Abstract
Background
Consciousness in patients with brain injury is traditionally assessed based on semiological evaluation at the bedside. This classification is limited because of low granularity, ill-defined and rigid nomenclatures incompatible with the highly fluctuating nature of consciousness, failure to identify specific brain states like cognitive motor dissociation, and neglect for underlying biological mechanisms. Here, the authors present a pragmatic framework based on consciousness endotypes that combines clinical phenomenology with all essential physiological and biological data, emphasizing recovery trajectories, therapeutic potentials and clinical feasibility.
Methods
The Neurocritical Care Society’s Curing Coma Campaign identified an international group of experts who convened in a series of online meetings between May and November 2020 to discuss and propose a novel framework for classifying consciousness.
Results
The expert group proposes Advanced Classification of Consciousness Endotypes (ACCESS), a tiered multidimensional framework reflecting increasing complexity and an aspiration to consider emerging and future approaches. Tier 1 is based on clinical phenotypes and structural imaging. Tier 2 adds functional measures including EEG, PET and functional MRI, that can be summarized using the Arousal, Volition, Cognition and Mechanisms (AVCM) score (where “Volition” signifies volitional motor responses). Finally, Tier 3 reflects dynamic changes over time with a (theoretically infinite) number of physiologically distinct states to outline consciousness recovery and identify opportunities for therapeutic interventions.
Conclusions
Whereas Tiers 1 and 2 propose an approach for low-resource settings and state-of-the-art expertise at leading academic centers, respectively, Tier 3 is a visionary multidimensional consciousness paradigm driven by continuous incorporation of new knowledge while addressing the Curing Coma Campaign’s aspirational goals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In clinical practice, the level of consciousness is typically characterized by using a combination of bedside examination techniques, which are subject to the examiner’s abilities and preferences, as well as by using standardized rating scales, such as the Glasgow Coma Scale [1, 2], the Full Outline of Unresponsiveness Score [3,4,5], and the Coma Recovery Scale-Revised (CRS-R) [6]. An attempt is then made to categorize the state of consciousness of a given patient into one of several states that are well established in the neurological literature despite their limitations [7], including coma [8], the vegetative state/unresponsive wakefulness syndrome (VS/UWS) [9], and the minimally conscious state (MCS) [10]; the latter may be subdivided into MCS “plus” and “minus”, depending whether or not there is (rudimentary) language processing [11].
With the advent of sophisticated functional neuroimaging and electroencephalography (EEG)-based technologies [12,13,14,15,16,17,18,19,20,21], new states have been described that defy established neurological paradigms [7]. These include cognitive motor dissociation (CMD), that is, the presence of brain modulation in response to verbal commands during functional magnetic resonance imaging (fMRI) and EEG despite the absence of volitional responsiveness at the bedside [22], and higher-order cortex motor dissociation, also termed “covert cortical processing” [23], that is, fMRI and EEG evidence of association cortex activity to passive stimuli in clinically low or unresponsive patients [22].
Thus, the existing framework for characterizing disorders of consciousness could be improved in four key areas.
Reliance on Motor Function to Assess Consciousness
Cognitive motor dissociation, now well recognized [22], represents a confound in which clinical examination fails because patients can have a repertoire of cognitive and emotional brain responses, detectable by functional imaging or EEG measures [12], but without being able to manifest these to the outside world through movement or speech. This confound can only be addressed by dissociating arousal, volitional responses, and cognitive capacity in a rational assessment of patients with disorders of consciousness.
Inadequate Prognostication
Location on the hierarchy of disorders of consciousness (i.e., from coma to MCS-plus) has, by itself, some prognostic significance, with patients in an MCS or above thought to have a greater likelihood of recovery [24]. However, with time, even patients who are in a VS/UWS may progress and sometimes show remarkable recoveries [25], and others, although in an MCS, show limited progress. Such variance in spontaneous recovery may be driven, to some extent, by different intrinsic host responses (e.g., varying potential for synaptogenesis and neurotrophin production). However, it is likely that a substantial proportion of this variance is due to the extent, type, and location of underlying injury, which is incompletely characterized by current clinical tools of structural imaging and conventional EEG analysis.
