Abstract
Background
Subarachnoid hemorrhage (SAH) is a disease with a high rate of unfavorable outcome, often related to delayed cerebral ischemia (DCI), i.e., ischemic injury that develops days–weeks after onset, with a multifactorial etiology. Disturbances in cerebral pressure autoregulation, the ability to maintain a steady cerebral blood flow (CBF), despite fluctuations in systemic blood pressure, have been suggested to play a role in the development of DCI. Pressure reactivity index (PRx) is a well-established measure of cerebral pressure autoregulation that has been used to study traumatic brain injury, but not extensively in SAH.
Objective
To study the relation between PRx and CBF in SAH patients, and to examine if PRx can be used to predict DCI.
Methods
Retrospective analysis of prospectively collected data. PRx was calculated as the correlation coefficient between mean arterial blood pressure (MABP) and intracranial pressure (ICP) in a 5 min moving window. CBF was measured using bedside Xenon-CT (Xe-CT). DCI was diagnosed clinically.
Results
47 poor-grade mechanically ventilated patients were studied. Patients with disturbed pressure autoregulation (high PRx values) had lower CBF, as measured by bedside Xe-CT; both in the early (day 0–3) and late (day 4–14) acute phase of the disease. PRx did not differ significantly between patients who developed DCI or not.
Conclusion
In mechanically ventilated and sedated SAH patients, high PRx (more disturbed CBF pressure autoregulation) is associated with low CBF, both day 0–3 and day 4–14 after onset. The role of PRx as a monitoring tool in SAH patients needs further studying.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage accounts for about 5 % of all strokes, with an overall global incidence of approximately 9/100 000 person years [1, 2]. Despite improvements in outcome during the last decades, it remains a disease with high rates of mortality and unfavorable outcome [3]. About 30 % die from the hemorrhage, and of those who survive, approximately 30 % do not regain full independence [4, 5]. A major cause of neurological deterioration and unfavorable outcome is delayed cerebral ischemia (DCI), neurological deterioration that occurs days–weeks after the initial hemorrhage, and affects approximately 30 % of SAH patients [6]. Originally DCI was thought to be caused solely by vascular spasm that reduces cerebral blood flow with subsequent hypoperfusion and infarction [7–9]. This explanation has proved incomplete as some patients with no evidence of vasospasm still develop neurological deficits and vice versa [10]. The pathophysiology of DCI is not completely understood, but is presently considered multifactorial with elements of endothelial dysfunction, blood–brain-barrier disruption, cortical spreading depolarizations, microvascular thrombosis and failure of cerebral autoregulation, as well as vascular spasm [11–13]. Various clinical secondary insults are also probably involved, both intracranial (e.g., high intracranial pressure and seizures) and systemic (e.g., hypotension and fever) [14, 15].
Cerebral pressure autoregulation is defined as the ability of the cerebral vasculature to maintain a stable and adequate CBF, despite variations in systemic blood pressure [16]. The direct mechanism of cerebral autoregulation is variations in vascular diameter in response to changes in transmural pressure, causing alterations in cerebrovascular resistance, that in turn keep CBF stable [17]. When pressure autoregulation is impaired, the vascular bed will not be able to compensate for events of low or high cerebral perfusion pressure (CPP), and the risk of developing ischemia or hyperperfusion, respectively, increases. Earlier studies in SAH using different methodologies have shown that failure of pressure autoregulation is associated with vasospasm, as well as with DCI and unfavorable clinical outcome [18–21]. Pressure reactivity index (PRx) is an autoregulatory index that is calculated as a moving correlation coefficient between mean arterial blood pressure (MABP) and intracranial pressure (ICP) based on spontaneous fluctuations in MABP. PRx has been used to study autoregulation in SAH in only a few previous studies [22–25]. No study has targeted the association between PRx and CBF in SAH patients. The purpose of the present study was twofold: to analyze the relationship between PRx and CBF measured by bedside Xenon-enhanced computed tomography (Xe-CT) in patients with SAH and to examine if PRx can be used to predict DCI.
Materials and Methods
Patients and Treatment Protocol
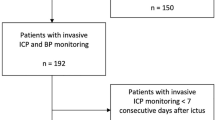
Patients with SAH admitted to the neurointensive care unit (NICU) at Uppsala University Hospital between October 2012 and February 2015 were eligible for this study. Inclusion criteria were mechanical ventilation, valid Xe-CT CBF data, and invasive ICP and MABP monitoring, i.e., patients with severe SAH were selected for the study.
