Abstract
Background
Individual extracerebral organ dysfunction is common after severe traumatic brain injury (TBI) and impacts outcomes. However, multiorgan failure (MOF) has received less attention in patients with isolated TBI. Our objective was to analyze the risk factors associated with the development of MOF and its impact in clinical outcomes in patients with TBI.
Methods
This was an observational, prospective, multicenter study using data from a nationwide registry that currently includes 52 intensive care units (ICUs) in Spain (RETRAUCI). Isolated significant TBI was defined as Abbreviated Injury Scale (AIS) ≥ 3 in the head area with no AIS ≥ 3 in any other anatomical area. Multiorgan failure was defined using the Sequential-related Organ Failure Assessment as the alteration of two or more organs with a score of ≥ 3. We analyzed the contribution of MOF to crude and adjusted mortality (age and AIS head) by using logistic regression analysis. A multiple logistic regression analysis was performed to analyze the risk factors associated with the development of MOF in patients with isolated TBI.
Results
A total of 9790 patients with trauma were admitted to the participating ICUs. Of them, 2964 (30.2%) had AIS head ≥ 3 and no AIS ≥ 3 in any other anatomical area, and these patients constituted the study cohort. Mean age was 54.7 (19.5) years, 76% of patients were men, and ground-level falls were the main mechanism of injury (49.1%). In-hospital mortality was 22.2%. Up to 185 patients with TBI (6.2%) developed MOF during their ICU stay. Crude and adjusted (age and AIS head) mortality was higher in patients who developed MOF (odds ratio 6.28 [95% confidence interval 4.58–8.60] and odds ratio 5.20 [95% confidence interval 3.53–7.45]), respectively. The logistic regression analysis showed that age, hemodynamic instability, the need of packed red blood cells concentrates in the initial 24 h, the severity of brain injury, and the need for invasive neuromonitoring were significantly associated with MOF development.
Conclusions
MOF occurred in 6.2% of patients with TBI admitted to the ICU and was associated with increased mortality. MOF was associated with age, hemodynamic instability, the need of packed red blood cells concentrates in the initial 24 h, the severity of brain injury, and the need for invasive neuromonitoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individual extracerebral organ dysfunction is common after severe traumatic brain injury (TBI) and has an impact in clinical outcomes [1,2,3]. However, development of multiorgan failure (MOF), which constitutes a well-known phenomena in different forms and trajectories in patients with severe trauma [4,5,6], has received less attention and has, therefore, been underestimated in patients with isolated TBI [3].
Krishnamoorthy et al. [3] have recently addressed the epidemiology, mechanisms, and management of MOF in patients with TBI, concluding that severe TBI results in significant dysfunction to extracranial organ systems, which contribute to secondary brain injuries and poor clinical outcomes [3]. The authors also concluded that the optimal prevention and treatment of MOF following severe TBI has the potential to improve clinical outcomes [3].
To evaluate the magnitude of burden of MOF in patients with TBI, our objective was to analyze the risk factors associated with the development of MOF in a large sample of isolated patients with TBI and its impact in clinical outcomes using data from the Spanish Trauma intensive care unit (ICU) Registry (RETRAUCI).
Methods
RETRAUCI is an observational, prospective, and multicenter nationwide registry that currently includes 52 ICUs in Spain. It is endorsed by the Neurointensive Care and Trauma Working Group of the Spanish Society of Intensive Care Medicine and currently works on a electronic database (retrauci.org). Ethics Committee approval for the registry was obtained (Hospital Universitario 12 de Octubre, Madrid: 12/209). Because of the retrospective analysis of deidentified collected data, informed consent was not obtained for this specific study.
Study Population
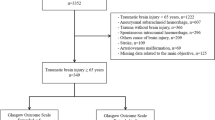
Significant TBI was defined as Abbreviated Injury Scale (AIS) ≥ 3 in the head area. Patients with AIS head < 3 or patients with AIS ≥ 3 in any other anatomical area were not included in this study. Patients with missing data about MOF or in-hospital mortality or incomplete data during the study period were excluded.
Patients were included in this study from March 2015 to December 2019 and were initially managed according to the Advanced Trauma Life Support (ATLS) principles. After ICU admission, the Brain Trauma Foundation guidelines principles were followed [7]. In this population, we analyzed the incidence, outcomes, and the risk factors associated with MOF in patients with isolated TBI admitted to the participating ICUs. Data on epidemiology, acute management in the prehospital and in-hospital stages, type and severity of injury, resources use, complications, and outcomes were recorded [6].
