Abstract
Background
Subclinical seizures are common in critically ill children and are best detected by continuous EEG (cEEG) monitoring. Timely detection of seizures requires pediatric intensive care unit (PICU) physicians to identify patients at risk of seizures and request cEEG monitoring. A recent consensus statement from the American Clinical Neurophysiology Society (ACNS) outlines the indications for cEEG monitoring in critically ill patients. However, adherence to these cEEG monitoring criteria among PICU physicians is unknown. Our project had two goals: 1. To assess adherence to cEEG monitoring indications and barriers toward their implementation; 2. To improve compliance with the ACNS cEEG monitoring criteria in our PICU.
Methods
This is a single-institution study. A total of 234 PICU admissions (183 unique patients) were studied. A 6-month retrospective chart review identified PICU patients meeting ACNS criteria for cEEG monitoring, and patients for whom monitoring was requested. This was followed by an 8-week quality improvement project. During this mentorship period, a didactic 15-min lecture and summary handouts regarding the ACNS indications for cEEG monitoring were provided to all PICU physicians. Requests for cEEG monitoring during the mentorship period were compared to baseline adherence to cEEG monitoring recommendations, and barriers toward timely cEEG monitoring were assessed.
Results
Nearly every fifth PICU patient met cEEG monitoring indications, and prevalences of patients meeting those indications were similar in the retrospective and the prospective mentorship period (18% vs. 19%). Almost all patients (98%) requiring cEEG as per ACNS criteria met the indication for monitoring already at the time of their PICU admission. During the retrospective period, 23% of patients meeting ACNS criteria had a request for cEEG monitoring, which increased to 83% during the mentorship period. The median delay to cEEG initiation was 16.7 h during the mentorship period, largely due to limited hours of EEG technician availability. Electrographic seizures were identified in 36% of patients monitored, all within the first 120 min of cEEG recording. The majority (79%) of cEEGs informed clinical management.
Conclusions
A brief teaching intervention supplemented by pictographic handouts significantly increased adherence to cEEG monitoring recommendations, and cEEGs guided clinical management. However, there were long delays to cEEG initiation. In order to promptly recognize subclinical seizures in critically ill children, we strongly advocate for a routine screening for cEEG monitoring indications as part of the PICU admission process, and a care model allowing for cEEG initiation around-the-clock.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients in the pediatric intensive care unit (PICU) are at risk for central nervous system (CNS) insults, including seizures [1, 2]. Seizures have been reported in 7–46% of comatose PICU patients [3,4,5,6,7,8,9,10], with 39–75% being exclusively subclinical [3, 4, 7, 9, 10]. Electrographic seizures impact pediatric patients in a dose–effect fashion, with higher seizure burdens predicting worse outcomes [11]. High seizure burdens, defined as a single seizure lasting at least 30 min or recurrent seizures occurring for at least 50% of the electroencephalogram (EEG) recording, are associated with increased mortality, increased length of stay in the intensive care unit (ICU), and poor neurological outcomes [1, 8, 12,13,14,15]. These findings are persistent even after adjusting for age, neurological diagnosis, illness severity, and EEG background activity [1, 13, 14]. A delayed EEG initiation and time to treatment in status epilepticus have been associated with increased mortality, highlighting the importance of prompt identification and treatment of seizures [16, 17].
The gold standard for detecting subclinical seizures is continuous EEG (cEEG) monitoring [18]. Unlike routine EEG recordings of typically around 30 min duration, cEEG monitoring is prolonged (usually ≥ 24 h) and has a much higher sensitivity for detecting subclinical seizures [19, 20]. However, restricted resources limit the access to cEEG monitoring, including insufficient machine and technologist availability [21].
Timely detection of seizures requires PICU physicians to identify patients at risk of subclinical seizures and request cEEG monitoring. A consensus statement listing indications for cEEG monitoring in critically ill children was published in 2016 by the American Clinical Neurophysiology Society (ACNS) [22]. However, adherence to these cEEG monitoring criteria among PICU physicians is unknown.
