Abstract
Primary immunodeficiencies (PI) are genetic defects of the immune system that result in chronic, serious, and often life-threatening infections, if not diagnosed and treated. Many patients with PI are undiagnosed, underdiagnosed, or misdiagnosed. In fact, recent studies have shown that PI may be more common than previously estimated and that as many as 1% of the population may be affected with a PI when all types and varieties are considered. In order to raise awareness of PI with the overall goal of reducing associated morbidity and mortality, the Jeffrey Modell Foundation (JMF) established a network of specialized centers that could better identify, diagnose, treat, and follow patients with PI disorders. Over the past decade, the Jeffrey Modell Centers Network (JMCN) has provided the infrastructure to accept referrals, provide diagnosis, and offer treatments. Currently, the network consists of 792 Expert Physicians at 358 institutions, in 277 cities, and 86 countries spanning 6 continents. JMF developed an annual survey for physician experts within the JMCN, using the categories and gene defects identified by the International Union of Immunological Societies Expert Committee for the Classification of PI, to report on the number of patients identified with PI; treatment modalities, including immunoglobulins, transplantation, and gene therapy; and data on gender and age. Center Directors also provided physician-reported outcomes and differentials pre- and post-diagnosis. The current physician-reported data reflect an increase in diagnosed patients, as well as those receiving treatment. Suspected patients are being identified and referred so that they can receive early and appropriate diagnosis and treatment. The significant increase in patients identified with a PI is due, in part, to expanding education and awareness initiatives, newborn screening, and the expansion of molecular diagnosis and sequencing. To our knowledge, this is the most extensive single physician report on patients with PI around the world.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary immunodeficiencies (PI) [1, 2] are genetic defects of the immune system that result in chronic, serious, and often life-threatening infections, and/or life-threatening autoimmunity if not diagnosed and treated [3, 4]. There are more than 350 genetically defined single-gene inborn errors of immunity [5]. In addition to diseases as serious as severe combined immunodeficiency (SCID), manifestations may include susceptibility to opportunistic infections, persistent inflammation, and severe organ-specific autoimmune conditions.
Recent studies have shown that PI may be more common than previously estimated [6] and that as many as 1% of the population may be affected with a PI when all types and varieties are considered [7]. This includes monogenic detriments leading to common infectious diseases such as severe influenza, as well as autoimmune diseases, such as cytopenias and systemic lupus erythematosus, and inflammatory diseases [5]. Recently, improvements in molecular diagnosis, genetic and exome sequencing, cutting edge research, and treatments have led to a better understanding of the immune system, as well as improved quality of life for those living with PI [8,9,10,11,12]. However, awareness of PI among physicians and the general public remains challenging, and there continues to be a need for improved and timely management of these conditions [13, 14].
In order to raise awareness of PI with the overall goal of reducing associated morbidity and mortality, the Jeffrey Modell Foundation (JMF) established a network of specialized centers that could better identify, diagnose, treat, and follow patients with PI disorders. Over the past decade, the Jeffrey Modell Centers Network (JMCN) has provided the infrastructure to accept referrals, provide diagnosis, and offer treatments. Currently, the network consists of 792 Expert Physicians at 358 institutions, in 277 cities, and 86 countries spanning 6 continents.
JMF developed a survey for physician experts within the JMCN to be able to report on the number of patients identified with PI, the treatment modalities, including immunoglobulins, transplantation, and gene therapy, as well as to acquire data on patient sex and age. Center Directors also provided physician-reported outcomes and differentials pre- and post-diagnosis.
Classification of primary immunodeficiency
In 1970, the World Health Organization (WHO) established a committee to catalog primary immunodeficiencies. Twenty years later, the International Union of Immunological Societies (IUIS) took the remit of the WHO commitment. The IUIS classification continues to serve as an indispensable reference for immunologists and researchers worldwide, as the field continues to grow in both size and complexity [15].
The current IUIS report includes 354 distinct disorders with 344 different gene defects listed, a remarkable spectrum of phenotypes. In the past 2 years, 85 new genes have been identified, while in the past 1 year alone, 35 new genes have been identified [15]. There has been a striking increase in the number of recognized disorders due in part to the increase in the application of next-generation sequencing. This has also resulted in a number of new inborn errors of immunity identified in a single or small number of kindreds, which may not provide a complete and accurate picture about prevalence and phenotype [15]. Additionally, the increase in the utilization of next-generation sequencing has resulted in significant expansion of the range of phenotypes associated with various diseases, adding to the complexity of appropriate diagnosis [15].