Definitions
-
Multiorgan failure was defined using the Sequential-related Organ Failure Assessment (SOFA) as the alteration of two or more organs (including central nervous system component) with a score of ≥ 3 [6, 8].
-
Hemodynamic condition was considered as follows [6]:
-
Stable: systolic blood pressure > 90 mm Hg during initial trauma care.
-
Unstable, responding to olumen replacement: systolic blood pressure < 90 mm Hg requiring olumen replacement for normalization.
-
Shock: systolic blood pressure < 90 mm Hg requiring olumen replacement, blood products, and vasoactive support for normalization.
-
Refractory shock: hypotension refractory to olumen replacement, blood products, or vasoactive support and activation of the massive bleeding protocol.
-
-
Trauma-associated coagulopathy: prolongation of the prothrombin and activated partial thromboplastin times more than 1.5 times the control values, or fibrinogen < 150 mg/dL or thrombocytopenia (< 100,000 mg/µL) in the first 24 h.
Statistical Analysis
Quantitative variables are shown as means ± standard deviations, and qualitative variables are shown as percentages. Categorical variables were analyzed using the χ2 or Fisher’s exact test. For continuous data, we studied normality with the Shapiro–Wilk test. Continuous data had a nonnormal distribution and were evaluated by using the nonparametric Kruskal–Wallis test. We analyzed the contribution of MOF to crude and adjusted mortality (age and AIS head) by using logistic regression analysis. A multiple logistic regression analysis was performed to analyze the risk factors associated with the development of MOF in patients with isolated TBI. The variables entered in the logistic regression analysis were those significantly associated with MOF in the univariate analysis. A p value < 0.10 was considered significant. Results are presented as odds ratios (ORs) with 95 percent confidence intervals (CIs). The discrimination of the logistic regression model was assessed by using the area under the receiver operating characteristic curve. Calibration was evaluated by using the χ2 Hosmer–Lemeshow test and calibration belt [9]. Additionally, we used nonhierarchical cluster analysis to identify phenotypes with different risks and profile of MOF. The K-means method was applied. The number of clusters (k) was determined with the Calinski and Harabasz pseudo-F index [10]. Included variables were age, systolic blood pressure pressure (on scene), cardiac rate (on scene), and probablity of survival calculated by the Trauma Score and Injury Severity Score. Variables were compared across the clusters. We reported all results as stated in the record statement [11]. Statistical analysis was performed with STATA 15 (StataCorp. 2017).
Results
During the study period, a total of 9,790 patients with trauma were admitted to the participating ICUs. Of them, 2964 (30.2%) had AIS head ≥ 3 and no AIS ≥ 3 in any other anatomical area. This was the study cohort. Mean age was 54.7 (19.5) years, 76% of patients were men, and ground-level falls were the main mechanism of injury (49.1%). Up to 26.2% received prehospital intubation. Mean Injury Severity Score was 18.4 (8). In-hospital mortality was 22.2%.
Up to 185 patients with TBI (6.2%) developed MOF during their ICU stay. Patients who presented with MOF were older, had hemodynamic instability, needed prehospital intubation and required blood products in the initial 24 h of ICU admission more frequently than patients without MOF (Table 1). Days of mechanical ventilation (12.48 [14.97] vs. 7.83 [2.48], p < 0.001) and ICU length of stay (days) (15.66 [17.40] vs. 9.22 [13.90], p < 0.001) were higher in patients with TBI and MOF.
Patients who developed MOF were more severely injured according to their neurological responses, as they had the lowest Glasgow Coma Scale scores, the worst pupillary reactivity, and higher AIS head scores and were more likely to receive invasive neuromonitoring and present intracranial hypertension (Table 2).
Crude and adjusted (age and AIS Head) ORs for mortality were 6.28 (95% CI 4.58–8.60) and 5.20 (95% CI 3.53–7.45). Moreover, in 38 out of the 185 patients who presented with MOF (20.54%) this was the main cause of death (Fig. 1).
