Abstract
Neurocritical patients (NCPs) in the intensive care unit (ICU) rapidly progress to respiratory and peripheral muscle dysfunctions, which significantly impact morbidity and death. Early mobilization in NCPs to decrease the incidence of ICU–acquired weakness has been showing rapid growth, although pertinent literature is still scarce. With this review, we summarize and discuss current concepts in early mobilization of critically ill patients within the context of neurologic pathology in NCPs. A narrative synthesis of literature was undertaken trying to answer the following questions: How do the respiratory and musculoskeletal systems in NCPs behave? Which metabolic biomarkers influence physiological responses in NCPs? Which considerations should be taken when prescribing exercises in neurocritically ill patients? The present review detected safety, feasibility, and beneficial response for early mobilization in NCPs, given successes in other critically ill populations and many smaller intervention trials in neurocritical care. However, precautions should be taken to elect the patient for early care, as well as monitoring signs that indicate interruption for intervention, as worse outcomes were associated with very early mobilization in acute stroke trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurocritical patients (NCPs) are defined as individuals suffering from severe neurological damage who are at risk of new nervous system impairment and require intensive treatment and close monitoring [1]. The most common causes of severe acute brain injury in adults are traumatic brain injury, acute ischemic stroke, and intracranial and subarachnoid hemorrhage [1].
Intensive care unit (ICU) admissions almost certainly imply bed rest, especially in patients requiring invasive mechanical ventilation (IMV) [2]. Critical neurological patients are alarmingly predisposed to several harmful and pathophysiological events that are associated with ICU-acquired weakness (ICU-AW) and worsen the clinical prognosis, increasing morbidity, mortality, and hospital costs [3]. In this sense, a paradigm shift in approaching NCPs has emerged. Health professionals and researchers around the world have been stimulating the mobilization of critical patients as soon as possible, armed with knowledge about the problems routinely found in these units and the patient’s recovery after discharge [4]. Physical therapists are notably at the heart of promoting physical activity for critically ill patients, but other professionals, such as physicians, occupational therapists, nurses, and nursing technicians, are also involved in this approach.
There is mounting evidence showing the effects of early mobilization (EM) in reducing IMV duration, improving muscle strength and functional status, and increasing hospital discharge rates [5, 6]. Nevertheless, it is still unclear whether EM can be implemented and/or extended in the neurocritical care population, as these patients present different pathophysiology. Moreover, current literature presents fragile methodologies, small samples, heterogeneous populations, and a scarcity of clinical trials to assess the outcomes related to EM protocols in NCPs [7]. In view of the above, this work aimed to perform a literature review of current concepts in EM of critically ill patients within the context of neurologic pathology.
Methods
This is a review study, and ethical committee approval is not required. A total of 31 articles were identified for this narrative review from the PubMed/Medline (National Library of Medicine), Latin American and Caribbean Health Sciences Literature database, Scientific Electronic Library Online, and Physiotherapy Evidence Database databases. Figure 1 represents an overview of the flow diagram.
Although it is not mandatory for narrative reviews, we decided to conduct a systematic search of prospective studies focused on population, intervention, comparisons, outcomes, and studies to facilitate the study selection, and the question of our study related to the intervention.
The criteria of the descriptor system used in this review were performed following Medical Subject Headings and Health Sciences Descriptors guidelines. The following descriptors were considered: “critical care,” “early mobility,” “early mobilization,” “early rehabilitation,” “intensive care mobility,” “neurocritical care,” and “neurologic pathology.” Boolean operators such as “AND” and “OR” or the combination of these words were also used. Reference lists from articles related to the topic were also searched.
Next, the following issues were addressed to summarize and discuss pathophysiological aspects and EM in NCPs: How do the respiratory and musculoskeletal systems in NCPs behave? Which metabolic biomarkers influence physiological responses in NCPs? Which EM interventions can be used in NCPs?
How Does the Respiratory System in NCPs Behave?
The lowered level of consciousness and the consequent deficit in airway protection associated with secondary physiological brain damage and decreased mobility predispose these patients to pulmonary complications, making it necessary to use mechanical ventilation [3]. However, the use of this therapeutic resource has proven to be challenging because of the close relationship between the nervous and respiratory systems [1].
Lowering the level of consciousness potentiates deleterious effects on critically ill patients, prolonging ventilatory weaning and increasing the length of hospital stay [8]. In this sense, individuals affected with acute neurological diseases often develop respiratory dysfunctions, which can significantly affect the brain physiology and functional outcomes of these individuals over the long term [9].
Aspiration pneumonia or neurogenic pulmonary edema are the main respiratory complications after a stroke or traumatic brain injury [10]. Although the pathomechanisms remain poorly understood, it is known that neurocritical injuries can impact pulmonary function, leading to various respiratory conditions and disorders, including adult respiratory distress syndrome and abnormal respiratory patterns [11].These complications are considered the most important causes of secondary morbidity and mortality in patients with a neurocritical profile [9] and are associated with risk factors, such as mechanical ventilation, dysphagia, and other patient-specific factors. Adult respiratory distress syndrome has a high mortality rate and requires specific treatment approaches, including protective ventilation and restricted fluid management. On the other hand, NPE is more common in patients with severe central nervous system injuries and can be predicted by heart rate variability [11].
How Does the Musculoskeletal System in NCPs Behave?
Because of the clinical complexity that NCPs present, these patients often need invasive monitoring and a mobility restriction period, which predispose them to develop neuromuscular and integumentary alterations [7], thus aggravating the condition of ICU-AW [12]. ICU-AW does not have an elucidated pathogenesis, with unavailability of specific drugs or targeted therapies [13].
ICU-AW is a generalized and symmetrical condition involving limb muscles and respiratory muscles. Tendon reflexes may be diminished or absent, and sensitivity altered or preserved [12]. Many risk factors contribute to the loss of muscle mass, including prolonged immobility and muscle electrical silencing due to the use of sedative analgesic drugs and muscle blockers [14]. Muscle weakness is associated with prolonged periods of mechanical ventilation and hospital stay, leading to significant deficiencies in functionality and cognitive functions, which can last for years after hospital discharge, thus causing an increase in costs and use of health care and a decline in quality of life [13].