Methods
JMF survey identifying defects and treatments
The JMF physician survey on PI was developed using the categories and gene defects identified by the IUIS Expert Committee for the Classification of PI [15] using the most recent version of the document available at the time [16]. Each defect in the survey is identified, when appropriate, as autosomal dominant inheritance, autosomal recessive inheritance, X-linked inheritance, gain-of-function mutation, loss-of-function mutation, and haplo insufficiency in accordance with the listings in the IUIS document.
Surveys were sent to all Center Directors via e-mail, requesting data in 2017. The 2017 survey incorporated new gene defects known to cause PI and a demographics section. Each JMCN Center Director was asked to provide information on the number of patients seen and followed with PI and the number of patients diagnosed with specific defects. Specific PI diagnoses were grouped according to the IUIS classifications. Physicians were given the opportunity to list “unspecified” or “other deficiencies” for any additional disorders or gene mutations not listed in the survey. Physician-reported outcomes were analyzed further according to regional geography.
The JMF survey also included questions assessing immunoglobulin therapies. Specifically, the survey included data fields to determine the number of patients receiving immunoglobulin therapy intravenously (in the clinic or at home), by subcutaneous administration, or other methods of administration. Information was also requested on the number of patients treated by gene therapy and hematopoietic stem cell transplantation (HSCT), including donor type and stem cell source. Physicians had the opportunity to report the sex and age of patients treated at each center.
Surveys were returned to JMF by e-mail or fax, at which point the data was entered into an extensive and protected Microsoft Excel spreadsheet. Data was randomly spot checked on a regular basis to ensure the quality of data entry. The survey data was then available to analyze within Microsoft Excel or could be exported to other programs, such as Microsoft Access or SPSS software, for further analysis if necessary. It is important to note that no patient identifying information was collected during this process, and all information provided was HIPAA compliant.
Physician reported clinical outcomes
Network Center Directors were asked to consider their records of PI patients 1 year before diagnosis and for the year subsequent to diagnosis and report on outcomes based upon their analysis. Eighty-five centers in the JMCN responded, and given that validation of outcomes was not required, it is important that these findings are considered as physician-reported.
Cost analysis measuring outcome improvement
Cost analysis estimates, reflecting the patient outcomes described in the previous section, were generated as follows: hospital charges and length of stay data were obtained from the Hospital Cost and Utilization Project (HCUP), Nationwide Inpatient Sample, under the auspices of the Agency for Healthcare Research and Quality (AHRQ) [17]. Data was collected by individual states and provided to AHRQ. Principal diagnosis was based on clinical classification software; charges were based on hospital accounting reports from the Centers for Medicare and Medicaid Services. Charges represent hospital billings, not hospital costs or percentage of costs actually collected by hospitals; a unit of analysis for HCUP data is a hospital stay, based on discharge data per patient. A patient admitted to the hospital multiple times in 1 year was counted each time as a separate discharge. The study assumes minimum frequency of adverse events, i.e., infections and hospitalizations. Costs related to SCID are not included in the study. Experts report significant costs of repeated or prolonged intensive care unit admissions in connection with SCID. “Inpatient” information was obtained from the HCUP website [17]; “outpatient” information was obtained from the Aetna website [18]. Charges are based on “in network” coverage, with “out of network” costs two to four times greater [18]. Health care cost data for privately insured patients were included [19, 20]; health care cost data from the Centers for Medicare and Medicaid statistics were included [21, 22]; economic factors underlying growth in Medicare spending were determined by Congressional Budget Office data [23]; and employer-sponsored coverage data was provided by the Employee Benefit Research Institute Issue: Washington, DC [24, 25]. Costs were updated using the Health Care Cost Institute (HCCI) data [26]. HCCI performed analysis on a subset of data for approximately 40 million insureds per year from 2010 through 2014. This generated approximately 5 billion claim lines and represents one of the largest data sets on the privately insured ever assembled.
Results
Prevalence
To evaluate the overall prevalence of patients followed and identified with a specific PI defect in the JMCN, the physician-reported prevalence of patients with PI among JMCN sites from 2013 was compared to that from 2018. The physician-reported prevalence of patients with PI among JMCN sites increased during this period. The number of patients followed in the JMCN from 2013 to 2018 increased by 57% in the USA and 35.4% globally (Table 1). The number of patients identified with a specific PI defect in the JMCN during the same 5-year period increased by 32.7% in the USA and 21.8% globally (Table 1). Given that the increase in the number of JMCN reporting sites between the 2013 and 2018 data was only 12%, the increase in prevalence as well as many of the other measures reported below were unlikely to be a feature of increased reporting centers. For this reason, the data presented were not normalized. To note, “international” represents reporting centers outside of the USA. “Global” represents the total of all center reports.