We hypothesized that PICU physicians at our center are under-monitoring patients meeting criteria for cEEG monitoring, which may contribute to under-recognition and under-treatment of seizures. Our hypothesis was based on informal observations that only one to two monitoring requests were made by our PICU per month, despite about 40 monthly patient admissions. Given the reported high prevalence of seizures in critically in children, we predicted a gap in detection and treatment of subclinical seizures in our PICU. In order to assess cEEG monitoring rates, characterize resource limitations, and to increase adherence to published cEEG monitoring recommendations, we conducted a quality improvement (QI) project in the PICU of our tertiary care center.
Materials and Methods
Study Design
We conducted a retrospective analysis of all children treated in our PICU during a 6-month period (January–June 2018), using our center’s computerized charting database (Epic, Verona, WI). A QI project was initiated on June 24, 2018, for an 8-week period, including all patients treated by the same service (mentorship period). Patients admitted multiple times during these study periods were regarded as separate cases for the purpose of data analysis. The retrospective chart review was approved by our institution’s research ethics review board, and an ethics waiver was obtained for the prospective study as it was categorized as a quality improvement project.
Patient Data
Clinical and demographic information including age, sex, seizure history, acute brain injury risk, and whether the patient met an indication for cEEG monitoring were collected for all children. The acute brain injury risk was defined in accordance with the ACNS consensus statement as the presence of at least one of the following: head trauma, CNS tumor, subarachnoid or intra-cerebral hemorrhage, ischemic stroke, CNS infection or inflammatory disease, sepsis associated encephalopathy, prolonged cardio-respiratory arrest, a neurosurgical procedure, extra-corporal membrane oxygenation or therapeutic hypothermia [22].
The clinical indications for cEEG monitoring as per ACNS were: (1) persisting altered mental status following a clinical seizure, (2) continuous intravenous antiseizure drug treatment for epilepsy, (3) altered mental status in a patient at risk of acute brain injury, (4) decline in mental status without known brain injury, (5) pharmacological paralysis in a patient with seizure risk, or (6) the presence of movements or autonomic disturbances that may represent seizures [22]. The impact of cEEG monitoring on clinical management was defined as any effect on (1) the use of antiseizure drugs (initiation, dose adjustment or discontinuation based on the results of cEEG monitoring), or (2) demonstrating that a specific event (motor or autonomic disturbance) was not a seizure. The use of cEEG to rule out electrographic seizures as a cause of altered mental status was not included as having an impact on clinical management if it did not affect antiseizure drug use.
Retrospective Chart Review
Patient charts were individually assessed using the electronic medical health record. When screening for an indication for cEEG monitoring, this was limited to notes signed by critical care physicians. If EEG was performed, the EEG report was assessed to determine monitoring duration and findings.
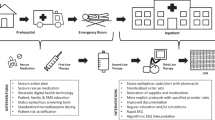
Educational Intervention and cEEG Mentorship
A 15-min didactic lecture was provided to all PICU physicians (residents, fellows, and staff) during the first week of the mentorship period. The lecture included a review of clinical presentation of seizures in PICU patients, prevalence of seizures in critically ill children, and indications for monitoring with cEEG as outlined in the 2016 ACNS consensus statement. As only very limited EEG teaching is included as part of medical school, residency or PICU fellowship, our lecture did not assume any knowledge of the topic. Attendees were asked prior to the teaching session if they were already familiar with the ACNS cEEG recommendations. This training was repeated for all new physicians rotating through the critical care service. Summary handouts of the recommendations (see Fig. 1) were attached to all mobile working stations.
Screening and Monitoring
Members of the circle of care (PICU staff, fellows, and residents) identified patients requiring cEEG monitoring in accordance with ACNS consensus statement recommendations. A medical student (JG) trained in cEEG monitoring recommendations was rounding daily under the supervision of a pediatric neurologist, and independent of the screening performed by PICU physicians, to identify patients requiring cEEG monitoring. The student relied on the discussion during rounds, as well as charted medical history, physical examination, and clinical assessment to determine if a cEEG indication was met. All cases were discussed with the pediatric neurologist to determine eligibility for cEEG monitoring. This assessment was considered the gold standard when determining if a patient met monitoring indications.