Both unilateral and bilateral muscular weakness are a common occurrence in patients experiencing the aftermath of a stroke and other neurological conditions. This weakness plays a central role in the development of prolonged disability [15].
Harmful and pathophysiological events are associated with ICU-AW in NCPs, including the following: (1) neuroendocrine events (imbalance between catabolism/anabolism and axonal dysfunction); (2) inflammatory milieu associated with immobility; (3) metabolic response to stress (catabolic hormones such as glucagon, catecholamines, and corticosteroids and by insulin resistance); (4) electrolyte disorder (hypocalcemia, hypomagnesemia, and hypokalemia); and (5) ventilator-induced diaphragmatic dysfunction [13].
Studies have demonstrated that nerve biopsies from critically ill patients with intracranial pressure (ICP) monitoring presented axonal degeneration of both sensory and motor nerve fibers [16, 17], resulting in important atrophy due to the denervation of respiratory and peripheral muscles [16]. In this context, the excessive behavior of oxidative stress is considered a synergistic point between the decompensation of the respiratory system and the musculoskeletal system. This leads to the inadequate physiological functioning of these systems [18].
Moreover, muscle weakness is associated with prolonged periods of IMV and hospital stay, leading to significant deficiencies in functionality and cognitive functions that can last for years after hospital discharge, thus causing an increase in health care costs and use, as well as a decline in quality of life [13]. Nevertheless, prolonged immobility is a compelling risk factor that can be avoided. Hence, it is important to prevent complications and restore patients to their functional capacity, reducing the risk of hospital readmission [19].
In this context, EM plays a prominent role in the recovery of critically ill patients within the context of neurologic pathology. In the ICU, the term mobilization is used to relate physical activity with intensity that provides physiological benefits, such as improvement in central and peripheral circulation, ventilation, metabolism, and alertness [20]. As an example, a prospective, two-group pre/post comparative study with data collection 4 months preintervention and postintervention, with a 4-month run-in period (Klein et al. [21]), introduced an EM program to a large neurointensive care unit. Postintervention patients with primary neurologic injury admitted to the neurologic ICU had higher mobility levels (p < 0.001), had shorter mean hospital and neurologic ICU length of stay (both p < 0.001), and were more likely to be discharged home (p = 0.033) compared with preintervention patients [21].
Which Metabolic Biomarkers Influence Physiological Responses in NCPs?
Oxidative stress arises from an imbalance between oxidizing compounds and antioxidants, favoring excessive synthesis of free radicals resulting from the extreme synthesis of free radicals or reduced clearance speed [18]. The unpaired electron that is centered on oxygen or nitrogen atoms is respectively called reactive oxygen species (ROS) and reactive nitrogen species [18]. ROS are classified into radicals (hydroxyl, superoxide [O2−°], peroxyl, and alkoxyl) and nonradicals (oxygen [O2], hydrogen peroxide, and hypochlorous acid). The main reactive nitrogen species are nitric oxide, nitric dioxide, and peroxynitrite [18].
These radicals participate in the energy synthesis process, phagocytosis, cell growth regulation, intercellular signaling, immunity, and cell defense, as well as in producing biological substances. However, an excess of these radicals damages the body, causing lipid peroxidation in the membrane, as well as damage to proteins, enzymes, carbohydrates, and DNA [18, 22]. Homeostatic imbalance in excessive synthesis or attenuation of free radical removal predisposes patients to these losses in biological functions [18], triggering pathological events that are involved in neurodegenerative, cardiovascular, and cardiogenic processes [23].
Antioxidant substances are considered capable of delaying or inhibiting oxidation rates [24] and protecting tissues and body fluids from injuries, which are determined using free radicals produced by normal metabolism, either in response to disease or from external sources. The antioxidant defense system is disposed of throughout the cytoplasm, organelles, and extracellular and vascular space [25].
The substances mentioned above are divided into two systems: (1) enzymatic: composed of enzymes synthesized by the body itself, and (2) nonenzymatic: composed of substances, whether of endogenous or dietary origin [26]. In the first case, the main active enzymes include superoxide dismutase, catalase, and glutathione peroxidase, which can act by inhibiting or attenuating the synthesis of free radicals that are involved in the genesis of chain reactions that lead to oxidative damage [18, 26]. It is noteworthy that the activity of these enzymes sometimes depends on participation of cofactors, especially dietary antioxidants. For example, superoxide dismutase, which depends on copper, zinc, and manganese, and glutathione peroxidase, which may depend on selenium [18].
Conversely, the nonenzymatic defense system consists of antioxidant elements of dietary origin, which include vitamins (ascorbic acid -vitamin C-, α-tocopherol, and β-carotene, precursors of vitamins E and A) and minerals (zinc, copper, selenium, and magnesium). Antioxidant potential of nonenzymatic compounds depends on components such as absorption and bioavailability under physiological conditions, and ideal plasma concentration to perform the antioxidant activity [18]. Thus, antioxidant substances act at different levels in protecting the body and maintaining cell integrity by inhibiting the formation of free radicals, preventing lesions from forming [24], as well as removing damaged DNA molecules and in reconstituting damaged membranes [26].
Fraser and Morrison [27] showed that brain tissue in neurological patients is sensitive to oxidative damage due to metabolic demands and the high level of oxygen consumption. The analysis of cerebrospinal fluid in people after acute brain injury showed an increase in oxidative stress levels and its association with disordered energy metabolism [28]. Excessive amount of ROS causes depletion of endogenous antioxidants, increased lipid peroxidation, protein oxidation, DNA fragmentation, and inhibition of the mitochondrial electron transport system, favoring the apoptosis or cell necrosis process [29].
A complex of oxidative stress markers, such as carbonyl proteins, lipid peroxides, reactive oxygen, and nitrogen species are notably synthesized in the brain when there is a brain injury, whereas the expression and activity of oxidative defense enzymes decrease [29]. In addition to the metabolic participation through oxidative stress, some studies also point to the participation of the inflammatory reaction in brain tissue in several acute pathologies of the brain, such as ischemic stroke, which is called neuroinflammation [30, 31].
