Abstract
Autoimmune thyroid disease (AITD), known as the most common organ-specific autoimmune disorder, is frequently accompanied by other organ and non-organ-specific autoimmune diseases, including rheumatoid arthritis (RA). Although the exact pathogenic mechanisms of the coexistence of autoimmune disorders are still not completely defined, genetics, immune defects, hormones and environmental factors may play key roles in polyautoimmunity. In this review, the prevalence of AITD and antithyroid autoantibodies in RA patients and rheumatic manifestations in association with thyroid autoimmunity are discussed. Finally, we review the role of genetics in the association of both AITD and RA, especially CTLA-4 and PTPN22 polymorphisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autoimmune thyroid disease (AITD) is the most prevalent organ-specific autoimmune disease characterized by the presence of antibodies against thyroid-specific components such as thyroglobulin (aTG), thyroid peroxidase (aTPO), thyrotropin receptor antigen (aTSHr) and sodium iodine symporter (NIS). Currently, AITDs, namely Graves’ disease (GD) and Hashimoto’s thyroiditis (HT), are the most frequent causes of goiters in countries without iodine deficiency with a prevalence of up to 5 % in the general population. However, the prevalence of subclinical disease manifested by the production of antithyroid antibodies (ATA) without clinical manifestation may be even higher [1]. AITD is the result of a complex interaction between genetics and environmental factors [2]. Susceptibility to the production of autoantibodies and thyroiditis is under independent genetic control, and environmental factors can induce thyroid autoimmunity in genetically susceptible strains of animals (reviewed in [3, 4]).
There is evidence that AITD is frequently accompanied by other organ-specific as well as non-organ-specific autoimmune disorders, because there is sharing of genetic and, possibly, environmental factors. These associations are well recognized in the autoimmune polyglandular syndrome, especially type 2, and also in around 4 % of type 1 patients. Clinical recommendations to perform thyroid autoimmunity screening have been made because of its benefit in patients with Addison’s disease, lymphocytic hypophysitis, pernicious anemia, primary biliary cirrhosis, celiac disease and myasthenia gravis [5, 6].
Rheumatoid arthritis (RA) is a chronic, progressive autoimmune systemic disease leading to joint destruction and organ impairment and subsequently leading to increased morbidity and mortality. The disease is about three times more frequent in women than in men, with a prevalence of 0.5–1.0 % in industrialized countries. Patients with RA commonly present a clinical picture of other autoimmune disorders, including AITD. Both disorders are associated because of similar pathogenic mechanisms and genetic susceptibility [7, 8].
The association of AITD with non-organ-specific autoimmune disorders, particularly RA, systemic lupus erythematosus (SLE) and primary Sjögren’s syndrome, has been demonstrated in many studies. Several authors documented a higher prevalence of non-organ-specific autoantibodies, especially antinuclear antibodies (ANA), in patients with AITD, ranging from 9 to 37 % [9, 10]. Unfortunately, their clinical significance is still uncertain [11–13]. Oppositely, the high prevalence of ATA as well as AITD in patients with autoimmune rheumatic disease, particularly RA, is also well documented in recent studies despite the fact that the pathogenic mechanisms for the coexistence of autoimmune disorders are still not completely recognized (for a review, see [14] ).
For several decades, an increased prevalence of AITD in patients suffering from RA has been documented. In addition, several authors have described rheumatologic and non-rheumatologic manifestations of AITD. Within these manifestations, it is noteworthy that the most common symptoms are polyarthralgia and unclassified arthritis, which are also the main features of RA [15, 16]. Several studies demonstrated a higher prevalence of ATA in RA patients and their families and, in contrast, a higher prevalence of RA in AITD patients and their families [17, 18].
Although different series have reported an increased prevalence of AITD in RA, there is still controversy between the presence of ATA and thyroid function. Atzeni et al. [10] have reported a 37.1 % prevalence of aTPO positivity and 22.9 % aTG positivity; hypothyroidism occurred in only 2.8 % of RA patients. A former study of Shiroky et al. [19] found a threefold higher prevalence of thyroid disease in adult women with RA, as compared with controls of the same demographic region. In general, positivity for the ATA has been detected in 11 % of patients with RA, ranging from 2 to 32 % in different series [12, 20, 21]. In a Colombian cohort of 800 patients with RA, the presence of antibodies was 37.8 % for aTPO and 20.8 % for aTG; polyautoimmunity was present in 14.1 % of patients [8].
Several studies reported the prevalence of autoantibodies against thyroid antigens. The prevalence of aTG ranged from 5 % in men from the UK and 6 %, regardless of gender, in Egypt and 31 % in RA patients from Japan. The prevalence of aTPO was within the range of 5 % in Egypt to 37 % in Italy. There is a worldwide prevalence of AITD in RA that varies considerably, ranging from 0.5 % in Morocco to 27 % in Slovakia. ATA prevalence ranges from 6 to 31 % for aTG, 5–37 % for aTPO and from 10.4–32 % for the presence of either of the two (reviewed in [8, 22] ).
This high prevalence variability may be explained by several factors. Firstly, there were no universal criteria for diagnosing AITD; secondly, different methods for assessment of ATA with different normal ranges were used in these studies. In addition, there is still no consensus on the normal upper limit of TSH levels and therefore for definition of hypothyroidism. A third explanation for a wide range of AITD prevalence involves iodine intake. It is well known that iodine has a particular property of inducing thyroid autoimmunity and, if increased, it could participate on the higher prevalence of AITD in some countries.
