Abstract
Background
Physiotherapy is an important part of treatment after severe brain injuries and stroke, but its effect on intracranial and systemic hemodynamics is minimally investigated. Therefore, the aim of this study was to assess the effects of an early bedside cycle exercise on intracranial and systemic hemodynamics in critically ill patients when admitted to a neurointensive care unit (NICU).
Methods
Twenty critically ill patients suffering from brain injuries or stroke were included in this study performed in the NICU at Sahlgrenska University Hospital. One early implemented exercise session was performed using a bedside cycle ergometer for 20 min. Intracranial and hemodynamic variables were measured two times before, three times during, and two times after the bedside cycling exercise. Analyzed variables were intracranial pressure (ICP), cerebral perfusion pressure (CPP), mean arterial blood pressure (MAP), heart rate (HR), peripheral oxygen saturation (SpO2), cardiac output (CO), stroke volume (SV), and stroke volume variation (SVV). The cycling intervention was conducted within 7 ± 5 days after admission to the NICU.
Results
Cycle exercise increased MAP (p = 0.029) and SV (p = 0.003) significantly. After exercise CO, SV, MAP, and CPP decreased significantly, while no changes in HR, SVV, SpO2, or ICP were noted when compared to values obtained during exercise. There were no differences in data obtained before versus after exercise.
Conclusion
Early implemented exercise with a bedside cycle ergometer, for patients with severe brain injuries or stroke when admitted to a NICU, is considered to be a clinically safe procedure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients admitted to intensive care units (ICU) due to critical illness often develop severe muscle wasting and impaired muscle function [1]. This may lead to delayed recovery, an extended ICU stay, increased morbidity, and could negatively affect the patient’s quality of life after hospital discharge [2, 3]. Early mobilization in the ICU has been shown to reduce delirium duration, mechanical ventilation, risk of hospital-acquired infections, length of stay in both the ICU and the hospital, and gives the patient a better functional status at hospital discharge [4–6]. The European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients states that the physiotherapist should be a part of the interdisciplinary team around the critically ill patient and that physiotherapy should start early after ICU admission [7].
Physiotherapy regarding mobilization in the ICU ranges from passive exercises to ambulation in the ward. For the most critically ill nonresponsive patients, the physiotherapy often starts with passive range of motion (ROM) performed manually by a physiotherapist [8]. The duration of passive ROM is often short, and one way to give the patient a longer treatment period is continuous passive motion (CPM). Very early CPM with a bedside cycle ergometer for patients with critical illness in a medical ICU is considered safe and feasible [9].
We have previously shown that shorter periods of passive ROM performed by a physiotherapist are considered safe for patients with severe brain injuries or stroke, treated in the neurointensive care unit (NICU) [10]. However, to our knowledge, a longer period of CPM with a bedside cycle ergometer has not previously been investigated in this patient cohort. Therefore, the primary aim of this study was to investigate if longer exercise periods are safe and feasible with regards to intracranial pressure (ICP) and cerebral perfusion pressure (CPP) after severe brain injuries or stroke. The secondary aim was to evaluate if this exercise has any impact on mean arterial blood pressure (MAP), heart rate (HR), cardiac output (CO), stroke volume (SV), stroke volume variation (SVV), and peripheral oxygen saturation (SpO2) in these patients.
Methods
Study Design and Setting
This study has a prospective design and was conducted in an eight-bed NICU at the Sahlgrenska University Hospital, Gothenburg, Sweden. The protocol followed the Helsinki declaration of human rights and was approved by the Gothenburg Regional Ethical Review Board, Sweden. Informed written consent for study participation was obtained from the patients' next of kin.
Patients
The patients were enrolled from August 2013 to July 2014 and November 2014 to February 2015. Patients with traumatic brain injury (TBI), cerebral infarction, or intracerebral/cerebellar hemorrhage requiring intensive care and in whom ICP was measured were included. Exclusion criteria were <18 years of age, subarachnoid hemorrhage due to the risk of vasospasm, fractures of the spine or lower extremities, severe infections, severe obesity, or non-Swedish-speaking relatives. None of the patients were paralyzed at any time, and the ongoing pharmacological treatment (Table 1) was not changed and no extra medications were given during the experimental procedure. Arterial blood pressure was measured by a radial artery catheter, and ICP was measured by an intraventricular or parenchymal catheter. The intraventricular catheter was closed for measurements during the whole procedure and was not used for drainage.