Therefore, it is important to highlight that the existing findings in the literature have certain limitations, including the lack of direct evidence linking ROS to central nervous system damage, as well as the absence of direct evidence demonstrating the reduction of ROS through antioxidant usage.
Brain damage from an ischemic stroke results in apoptosis and necrosis, which leads to an inflammatory reaction controlled by the discharge of ROS and cytokines. After the inflammatory process starts in the brain tissue, there is an increase in the discharge of several cytokines in the brain tissue and peripheral blood. Thus, these cytokines are involved in cerebral infarction progression, which influences the disease severity and outcome [32].
Tumor necrosis factor-α (TNF-α) and interleukin 6 (IL-6) stand out among the proinflammatory cytokines present in brain lesions. TNF-α is considered one of the first cytokines to appear in the context of the inflammatory reaction after brain injury, participating in stimulating the inflammatory process in the cerebrospinal fluid and blood serum. Furthermore, it was observed that different cytotypes can produce IL-6 after a brain injury, which is an indicator of inflammation during stroke, as this cytokine causes the liver cell to produce fibrinogen and C protein reactive. Although the IL-6 concentration under healthy conditions is relatively modest, several studies have shown that it significantly increases in serum no more than a few hours after the onset of the condition; persisting with this peak up to 90 days after brain injury [32].
There is a need for research that can more accurately investigate the behavior of oxidant and inflammatory substances in different types of brain injuries, as well as the importance of implementing interventions that promote antioxidant and anti-inflammatory reactions in these patients. Overall, prescribing exercises for neurocritically ill patients should focus on minimizing oxidative stress, promoting antioxidant activity, supporting brain function and recovery, and considering the inflammatory response and disease severity. Table 1 provides a comprehensive overview of the essential components involved in the planning of an EM program specifically designed for NCPs.
Which Considerations Should be Taken When Prescribing Exercises in Neurocritically Ill Patients?
Given the previously reported assumptions, it is observed that some authors have tried to develop strategies such as conducting EM to reduce the effect of oxidative stress in critically ill patients and avoid ICU-AW in NCPs. As observed in the studies by França et al. [33] and França et al. [34], cycle ergometer performance promoted a reduction in nitric oxide levels, using both passive cycle ergometers and peripheral neuromuscular electrostimulation, which resulted in a reduction in nitric oxide concentrations one hour after the intervention, inferring that these therapeutic resources can reduce the oxidative stress when applied separately. However, there are still no reports of clinical trials that assess the effect of EM, especially for a cycle ergometer and NMES on oxidative stress in NCPs.
EM in critically ill patients aims to attenuate the harmful effects of immobility and modify the risk of developing sequelae at the physical and functional level, which are closely related to muscle strength loss [35], in addition to accelerating the postdischarge functional recovery of patients who survived hospitalization in an ICU. In this regard, studies in other patient populations (general and surgical critical care) have demonstrated that early mobility in the ICU is safe and feasible, with a potential reduction in short-term physical impairment [5, 33, 36, 37].
Despite positive effects associated with EM, a multicenter study conducted with 750 adult patients in the ICU who were undergoing IMV and without brain injury showed no favorable results for EM. When comparing an increased EM protocol (sedation minimization and daily physiotherapy) with usual care (the mobilization level that was normally provided in each ICU), on the number of days patients remained alive and out of the hospital after 180 days, the results indicated that the increase in early active mobilization did not result in a significantly greater number of days that patients were alive and out of the hospital compared with the usual mobilization level in the ICU. In addition, a higher frequency of adverse events was observed in the group undergoing EM [38].
Moreover, there is still a paucity of high-quality evidence that assesses the effects of EM in NCPs in the ICU, whether due to the small sample size or the research design, lack of blinding of participants, heterogeneity of interventions or inadequate description of the methods used, or variation of outcomes or assessment instruments. Moreover, different exercise types and intensities can be used in EM protocols. This may have contributed to the lack of difference in the main outcome reported in the literature. Mobility activities in bed, cycle ergometer, peripheral NMES, assisted exercises, ample active motion exercises, activities of daily living, transference training, prewalking exercises, and walking are common types of interventions used during EM [39]. It is noteworthy that characteristics inherent to specific interventions, such as the modality, resources used, exercise prescription (time, frequency, intensity, adaptation, and progression), as well as the heterogeneity and the patient’s ability to develop training can interfere with the intervention effectiveness [39].
Considering that EM in patients with acute neurological injuries changes according to the different managements and processes of the disease, its use in NCPs is still a challenge [40] because of the potential of brain injury to promote neurological deterioration and hemodynamic lability in the acute phase of the injury [41].
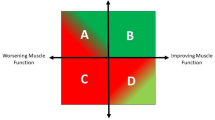
A study conducted by an interdisciplinary workgroup built a mobility algorithm in a neurocritical ICU, incrementally performing passive or active mobilization based on the consciousness and motor function levels to facilitate implementing EM protocols in a safe and viable way in the respective units. This algorithm allows professionals to choose the best way to safely perform EM in NCPs and thus mitigate existing gaps to routinely implement mobilization of these patients. This instrument lists the main determining factors for choosing the modality (passive or active) to be used to perform EM of critically ill patients. Active mobilization is subdivided into eight levels that range from performing active exercises in bed to walking 250 feet. In contrast, passive mobilization is divided into three phases (from cycle ergometer exercises in bed with the head elevated to 45º, to cycle ergometer exercises with the patient completely seated in bed). It is worth emphasizing the importance of monitoring the emergence of mobilization interruption criteria throughout the intervention [41].
A progressive mobility protocol was also implemented in a study conducted with 637 NCPs, consisting of four milestones and 16 levels of mobility progression. This protocol measured the highest level of mobility achieved each day during the first 13 days of ICU admission. The study found that early implementation of the protocol led to increased mobility among patients, facilitating earlier discharge and reducing hospital stay. However, there were no observed improvements in quality metrics or psychological profile [21].