The logistic regression analysis showed that age, hemodynamic instability, the need of packed red blood cells concentrates in the initial 24 h, the severity of brain injury and the need of invasive neuromonitoring were significantly associated with MOF development. Performance of emergency neurosurgery was a protective factor (Table 3) of MOF development. The calibration and goodness of fit for the final model are presented in the area under the receiver operating characteristic curve and calibration belt plots (Figs. 2, 3). In the group of 185 patients with TBI who developed MOF, 67 received emergency neurosurgery and 118 did not. In the later group (nonoperated MOF), 27.1% of the patients received intensive care oriented to organ donation, compared with 2.9% in the surgical group (p < 0.001).
The clustering analysis identified four different phenotypes of patients with TBI with different clinical characteristics, incidence of MOF, and risk of death (Fig. 4). The type 1 cluster included middle-aged, hemodynamically stable patients with TBI with less severe brain injury and low risk of MOF and death. The type 2 cluster included aged patients with severe TBI and more hemodynamic compromise. The type 3 cluster were patients initially atended in an “in-extremis” condition, as stated by its high mortality, and the type 4 were geriatric patients, hemodynamically stable with moderate brain injury and low risk of MOF. The characteristics of the different clusters are summarized in Table 4.
Discussion
The main results of our study were as follows: multiorgan failure occurred in 6.2% of patients with TBI admitted to the ICU. MOF was associated with increased crude and adjusted mortality. MOF was associated with age, hemodynamic instability, the need of packed red blood cells concentrates in the initial 24 h, the severity of brain injury, and the need for invasive neuromonitoring.
Extracranial organ dysfunction is common after TBI and may impact clinical care and outcomes [1, 2, 12]. However, it has been usually addressed from an individual organ dysfunction approach, being studies less focused in MOF [3]. MOF can be associated with reduced cerebral blood flow, cerebral hipoxia, altered metabolism, acidosis, and bleeding, turning into a vicious circle of secondary brain injury and poor clinical outcomes [3]. Indeed, a recent study by the Transforming Research and Clinical Knowledge in traumatic brain injury (TRACK-TBI) investigators in 373 patients with moderate-to-severe TBI showed that early multiple organ dysfunction was common (up to 68%) and independently impacted multiple domains (mortality, function, and disability) over the year following injury [13].
In our study, we observed an incidence of 6.2%. Our incidence is low in comparison to previous studies addressing this topic, but it has to be considered that heterogeneity in the definitions used imply that comparison shoud be considered with caution [3]. We used the SOFA score, which—in the general population of patients with trauma—shows the best balance between sensitivity and specifity [14] and is gaining attention in patients with TBI [15]. Even using this score, different cutoff points have been used so it has to be taken into account when performing comparisons. In any case, our results are consistent with previous studies in the general trauma population that showed low incidence of MOF with late MOF being almost residual [4, 6].
We also observed that both crude and adjusted (age and AIS head) mortality clearly increased in patients with TBI who developed MOF, both because of direct mortality (it was considered the main cause of mortality in 20.54% of the patients who developed MOF) and because of its role in worsening secondary brain injury through different mechanisms [3].
We then used nonhierarchical cluster nálisis to identify phenotypes with different risks and profile of MOF, showing four different patterns with specifical risk of MOF and death at ICU admission. The identification of these phenotypes allowed us to deepen into the underlying pathophysiologies of MOF, and could potentially lead to personalization of critical care supporting measures. Clusters include information that can provide a signifcantly better explanation beyond that provided by commonly used variables [16].
Krishnamoorthy et al. [3] support that prevention and management of extracranial organ dysfunction is a clinical priority, since management of severe TBI requires balancing the optimization of often competing management strategies. MOF in patients with TBI is usually associated with prolonged forms in survivors [4] and short time to death in nonsurvivors [5]. Treament must rely on primary injury management and well-established fundamentals of supportive critical care [3]. However, we found that associated risk factors to the development of MOF were related to the severity of injury (initial hemodynamic condition, AIS head and need of invasive monitoring) and to patient factors (age) which are not modifiable. Only the need of packed red blood cells concentrates in the first 24 h could be a modifiable factor by providing restrictive strategies. However, this is a controversial topic since there is insufficient evidence to make strong recommendations of which hemoglobin threshold must be used as a transfusion trigger in critically-ill patients with TBI [17, 18]. The “protective” role of emergency neurosurgery in MOF development cannot be clearly explained by the data collected in our registry. We can only speculate three different factors influencing this finding, that in any case, warrants further studies:
-
Patients who developed MOF and were not operated presented a high percentage of patients who received ICU oriented to organ donation. Those patients can receive neuromonitoring and have a high mortality. This is a common TBI population in our environment [19, 20].
