Abstract
Purpose
Risk stratification based on somatic mutations in TERT promoter and BRAF/RAS has been well established for papillary thyroid cancer (PTC), and there is emerging evidence showed that TERT promoter methylation was frequently observed in thyroid cancer patients with adverse features. This study was aimed to comprehensive explore the prognostic value of BRAF/RAS mutations, TERT promoter mutations, and TERT promoter methylation in PTC.
Methods
The relationships of BRAF/RAS mutations, TERT promoter mutations, and TERT promoter methylation with clinical characteristics and outcomes of PTC were analyzed in 382 patients with PTC.
Results
TERT promoter mutation and hypermethylation were collectively observed in 52 (13.6%) samples and associated with BRAF/RAS mutation, aggressive clinical characteristics, and poor clinical outcomes of PTC. Coexistence of BRAF/RAS and TERT alterations was found in 45 of 382 (11.8%) PTC patients and strongly associated with old patient age, extrathyroidal extension, advanced pathologic T stage and metastasis. Importantly, patients with both BRAF/RAS and TERT alterations had higher rates of tumor recurrence (13.6% vs 1.5%, P = 0.042) and disease progression (24.4% vs 3.3%, P < 0.001) than patients without any alterations, and cox regression analysis revealed that the coexistence of BRAF/RAS and TERT alterations, but not BRAF/RAS or TERT alterations alone, increased the risk of progression-free interval with an adjusted HR of 10.35 (95% CI: 1.79–59.81, P = 0.009).
Conclusions
This study suggested that comprehensively analysis of BRAF/RAS mutations, TERT promoter mutation and methylation is an effective strategy to identify high-risk patients with PTC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer is the most common malignancy of the endocrine system, diagnosed in 586,202 people over the world in 2020 [1]. Papillary thyroid cancer (PTC) accounts for 85–90% of all thyroid cancer cases and its incidence rises rapidly in the past several decades [2]. Although over 93% of PTC patients have favorable prognosis within 5 years after initial treatment [3], studies with long-term follow-up time showed that tumor recurrence and disease-specific death rates increased up to 29% and 9%, respectively [4, 5]. Precision identification of the high-risk patients remains a major challenge in the clinic, since the risk stratification system based on conventional clinicopathological risk factors is not accurate enough for identifying the patients with poor prognosis [6].
Molecular-based risk stratification of PTC using genetic markers showed great advantages and has been well accepted in recent years [7]. Among the various genetic alterations in PTC, BRAF V600E, RAS mutations, and hotspot mutations in the promoter of telomerase reverse transcriptase (TERT) had been well investigated [8]. BRAF V600E, the most common driver mutation in PTC, is capable of constitutively activating the mitogen-activated protein kinase (MAPK) pathway. The RAS mutation occurs in about 10% of PTC cases and mutually exclusive with BRAF mutation. The two mutually exclusive point mutations (C228T and C250T) in TERT promoter, collectively occurs in about 11% of PTC [9], generates de novo binding sites for the GABP complex and leads to TERT activation and telomere length maintain [10,11,12]. Numerous studies have demonstrated that either BRAF or TERT mutations has been associated with high risk of tumor recurrence and PTC-specific mortality [13,14,15,16]. Interestingly, TERT promoter mutations tend to coexist with BRAF and RAS mutations, and the patients harboring both BRAF/RAS and TERT mutations showed more aggressive characteristics and worse clinical outcomes than the ones harboring TERT or BRAF/RAS mutation alone [9, 17,18,19,20]. It should be noticed that the frequency of cases harboring both BRAF/RAS and TERT promoter mutations is 6–8%, which is lower than the proportion of patients that showed aggressive characteristics in the clinic. Therefore, other biomarkers are needed to be identified and enrolled in the molecular -based risk stratification system.
In addition to the two hotspot mutations, DNA hypermethylation in the upstream of the transcription start site (UTSS) of TERT gene was frequently observed in multiple types of human cancer [21, 22]. And there is accumulating evidence that TERT promoter hypermethylation was associated with disease progression and poor prognosis of several cancers, including pediatric brain tumor [23], breast cancer [24], bladder cancer [25], pancreatic cancer [26], and pituitary adenoma [27]. For thyroid cancer, few preliminary studies had shown a correlation between TERT methylation and aggressive features and/or poor outcome [28,29,30], suggesting that TERT promoter methylation might be a prognostic marker for PTC. Herein, in this study, we comprehensively analyzed the association of BRAF/RAS mutations, TERT promoter mutations and methylation with clinicopathologic outcomes of PTC and assessed the possibility of enrolling TERT promoter methylation into the well-established risk stratification system based on the genetic duet of BRAF/RAS and TERT mutations.