In addition, a protocol guided by the PUMP Plus algorithm was developed and refined based on existing evidence and guidelines. The addition of the term “Plus” to this protocol included the introduction of six additional levels for patient rehabilitation. These additional steps provide clearer expectations for patients, going beyond the simple “getting out of bed to sit,” which was previously considered the ultimate goal of mobility for ICU patients. It was observed that among patients in the neurointensive care unit, increased mobility did not result in an increase in adverse events, measured by falls or inadvertent line disconnections, and this improvement can be achieved quickly and safely. Furthermore, there were associated reductions in length of stay and hospital-acquired infections through the application of the PUMP Plus program [42]. The level of consciousness is one of the main determining factors for choosing the modality (passive or active) to be used to perform EM in NCPs. Thus, because of low scores on the Glasgow Coma Scale, passive mobilization appears to be the most prevalent modality in this population [41]. Therefore, the use of a passive cycle ergometer and peripheral neuromuscular electrical stimulation seem to constitute adequate resources to perform this type of intervention.
A cycle ergometer is a stationary device which allows cyclic rotations and can be used to perform passive exercises [43]. This device helps to recover peripheral muscle strength [44], promotes an increase in muscle circumference [45], reduces IMV duration and the length of stay in the ICU [46]. However, despite these benefits being reported in patients admitted to a general ICU, little is known about their effects on NCPs. A study conducted with 27 NCPs using an external ventricular drain and in the ICU performed a cycle ergometry protocol with active or passive cycling settings at a speed of 20 rpm, and observed that there was no record of any clinically significant change in the level of consciousness (Glasgow Coma Scale), in hemodynamic variables (mean arterial pressure, heart rate, PIC, and PPC), nor any type of adverse event that would present the need to interrupt the session [43]. Limitations of the study are sample size and cross-sectional design, pointing to the need for further trials in order to determine the effectiveness and ideal dose of cycle ergometry as a treatment for NCPs.
Thelanderson et al. [47] conducted a study with 20 NCPs admitted to an ICU of a hospital in Sweden who underwent a passive cycle ergometer session with a speed of 20 rpm for 20 min, approximately 5 days after admission to the ICU. The results showed that there was a significant decrease in cardiac output, stroke volume, mean arterial pressure, and cerebral perfusion pressure (CPP) after the proposed intervention, but there was no change in heart rate, peripheral oxygen saturation or ICP. However, it is important to emphasize that although a statistically significant change occurred, this alteration did not have clinical relevance. Furthermore, the authors also demonstrated the absence of detrimental circulatory effects or any other type of adverse event. Thus, it can be stated that the use of a cycle ergometer is safe and efficient for this profile of patients. Even so, most studies are concerned with evaluating the effect of this therapeutic resource on hemodynamic variables, with few findings on respiratory variables and no results regarding the influence of these resources on metabolic variables such as oxidative stress and inflammation.
In addition, a randomized clinical trial (RCT) conducted with 20 patients post stroke evaluated the effects of an EM protocol with a cycle ergometer for the lower limbs 24 h after patient admission to the stroke unit when compared with conventional physical therapy for five consecutive days. The authors observed that the group that used the cycle ergometer showed improvement in lower limb muscle strength, gait speed, balance, mobility, and functionality of individuals with acute stroke during the hospitalization period [48].
Despite the various benefits reported by the cycle ergometer, its use has some limitations in patients who present some deformity in the lower limbs, such as contractures and fractures. Alternatively, muscle contraction induced by electrical activation with different NMES modalities has been considered a promising treatment to reduce the functional and clinical impacts of ICU stay [49].
In fact, an RCT in 60 critically ill patients with traumatic brain injury was performed to compare those who only received conventional physiotherapy (control group) with the NMES group which additionally underwent daily NMES for 14 days in the lower limb muscles. Twenty study participants from each group completed the trial. After 14 days, the control group presented a significant reduction in muscle thickness of tibialis anterior and rectus femoris, mean of − 0.33 mm (− 14%) and − 0.49 mm (− 21%), p < 0.0001, respectively, whereas muscle thickness was preserved in the NMES group. The control group also presented a higher incidence of neuromuscular electrophysiological disorder: 47% vs. 0% in the NMES group, p < 0.0001, risk ratio of 16, and the NMES group demonstrated an increase in the evoked peak force (2.34 kg/f, p < 0.0001), in contrast with the control group (− 1.55 kg/f, p < 0.0001). The time needed for the NMES protocol to prevent muscle architecture disorders and treat weakness was at least 7 days, and 14 days to treat neuromuscular electrophysiological disorder [50].
Converging with results in favor of NMES intervention, a clinical study was carried out with 14 patients with consciousness disorders admitted to the ICU who were allocated between a control and the NMES group. NMES was performed daily from the 7th day of admission, and it was observed through computed tomography that the control group showed a decrease in the cross-sectional area of the anterior and posterior muscle compartment of the thigh when compared to the NMES group. These results show that NMES is effective in preventing disuse muscle atrophy in this population [51].
Considering the effects demonstrated using cycle ergometers and NMES, the literature has demonstrated the need to work these two resources synergistically in order to enhance the effects of these techniques in critically ill patients. A study performed in a general ICU with 35 patients demonstrated that the use of a cycle ergometer and peripheral NMES in critically ill patients can promote a decrease in nitric oxide levels, reducing oxidative stress [34]. However, the effectiveness of these resources on the behavior of metabolic variables, especially on oxidative stress in NCPs is still unclear in the literature.
Table 2 describes the key characteristics of interventions that involve the use of cycle ergometry and neuromuscular electrical stimulation in the studies included in the review. Moreover, despite literary evidence that recommends the use of EM in NCPs, an important AVERT clinical trial carried out in patients admitted to 56 acute stroke units observed that patients allocated to the EM group had unfavorable outcomes when compared with the group of usual treatment [52]. In turn, this result influences discouraging the implementation of EM protocols in NCPs. Nevertheless, it is worth noting that patients in this multicenter study were mobilized within the first 24 h of the neurological insult and with higher mobilization doses [52] than the usual protocols, which may have culminated in unfavorable outcomes.
The exercises proposed in the EM protocol of this multicenter study encompassed a variety of activities exclusively performed outside the bed, such as sitting, standing, and walking. This approach contrasts with the majority of current studies involving NCPs, in which EM is initiated after 24 h from the neurological event and prioritizes commencing the protocol with bedside activities, subsequently progressing according to the level of consciousness and patient tolerance [41, 43, 47, 48, 50].
