Abstract
Background
Vasopressin is one of the vasopressors used to augment blood pressure in subarachnoid hemorrhage (SAH) patients with clinically significant vasospasm. The purpose of the present study was to determine whether the administration of vasopressin to a population of SAH patients was an independent predictor of developing hyponatremia.
Methods
A retrospective review on the health records of 106 patients admitted to the University of Alberta Hospital Neurosciences ICU, Edmonton AB, Canada, with SAH from June 2013 to December 2015 was conducted. Serum sodium changes in patients receiving vasoactive drugs were compared. In addition, independent predictors for hyponatremia (Na < 135 mmol/L) were determined using a multivariate logistic regression model.
Results
Patients treated with vasopressin in addition to other vasoactive drugs had significantly higher sodium changes compared to those treated with other vasoactive drugs (−4.7 ± 6 vs −0.1 ± 2.4 mmol/L, respectively, p value 0.001). Hyponatremia occurred in 14 patients (70 %) treated with vasopressin, 10 patients (44 %) treated with vasoactive drugs other than vasopressin (p value 0.081), and 24 patients (38 %) who did not receive any vasoactive drug (p value 0.013). In multivariate logistic regression analysis, when adjusting for disease severity, age, sex, aneurysm location, and treatment, vasopressin was associated with hyponatremia (OR 3.58, 95 % CI, 1.02–12.5, p value 0.046).
Conclusions
The results of the present study suggest that hyponatremia may be more common in SAH patients treated with exogenous vasopressin compared to those who did not receive it. Serum sodium should be monitored closely when vasopressin is being used in the SAH population. Further studies are needed to confirm the effect of exogenous vasopressin on serum sodium levels in SAH populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH) is a neurological emergency characterized by the extravasation of blood into the subarachnoid space. Although SAH accounts for 5 % of all strokes, given the relatively younger age at onset, it has a significant burden on productive life years. The average mortality rate for SAH has been reported to range from 30 to 50 %, with a significant proportion of survivors left with disability. Neurological and medical complications are common after SAH and contribute significantly to the overall prognosis. These include seizures (1–20 %), re-bleeding (5–10 % over the first 72 h), hydrocephalus (~20 %), cerebral vasospasm (~50 %), delayed cerebral ischemia (DCI) (~30 %), and hyponatremia (10–50 %) [1–3].
Cerebral vasospasm and DCI are significant contributors to disability for SAH patients who survive the initial bleed. Once symptomatic vasospasm and/or DCI are evident, induced hypertension using vasopressors, in addition to maintaining euvolemia, is indicated to increase cerebral perfusion [1]. In addition to their use in DCI, vasopressors are also used to augment blood pressure in hemodynamically unstable patients. The most commonly used vasopressors in the neurocritical care are norepinephrine and phenylephrine. In addition, vasopressin might be used if other agents are not effective or not tolerated [4].
Vasopressin, also known as antidiuretic hormone, is a hormone secreted endogenously from the neurohypophysis then released by the posterior pituitary gland in response to hyperosmolality and hypovolemia. It causes vasoconstriction by acting on V1 receptors and water retention by acting on V2 receptors with subsequent free water reabsorption at the renal collecting ducts [5]. Despite acting on V2 receptors with potential to cause water intoxication and subsequent hyponatremia, exogenous vasopressin has rarely been associated with hyponatremia in septic shock patients [6]. Only a few cases of exogenous vasopressin-induced hyponatremia have been reported [7]. Those cases received vasopressin infusion for septic shock. Serum sodium declined rapidly 16–24 h following the start of vasopressin with abrupt increase following vasopressin discontinuation [7]. Conversely, SAH patients being treated with vasopressin may often develop hyponatremia. Hyponatremia is the most common electrolyte complication after SAH. Hyponatremia has been reported to be associated with longer hospital stay and increased morbidity, risk of vasospasm, and cerebral infarction [8, 9]. However, it is not known whether vasopressin administration may independently increase the risk of hyponatremia in SAH patients.
The purpose of the present retrospective study was to determine whether the administration of vasopressin to a population of SAH patients was an independent predictor of developing hyponatremia.