Materials and methods
Patients
The patients with PTC used for this study were originated from The Cancer Genome Atlas (TCGA) thyroid cancer (THCA) dataset. Only the samples containing all the following information were included in the present study: BRAF mutation, RAS mutation, TERT promoter mutation, TERT methylation, and TERT mRNA expression.
Data acquisition
The mutation status of BRAF, RAS, and TERT promoter were obtained from the 2014 TCGA thyroid cancer paper [31], the methylation level (β-value) of a specific CpG probe (cg11625005) in TERT promoter and relative mRNA expression of TERT (from Illumina HiSeq) in PTC patients were downloaded from TCGA database by the UCSC Xena platform [32]. The methylation levels of cg11625005 in TCGA normal thyroid tissues were downloaded by the Shiny Methylation Analysis Resource Tool (SMART) [33]. The following clinical characteristics and outcomes as well as related follow-up times for each PTC patients were downloaded and collected from the TCGA Clinical Data Resource [34]: age at diagnosis, sex, extrathyroidal extension, pathologic T/N/M, overall survival (OS), disease-specific survival (DSS), disease-free interval (DFI) and progression-free interval (PFI).
Definition of TERT hypermethylation
The methylation level of cg11625005 was selected for representing the overall methylation level of TERT promoter region [24, 25]. The cut-off β-value for TERT promoter hypermethylation in thyroid cancer was defined as the mean β-value + 2*SD of the normal samples [22]. According to this formula, the cut-off β-value was set at 0.494 for TERT hypermethylation in the current study.
Statistical analysis
The categorical data were summarized with frequencies and percentages, and compared by using chi-square test or Fisher’s exact test. The continuous data were summarized with means ± standard errors or medians and interquartile ranges (IQR), and compared by independent t test or Wilcoxon–Mann–Whitney test, respectively. Kaplan–Meier survival curves with log-rank test were used to compare the progression-free interval (PFI) between different genotypes. Univariate and multivariate survival analyses were performed using Cox regression to assess the association between genomic alterations and clinical outcomes of PTC. All P values were two sided, and statistical significance was set at P < 0.05. Statistical analyses were performed using Stata (version 10.1; Stata Corp., College Station, TX, USA) and GraphPad Prism (version 7; GraphPad Software, San Diego, CA, USA).
Results
BRAF/RAS mutation and TERT alteration in PTC
According to the patients’ enrollment criteria, a total of 382 PTC patients were included in the current study. The BRAF and RAS mutations were detected in 236 (61.8%) and 49 (12.8%) of the samples, respectively; TERT promoter mutation and hypermethylation occurred in 36 (9.4%) and 21 (5.5%) samples, respectively (Fig. 1A). Compared with the patients harboring wild-type TERT promoter, patients harboring TERT promoter mutations had a significant increased level of TERT expression (P < 0.001, Fig. 1B); Similarly, TERT expression was significantly higher in patients with TERT promoter hypermethylation than that in patients with hypomethylated TERT promoter (P < 0.001, Fig. 1C). Therefore, we combined TERT promoter mutation and hypermethylation into one group (named as the TERT alteration group) in the following analysis. Collectively, BRAF or RAS mutation occurred in 284 (74.3%) samples and TERT alteration occurred in 52 (13.6%) samples.
The association of TERT alterations with BRAF/RAS mutation and TERT expression. A Distribution of BRAF mutation, RAS mutation, TERT promoter mutations and hypermethylation in 382 papillary thyroid cancer (PTC) patients from the TCGA dataset. B Relative TERT expression in TERT promoter wild-type (wt) and mutated PTC samples. C Relative TERT expression in TERT promoter hypomethylated and hypermethylated PTC samples. ***P < 0.001
The association of BRAF/RAS mutation and TERT alteration with clinical characteristics and outcomes of PTC
Compared with the patients without BRAF or RAS mutation, the BRAF/RAS mutation positive patients had higher rates of extrathyroidal extension (33.1% vs. 14.9%, P = 0.001) and advanced pathologic T stage (39.6% vs 26.8%, P = 0.024). Disease progression was 32 of 284 (11.3%) in BRAF/RAS mutation positive patients versus 4 of 98 (4.1%) in BRAF/RAS mutation negative patients (P = 0.043, Table 1). In addition to extrathyroidal extension and pathologic T stage, the TERT alterations were found to be significantly correlated with old patient age and pathologic M stage (Table 2). And patients with TERT alterations had higher rates of overall mortality (13.5% vs 2.1%, P < 0.001), disease-specific mortality (8.0% vs 0.3%, P = 0.001) and progression (23.1% vs 7.3%, P < 0.001) than patients without any TERT alteration (Table 2).