Another factor which may have influenced the unfavorable outcomes in the AVERT study is the interruption criteria established by the protocol, which set a systolic blood pressure drop equal to or greater than 30 mm Hg as the threshold, diverging from the recommendations outlined in the consensus statement of the American Autonomic Society and the American Academy of Neurology. These entities recommend a value equal to or greater than 20 mm Hg as the diagnostic criterion for orthostatic hypotension [53, 54].
In view of the above, it becomes challenging for health professionals to generalize the results of certain studies to the clinical specificities of each profile of NCPs because of the different recommendations and presentations, as well as the different management of patients.
The mobilization team must understand the clinical condition and the disease process of the NCP, the effects of performing and increasing activities, and monitoring during mobilization [55]. In this sense, considering the specificity of the neurocritical population, some safety criteria must be considered such as the ICP and blood pressure, in addition to those already observed in EM protocols in critically ill patients for safe intervention.
The cerebral autoregulation of these patients is commonly impaired, and therefore the mobilization team must be fully alert to the rigorous assessment of hemodynamic stability through ICP and BP in order to initiate the EM protocol in these patients [55]. ICP values greater than 20 mm Hg are an absolute contraindication factor for EM. It is recommended that blood pressure values do not exceed 140 mm Hg [40]. Of note, typically, thresholds for stopping activity or treating blood pressure are individualized. Therefore, it is important to state that a person assisting a patient with mobility should be mindful of the ordered blood pressure goals. In complement to hemodynamic stability, it is crucial to monitor and carefully handle intracranial devices that can cause bleeding or significant infection if dislodged [56]. Thus, it is important to check if the catheter fixation is adequate to avoid traction and loss of devices [55].
Most studies recommend that the mobilization start time in NCPs be performed 24 h after the injury (cerebrovascular accident, traumatic brain injury, intracerebral hemorrhage), except for subarachnoid hemorrhage, which is recommended to start in a period of 24 to 48 h after brain injury [56].
Thus, it is understood that EM of patients with brain injury is modifiable by the disease’s different injuries, processes, and management. There are published studies which have evaluated the effect of individualized EM through specifying the type of injury. Despite this concern, there are still few discrete recommendations available for managing critically ill patients according to injury type. It is recommended that mobilization for a patient with stroke be contraindicated if the patient shows signs of ischemia related to changes in blood pressure, such as increased lethargy, weakness, and language dysfunction [55]. Furthermore, it is recommended that blood pressure treatment be started in the acute phase of the stroke when systolic blood pressure is greater than 220 mm Hg and the diastolic blood pressure is less than 120 mm Hg [55]. Therefore, the presence of multidisciplinary collaboration is mandatory to ensure safe mobilization.
Strict monitoring of ICP and CPP values should be advocated, in cases of aneurysmal subarachnoid hemorrhage, as well as rest or limited exercise in situations of aneurysms that have not yet been repaired [56]. Constant surveillance for the presence of vasospasm observed by changes in hemodynamic stability is recommended in corrected aneurysms [55]. It is also recommended to assess the presence of behavioral changes in patients with traumatic brain injury before starting the EM protocol [55]. Persistent changes in ICP, loss of cerebral autoregulation, and hematoma expansion can be considered barriers to implementing of EM in traumatic brain injury [56].
EM in the neurological ICU is still a challenge, as the main consequential effects of EM in NCPs hospitalized in the ICU, in terms of its prescription, remain divergent. It is believed that there is an unknown mechanism together with higher and more frequent doses within the first 24 h after a neurological injury which has disabling consequences [52]. However, this effect has specifically been reported in stroke patients, and it is unclear for other neurological subpopulations.
It is known that one should consider the effect of positional changes and exercise, the time from the onset of symptoms to the onset of EM, and the prescribed exercise type and intensity when implementing an EM protocol in NCPs. However, there is a huge gap in available studies on this population, as well as in the existing studies, which have important methodological biases so that we can affirm the effectiveness and safety of implementing EM in the neurological ICU.
This review provided current concepts in physiotherapy management of neurocritically ill patients within the context of their neurologic pathology based on available literature. There is still no consensus on EM settings nor on the ideal time to start in NCPs. Nevertheless, we understand that EM with different protocols have been shown to be a useful, feasible and safe tool for use in NCPs. The proposed EM protocols must be well chosen and used judiciously by the health professional, on an individual basis, taking into account safety criteria and the pathophysiology of the neurocritical illness.
Conclusions
Diseases that affect the central and peripheral nervous systems are highly predisposed to hospitalization in ICUs. Critical neurological patients are predisposed to several harmful and pathophysiological events, which are associated with ICU-AW and worsen the clinical prognosis, increasing morbidity, mortality, and hospital costs.
In this context, in the present review we have identified that neural system injury in an NCP is the primary cause of a decrease in the level of consciousness in these patients, leading to an inability to protect the airways. This necessitates prolonged mechanical ventilation, ultimately resulting in muscular atrophy, particularly of the respiratory muscles. This predisposes the patient to complications associated with ventilator use, such as severe pneumonia. Given the complexity of these patients, bedridden immobility, and the presence of axonal degeneration of nerve fibers, there is severe muscle atrophy, which enhances the development of ICU-AW. Furthermore, patients with acute brain injury are predisposed to a significant increase in oxidative stress, evidenced by the presence of carbonylated proteins, lipid peroxides, and reactive oxygen and nitrogen species. Additionally, an elevated inflammatory process is observed, primarily characterized by the substantial elevation of TNF-α and IL-6. These intricate interactions among the neurological, muscular, and inflammatory systems in NCPs underscore the need for a multidisciplinary and individualized approach to optimize the treatment and rehabilitation of these patients. Therefore, EM has been used worldwide in critically ill patients, proving to be a safe and effective strategy to combat ICU-AW, even among intubated patients. However, implementing the EM routine in the neurological ICU is still challenging. Although many studies demonstrate that EM in NCPs is safe and feasible, there is evidence that points to divergent results, including negative effects of very EM in patients post stroke, which requires great caution. Moreover, there is no consensus in the literature on the ideal time and adequate dosage to perform the intervention according to the individualized clinical condition of the brain injury. Last but not least, future well-controlled RCTs are required to reinforce the recommendation of EM as an important rehabilitation treatment in NCPs, as well as to assess its effectiveness in various respiratory, musculoskeletal, and metabolic variables.