Interventions
A 20-min leg exercise using a bedside cycle ergometer was performed soon after NICU admission and after approval from the attending neurosurgeon. The bedside cycle used was a MOTOmed letto (RECK, Betzenweiler, Germany), an electric cycle available for both passive and active exercise. During exercise, the patients were in the supine position with the backrest of the bed slightly elevated. The bedside cycle was placed at the foot of the bed and the patients' feet were fixed on the pedals with soft straps. During passive exercise the pedal rate was fixed at 20 revolutions per minute, and in the case of active cycling the gear was set at zero. The patients could also change back and forth between passive and active cycling without any interruptions of the exercise. ICP, CPP (= MAP−ICP), MAP, HR, CO, SV, SVV, and SpO2 were measured twice (at 10 and 5 min) before, three times (at 5, 10, and 20 min) during, and twice (5 and 10 min) after the exercise. ICP, CPP, SpO2, MAP, and HR were monitored and calculated on line using a Philips IntelliVue MX800 monitoring system (Philips Healthcare, DA Best, The Netherlands). For monitoring and calculations of CO, SV, and SVV, a Vigileo Flotrac system (Edwards Lifesciences, CA, USA) was used. These variables were calculated from the arterial pulse contour from a catheter placed in the radial artery. Pre-study defined criteria for discontinuation of the experimental procedure were ICP > 20–25 mmHg, CPP < 60 mmHg, BP > 180 mmHg, HR > 100 or <40 beats per minute, and SpO2 less than 95 %.
Statistical Analyses
All calculations were made with the IBM SPSS Statistics for Windows version 22 (IBM Corp, Armonk, NY, USA). Data are presented as mean ± standard deviation (SD). To evaluate the effects of exercise on intracranial and systemic hemodynamics, a paired sample t-test was used. A p-value of ≤0.05 was considered as statistically significant.
Results
In all, 20 patients consisting of 7 women and 13 men were included in the trial. The clinical trial profile is shown in Fig. 1. Patient characteristics, diagnoses, and ICU treatments are described in Table 1. All patients completed the intervention without any adverse events during this early implemented exercise. The majority of the patients were comatose and/or sedated and thus were unable to actively contribute to the exercise. However, two of the patients did actively pedal for about five out of 20 min. The patients were included in the study 7 ± 5 days after admittance to the NICU.
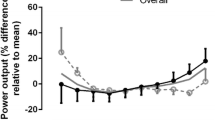
Data on the intracranial and systemic hemodynamics are presented in Table 2. In general, changes in intracranial and systemic hemodynamics during this early bedside cycling exercise were small (3–6 %). A 20-min bedside cycle exercise increased MAP (p = 0.029) and SV (p = 0.003) significantly, and there was a trend for an increase in CO (p = 0.066) and CPP (p = 0.057). After exercise CPP, MAP, CO, and SV decreased significantly versus during exercise. During the experimental procedure, there were no significant changes in ICP, HR, SVV, or SpO2. There were no differences between data obtained before versus after exercise in any of the recorded variables.
Further, we found that the semi-awake patients did not have the capability to cooperate for more than 20 min even though it was passive pedaling as they tried to take their feet off the pedals after 17–20 min of cycling. For one patient, who had high leg muscle tone, it was difficult to place the feet in the pedals; but the increased leg muscle tone vanished after 20 min of exercise. In three patients, the cycle ergometer stopped and the monitor alarmed for detected spasm; this could be overcome by letting the cycle ergometer pedal backwards.
Discussion
In this study, 20 patients that were critically ill due to severe brain injury or stroke underwent 20 min of early exercise with a bedside cycle ergometer without the occurrence of any deleterious circulatory effects or adverse events. The major findings of the present study were that early exercise with a bedside cycle did not affect ICP but caused minor increases in SV and MAP.
A significantly higher MAP during exercise, compared to before or after, was noted in the present study. When using the bedside cycle ergometer in a mixed medical and surgical ICU, Burtin et al. [11] reported that, in general, there were no changes in arterial blood pressure during cycling; but they had to terminate the cycle exercise prematurely in 6 of 425 sessions due to a rise in systolic blood pressure above 180 mmHg [11]. Pires-Neto et al. did not find any clinically relevant hemodynamic changes in a group of deeply sedated patients within the first 72 h of mechanical ventilation [9]. When they studied the cardiorespiratory changes during active cycle exercise in critically ill conscious patients, they found that exercise increased respiratory rate and heart rate but not the arterial blood pressure [12]. The rise in MAP in our study was very small (3 %), not clinically relevant, yet statistically significant showing that there seems to be a relevant physiologic response to longer periods of exercise even when it is at a very low effort level for the patient.