-
Type 3 patients, those who were initially attended in an “in-extremis” condition, were monitored and had a high incidence of MOF and a low incidence of emergency neurosurgery and 80% mortality.
-
There was a disbalance of focal vs. diffuse injuries in both groups.
More intriguing is the recent evidence suggesting that TBI is also associated with a higher risk of chronic cardiovascular, endocrine, and neurological comorbidities, even in young and healthy study participants [21, 22], suggesting that TBI is a multisystem condition [22]. Whether early MOF and its potential treatment has an impact on these chronic multiple organ diseases needs to be addressed yet.
Our study has several strengths, including a large sample of patients with TBI admitted to the participating ICUs with MOF classified according to the SOFA score. We believe that it helps to delineate the epidemiology of MOF in patients with isolated TBI. The use of clustering analysis constitute an added value, since characterizing different MOF subtypes could be relevant to understand underlying pathophysiologies, to develope new therapeutic approaches and to design clinical studies [4, 16]. Overall, our findings support the usefulness of trauma registries in the management and benchmarking of patients with trauma [23]. However, we must also keep in mind our limitations: First, unless patients were initially managed following the ATLS principles we cannot rule out deviations so this could affect patients’ management and therefore the incidence of MOF. Second, as previously stated, definitions of MOF are heterogeneus and this may impact incidences reported [14]. Lastly, because of the design of the registry, we did not take into account comorbidities which may, in turn, predispose to MOF development.
In conclusion, MOF occurred in 6.2% of patients with TBI admitted to the ICU and was associated with increased crude and adjusted mortality. MOF was associated with age, hemodynamic instability, the need of packed red blood cells concentrates in the initial 24 h, the severity of brain injury, and the need for invasive neuromonitoring.
References
Robba C, Bonatti G, Pelosi P, Citerio G. Extracranial complications after traumatic brain injury: targeting the brain and the body. Curr Opin Crit Care. 2020;26(2):137–46.
Mascia L, Sakr Y, Pasero D, Payen D, Reinhart K, Vincent JL, Sepsis Occurrence in Acutely Ill Patients (SOAP) Investigators. Extracranial complications in patients with acute brain injury: a post-hoc analysis of the SOAP study. Intensive Care Med. 2008;34(4):720–7.
Krishnamoorthy V, Komisarow JM, Laskowitz DT, Vavilala MS. Multiorgan dysfunction after severe traumatic brain injury: epidemiology, mechanisms, and clinical management. Chest. 2021;160(3):956–64.
Cole E, Gillespie S, Vulliamy P, Brohi K, Organ Dysfunction in Trauma (ORDIT) study collaborators. Multiple organ dysfunction after trauma. Br J Surg. 2020;107(4):402–12.
Eriksson J, Nelson D, Holst A, Hellgren E, Friman O, Oldner A. Temporal patterns of organ dysfunction after severe trauma. Crit Care. 2021;25(1):165.
Barea-Mendoza JA, Chico-Fernández M, Molina-Díaz I, Moreno-Muñoz G, Toboso-Casado JM, Viña-Soria L, Neurointensive Care and Trauma Working Group of the Spanish Society of Intensive Care Medicine (SEMICYUC), et al. Risk factors associated with early and late posttraumatic multiorgan failure: an analysis from RETRAUCI. Shock. 2021;55(3):326–31.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80(1):6–15.
Dewar D, Moore FA, Moore EE, Balogh Z. Postinjury multiple organ failure. Injury. 2009;40(9):912–8.
Nattino G, Lemeshow S, Phillips G, Finazzi S, Bertolini G. Assessing the calibration of dichotomous outcome models with the calibration belt. Stand Genom Sci. 2017;17(4):1003–14.
Castela Forte J, Perner A, van der Horst ICC. The use of clustering algorithms in critical care research to unravel patient heterogeneity. Intensive Care Med. 2019;45(7):1025–8.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, RECORD Working Committee, et al. The REporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12:e1001885.