Failure to Incorporate Mechanisms Responsible for Disorders of Consciousness into Therapeutic Stratification
Emergence from disorders of consciousness can be facilitated by pharmacological interventions that enhance arousal systems [26] or by neural stimulation, either peripherally (e.g., median nerve or vagal stimulation) or centrally (e.g., deep brain stimulation) [27]. However, responses to these interventions are by no means consistent, and there is, as yet, limited evidence to support a rational approach for “arousal agents” (to augment select neurochemical systems) or submitting patients to a potentially hazardous surgical intervention (or locating the optimal target for deep brain stimulation).
Clinical Translation for the Nonexpert
Although the CRS-R is a rigorous and well-validated tool, it has not gained the widespread adoption beyond specialist clinicians and researchers. Consequently, the CRS-R has not become part of everyday clinical discourse. The simplicity of the UWS and MCS classification and the Glasgow Coma Scale has resulted in common clinical usage, but these methods still fail to provide a complete description of patients.
Recent guidelines from the American [28] and European [29] Academies of Neurology synthesized the pertinent data from clinical examination and functional imaging/electrophysiology but did not attempt to provide a novel framework for classifying disorders of consciousness that would resolve the challenges outlined. There is a need for a different approach that is flexible enough to adapt to available resources, that more completely characterizes patients in everyday clinical management, and that allows for incorporation of new knowledge as it arises. Restated, the field of consciousness research must move forward from consciousness phenotypes to consciousness endotypes, that is, designations that consider complex concepts, such as biological mechanisms, clinical trajectories, and treatment targets.
In this article, the authors propose a rational precision medicine framework, combining clinical phenomenology with physiological and biological data, to emphasize recovery trajectories and therapeutic potentials while at the same time considering pragmatism and clinical feasibility.
Methods
The Neurocritical Care Society’s Curing Coma Campaign identified an international group of experts, one of five Coma Science Working Groups, taking into account geographical distribution, scientific track records, earlier and later career stages, and lack of conflicts of interest.
The objective was to develop a conceptual framework for disorders of consciousness that (1) preserves key etiological and temporal information about the patient; (2) dissociates clinically assessed arousal and volitional motor responses from cognitive capacity, including recognition and integration of covert cognition into overall patient assessment; (3) incorporates information about underlying mechanistic causes of disorders of consciousness, potentially identifying structural, functional, or modulatory deficits; (4) does not depend on a given theoretical framework of consciousness; (5) provides information on clinical trajectory through serial assessment; (6) identifies likelihood of response to therapy (or specific therapies); (7) incorporates data on prognosis; (8) provides an accessible summary for clinical communication; (9) is applicable to low-resource and high-resource settings, including state-of-the-art academic centers; (10) allows for incorporation of novel knowledge as it arises; and (11) considers the degree of confidence in the drawn conclusion.
The group convened in a series of online meetings between May 17 and November 6, 2020, to discuss and propose a new consciousness framework using an evidence synthesis and gap analysis approach [30]. Disagreement was resolved by consensus, and the final manuscript was approved by all group members.
Results
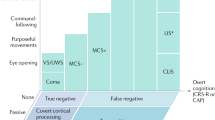
The authors propose Advanced Classification of Consciousness Endotypes (ACCESS), a framework for disorders of consciousness in brain injury that is based on a three-tiered approach reflecting increasing levels of complexity and scientific ambitions (Fig. 1). Because consciousness evaluation depends on factors such as clinical proficiency, technological expertise, and suitability of analytical methods, examiners would be asked to rate their degree of confidence (low vs. high) in each of the three tiers.