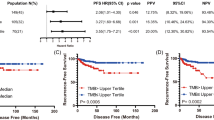
We next performed Kaplan-Meier and Cox-regression analyses of progression-free interval (PFI) by genotype. Although the PFI curve had a modest decline in patients harboring BRAF or RAS mutation, the BRAF/RAS mutation was not significantly associated with PFI (log-rank P = 0.071; HR = 2.52, 95% CI: 0.89–7.12, P = 0.082; Fig. 2A and Table 3). While the Kaplan–Meier curve showed that the presence of TERT alteration was significantly associated with PFI in PTC (log-rank P < 0.001, Fig. 2B), and the hazard ratio (HR) of TERT alteration for PFI was 3.48 (95% CI: 1.74–6.96, P < 0.001), which lost significance after adjustment for aggressive tumor behaviors (Table 3).
Kaplan–Meier analyses of the impacts of BRAF/RAS mutation and TERT alterations on progression-free interval (PFI) of patients with papillary thyroid cancer. A Effect of BRAF/RAS mutation on PFI. B Effect of TERT alteration on PFI. C Effects of BRAF/RAS mutation or TERT alteration alone or their coexistence on PFI
Impacts of BRAF/RAS mutation, TERT alteration and their coexistence on clinicopathologic outcomes of PTC
Since it has been well established that TERT promoter mutation tends to be coexist with BRAF/RAS mutation, we next analyzed the association of TERT alterations (TERT promoter mutation + hypermethylation) with BRAF/RAS mutation. As a result, TERT alteration was found in 7 of 98 (7.1%) BRAF/RAS mutation -negative patients versus 45 of 284 (15.8%) BRAF/RAS mutation -positive patients, while BRAF/RAS mutation was found in 239 of 330 (72.4%) TERT alteration -negative patients versus 45 of 52 (86.5%) TERT alteration -positive patients (P = 0.030), suggesting a significant positive association between the presence of TERT alteration and BRAF/RAS mutation in PTC. Coexistence of BRAF/RAS and TERT alteration was found in 45 of 382 (11.8%) PTCs. Next, we divided the patients into 4 groups according to BRAF/RAS and TERT alteration status, and analyzed the association of BRAF/RAS mutation alone, TERT alteration alone, and the coexisting of BRAF/RAS and TERT alterations with clinicopathologic characteristics and outcomes of PTC.
As shown in Table 4, in comparison with the 91 patients with neither BRAF/RAS mutation nor TERT alteration, BRAF/RAS mutation alone was associated with extrathyroidal extension (30.6% vs 14.8%, P = 0.006), TERT alteration alone was not associated with any of the aggressive characteristics of PTC, while coexistence of BRAF/RAS mutation and TERT alteration was strongly associated with several high-risk clinicopathologic characteristics, including older age (mean value of 62 vs 47, P < 0.001), extrathyroidal extension (46.3% vs 14.8%, P < 0.001), advanced pathologic T stages (T3 + T4, 57.8% vs 26.4%, P < 0.001) and metastasis (13.8% VS 0%, P = 0.024). Importantly, patients with both BRAF/RAS mutation and TERT alteration had higher rates of tumor recurrence (13.6% vs 1.5%, P = 0.042) and disease progression (24.4% vs 3.3%, P < 0.001) than patients without any alterations in BRAF, RAS or TERT (Table 4).
On Kaplan–Meier analysis of the impacts of the 4 groups on PFI of patients with PTC, the PFI curve of patients harboring neither alteration was almost flat, the curves of patients harboring BRAF/RAS mutation alone or TERT alteration alone showed modest decline, while the curve of patients with coexisting of BRAF/RAS and TERT alterations declined more sharply and dramatically than the other 3 groups (log-rank P = 0.001, Fig. 2C). PFI per 1000-person years in patients with neither alteration, BRAF/RAS mutation alone, TERT alteration alone, or both BRAF/RAS mutation and TERT alteration were 11.21 (95% CI: 3.62–34.76), 25.69 (95% CI: 16.75–39.40), 80.24 (95% CI: 11.30–569.61), and 78.39 (95% CI: 43.41–141.54), respectively (Table 5). In the Cox regression analysis, the HRs of BRAF/RAS mutation alone and TERT alteration alone for PFI were not significant; the HR of coexisting BRAF/RAS and TERT alterations for PFI was 7.25 (95% CI: 2.02–26.01, P = 0.002), which remained significant at 10.35 (95% CI: 1.79–59.81, P = 0.009) after adjustment for multiple aggressive tumor characteristics (Table 5). Moreover, compared with patients harboring BRAF/RAS mutation, patients with both BRAF/RAS mutation and TERT alteration had a higher risk of PFI (HR = 2.98, 95% CI: 1.44–6.19, P = 0.003).