Regional prevalence trends
Identifying regional trends in the number of patients followed in the JMCN is important to understand the overall picture of patient prevalence. The number of patients followed in the JMCN over the past 5 years was compared across nine global regions. The number of patients followed in Latin America increased by 132.2% during this time frame, while increasing by 29.6% in the Middle East and 28.1% in Western Europe (Table 2). It is of note that the number of reporting sites in Latin America increased by 71% during this period, which accounts for only a portion of this increase in patients followed. The number of reporting sites in the Middle East slightly decreased, while in Western Europe, the increase in reporting sites matched that of the global increase.
The number of patients identified with specific PI defects in the JMCN over the past 5 years was also compared across nine global regions. The number of patients identified with specific PI defects in Latin America increased by 64%, while increasing by 29.6% in the Middle East, 27.9% in Asia, and 25.5% in Africa (Table 2). Importantly, the number of reporting sites in Asia did not substantially increase, and in Africa, the number of reporting sites slightly decreased.
Classification of PI
In addition to identifying regional trends in patient prevalence, it is important to examine the distribution of patients diagnosed with PI, using the categories defined by the IUIS Expert Committee for the classification of PI. The number of patients in each IUIS category in 2018 was compared in the USA, internationally, and globally. As a percentage of all patients identified with a specific PI defect, predominantly antibody deficiencies were reported by physicians to account for 57% of these patients in the USA, 40% internationally, and 45% globally (Table 3). Combined immunodeficiencies with associated syndromic features was 16% in the USA, 12% internationally, and 13% globally. Notably, unspecified or other deficiencies were reported to account for 10% of these patients in the USA, 17% internationally, and 15% globally.
Regional trends in classification of PI
To further examine the distribution of patients diagnosed with PI, 18 of the most prevalent PI defects were compared across nine global regions. Predominantly antibody deficiencies, including selective IgA deficiency, unspecified hypogammaglobulinemia, and hyper-IgM syndrome, was the most prevalent with 17.5% in the USA, 12.7% internationally, and 14.2% globally (Table 4). Notably, selective IgA deficiency was the most prevalent of these, followed by unspecified hypogammaglobulinemia, and then hyper-IgM syndrome. Common variable immunodeficiency (CVID) showed a prevalence of 15.8% in the USA, 11.3% internationally, and 12.7% globally. It is noteworthy that Canada had 21.1% prevalence for CVID and Australia had 35% prevalence for CVID. The Middle East reported 28.4% familial Mediterranean fever compared to 4.2% globally. Africa reported 5.8% ataxia telangiectasia (A-T) compared to 2.7% globally, and 14.2% “immunodeficiencies affecting cellular and humoral immunity, including SCID” compared to 2.3% globally. The 18 most prevalent PI defects in 2018 were very similar to those in 2013, with only slight variations in order, which could very well be due to changes in classification.
Treatment with IgG
The JMF survey included questions assessing treatment with immunoglobulin therapies, as this information is vital in adequately describing the PI patient population. It should be recognized that many of the centers did not report data for patients receiving Ig therapies, possibly due to local access issues or hospital regulations. Treatment with immunoglobulin therapy by modality in 2018 was compared with that of 2013. There was a 39% overall increase in the number of patients receiving IgG since 2013, according to the physician report (Table 5). Of all patients in the JMCN database diagnosed with a PI defect, 25% are on immunoglobulin replacement therapy. Since 2013, there was an increase of 170% in patients receiving subcutaneous immunoglobulin (SCIG). It is noteworthy that since 2013, there was a 42% increase in the number of patients receiving Intravenous immunoglobulin therapy (IVIG) in the hospital or clinic. Although there was a decrease of 25% in the number of patients receiving IVIG at home since 2013, this was more than offset by the 170% increase in patients receiving SCIG.
Treatment with immunoglobulin therapy by modality was also compared across nine global regions. Western Europe reported 47% of their patients requiring IgG receive SCIG compared to 32% globally (Table 6). In Latin America, 82% of patients receiving IgG are treated in the clinic or hospital compared to 53% globally. In the USA, 27% of patients receiving IgG are treated at home compared to 13% globally.
