured guidelines for BD/DNC determination have emphasized the qualifications and ongoing education for clinicians who perform the brain death examination [4].
Another significant finding in our study is the high rate of cardiac arrest during the BD/DNC determination process. Managing critically ill patients with brain death can be extremely challenging and may explain most of the cardiac arrest incidents that occurred during the determination process. Our study, a retrospective analysis using nationwide data across 80 hospitals, may indicate heterogeneity in the management of patients with brain death. Regardless, it is well known that cardiac arrest often occurs shortly after brain death, which makes managing donors extremely challenging [13,14,15]. These findings underscore the urgent need to develop efficient and streamlined approaches to brain death diagnosis to minimize delays. Delays in diagnosing brain death can lead to unnecessary suffering and prolongation of treatment and can potentially compromise the quality and viability of organs for transplantation. The primary goal of condensing the time taken for BD/DNC determination is not to reduce the occurrence of cardiac arrest, but rather to prevent noncompleted donations that result from delaying the diagnosis of already-occurred brain deaths [9, 16].
The WBDP emphasizes a clinical diagnosis of BD/DNC, with prerequisites that include apparent irreversible neurologic injury resulting in the loss of all brain functions and the exclusion of confounding factors. If these prerequisites are firmly established, the need for the mandatory duration of the first and second BD/DNC examinations may be considered redundant [6]. Similarly, the Korean enforcement decree outlines specific prerequisites for BD/DNC; however, it does not specify the extent of brain injury required or explicitly confirm whole-brain death as the biological basis for BD/DNC [17]. By establishing more specific and comprehensive prerequisite requirements, there is potential for reducing the number of patients classified as NBD through a more selective patient evaluation. This, in turn, could simplify the subsequent confirmation process, leading to fewer unnecessary delays and extraneous requirements, thereby reducing the potential risk of cardiac arrest during the determination process. Overall, our study suggests there is a need for legal and procedural reforms to update the brain death determination protocols in Korea. The medical field evolves rapidly, and legal standards must adapt to reflect current scientific understanding and best practices to ensure that brain death determinations are both scientifically valid and ethically sound. Revising these protocols to include a broader range of necessary clinical examinations, such as motor function tests, and reevaluating the role of EEG could help align more closely with international standards. These changes would undoubtedly contribute to more accurate and efficient brain death assessments, ultimately improving patient care and trust in the organ donation process.
Despite the valuable insights gained from our study, it is crucial to acknowledge certain limitations that should be taken into account when interpreting the findings. First, one limitation of this study is the use of nonmedical record data, although the data were primarily collected by registered nurses. The reliance on nonmedical record sources may have introduced some inconsistencies or inaccuracies in the data. Secondly, this study adopted a retrospective design, which can present inherent limitations in assessing patients with brain death and their management. The inability to control the timing and selection of data points might have introduced biases and limitations in analyzing the heterogeneous population of patients with brain death. As a result, causative relationships cannot be established, and potential confounding factors may not be fully accounted for. Having a nationwide prospective registry and access to comprehensive medical records would greatly enhance the level of evidence and the quality of research conducted in the field of brain death determination. Moreover, access to comprehensive medical records would provide detailed information about the specific neurologic examinations performed, the management protocols followed, and other relevant clinical variables.
In conclusion, our analysis of the BD/DNC process in Korea over the past 10 years has identified several areas with potential for improvement, aiming to reduce noncompleted donations. The implications of our study extend beyond the Korean context and emphasize the need for ongoing efforts to optimize the BD/DNC determination process globally to ensure the ethical and accurate determination of death and facilitate the provision of lifesaving organ donations.
References
Lewis A, Liebman J, Bakkar A, Kreiger-Benson E, Kumpfbeck A, Shemie SD, et al. Determination of brain death/death by neurologic criteria in countries in Asia and the Pacific. J Clin Neurol. 2020;16(3):480–90.
Wijdicks EF. Brain death worldwide: accepted fact but no global consensus in diagnostic criteria. Neurology. 2002;58(1):20–5.
Wahlster S, Wijdicks EF, Patel PV, Greer DM, Hemphill JC 3rd, Carone M, et al. Brain death declaration: practices and perceptions worldwide. Neurology. 2015;84(18):1870–9.
