Abstract
Purpose
This review focuses on post-operative thyroid hormone replacement and thyrotropin suppression therapy in patients with differentiated thyroid cancer.
Methods
A clinical review.
Results
Differentiated thyroid cancers (DTC), including papillary and follicular thyroid cancers, have an excellent prognosis and their management leverages a unique set of clinical tools arising from homology to the normal thyroid follicular cell. Surgery is the cornerstone of initial management, and post-operative care often requires thyroid hormone replacement therapy, which may be approached with the intent of physiologic normalization or used pharmacologically to suppress TSH as part of a DTC treatment.
Conclusion
Management of DTC and approaches to TSH suppression are tailored to an individual’s risk of DTC recurrence and are adjusted to a patient’s clinical status and comorbidities over time with the goal of mitigating risk and maximizing benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Differentiated thyroid cancer overview
Thyroid cancer is the most common endocrine malignancy, occurring with a global age-standardized incidence of 10.1 per 100,000 women and 3.1 per 100,000 men [1]. Most thyroid carcinomas arise from the thyroid follicular epithelial cell and exist in a broad spectrum of histologic differentiation and behavior, ranging from common indolent classical papillary cancers to rare and aggressive undifferentiated/anaplastic cancers. The majority are considered well-differentiated thyroid cancers (DTCs) which is a collective term for common papillary thyroid cancers (PTCs) and rarer follicular thyroid cancers (FTCs). While PTCs and FTCs exhibit unique clinical features and molecular signatures, they are grouped together because of a close phenotypic resemblance to the thyroid follicular epithelial cell, a comparable excellent prognosis for most patients, and similar management strategies [2]. The incidence of DTC has been rapidly rising over time, mostly due to overdiagnosis of small PTCs [3]. Most patients with DTC present at an early stage and 10-year survival rates approach 99% for American Joint Committee on Cancer Stage I, and 94% for Stage II disease [4].
Management
Similar to the originating thyroid follicular cell, most DTCs express the TSH receptor, the sodium iodide symporter, and thyroglobulin, all of which have been leveraged to develop clinical tools unique to thyroid cancer [5]. The use of supraphysiologic thyroid hormone replacement will suppress TSH through hypothalamic and pituitary feedback inhibition and thereby suppress thyrocyte/cancer function and proliferation. Once normal thyroid tissue is surgically removed and/or ablated, serum thyroglobulin becomes an effective tumor marker. Lastly, the sodium iodine exchanger can be co-opted to deliver tumoricidal treatment with beta radiation through radioactive iodine (RAI), which was pioneered in the early 1940s and likely reflects the first “targeted” therapy for cancer [6].
Surgery is the most important initial treatment for DTC and serves as definitive therapy in many cases [7]. Active surveillance is also a well-validated alternative option for small tumors [8]. The American Thyroid Association (ATA) Risk of Recurrence System is widely used to risk-stratify patients after surgery and to guide surveillance intervals, recommended serum TSH suppression targets, and the timing and nature of additional treatments [2]. This review will highlight the importance of thyroid hormone medical therapy in patients with DTC, focusing on its physiologic use in the treatment of post-operative hypothyroidism, as well as its pharmacologic role through suppression of serum TSH.
Thyroid hormone replacement after thyroidectomy
Surgical approach and risk of post-operative hypothyroidism
Total thyroidectomy is defined as the complete removal of thyroid tissue, whereas a near-total thyroidectomy involves leaving a small remnant to reduce the risk of complications; both unequivocally lead to post-operative hypothyroidism. Hemithyroidectomy, otherwise known as partial thyroidectomy or thyroid lobectomy involves removal of a subtotal portion of the thyroid gland including the ipsilateral isthmus. Patients with small, localized tumors without imaging evidence of locoregional lymph node involvement are good candidates for conservative treatment with hemithyroidectomy. After hemithyroidectomy, 23.6–73% of patients require thyroid hormone supplementation to maintain euthyroidism [9, 10]. Multiple predictors for developing a hormone requirement after hemithyroidectomy have been identified, including pre-operative TSH levels >2.0–2.5, and lower thyroid volumes; the effect of female sex and positive anti-thyroid antibodies is debated [11, 12]. Up to two-thirds of patients who develop subclinical hypothyroidism after hemithyroidectomy may experience subsequent TSH normalization without treatment [13].