Methods
We conducted a retrospective chart review of 106 patients admitted to the University of Alberta Hospital Neurosciences ICU, Edmonton, Alberta, Canada, with aneurysmal SAH from June 2013 to December 2015. Patients were over 17 years of age, had aneurysmal SAH, and their ruptured aneurysm treated with either endovascular coiling or surgical clipping. The study has been approved by the Health Research Ethics Board (HREB) of the University of Alberta. Data were abstracted from both an ICU electronic medical record and paper records and managed using REDCap electronic data capture tools hosted at University of Alberta [10, 11].
Baseline patient characteristics were recorded. This included patient demographics (age, sex, height, and weight), past medical and social history, Glasgow Coma Scale (GCS) on admission, World Federation of Neurological Surgeons Grading System for Subarachnoid Hemorrhage (WFNS) grade, Acute Physiology and Chronic Health Evaluation (APACHE II) score, admission serum sodium and creatinine, aneurysm location, and aneurysm treatment. APACHE II physiological subscore was calculated by subtracting the patient’s age and GCS score from APACHE II score. Duration of the ICU and hospital stay, disposition (home, transfer to another facility, death), seizures, aneurysm re-rupture, mechanical ventilation, and angiographic vasospasm were recorded.
Information on intravenous vasoactive drug use during the ICU stay was recorded. This included vasopressin, epinephrine, norepinephrine, phenylephrine, dopamine, and milrinone. In addition, the use of mannitol, hypertonic saline (3 % saline), 0.45 % saline, normal saline, PlasmaLyte, and 5 % dextrose were also recorded. Those who received vasopressin infusion at any point during their ICU stay with or without other vasoactive agents were allocated to the “Vasopressin” group. Patients who received vasoactive agents other than vasopressin were allocated to “Other Pressors” group. Those who did not receive any vasoactive agent during their ICU stay were allocated to the “No Pressors” group.
Serum sodium was recorded as a time-dependent variable for up to 21 days during the ICU stay. Occurrence of hyponatremia was recorded. Hyponatremia was defined as serum sodium level of <135 mmol/L, similar to what has been reported previously [2, 8]. For patients treated with vasoactive drugs, serum sodium at baseline before the start of the vasoactive drug infusion (Nabaseline), the lowest serum sodium measurement during the infusion (Namin), and serum sodium 24 h following the end of the infusion (Na24hpost) were compared. The change in sodium was calculated as the difference between Nabaseline and Namin.
Statistical Analysis
Continuous variables are presented as mean ± standard deviation. Categorical variables are presented as frequencies and percentages, n (%). Fisher’s exact test or chi-square tests were used to compare categorical variables. Continuous variables were compared using Student’s t test. Sodium changes during vasoactive drug infusions were compared using repeated measures ANOVA followed by Tukey’s multiple comparisons test. Paired t test was used to compare Nabaseline and Namin. Adjusted odds ratios (OR) were determined using multivariate logistic regression analysis. The fit of the final model was confirmed using Hosmer–Lemeshow goodness-of-fit test. Pearson correlation coefficient and linear regression were used to determine the correlation between the duration of vasoactive drugs infusion and the change of sodium and duration of hypertonic saline infusion. Level of significance was set at p < 0.05. Statistical analysis was done using STATA version 14 (STATA Corp, College Station, Texas). Figures were plotted using GraphPad Prism version 7 (GraphPad Software, La Jolla, CA).
Results
Table 1 depicts the characteristics of patients included in the current study. Compared to the No Pressors group, patients treated with vasoactive drugs were sicker as manifested by higher WFNS grade, higher APACHE II score, and lower GCS on admission (Table 1). A total of 43 patients received vasoactive drugs, of which 20 patients received vasopressin (1 received vasopressin alone and 19 received vasopressin in addition to other vasoactive agents) and 23 received vasoactive drugs other than vasopressin. Detailed vasopressor/hypertonic saline infusions were not available in 2 patients (1 from each group). Therefore, data presented in Table 2 are based on 19 patients in the Vasopressin and 22 patients in the Other Pressors groups. As depicted in Table 2, most of the patients were treated with norepinephrine. There were more patients treated with phenylephrine in the Vasopressin group compared to the Other Pressors group (63 vs 23 %, respectively, p value 0.009). With regard to intravenous fluids, all patients in the Vasopressin group (100 %) had normal saline running at an average rate of 94 ± 34 ml/h with the rate adjusted to maintain euvolemia. On the other hand, 20 patients (91 %) in the Other Pressors group had normal saline running at an average rate of 94 ± 30 ml/h (p value 0.985) and 2 patients (9 %) had PlasmaLyte running at 75 ml/h. In addition, 0.45 % saline was running briefly in 2 patients in the Vasopressin group and discontinued 4–9 h from the start of vasopressin infusion.