Additionally, treatment with immunoglobulin therapy in each of nine global regions in 2018 was compared to that of 2013. The number of patients in the JMCN receiving IgG increased across the globe by 39% from 2013 to 2018, despite the overall number of reporting centers only increasing by 12%. Australia and Latin America had such a substantial increase because of the increase in reporting centers (Table 7).
Other treatment modalities
The JMF survey also included questions assessing other treatment by methods such as gene therapy, PEG-ADA, and HSCT, including donor type and stem cell source. There were commensurate increases in patients receiving treatments for PI via these methods as well. The number of patients reported to be receiving these treatments was compared across nine regions globally. HSCT was the most common globally, followed by gene therapy, and then PEG-ADA (Table 8). Notably, Western Europe had the greatest number of patients receiving gene therapy. The number of patients treated with PEG-ADA increased by 47% since 2013.
Stem cell donor type used for patients having received HSCT in 2018 was compared to that of 2013. There was a 113% overall increase in patients treated by HSCT or thymus transplantation since 2013, with the number of patients receiving matched donor transplants increasing by 143%, matched unrelated donor transplants increasing by 119%, mismatched unrelated donor transplants increasing by 114%, and parental haplo transplants increasing by 99% (Table 9). Stem cell donor type used for patients having received HSCT in 2018 was also compared across nine global regions. Matched unrelated donor transplants were the most common globally, followed by matched related donor transplants (Table 10). However, in the Middle East, Africa, and Latin America, matched related donor transplants were the most common. Notably, the number of parental haplo transplants in Western Europe was substantially higher, at 31%, than the other eight regions.
To further examine the treatment modalities utilized, the stem cell source used for patients having received HSCT in 2018 was compared to that of 2013. Since 2013, use of bone marrow as the source of stem cells increased by 147%, while cord blood as the stem cell source increased by 191% (Table 11). There was a 71% overall increase in cord blood transplants in the past 2 years. Stem cell source used for patients having received HSCT was also compared across nine global regions. While there was a 113% increase in the number of patients having received HSCT since 2013, specific stem cell sources varied significantly by region and source (Table 12). Latin America reported 71% of the transplants used bone marrow as the stem cell source, as opposed to 64% globally. The Middle East reported that 29% of the transplants were peripheral stem cells as opposed to 22% globally. Asia reported that 53% of the transplants were cord blood, compared to 14% globally. These large percent increases were due, in part, to sustained programs of newborn screening, especially in the USA, and increasingly other regions of the world. Molecular diagnosis and sequencing also were significant contributing factors. This differential may call for further analysis going forward.
Demographics
Patient demographics, including sex and age, in 2018 were compared with that of 2013. Center Directors reported on 44,582 patients with respect to sex and 39,027 patients with respect to age (Table 13). Male patients accounted for 58% globally, while female patients accounted for 42%. In the USA, 56% of the patients were male, and 44% of patients were female. Globally, 64% of the patients were 19 years of age or younger, while 36% were 20 years of age or older.
Physician reported clinical outcomes
Network Center Directors were asked to examine records of PI patients 1 year before diagnosis and for the year subsequent to diagnosis and then report on outcomes based upon their analysis. Eighty-five centers in the JMCN responded. The average number of episodes decreased for each condition investigated post-diagnosis as compared to 1 year before diagnosis. The number of hospitalization days, visits to the physician and ER, days on antibiotics, and days of school or work missed all decreased post-diagnosis. Early diagnosis resulted in decreased morbidity and mortality.
Additionally, early diagnosis resulted in lower costs post-diagnosis as compared to the year prior to diagnosis, even if regular IgG replacement therapy was required (Table 14). The annual savings to the health care system for each diagnosed patient is $85,882. Even for patients that are diagnosed and treated with IgG, this amount remains at $55,882 saved annually. The cost of the most frequent conditions affecting patients with PI pre- and post-diagnosis and the post-diagnosis average annual savings are shown in Table 14.
Discussion
To our knowledge, this is the most extensive collection of physician-reported prevalence and outcomes for patients with PI around the world. These data reflect an increase in diagnosed patients, as well as those receiving treatment. Importantly, this is despite there having not been a significant net increase in return of survey instruments to the JMF. Nearly 15 years after the initiation of physician education and public awareness activities and the inception of the JMCN, there has been a continued increase, reported by physicians, in the number of patients with PI identified, diagnosed, and treated. Suspected patients are being identified and referred, so that they can receive early and appropriate diagnosis and treatment. The significant increase in patients identified with a PI is most probably due in part to expanding education and awareness initiatives, newborn screening, and the expansion of molecular diagnosis and sequencing. Treatment modalities have been enhanced and refined, in connection with IgG therapy and HSCT intervention. Physician-reported outcomes, pre- and post-diagnosis, have shown substantial differentials reflected by independently documented cost analyses. The rate of patients identified with a specific defect has risen less dramatically in recent years because JMF has expanded in regions in which there is little or no molecular diagnosis and deep sequencing.