In the present study, there was a nonsignificant increase in CO during exercise, which was caused by an increase in SV as HR was not affected by the exercise. A rise in CO and SV during passive exercise, without a change in HR, was also found by Nóbrega et al. [13] in healthy individuals. This response was in contrast to that seen in healthy individuals performing active cycle exercise, where CO increased due to an increase in HR, not in SV [13]. Thus, the increase in CO during passive cycle exercise is most likely caused by an increased venous return from the legs, thereby enhancing cardiac preload, SV, and CO.
To our knowledge, this is the first study evaluating the effects of passive cycle exercise on systemic and intracranial hemodynamics in patients with severe brain injuries or stroke while admitted to a NICU. There are, however, some previous studies evaluating the effects of shorter periods of passive ROM on intracranial hemodynamics [10, 14, 15]. Thelandersson et al. found that a session of passive ROM caused a decrease in ICP after the intervention with no changes in CPP or BP [10]. Koch et al. studied the effect of short periods (7 min) of passive ROM in a population of spontaneous breathing or mechanically ventilated neurosurgical/neurological patients with no intracranial hypertension and found that passive ROM caused no changes in ICP, CPP, or BP [14]. Brimioulle et al. found that passive ROM did not affect ICP or CPP in the head-up position but tended to decrease ICP and increase CPP in the supine position [15]. In patients with high ICP they demonstrated that passive ROM also decreased ICP and increased CPP [15]. Recently, Roth et al. studied the effects of 20–30 min passive ROM in patients admitted to a NICU and found that passive ROM caused a decrease in ICP and an increase in CPP with no changes in MAP [16]. Brimioulle et al. suggested that the decrease in ICP with passive ROM was caused by a passive ROM-induced sensory stimulation and improved consciousness, as sensory stimulation has previously been shown to decrease ICP [15]. In none of these studies were systemic arterial blood pressure affected by passive ROM. This could be explained by the lack of effect of passive ROM on venous return and CO. In contrast to the above-mentioned studies, in the present study MAP increased during passive cycling exercise with no significant effects on ICP, with a consequent increase in CPP. One could speculate that the lack of effect of cycle exercise on ICP could be the lack of sensory stimulation from the cycle ergometer compared to that experienced by the patient from passive ROM offered by a physiotherapist.
The bedside cycle ergometer MOTOmed letto is a very useful and simple way of giving the patients longer periods of exercise in the ICU. It is simple to use, patient-friendly, and it can be used for passive as well as active exercises. From the cycle’s operating panel, different variables such as time and distance cycled is noted, giving the patient who is awake and the care provider the opportunity to compare day-to-day results and making it a useful tool for researchers.
There are a few limitations with this study: first, the inclusion was between 7 ± 5 days from admission, making it a very broad timespan. This was mainly dependent on the different attending neurosurgeons' opinions on when the patients were eligible for exercise and nothing the researchers could have an impact on. When we excluded the patients that were most fragile and were included 10 days or more after admission, the mean time was 4.5 days to inclusion. Secondly, the exercise was very modest with a pedal rate of 20 RPM and mostly passive cycling; and the patients were quite stable when they were included, making it a fairly safe intervention already from the beginning. However, the patients were still very fragile and their hemodynamic variables could easily be influenced. Thirdly, according to the generalizability, the sample size was quite small and males were overrepresented; it encompasses, however, the real population of patients with severe head injuries or stroke that are monitored for ICP changes in the NICU. Also, we only included patients with ICP measurements and excluded those who needed drainage of CSF to maintain stability. Most of the patients in this study suffered from TBI, which is an umbrella term with a variety of hematomas and locations of them so it encompasses many of the other diagnoses seen in the NICU. Finally, using a Vigileo Flotrac system for CO, SV, and SVV measurements is a simple way of monitoring systemic hemodynamics, since all of these patients that are critically ill already have an arterial line. However, in order to get reliable measurements, the Vigileo Flotrac system requires the patient to hold their arm and hand almost completely still during the continuous procedure due to its dependence on the waveform of the arterial line. This problem was solved by gently holding the patients' hand when needed.