Physiologic rationale behind thyroid hormone replacement therapy
Under normal conditions, the thyroid produces 80–100 mcg of thyroxine/T4 and 3–6 mcg of triiodothyronine/T3, which are the dominant forms of thyroid hormone in circulation. The majority (80–85%) of systemic T3 is generated extra-thyroidally through 5’-monodeiodination of T4 by deiodinase enzymes. T3 exhibits a 10-fold greater affinity for binding intranuclear thyroid hormone receptors compared to T4 and thus thyroxine is mostly considered a pro-hormone. Thyroid hormone receptors exist in two major isoforms with differing tissue distributions, which mediate thyroid hormone’s myriad effects on energy homeostasis, metabolism, heat production, organ activity, etc. Thyroid hormone production is tightly regulated by the hypothalamic-pituitary-thyroid axis through a classic endocrine feedback loop. Low levels of circulating thyroxine/thyronine lead to thyrotropin-releasing hormone from the hypothalamus, which in concert with insufficient T4/T3, stimulates TSH secretion from thyrotrophs in the anterior pituitary. TSH binds to thyrotropin receptors on the thyrocyte basolateral membrane and stimulates nearly every step in hormonogenesis including iodine uptake and organification, and thyroid hormone synthesis and release [14, 15].
Practical aspects of post-operative thyroid hormone replacement therapy
The goal of thyroid hormone replacement therapy is the elimination of the signs/symptoms of hypothyroidism and the biochemical normalization of thyroid function tests, of which circulating TSH is most sensitive. The current standard of care involves postoperative initiation of oral levothyroxine, the synthetic but identical levo enantiomer of endogenous human thyroxine. Levothyroxine has an elimination half-life of approximately 6–7 days and oral bioavailability of 60–90%; most absorption occurs in the duodenum and ileum over 2–3 h. Approximately 1.6–1.7 mcg/kg/day (actual body weight) of levothyroxine is needed to normalize serum TSH in anatomically or functionally athyreotic adults, although higher doses (1.9–2.2 mcg/kg/day) are used when the goal is TSH suppression [16]. Levothyroxine is commercially available in tablets, gel capsules, and liquids. Gel and liquid formulations may be more rapidly absorbed [17]. There are many branded and generic products that are identical in their active hormone constituent but differ in excipients. Levothyroxine is typically administered in the morning on an empty stomach 30–60 min before eating, ideally with water, since foods and caloric beverages, especially those containing calcium, iron, and fiber, negatively impact absorption.
A weight-based dose of levothyroxine is typically started the day after total thyroidectomy. After hemithyroidectomy, a serum TSH is usually obtained 4–6 weeks after surgery to assess the adequacy of remnant hormone production. If serum TSH values are not at target, levothyroxine is often initiated at doses between 25–75 mcg; a common titration strategy involves adjustment in 12.5–25 mcg increments every 6–12 weeks with serial TSH testing that is gradually spaced out after stability [2, 18].