Oppositely, some authors have also studied the prevalence of systemic autoimmune disorders in AITD patients. The frequency of another autoimmune disease in a study from Germany was 9.67 % for GD and 14.3 % for HT. RA was the most common coexisting autoimmune disorder in this study [18].
The relationship between ATA and RA activity has also been extensively studied. Some of the studies did not find a relationship between the presence of ATA and anti-citrullinated peptide antibodies (ACPA) [23]. However, others found that women with RA and clinical hypothyroidism had a higher Disease Activity Score (DAS) 28 compared to those without clinical hypothyroidism [24]; additionally, thyroid dysfunction was associated with increased incidence and mean duration of morning stiffness [25].
In a recent study by Koszarny et al. [26], 75 consecutive hospitalized patients with RA were studied for the presence of ATA. ATA were positive in 13.3 % of patients (aTPO in 9.3 %, aTG in 8 %, and both aTPO and aTG in 4 %). Significant positive correlations were observed between aTPO and DAS28 score, aTG and erythrocyte sedimentation rate, and between aTG and C-reactive protein level. There were significant differences in the mean DAS28 between aTPO-positive and aTPO-negative groups and also between aTG-positive and aTG-negative groups. These results suggest that RA activity may be associated with the presence of ATA. This finding could also be useful in the clinical evaluation of RA patients.
Rheumatic manifestations in AITD
A variety of rheumatic manifestations have been described in association with autoimmune thyroiditis. In the past, most of these manifestations were attributed to an underlying thyroid dysfunction, particularly hypothyroidism. However, mechanisms involved in autoimmunity seem to be amenable rather than a direct action of thyroid hormones for rheumatic manifestations. This is supported by evidence that some rheumatic manifestations may occur even in euthyroid patients or that they are more frequent in hypothyroid patients with autoimmune thyroiditis than in those without the disease [27].
Patients with AITD may be affected by polyarthralgias, even in the absence of hypothyroidism. In case of simultaneous hypothyroidism, replacement therapy with levothyroxine may induce a progressive but gradual improvement in symptoms.
Rheumatic manifestations in AITD patients may involve a variety organs and tissues, even if the most representative are symptoms are those affecting the joints, muscles and skin. In a study of Punzi et al. [28], the most common rheumatic manifestations in AITD were polyarthralgias, unclassified arthritis, sicca syndrome without Sjögren’s syndrome, and muscle pain or weakness.
There is also evidence that AITD manifestations independent of thyroid function may resemble those presented by RA. Some symptoms are exacerbated when both diseases co-occur.
Current data indicate that the presence of arthritis in patients with AITD with normal thyroid function is now being increasingly recognized. There is considerable evidence to suggest that AITD is highly associated with fibromyalgia syndrome. A recently published study evaluated the presence of rheumatic manifestations of euthyroid patients with AITD but without a well-defined connective tissue disease. Forty-six consecutive patients with aTPO and/or aTG antibodies positivity, along with normal thyroid function in the absence of a well-defined connective tissue disease, were included in a case-cohort study. Arthralgias were a presenting complaint in 98 % of patients. Fibromyalgia syndrome was found in 59 % of patients. Raynaud’s phenomenon occurred in 28 % and sicca symptoms in 26 % of patients. Two patients had seronegative arthritis resembling RA. Arthritis was radiographically present in 88 % of patients, with the spine affected in 45 % of this subset. Rheumatic manifestations frequently occur in patients with chronic lymphocytic thyroiditis in the absence of overt thyroid dysfunction and mimic the presentation of the well-defined connective tissue diseases [29, 30].
Endothelial dysfunction independent on lipid profile has also been demonstrated by some authors. In a study from Colombia, cardiovascular disease (CVD) was the sole extraarticular manifestation. Results of this study are in agreement with others confirming that the presence of hypothyroidism, including HT, is a risk factor for CVD in patients with RA with hazard ratio of 2.7 (95 % CI 1.1–6.3) [31, 32].
Pathogenic mechanisms of autoimmunity in AITD and RA
Although the exact pathogenic mechanisms of autoimmune disorders are still not sufficiently defined, most of factors involved in the development of autoimmunity can be characterized as follows:
-
genetic
-
environmental—infectious agents, vaccines, smoking, drugs, stress factors, endocrine disruptors and others [33, 34].
Recent advances in our understanding of genetic–epigenetic interactions have uncovered new mechanisms involved in the etiopathogenesis of complex autoimmune diseases.
Epidemiological data point to an interaction between genetic susceptibility and environmental triggers as the key factor leading to the breakdown of tolerance and to the development of autoimmune disease. Among the shared susceptibility genes involved in the pathogenesis of AITD, HLA-DRβ1-Arg74 (human leukocyte antigen DR containing an arginine at position beta 74) confers the strongest risk. Most genes are common for both GD and HT, although several are unique to one or the other. The TSH receptor gene, CD40 and CD25 have been demonstrated to be strongly associated with GD, whereas 12q (B cell translocation gene 1, BTG1) is related to HT. Besides HLA-DRβ1-Arg74, data demonstrating thyroglobulin (Tg) as a major susceptibility gene supports a key role for Tg in triggering AITD [35, 36]. In addition to HLA-DR, other genes involved in T cell activation and regulation are associated with AITD: cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and protein tyrosine phosphatase non-receptor type 22 (PTPN22). The CD25 gene has been reported in association with GD and some polymorphisms of CD25 reducing the function of T regulatory cells may promote autoimmunity development [37, 38].