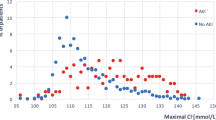
Patients treated with vasopressin had a significantly higher change in sodium compared to those in the Other Pressors group (−4.7 ± 6 vs −0.1 ± 2.4 mmol/L, respectively, p value 0.001). As shown in Fig. 1a, b, Nabaseline and Namin in the Vasopressin group were significantly different (143 ± 8 vs 138 ± 10 mmol/L, respectively, p value 0.002). Conversely, this did not reach statistical significance in the Other Pressors group (139 ± 4 vs 139 ± 5 mmol/L, respectively, p value 0.929). Three patients in the Vasopressin group had baseline serum sodium above 150 mmol/L. One of those patients was on mannitol around the clock for more than 24 h. On the other hand, none of the patients in the Other Pressors groups had sodium levels above 150 mmol/L. This explained the higher baseline sodium values in the Vasopressin group. However, when those sodium values were excluded, the effect of vasopressin on serum sodium still existed (Nabaseline 140 ± 6 vs Namin 135 ± 8 mmol/L, respectively, p value 0.005). The average time between Nabaseline and Namin was 28 ± 15 h from the start of vasopressin infusion in the Vasopressin group. Serum sodium returned to baseline 24 h after stopping vasopressin infusion (Fig. 1c). Eight patients (42 %) in the Vasopressin group had serum sodium levels decrease more than 5 mmol/L during vasopressin infusion. Interestingly, 6 of those patients (75 %) had their aneurysm clipped and 6 (75 %) were females as opposed to 4 (36 %) and 4 (36 %) in those whose sodium levels decreased less than 5 mmol/L while on vasopressin. However, the difference did not reach statistical significance (p value 0.096). In addition, a change in sodium levels significantly correlated with vasopressin infusion duration as opposed to norepinephrine infusion (Fig. 2a).
a Baseline serum sodium (Nabaseline) and lowest serum sodium (Namin) in Vasopressin group (n = 19) *p < 0.05 versus Namin; b Baseline serum sodium (Nabaseline) and lowest serum sodium (Namin) in Other Pressors group (n = 22); c Serum sodium in the Vasopressin group before, during and 24 h after infusion (Na24hpost) (n = 14) *p < 0.05 versus Namin and Na24hpost; d Serum sodium in the Other Pressors group before, during and 24 h after infusion, (n = 17). The average time between Nabaseline and Namin was 28 ± 15 h and 65 ± 45 h in the Vasopressin and Other Pressors groups, respectively (p = 0.01)
Hypertonic saline (3 % NaCl) infusion was started in 10 patients in the Vasopressin group versus 7 patients in the Other Pressors group (p value 0.623). There appeared to be a longer duration of 3 % NaCl infusion in the Vasopressin group compared to the Other Pressors group but it did not reach statistical significance (Table 2). In the Vasopressin group, 3 % NaCl was initiated following vasopressin start in 5 patients (50 %) and discontinued with vasopressin discontinuation in 7 patients (70 %). On the other hand, in the Other Pressors group, 3 % NaCl was initiated following the other pressors start in 1 patient (14 %) and discontinued with their discontinuation in 4 patients (57 %). The duration of 3 % NaCl infusion was significantly directly correlated with vasopressin duration of infusion (r = 0.79, p value 0.007) (Fig. 2b), whereas this correlation did not exist for norepinephrine in the Other Pressors group (r = −0.1, p value 0.835). In addition, such correlation did not reach statistical significance when 3 % NaCl was tested in patients treated with phenylephrine or milrinone.