Advanced Classification of Consciousness Endotypes (ACCESS), a proposed framework based on a three-tiered approach of increasing scientific complexity and ambition. Tier 1 is designed to meet possibilities in low-resource settings and takes into consideration clinical examination and structural neuroimaging. Tier 2 adds measures of brain function, allowing detection of covert consciousness in unresponsive patients. Data from tier 2 can be conveniently summarized by using the arousal, volition, cognition, and mechanisms (AVCM) score. Finally, tier 3 accommodates all relevant biological and physiological data and allows one to follow evolution of consciousness endotypes over time (i.e., clinical trajectories) and to identify and test therapeutic interventions. This scheme can flexibly incorporate future developments on the molecular and cellular level to better characterize brain function (consciousness endotypes). Of note, clinical proficiency, availability of technology, and technological expertise, as well as appropriateness of analytical methods, all influence the level of certainty with which conclusions about consciousness levels are made; the framework therefore requires investigators to state their degree of confidence (low, intermediate, or high) to account for these caveats. CRS-R Coma Recovery Scale–Revised, CT computed tomography, EEG electroencephalography, fMRI functional magnetic resonance imaging, MRI magnetic resonance imaging, PET positron emission tomography, T1 and T2 time points 1 and 2
Tier 1
This tier takes into account low-resource settings, which typically are restricted to clinical examination and structural neuroimaging (Fig. 1).
For clinical examination, the CRS-R [6] remains the best validated tool [31], allowing one to detect signs of preserved responsiveness in up to 40% of patients who are (mis)classified as in a VS/UWS on the basis of unstructured neurological examination alone [32]. Scales akin to the CRS-R yet customized to specific settings, such as intensive care, are emerging [33]. The utility of even more subtle clinical signs suggestive of preserved responsiveness is increasingly recognized: for instance, low-cost bedside markers that lack sufficient formal evidence but, nevertheless, appear promising include command following as assessed by automated pupillometry [34, 35]; resistance to eye opening [36]; habituation of the auditory startle reflex [37]; quantitative assessment of visual tracking [38, 39]; standardized rating of spontaneous motor behavior [40]; possibility of oral feeding [41]; exploitation of vegetative responses, such as increased salivation following gustatory stimuli [42], olfactory sniffing [43], or modulations of the cardiac cycle [44, 45]; evidence of circadian rhythms [46]; and observations made by nursing staff [47]. Simple clinical tools may provide substantial insights—carinal stimulation (by tracheal suctioning in an intubated or tracheostomized patient [48]) can produce intense arousal and improve motor responsiveness—suggesting the potential for progress in the acute phase or (potentially) responsiveness to pharmacological arousal agents in the chronic phase.
For structural neuroimaging, computed tomography of the brain is increasingly available in low-resource settings [49] such that common etiologies of disorders of consciousness are readily identifiable most of the time (e.g., hemorrhagic or ischemic stroke), including actionable therapeutic opportunities, occasionally, even in prolonged disorders of consciousness, for example, improved arousal following ventriculoperitoneal shunting in late-onset hydrocephalus [50].
Tier 2
Tier 2 is based on assessments from clinical examination, structural imaging, and both resting-state and task-based assessment of responsiveness using functional imaging and neurophysiology. In contrast to tier 1, this allows for identification of dissociated states between behavior and cognitive abilities using an easy-to-use scheme, the Arousal, Volition, Cognition, Mechanisms (AVCM) score (Table 1).
In the AVCM score, “arousal” is given a value from 1 (nonrousable) to 5 (sustained spontaneous arousal); “volitional motor output,” a value from 1 (none) to 4 (complex); and “cognitive content,” a value from 1 (none) to 5 (complex); whereas “mechanistic basis” is optional and denotes major disease mechanisms. Of note, although “arousal” and “volitional motor output” are clinically observable, “cognitive content” may also be identified by using functional measures, including fMRI or EEG; thus, this item of the AVCM score allows for identification of states such as higher-order cortex motor dissociation and CMD.
Regarding “mechanistic basis,” characterization of the type and extent of injury shows a clinically plausible hierarchy, seeking to identify the likely structural/functional cause of disorders of consciousness (i.e., massive parenchymal injury is greater than structural disconnection, which is greater than functional disconnection, which is greater than neuromodulatory deficits) while also making allowance for extracranial causes that can be suspected or confirmed (e.g., metabolic coma or drugs). Because the clinical picture in a given patient may be due to a combination of structural damage, white matter disconnection, and functional disconnection due to neuromodulatory deficits, the initial assessment of the dominant (or the dominant treatable) cause of the clinical picture may depend on clinical judgment, which is proven or refuted by additional investigations (and response to therapy). Data collection by using these tools is accessible in many centers, and new emerging analytic approaches may offer additional insights. Examples include using efficient analytical approaches, such as machine learning, to identify task responsiveness [51] or characterizing structural (tractography) [52] and functional (resting-state fMRI) connectivity between brainstem arousal centers and cortical structures.