The genetic variants mentioned above provide a primary risk for AITD and its manifestations. However, this primary risk can interact with environmental factors (diet, lifestyle, infection, iodine exposure, etc.), representing an epigenetic modulation. Epigenetic modulation is emerging as a major mechanism by which environmental factors interact with AITD susceptibility genes [36, 39].
It is also well established that genetic and environmental factors participate in the mechanisms of RA pathogenesis. In the past, many studies demonstrated that patients with RA tend to share the same HLA genes and serotyping experiments subsequently identified an increased number of RA patients who were positive for the HLA allele HLA-DRw4 as compared to healthy controls. Later on, further characterization of the HLA locus identified multiple risk alleles within HLA-DRB+, leading to the “shared epitope” hypothesis (for a review, see [40]).
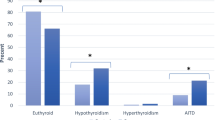
Outside the MHC region, candidate gene studies performed prior to 2007 had identified only a handful of RA susceptibility loci, including PTPN22, STAT4 (signal transducer and activator of transcription 4), PADI4 (peptidyl arginine deiminase, type IV), TRAF1/C5 (TNF receptor-associated Factor 1/complement component 5) and CTLA-4. Other polymorphisms seem to be responsible for more aggressive disease phenotypes, such as those located at tumor necrosis factor (TNF), interleukin (IL)-1, IL-6, IL-4, IL-5, osteopontin and perforin 1 (PRF1) [41–43]. However, the genetic background of RA still remains to be clearly depicted, and the efforts in the post-genomic era can bring to an estimation of the real likelihood of the genetic effect on RA. Finally, the discovery of new genes associated with the disease can be relevant in searching for potential biomarkers that can be useful in diagnosis and treatment. By 2007, genome wide association studies (GWAS) discovered around 60 risk loci for RA in Asian and European populations [44–47]. Figure 1 shows susceptibility genes for AITD and RA. Some genes are common for both AITD and RA, although several are unique to AITD or to RA. Recent GWA studies demonstrate that additional genes are likely involved.
Possible susceptibility genes for AITD and RA. Polymorphisms of HLA-DR B1, CTLA4, PTPN22, FCRL3 and IL2RA are common for both AITD and RA, whereas some are specific for one or for the other disease. TSHR thyroid-stimulating hormone receptor, Tg thyroglobulin, ARID5B AT-rich interactive domain-containing protein 5B, BTG1 B cell translocation gene 1, HLA-DR-B1 human leukocyte antigen DR B1, CTLA-4 cytotoxic T-lymphocyte-associated antigen 4, PTPN22 protein tyrosine phosphatase non-receptor type 22, FCRL3 Fc receptor-like 3, IL2RA interleukin 2 receptor subunit alpha, PADI4 post-translational conversion of arginine residues to citrulline. TRAF1 TNF receptor-associated factor 1, CCRG chemokine receptor expressed by CD4+, TNFAIP3 TNF-induced protein 3
The role of CTLA-4
CTLA-4 is a member of the immunoglobulin superfamily, and it is a costimulatory molecule expressed by activated T cells. Simultaneously, CTLA-4 is a structural homolog of CD28 but plays a negative regulatory role in T cell response, i.e., suppression of immune response [48].
The human CTLA-4 gene is located on chromosome 2q33 and encodes the CTLA-4 molecule, which is involved in the control of T cell proliferation and accumulation of IL-2. It mediates T cell apoptosis by binding B7 molecules on antigen-presenting cells constituting the B7/CD28-CTLA-4 costimulatory pathway of T cell activation. Thus, the CTLA-4 gene is a strong candidate for susceptibility to T cell-mediated autoimmune diseases. CTLA-4 gene polymorphisms have been shown to be associated with many autoimmune diseases. Three single nucleotide polymorphisms (SNPs) in the CTLA-4 gene, such as C318T, A49G and C60T, have been demonstrated to be associated with diabetes mellitus type 1, RA, SLE, celiac disease, multiple sclerosis, as well as AITD. However, the results are inconsistent in different ethnic populations [49–51].
To assess the relations of the GG genotype or G allele of the A49G polymorphism in various ethnic cohorts with RA, Han et al. [52] performed a metaanalysis. The results of this study suggest that CTLA-4 exon 1 49G allele is not a risk factor for RA in Europeans but might play role in RA susceptibility for Asians. Regarding the susceptibility to AITD development, many studies confirmed the association between the promoter, exon 1 and 3′untranslated region of CTLA-4 gene polymorphisms and AITD, including GD and HT. In the study of Zaletel et al. [53], the authors provide evidence that CTLA-4 A49G exon 1 polymorphism is associated with ATA status in patients with HT. There are few reports comparing the frequency of the GG genotype of the A49G polymorphism of the CTLA-4 gene in patients with both RA and HT to the frequency of this genotype in controls. In the study of Vaidya et al. [54], an association was found between the G allele and RA, but the authors noted that this fact was largely explained by individuals with coexisting autoimmune endocrinopathies. In this study, the frequency of G allele in CTLA-4 A49G polymorphism was significantly increased in probands with early RA compared to controls. In Slovak study, the prevalence of 49GG genotype and G allele in RA patients was not significantly higher in comparison with controls (10.53 vs. 9.8 %, OR 1.39 and 39.47 vs. 34.31 % OR 1.25) and the frequency of the GG genotype was slightly but not significantly higher in patients with HT when compared to the control group (19.3 vs. 9.8 %, OR 2.27, p = 0.17). However, the frequency of the GG genotype and G allele in patients with both RA and HT was significantly higher than that observed in the control group (29.41 9.8 %, OR 4.49, p = 0.02 and 51.47 vs. 34.31 %, OR 2.02, p = 0.03). We concluded that the prevalence of the GG genotype of CTLA-4 A49G gene polymorphism in patients with RA is not significantly higher in comparison with the control group. However, RA patients carrying the GG genotype may be susceptible to developing HT [55].