With regard to hyponatremia, there were significantly higher percentage hyponatremia episodes experienced in the Vasopressin group compared to the No Pressors group. Hyponatremia developed in 14 patients (70 %) and 24 patients (38 %) in the Vasopressin and No Pressors groups, respectively (p value 0.013). When compared with patients in the Other Pressors group, a group of patients with similar characteristics to the Vasopressin group, the difference in hyponatremia did not reach statistical significance (Table 3). In multivariate logistic regression analysis (Table 4), when adjusting for disease severity, age, sex, aneurysm location, and treatment, vasopressin use in addition to standard vasoactive therapy was associated with hyponatremia (OR 3.58, 95 % CI, 1.02–12.5, p value 0.046). Age, sex, higher-grade SAH, higher APACHE II physiological subscore were not associated with increased hyponatremia risk. Conversely, patients with aneurysmal SAH secondary to ruptured middle cerebral artery (MCA) aneurysm had significantly lower odds for hyponatremia compared to patients with ruptured anterior communicating artery (ACoA) aneurysms (OR 0.18, 95 %, CI 0.04–0.76, p value 0.019). With regard to aneurysm treatment, surgical clipping was associated with higher risk of hyponatremia compared to endovascular coiling. As shown in Table 3, the Vasopressin group did not differ from the Other Pressors group in terms of hospital course and disposition. Catheter angiogram was recorded in 23 patients who received vasoactive drugs. Hyponatremia was recorded in 9/18 patients (50 %) who had angiographic vasospasm compared to 3/5 (60 %) who had no evidence of vasospasm (p value 1.00). Angiographic vasospasm was confirmed in 11 out of 12 patients (92 %) in the Vasopressin group and 7 out of 11 patients (64 %) in the Other Pressors group (p value 0.155).
Discussion
Hyponatremia is the most common electrolyte complication after SAH. Hyponatremia has been reported to be associated with longer hospital stay and increased morbidity, risk of vasospasm, and cerebral infarction [8, 9]. The results of the present study suggest that hyponatremia may be more common in SAH patients treated with vasopressin compared to those who did not receive vasopressin. The prevalence of hyponatremia in non-vasopressin-treated patients in the present study was within what has been previously reported in the literature (10–50 %) [1, 2]. A recent systematic review of 13 studies has reported a combined prevalence of hyponatremia of 36 %, which is similar to our observation in patients not treated with vasopressors [8]. The effect of vasopressin infusion on serum sodium was manifested by significantly lower Namin in Vasopressin group (Fig. 1a) within approximately 1 day from the start of vasopressin infusion. In addition, a change in sodium was significantly correlated with vasopressin exposure (Fig. 2a), suggesting that longer durations of vasopressin could be associated with more profound sodium changes. When vasopressin infusion was discontinued, serum sodium returned to baseline (Fig. 1c), suggesting a transient effect. However, this provides further evidence for the contribution of exogenous vasopressin on serum sodium changes. The use of 3 % NaCl in 10 and 7 patients in the Vasopressin and Other Pressors groups, respectively, could be attributed to the acuity of the conditions of those patients rather than the use of the vasoactive drugs. However, 3 % NaCl was initiated following vasopressin start and discontinued with its discontinuation in 50 % and 70 % of the patients, respectively. Those patients were started on 3 % NaCl for hyponatremia. This could explain the correlation observed between 3 % NaCl infusion and vasopressin exposure, suggesting possible contribution of vasopressin in hyponatremia requiring treatment.
In our institution, vasopressin is used to induce hypertension in SAH patients who have clinically significant vasospasm/DCI in addition to other pressors. Also, it is used to augment blood pressure in hemodynamically unstable patients. Generally, it is used when other vasopressors are not effective or not tolerated. Vasopressin use in SAH has been reported by Muehlschlegel et al. [4] as an alternative add-on therapy for patients with clinical vasospasm with no adverse effects on cerebral perfusion. The authors have not found a significant difference in the percentage of hyponatremia between patients treated with vasopressin + phenylephrine and historical controls treated with vasoactive drugs other than vasopressin. However, in our study, when we controlled for potential confounding variables we found that vasopressin may be associated with increased risk of hyponatremia. In addition, the fall in serum sodium in vasopressin-treated patients has been reported to be similar between groups. This observed discrepancy could be explained by a few reasons. First, while the standard intravenous (IV) fluid used in all patients in the current study was normal saline with the aim of euvolemia per the current SAH management guidelines [1], the standard IV therapy used by Muehlschlegel et al. was 5 % dextrose - 0.9 % saline in addition to around the clock 5 % albumin with the aim for hypervolemia and hemodilution, reflecting the current practice back then, which could have different effects on serum sodium. Second, the authors included patients with confirmed or potential vasospasm and excluded patients receiving vasopressin for hemodynamic instability. However, in our study we included all SAH patients treated with vasopressin regardless of the indication, which could have contributed to different results. Third, we conducted multivariate logistic regression analysis to control for confounding factors.