There are several pitfalls that can preclude the achievement of a euthyroid state. Unintentional iatrogenic hyperthyroidism is not infrequent [19, 20]. Patient non-adherence or malabsorption due to concomitant ingestion of levothyroxine with foods/drinks and/or gastrointestinal comorbidities is a common problem, especially since many patients find ideal administration practices to be inconvenient. There is a long list of potentially interfering medications that have been thoughtfully reviewed elsewhere; calcium/iron/multivitamin supplements, proton pump inhibitors, bile acid sequestrants, and phosphorus binders are common culprits [21]. Fluctuations in weight and advancing age can lead to changes in dose requirements over time. Furthermore, several endogenous and exogenous substances can interfere with thyroid hormone testing, the most notable of which is high-dose biotin supplementation, which can cause spurious hyperthyroidism. Anti-animal, anti-TSH, and non-specific cross-linking antibodies in patient sera can lead to persistent TSH abnormalities (typically, elevation). Assay interference should be considered when thyroid function testing does not respond to dose titration as expected, as well as when assay results do not fit with patient signs and symptoms [22].
Is there a role for T3-containing regimens?
While levothyroxine is widely considered a standard of care in the management of hypothyroidism, desiccated thyroid extracts (TEs) and synthetic liothyronine bear mention [18, 23]. Animal-derived TEs containing a mixture of thyroxine and thyronine were the dominant form of thyroid hormone replacement for nearly a hundred years after their first reported use in the early 1880s. Synthetic levothyroxine was synthesized and became available in the 1950s; over the next 30 years, levothyroxine became increasingly popular due to more consistent potency, comparable and then lower cost, and arguably lower rates of iatrogenic thyrotoxicosis, compared to TEs. When research in the 1970s identified that most serum thyronine was generated and regulated by enzymatic deiodination of thyroxine, coupled with levothyroxine’s superior ability to fully normalize newly developed TSH, T4, and T3 assays (animal-derived TE has a higher T3:T4 ratio compared to human thyroid tissue), levothyroxine monotherapy quickly grew to supplant TEs in widespread use [24].
Since that time, mounting evidence suggests that levothyroxine monotherapy may not normalize all signs, symptoms, and biochemical markers of euthyroidism in all individuals. Levothyroxine-treated patients have been reported to exhibit a 5–10% lower resting energy expenditure, higher total cholesterol and low-density lipoprotein levels, and modestly higher weight, compared to euthyroid controls [25]. Additionally, a subset of hypothyroid patients report persistent neurocognitive and other non-specific symptoms, and some patients are dissatisfied with current therapy [26]. Lower serum T3 levels, or sub-optimally elevated T4:T3 ratios have been proposed, with some controversy, as possible mechanisms for treatment-refractory symptoms. Calls for expanded study and use of TE and/or synthetic combination therapy with levothyroxine and liothyronine have naturally followed. The identification of deiodinase polymorphisms that may impact peripheral T4-to-T3 conversion and predict a positive response to T3-containing regimens has further intensified the debate. To date, over 17 randomized controlled trials have examined levothyroxine in comparison to TE and/or synthetic combination therapy. Results have been inconsistent, and conclusions/generalizations are hampered by significant methodologic concerns. A recent joint consensus statement from the American, British, and European Thyroid Associations was released to summarize the state of the field and to articulate proper methods for future well-designed clinical trials [27]. Hopefully, future trials will include sufficient symptomatic patients with post-operative hypothyroidism and inform when, in whom, and how combination therapy might be most effectively used.
Thyrotropin suppression therapy
History and benefits of TSH suppression
The development of RAI paved the way for the physiologic basis of TSH suppression in DTC, especially in younger individuals and those with metastatic disease. Prolonged hypothyroidism or TSH injections were observed to stimulate growth and iodine concentration in metastases from DTC [28, 29]. The first published case of TSH suppression therapy for DTC was in 1954, in which a 37-year-old woman with pulmonary metastases was treated with TE after RAI, which led to decreased chest iodine uptake, resolution of chest-X-ray findings, and improvement in pulmonary function [30]. Subsequent work by Mazzaferri revealed a significant drop in the risk of recurrence in patients with DTC > 1.5 cm when treated with total thyroidectomy followed by RAI and TSH suppression therapy [31, 32]. A meta-analysis of similar studies showed this approach led to a relative risk reduction of 71% in the combined endpoint of disease progression, recurrence, and death [33]. However, it was also increasingly recognized that TSH suppression is associated with long-term risks.