Discussion
The discovery of TERT promoter mutation is a milestone in the genetic field of thyroid cancer. The diagnostic and prognostic value of TERT promoter mutation have been well established in the past 10 years. A large number of studies have shown that TERT promoter mutation associated with almost all the adverse features of PTC and patients harboring TERT mutation were at high risk of radioiodine refractory, tumor recurrence and death from thyroid cancer [15, 16, 35,36,37]. Mechanismly, the GABPA/BABPB transcription factor complex and ETV5 selectively binds to and activates the mutant TERT promoter, leading to increased TERT expression and thus confers oncogenic functions in thyroid tumorigenesis and development [38, 39].
In addition to promoter mutation, pan-cancer analysis revealed that TERT overexpression was seen in patients harboring several other types of genetic and epigenetic alterations, including TERT amplification, structural variation, and DNA methylation [21]. Although whether TERT promoter methylation activates its expression is still controversial [22, 40,41,42,43,44], emerging studies have shown that TERT methylation was associated with increased TERT expression and aggressive clinical behaviors in thyroid cancer [28,29,30]. Consistently, in this study, we found that TERT expression is significantly higher in PTC patients with TERT hypermethylation than that in patients with TERT hypomethylation.
In this study, the TERT promoter mutation was observed in 9.4% of PTC patients, TERT hypermethylation was observed in 5.5% of PTCs, and they were collectively present in 13.6% of patients with PTC. These two types of TERT alterations were associated with old patient age, extrathyroidal extension, advanced T and M stage, and poor outcomes. These results are in line with a recent study indicating that both TERT promoter mutation and methylation were frequently observed in clinically aggressive thyroid cancers [30].
Although the hotspot mutations in BRAF and RAS genes had been identified 10 years earlier than TERT mutation, the association between BRAF/RAS mutation and prognosis of PTC is still controversial. However, there is no doubt that BRAF mutation is not an effective biomarker for aggressive PTCs since the frequency of BRAF mutation is much higher than the frequency of aggressive cases among all the patients with PTC. Unlike other well-known somatic mutations, the RAS mutations could be frequently identified not only in malignant thyroid nodules but also in benign nodules, two recent cohort studies with large patient number showed that RAS mutation alone was likely to be a favorable marker of thyroid cancer [45], while coexisting of RAS mutation with additional oncogenic alteration associated with more aggressive phenotype and increased risk of recurrence and mortality in differentiated thyroid cancer [46]. Consistently, in this study, we found that patients harboring BRAF or RAS mutation had higher rates of extrathyroidal extension and advanced pathologic T stage, but the BRAF/RAS mutation was not an independent risk factor for the prognosis of PTC.
Importantly, it has been well established that TERT promoter mutations were associated with BRAF/RAS mutations in PTC, and the patients harboring both BRAF/RAS and TERT mutations were associated with the most aggressive behaviors and worst clinical outcomes of PTC. In this study, we showed that the presence of both BRAF/RAS mutation and TERT alteration significantly associated with multiple aggressive characteristics of PTC, including old age, extrathyroidal extension, advanced pathologic T stage and metastasis. Moreover, we observed that patients harboring both BRAF/RAS and TERT alterations had remarkable increased rate of DFI and PFI. Importantly, Cox regression analysis revealed that the coexistence of BRAF/RAS and TERT alterations, but not BRAF/RAS alone or TERT alterations alone, increased the risk of PFI of PTC, suggesting a cooperative role of BRAF/RAS and TERT alterations in PTC progression. These data suggested an updated risk stratification model for PTC prognosis with a risk order of the coexisting of BRAF/RAS mutation and TERT alteration »» BRAF/RAS mutation alone = TERT alteration alone > wild type for the 3 genes.
Here we enrolled TERT methylation in the risk stratification system for PTC, compared with previous established BRAF/RAS and TERT mutations -based risk stratification system, enrollment of TERT methylation as a high-risk marker will identify more patients which potentially at high risk of poor outcomes. This is particularly the case for PTC patients in Asian, since TERT promoter mutation was reported in 2–3% of PTC patients in Asian countries and the frequency of coexisting of BRAF/RAS and TERT mutations was 1–2% in Asian patients with PTC [47,48,49], which is much lower than the frequency of clinically high-risk patients.
Conclusions
In conclusion, TERT promoter mutation and hypermethylation are common events in PTC and they associate with adverse features and poor clinical outcome of PTC. Patients harboring both TERT alterations and BRAF/RAS mutations showed more aggressive characteristics and worse prognosis than patients harboring TERT alterations alone, BRAF/RAS mutations alone, or no alteration. Comprehensively analysis of hotspot somatic mutations in BRAF, RAS, and TERT genes, in combination with TERT promoter methylation could identify high-risk patients and lead to a better management for the patients with PTC.