The results of this study are based on 20 patients, but more and larger studies on the safety of early exercise in these patients are needed. It also raises a lot of new questions for further research: could bedcycling enhance the outcome of the patients making them stronger and more fit when leaving the NICU, could it be used to reduce spasticity, could it be used to reduce motorical stress and anxiety in the patients, and could it change the patients' demand of medication as sedatives and analgesics.
In this study of 20 patients with severe brain injury or stroke, we have demonstrated that early exercise with a bedside cycle ergometer in this cohort of patients could be started early during treatment in an NICU; but one should start with a maximum of 20 min of exercise until the patient is comfortable with the device. Finally, it is important to monitor the patients’ reactions to the treatment during the whole procedure.
Conclusion
Early passive exercise with a bedside cycle ergometer for patients with severe brain injuries or stroke is considered a safe procedure as it does not increase ICP and, if anything, increases CPP.
References
Koukourikos K, Tsaloglidou A, Kourkouta L. Muscle atrophy in intensive care unit patients. ACTA Inform Med. 2014;22:406–10.
Kress J. Clinical trials of early mobilization of critically ill patients. Crit Care Med. 2009;37:442–7.
Soliman I, Lange D, Peelen L, et al. Single-center large-cohort study into quality of life in Dutch intensive care unit subgroups, 1 year after admission, using EuroQol-6D-3l. J Crit Care. 2014;30:181–6.
Stiller K. Physiotherapy in intensive care an updated systematic review. Chest. 2013;144:825–47.
Titsworth L, Hester J, Correia T, et al. The effect of increased mobility on morbidity in the neurointensive care unit. J Neurosurg. 2012;116:1379–88.
Schweickert W, Pohlman M, Pohlman A, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial. Lancet. 2009;30:1874–82.
Gosselink R, Bott J, Johnson M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European respiratory Society and European Society of Intensive Care Medicine task force on physiotherapy for critically ill patients. Intensive Care Med. 2008;34:1188–99.
Sommers J, Engelbert R, Dettling-Ihnenfeldt D, et al. Physiotherapy in the intensive care unit: an evidence-based, expert driven, practical statement and rehabilitation recommendations. Clin Rehabil. 2015;29:1051–63.
Pires-Neto R, Kawaguchi Y, Hirota A, et al. Very early passive cycling exercise in mechanically ventilated critically ill patients: physiological and safety aspects—a case series. PLoS ONE. 2013;8:1–7.
Thelandersson A, Cider Å, Volkmann R. Cerebrovascular and systemic haemodynamic parameters during passive exercise. Adv Physiother. 2010;12:58–63.
Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009;37:2499–505.
Pires-Neto R, Pires-Neto RC, Pereira AL, et al. Characterization of the use of a cycle ergometer to assist in the physical therapy treatment of critically ill patients. Rev Bras Ter Intensiva. 2013;25(1):39–43.
Nóbrega A, Williamson J, Friedman D, Araújo C, Mitchell J. Cardiovascular responses to active and passive cycling movements. Med Sci Sports Exerc. 1994;26:709–14.
Koch SM, Fogarty S, Signorino C, Parmley L, Mehlhorn U. Effect of passive range of motion on intracranial pressure in neurosurgical patients. J Crit Care. 1996;11(4):176–9.
Brimioulle S, Moraine JJ, Norrenberg D, Kahn RJ. Effects of positioning and exercise on intracranial pressure in a neurosurgical intensive care unit. Phys Ther. 1997;77:1682–9.
Roth C, Stitz H, Kalhout A, Kleffmann J, Deinsberger W, Ferbert A. Effect of Early Physiotherapy in Intracranial Pressure and Cerebral Perfusion Pressure. Neurocrit Care. 2013;18:33–8.
Acknowledgments
We wish to thank all the nurses and assistant nurses at the NICU at Sahlgrenska University Hospital for all their help during this study.
Funding
The work was supported by grants from The Local Research and Development Board of Gothenburg and Renée Eander Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
There were no conflicts of interest.
Rights and permissions
About this article
Cite this article
Thelandersson, A., Nellgård, B., Ricksten, SE. et al. Effects of Early Bedside Cycle Exercise on Intracranial Pressure and Systemic Hemodynamics in Critically Ill Patients in a Neurointensive Care Unit. Neurocrit Care 25, 434–439 (2016). https://doi.org/10.1007/s12028-016-0278-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0278-2