Long-term risks of TSH suppression
Long-term risks of TSH suppression for DTC are similar to those seen in cases of subclinical or overt hyperthyroidism, including cardiac morbidity (especially atrial tachyarrhythmias and cardiac remodeling), loss of bone density and higher fracture risk, impaired quality of life, and a question of increased risk of other cancers [34].
The cardiac adverse effects of hyperthyroidism are numerous: left ventricular hypertrophy, higher heart rates and atrial premature beats, and increased systolic function have all been observed in patients with DTC under TSH suppression [35]. Higher rates of atrial fibrillation have been reported, albeit inconsistently; the duration of hyperthyroidism may be more impactful than degree of TSH suppression, although levels <0.1 mIU/L appear enriched in morbidity [36, 37]. Traditional risk factors for atrial fibrillation such as age appear to remain independent risk factors [38]. Interestingly, one study showed that the cumulative risk of RAI was a major risk factor for atrial fibrillation, perhaps due to independent effects on the heart [36]. Higher cardiovascular mortality has also been observed in patients with DTC, with a 3.08 hazard ratio for each 10-fold decrease in geometric mean TSH level [39].
Supraphysiologic thyroid hormone levels accelerate bone turnover more so than bone formation, an effect which is disproportionately seen in post-menopausal women under TSH suppressive therapy for DTC, compared to premenopausal women [40]. Age, degree of TSH suppression, and duration of suppressive therapy are all associated with a higher risk of loss of bone mineral density and various markers of bone quality which, coupled with negative effects on muscle strength and weight, create a setup for fractures. Indeed, fracture risks are up to 4-fold higher in post-menopausal women with TSH levels lower than 0.1 mIU/L in one study, although it did not specifically evaluate individuals with DTC [41]. Higher fracture risk with low TSH levels has been confirmed through meta-analytic methods [42].
Quality of life appears to be lower in TSH-suppressed individuals with DTC, although it is challenging to sort out the effects from post-operative hypothyroidism and knowledge of a cancer diagnosis [43, 44]. Lastly, high free T4 levels, but interestingly not low TSH levels, have been associated with a higher risk (HR 1.42) of solid organ malignancies, especially lung and breast cancers.
A risk-adapted approach to TSH suppression
In addition to recognition of the risks of TSH suppression, it is now clear that not all patients benefit, and that the degree and duration of TSH suppression are important. Data supporting TSH suppression are unequivocally strongest for patients with known/active DTC persistence/recurrence or distant metastases, and patients who are at the highest risk for recurrence. However, suppression of TSH below the limit of detectability appears no better than suppression below 0.1 mIU/L [45]. Benefits appear much more modest or even non-existent in patients with low-to-intermediate risk tumors [46]. The National Thyroid Cancer Treatment Cooperative Study Group has been a seminal source of large-volume long-term prospective registry data examining TSH suppression and has demonstrated that moderately suppressed TSH values 0.1–0.4 mIU/L led to better outcomes in the first 5 years of follow-up, but not beyond 5 years [47]. Another large prospective study from the Netherlands demonstrated that median TSH values < 2 mIU/L were associated with better outcomes compared to >2 mIU/L [48].
Contemporary approaches to TSH suppression in DTC rely on a judicious patient risk-adapted, and tailored complication-mitigating approach. To date, the most prescriptive guidelines are the 2015 ATA Guidelines for Thyroid Cancer, in which recommended TSH targets are graded to the risk of DTC recurrence [2]. TSH targets are then modified during dynamic risk-re-stratification, which is performed after initial treatment with thyroid surgery and/or RAI and re-evaluated during subsequent long-term surveillance. An individual’s risk factors and comorbidities are used to further personalize TSH targets, with higher risk conditions leading to a stepwise de-escalation of the magnitude of suppression. A summary of ATA risk of recurrence groups and dynamic risk re-stratification category definitions are summarized in Table 1. Risk-adapted TSH targets for each category are represented in Table 2.