Early recognition of PI is essential to avoid associated morbidities and mortality and outcomes for patients with a wide array of diagnoses has improved drastically over the last few decades (such as is clear for CVID and hyper-IgM) [27,28,29]. Additionally, the annual savings to the health care system for each diagnosed patient is calculated to be $85,882. This amount remains substantial for patients that are diagnosed and treated with IgG, at $55,882 annually (when the costs of Ig therapy are removed from any savings). This, taken into account along with the fact that in 2016, four federal agencies, the Environmental Protection Agency, Food and Drug Administration, Department of Transportation, and the US Department of Health and Human Services, estimated the statistical value of one life saved to be $9.7 million [30], emphasizes the importance of early diagnosis, appropriate treatment, and lives saved. The value of statistical life takes into consideration factors that contribute to the society, including productive output, revenue produced, consumer spending, taxes, and reduced health care costs, among other factors. The calculated incremental cost-effective ratio and quality of adjusted life years is $135,714 per year and projects an average life span of 70 years.
Overall, health care spending increased 3.9% over the past 2 years in the USA. Costs were constrained by additional outpatient care, limiting hospital costs. Another significant constraint on costs was that a greater number of Americans were covered under the Affordable Care Act, limiting the number of emergency room visits and hospital stays. Finally, in a study from the National Center for Biotechnology, information dated June 2014, entitled “Economic impact of infections among patients with primary immunodeficiency disease receiving IVIG therapy,” the economic consequences are confirmed within 10% [31].
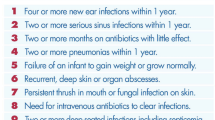
In an effort to promote awareness of PI, facilitate early identification and diagnosis of patients, and benefit from the associated cost-savings, JMF created SPIRIT® (Software for Primary Immunodeficiency Recognition, Intervention, and Tracking) Analyzer, which matches 352 ICD-10 codes to JMF’s 10 warning signs of PI, which can be seen in Figs. 1 and 2, to identify at-risk patients. The software, which can analyze over a million claims per hour, calculates risk points in large existing databases, establishing low-, medium-, and high-risk categories. The software also calculates antibiotic use risk scores identifying frequency and dosage of antibiotics, antifungals, steroids, IVIG, and related treatment modalities. The software includes 17,868 updated National Drug pharmacy and Healthcare Common Procedure codes. Thus, the patient’s total risk score is made up of the ICD-10-related component and antibiotic use-related component. Statistical analysis was conducted using the two-way ANOVA test, producing p values of less than 0.05, indicating that the data results did not occur by chance, and there was a better than 95% probability that the data is valid. The SPIRIT® Analyzer software is distributed to medical providers and health care insurance companies as a public service by JMF. Full implementation and utilization of SPIRIT® allows health care organizations to alert physicians of medium- and high-risk patients with recurring infections and encourages appropriate assessment, ultimately leading to disease prevention, electronic recognition and tracking, significant reduction of health care costs, and improved quality of life for patients, allowing them to lead full and independent lives.
Over the past decade, improvements in diagnostics and implementation of newborn screening programs for SCID have led to a greater understanding of PI and allowed for clearer assessments of prevalence. Simultaneously, advancement in genomic technologies has led to a better understanding of the underlying mechanisms that lead to monogenic defects of the immune system [32]. These advancements and new discoveries will continue to impact the field of immunology, as well as contribute to related fields such as genomics, infectious disease, and oncology [32].
There are many PIs, however, that remain undiscovered. As genomic sequencing technologies advance in concert with ongoing persistence in the biological investigation of the gene candidates additional causative defects will be identified, contributing to an understanding of the mechanisms of diseases of the immune system, as well as basic cellular pathophysiology [32]. It is important that as genetic technologies advance, access to these technologies also broadens in order to reduce inequalities in diagnostics worldwide.
