Abstract
Purpose
Few studies have assessed the clinical features of pheochromocytoma and paraganglioma (PPGL) not producing excessive catecholamine. We aimed to clarify the clinical characteristics of PPGL patients with negative results for urinary metanephrines.
Methods
This is a retrospective cross-sectional study. We established a database by combining datasets from the Nationwide Cohort Study on the Development of Diagnosis and Treatment of Pheochromocytoma in Japan (PHEO-J) and the Advancing Care and Pathogenesis of Intractable Adrenal diseases in Japan (ACPA-J). We compared the clinical differences between PPGL patients with negative results for urinary metanephrines and those with catecholamine-producing PPGL.
Results
Five hundred PPGL patients in the combined database were analyzed. Among them, 31 were negative for metanephrines. PPGL with negative results for urinary metanephrines was significantly associated with extra-adrenal disease (Odds ratio (OR) 6.58, 95% CI (confidence interval) 3.03–14.3, p < 0.001), the presence of metastatic disease (OR 4.22, 95% CI 1.58–11.3, p = 0.004), and negativity on meta-iodobenzylguanidine (MIBG) scintigraphy (OR 0.15, 95% CI 0.03–0.77, p = 0.023).
Conclusions
Our findings demonstrate that PPGL patients with negative results for urinary metanephrines are associated with extra-adrenal lesions, metastatic disease, and negative MIBG findings. This suggests that PPGL patients with negative results for urinary metanephrines have a greater need for systemic whole-body imaging other than MIBG scintigraphy and close follow-up to monitor for metastasis than do patients with PPGL overtly producing excessive catecholamine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pheochromocytoma and paraganglioma (PPGL) are neuroendocrine tumors that originate, respectively, from chromaffin cells in the adrenal medulla and paraganglia in the sympathetic and parasympathetic nervous systems [1]. PPGLs are rare diseases with a combined incidence of 0.57 cases per 100,000 person-years [2]. Typically, these tumors produce catecholamines, which cause patients to develop such symptoms as hypertension, glucose intolerance, panic attacks, and arrhythmias [1]. Catecholamines are converted to metanephrines by catechol-O-methyltransferase (COMT) within the cells of the catecholamine-producing tumors and are then released into the circulation [3]. Consequently, for a diagnosis of PPGL, measurements of metanephrines are a more sensitive indicator than measurements of catecholamines [4]. However, in a portion of PPGL patients, metanephrines levels are not elevated. In the recent Endocrine Society guidelines, these patients were described as being rare [4], and there have been few reports analyzing their clinical features [5, 6]. The aim of the present study, therefore, was to clarify the characteristics of PPGL patients with negative results for urinary metanephrines. To do so, we compared the clinical characteristics of patients with catecholamine-producing PPGL and those with negative results for urinary metanephrines by an analysis of data from two large databases: the Advancing Care and Pathogenesis of Intractable Adrenal Diseases in Japan (ACPA-J) and the Nationwide Cohort Study on the Development of Diagnosis and Treatment of Pheochromocytoma in Japan (PHEO-J) registries.
Materials and methods
Study population
This is a retrospective, cross-sectional study. We obtained the clinical data on PPGL patients from the PHEO-J and ACPA-J databases. The PHEO-J was built to establish a disease registry for elucidation of prognoses and the effects of treatments in PPGL patients and to establish a method for early diagnosis of PPGL based on histopathological markers. The purpose of the ACPA-J is to build a registration system and cohort for patients with adrenal tumors and to produce new evidence to apply to the management of adrenal tumors and contribute to clinical guidelines. The ACPA-J focuses not only on patients with PPGL but also on those with other adrenal diseases, such as Cushing syndrome, subclinical Cushing syndrome, and adrenocortical cancer.
In the PHEO-J study, PPGL patients who visited outpatient clinics and hospitals between April 1, 2008, and March 31, 2012, were registered, regardless of their age. There were 178 participating institutions. In the ACPA-J study, patients aged 20 to 90 who were diagnosed with PPGL between January 2006 to December 2015 were enrolled. The ACPA-J study was established at 10 centers, including the National Center for Global Health and Medicine, National Hospital Organization Kyoto Medical Center, St. Marianna University Yokohama City Seibu Hospital, Tottori University Hospital, Tokyo Medical and Dental University, Osaka University Graduate School of Medicine, Kyoto University, Kanazawa University Graduate School of Medical Science, Tenri Hospital, and Saiseikai Yokohama-shi Tobu Hospital.