The patients were managed according to a standardized NICU protocol using multimodal physiological and neurological monitoring to rapidly detect and treat secondary insults [15]. Unconscious patients (GCS motor score ≤5) were intubated and ventilated mechanically, and received a ventriculostomy for ICP monitoring and CSF drainage (Liquor-Drainage-Set, HanniSet® Xtrans, Smith Medical GmbH, Glasbrunn, Germany). Propofol (Propofol®, B. Braun Medical AB, Melsungen, Germany) was given for sedation and Morphinechloride (Morphine®, Meda, Solna, Sweden) for analgesia. The treatment protocol aimed at ICP <20 mm Hg, cerebral perfusion pressure (CPP) >60 mm Hg, normotension, normovolemia or mild hypervolemia, body temperature <38 °C, and normal electrolyte levels. Hydrocephalus and intracranial hypertension were treated with CSF drainage against a pressure level of 15 mm Hg. Hypotension was treated with 20 % albumin and crystalloids, with the addition of dobutamine and in a few cases norepinephrine, if necessary. Aneurysms were treated early with endovascular coiling or surgical clipping.
DCI was diagnosed clinically when neurological deficits/deterioration occurred without any other explanation, such as hematoma, hydrocephalus, infection, etc. Triple-H therapy (hypertension, hypervolemia, and hemodilution) by the administration of Dextran 40 solution, 500 ml/day (Rheomacrodex®, 100 mg/ml, Meda AB, Solna, Sweden), and Albumin 100 ml, 2 × daily (200 mg/ml, Baxter Medical AB, Kista, Sweden) was used to treat DCI [26–28]. All patients received prophylactic nimodipine.
Data Collection
Physiological data were prospectively collected and stored in a database by the ODIN multimodality monitoring system, developed at Uppsala University and Edinburgh University [29].
Xenon-CT CBF Measurement
Cerebral blood flow was measured bedside with Xe-CT [30]. Xenon is an inert, radio-opaque gas that diffuses freely across the blood–brain-barrier and can be used as an inhaled contrast agent. A gas mixture with 28 % Xenon gas is distributed to the patient via the ventilator, and repeated scans of four 1-cm-thick slices are performed during the wash-in phase. CBF can then be calculated by a modified Kety-Schmidt method, which provides a quantitative measurement of CBF. A portable CT scanner (CereTom®, Neurologica, Boston, USA) was used with the Enhancer 3000 Xenon delivery system (Diversified Diagnostic Products Inc., Houston, USA). It was considered to be an advantage that a system with a portable CT scanner was used, since CBF could be measured bedside in the NICU without transporting the patient to the radiology department. The CBF values, though being snapshots, probably more reliably reflect the “true” CBF during standard neurointensive care than CBF measurements after transportation to another location, when sedation and ventilation parameters are likely to be different.
According to a standardized protocol, all intubated patients should undergo Xe-CT three times: day 0–1, day 4–7 and day 8–12 after onset of disease. Xe-CT scans were sometimes omitted or added for the clinical reasons. In this study, Xe-CT scans up to day 14 after onset were used, and sorted into two time windows, day 0–3 and 4–14 after onset, i.e., roughly before and during expected peak incidence of DCI. If a patient was scanned multiple times in one time window, only the first scan was used. Arterial pO2 and pCO2 were measured in conjunction with the Xe-CT exam. Time of the diagnostic CT scan was used as a surrogate for onset of the disease, as this CT generally is done very close to the hemorrhage [31].
Pressure Reactivity
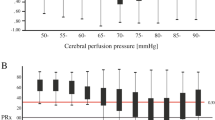
ICP was measured through external ventricular drain, and ICP data for PRx calculation were used both in the case of open or closed drain. PRx was calculated as the correlation coefficient between 30 consecutive average values over 10 s of MABP and ICP, with ICP on the Y-axis and MABP on the X-axis [32]. This 5-minute window was moved forward in increments of 12 s, generating 5 PRx values each minute. One-minute averages for PRx were then calculated.
In studies, PRx is often averaged over long time periods. We calculated mean PRx for 6, 4, and 2 h before each Xe-CT exam to examine if PRx could be used to predict CBF, and if different time averages had equal predictive value. Mean PRx in the different time intervals was used to group patients into high PRx (>0.1) and low PRx (≤0.1) groups, to reflect more or less disturbed pressure autoregulation, respectively.