However, as molecular technology continues to significantly advance, deep sequencing including whole genome, whole exome, and next-generation sequencing, is becoming much more routine [33]. The trend toward “personalized medicine” is being driven by increasing numbers of medically actionable genotypes, or DNA variants that confer risk and are treatable. Further advancements and improvements in this new technology, along with greater public acceptance, will lead to the identification of rare genotypes, as well as “immunophenotypic” expansions of known genotypes all with relevant clinical consequences [33]. In the not so distant future, it is possible that newborns will have their entire genomes sequenced at birth, providing risk assessments for a myriad of health conditions, including SCID and other defects of the immune system, along with more common late-onset multifactorial immune disorders. However, since genotypes do not always fully predict phenotype, much more investigation is needed to be able to appropriately position these strategies from an immunological perspective [33].
Currently, over 350 PI defects have been identified [5, 15, 34]. A review of the most recent IUIS Expert Committee Classification of PI found that over 100 new genes were discovered at Jeffrey Modell Centers during the previous 5-year period, through a specific focus on molecular diagnosis, whole genome and exome sequencing, and advanced immunobiological investigation. Jeffrey Modell Centers have also made strides toward novel cures and have reported advances in re-programming SCID mutations in patient hematopoietic stem cells employing CRISPR technology and genome editing [35]. Antiviral immunotherapy, by means of virus specific cytotoxic T cells, is underway at a number of JMF Centers in the network and represents another important novel option in advancing patients to cures [36, 37]. The JMF survey report and resulting database demonstrates substantive numbers of various genotypes and expanding patient diagnosis across established centers. It aims to continue to provide a strong platform for collaboration, contributing to international coordination of studies to promote further gene discovery, of which important recent examples exist [8, 12, 38, 39].
Overall, our findings show that there are important regional differences throughout the network, which likely reflect greater prevalence of specific gene defects based on occurrences such as founder effect and consanguinity [13]. Because of this, awareness campaigns must be targeted to meet the unique needs in each of these diverse geographical regions. Furthermore, it is important to expand on epidemiological and demographic assessments of specific genes, which may lead to more targeted efforts, and lead to tailoring of continuing medical education, with more precise risk categories identified. Finally, the opportunity to engage in targeted education and resourcing, which has likely increased the diagnosis of patients in the Latin American region, is something that must be continued and advanced in order to save lives and empower experts who can make a difference for those who might otherwise suffer from chronic and symptomatic immunodeficiency.
Summary
The JMCN continues to materially impact the field of immunology worldwide. The network serves as a unique resource, creating greater awareness of PIs, conducting physician and patient education, and facilitating access to diagnosis and treatment. The network infrastructure is in place, established, and matured. This platform will allow the PI community to leverage research advances, earlier diagnosis, improved treatments, and clinical care through increased connectivity so that patients can experience healthier outcomes and a better quality of life.
Abbreviations
- PI:
-
Primary immunodeficiencies
- JMF:
-
Jeffrey Modell Foundation
- JMCN:
-
Jeffrey Modell Centers Network
- SCID:
-
Severe combined immunodeficiency
- IUIS:
-
International Union of Immunological Societies
- HSCT:
-
Hematopoietic stem cell transplantation
- CVID:
-
Common variable immunodeficiency
- IG:
-
Immunoglobulin therapy
- IVIG:
-
Intravenous immunoglobulin therapy
- SCIG:
-
Subcutaneous immunoglobulin therapy
- PEG-ADA:
-
Polyethylene glycol-conjugated adenosine deaminase
- BM:
-
Bone marrow
- PBSC:
-
Peripheral blood stem cell
- Cord:
-
Cord blood
- MUD:
-
Matched unrelated donor
- mMUD:
-
Mismatched unrelated donor
- MRD:
-
Matched related donor
- NBS:
-
Newborn screening
- HCUP:
-
Hospital Cost and Utilization Project
- AHRQ:
-
Agency for Healthcare Research and Quality
- HCCI:
-
Health Care Cost Institute
References
Modell V. The impact of physician education and public awareness on early diagnosis of primary immunodeficiencies. Immunol Res. 2007;38:43–7.
Modell F. Immunology today and new discoveries: building upon legacies of Dr. Robert a. Good. Immunol Res. 2007;38:48–50.
Cunningham-Rundles C, Ponda PP. Molecular defects in T- and B-cell primary immunodeficiency diseases. Nat Rev Immunol. 2005;5:880–92.
Cooper MA, Pommering TL, Koranyi K. Primary immunodeficiencies. Am Fam Physician. 2003;68:2001–8.
Bousfiha A, Jeddane L, Al-Herz W, Ailal F, Casanova JL, Chatila T, et al. The 2015 IUIS phenotypic classification for primary immunodeficiencies. J Clin Immunol. 2015;35:727–38. https://doi.org/10.1007/s10875-015-0198-5.