The AVCM score could provide a stand-alone option for assessment of coma and disorders of consciousness that incorporates covert cognition and accounts for CMD (see Table 1 for clinical examples). However, it also provides a foundation for tier 2 of the tiered approach described in this article. With additional experience with neuroimaging and EEG, parts of the AVCM score can be parsed out to the three axes of tier 2. The clinical phenotype (on the x-axis) would scale with the arousal and volitional motor output subscores and with clinically elicitable parts of the cognitive content subscore. The y-axis, which characterizes brain structure, would subsume parts of the AVCM mechanisms subscore that was based on increasingly sophisticated structural neuroimaging (progressing from computed tomography to conventional and diffusion-weighted magnetic resonance imaging). Those parts of the cognitive content subscore that require access to functional imaging or EEG might be best aligned with the z-axis, which describes brain function.
Tier 3
Similar to tier 2, the assumption in tier 3 is that no matter what the clinical scenario or what the future brings, there will always be a clinical phenotype to observe at the bedside and there will always be some type of brain structural and functional change (Fig. 1). Accordingly, tier 3 is ordered around the same three major axes as tier 2, yet in contrast to tier 2, these axes include an (in-principle) infinite number of dimensions (Fig. 2): clinical phenotype (x-axis), brain structure (y-axis), and brain function (z-axis). The y-axis and z-axis are ordered from the molecular level and microcircuits to large-scale networks, respectively, and from cellular to macrocellular levels. Consciousness is classified on those axes by using as many dimensions and concepts as deemed appropriate (× 1…xn; y1…yn; z1…zn). Still controversial concepts, such as the glymphatic system, could be removed if they do not stand the test of time; others could be added in the future as needed. Brain functions and brain structures can be quantified on each of those dimensions as being normal, compromised, or absent. Given the theoretically endless number of features, this seems to be the least common denominator; however, it does not exclude the possibility of introducing more granular distinctions for certain features. Unactionable conditions, such as age, sex, previous brain health, endogenic brain reserve, and genotypes, are acknowledged (indicated by reversed arrowheads in the figures). Clinical trajectories are denoted by arrows: green indicating improvement and red indicating worsening. Consequently, brain states can be visualized in space, reflecting dynamic changes over time (T1, T2). The therapeutic implication is that patients need to be pushed as far into the green areas as possible along all three axes (Tpotential). The result is the identification of consciousness endotypes (as opposed to phenotypes; Fig. 3).
Close-up of tier 3 showing (some of an in-principle infinite number of) structural and functional features that allow comprehensive coverage of consciousness endotypes. These features can be scored as normal, compromised, and absent and intact, compromised, and lost, respectively. Unactionable features, such as age or previous brain health, are indicated by reversed arrowheads. Time points 1 and 2 (T1 and T2) denote consciousness endotypes at different time points, and Tpotential shows potential for consciousness recovery and therapeutic interventions. Clinical trajectories are indicated by arrows: green for improvement and red for worsening. CSF cerebrospinal fluid
Discussion
This position paper introduces ACCESS, a precision medicine framework that captures salient elements and presentations of consciousness disorders, taking into account brain injury trajectories, while at the same time being applicable in both high-resource and low-resource settings and allowing for flexible addition of future knowledge as scientific progress is being made. ACCESS is based on a three-tiered approach with evolving concepts of increasing clinical and scientific complexity. Tier 1 reflects a level of proficiency that seems achievable in many (but probably not all) low-resource settings; tier 2 is based on current state-of-the-art, allowing for detection of preserved consciousness that escapes clinical examination (i.e., CMD); and tier 3 is conceptualized as a quasi-complete representation of all aspects of consciousness disorders after brain injury, including dynamic changes over time, outlining potentials for recovery and therapeutic opportunities. The mapping of an extended temporal dimension in this tier establishes the basis for endotype discovery and characterization. Finally, this article introduces the AVCM score, a convenient scale to summarize clinical phenotypes, brain structure, and brain functions.