Contribution to the Field Statement
Neurocritical patients rapidly progress to respiratory and peripheral muscle dysfunctions, which significantly impact morbidity and death. Despite EM protocols being part of physical therapy management in the ICU, the EM for NCPs still evokes insecurity and resistance in the interdisciplinary team. This review will allow health professionals and researchers to know the main pathophysiological aspects of the respiratory, muscular, and metabolic systems in NCPs, as well as to understand the physiotherapeutic treatments performed in these patients, ensuring an effective and at the same time economical intervention for these individuals. Furthermore, this study will guide the development of robust research aimed at evaluating the effectiveness of EM in NCPs, strengthening the implementation of evidence-based practices in clinical routine.
References
Borsellino B, Schultz MJ, Gama de Abreu M, Robba C, Bilotta F. Mechanical ventilation in neurocritical care patients: a systematic literature review. Exp Rev Respir Med. 2016;10(10):1123–32. https://doi.org/10.1080/17476348.2017.1235976.
Engels PT, Beckett AN, Rubenfeld GD, Kreder H, Finkelstein JA, da Costa L, Papia G, Rizoli SB, Tien HC. Physical rehabilitation of the critically ill trauma patient in the ICU. Crit Care Med. 2013;41(7):1790–801.
Lee K, Rincon F. Pulmonary complications in patients with severe brain injury. Crit Care Res Pract. 2012;2012: 207247. https://doi.org/10.1155/2012/207247.
Hashem DM, Nelliot A, Needham DM. Early mobilization and rehabilitation in the ICU: moving Back to the future. Respir Care. 2016;61(7):971–9. https://doi.org/10.4187/respcare.04741. (Epub 2016 Apr 19 PMID: 27094396).
Zhang L, Hu W, Cai Z, Liu J, Wu J, Deng Y, Yu K, Chen X, Zhu L, Ma J, Qin Y. Early mobilization of critically ill patients in the intensive care unit: a systematic review and meta-analysis. PLoS ONE. 2019;14(10): e0223185. https://doi.org/10.1371/journal.pone.0223185.
Arias-Fernández P, Romero-Martin M, Gómez-Salgado J, Fernández-García D. Rehabilitation and early mobilization in the critical patient: systematic review. J Phys Ther Sci. 2018;30(9):1193–201. https://doi.org/10.1589/jpts.30.1193.
Newman ANL, Gravesande J, Rotella S, Wu SS, Topp-Nguyen N, Kho ME, Harris JE, Fox-Robichaud A, Solomon P. Physiotherapy in the neurotrauma intensive care unit: a scoping review. J Crit Care. 2018;48:390–406. https://doi.org/10.1016/j.jcrc.2018.09.037.
Miranda FEMH, Dias BCA, Macedo LB, Dias CMCC. Eletroestimulação em doentes críticos: uma revisão sistemática. Rev Pesq Fisiot. 2013;3(1):79–91. https://doi.org/10.17267/2238-2704rpf.v3i1.111.
Seder DB, Bösel J. Airway management and mechanical ventilation in acute brain injury. Handb Clin Neurol. 2017;140:15–32. https://doi.org/10.1016/B978-0-444-63600-3.00002-7.
Hannawi Y, Hannawi B, Rao CP, Suarez JI, Bershad EM. Stroke-associated pneumonia: major advances and obstacles. Cerebrovasc Dis. 2013;35(5):430–43. https://doi.org/10.1159/000350199.
Wen J, Chen J, Chang J, Wei J. Pulmonary complications and respiratory management in neurocritical care: a narrative review. Chin Med J (Engl). 2022;135(7):779–89. https://doi.org/10.1097/CM9.0000000000001930.PMID:35671179;PMCID:PMC9276382.
Friedrich O, Reid MB, Van den Berghe G, Vanhorebeek I, Hermans G, Rich MM, Larsson L. The sick and the weak: neuropathies/myopathies in the critically Ill. Physiol Rev. 2015;95(3):1025–109. https://doi.org/10.1152/physrev.00028.2014.
Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Med. 2020;46(4):637–53. https://doi.org/10.1007/s00134-020-05944-4.
Truong AD, Kho ME, Brower RG, Feldman DR, Colantuoni E, Needham DM. Effects of neuromuscular electrical stimulation on cytokines in peripheral blood for healthy participants: a prospective, single-blinded Study. Clin Physiol Funct Imaging. 2017;37(3):255–62. https://doi.org/10.1111/cpf.12290.
Deluzio S, Vora I, Kumble S, Zink EK, Stevens RD, Bahouth MN. Feasibility of early, motor-assisted cycle ergometry in critically ill neurological patients with upper limb weakness and variable cognitive status: a case series. Am J Phys Med Rehabil. 2018;97(5):e37–41. https://doi.org/10.1097/PHM.0000000000000857. (PMID: 29095167).
Mendez-Tellez PA, Nusr R, Feldman D, Needham DM. Early physical rehabilitation in the ICU: a review for the neurohospitalist. Neurohospitalist. 2012;2(3):96–105. https://doi.org/10.1177/1941874412447631.
Bolton CF, Gilbert JJ, Hahn AF, Sibbald WJ. Polyneuropathy in critically ill patients. J Neurol Neurosurg Psychiatry. 1984;47(11):1223–31. https://doi.org/10.1136/jnnp.47.11.1223.
Barbosa KBF, Costa NMB, Alfenas RCG, De Paula SO, Minim VPR, Bressan J. Oxidative stress: concept, implications and modulating factors. Rev Nutr. 2010;23(4):629–43. https://doi.org/10.1590/S1415-52732010000400013.
De Jonghe B, Shashar T, Lefaucheur JP, et al. Presis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002;288:2859–67.
Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of early rehabilitation during intensive care unit stay on functional status: systematic review and meta-analysis. PLoS ONE. 2015;10:0130722.