The role of PTPN22
The most studied polymorphism in RA to date is PTPN22 non-synonymous Arg620Trp SNP, rs2476601. The PTPN22 gene encodes the lymphoid tyrosine phosphatase protein that is a negative regulator of T cell receptor signaling, and some of its polymorphisms have been found to be associated with AITD as well as other autoimmune diseases [56, 57]. Polymorphisms in PTPN22 are associated with several autoimmune diseases, such as SLE, RA, AITD and type 1 diabetes mellitus [58].
PTPN22 is a tyrosine phosphatase and functions as a damper of TCR signals. A C-to-T SNP located at position 1858 of human PTPN22 cDNA, which converts an arginine (R620) to tryptophan (W620), confers the highest risk of RA among non-HLA genetic variations that are known to be associated with this disease. The effect of the R-to-W conversion on the phosphatase activity of PTPN22 protein and the impact of the minor T allele of the C1858T SNP on the activation of T cells has remained controversial. In addition, how the overall activity of PTPN22 is regulated and how the R-to-W conversion contributes to RA is still poorly understood. More importantly, the level of PTPN22.6, the alternative splice form of human PTPN22, in peripheral blood correlates with disease activity of RA suggesting that PTPN22.6 could be a novel biomarker of RA [59].
Many studies evaluated the possible association of PTPN22 polymorphisms with RA and/or AITD. One of them showed that the R620W PTPN22 polymorphism appears to be a risk factor for concurrent AITD and SLE, but it has not been demonstrated for both AITD and RA. Another polymorphism of PTPN22, i.e., C1858T, was demonstrated to be associated with RA susceptibility in different ethnic groups, especially in Europeans, and the PTPN22 C1858T polymorphism T allele was significantly more prevalent in RF-positive patients than in RF-negative patients [60, 61].
Some meta-analytic studies confirmed that both smoking and the PTPN22 risk allele are associated with the risk of ACPA positivity. There was insufficient evidence to establish a relationship in either direction between PTPN22 and smoking with erosive damage, despite evidence that ACPA positivity is associated with erosive damage [62]. Nevertheless, the role of PTPN22 polymorphisms in concurrent presence of both disorders is still controversial and requires further studies.
Biological treatment of RA and its influence on thyroid autoimmunity
Currently, little data exist that indicate the influence of anti-TNF-alpha therapy on thyroid autoimmunity. Caramaschi et al. [63] did not observe any cases of new autoimmune disorder onset in patients with RA on infliximab therapy; additionally, ATA were found in only a few patients without clinical symptoms of AITD. In another study, aTPO levels in patients receiving anti-TNF treatment were high in a significantly lower number of patients as compared to a group of patients without anti-TNF-alpha treatment [64]. On the other end of the spectrum, in a study of Elkayam et al. [65], treatment with infliximab was found to be associated with the appearance of ANA. Results of an experimental study of Chen et al. [66] suggest that anti-TNF-alpha may regulate expression of proinflammatory cytokines and apoptosis in the thyroid, resulting in less inflammation, earlier resolution and reduced fibrosis. Whether anti-TNF-alpha therapy in RA patients may markedly improve levels of ATA as well as thyroid autoimmunity development is not yet clear and additional studies are suggested.
Conclusion
Although the association of AITD with RA has been confirmed by many studies and evaluation of thyroid autoimmunity in patients with RA is generally recommended, there are still unresolved questions concerning the genetic basis and potential epigenetic modulations of this association. Further studies, especially GWAS, are needed to answer these questions.
References
Weetman AP. Autoimmune thyroid disease. In: DeGroot LJ, Jameson JL, editors. Endocrinology, 5th Edition, volume 2. Philadelphia: W.B. Saunders comp; 2006. p. 1979–1993.
Iddah MA, Macharia BN. Autoimmune thyroid disorders. ISRN Endocrinol. 2013. doi:10.1155/2013/509764.
Rose NR. The genetics of autoimmune thyroiditis: the first decade. J Autoimmun. 2011;37:88–94.
Weetman AP. The immunopathogenesis of chronic autoimmune thyroiditis one century after hashimoto. Eur Thyroid J. 2012;1:243–50.
Weetman AP. Non-thyroid autoantibodies in thyroid disease. Best Pract Res Clin Endocrinol Metab. 2005;19:17–32.
Weetman AP. Diseases associated with thyroid autoimmunity: explanations for the expanding spectrum. Clin Endocrinol (Oxf). 2011;74:411–8.
Puttevils D, DeVusser P, Geusens P, Dens J. Increased cardiovascular risk in patients with rheumatoid arthritis: an overview. Acta Cardiol. 2014;69:111–8.