To be of enduring use, tiers 2 and 3 are flexible so that as additional scientific insights emerge, the classification can be enriched in many conceivable ways: for instance, genetic polymorphisms might identify neurochemical reserve, injury mechanisms, or recovery processes; new imaging or electrophysiological biomarkers might be discovered; extreme disease trajectories might identify endotypic variations or continuing active disease processes (e.g., neuroinflammation, amyloid/tau pathology) amenable to treatment; and molecular imaging might characterize individual ascending neurotransmitter systems (dopaminergic, noradrenergic, serotoninergic, histaminergic, cholinergic, or glutamatergic), providing a rational basis for selecting specific therapies (e.g., pharmacological stimulant therapies targeting dopaminergic systems).
ACCESS is a framework with several strengths: First, it allows for precise and dynamic mapping of consciousness levels and brain states over time, including, as stated, therapeutic potentials, clinical trajectories, treatment responses, and outcome. It also allows for consideration of the fluctuating nature of consciousness recovery trajectories, including phases of improvement and worsening. Second, it incorporates relevant biological data related to brain function (the “software”) and brain structure (the “hardware”). Third, it can be applied to the entire range of the traditional disorders of consciousness (e.g., coma, VS/UWS) as well as those that require advanced technologies (e.g., CMD). Fourth, it can function as a communication tool to describe consciousness among clinicians and researchers (i.e., by using the AVCM score). Furthermore, the number of dimensions can be adjusted as needed: increased for research purposes and reduced in clinical settings, for instance, when structural, but not functional, neuroimaging is available. Finally, because the model allows for an indefinite number of dimensions, it can be easily updated as knowledge increases over time.
Limitations are related to the fact that the framework may be challenging to put into plain language (in contrast, “coma” is an imprecise but pragmatic term in clinical practice), but it is easy to visualize, and the AVCM score captures complex consciousness configurations using a very simple code consisting of a few letters and numbers. Furthermore, although the framework is feasible for advanced analyses, including machine learning approaches, external validation may be possible for parts of it (e.g., clinical trajectories) but difficult for the entire framework, given that existing labels that would be used to validate the framework are already part of it. This is a circular problem, not uncommon in consciousness research, owing to the absence of a “ground-truth” to define consciousness. Finally, it is important to be aware of a major clinical caveat: Given fluctuations in arousal, any assessment tool may miss episodes of volitional response. Restated, both neurophysiology and fMRI can show false negatives in detecting responses in CMD. Consequently, a negative volitional response, regardless of the means used to achieve it, is still inconclusive.
Next, the proposed framework must (1) be improved by encouraging and collecting feedback from the clinical and scientific communities and (2) be validated, including face and construct validity (albeit this likely will be restricted to specific parts of the framework, as stated earlier). For instance, the AVCM score could be tested for clinical feasibility, for example, how effective it is as a clinical communication tool, and prospectively validated for prognostication, linking AVCM scores in clinical cohorts to specific outcomes.
Conclusions
The ACCESS framework, including the AVCM score, suggests a means to advance the characterization of disorders of consciousness from a clinical phenotypic assessment to the identification of endotypes on the basis of individual clinical trajectories and treatment responses. Although the proposed paradigm is not realistically amenable to validation as a whole, the authors expect that individual components could be the object of exploration and confirmation in prospective large-scale multicenter studies.
References
Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol. 2014;13(8):844–54.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness A practical scale. Lancet. 1974;2(7872):81–4.
Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a new coma scale: the FOUR score. Ann Neurol. 2005;58(4):585–93.
Almojuela A, Hasen M, Zeiler FA. The Full Outline of UnResponsiveness (FOUR) score and its use in outcome prediction: a scoping systematic review of the adult literature. Neurocrit Care. 2019;31(1):162–75.