Klein K, Mulkey M, Bena JF, Albert NM. Clinical and psychological effects of early mobilization in patients treated in a neurologic ICU: a comparative study. Crit Care Med. 2015;43(4):865–73. https://doi.org/10.1097/CCM.0000000000000787. (PMID: 25517476).
Oliveira MC, Schoffen JPF. Oxidative stress action in cellular aging. Braz Arch Biol Technol. 2010;53(6):1333–42. https://doi.org/10.1590/S1516-89132010000600009.
Ferrari CK. Functional foods, herbs and nutraceuticals: towards biochemical mechanisms of healthy aging. Biogerontology. 2004;5(5):275–89. https://doi.org/10.1007/s10522-004-2566-z.
Neha K, Haider MR, Pathak A, Yar MS. Medicinal prospects of antioxidants: a review. Eur J Med Chem. 2019;15(178):687–704. https://doi.org/10.1016/j.ejmech.2019.06.010.
Powers SK, Jackson MJ. Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production. Physiol Rev. 2008;88(4):1243–76. https://doi.org/10.1152/physrev.00031.2007.
Brito AF, Oliveira CVC, Cardoso GA, Lucena JMS, Sousa JPS, Souza AA. Oxidative stress and vascular diseases: effect of physical exercise. Free Radical Antioxidants Disease. 2018. https://doi.org/10.5772/intechopen.76576.
Fraser DD, Morrison G. Brain oxidative stress after traumatic brain injury cool it? Crit Care Med. 2009;37(2):787–8. https://doi.org/10.1097/CCM.0b013e318194be10.
Bayir H, Marion DW, Puccio AM, Wisniewski SR, Janesko KL, Clark RS, Kochanek PM. Marked gender effect on lipid peroxidation after severe traumatic brain injury in adult patients. J Neurotrauma. 2004;21(1):1–8. https://doi.org/10.1089/089771504772695896.
Toklu HZ, Tümer N. Oxidative stress, brain edema, blood–brain barrier permeability, and autonomic dysfunction from traumatic brain injury. In: Kobeissy FH, editor. Brain neurotrauma: Molecular, neuropsychological, and rehabilitation aspects. Boca Raton, FL: CRC Press; 2015.
Jayaraj RL, Azimullah S, Beiram R, Jalal FY, Rosenberg GA. Neuroinflammation: friend and foe for ischemic stroke. J Neuroinflammation. 2019;16(1):142. https://doi.org/10.1186/s12974-019-1516-2.
Sulhan S, Lyon KA, Shapiro LA, Huang JH. Neuroinflammation and blood-brain barrier disruption following traumatic brain injury: pathophysiology and potential therapeutic targets. J Neurosci Res. 2020;98(1):19–28. https://doi.org/10.1002/jnr.24331.
Maida CD, Norrito RL, Daidone M, Tuttolomondo A, Pinto A. Neuroinflammatory mechanisms in ischemic stroke: focus on cardioembolic stroke, background, and therapeutic approaches. Int J Mol Sci. 2020;21(18):6454. https://doi.org/10.3390/ijms21186454.
França EE, Ribeiro LC, Lamenha GG, Magalhães IK, Figueiredo TG, Costa MJ, Elihimas UF Jr, Feitosa BL, Andrade MD, Correia MA Jr, Ramos FF, Castro CM. Oxidative stress and immune system analysis after cycle ergometer use in critical patients. Clinics Sao Paulo. 2017;72(3):143–9. https://doi.org/10.6061/clinics/2017(03)03.
França EET, Gomes JPV, De Lira JMB, Amaral TCN, Vilaça AF, Paiva Júnior MDS, Elihimas Júnior UF, Correia Júnior MAV, Forgiarini Júnior LA, Costa MJC, Andrade MA, Ribeiro LC, De Castro CMMB. Acute effect of passive cycle-ergometry and functional electrical stimulation on nitrosative stress and inflammatory cytokines in mechanically ventilated critically ill patients: a randomized controlled trial. Braz J Med Biol Res. 2020;53(4): e8770. https://doi.org/10.1590/1414-431X20208770.
Azevedo PMDS, Gomes BP. Effects of early mobilisation in the functional rehabilitation of critically ill patients: a systematic review. J Nurs Refer. 2015;4(5):129–38. https://doi.org/10.12707/RIV14035.
Morris PE, Griffin L, Berry M, Thompson C, Hite RD, Winkelman C, Hopkins RO, Ross A, Dixon L, Leach S, Haponik E. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. Am J Med Sci. 2011;341(5):373–7. https://doi.org/10.1097/MAJ.0b013e31820ab4f6.
Dantas CM, Silva PF, Siqueira FH, Pinto RM, Matias S, Maciel C, Oliveira MC, Albuquerque CG, Andrade FM, Ramos FF, França EE. Influence of early mobilization on respiratory and peripheral muscle strength in critically ill patients. Rev Bras Ter Intensiva. 2012;24(2):173–8.
TEAM Study Investigators and the ANZICS Clinical Trials Group; Hodgson CL, Bailey M, Bellomo R, Brickell K, Broadley T, Buhr H, Gabbe BJ, Gould DW, Harrold M, Higgins AM, Hurford S, Iwashyna TJ, Serpa Neto A, Nichol AD, Presneill JJ, Schaller SJ, Sivasuthan J, Tipping CJ, Webb S, Young PJ. Early Active Mobilization during Mechanical Ventilation in the ICU. N Engl J Med. 2022;387(19):1747–1758. https://doi.org/10.1056/NEJMoa2209083.
Doiron KA, Hoffmann TC, Beller EM. Early intervention mobilization or active exercise for critically ill adults in the intensive care unit. Cochrane Database Syst Rev. 2018;3(3):CD010754. https://doi.org/10.1002/14651858.CD010754.pub2.
Olkowski BF, Shah SO. Early mobilization in the neuro-ICU: how far can we go? Neurocrit Care. 2017;27(1):141–50. https://doi.org/10.1007/s12028-016-0338-7.
Bahouth MN, Power MC, Zink EK, Kozeniewski K, Kumble S, Deluzio S, Urrutia VC, Stevens RD. Safety and feasibility of a neuroscience critical care program to mobilize patients with primary intracerebral hemorrhage. Arch Phys Med Rehabil. 2018;99(6):1220–5. https://doi.org/10.1016/j.apmr.2018.01.034.