Bousfiha AA, Jeddane L, Ailal F, Benhsaien I, Mahlaoui N, Casanova JL, et al. Primary immunodeficiency diseases worldwide: more common than generally thought. J Clin Immunol. 2013;33(1):1–7.
Boyle JM, Buckley RH. Population prevalence of diagnosed primary immunodeficiency diseases in the United States. J Clin Immunol. 2007;27(5):497–502.
Stray-Pedersen A, Sorte HS, Samarakoon P, Gambin T, Chinn IK, Coban Akdemir ZH, et al. Primary immunodeficiency diseases: genomic approaches delineate heterogeneous Mendelian disorders. J Allergy Clin Immunol. 2017;139(1):232–45. https://doi.org/10.1016/j.jaci.2016.05.042.
Rider NL, Kutac C, Hajjar J, Scalchunes C, Seeborg FO, Boyle M, et al. Health-related quality of life in adult patients with common variable immunodeficiency disorders and impact of treatment. J Clin Immunol. 2017;37(5):461–75. https://doi.org/10.1007/s10875-017-0404-8.
Quinti I, Di Pietro C, Martini H, Pesce AM, Lombardi F, Baumghartner M, et al. Health related quality of life in common variable immunodeficiency. Yonsei Med J. 2012;53(3):603–10. https://doi.org/10.3349/ymj.2012.53.3.603.
Casanova JL, Abel L, Quintana-Murci L. Immunology taught by human genetics. Cold Spring Harb Symp Quant Biol. 2013;78:157–72. https://doi.org/10.1101/sqb.2013.78.019968.
Meyts I, Bosch B, Bolze A, Boisson B, Itan Y, Belkadi A, et al. Exome and genome sequencing for inborn errors of immunity. J Allergy Clin Immunol. 2016;138(4):957–69. https://doi.org/10.1016/j.jaci.2016.08.003.
Modell V, Gee B, Lewis DB, Orange JS, Roifman CM, Routes JM, et al. Global study of primary immunodeficiency diseases (PI)—diagnosis, treatment, and economic impact: an updated report from the Jeffrey Modell Foundation. Immunol Res. 2011;51:61–70.
Modell F, Puente D, Modell V. From genotype to phenotype. Further studies measuring the impact of a physician education and public awareness campaign on early diagnosis and management of primary immunodeficiencies. Immunol Res. 2009;44(1–3):132–49.
Picard C, Gaspar BH, Al-Herz W, Bousfiha A, Casanova JL, Chatila T, et al. International Union of Immunological Societies: 2017 primary immunodeficiency diseases committee report on inborn errors of immunity. J Clin Immunol. 2018;38(1):96–128. https://doi.org/10.1007/s10875-017-0464-9.
Picard C, Al-Herz W, Bousfiha A, Casanova JL, Chatila T, Conley ME, et al. Primary immunodeficiency diseases: an update on the classification from the international union of immunological societies expert committee for primary immunodeficiency 2015. J Clin Immunol. 2015;35(8):696–726. https://doi.org/10.1007/s10875-015-0201-1.
Agency for Healthcare Research and Quality. http://www.hcup.ahrq.gov (2015).
Aetna Member Navigator. http://www.aetna.com (2015).
Bundorf KM, Royalty A, Baker LC. Health care cost growth among the privately insured. Health Aff. 2009;28(5):1294–304.
Truven Health Analytics. Healthcare Spending Index for Employer-Sponsored Insurance. 2014.
Centers for Medicare and Medicaid Services. Berenson-eggers type of service (BETOS). 2015. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/BETOS.html.
Centers for Medicare and Medicaid Services. Medicare current beneficiary survey (MCBS). 2015. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/index.html?redirect=/mcbs.
Congressional Budget Office. Factors underlying the growth in medicare’s spending for physicians’ services. 2007. Retrieved 28 Apr 2010, from http://www.cbo.gov/ftpdocs/81xx/doc8193/06-06-MedicareSpending.pdf.
Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 2013 current population survey, vol 390. EBRI (Employee Benefit Research Institute) Issue Brief No. 390, September 2013, Washington, DC; 2013. p. 1–36.
Chan K, Davis J, Pai SY, Bonilla FA, Puck JM, Apkon M. A Markov model to analyze cost-effectiveness of screening for severe combined immunodeficiency (SCID). Mol Genet Metab. 2011;104(3):383–9.