Bruno M-A, Ledoux D, Lambermont B, Damas F, Schnakers C, Vanhaudenhuyse A, et al. Comparison of the Full Outline of UnResponsiveness and Glasgow Liege Scale/Glasgow Coma Scale in an intensive care unit population. Neurocrit Care. 2011;15(3):447–53.
Giacino JT, Kalmar K, Whyte J. The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. 2004;85(12):2020–9.
Naccache L. Minimally conscious state or cortically mediated state? Brain. 2018;141(4):949–60.
Posner JB, Saper CB, Schiff ND, Plum F. Plum and Posner’s diagnosis of stupor and coma. 4th ed. New York: Oxford University Press; 2007.
Laureys S, Celesia GG, Cohadon F, Lavrijsen J, León-Carrión J, Sannita WG, et al. Task Force on Disorders of Consciousness. Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med. 2010;8:68.
Giacino JT, Ashwal S, Childs N, Cranford R, Jennett B, Katz DI, et al. The minimally conscious state: definition and diagnostic criteria. Neurology. 2002;58(3):349–53.
Bruno M-A, Vanhaudenhuyse A, Thibaut A, Moonen G, Laureys S. From unresponsive wakefulness to minimally conscious PLUS and functional locked-in syndromes: recent advances in our understanding of disorders of consciousness. J Neurol. 2011;258(7):1373–84.
Kondziella D, Friberg CK, Frokjaer VG, Fabricius M, Møller K. Preserved consciousness in vegetative and minimal conscious states: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2016;87(5):485–92.
Edlow BL, Chatelle C, Spencer CA, Chu CJ, Bodien YG, O’Connor KL, et al. Early detection of consciousness in patients with acute severe traumatic brain injury. Brain. 2017;140(9):2399–414.
Fischer DB, Boes AD, Demertzi A, Evrard HC, Laureys S, Edlow BL, et al. A human brain network derived from coma-causing brainstem lesions. Neurology. 2016;87(23):2427–34.
Landsness E, Bruno M-A, Noirhomme Q, Riedner B, Gosseries O, Schnakers C, et al. Electrophysiological correlates of behavioural changes in vigilance in vegetative state and minimally conscious state. Brain. 2011;134(Pt 8):2222–32.
Kondziella D, Fisher PM, Larsen VA, Hauerberg J, Fabricius M, Møller K, et al. Functional MRI for assessment of the default mode network in acute brain injury. Neurocrit Care. 2017;27(3):401–6.
Rosanova M, Gosseries O, Casarotto S, Boly M, Casali AG, Bruno M-A, et al. Recovery of cortical effective connectivity and recovery of consciousness in vegetative patients. Brain. 2012;135(Pt 4):1308–20.
Bodart O, Gosseries O, Wannez S, Thibaut A, Annen J, Boly M, et al. Measures of metabolism and complexity in the brain of patients with disorders of consciousness. NeuroImage Clin. 2017;14:354–62.
Othman MH, Bhattacharya M, Møller K, Kjeldsen S, Grand J, Kjaergaard J, et al. Resting-state NIRS–EEG in unresponsive patients with acute brain injury: a proof-of-concept study. Neurocrit Care. 2021;34(1):31–44.
Vanhaudenhuyse A, Laureys S, Perrin F. Cognitive event-related potentials in comatose and post-comatose states. Neurocrit Care. 2008;8(2):262–70.
Edlow BL, Giacino JT, Hirschberg RE, Gerrard J, Wu O, Hochberg LR. Unexpected recovery of function after severe traumatic brain injury: the limits of early neuroimaging-based outcome prediction. Neurocrit Care. 2013;19(3):364–75.
Schiff ND. Cognitive motor dissociation following severe brain injuries. JAMA Neurol. 2015;72(12):1413–5.
Edlow BL, Claassen J, Schiff ND, Greer DM. Recovery from disorders of consciousness: mechanisms, prognosis and emerging therapies. Nat Rev Neurol. 2021;17(3):135–56.
Faugeras F, Rohaut B, Valente M, Sitt J, Demeret S, Bolgert F, et al. Survival and consciousness recovery are better in the minimally conscious state than in the vegetative state. Brain Inj. 2018;32(1):72–7.