Titsworth WL, Hester J, Correia T, Reed R, Guin P, Archibald L, Layon AJ, Mocco J. The effect of increased mobility on morbidity in the neurointensive care unit. J Neurosurg. 2012;116(6):1379–88. https://doi.org/10.3171/2012.2.JNS111881. (Epub 2012 Mar 30 PMID: 22462507).
Zink EK, Kumble S, Beier M, George P, Stevens RD, Bahouth MN. Physiological responses to in-bed cycle ergometry treatment in Intensive Care Unit patients with external ventricular drainage. Neurocrit Care. 2021;35(3):707–13. https://doi.org/10.1007/s12028-021-01204-5.
Machado ADS, Pires-Neto RC, Carvalho MTX, Soares JC, Cardoso DM, Albuquerque IM. Effects of passive cycling exercise on muscle strength, duration of mechanical ventilation, and length of hospital stay in critically ill patients: a randomized clinical trial. J Bras Pneumol. 2017;43(2):134–9. https://doi.org/10.1590/S1806-37562016000000170.
Woo K, Kim J, Kim HB, Choi H, Kim K, Lee D, Na S. The effect of electrical muscle stimulation and in-bed cycling on muscle strength and mass of mechanically ventilated patients: a pilot study. Acute Crit Care. 2018;33(1):16–22. https://doi.org/10.4266/acc.2017.00542.
Yu L, Jiang JX, Zhang Y, Chen YZ, Shi Y. Use of in-bed cycling combined with passive joint activity in acute respiratory failure patients receiving mechanical ventilation. Ann Palliat Med. 2020;9(2):175–81. https://doi.org/10.21037/apm.2020.02.1247.
Thelandersson A, Nellgård B, Ricksten SE, Cider Å. Effects of early bedside cycle exercise on intracranial pressure and systemic hemodynamics in critically Ill patients in a neurointensive care unit. Neurocrit Care. 2016;25(3):434–9. https://doi.org/10.1007/s12028-016-0278-2.
da Rosa Pinheiro DR, Cabeleira MEP, da Campo LA, Corrêa PS, Blauth AHEG, Cechetti F. Effects of aerobic cycling training on mobility and functionality of acute stroke subjects: a randomized clinical trial. NeuroRehabilitation. 2021;48(1):39–47. https://doi.org/10.3233/NRE-201585.
Liu M, Luo J, Zhou J, Zhu X. Intervention effect of neuromuscular electrical stimulation on ICU acquired weakness: a meta-analysis. Int J Nurs Sci. 2020;7(2):228–37. https://doi.org/10.1016/j.ijnss.2020.03.00250.
Silva PE, de Cássia Marqueti R, Livino-de-Carvalho K, de Araujo AET, Castro J, da Silva VM, Vieira L, Souza VC, Dantas LO, Cipriano G Jr, Nóbrega OT, Babault N, Durigan JLQ. Neuromuscular electrical stimulation in critically ill traumatic brain injury patients attenuates muscle atrophy, neurophysiological disorders, and weakness: a randomized controlled trial. J Intensive Care. 2019;12(7):59. https://doi.org/10.1186/s40560-019-0417-x.
Hirose T, Shiozaki T, Shimizu K, Mouri T, Noguvhi K, Ohnishi M, Shimazu T. The effect of electrical muscle stimulation on the prevention of disuse muscle atrophy in patients consciousness disturbance in the intensive care unit. J Crit Care. 2013;28(4):536. https://doi.org/10.1016/j.jcrc.2013.02.010.
AVERT Trial Collaboration group. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet. 2015;386(9988):46–55. https://doi.org/10.1016/S0140-6736(15)60690-0.
Thijs RD, Brignole M, Falup-Pecurariu C, Fanciulli A, Freeman R, Guaraldi P, Jordan J, Habek M, Hilz M, Pavy-LeTraon A, Stankovic I, Struhal W, Sutton R, Wenning G, van Dijk JG. Recommendations for tilt table testing and other provocative cardiovascular autonomic tests in conditions that may cause transient loss of consciousness : consensus statement of the European Federation of Autonomic Societies (EFAS) endorsed by the American Autonomic Society (AAS) and the European Academy of Neurology (EAN). Auton Neurosci. 2021;233: 102792. https://doi.org/10.1016/j.autneu.2021.102792. (Epub 2021 Mar 19 PMID: 33752997).
Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurology. 1996;46(5):1470. https://doi.org/10.1212/wnl.46.5.1470. PMID: 8628505.
Kocan MJ, Lietz H. Special considerations for mobilizing patients in the neurointensive care unit. Crit Care Nurs Q. 2013;36(1):50–5. https://doi.org/10.1097/CNQ.0b013e3182750b12.
Kumar MA, Romero FG, Dharaneeswaran K. Early mobilization in neurocritical care patients. Curr Opin Crit Care. 2020;26(2):147–54. https://doi.org/10.1097/MCC.0000000000000709.
Funding
Self-funding.
Author information
Authors and Affiliations
Contributions
TM: Determination of search criteria and eligibility of articles, literary search, manuscript preparation, and manuscript review. PM: writing-reviewing and editing. DS: determination of search criteria and eligibility of articles, literary search, and manuscript review. JG: writing-reviewing and editing. PS: writing-reviewing and editing. AB: determination of search criteria and eligibility of articles, literary search, and manuscript review. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of Interest
None.
Ethical Approval/Informed Consent
The authors confirm adherence to ethical guidelines. According to research ethics guidelines, literature reviews do not require approval from an ethics committee, as they do not involve the collection of primary data, the handling of personal information, or any direct interaction with human study participants. Our article is a review study, based on the analysis of previously published literature and publicly available information. Therefore, ethical committee approval was not necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maia, T.F.L.D., Magalhães, P.A.F., Santos, D.T.S. et al. Current Concepts in Early Mobilization of Critically Ill Patients Within the Context of Neurologic Pathology. Neurocrit Care 41, 272–284 (2024). https://doi.org/10.1007/s12028-023-01934-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01934-8