At our institution, cEEG monitoring initiation was available between 8 a.m. and 4 p.m. Monday to Friday, and between 10:30 a.m. and 2:15 p.m. on weekends and holidays. There were four cEEG machines available for inpatient or outpatient use, none dedicated to the PICU. The neurologist on call determined the priority in allocating EEG machines when monitoring demands exceeded available resources. Requisitions were made electronically, after authorization by the on-call neurology service, as per our institution’s protocol. If the neurology attending agreed with cEEG monitoring, and EEG technologists and monitors were available, patients received their monitoring as soon as the indication for monitoring was established. Any delay between ordering cEEG and initiation of monitoring was assessed through our electronic medical record system, and reasons for the delay were characterized via inquiry with the EEG technologists. If resources permitted, patients continued to be monitored for at least 24 h or as long as clinically indicated, as per published recommendations [22]. EEGs of less than 1 h in duration were not classified as cEEG monitoring and therefore not included in the study.
Statistical Analysis
Descriptive statistics was used to characterize the adherence to ACNS consensus cEEG monitoring recommendations for both the retrospective and the prospective mentorship period. A comparison of cEEG monitoring rates between the retrospective and mentorship period was made using a χ2 test.
Results
A total of 234 admissions (183 unique patients) were studied across the retrospective period (January 1, 2018 to June 23, 2018) and mentorship period (June 24, 2018 to August 23, 2018). No significant differences in patient characteristics and cEEG monitoring requirements were noted between study periods (Table 1). During the retrospective period, 18% of patients admitted to PICU met cEEG monitoring indications, compared to 19% during the mentorship period.
Throughout the retrospective and mentorship period, all but one patient met the indication for cEEG monitoring at the time of admission (42 of 43 patients, 98%). The majority of patients met monitoring criteria outside of working hours of EEG technologists (Fig. 2).
cEEG Monitoring
None of the PICU physicians, fellows or residents were familiar with the ACNS recommendations for cEEG monitoring prior to the teaching intervention. PICU staff requested monitoring for only seven (23%) out of 31 patients who met the criteria during the retrospective period. In contrast, PICU staff requested monitoring for ten (83%) out of 12 patients who met the criteria during the mentorship period (23% vs. 83%; p < 0.001) (Fig. 3). Among the ten cEEGs requested, two were not performed as the patients no longer met an indication when an EEG machine became available, and one patient received a routine EEG instead of a cEEG due to limited machine availability (Table 2). Throughout both study periods, all but one cEEG monitoring requests by PICU physicians were accepted by neurology (14 of 15 requests, 93%). Neurology did not approve of one cEEG referral as the patient’s clinical status had improved by the time of neurology assessment, the patient no longer meeting indications for monitoring. A higher percentage of patients were monitored during the mentorship period compared to the retrospective period (58% vs. 23%; p < 0.05).
Delays to cEEG Initiation
All seven patients monitored with cEEG during the mentorship period met the indication for monitoring on admission, five out of the seven patients having met the indication outside of institutional hours of operation for cEEG initiation. A workflow limitation delayed the monitoring request for four out of seven patients—PICU physicians were waiting until morning rounds. Once a request for monitoring was made, five out of seven patients received their cEEG within 3 h; however, there was a delay of more than 24 h for two patients due to limited machine availability (Table 3).
Impact on Clinical Management
Throughout the retrospective and mentorship periods, 11 out of 14 cEEGs (79%) affected clinical management. Five cEEGs revealed electrographic seizure activity, all identified within the first 120 min of the recording. The cEEG for one patient on continuous intravenous antiseizure drug therapy did not reveal ictal activity, which prompted medication weaning. Antiseizure drugs were stopped in two patients with presumed clinical seizures after cEEG ruled out epileptiform activity during their motor paroxysms. In three patients, cEEG assisted in ruling out seizures as an etiology of motor/autonomic spells (Table 4). In three instances where cEEG did not directly affect clinical management, cEEG ruled out subclinical seizures in patients with acute brain injury risk presenting with altered mental status.
Discussion
Adherence to Monitoring Criteria
We identified overt under-monitoring of PICU patients at risk for subclinical seizures: At baseline, only 23% of PICU patients meeting cEEG monitoring criteria were monitored. This is similar to a prospective study in an adult ICU patient cohort, where only 37% of patients meeting indications for routine EEG assessment received EEGs [23]. Hence, adherence to both cEEG and routine EEG monitoring recommendations among ICU physicians appears to be low, which may contribute to under-treatment of subclinical seizures and worse outcomes for critically ill patients.