Astarabadi M, Khurrum M, Asmar S, Bible L, Chehab M, Castanon L, et al. The impact of non-neurological organ dysfunction on outcomes in severe isolated traumatic brain injury. J Trauma Acute Care Surg. 2020;89(2):405–10.
Krishnamoorthy V, Temkin N, Barber J, Foreman B, Komisarow J, Korley FK, Transforming Clinical Research and Knowledge in TBI (TRACK-TBI) Investigators, et al. Association of early multiple organ dysfunction with clinical and functional outcomes over the year following traumatic brain injury: a transforming research and clinical knowledge in traumatic brain injury study. Crit Care Med. 2021;49(10):1769–78.
Fröhlich M, Wafaisade A, Mansuri A, Koenen P, Probst C, Maegele M, et al. Which score should be used for posttraumatic multiple organ failure?—Comparison of the MODS, Denver- and SOFA-scores. Scand J Trauma Resusc Emerg Med. 2016;24(1):130.
Lee S, Hwang H, Yamal JM, Goodman JC, Aisiku IP, Gopinath S, et al. IMPACT probability of poor outcome and plasma cytokine concentrations are associated with multiple organ dysfunction syndrome following traumatic brain injury. J Neurosurg. 2019;131(6):1931–7.
Åkerlund CAI, Holst A, Stocchetti N, Steyerberg EW, Menon DK, Ercole A, Nelson DW, CENTER-TBI Participants and Investigators. Clustering identifies endotypes of traumatic brain injury in an intensive care cohort: a CENTER-TBI study. Crit Care. 2022;26(1):228.
East JM, Viau-Lapointe J, McCredie VA. Transfusion practices in traumatic brain injury. Curr Opin Anaesthesiol. 2018;31(2):219–26.
Egea-Guerrero JJ, García-Sáez I, Quintana-Díaz M. Trigger transfusion in severe traumatic brain injury. Med Intensiva (Engl Ed). 2022;46(3):157–60.
Domínguez-Gil B, Coll E, Elizalde J, Herrero JE, Pont T, Quindós B, et al. Expanding the donor pool through intensive care to facilitate organ donation: results of a Spanish multicenter study. Transplantation. 2017;101(8):e265–72.
Escudero Augusto D, Martínez Soba F, de la Calle B, Pérez Blanco A, Estébanez B, Velasco J, et al. Intensive care to facilitate organ donation. ONT-SEMICYUC recommendations. Med Intensiva. 2021;45(4):234–42.
Izzy S, Chen PM, Tahir Z, Grashow R, Radmanesh F, Cote DJ, et al. Association of traumatic brain injury with the risk of developing chronic cardiovascular, endocrine, neurological, and psychiatric disorders. JAMA Netw Open. 2022;5(4):e229478.
Krishnamoorthy V, Vavilala MS. Traumatic brain injury and chronic implications beyond the brain. JAMA Netw Open. 2022;5(4):e229486.
Lecky F, Woodford M, Edwards A, Bouamra O, Coats T. Trauma scoring systems and databases. Br J Anaesth. 2014;113(2):286–94.
Acknowledgements
The authors thank all the RETRAUCI investigators for their continuous effort.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: JAB-M, MC-F, JAL-P. Methodology: JAB-M, MC-F, JAL-P. Data collection: JAB-M, MC-F, LS-G, MQ-D, IG-S, MAB-S, AI-S, IM-D, JG-R, AF-C, JP-B, JAL-P. Formal analysis and investigation: JAB-M, MC-F, JAL-P. Writing—original draft: JAB-M, JAL-P. Writing—review and editing: JAB-M, MC-F, LS-G, MQ-D, IG-S, MAB-S, AI-S, IM-D, JG-R, AF-C, JP-B, JAL-P. Funding acquisition: N/A. Supervision: MC-F, JAL-P. All authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest related to this article.
Ethical Approval/Informed Consent
The article adheres to ethical guidelines. Ethics Committee approval for the registry was obtained (Hospital Universitario 12 de Octubre, Madrid: 12/209). Because of the retrospective analysis of deidentified collected data, informed consent was not required for this specific study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barea-Mendoza, J.A., Chico-Fernández, M., Serviá-Goixart, L. et al. Associated Risk Factors and Impact in Clinical Outcomes of Multiorgan Failure in Patients with TBI. Neurocrit Care 39, 411–418 (2023). https://doi.org/10.1007/s12028-023-01698-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01698-1