Greer DM, Kirschen MP, Lewis A, et al. Pediatric and adult brain death/death by neurologic criteria consensus guideline. Report of the AAN Guidelines Subcommittee. AAP, CNS, and SCCM; 2023. https://doi.org/10.1212/WNL.0000000000207740.
Greer DM. Determination of brain death. N Engl J Med. 2021;385(27):2554–61.
Greer DM, Shemie SD, Lewis A, Torrance S, Varelas P, Goldenberg FD, et al. Determination of brain death/death by neurologic criteria: the World Brain Death Project. JAMA. 2020;324(11):1078–97.
Internal Organs Transplant Act, Ministry of Government Legislation. [Enforcement Date October 8, 2020] [Act No. 17214, April 7, 2020, Partial Amendment].
Enforcement Decree of the Internal Organs, Etc. Transplant Act: The Attached Table 4: Facilities, Equipment, Personnel, Etc. of Transplant Medical Institutions, Ministry of Government Legislation. [Enforcement Date November 22, 2022] [Act No. 33000, November 22, 2022, Amendment].
Lustbader D, O’Hara D, Wijdicks EF, MacLean L, Tajik W, Ying A, et al. Second brain death examination may negatively affect organ donation. Neurology. 2011;76(2):119–24.
Varelas PN, Rehman M, Mehta C, et al. Comparison of 1 versus 2 brain death examinations on time to death pronouncement and organ donation. A 12-year single center experience. Neurology. 2021;96(10):e1453-61.
Joffe AR, Anton NR, Duff JP, Decaen A. A survey of American neurologists about brain death: understanding the conceptual basis and diagnostic tests for brain death. Ann Intensive Care. 2012;2(1):4.
Chambade E, Nguyen M, Bernard A, Nadji A, Bouhemad B. Adherence to the law in brain death diagnosis: a national survey. Anaesth Crit Care Pain Med. 2019;38(2):187–8.
Krishnamoorthy V, Prathep S, Sharma D, Fujita Y, Armstead W, Vavilala MS. Cardiac dysfunction following brain death after severe pediatric traumatic brain injury: a preliminary study of 32 children. Int J Crit Illn Inj Sci. 2015;5(2):103–7.
Szabó G. Physiologic changes after brain death. J Heart Lung Transplant. 2004;23(9 Suppl):S223–6.
Power BM, Van Heerden PV. The physiological changes associated with brain death–current concepts and implications for treatment of the brain dead organ donor. Anaesth Intensive Care. 1995;23(1):26–36.
Sung G, Greer D. The case for simplifying brain death criteria. Neurology. 2011;76(2):113–4.
Enforcement Decree of the Internal Organs, Etc. Transplant Act, Ministry of Government Legislation. [Enforcement Date November 22, 2022] [Act No. 33000, November 22, 2022, Amendment by Other Act].
Acknowledgements
We thank the Korea Organ Donation Agency for their collaboration of data analysis and collection. We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This work was supported by National Research Foundation of Korea (NRF) grants funded by the Korean government (Ministry of Science and ICT) (NRF2019R1A5A2026045 and NRF-2021R1F1A1061819) and a grant from the Korean Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (HR21C1003). This research was also supported by Bio-convergence Technology Education Program through the Korea Institute for Advancement Technology funded by the Ministry of Trade, Industry, and Energy.
Author information
Authors and Affiliations
Contributions
Conceptualization: Choi JY. Data curation: Koh S. Formal analysis: Koh S. Park S. Funding acquisition: Choi JY. Methodology: Koh S, Park S, Lee J-M, Choi JY. Writing—original draft: Koh S, Park S, Lee J-M, Choi JY. Writing—review & editing: Kim H, Lee WJ, Lee J-M. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Ethical Approval/Informed Consent
We confirm adherence to ethical guidelines, and this study was approved by the ethics committee (Institutional Review Board of Ajou University Medical Center; no. AJOUIRB-DB-2022–534), and the requirement to obtain informed consent was waived owing to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koh, S., Park, S., Lee, M. et al. Assessing the Brain Death/Death by Neurologic Criteria Determination Process in Korea: Insights from 10-Year Noncompleted Donation Data. Neurocrit Care (2024). https://doi.org/10.1007/s12028-024-02072-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-024-02072-5