Approximately one in five children in our PICU met an indication for cEEG monitoring. To our knowledge, there are no other studies evaluating the incidence of PICU patients meeting ACNS criteria for cEEG monitoring. In view of the consistency of the rate of patients meeting criteria between our two study periods, we believe that we can generalize this finding, stating that about 20% of PICU patients will require cEEG monitoring. At our center, this would translate into at least one cEEG being performed at any given point in time. If this assumption is correct, PICUs may have to be equipped with dedicated EEG monitoring devices to avoid under-monitoring and delays in seizure treatment.
Notably, none of the PICU physicians, fellows or residents were aware of the cEEG monitoring recommendations prior to teaching interventions. Our teaching was highly effective in increasing the adherence to cEEG monitoring recommendations. During the mentorship period, 83% of patients meeting ACNS indications for cEEG monitoring were appropriately identified by PICU physicians, as opposed to only 23% at baseline. As ICU physicians are responsible for screening patients at risk for seizures, it should be incumbent on these providers to be aware of current EEG monitoring recommendations. Furthermore, we have noticed that non-physician members of the care team would often refer to the pictographic summary of cEEG recommendations during patient rounds to discuss the use of cEEG monitoring. We therefore strongly advocate that all PICU care providers, including nurses, receive teaching on cEEG monitoring recommendations.
Limited resources contributed to lower cEEG monitoring. Notably, two patients appropriately identified as requiring monitoring no longer met an indication for monitoring when an EEG machine became available (see Table 2). Additionally, one patient only received a routine EEG instead of cEEG due to limited machine availability. This is in keeping with a recent survey of 146 pediatric neurologists who are members of the Child Neurology Society, with 34% of respondents reporting barriers to performing cEEG monitoring. The three most common barriers included inadequate availability of EEG technicians, EEG machines, and EEG readers [24]. Although resource limitations interfered with timely monitoring at our center, we were able to nearly triple monitoring rates despite unchanged resources. Thus, increasing adherence to cEEG monitoring criteria may be an effective tool to significantly improve recognition of subclinical seizures in the PICU, even if inadequate resources may still interfere with achieving timely cEEG monitoring.
cEEG Monitoring
For the vast majority (98%) of our patients requiring cEEG monitoring, indications were already met at the time of their PICU admission. We therefore strongly advocate for a routine screening for an indication for cEEG monitoring as part of the admission process of critically ill children. cEEG monitoring criteria should be included in the PICU admission checklist, similar to other routine investigations such as chest X-ray and ECG.
Thirty-six percent of our EEG-monitored PICU patients had electrographic seizures (five out of 14 patients monitored). We are not aware of other studies describing the seizure detection rate among children meeting the new ACNS monitoring criteria. In view of the fact that more than one out of three patients meeting ACNS criteria had subclinical seizures, the recommendations appear to adequately identify PICU patients at very high risk of seizures. However, for assessing the sensitivity of the recommendations, and the true incidence of subclinical seizures among PICU patients, systematic cEEG screening of all patients would be required in future resource-intense studies.
Of note, all seizures were detected within the first 120 min of cEEG recording, and three of the five seizures even within the first 30 min of EEG recording (60%). Although limited by a small sample size, this is consistent with studies demonstrating that traditional 30–60 min EEG recordings identify nonconvulsive seizures in 52–74% of patients in whom seizures are eventually recorded [9, 19, 25]. In accordance with our study, it has been reported that in patients without epileptiform activity during the first 4 h of monitoring, no seizures were subsequently detected in a study of 242 adult patients undergoing cEEG monitoring [25]. These findings suggest that the first 4 h of cEEG monitoring are critical in determining which patients may require prolonged monitoring, which may assist in managing EEG machine use in resource-restricted centers.
We were able to demonstrate that 79% of cEEGs informed clinical management, whether through direct effect on pharmacotherapy or in determining the etiology of motor/autonomic paroxysms. These findings are consistent with a prospective study of 100 children undergoing cEEG monitoring, where 57% of cEEGs affected clinical management [26]. Thus, cEEG is a highly effective tool in guiding treatment when performed in the pediatric critical care setting, especially in informing pharmacotherapy.