Roldán JC, Amaya-Amaya J, Castellanos-de la Hoz J, Girald-Villamil J, Montoya-Ortiz G, Cruz-Tapias P, Rojas-Villarraga A, Mantilla RD, Anaya JM. Autoimmune thyroid disease in rheumatoid arthritis: a global perspective. Arthritis. 2012. doi:10.1155/2012/864907.
Soy M, Guldiken S, Arikan E, Altun BU, Turgul A. Frequency of rheumatic diseases in patients with autoimmune thyroid disease. Rheumatol Int. 2007;27:575–7.
Atzeni F, Doria A, Ghirardello A, Turiel M, Batticciotto A, Carrabba M, Sarzi-Puttini P. Anti-thyroid antibodies and thyroid dysfunction in rheumatoid arthritis: prevalence and clinical value. Autoimmunity. 2008;41:111–5.
Tektonidou MG, Anapliotou M, Vlachoyiannopoulos P, Moutsopoulos HM. Presence of systemic autoimmune disorders in patients with autoimmune thyroid disease. Ann Rheum Dis. 2004;63:1159–61.
Lazúrová I, Benhatchi K, Rovenský J, Kozáková D, Wagnerová H, Tajtáková M, Shoenfeld Y, Macejova Z. Autoimmune thyroid disease and autoimmune rheumatic disorders: a two sided analysis. Ann N Y Acad Sci. 2009;1173:211–6.
Biró E, Szekanecz Z, Czirják L, Dankó K, Kiss E, Szabó NA, Szucs G, Zeher M, Bodolay E, Szegedi G, Bakó G. Association of systemic and thyroid autoimmune disease. Clin Rheumatol. 2006;25:240–5.
Lazurova I, Benhatchi K. Autoimmune thyroid diseases and non organ specific autoimmunity. Pol Arch Med Wewn. 2012;122:55–9.
Innocencio RM, Romaldini JH, Ward LS. High prevalence of thyroid autoantibodies in systemic sclerosis and rheumatoid arthritis but not in the antiphospholipid syndrome. Clin Rheumatol. 2003;22:494.
Punzi L, Betterle C. Chronic autoimmune thyroiditis and rheumatic manifestations. Joint Bone Spine. 2004;71:275–83.
Mosca M, Carli L, d’Ascanio A, Tani C, Talarico R, Baldini C, Bazzichi L, Tavoni A, Migliorini P, Bombardieri S. Occurrence of organ-specific and systemic autoimmune diseases among the first- and second-degree relatives of Caucasian patients with connective tissue diseases: report of data obtained through direct patient interviews. Clin Rheumatol. 2008;27:1045–8.
Boelaert K, Newby PR, Simmonds MJ, Holder RL, Carr-Smith JD, Heward JM, Manji N, Allahabadia A, Armitage M, Chatterjee KV, Lazarus JH, Pearce SH, Vaidya B, Gough SC, Franklyn JA. Prevalence and relative risk of other autoimmune diseases in subjects with autoimmune thyroid disease. Am J Med. 2010;123:1–9.
Shiroky JB, Cohen M, Ballachey ML, Neville C. Thyroid dysfunction in rheumatoid arthritis: a controlled prospective survey. Ann Rheum Dis. 1993;52:454–6.
Innocencio RM, Romaldini JH, Ward LS. Thyroid autoantibodies in autoimmune diseases. Medicina (B Aires). 2004;64:227–30.
Chan AT, Al-Saffar Z, Bucknall RC. Thyroid disease in systemic lupus erythematosus and rheumatoid arthritis. Rheumatology (Oxford). 2001;40:353–4.
Gonçalves FT, Feibelmann TCM, Ranza R, Daud MS, Taliberti BHB, Pinto RMC, Jorge PT. Autoimmune thyroiditis and rheumatoid arthritis: is there really an association? Endocrinologist. 2009;19:31–4.
Charles PJ, Plant D, Chowdhury W, Worthington J, Venables P. Antibodies to thyroglobulin and thyroid peroxidase in rheumatoid arthritis: environmental and genetic associations. Ann Rheum Dis. 2011;70:A88–9.
Cojocaru-Gofita IR, Ciurea P, Rosu A, Musetescu AE, Vreju F, Barbulescu A. Hypothyroidism-risk factor for treatment resistent, aggressive rheumatoid arthritis onset. Scand J Rheumatol. 2010;39:29.
Delamere JP, Scott DL, Felix-Davies DD. Thyroid dysfunction and rheumatic diseases. J R Soc Med. 1982;13:81–2.
Koszarny A, Majdan M, Suszek D, Wielosz E, Dryglewska M. Relationship between rheumatoid arthritis activity and antithyroid antibodies. Pol Arch Med Wewn. 2013;123:394–9.
Tagoe CE, Zezon A, Khattri S, Castellanos P. Rheumatic manifestations of euthyroid, anti-thyroid antibody-positive patients. Rheumatol Int. 2013;33:1745–1752.
Punzi L, Sfriso P, Pianon M, Schiavon F, Ramonda R, Cozzi F, Todesco S. Clinical manifestations and outcome of polyarthralgia associated with chronic lymphocytic thyroiditis. Semin Arthritis Rheum. 2002;32:51–5.
Tagoe CE, Zezon A, Khattri S. Rheumatic manifestations of autoimmune thyroid disease: the other autoimmune disease. J Rheumatol. 2012;39:1125–9.
Ahmad J, Tagoe CE. Fibromyalgia and chronic widespread pain in autoimmune thyroid disease. Clin Rheumatol. 2014;33:885–91.