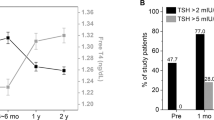
An area of active debate is whether patients with low-risk disease, especially those who have undergone lobectomy, need to have serum TSH levels maintained below 2 mIU/L [49]. When using a target of less than 2 mIU/L, 84% of patients required initiation of levothyroxine in one retrospective analysis [50]. Whether or not an optimal TSH target exists is unclear. To our knowledge, the only study to demonstrate the benefit of a specific TSH target after hemithyroidectomy is that by Park et al. which demonstrated a higher risk of recurrence in patients with a TSH > 1.85 mIU/L [51]. In contrast, two large retrospective studies by Lee et al. and Xu et al. did not demonstrate a higher risk of recurrence with TSH levels >2 mIU/L, or even when TSH levels were above the reference range; this finding persisted even amongst patients at intermediate risk of recurrence [52, 53]. A large prospective randomized controlled clinical trial investigated TSH levels between 0.3 and 1.99 uIU/mL versus 2.0 to 7.99 uIU/mL patients post-hemithyroidectomy and is currently underway in Korea [54]. Similar questions about the role of TSH suppression and/or targets arise in the care of patients under active surveillance for DTC. Higher TSH levels have been associated with the progression of papillary thyroid microcarcinomas under active surveillance, especially in younger people, in some but not all studies [55,56,57,58] Whether administration of levothyroxine to lower TSH levels abrogates risk of progression has not yet been proven. Prospective data are sorely needed, especially given the risk of bias in retrospective studies; levothyroxine is most likely to be offered to patients at higher risk of progression) [59].
While the guidelines have made great strides in canonizing a logical and evidence-based treatment approach, there are ongoing active efforts to better refine risk categories. The observation that 1–2% of patients with low-risk disease are found to have distant metastases emphasizes the need to better articulate the low-risk category so patients can be safely triaged to more conservative therapy [60, 61]. How to better integrate the risk of multifocality, degree, and location of extrathyroidal extension, positive margins, and emerging molecular data are areas of active investigation [62,63,64,65,66]. However, despite the availability of thoughtfully informed guidelines, and evidence that real-world TSH suppression practices significantly exceed the duration and extent of guideline recommendations; effective guideline implementation and dissemination to clinicians may be just as critical as guideline development itself [67].
References
M. Pizzato et al. The epidemiological landscape of thyroid cancer worldwide: Globocan estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 10(4), 264–272 (2022)
B.R. Haugen et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1), 1–133 (2016)
L. Davies, H.G. Welch, Current thyroid cancer trends in the United States. JAMA Otolaryngol. Head. Neck Surg. 140(4), 317–322 (2014)
S.H. Nam et al. A comparison of the 7th and 8th editions of the AJCC staging system in terms of predicting recurrence and survival in patients with papillary thyroid carcinoma. Oral. Oncol. 87, 158–164 (2018)
M. Schlumberger, S. Leboulleux, Current practice in patients with differentiated thyroid cancer. Nat. Rev. Endocrinol. 17(3), 176–188 (2021)