Xe-CT Parameters
In the four 1-cm-thick Xe-CT slices, the cortical mantle was divided into 20 approximately 3–4 cm3 sized regional volumes of interest (rVOI, see Fig. 1). If a Xe-CT slice was too superior or inferior to allow for CBF calculation (i.e., due to partial volume effects of the calvarium or skull base), it was excluded. Regional VOIs including intracerebral haematoma were also excluded. Three CBF parameters were calculated: (1) Mean global CBF (all rVOIs), (2) CBF % < 20, and (3) CBF % < 10. The two latter were calculated as follows:
Example of CBF measurements. Only one 1-cm-thick slice is shown. The cortical mantle is divided into 20 regional volumes of interest (rVOI) with mean CBF in each rVOI shown in the table. The calculated CBF is measured in ml × 100 g−1 × min−1. Mean = mean rVOI CBF. Area = number of pixels in each 1-cm-thick rVOI, 100 pixels correspond to 1 cm3
The CBF thresholds of 20 and 10 ml × 100 mg−1 × min−1 were chosen to correspond to tissue at intermediate and high risk of ischemia, respectively [33, 34].
Statistical Methods
Patients were divided into high PRx and low PRx groups (PRx > 0.1 and PRx ≤ 0.1), i.e., more disturbed/less disturbed pressure autoregulation. Differences in variables between PRx groups were calculated with a non-parametric test (Mann–Whitney U-test), since the physiological parameters were non-normally distributed and the demographic data did not meet the assumptions for a parametric test. Separate calculations were done in the different time windows. When comparing repeated measures, Wilcoxon-matched pairs test was used.
A p value <0.05 was considered statistically significant.
Ethics
The Uppsala Regional Ethical Review Board for clinical research and the local radiation safety authority granted permission to undertake the study.
Results
47 patients (34 female, 13 male; age 28–81 years, median 59 years) had valid PRx and CBF data and were included in the study. Median Hunt & Hess score at admission was 3 (range 1–5) and median CT Fisher score of the diagnostic CT scan was 4 (range 2–4) [35, 36]. The patients with low Hunt & Hess grade at admission in this study later deteriorated and were intubated, and could therefore be included in the study. Thirty-nine patients were treated with endovascular embolization and eight patients with surgical clipping. Thirty-eight patients were examined in the pre-DCI time window (day 0–3 after onset) and 30 patients in the DCI time window (day 4–14 after onset). Twenty-one patients were examined in both time windows.
For comparison, the total number of aneurysmal SAH patients at our institution during the study time was 229 (average age 58.7 years, 64 % female).
Pre-DCI Window (Day 0–3 After Onset)
Patient characteristics and physiological data for the 38 patients with valid Xe-CT exams and PRx data day 0–3 after onset are presented in Table 1. A consistent finding was that high PRx patients (PRx > 0.1, i.e., more disturbed pressure autoregulation) had lower CBF parameters compared to low PRx patients (PRx ≤ 0.1, less disturbed pressure autoregulation) (Table 2). The differences were statistically significant for CBF % < 10 (6-h mean PRx value). None of the other recorded parameters (age, Hunt & Hess grade, CT Fisher grade, pO2, pCO2, ICP, MABP, and CPP) differed significantly between high PRx and low PRx groups (6-h mean PRx, Table 1).
DCI Window (Day 4–14 After Onset)
Patient characteristics and physiological data for the 30 patients with valid Xe-CT exams and PRx data day 4–14 after onset are presented in Table 3. As well as in the pre-DCI window, there was a consistent trend toward lower CBF parameters in high PRx patients. The difference was statistically significant regarding CBF % < 10 (6-h mean PRx, Table 4). Using 6-h mean PRx, there was no significant difference in age, Hunt & Hess grade, CT Fisher grade, pO2, pCO2, ICP, MABP, or CPP between high PRx and low PRx patients (Table 3).
Comparisons Between Pre-DCI and DCI Time Window
Twenty-one patients were examined both in the pre-DCI and the DCI time window. Comparisons between CBF and physiological parameters in the different time windows in these patients are presented in Table 5. There were no statistically significant differences except in pCO2, which was slightly higher in the DCI time window (median 5.6 vs. 5.1).