Data availability
Publicly available TCGA thyroid cancer datasets analyzed in this study can be found at https://portal.gdc.cancer.gov/ or https://xena.ucsc.edu/. Further specific inquiries can be directed to the corresponding author.
References
H. Sung, J. Ferlay, R.L. Siegel, M. Laversanne, I. Soerjomataram, A. Jemal, F. Bray, Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021)
C.M. Kitahara, J.A. Sosa, The changing incidence of thyroid cancer. Nat. Rev. Endocrinol. 12, 646–653 (2016)
L. Dal Maso, A. Tavilla, F. Pacini, D. Serraino, B.A.C. van Dijk, M.D. Chirlaque, R. Capocaccia, N. Larranaga, M. Colonna, D. Agius, E. Ardanaz, J. Rubio-Casadevall, A. Kowalska, S. Virdone, S. Mallone, H. Amash, R. De Angelis, E.-W. Group, Survival of 86,690 patients with thyroid cancer: A population-based study in 29 European countries from EUROCARE-5. Eur. J. Cancer 77, 140–152 (2017)
R.H. Grogan, S.P. Kaplan, H. Cao, R.E. Weiss, L.J. Degroot, C.A. Simon, O.M. Embia, P. Angelos, E.L. Kaplan, R.B. Schechter, A study of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery 154, 1436–1446 (2013)
W. Dong, K. Horiuchi, H. Tokumitsu, A. Sakamoto, E. Noguchi, Y. Ueda, T. Okamoto, Time-varying pattern of mortality and recurrence from papillary thyroid cancer: lessons from a long-term follow-up. Thyroid 29, 802–808 (2019)
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26, 1–133 (2016)
M. Xing, B.R. Haugen, M. Schlumberger, Progress in molecular-based management of differentiated thyroid cancer. Lancet 381, 1058–1069 (2013)
J.A. Fagin, S.A. Wells Jr, Biologic and clinical perspectives on thyroid cancer. N. Engl. J. Med 375, 1054–1067 (2016)
R. Liu, M. Xing, TERT promoter mutations in thyroid cancer. Endocr. Relat. Cancer 23, R143–R155 (2016)
R.J. Bell, H.T. Rube, A. Kreig, A. Mancini, S.D. Fouse, R.P. Nagarajan, S. Choi, C. Hong, D. He, M. Pekmezci, J.K. Wiencke, M.R. Wrensch, S.M. Chang, K.M. Walsh, S. Myong, J.S. Song, J.F. Costello, Cancer. The transcription factor GABP selectively binds and activates the mutant TERT promoter in cancer. Science 348, 1036–1039 (2015)
K. Chiba, J.Z. Johnson, J.M. Vogan, T. Wagner, J.M. Boyle, D. Hockemeyer, Cancer-associated TERT promoter mutations abrogate telomerase silencing. Elife 4, e07918 (2015)
A.M. McKinney, R. Mathur, N.O. Stevers, A.M. Molinaro, S.M. Chang, J.J. Phillips, J.F. Costello, GABP couples oncogene signaling to telomere regulation in TERT promoter mutant cancer. Cell Rep. 40, 111344 (2022)
M. Xing, A.S. Alzahrani, K.A. Carson, D. Viola, R. Elisei, B. Bendlova, L. Yip, C. Mian, F. Vianello, R.M. Tuttle, E. Robenshtok, J.A. Fagin, E. Puxeddu, L. Fugazzola, A. Czarniecka, B. Jarzab, C.J. O’Neill, M.S. Sywak, A.K. Lam, G. Riesco-Eizaguirre, P. Santisteban, H. Nakayama, R.P. Tufano, S.I. Pai, M.A. Zeiger, W.H. Westra, D.P. Clark, R. Clifton-Bligh, D. Sidransky, P.W. Ladenson, V. Sykorova, Association between BRAF V600E mutation and mortality in patients with papillary thyroid cancer. JAMA 309, 1493–1501 (2013)
M. Xing, A.S. Alzahrani, K.A. Carson, Y.K. Shong, T.Y. Kim, D. Viola, R. Elisei, B. Bendlova, L. Yip, C. Mian, F. Vianello, R.M. Tuttle, E. Robenshtok, J.A. Fagin, E. Puxeddu, L. Fugazzola, A. Czarniecka, B. Jarzab, C.J. O’Neill, M.S. Sywak, A.K. Lam, G. Riesco-Eizaguirre, P. Santisteban, H. Nakayama, R. Clifton-Bligh, G. Tallini, E.H. Holt, V. Sykorova, Association between BRAF V600E mutation and recurrence of papillary thyroid cancer. J. Clin. Oncol. 33, 42–50 (2015)