R.M. Tuttle et al. Controversies, consensus, and collaboration in the use of (131) I therapy in differentiated thyroid cancer: a joint statement from the American Thyroid Association, the European Association of nuclear medicine, the society of nuclear medicine and molecular imaging, and the European Thyroid Association. Thyroid 29(4), 461–470 (2019)
F. Vaisman et al. Initial therapy with either thyroid lobectomy or total thyroidectomy without radioactive iodine remnant ablation is associated with very low rates of structural disease recurrence in properly selected patients with differentiated thyroid cancer. Clin. Endocrinol. (Oxf.) 75(1), 112–119 (2011)
R.M. Tuttle, L. Zhang, A. Shaha, A clinical framework to facilitate selection of patients with differentiated thyroid cancer for active surveillance or less aggressive initial surgical management. Expert Rev. Endocrinol. Metab. 13(2), 77–85 (2018)
D. De Carlucci Jr et al. Thyroid function after unilateral total lobectomy: risk factors for postoperative hypothyroidism. Arch. Otolaryngol. Head. Neck Surg. 134(10), 1076–1079 (2008)
Z. Li et al. Prevalence of and risk factors for hypothyroidism after hemithyroidectomy: a systematic review and meta-analysis. Endocrine 70(2), 243–255 (2020)
N. Addasi, A. Fingeret, W. Goldner, Hemithyroidectomy for thyroid cancer: a review. Medicina (Kaunas) 56(11), 586 (2020). https://doi.org/10.3390/medicina56110586
M. Wilson et al. Postoperative thyroid hormone supplementation rates following thyroid lobectomy. Am. J. Surg. 220(5), 1169–1173 (2020)
S. Park et al. Clinical features of early and late postoperative hypothyroidism after lobectomy. J. Clin. Endocrinol. Metab. 102(4), 1317–1324 (2017)
P.R. Larsen, A.M. Zavacki, The role of the iodothyronine deiodinases in the physiology and pathophysiology of thyroid hormone action. Eur. Thyroid J. 1(4), 232–242 (2012)
B. Rousset et al. Chapter 2 Thyroid Hormone Synthesis And Secretion, in Endotext, K.R. Feingold, et al., Editors. 2000, MDText.com, Inc. Copyright © 2000-2023, MDText.com, Inc. South Dartmouth (MA)
P. Colucci et al. A review of the pharmacokinetics of levothyroxine for the treatment of hypothyroidism. Eur. Endocrinol. 9(1), 40–47 (2013)
E.V. Nagy et al. New formulations of levothyroxine in the treatment of hypothyroidism: trick or treat? Thyroid 31(2), 193–201 (2021)
J. Jonklaas et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid 24(12), 1670–1751 (2014)
J.G. Watsky, M.A. Koeniger, Prevalence of iatrogenic hyperthyroidism in a community hospital. J. Am. Board Fam. Pr. 11(3), 175–179 (1998)
S.K. Krishnan et al. High prevalence of iatrogenic hyperthyroidism in elderly patients with atrial fibrillation in an anticoagulation clinic. Mo Med 108(4), 280–283 (2011)
H.B. Burch, Drug effects on the thyroid. N. Engl. J. Med. 381(8), 749–761 (2019)
D.J. Halsall, E. English, V.K. Chatterjee, Interference from heterophilic antibodies in TSH assays. Ann. Clin. Biochem. 46(Pt 4), 345–346 (2009)
W.M. Wiersinga et al. 2012 ETA guidelines: the use of L-T4 + L-T3 in the treatment of hypothyroidism. Eur. Thyroid J. 1(2), 55–71 (2012)
E.A. McAninch, A.C. Bianco, The history and future of treatment of hypothyroidism. Ann. Intern Med. 164(1), 50–56 (2016)
E.A. McAninch, A.C. Bianco, The swinging pendulum in treatment for hypothyroidism: from (and toward?) combination therapy. Front Endocrinol. (Lausanne) 10, 446 (2019)
S.J. Peterson et al. An online survey of hypothyroid patients demonstrates prominent dissatisfaction. Thyroid 28(6), 707–721 (2018)
J. Jonklaas et al. Evidence-based use of levothyroxine/liothyronine combinations in treating hypothyroidism: a consensus document. Thyroid 31(2), 156–182 (2021)