DCI, Relation to CBF, Epidemiological and Physiological Parameters
Fourteen patients were judged clinically to have developed DCI, and were treated with triple-H therapy. Eleven of those had CBF and PRx data in the pre-DCI window. There were no significant differences in CBF or PRx data between DCI/non-DCI patients, though DCI patients had lower mean global CBF with borderline significance. There was no difference regarding epidemiological or physiological parameters (Table 6).
Discussion
A few previous papers have used PRx to study pressure reactivity in subarachnoid hemorrhage: [22–25] Bijlenga et al. studied poor-grade SAH patients, and found that survivors had lower PRx at their calculated optimal CPP compared to non-survivors [24]. In a small study, Barth et al. found no correlation between PRx and clinical outcome according to Glasgow outcome scale (GOS), nor any difference in PRx between patients who did and did not develop infarcts [22]. Eide et al. found that PRx could differentiate between survivors and non-survivors, but not between survivors with dependent and independent outcome [23]. Altogether, it appears as CBF pressure autoregulation plays a role for the clinical course of SAH patients. The mechanisms for this are poorly investigated. In order to get a better insight into the pathophysiology of SAH, we studied the relation between PRx and CBF in patients with severe SAH.
The results of this study showed that in the pre-DCI window (day 0–3 after onset) high PRx, i.e., more disturbed autoregulation, was associated with lower CBF, both regional and global, but was only statistically significant in CBF % < 10 ml × 100 mg−1 × min−1 with 6-h mean value of PRx. The 4- and 2-h PRx averages did not produce significant associations with any of the studied CBF parameters. This may be explained by the inherent noise in the PRx signal, requiring longer time averages to cancel out the noise [37]. In the DCI window (day 4–14 after onset), high PRx was also associated with lower CBF in general, although the difference was only statistically significant in CBF % < 10 when 6-h mean PRx was used. These results underline the importance of avoiding hypotension particularly in patients with high PRx. It is also likely that the patients included in this study, i.e., sedated and mechanically ventilated patients with severe SAH, are more hypotensive than those patients who are awake. The result may not have been the same in unsedated patients with less severe disease.
The differences in mean global CBF in Tables 2 and 4 are probably not clinically significant. However, the differences found in CBF % < 10 may be of high importance even if they are small in absolute numbers, since an increase in brain tissue with CBF < 10 ml × 100 g−1 × min−1 increases the risk of ischemia with potentially devastating effects. Mean global CBF may not be a good parameter to estimate tissue at risk of ischemia, since mean CBF may be normal when some areas are ischemic if other regions simultaneously are hyperemic.
A PRx threshold of 0.1 was chosen to dichotomize patients into low/high PRx groups. In a study with greater number of included patients, three PRx groups would be preferable (low/intermediate/high PRx). Since the present study is relatively small, we chose a study design with two PRx groups to achieve greater statistical power. With this in mind, PRx 0.1 seems a suitable threshold to divide patients. This must be considered when interpreting the results, as “intermediate” PRx patients will be included in the low and high PRx groups, respectively.
A methodological problem that must be addressed is assessing PRx when the ventricular drain is open, since this may affect both the level and the curve pattern of ICP. In case of an open-ventricular drain system, craniospinal compliance may be altered. In that case, changes in ICP following changes in MABP may be diminished and PRx values are inaccurate. Bijlenga used monitoring data from time periods with closed ventricular systems only [24]. Eide came to similar results without excluding open-ventricular drain data [23]. In this paper, the ICP values used for PRx calculation were derived from the ventricular drains irrespective of if the system was open or closed. However, in another preliminary study, we found no difference in CPP or PRx when data from closed/open drainage systems were compared (data not shown). Our ventricular drain system (Liquor-Drainage-Set, HanniSet® Xtrans, Smith Medical GmbH, Glasbrunn, Germany) has a rubber valve at the outflow tube, which causes an outflow resistance so the ICP amplitudes are visible even when the system is open for CSF drainage. Therefore, we assumed that quick changes in MABP would induce enough changes in ICP to produce relatively accurate PRx values. As acute hydrocephalus and CSF drainage with ventricular drain are common in these patients, we decided to include open-ventricular drain data to avoid losing information. This approach is supported by a recent publication by Aries and co-workers who concluded that PRx values derived from open-ventricular drains are valid as long as the ICP curve has normal configuration [25]. Although the results by Aries are encouraging, the study is a small pilot study with only 10 included patients and this must be repeated in larger studies before ICP data from open-ventricular drains can be completely relied upon in PRx calculation. In a recently completed study, however, we found the same in 80 SAH patients showing only a very small and clinically insignificant decrease of PRx when the ventriculostomy was opened (submitted manuscript).