M. Melo, A.G. da Rocha, J. Vinagre, R. Batista, J. Peixoto, C. Tavares, R. Celestino, A. Almeida, C. Salgado, C. Eloy, P. Castro, H. Prazeres, J. Lima, T. Amaro, C. Lobo, M.J. Martins, M. Moura, B. Cavaco, V. Leite, J.M. Cameselle-Teijeiro, F. Carrilho, M. Carvalheiro, V. Maximo, M. Sobrinho-Simoes, P. Soares, TERT promoter mutations are a major indicator of poor outcome in differentiated thyroid carcinomas. J. Clin. Endocrinol. Metab. 99, E754–E765 (2014)
J. Yang, Y. Gong, S. Yan, H. Chen, S. Qin, R. Gong, Association between TERT promoter mutations and clinical behaviors in differentiated thyroid carcinoma: a systematic review and meta-analysis. Endocrine 67, 44–57 (2020)
M. Xing, R. Liu, X. Liu, A.K. Murugan, G. Zhu, M.A. Zeiger, S. Pai, J. Bishop, BRAF V600E and TERT promoter mutations cooperatively identify the most aggressive papillary thyroid cancer with highest recurrence. J. Clin. Oncol. 32, 2718–2726 (2014)
Y.S. Song, J.A. Lim, H. Choi, J.K. Won, J.H. Moon, S.W. Cho, K.E. Lee, Y.J. Park, K.H. Yi, D.J. Park, J.S. Seo, Prognostic effects of TERT promoter mutations are enhanced by coexistence with BRAF or RAS mutations and strengthen the risk prediction by the ATA or TNM staging system in differentiated thyroid cancer patients. Cancer 122, 1370–1379 (2016)
R. Liu, J. Bishop, G. Zhu, T. Zhang, P.W. Ladenson, M. Xing, Mortality risk stratification by combining BRAF V600E and TERT promoter mutations in papillary thyroid cancer: genetic duet of BRAF and TERT promoter mutations in thyroid cancer mortality. JAMA Oncol. 3, 202–208 (2017)
X. Shen, R. Liu, M. Xing, A six-genotype genetic prognostic model for papillary thyroid cancer. Endocr. Relat. Cancer 24, 41–52 (2017)
F.P. Barthel, W. Wei, M. Tang, E. Martinez-Ledesma, X. Hu, S.B. Amin, K.C. Akdemir, S. Seth, X. Song, Q. Wang, T. Lichtenberg, J. Hu, J. Zhang, S. Zheng, R.G. Verhaak, Systematic analysis of telomere length and somatic alterations in 31 cancer types. Nat. Genet 49, 349–357 (2017)
D.D. Lee, R. Leao, M. Komosa, M. Gallo, C.H. Zhang, T. Lipman, M. Remke, A. Heidari, N.M. Nunes, J.D. Apolonio, A.J. Price, R.A. De Mello, J.S. Dias, D. Huntsman, T. Hermanns, P.J. Wild, R. Vanner, G. Zadeh, J. Karamchandani, S. Das, M.D. Taylor, C.E. Hawkins, J.D. Wasserman, A. Figueiredo, R.J. Hamilton, M.D. Minden, K. Wani, B. Diplas, H. Yan, K. Aldape, M.R. Akbari, A. Danesh, T.J. Pugh, P.B. Dirks, P. Castelo-Branco, U. Tabori, DNA hypermethylation within TERT promoter upregulates TERT expression in cancer. J. Clin. Invest 129, 223–229 (2019)
P. Castelo-Branco, S. Choufani, S. Mack, D. Gallagher, C. Zhang, T. Lipman, N. Zhukova, E.J. Walker, D. Martin, D. Merino, J.D. Wasserman, C. Elizabeth, N. Alon, L. Zhang, V. Hovestadt, M. Kool, D.T. Jones, G. Zadeh, S. Croul, C. Hawkins, J. Hitzler, J.C. Wang, S. Baruchel, P.B. Dirks, D. Malkin, S. Pfister, M.D. Taylor, R. Weksberg, U. Tabori, Methylation of the TERT promoter and risk stratification of childhood brain tumours: an integrative genomic and molecular study. Lancet Oncol. 14, 534–542 (2013)
J.D. Apolonio, J.S. Dias, M.T. Fernandes, M. Komosa, T. Lipman, C.H. Zhang, R. Leao, D. Lee, N.M. Nunes, A.T. Maia, J.L. Morera, L. Vicioso, U. Tabori, P. Castelo-Branco, THOR is a targetable epigenetic biomarker with clinical implications in breast cancer. Clin. Epigenet. 14, 178 (2022)
R. Leao, D. Lee, A. Figueiredo, T. Hermanns, P. Wild, M. Komosa, I. Lau, M. Mistry, N.M. Nunes, A.J. Price, C. Zhang, T. Lipman, C. Poyet, N. Valtcheva, K. Oehl, H. Coelho, R. Sayyid, A.M. Gomes, E.C.L. Prado, J. Sweet, J. Vinagre, J. Apolonio, D. Stephens, I. Faleiro, K. Fadaak, P.O. Richard, G. Kulkarni, A.R. Zlotta, R.J. Hamilton, P. Castelo-Branco, U. Tabori, Combined genetic and epigenetic alterations of the TERT promoter affect clinical and biological behavior of bladder cancer. Int J. Cancer 144, 1676–1684 (2019)