McCoy SS, Crowson CS, Gabriel SE, Matteson EL. Hypothyroidism as a risk factors for development of cardiovascular disease in patients with rheumatoid arthritis. J Rheumatol. 2012;39:954–8.
Raterman HG, van Halm VP, Voskuyl AE, Simsek S, Dijkmans B, Nurmohamed MT. Increased prevalence of antithyroid antibodies in rheumatoid arthritis patients with a low prevalence of hormonal alterations. Autoimmunity. 2008;41:337.
Pyne D, Isenberg DA. Autoimmune thyroid disease in systemic lupus erythematosus. Ann Rheum Dis. 2002;61:70–2.
de Carvalho F, Pereira RM, Shoenfeld Y. The mosaic of autoimmunity: the role of environmental factors. Front Biosci. 2009;1:501–9.
Jacobson M, Concepcion E, Ho K, Kopp P, Toniolo JV, Tomer Y. cDNA immunization of mice with human thyroglobulin generates both humoral and T cell responses: a novel model of thyroid autoimmunity. PLoS One. 2011;6:e19200.
Tomer Y. Mechanisms of autoimmune thyroid disease: from genetics to epigenetics. Annu Rev Pathol. 2014;9:147–56.
Brand OJ, Lowe CE, Heward JM, Franklyn JA, Cooper JD, Todd JA, Gough SC. Association of the Interleukin 2 receptor alpha (IL2 Ralpha)/CD25 gene region with Graves´ disease using a multilocus test and tag SNPs. Clin Endocrinol. 2007;66:508–12.
Andre S, Tough DF, Lacroix-Desmazes S, Kaveri SV, Bayry J. Surveillance of antigen-presenting cells by CD4+CD25+regulatory T cells in autoimmunity: immunopathogenesis and therapeutic implications. Am J Pathol. 2009;174:1575–87.
Davies TF, Latif R, Yin X. New genetic insights from autoimmune thyroid disease. J Thyroid Res. 2012;2012:623852.
Viatte S, Plant D, Raychaudhuri S. Genetics and epigenetics of rheumatoid arthritis. Nat Rev Rheumatol. 2013;9:141–53.
Begovich AB, Carlton VE, Honigberg LA, Schrodi SJ, Chokkalingam AP, Alexander HC, Ardlie KG, Huang Q, Smith AM, Spoerke JM, Conn MT, Chang M, Chang SY, Saiki RK, Catanese JJ, Leong DU, Garcia VE, McAllister LB, Jeffery DA, Lee AT, Batliwalla F, Remmers E, Criswell LA, Seldin MF, Kastner DL, Amos CI, Sninsky JJ, Gregersen PK. A missense single-nucleotide polymorphism in a gene encoding a protein tyrosine phosphatase (PTPN22) is associated with rheumatoid arthritis. Am J Hum Genet. 2004;75:330–7.
Suzuki A, Yamada R, Chang X, Tokuhiro S, Sawada T, Suzuki M, Nagasaki M, Nakayama-Hamada M, Kawaida R, Ono M, Ohtsuki M, Furukawa H, Yoshino S, Yukioka M, Tohma S, Matsubara T, Wakitani S, Teshima R, Nishioka Y, Sekine A, Iida A, Takahashi A, Tsunoda T, Nakamura Y, Yamamoto K. Functional haplotypes of PADI4, encoding citrullinating enzyme peptidylarginine deiminase 4, are associated with rheumatoid arthritis. Nat Genet. 2003;34:395–402.
Plenge RM, Padyukov L, Remmers EF, Purcell S, Lee AT, Karlson EW, Wolfe F, Kastner DL, Alfredsson L, Altshuler D, Gregersen PK, Klareskog L, Rioux JD. Replication of putative candidate-gene associations with rheumatoid arthritis in 4,000 samples from North America and Sweden: association of susceptibility with PTPN22, CTLA4 and PADI4. Am J Hum Genet. 2005;77:1044–60.