Large amounts of extravasated blood and poor clinical condition are known predictors for DCI [36, 38]. In our study, we found no association between Fischer or Hunt & Hess score at admission and the subsequent development of DCI. This may be partly explained by small sample size with the lack of statistical power. Also, the study was done on a selected group of patients, all in poor clinical condition. Although there was no statistically significant difference, no patients with Fisher grade of 2–3 developed DCI.
We found no association between CBF parameters day 0–3 and subsequent development of DCI. Small sample size may be an explanation here as well. However, we noted lower global CBF in patients who later developed DCI, with a p value of 0.05. This is in line with findings in a previous pilot study at our institution, suggesting that patients with initial low global CBF (<27 ml × 100 g−1 × min−1) are more likely to develop DCI [39]. Previous studies suggest an association between dysfunction of pressure autoregulation and DCI [19, 20, 40]. The lack of association in our study between PRx day 0–3 and later development of DCI may be partly explained by how vasospasm affects PRx, as discussed below. It should also be noted that the development of DCI is a multifactorial process, and single predictors such as PRx or CBF may not be enough to produce statistical significance. [11–13] Associations may be especially hard to prove in patients with severe disease, such as in the present study, who are more likely to develop DCI and achieve unfavorable outcome than those with less severe disease.
PRx is an index that relies on spontaneous fluctuations in ICP and MABP, and it is important to consider how this relation between these parameters may be affected by vascular spasm or loss of vascular tone. Pressure autoregulation is thought to be mediated mostly by pial and parenchymal vessels, distally in the cerebral vascular tree [41]. In case of vasospasm affecting vessels at this level, the possibility to modulate vessel diameter in response to changes in CPP will be lost. The plateau of the autoregulatory curve (and pressure autoregulation by definition) will be lost, and CBF depends passively on MABP [42]. In this instance, the correlation coefficient between MABP and ICP will be decreased and PRx will show false low values, indicating more intact autoregulation than what is true. On the other hand, in case of vasospasm in the proximal arteries with preserved autoregulation distally, distal vasodilatation will occur as an adequate pressure autoregulation response [43]. In this instance, the possibility to autoregulate by modulation of vessel diameter will still be preserved, and PRx will still be a valid index of autoregulation, but the autoregulatory curve will be shifted to the right. Considering the opposite of vasospasm, namely loss of vasomotor tone, autoregulation will be lost, and CBF depends passively on MABP. PRx in this instance will, however, still be a valid indicator of pressure autoregulation (Fig. 2).Caution must therefore be used when PRx values are interpreted, since it may not always be a reliable indicator of the status of autoregulation. This is supported by a recent small study which found that worsening impairment of an autoregulatory index (Mx) based on spontaneous fluctuations of mean MABP and transcranial Doppler mean flow velocities was related to DCI but only when also taking blood flow velocities in intracerebral arteries into account [44]. The relation between PRx and the “true” status of pressure reactivity in patients with alterations in vasomotor tone deservers further study.
Theoretical implications of vasomotor tonus and autoregulation. 1 Normal vasomotor tonus and normal autoregulation. PRx is a valid index of autoregulation. 2 Proximal vasospasm and normal distal vasomotor reactivity. Preserved autoregulation. PRx is valid, but the autoregulatory curve is shifted to the right. 3 Distal vasospasm. Loss of autoregulation. PRx is invalid due to false low values. 4 Loss of vasomotor tonus. Loss of autoregulation. PRx is valid
Conclusions
In mechanically ventilated and sedated SAH patients, high PRx (more disturbed CBF pressure autoregulation) is associated with low CBF, both in day 0–3 and day 4–14 after onset. PRx must be interpreted with caution in patients with SAH and vasospasm.
References
de Rooij NK, Linn FHH, van der Plas JA, Algra A, Rinkel GJE. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78(12):1365–72.
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project–1981-86. 2. Incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1990;53(1):16–22.
Koffijberg H, Buskens E, Granath F, et al. Subarachnoid haemorrhage in Sweden 1987–2002: regional incidence and case fatality rates. J Neurol Neurosurg Psychiatry. 2008;79(3):294–9.
Nieuwkamp DJ, Setz LE, Algra A, Linn FHH, de Rooij NK, Rinkel GJE. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol. 2009;8(7):635–42.