I. Faleiro, J.D. Apolonio, A.J. Price, R.A. De Mello, V.P. Roberto, U. Tabori, P. Castelo-Branco, The TERT hypermethylated oncologic region predicts recurrence and survival in pancreatic cancer. Future Oncol. 13, 2045–2051 (2017)
Y. Miyake, J.I. Adachi, T. Suzuki, K. Mishima, R. Araki, R. Mizuno, R. Nishikawa, TERT promoter methylation is significantly associated with TERT upregulation and disease progression in pituitary adenomas. J. Neurooncol. 141, 131–138 (2019)
N. Wang, H. Kjellin, A. Sofiadis, O. Fotouhi, C.C. Juhlin, M. Backdahl, J. Zedenius, D. Xu, J. Lehtio, C. Larsson, Genetic and epigenetic background and protein expression profiles in relation to telomerase activation in medullary thyroid carcinoma. Oncotarget 7, 21332–21346 (2016)
J.J. Li, P.C.J. Zheng, Y.Z. Wang, The correlations between DNA methylation and polymorphisms in the promoter region of the human telomerase reverse transcriptase (hTERT) gene with postoperative recurrence in patients with thyroid carcinoma (TC). World J. Surg. Oncol. 15, 114 (2017)
C. Montero-Conde, L.J. Leandro-Garcia, A.M. Martinez-Montes, P. Martinez, F.J. Moya, R. Leton, E. Gil, N. Martinez-Puente, S. Guadalix, M. Curras-Freixes, L. Garcia-Tobar, C. Zafon, M. Jorda, G. Riesco-Eizaguirre, P. Gonzalez-Garcia, M. Monteagudo, R. Torres-Perez, V. Mancikova, S. Ruiz-Llorente, M. Perez-Martinez, G. Pita, J.C. Galofre, A. Gonzalez-Neira, A. Cascon, C. Rodriguez-Antona, D. Megias, M.A. Blasco, E. Caleiras, S. Rodriguez-Perales, M. Robledo, Comprehensive molecular analysis of immortalization hallmarks in thyroid cancer reveals new prognostic markers. Clin. Transl. Med. 12, e1001 (2022)
Cancer Genome Atlas Research N, Integrated genomic characterization of papillary thyroid carcinoma. Cell 159, 676–690 (2014)
M.J. Goldman, B. Craft, M. Hastie, K. Repecka, F. McDade, A. Kamath, A. Banerjee, Y. Luo, D. Rogers, A.N. Brooks, J. Zhu, D. Haussler, Visualizing and interpreting cancer genomics data via the Xena platform. Nat. Biotechnol. 38, 675–678 (2020)
Y. Li, D. Ge, C. Lu, The SMART App: an interactive web application for comprehensive DNA methylation analysis and visualization. Epigenet. Chromatin 12, 71 (2019)
J. Liu, T. Lichtenberg, K.A. Hoadley, L.M. Poisson, A.J. Lazar, A.D. Cherniack, A.J. Kovatich, C.C. Benz, D.A. Levine, A.V. Lee, L. Omberg, D.M. Wolf, C.D. Shriver, V. Thorsson, Cancer Genome Atlas Research N, Hu H. An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell 173, 400–416 e411 (2018)
M. Bullock, Y. Ren, C. O’Neill, A. Gill, A. Aniss, M. Sywak, S. Sidhu, L. Delbridge, D. Learoyd, F. de Vathaire, B.G. Robinson, R.J.T.E.R.T. Clifton-Bligh, promoter mutations are a major indicator of recurrence and death due to papillary thyroid carcinomas. Clin. Endocrinol. (Oxf.) 85, 283–290 (2016)
X. Yang, J. Li, X. Li, Z. Liang, W. Gao, J. Liang, S. Cheng, Y. Lin, TERT promoter mutation predicts radioiodine-refractory character in distant metastatic differentiated thyroid cancer. J. Nucl. Med 58, 258–265 (2017)
J. Liu, R. Liu, X. Shen, G. Zhu, B. Li, M. Xing, The genetic duet of BRAF V600E and TERT promoter mutations robustly predicts loss of radioiodine avidity in recurrent papillary thyroid cancer. J. Nucl. Med 61, 177–182 (2020)
R. Liu, T. Zhang, G. Zhu, M. Xing, Regulation of mutant TERT by BRAF V600E/MAP kinase pathway through FOS/GABP in human cancer. Nat. Commun. 9, 579 (2018)