Barriers
Our institutional limitation of cEEG initiation between 8 a.m. and 4 p.m. has contributed to significant delays in cEEG monitoring for our PICU patients. Unsurprisingly, 69% of patients throughout both study periods met an indication for monitoring after hours. In a 2011 survey of 58 North American PICUs, 21% of centers noted that technologists were not always available, and 51% of centers reported that technologists were always available but sometimes only by call-back [21].
The requirement for the neurology in-patient service to approve cEEG monitoring requests at our center also contributed to a delay in monitoring in the form of a workflow limitation. Based on our observations, PICU physicians typically awaited patient rounding in the morning to make the requisition with neurology instead of requesting a cEEG as soon as the monitoring indication was established. The median delay before PICU physicians placed a cEEG request was 14 h. As 14 out of 15 monitoring requests (93%) throughout both study periods were accepted by neurology, we advocate for enabling trained PICU physicians to order cEEG monitoring without prior approval by neurologists, with the goal of minimizing monitoring delays. PICU physicians should ideally request monitoring as soon as an indication for monitoring is established.
We believe the gold standard for cEEG monitoring is a care model allowing for cEEG initiation and interpretation around-the-clock. In order to initiate cEEG recordings after hours, some centers train nurses to apply electrode templates or EEG caps [27]. The general trend to increase cEEG monitoring may burden EEG readers. In most centers, EEG readers are facing competing in- and outpatient demands potentially interfering with a timely interpretation of cEEG recordings.
Quantitative EEG allows for interpretation of large volumes of EEG data produced by cEEG through software tools [28]. Although quantitative EEG analysis allows for rapid bedside EEG activity interpretation by PICU staff, the sensitivity and specificity for detection of seizures is poor when compared to the interpretation of raw cEEG recordings [28,29,30,31,32,33]. In order to address the larger burden of EEGs requiring interpretation by regular EEG readers, cEEG screening of raw EEG recordings for seizure detection might be a clinically relevant skill for bedside staff, including PICU attendings, fellows, residents, and nursing staff. The combination between quantitative and raw EEG analysis in a multifaceted screening process may increase efficiency and facilitate treatment decisions by PICU physicians. Whether non-expert EEG readers can be trained in basic bedside EEG interpretation requires further investigation.
There are limited studies in children on the delay of treatment of subclinical seizures and its effect on patient outcomes. Many studies have established an association of higher seizure burdens with higher mortality and worse neurological outcome in children, after adjustment for illness severity and diagnosis [1, 14, 15, 34]. Notably, in a retrospective study of 237 children with status epilepticus, seizure duration of 210 min as compared to 30 min was associated with worse outcome defined as mortality, development of new neurological deficits or development of epilepsy [34]. Treatment delay of more than 10 min in convulsive status epilepticus was associated with increased mortality, as reported in a study of 218 children with refractory status epilepticus [16]. Time to EEG has been independently associated with increased mortality in critically ill children [17]. These and other similar findings are reflected in the most recent Neurocritical Care Society guideline that cEEG should be used to identify nonconvulsive status epilepticus in comatose patients, and that treatment should be initiated rapidly until both clinical and electrographic seizures cease [35].
Limitations
This is a single center study limited by a modest sample size of 176 patients. As cEEG initiation protocols and access to resources may differ at other pediatric centers, the external validity of our findings may be limited. Our experiences with cEEG monitoring may not be applicable to larger centers with additional resources. Although cEEG requests increased following teaching interventions, we did not assess the long-term retention of good monitoring practices learnt from mentorship.
Conclusion
Our study demonstrated overt under-monitoring of patients at risk of subclinical seizures, which significantly improved through teaching interventions. In order to promptly recognize subclinical seizures in the PICU, a care model which allows for cEEG initiation outside of regular hours should be considered. Future studies may evaluate cEEG initiation by PICU nurses and bedside interpretation by non-neurologists, allowing for prompt recognition and treatment of seizures, thereby improving patient outcomes.
References
Abend NS, Arndt DH, Carpenter JL, Chapman KE, Cornett KM, Gallentine WB, et al. Electrographic seizures in pediatric ICU patients: cohort study of risk factors and mortality. Neurology. 2013;81:383–91.