Health Care Cost Institute (HCCI) 2014 Health Care Cost and Utilization Report. 2015. http://www.healthcostinstitute.org/files/2014%20HCCUR%2010.29.15.pdf.
Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: clinical and immunological features of 248 patients. Clin Immunol. 1999;92(1):34–48.
Chapel H, Cunningham-Rundles C. Update in understanding common variable immunodeficiency disorders (CVIDs) and the management of patients with these conditions. Br J Haematol. 2009;145(6):709–27. https://doi.org/10.1111/j.1365-2141.2009.07669.x.
de la Morena MT, Leonard D, Torgerson TR, Cabral-Marques O, Slatter M, Aghamohammadi A, et al. Long-term outcomes of 176 patients with X-linked hyper-IgM syndrome treated with or without hematopoietic cell transplantation. J Allergy Clin Immunol. 2017;139(4):1282–92. https://doi.org/10.1016/j.jaci.2016.07.039.
Merrill D. No one values your life more than the federal government. Bloomberg. October 19, 2017. https://www.bloomberg.com/graphics/2017-value-of-life/.
Menzin J, Sussman M, Munsell M, Zbrozek A. Economic impact of infections among patients with primary immunodeficiency disease receiving IVIG therapy. Clinicoecon Outcomes Res. 2014;6:297–302.
Milner JD, Holland SM. The cup runneth over: lessons from the ever-expanding pool of primary immunodeficiency diseases. Immunology. 2013;13:635–48.
Puck J. Laboratory Technology for Population-based Screening for SCID in neonates: the winner is T-cell receptor excision circles (TRECs). J Allergy Clin Immunol. 2012;129(3):607–16. Published online 2012 Jan 29. https://doi.org/10.1016/j.jaci.2012.01.032.
Bharat ST, Alizadehfar R, Desrosiers M, Shuster J, Pant N, Tsoukasa CM. Adult primary immune deficiency: what are we missing? Am J Med. 2012;125(8):779–86.
Pollack A. Jennifer Doudna, a Pioneer Who Helped Simplify Genome Editing. Profiles in Science, NY Times. 2015. http://www.nytimes.com/2015/05/12/science/jennifer-doudna-crispr-cas9-genetic-engineering.html?_r=0. Accessed 13 May 2015.
Keller MD, Bollard CM, Hanley PJ, McCormack S, Heimall J, Bunin N, et al. Viral-specific T lymphocytes for treatment of viral infections in primary immunodeficiency. Biol Blood Marrow Trans. 2015;21(2):S229–30.
Naik S, Nicholas SK, Martinez CA, Leen AM, Hanley PJ, Gottschalk SM, et al. Adoptive immunotherapy for primary immunodeficiency disorders with virus-specific T lymphocytes. J Allergy Clin Immunol. 2016 May;137(5):1498–1505.e1. https://doi.org/10.1016/j.jaci.2015.12.1311.
Maffucci P, Filion CA, Boisson B, Itan Y, Shang L, Casanova JL, et al. Genetic diagnosis using whole exome sequencing in common variable immunodeficiency. Front Immunol. 2016;7:220. https://doi.org/10.3389/fimmu.2016.00220. eCollection 2016
Abolhassani H, Chou J, Bainter W, Platt CD, Tavassoli M, Momen T, et al. Clinical, immunologic, and genetic spectrum of 696 patients with combined immunodeficiency. J Allergy Clin Immunol. 2017;141:1450–8. https://doi.org/10.1016/j.jaci.2017.06.049.
Acknowledgements
The authors thank the Jeffrey Modell Center Directors for their generous support and continued commitment to the Jeffrey Modell Foundation and the global primary immunodeficiency communities. We thank Dr. Chaim Roifman, Founder, and Director of the Jeffrey Modell Centers Network, for his vision, and Dr. Jordan Orange for his expertise and guidance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest except for the following:
Jordan Orange, MD, PhD: Shire Consultant, Grifols Consultant, CSL consultant, received speaking honoraria from Shire, ADMA Scientific Advisory Board, author of the chapter on IVIG in Up to Date for which he receives royalties.
Rights and permissions
About this article
Cite this article
Modell, V., Orange, J.S., Quinn, J. et al. Global report on primary immunodeficiencies: 2018 update from the Jeffrey Modell Centers Network on disease classification, regional trends, treatment modalities, and physician reported outcomes. Immunol Res 66, 367–380 (2018). https://doi.org/10.1007/s12026-018-8996-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-018-8996-5