Lander ES, Linton LM, Birren B, Nusbaum C, Zody MC, Baldwin J, Devon K, Dewar K, Doyle M, FitzHugh W, Funke R, Gage D, Harris K, Heaford A, Howland J, Kann L, Lehoczky J, LeVine R, McEwan P, McKernan K, Meldrim J, Mesirov JP, Miranda C, Morris W, Naylor J, Raymond C, Rosetti M, Santos R, Sheridan A, Sougnez C, Stange-Thomann N, Stojanovic N, Subramanian A, Wyman D, Rogers J, Sulston J, Ainscough R, Beck S, Bentley D, Burton J, Clee C, Carter N, Coulson A, Deadman R, Deloukas P, Dunham A, Dunham I, Durbin R, French L, Grafham D, Gregory S, Hubbard T, Humphray S, Hunt A, Jones M, Lloyd C, McMurray A, Matthews L, Mercer S, Milne S, Mullikin JC, Mungall A, Plumb R, Ross M, Shownkeen R, Sims S, Waterston RH, Wilson RK, Hillier LW, McPherson JD, Marra MA, Mardis ER, Fulton LA, Chinwalla AT, Pepin KH, Gish WR, Chissoe SL, Wendl MC, Delehaunty KD, Miner TL, Delehaunty A, Kramer JB, Cook LL, Fulton RS, Johnson DL, Minx PJ, Clifton SW, Hawkins T, Branscomb E, Predki P, Richardson P, Wenning S, Slezak T, Doggett N, Cheng JF, Olsen A, Lucas S, Elkin C, Uberbacher E, Frazier M, Gibbs RA, Muzny DM, Scherer SE, Bouck JB, Sodergren EJ, Worley KC, Rives CM, Gorrell JH, Metzker ML, Naylor SL, Kucherlapati RS, Nelson DL, Weinstock GM, Sakaki Y, Fujiyama A, Hattori M, Yada T, Toyoda A, Itoh T, Kawagoe C, Watanabe H, Totoki Y, Taylor T, Weissenbach J, Heilig R, Saurin W, Artiguenave F, Brottier P, Bruls T, Pelletier E, Robert C, Wincker P, Smith DR, Doucette-Stamm L, Rubenfield M, Weinstock K, Lee HM, Dubois J, Rosenthal A, Platzer M, Nyakatura G, Taudien S, Rump A, Yang H, Yu J, Wang J, Huang G, Gu J, Hood L, Rowen L, Madan A, Qin S, Davis RW, Federspiel NA, Abola AP, Proctor MJ, Myers RM, Schmutz J, Dickson M, Grimwood J, Cox DR, Olson MV, Kaul R, Raymond C, Shimizu N, Kawasaki K, Minoshima S, Evans GA, Athanasiou M, Schultz R, Roe BA, Chen F, Pan H, Ramser J, Lehrach H, Reinhardt R, McCombie WR, de la Bastide M, Dedhia N, Blöcker H, Hornischer K, Nordsiek G, Agarwala R, Aravind L, Bailey JA, Bateman A, Batzoglou S, Birney E, Bork P, Brown DG, Burge CB, Cerutti L, Chen HC, Church D, Clamp M, Copley RR, Doerks T, Eddy SR, Eichler EE, Furey TS, Galagan J, Gilbert JG, Harmon C, Hayashizaki Y, Haussler D, Hermjakob H, Hokamp K, Jang W, Johnson LS, Jones TA, Kasif S, Kaspryzk A, Kennedy S, Kent WJ, Kitts P, Koonin EV, Korf I, Kulp D, Lancet D, Lowe TM, McLysaght A, Mikkelsen T, Moran JV, Mulder N, Pollara VJ, Ponting CP, Schuler G, Schultz J, Slater G, Smit AF, Stupka E, Szustakowski J, Thierry-Mieg D, Thierry-Mieg J, Wagner L, Wallis J, Wheeler R, Williams A, Wolf YI, Wolfe KH, Yang SP, Yeh RF, Collins F, Guyer MS, Peterson J, Felsenfeld A, Wetterstrand KA, Patrinos A, Morgan MJ, de Jong P, Catanese JJ, Osoegawa K, Shizuya H, Choi S, Chen YJ. International Human Genome Sequencing Consortium. Initial sequencing and analysis of the human genome. Nature. 2001;409:860–921.
Okada Y, Terao C, Ikari K, Kochi Y, Ohmura K, Suzuki A, Kawaguchi T, Stahl EA, Kurreeman FA, Nishida N, Ohmiya H, Myouzen K, Takahashi M, Sawada T, Nishioka Y, Yukioka M, Matsubara T, Wakitani S, Teshima R, Tohma S, Takasugi K, Shimada K, Murasawa A, Honjo S, Matsuo K, Tanaka H, Tajima K, Suzuki T, Iwamoto T, Kawamura Y, Tanii H, Okazaki Y, Sasaki T, Gregersen PK, Padyukov L, Worthington J, Siminovitch KA, Lathrop M, Taniguchi A, Takahashi A, Tokunaga K, Kubo M, Nakamura Y, Kamatani N, Mimori T, Plenge RM, Yamanaka H, Momohara S, Yamada R, Matsuda F, Yamamoto K. Meta-analysis identifies nine new loci associated with rheumatoid arthritis in the Japanese population. Nat Genet. 2012;44:511–6.
Stahl EA, Raychaudhuri S, Remmers EF, Xie G, Eyre S, Thomson BP, Li Y, Kurreeman FA, Zhernakova A, Hinks A, Guiducci C, Chen R, Alfredsson L, Amos CI, Ardile KG, BIRAC Consortium, Barton A, Bowes J, Brouwer E, Burtt NP, Catanese JJ, Coblyn J, Coenen MJ, Costenbader KH, Criswell LA, Crusius JB, Cui J, de Bakker PI, De Jager PL, Ding B, Emery P, Flynn E, Harrison P, Hocking LJ, Huizinga TW, Kastner DL, Ke X, Lee AT, Liu X, Martin P, Morgan AW, Padyukov L, Posthumus MD, Radstake TR, Reid DM, Seielstad M, Seldin MF, Shadick NA, Steer S, Tak PP, Thomson W, van der Helm-van Mil MH, van der Horst-Bruinsma IE, van der Schoot CE, van Riel PL, Weinblatt ME, Wilson AG, Wolbink GJ, Wordsworth BP, YEAR Consortium, Wijmenga C, Karlson EW, Toes RE, de Vries N, Begovich AB, Worthington J, Siminovitch KA, Gregersen PK, Klareskog L, Plenge RM. Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nat Genet. 2010;42:508–14.
Perricone C, Ceccarelli F, Valesini G. An overview on the genetic of rheumatoid arthritis: a never-ending story. Autoimmun Rev. 2011;10:599–608.