Fink EL, Kochanek PM, Tasker RC, Beca J, Bell MJ, Clark RSB, et al. International survey of critically ill children with acute neurologic insults: the prevalence of acute critical neurological disease in children: a global epidemiological assessment study. Pediatr Crit Care Med. 2017;18:330–42.
Williams K, Jarrar R, Buchhalter J. Continuous video-EEG monitoring in pediatric intensive care units. Epilepsia. 2011;52:1130–6.
Jette N, Claassen J, Emerson RG, Hirsch LJ. Frequency and predictors of nonconvulsive seizures during continuous electroencephalographic monitoring in critically ill children. Arch Neurol. 2006;63:1750–5.
Hosain SA, Solomon GE, Kobylarz EJ. Electroencephalographic patterns in unresponsive pediatric patients. Pediatr Neurol. 2005;32:162–5.
Shahwan A, Bailey C, Shekerdemian L, Harvey AS. The prevalence of seizures in comatose children in the pediatric intensive care unit: a prospective video-EEG study. Epilepsia. 2010;51:1198–204.
McCoy B, Sharma R, Ochi A, Go C, Otsubo H, Hutchison JS, et al. Predictors of nonconvulsive seizures among critically ill children. Epilepsia. 2011;52:1973–8.
Kirkham FJ, Wade AM, McElduff F, Boyd SG, Tasker RC, Edwards M, et al. Seizures in 204 comatose children: incidence and outcome. Intensive Care Med. 2012;38:853–62.
Abend NS, Gutierrez-Colina AM, Topjian AA, Zhao H, Guo R, Donnelly M, et al. Nonconvulsive seizures are common in critically ill children. Neurology. 2011;76:1071–7.
Schreiber JM, Zelleke T, Gaillard WD, Kaulas H, Dean N, Carpenter JL. Continuous video EEG for patients with acute encephalopathy in a pediatric intensive care unit. Neurocrit Care. 2012;17:31–8.
Lalgudi Ganesan S, Hahn CD. Electrographic seizure burden and outcomes following pediatric status epilepticus. Epilepsy Behav. 2019;101:106409. https://doi.org/10.1016/j.yebeh.2019.07.010.
Gwer S, Idro R, Fegan G, Chengo E, Garrashi H, White S, et al. Continuous EEG monitoring in Kenyan children with non-traumatic coma. Arch Dis Child. 2012;97:343–9.
Topjian AA, Gutierrez-Colina AM, Sanchez SM, Berg RA, Friess SH, Dlugos DJ, et al. Electrographic status epilepticus is associated with mortality and worse short-term outcome in critically III children. Crit Care Med. 2013;41:215–23.
Payne ET, Zhao XY, Frndova H, McBain K, Sharma R, Hutchison JS, et al. Seizure burden is independently associated with short term outcome in critically ill children. Brain. 2014;137:1429–38.
Abend NS, Wagenman KL, Blake TP, Schultheis MT, Radcliffe J, Berg RA, et al. Electrographic status epilepticus and neurobehavioral outcomes in critically ill children. Epilepsy Behav. 2015;49:238–44. https://doi.org/10.1016/j.yebeh.2015.03.013.
Gaínza-Lein M, Fernández IS, Jackson M, Abend NS, Arya R, Nicholas Brenton J, et al. Association of time to treatment with short-term outcomes for pediatric patients with refractory convulsive status epilepticus. JAMA Neurol. 2018;75:410–8.
Sánchez Fernández I, Sansevere AJ, Guerriero RM, Buraniqi E, Pearl PL, Tasker RC, et al. Time to electroencephalography is independently associated with outcome in critically ill neonates and children. Epilepsia. 2017;58:420–8.
Wilson CA. Continuous electroencephalogram detection of non-convulsive seizures in the pediatric intensive care unit: review of the utility and impact on management and outcomes. Transl Pediatr. 2015;4:283–9.
Claassen J, Mayer SA, Kowalski RG, Emerson RG, Hirsch LJ. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology. 2004;62:1743–8.
Fogang Y, Legros B, Depondt C, Mavroudakis N, Gaspard N. Yield of repeated intermittent EEG for seizure detection in critically ill adults. Neurophysiol Clin. 2017;47:5–12. https://doi.org/10.1016/j.neucli.2016.09.001.