Physiologically, through stimulation of V2 receptors, vasopressin results in increased water reabsorption leading to a decrease in urine output and potentially leading to hyponatremia [5]. The prevalence of vasopressin-induced hyponatremia in septic shock patients has been rare [6, 12]. For instance, in the randomized controlled trial by Russell et al. [6] they reported 0.3 % hyponatremia in vasopressin-treated patients. They defined hyponatremia as serum sodium <130 mmol/L, in contrast to our study. The explanation of the rarity of exogenous vasopressin-induced hyponatremia is not well known. It has been attributed to systemic inflammation seen in patients with septic shock. Endotoxin administration in animal models has been found to downregulate V2 receptors [13], which could explain the reduced antidiuretic effect of vasopressin in septic shock. In addition, this could be attributed to endogenous vasopressin level depletion in septic shock patients [14]. With regard to SAH patients, we speculate that the higher prevalence of hyponatremia in vasopressin-treated patients could be explained by two reasons. First, endogenous vasopressin levels could be elevated in SAH [15, 16]. The study by Mather et al. [15] has shown that approximately 25 % of patients with SAH had increased concentrations of endogenous vasopressin. In addition, endogenous vasopressin has been found to be present in the plasma of SAH patients at osmolality levels that normally suppress its release [17]. This could lead to hyponatremia as a result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). It has been reported that SIADH could be responsible for up to 71 % of hyponatremias in SAH patients, with endogenous vasopressin levels increasing before and during the episodes of hyponatremia and declining when hyponatremia is resolved [18]. Administration of exogenous vasopressin might add to the endogenously elevated vasopressin, contributing to more patients with hyponatremia. On the other hand, it has been reported that levels of endogenous vasopressin might not correlate with hyponatremia in some SAH patients [19] as in the case of cerebral salt wasting, which could have different response to exogenous vasopressin. Second, most patients post-SAH who are not in septic shock receive vasopressin as part of hypertensive therapy for symptomatic vasospasm, which might have intact V2 receptors compared to septic shock patients. Further studies might be needed to confirm the above assumptions.
In the present study, SAH secondary to ruptured MCA aneurysms was associated with lower odds of hyponatremia when compared with those resulting from ruptured ACoA aneurysms (Table 4). This observation agrees to what has been reported in a study of 169 SAH patients. They have reported a higher prevalence of hyponatremia in patients with ruptured ACoA aneurysms (51 %) compared to only 18 % in patients with ruptured MCA aneurysms [20]. This has been explained by the fact that ruptured aneurysms in the area of ACoA could alter endogenous vasopressin release [21]. In the study by Mather et al. [15], 70 % of patients who had elevated vasopressin levels had ruptured ACoA aneurysms. Different aneurysm treatment modalities (coiling vs clipping) were found to have different risks of hyponatremia. The reason for this observation is not clear, especially since previous reports have shown no difference [8].
The present study has many limitations. First is the retrospective nature of the study. In this study, we used historic data, which are more prone to bias due to lack of randomization and the presence of inconsistent or missing information. Second, limitation is confounding. We were able to control for several variables such as disease severity, aneurysm location, and treatment; but there could be some other unknown confounding factors that might correlate directly or inversely with serum sodium levels. In addition, we could not capture the hydrocortisol status, presence of SIADH or cerebral salt wasting, incidence, and risks of DCI in the present study, which could be confounders in serum sodium alterations. Third, we did not compare patient outcomes because vasopressin is generally used in sicker patients (confounded by indication) as a second-line agent when other vasoactive agents failed or were not tolerated.