Kouki T, Sawai Y, Gardine CA, Fisfalen ME, Alegre ML, DeGroot LJ. CTLA-4 gene polymorphism at position 49 in exon 1 reduces the inhibitory function of CTLA-4 and contributes to the pathogenesis of Graves´ disease. J Immunol. 2000;165:6606–11.
Mäurer M, Loserth S, Kolb-Mäurer A, Ponath A, Wiese S, Kruse N, Rieckmann P. A polymorphism in the human cytotoxic T-lymphocyte antigen 4 (CTLA4) gene (exon 1 +49) alters T-cell activation. Immunogenetics. 2002;54:1–8.
Anjos S, Nguyen A, Ounissi-Benkalha H, Tessier MC, Polychronakos C. A common autoimmunity predisposing signal peptide variant of the cytotoxic T-lymphocyte antigen 4 results in inefficient glycosylation of the susceptibility allele. J Biol Chem. 2002;277:46478–86.
Xu Y, Graves PN, Tomer Y, Davies TF. CTLA-4 and autoimmune thyroid disease: lack of influence of the A49G signal peptide polymorphism on functional recombinant human CTLA-4. Cell Immunol. 2002;215:133–40.
Han S, Li Y, Mao Y, Xie Y. Meta-analysis of the association of CTLA4 exon-1+49A/G polymorphism with rheumatoid arthritis. Hum Genet. 2005;118:123–32.
Zaletel K, Krhin B, Gaberšček S, Hojker S. Thyroid autoantibody production is influenced by exon l and promoter CTLA4 polymorphisms in patients with Hashimoto´s thyroiditis. Int J Immunogenet. 2006;33:87–91.
Vaidya B, Pearce SH, Charlton S, Marshall N, Rowan AD, Griffiths ID, Kendall-Taylor P, Cawston TE, Young-Min S. An association between the CTLA4 exon 1 polymorphism and early rheumatoid arthritis with autoimmune endocrinopathies. Rheumatology (Oxford). 2002;41:180–3.
Benhatchi K, Jochmanova I, Habalova V, Wagnerova H, Lazurova I. CTLA4 exon1 A49G polymorphism in Slovak patients with rheumatoid arthritis and Hashimoto thyroiditis—results and the review of the literature. Clin Rheumatol. 2011;30:1319–24.
Kochi Y, Suzuki A, Yamada R, Yamamoto K. Ethnogenetic heterogeneity of rheumatoid arthritis-implications for pathogenesis. Nat Rev Rheumatol. 2010;6:290–5.
Effraimidis G, Wiersinga WM. Mechanisms in endocrinology: autoimmune thyroid disease: old and new players. Eur J Endocrinol. 2014;170:R241–52.
Fousteri G, Liossis SW, Battaglia M. Roles of the protein tyrosine phosphatase PTPN22 in immunity and autoimmunity. Clin Immunol. 2013;149:556–65.
Chang HH, Tai TS, Lu B, Iannaccone C, Cernadas M, Weinblatt M, Shadick N, Miaw SC, Ho IC. PTPN22.6, a dominant negative isoform of PTPN22 and potential biomarker of rheumatoid arthritis. PLoS One. 2012;7:e33067.
Song GG, Bae SC, Kim JH, Lee YH. The PTPN22 C1858T polymorphism and rheumatoid arthritis: a meta-analysis. Rheumatol Int. 2013;33:1991–9.
Chabchoub G, Teixiera EP, Maalej A, Ben Hamad M, Bahloul Z, Cornelis F, Ayadi H. The R620W polymorphism of the protein tyrosine phosphatase 22 gene in autoimmune thyroid diseases and rheumatoid arthritis in the Tunisian population. Ann Hum Biol. 2009;36:342–9.
Taylor LH, Twigg S, Worthington J, Emery P, Morgan AW, Wilson AG, Teare MD. Metaanalysis of the association of smoking and PTPN22 R620W genotype on autoantibody status and radiological erosions in rheumatoid arthritis. J Rheumatol. 2013;40:1048–53.
Caramaschi P, Biasi D, Colombatti M, Pieropan S, Martinelli N, Carletto A, Volpe A, Pacor LM, Bambara LM. Anti-TNF alpha therapy in rheumatoid arthritis and autoimmunity. Rheumatol Int. 2006;26:209–14.
Tarhan F, Oruk G, Niflioglu O, Ozer S. Thyroid involvement in ankylosing spondylitis and relationship of thyroid dysfunction with anti-TNF alpha treatment. Rheumatol Int. 2013;33:853–7.
Elkayam O, Burke M, Vardinon N, Zakut V, Yitzhak RB, Paran D, Levartovsky D, Litinsky I, Caspi D. Autoantibodies profile of rheumatoid arthritis patients during treatment with infliximab. Autoimmunity. 2005;38:155–60.
Chen K, Wei Y, Sharp GC, Braley-Mullen H. Decreasing TNF-alpha results in less fibrosis and earlier resolution of granulomatous experimental autoimmune thyroiditis. J Leukoc Biol. 2007;81:306–14.
Conflict of Interests
Ivica Lazúrová, Ivana Jochmanová, Karim Benhatchi and Štefan Sotak declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lazúrová, I., Jochmanová, I., Benhatchi, K. et al. Autoimmune thyroid disease and rheumatoid arthritis: relationship and the role of genetics. Immunol Res 60, 193–200 (2014). https://doi.org/10.1007/s12026-014-8598-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-014-8598-9