M. Bullock, G. Lim, Y. Zhu, H. Aberg, S. Kurdyukov, R. Clifton-Bligh, ETS factor ETV5 activates the mutant telomerase reverse transcriptase promoter in thyroid cancer. Thyroid 29, 1623–1633 (2019)
J.L. Stern, R.D. Paucek, F.W. Huang, M. Ghandi, R. Nwumeh, J.C. Costello, T.R. Cech, Allele-specific DNA methylation and its interplay with repressive histone marks at promoter-mutant TERT genes. Cell Rep. 21, 3700–3707 (2017)
B.A. Avin, Y. Wang, T. Gilpatrick, R.E. Workman, I. Lee, W. Timp, C.B. Umbricht, M.A. Zeiger, Characterization of human telomerase reverse transcriptase promoter methylation and transcription factor binding in differentiated thyroid cancer cell lines. Genes Chromosomes Cancer 58, 530–540 (2019)
D. Esopi, M.K. Graham, J.A. Brosnan-Cashman, J. Meyers, A. Vaghasia, A. Gupta, B. Kumar, M.C. Haffner, C.M. Heaphy, A.M. De Marzo, A.K. Meeker, W.G. Nelson, S.J. Wheelan, S. Yegnasubramanian, Pervasive promoter hypermethylation of silenced TERT alleles in human cancers. Cell Oncol. (Dordr.) 43, 847–861 (2020)
T.J. Rowland, A.J. Bonham, T.R. Cech, Allele-specific proximal promoter hypomethylation of the telomerase reverse transcriptase gene (TERT) associates with TERT expression in multiple cancers. Mol. Oncol. 14, 2358–2374 (2020)
D.D. Lee, M. Komosa, N.M. Nunes, U. Tabori, DNA methylation of the TERT promoter and its impact on human cancer. Curr. Opin. Genet Dev. 60, 17–24 (2020)
H. Guan, G. Toraldo, S. Cerda, F.A. Godley, S.R. Rao, D. McAneny, G. Doherty, L. Braverman, S.L. Lee, Utilities of RAS mutations in preoperative fine needle biopsies for decision making for thyroid nodule management: results from a single-center prospective cohort. Thyroid 30, 536–547 (2020)
A. Bikas, S. Ahmadi, T. Pappa, E. Marqusee, K. Wong, M.A. Nehs, N.L. Cho, J. Haase, G.M. Doherty, K. Sehgal, J.A. Barletta, E.K. Alexander, I. Landa, Additional oncogenic alterations in RAS-driven differentiated thyroid cancers associate with worse clinicopathologic outcomes. Clin. Cancer Res. OF1-OF8. 29, 2678–2685 (2023)
J. Liang, W. Cai, D. Feng, H. Teng, F. Mao, Y. Jiang, S. Hu, X. Li, Y. Zhang, B. Liu, Z.S. Sun, Genetic landscape of papillary thyroid carcinoma in the Chinese population. J. Pathol. 244, 215–226 (2018)
H. Yang, H. Park, H.J. Ryu, J. Heo, J.S. Kim, Y.L. Oh, J.H. Choe, J.H. Kim, J.S. Kim, H.W. Jang, T.H. Kim, S.W. Kim, J.H. Chung, Frequency of TERT promoter mutations in real-world analysis of 2,092 thyroid carcinoma patients. Endocrinol. Metab. (Seoul.) 37, 652–663 (2022)
H.Y. Na, H.W. Yu, W. Kim, J.H. Moon, C.H. Ahn, S.I. Choi, Y.K. Kim, J.Y. Choi, S.Y. Park, Clinicopathological indicators for TERT promoter mutation in papillary thyroid carcinoma. Clin. Endocrinol. (Oxf.) 97, 106–115 (2022)
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 82072952 and No. 82222051) and the Fundamental Research Funds for the Central Universities, Sun Yat-sen University (No. 22ykqb05).
Author information
Authors and Affiliations
Contributions
R.L. and Y.S. designed the research; Y.S., G.H., J.X., M.C., and S.H. collected the data; Y.S., G.H., J.X., and R.L. analyzed the data; R.L. and Y.S. drafted the manuscript, with inputs from all authors. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sang, Y., Hu, G., Xue, J. et al. Risk stratification by combining common genetic mutations and TERT promoter methylation in papillary thyroid cancer. Endocrine 85, 304–312 (2024). https://doi.org/10.1007/s12020-024-03722-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-024-03722-6