M.A. Greer, E.B. Astwood, Treatment of simple goiter with thyroid. J. Clin. Endocrinol. Metab. 13(11), 1312–1331 (1953)
G. Crile Jr, Endocrine dependency of papillary carcinomas of the thyroid. Jama 195(9), 721–724 (1966)
H.W. Balme, Metastatic carcinoma of the thyroid successfully treated with thyroxine. Lancet 263(6816), 812–813 (1954)
E.L. Mazzaferri, R.L. Young, Papillary thyroid carcinoma: a 10-year follow-up report of the impact of therapy in 576 patients. Am. J. Med. 70(3), 511–518 (1981)
E.L. Mazzaferri et al. Papillary thyroid carcinoma: the impact of therapy in 576 patients. Med. (Baltim.) 56(3), 171–196 (1977)
N.J. McGriff et al. Effects of thyroid hormone suppression therapy on adverse clinical outcomes in thyroid cancer. Ann. Med. 34(7-8), 554–564 (2002)
B. Biondi, D.S. Cooper, Thyroid hormone suppression therapy. Endocrinol. Metab. Clin. North Am. 48(1), 227–237 (2019)
B. Biondi et al. Cardiac effects of long-term thyrotropin-suppressive therapy with levothyroxine. J. Clin. Endocrinol. Metab. 77(2), 334–338 (1993)
E.N. Klein Hesselink et al. Increased risk of atrial fibrillation after treatment for differentiated thyroid carcinoma. J. Clin. Endocrinol. Metab. 100(12), 4563–4569 (2015)
N. Pajamaki et al. Long-term cardiovascular morbidity and mortality in patients treated for differentiated thyroid cancer. Clin. Endocrinol. (Oxf.) 88(2), 303–310 (2018)
A. Abonowara et al. Prevalence of atrial fibrillation in patients taking TSH suppression therapy for management of thyroid cancer. Clin. Invest. Med. 35(3), E152–E156 (2012)
E.N. Klein Hesselink et al. Long-term cardiovascular mortality in patients with differentiated thyroid carcinoma: an observational study. J. Clin. Oncol. 31(32), 4046–4053 (2013)
K.A. Heemstra et al. The effects of thyrotropin-suppressive therapy on bone metabolism in patients with well-differentiated thyroid carcinoma. Thyroid 16(6), 583–591 (2006)
M.R. Turner et al. Levothyroxine dose and risk of fractures in older adults: nested case-control study. BMJ 342, d2238 (2011)
M.R. Blum et al. Subclinical thyroid dysfunction and fracture risk: a meta-analysis. JAMA 313(20), 2055–2065 (2015)
S. Tagay et al. Health-related quality of life, anxiety and depression in thyroid cancer patients under short-term hypothyroidism and TSH-suppressive levothyroxine treatment. Eur. J. Endocrinol. 153(6), 755–763 (2005)
M.H. Samuels et al. The effects of levothyroxine replacement or suppressive therapy on health status, mood, and cognition. J. Clin. Endocrinol. Metab. 99(3), 843–851 (2014)
S. Diessl et al. Impact of moderate vs stringent TSH suppression on survival in advanced differentiated thyroid carcinoma. Clin. Endocrinol. (Oxf.) 76(4), 586–592 (2012)
S. Leboulleux et al. Thyroidectomy without radioiodine in patients with low-risk thyroid cancer. N. Engl. J. Med. 386(10), 923–932 (2022)
A.A. Carhill et al. Long-term outcomes following therapy in differentiated thyroid carcinoma: NTCTCS registry analysis 1987–2012. J. Clin. Endocrinol. Metab. 100(9), 3270–3279 (2015)
G.C. Hovens et al. Associations of serum thyrotropin concentrations with recurrence and death in differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 92(7), 2610–2615 (2007)
L. Bischoff, M.R. Haymart, Optimal thyrotropin following lobectomy for papillary thyroid cancer: does it exist? Thyroid 32(2), 117–118 (2022)
M.A. Schumm et al. Frequency of thyroid hormone replacement after lobectomy for differentiated thyroid cancer. Endocr. Pr. 27(7), 691–697 (2021)
J.H. Park et al. The prognostic value of serum thyroid-stimulating hormone level post-lobectomy in low- and intermediate-risk papillary thyroid carcinoma. J. Surgical Oncol. 118(3), 390–396 (2018)