Hop JW, Rinkel GJE, Algra A, van Gijn J. Case-fatality rates and functional outcome after subarachnoid hemorrhage a systematic review. Stroke. 1997;28(3):660–4.
Rabinstein AA, Friedman JA, Weigand SD, et al. Predictors of Cerebral Infarction in Aneurysmal Subarachnoid Hemorrhage. Stroke. 2004;35(8):1862–6.
Ecker A, Riemenschneider PA. Arteriographic demonstration of spasm of the intracranial arteries, with special reference to saccular arterial aneurysms. J Neurosurg. 1951;8(6):660–7.
Harders AG, Gilsbach JM. Time course of blood velocity changes related to vasospasm in the circle of Willis measured by transcranial Doppler ultrasound. J Neurosurg. 1987;66(5):718–28.
Allcock JM, Drake CG. Postoperative angiography in cases of ruptured intracranial aneurysms. J Neurosurg. 1963;20:752–9.
Etminan N, Vergouwen MDI, Ilodigwe D, Macdonald RL. Effect of pharmaceutical treatment on vasospasm, delayed cerebral ischemia, and clinical outcome in patients with aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 2011;31(6):1443–51.
Dóczi T. The pathogenetic and prognostic significance of blood-brain barrier damage at the acute stage of aneurysmal subarachnoid haemorrhage. Clinical and experimental studies. Acta Neurochir (Wien). 1985;77(3–4):110–32.
Sarrafzadeh A, Santos E, Wiesenthal D, et al. Cerebral glucose and spreading depolarization in patients with aneurysmal subarachnoid hemorrhage. Acta Neurochir Suppl. 2013;115:143–7.
Stein SC, Browne KD, Chen X-H, Smith DH, Graham DI. Thromboembolism and delayed cerebral ischemia after subarachnoid hemorrhage: an autopsy study. Neurosurgery. 2006;59(4):781–7 (discussion 787–8).
Enblad P, Persson L. Impact on clinical outcome of secondary brain insults during the neurointensive care of patients with subarachnoid haemorrhage: a pilot study. J Neurol Neurosurg Psychiatry. 1997;62(5):512–6.
Ryttlefors M, Howells T, Nilsson P, Ronne-Engström E, Enblad P. Secondary insults in subarachnoid hemorrhage: occurrence and impact on outcome and clinical deterioration. Neurosurgery. 2007;61(4):704–14 (discussion 714–5).
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H. Cerebral autoregulation dynamics in humans. Stroke J Cereb Circ. 1989;20(1):45–52.
Lassen NA. Autoregulation of cerebral blood flow. Circ Res. 1964;15(SUPPL):201–4.
Budohoski KP, Czosnyka M, Smielewski P, et al. Cerebral autoregulation after subarachnoid hemorrhage: comparison of three methods. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 2013;33(3):449–56.
Jaeger M, Schuhmann MU, Soehle M, Nagel C, Meixensberger J. Continuous monitoring of cerebrovascular autoregulation after subarachnoid hemorrhage by brain tissue oxygen pressure reactivity and its relation to delayed cerebral infarction. Stroke. 2007;38(3):981–6.
Budohoski KP, Czosnyka M, Smielewski P, et al. Impairment of cerebral autoregulation predicts delayed cerebral ischemia after subarachnoid hemorrhage a prospective observational study. Stroke. 2012;43(12):3230–7.
Lam JM, Smielewski P, Czosnyka M, Pickard JD, Kirkpatrick PJ. Predicting delayed ischemic deficits after aneurysmal subarachnoid hemorrhage using a transient hyperemic response test of cerebral autoregulation. Neurosurgery. 2000;47(4):819–25 (discussions 825–6).
Barth M, Woitzik J, Weiss C, et al. Correlation of clinical outcome with pressure-, oxygen-, and flow-related indices of cerebrovascular reactivity in patients following aneurysmal SAH. Neurocrit Care. 2010;12(2):234–43.
Eide PK, Sorteberg A, Bentsen G, Marthinsen PB, Stubhaug A, Sorteberg W. Pressure-derived versus pressure wave amplitude-derived indices of cerebrovascular pressure reactivity in relation to early clinical state and 12-month outcome following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2012;116(5):961–71.
Bijlenga P, Czosnyka M, Budohoski KP, et al. “Optimal cerebral perfusion pressure” in poor grade patients after subarachnoid hemorrhage. Neurocrit Care. 2010;13(1):17–23.