Formisano R, D’Ippolito M, Catani S. Functional locked-in syndrome as recovery phase of vegetative state. Brain Inj. 2013;27(11):1332.
Giacino JT, Whyte J, Bagiella E, Kalmar K, Childs N, Khademi A, et al. Placebo-controlled trial of amantadine for severe traumatic brain injury. N Engl J Med. 2012;366(9):819–26.
Thibaut A, Schiff N, Giacino J, Laureys S, Gosseries O. Therapeutic interventions in patients with prolonged disorders of consciousness. Lancet Neurol. 2019;18(6):600–14.
Giacino JT, Katz DI, Schiff ND, Whyte J, Ashman EJ, Ashwal S, et al. Practice guideline update recommendations summary: disorders of consciousness: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology. 2018;91(10):450–60.
Kondziella D, Bender A, Diserens K, van Erp W, Estraneo A, Formisano R, et al. European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur J Neurol. 2020;27(5):741–56.
Provencio JJ, Hemphill JC, Claassen J, Edlow BL, Helbok R, Vespa PM, et al. The Curing Coma Campaign: framing initial scientific challenges—proceedings of the first Curing Coma Campaign Scientific Advisory Council meeting. Neurocrit Care. 2020;33(1):1–12.
Seel RT, Sherer M, Whyte J, Katz DI, Giacino JT, Rosenbaum AM, et al. American Congress of Rehabilitation Medicine; Brain Injury-Interdisciplinary Special Interest Group; Disorders of Consciousness. Task Force Assessment scales for disorders of consciousness: evidence-based recommendations for clinical practice and research. Arch Phys Med Rehabil. 2010;91(12):1795–813.
Schnakers C, Vanhaudenhuyse A, Giacino J, Ventura M, Boly M, Majerus S, et al. Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC Neurol. 2009;9:35.
Aubinet C, Cassol H, Bodart O, Sanz LRD, Wannez S, Martial C, et al. Simplified Evaluation of CONsciousness Disorders (SECONDs) in individuals with severe brain injury: a validation study. Ann Phys Rehabil Med. 2020. https://doi.org/10.1016/j.rehab.2020.09.001.
Stoll J, Chatelle C, Carter O, Koch C, Laureys S, Einhäuser W. Pupil responses allow communication in locked-in syndrome patients. Curr Biol. 2013;23(15):R647–8.
Vassilieva A, Olsen MH, Peinkhofer C, Knudsen GM, Kondziella D. Automated pupillometry to detect command following in neurological patients: a proof-of-concept study. PeerJ. 2019;7:e6929.
van Ommen HJ, Thibaut A, Vanhaudenhuyse A, Heine L, Charland-Verville V, Wannez S, et al. Resistance to eye opening in patients with disorders of consciousness. J Neurol. 2018;265(6):1376–80.
Hermann B, Salah AB, Perlbarg V, Valente M, Pyatigorskaya N, Habert MO, et al. Habituation of auditory startle reflex is a new sign of minimally conscious state. Brain. 2020;143:2154–72.
Trojano L, Moretta P, Masotta O, Loreto V, Estraneo A. Visual pursuit of one’s own face in disorders of consciousness: a quantitative analysis. Brain Inj. 2018;32(12):1549–55.
Trojano L, Moretta P, Loreto V, Santoro L, Estraneo A. Affective saliency modifies visual tracking behavior in disorders of consciousness: a quantitative analysis. J Neurol. 2013;260(1):306–8.
Pincherle A, Jöhr J, Chatelle C, Pignat J-M, Du Pasquier R, Ryvlin P, et al. Motor behavior unmasks residual cognition in disorders of consciousness. Ann Neurol. 2019;85(3):443–7.
Mélotte E, Maudoux A, Delhalle S, Martial C, Antonopoulos G, Larroque SK, et al. Is oral feeding compatible with an unresponsive wakefulness syndrome? J Neurol. 2018;265(4):954–61.