S. Xu et al. Optimal serum thyrotropin level for patients with papillary thyroid carcinoma after lobectomy. Thyroid 32(2), 138–144 (2022)
M.C. Lee et al. Postoperative thyroid-stimulating hormone levels did not affect recurrence after thyroid lobectomy in patients with papillary thyroid cancer. Endocrinol. Metab. (Seoul.) 34(2), 150–157 (2019)
E.K. Lee et al. A multicenter, randomized, controlled trial for assessing the usefulness of suppressing thyroid stimulating hormone target levels after thyroid lobectomy in low to intermediate risk thyroid cancer patients (MASTER): a study protocol. Endocrinol. Metab. (Seoul.) 36(3), 574–581 (2021)
H.I. Kim et al. Effect of TSH levels during active surveillance of PTMC according to age. Endocr. Relat. Cancer 29(4), 191–200 (2022)
I. Sugitani, Y. Fujimoto, K. Yamada, Association between serum thyrotropin concentration and growth of asymptomatic papillary thyroid microcarcinoma. World J. Surg. 38(3), 673–678 (2014)
Y. Ito et al. Thyroid-stimulating hormone, age, and tumor size are risk factors for progression during active surveillance of low-risk papillary thyroid microcarcinoma in adults. World J. Surg. 47(2), 392–401 (2023)
H.I. Kim et al. High serum TSH level is associated with progression of papillary thyroid microcarcinoma during active surveillance. J. Clin. Endocrinol. Metab. 103(2), 446–451 (2018)
M. Yamamoto, A. Miyauchi, Y. Ito, M. Fujishima, T. Sasaki, T. Kudo, Active Surveillance Outcomes of Patients with Low-Risk Papillary Thyroid Microcarcinoma According to Levothyroxine Treatment Status. Thyroid. 2023. https://doi.org/10.1089/thy.2023.0046. Epub ahead of print
A. Matrone et al. Postoperative thyroglobulin and neck ultrasound in the risk restratification and decision to perform 131I ablation. J. Clin. Endocrinol. Metab. 102(3), 893–902 (2017)
M. Mujammami et al. Long-term outcomes of patients with papillary thyroid cancer undergoing remnant ablation with 30 milliCuries radioiodine. Thyroid 26(7), 951–958 (2016)
R. Forleo et al. Minimal extrathyroidal extension in predicting 1-year outcomes: a longitudinal multicenter study of low-to-intermediate-risk papillary thyroid carcinoma (ITCO#4). Thyroid 31(12), 1814–1821 (2021)
V. Harries et al. Does macroscopic extrathyroidal extension to the strap muscles alone affect survival in papillary thyroid carcinoma? Surgery 171(5), 1341–1347 (2022)
H. Kim, H. Kwon, B.I. Moon, Association of multifocality with prognosis of papillary thyroid carcinoma: a systematic review and meta-analysis. JAMA Otolaryngol. Head. Neck Surg. 147(10), 847–854 (2021)
Z.F. Khan et al. Margin positivity and survival outcomes: a review of 14,471 patients with 1-cm to 4-cm papillary thyroid carcinoma. J. Am. Coll. Surg. 232(4), 545–550 (2021)
Y. Tao et al. BRAF V600E status sharply differentiates lymph node metastasis-associated mortality risk in papillary thyroid cancer. J. Clin. Endocrinol. Metab. 106(11), 3228–3238 (2021)
M. Papaleontiou et al. Thyrotropin suppression for papillary thyroid cancer: a physician survey study. Thyroid, 2021.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the review conception, outline, and literature review. The first draft of the manuscript was written by Benjamin Gigliotti. Both authors performed editing and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gigliotti, B.J., Jasim, S. Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy. Endocrine 83, 251–258 (2024). https://doi.org/10.1007/s12020-023-03548-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03548-8