Conclusions
The results of the present study suggest that hyponatremia may be more common in SAH patients treated with exogenous vasopressin compared to those who did not receive it. Serum sodium should be monitored closely when vasopressin is being used in the SAH population. Further studies are needed to confirm the effect of vasopressin on serum sodium levels in SAH populations.
References
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2012;43:1711–37.
Diringer MN, Bleck TP, Claude Hemphill J 3rd, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care. 2011;15:211–40.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–96.
Muehlschlegel S, Dunser MW, Gabrielli A, Wenzel V, Layon AJ. Arginine vasopressin as a supplementary vasopressor in refractory hypertensive, hypervolemic, hemodilutional therapy in subarachnoid hemorrhage. Neurocrit Care. 2007;6:3–10.
Rang HP, Ritter JM, Flower RJ, Henderson G. The pituitary and the adrenal cortex. In: Rang and Dale's pharmacology. 8th ed. Edinburgh; New York: Elsevier/Churchill Livingstone; 2015. p. 402–417.
Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358:877–87.
Salazar M, Hu BB, Vazquez J, Wintz RL, Varon J. Exogenous vasopressin-induced hyponatremia in patients with vasodilatory shock: two case reports and literature review. J Intensive Care Med. 2015;30:253–8.
Mapa B, Taylor BE, Appelboom G, Bruce EM, Claassen J, Connolly ES. Impact of hyponatremia on morbidity, mortality, and complications after aneurysmal subarachnoid hemorrhage: a systematic review. World Neurosurg. 2016;85:305–14.
Wijdicks EFM, Vermeulen M, Hijdra A, Van Gijn J. Hyponatremia and cerebral infarction in patients with ruptured intracranial aneurysms: is fluid restriction harmful? Ann Neurol. 1985;17:137–40.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Obeid JS, McGraw CA, Minor BL, et al. Procurement of shared data instruments for research electronic data capture (REDCap). J Biomed Inform. 2013;46:259–65.
Obritsch MD, Jung R, Fish DN, MacLaren R. Effects of continuous vasopressin infusion in patients with septic shock. Ann Pharmacother. 2004;38:1117–22.
Grinevich V, Knepper MA, Verbalis J, Reyes I, Aguilera G. Acute endotoxemia in rats induces down-regulation of V2 vasopressin receptors and aquaporin-2 content in the kidney medulla. Kidney Int. 2004;65:54–62.
Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D. Circulating vasopressin levels in septic shock. Crit Care Med. 2003;31:1752–8.
Mather HM, Ang V, Jenkins JS. Vasopressin in plasma and CSF of patients with subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1981;44:216–9.
Liu ZW, Gu H, Zhang BF, et al. Rapidly increased vasopressin promotes acute platelet aggregation and early brain injury after experimental subarachnoid hemorrhage in a rat model. Brain Res. 2016;1639:108–19.
Diringer MN, Wu KC, Verbalis JG, Hanley DF. Hypervolemic therapy prevents volume contraction but not hyponatremia following subarachnoid hemorrhage. Ann Neurol. 1992;31:543–50.
Hannon MJ, Behan LA, O’Brien MM, et al. Hyponatremia following mild/moderate subarachnoid hemorrhage is due to SIAD and glucocorticoid deficiency and not cerebral salt wasting. J Clin Endocrinol Metab. 2014;99:291–8.
Wijdicks EF, Vermeulen M, ten Haaf JA, Hijdra A, Bakker WH, van Gijn J. Volume depletion and natriuresis in patients with a ruptured intracranial aneurysm. Ann Neurol. 1985;18:211–6.
Sayama T, Inamura T, Matsushima T, Inoha S, Inoue T, Fukui M. High incidence of hyponatremia in patients with ruptured anterior communicating artery aneurysms. Neurol Res. 2000;22:151–5.
Saramma P, Menon RG, Srivastava A, Sarma PS. Hyponatremia after aneurysmal subarachnoid hemorrhage: implications and outcomes. J Neurosci Rural Pract. 2013;4:24–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Marr, N., Yu, J., Kutsogiannis, D.J. et al. Risk of Hyponatremia in Patients with Aneurysmal Subarachnoid Hemorrhage Treated with Exogenous Vasopressin Infusion. Neurocrit Care 26, 182–190 (2017). https://doi.org/10.1007/s12028-016-0300-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0300-8