Sanchez SM, Carpenter J, Chapman KE, Dlugos DJ, Gallentine WB, Giza CC, et al. Pediatric ICU EEG monitoring: current resources and practice in the United States and Canada. J Clin Neurophysiol. 2013;30:156–60.
Herman ST, Abend NS, Bleck TP, Chapman KE, Drislane FW, Emerson RG, et al. Consensus statement on continuous EEG in critically Ill adults and children, part I: indications. J Clin Neurophysiol. 2015;32:87–95.
Park A, Chapman M, McCredie VA, Debicki D, Gofton T, Norton L, et al. EEG utilization in Canadian intensive care units: a multicentre prospective observational study. Seizure. 2016;43:42–7. https://doi.org/10.1016/j.seizure.2016.10.021.
Yuliati A, Weber ARB. Use of continuous EEG monitoring in children presenting with encephalopathy following convulsive status epilepticus. J Clin Neurophysiol. 2019;36:181–5.
Shafi MM, Westover MB, Cole AJ, Kilbride RD, Hoch DB, Cash SS. Absence of early epileptiform abnormalities predicts lack of seizures on continuous EEG. Neurology. 2012;79:1796–801.
Abend NS, Topjian AA, Gutierrez-Colina AM, Donnelly M, Clancy RR, Dlugos DJ. Impact of continuous EEG monitoring on clinical management in critically ill children. Neurocrit Care. 2011;15:70–5.
Kolls BJ, Lai AH, Srinivas AA, Reid RR. Integration of EEG lead placement templates into traditional technologist-based staffing models reduces costs in continuous video-EEG monitoring service. J Clin Neurophysiol. 2014;31:187–93.
Swisher CB, White CR, Mace BE, Dombrowski KE, Husain AM, Kolls BJ, et al. Diagnostic accuracy of electrographic seizure detection by neurophysiologists and non-neurophysiologists in the adult ICU using a panel of quantitative EEG trends. J Clin Neurophysiol. 2015;32:324–30.
Pensirikul AD, Beslow LA, Kessler SK, Sanchez SM, Topjian AA, Dlugos DJ, et al. Density spectral array for seizure identification in critically ill children. J Clin Neurophysiol. 2013;30:371–5.
Stewart CP, Otsubo H, Ochi A, Sharma R, Hutchison JS, Hahn CD. Seizure identification in the ICU using quantitative EEG displays. Neurology. 2010;75:1501–8.
Topjian AA, Fry M, Jawad AF, Herman ST, Nadkarni VM, Ichord R, et al. Detection of electrographic seizures by critical care providers using color density spectral array after cardiac arrest is feasible. Pediatr Crit Care Med. 2015;16:461–7.
Du Pont-Thibodeau G, Sanchez SM, Jawad AF, Nadkarni VM, Berg RA, Abend NS, et al. Seizure detection by critical care providers using amplitude-integrated electroencephalography and color density spectral array in pediatric cardiac arrest patients. Pediatr Crit Care Med. 2017;18:363–9.
Lalgudi Ganesan S, Stewart CP, Atenafu EG, Sharma R, Guerguerian AM, Hutchison JS, et al. Seizure identification by critical care providers using quantitative electroencephalography. Crit Care Med. 2018;46:e1105–11.
Lambrechtsen FACP, Buchhalter JR. Aborted and refractory status epilepticus in children: a comparative analysis. Epilepsia. 2008;49:615–25.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23.
Acknowledgments
We thank Sara Victoria Ieradi for providing research administrative support for our study.
Funding
This study is not sponsored or funded.
Author information
Authors and Affiliations
Contributions
JG contributed to data acquisition, analysis, and interpretation. RJW and DP contributed to data interpretation. All authors contributed to the conception, drafting, critical revision and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interest to disclose.
Ethical Approval
The study complies with all applicable ethical guidelines. The retrospective chart review was approved by our institution’s research ethics review board, and an ethics waiver was obtained for the prospective study as it was categorized as a quality improvement project. The study complies with the SQUIRE checklist for quality improvement studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghossein, J., Alnaji, F., Webster, R.J. et al. Continuous EEG in a Pediatric Intensive Care Unit: Adherence to Monitoring Criteria and Barriers to Adequate Implementation. Neurocrit Care 34, 519–528 (2021). https://doi.org/10.1007/s12028-020-01053-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01053-8