Wilhelm B, Jordan M, Birbaumer N. Communication in locked-in syndrome: effects of imagery on salivary pH. Neurology. 2006;67(3):534–5.
Arzi A, Rozenkrantz L, Gorodisky L, Rozenkrantz D, Holtzman Y, Ravia A, et al. Olfactory sniffing signals consciousness in unresponsive patients with brain injuries. Nature. 2020;581(7809):428–33.
Raimondo F, Rohaut B, Demertzi A, Valente M, Engemann DA, Salti M, et al. Brain-heart interactions reveal consciousness in noncommunicating patients. Ann Neurol. 2017;82(4):578–91.
Riganello F, Larroque SK, Bahri MA, Heine L, Martial C, Carrière M, et al. A heartbeat away from consciousness: heart rate variability entropy can discriminate disorders of consciousness and is correlated with resting-state fMRI brain connectivity of the central autonomic network. Front Neurol. 2018;9:769.
Blume C, Lechinger J, Santhi N, del Giudice R, Gnjezda M-T, Pichler G, et al. Significance of circadian rhythms in severely brain-injured patients. Neurology. 2017;88(20):1933–41.
Hermann B, Goudard G, Courcoux K, Valente M, Labat S, Despois L, et al. Wisdom of the caregivers: pooling individual subjective reports to diagnose states of consciousness in brain-injured patients, a monocentric prospective study. BMJ Open. 2019;9(2):e026211.
Rass V, Ianosi B-A, Lindner A, Kofler M, Schiefecker AJ, Pfausler B, et al. Hemodynamic response during endotracheal suctioning predicts awakening and functional outcome in subarachnoid hemorrhage patients. Crit Care. 2020;24(1):432.
World Health Organization. Global maps for diagnostic imaging. https://www.who.int/diagnostic_imaging/collaboration/global_collab_maps/en/.
Arnts H, van Erp WS, Sanz LRD, Lavrijsen JCM, Schuurman R, Laureys S, et al. The dilemma of hydrocephalus in prolonged disorders of consciousness. J Neurotrauma. 2020;37(20):2150–6.
Claassen J, Doyle K, Matory A, Couch C, Burger KM, Velazquez A, et al. Detection of brain activation in unresponsive patients with acute brain injury. N Engl J Med. 2019;380(26):2497–505.
Snider SB, Bodien YG, Bianciardi M, Brown EN, Wu O, Edlow BL. Disruption of the ascending arousal network in acute traumatic disorders of consciousness. Neurology. 2019;93(13):e1281–7.
Acknowledgements
This effort was underpinned by the Curing Coma Campaign [30] and draws on important insights provided by the publications “Practice Guideline Update Recommendations Summary: Disorders of Consciousness: Report of…the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research” [28 and “European Academy of Neurology Guideline on the Diagnosis of Coma and Other Disorders of Consciousness” [29]. Contributing collaborators of the Curing Coma Campaign are as follows: Jan Claassen, Brian Edlow, Jed Hartings, Claude Hemphill, Theresa Human, Molly McNett, DaiWai Olson, Adrian Owen, Len Polizzotto, Javier Provencio, Louis Puybasset, Eric Rosenthal, Amy Wagner, John Whyte, and Wendy Ziai. Other campaign participants are listed in Supplementary Table 1. Figures 1, 2 and 3 were created with biorender.com.
Author information
Authors and Affiliations
Consortia
Contributions
All authors have reviewed and approved the text.
Corresponding authors
Ethics declarations
Source of support
Individual authors were supported in these efforts by specific funders, including the James S. McDonnell Foundation (DKM and LN); the Brain, Mind and Consciousness program of the Canadian Institute for Advanced Research (DKM); the Lundbeck Foundation (DK); and Rådet for Offerfonden (DK).
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the collection “Curing Coma Campaign”.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kondziella, D., Menon, D.K., Helbok, R. et al. A Precision Medicine Framework for Classifying Patients with Disorders of Consciousness: Advanced Classification of Consciousness Endotypes (ACCESS). Neurocrit Care 35 (Suppl 1), 27–36 (2021). https://doi.org/10.1007/s12028-021-01246-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01246-9