Aries MJH, de Jong SF, van Dijk JMC, et al. Observation of autoregulation indices during ventricular CSF drainage after aneurysmal subarachnoid hemorrhage: a pilot study. Neurocrit Care. 2015;23(3):347–54.
Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43(6):1711–37.
Friedman JA, Pichelmann MA, Piepgras DG, et al. Pulmonary complications of aneurysmal subarachnoid hemorrhage. Neurosurgery. 2003;52(5):1025–32.
Diringer MN, Bleck TP, Iii JCH, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care. 2011;15(2):211–40.
Howells T, Elf K, Jones PA, et al. Pressure reactivity as a guide in the treatment of cerebral perfusion pressure in patients with brain trauma. J Neurosurg. 2005;102(2):311–7.
Yonas H, Sekhar L, Johnson DW, Gur D. Determination of irreversible ischemia by xenon-enhanced computed tomographic monitoring of cerebral blood flow in patients with symptomatic vasospasm. Neurosurgery. 1989;24(3):368–72.
Zetterling M, Hallberg L, Hillered L, Karlsson T, Enblad P, Ronne Engström E. Brain energy metabolism in patients with spontaneous subarachnoid hemorrhage and global cerebral edema. Neurosurgery. 2010;66(6):1102–10.
Brady KM, Shaffner DH, Lee JK, et al. Continuous monitoring of cerebrovascular pressure reactivity after traumatic brain injury in children. Pediatrics. 2009;124(6):e1205–12.
Astrup J, Siesjö BK, Symon L. Thresholds in cerebral ischemia—the ischemic penumbra. Stroke. 1981;12(6):723–5.
Kaufmann AM, Firlik AD, Fukui MB, Wechsler LR, Jungries CA, Yonas H. Ischemic core and penumbra in human stroke. Stroke J Cereb Circ. 1999;30(1):93–9.
Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968;28(1):14–20.
Fisher CMMD, Kistler JPMD, Davis JMMD. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980;6(1):1–9.
Czosnyka M, Brady K, Reinhard M, Smielewski P, Steiner LA. Monitoring of cerebrovascular autoregulation: facts, myths, and missing links. Neurocrit Care. 2009;10(3):373–86.
Dupont SA, Wijdicks EFM, Manno EM, Lanzino G, Rabinstein AA. Prediction of angiographic vasospasm after aneurysmal subarachnoid hemorrhage: value of the Hijdra sum scoring system. Neurocrit Care. 2009;11(2):172–6.
Rostami E, Engquist H, Johnson U, et al. Monitoring of cerebral blood flow and metabolism bedside in patients with subarachnoid hemorrhage—a xenon-CT and microdialysis study. Front Neurol. 2014;5:89.
Fontana J, Wenz H, Schmieder K, Barth M. Impairment of dynamic pressure autoregulation precedes clinical deterioration after aneurysmal subarachnoid hemorrhage. J Neuroimaging Off J Am Soc Neuroimaging. 2015;. doi:10.1111/jon.12295.
Kontos HA, Wei EP, Navari RM, Levasseur JE, Rosenblum WI, Patterson JL. Responses of cerebral arteries and arterioles to acute hypotension and hypertension. Am J Physiol. 1978;234(4):H371–83.
Yundt KD, Grubb RL, Diringer MN, Powers WJ. Autoregulatory vasodilation of parenchymal vessels is impaired during cerebral vasospasm. J Cereb Blood Flow Metab. 1998;18(4):419–24.
Soehle M, Czosnyka M, Pickard JD, Kirkpatrick PJ. Critical closing pressure in subarachnoid hemorrhage: effect of cerebral vasospasm and limitations of a transcranial Doppler-derived estimation. Stroke J Cereb Circ. 2004;35(6):1393–8.
Calviere L, Nasr N, Arnaud C, et al. Prediction of delayed cerebral ischemia after subarachnoid hemorrhage using cerebral blood flow velocities and cerebral autoregulation assessment. Neurocrit Care. 2015;23(2):253–8.
Acknowledgments
The authors wish to express warm gratitude to Johan Bäckander for his excellent work with the Xe-CT exams.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnson, U., Engquist, H., Howells, T. et al. Bedside Xenon-CT Shows Lower CBF in SAH Patients with Impaired CBF Pressure Autoregulation as Defined by Pressure Reactivity Index (PRx). Neurocrit Care 25, 47–55 (2016). https://doi.org/10.1007/s12028-016-0240-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0240-3