Patients enrolled in both studies were mainly treated with surgery; however, a few patients diagnosed with PPGL at each institution did not undergo surgery, based upon the assessment of data that included the levels of catecholamine metabolites and the results of 123I/131I-meta-iodobenzylguanidine (MIBG) scintigraphy or magnetic resonance imaging. Some patients were registered in both the PHEO-J and ACPA-J studies. For those patients, we analyzed the clinical data in the ACPA-J study.
The PHEO-J study collected the patients’ clinical characteristics, results of biochemical examinations, and radiological and pathological findings at the time of their initial diagnosis, at the time of enrollment, and six months after enrollment. These data were obtained throughout a web registry system. The ACPA-J study gathered these data at the time of enrollment, and no follow-up data is available at present. Collected data were registered to another web registry system. The present study was conducted using a dataset validated in March 2013 for the PHEO-J study and March 2019 for the ACPA-J study.
Of 188 PPGL patients enrolled in the ACPA-J study, we excluded 16 patients for whom there were no data on urinary metanephrine or normetanephrine. Forty PPGL patients were not categorized as having a catecholamine-producing PPGL or a PPGL with negative results for urinary metanephrines. Hence, they were not included in the analysis. Twenty-six patients who had been previously diagnosed at another institution were also excluded. A total of 939 PPGL patients were registered in the PHEO-J study. In the same way, we excluded 451 patients whose data on urinary metanephrine or normetanephrine were unavailable. Sixty-one patients were not categorized as having a catecholamine-producing PPGL or a PPGL with negative results for urinary metanephrines. Nine patients were removed due to double registration, and 24 were eliminated because they were also registered in the ACPA-J study.
Analysis
We collected data on age, sex, family history, and blood chemistry, including urinary adrenaline, urinary noradrenaline, urinary dopamine, urinary metanephrine, and urinary normetanephrine. We also gathered radiological findings, including the location of the tumor, the presence of metastasis, and the results of MIBG scintigraphy. Metastatic PPGL was diagnosed when there were tumors in non-chromaffin cells, such as lymph nodes, liver, lung, or bones. Patients who had already been diagnosed with PPGL and received surgery in other hospitals were excluded from the analysis. The information from MIBG scintigraphy was only available for patients registered in the ACPA-J.
For the present study, PPGL with negative results for urinary metanephrines was defined when both urinary metanephrine and normetanephrine did not exceed their upper reference limits. PPGL was defined as catecholamine-producing when either urinary metanephrine or normetanephrine exceeded a level three times higher than its upper reference limit.
We also collected data on metabolic parameters, including body mass index (BMI), fasting blood sugar, HbA1c [NGSP, National Glycohemoglobin Standardization Program], total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol (calculated using Friedewald equation), and triglyceride from the ACPA-J database.
Patients were considered to have hypertension or dyslipidemia after confirming a history of hypertension or dyslipidemia in the dataset. A diagnosis of glucose intolerance was made when PPGL patients had FPG ≥ 110 mg/dL, a 75 g oral glucose tolerance test with a two-hour plasma glucose level of 140 mg/dL or greater, HbA1c ≥ 6.2%, or were taking medication for diabetes mellitus.
Assay methods
Urinary adrenaline, noradrenaline, dopamine, metanephrine, and normetanephrine were measured using high-performance liquid chromatography (HPLC). We defined the upper reference limit for metanephrine as 0.18 mg/day and that for normetanephrine as 0.28 mg/day.
Statistical methods
We used JMP® ver. 13.2.1 developed by the SAS Institute Inc. and Stata®/SE ver. 14 developed by LightStone®. Results are presented as the median (interquartile range) and frequencies (positive/total observations) unless otherwise stated. The Wilcoxon signed-rank test was used for quantitative variables. Pearson’s χ2 test was used for categorical variables. The odds of an event occurring are expressed as the odds ratio (OR) with the 95% confidence interval (CI).
Ethics
The PHEO-J study was conducted in accordance with the Declaration of Helsinki and the guidelines for clinical studies published by the Ministry of Health and Labour, Japan and was approved by the Ethics Committee of the National Hospital Organization Kyoto Medical Center as the project-leading center and by the institutional ethics committees of the participating centers. The present retrospective study received ethical approval for the use of the opt-out consent method according to the Ethics Guidelines for Medical Research for Humans in Japan.
The ACPA-J study was conducted in accordance with the Declaration of Helsinki and the guidelines for clinical studies published by the Ministry of Health, Labour, and Welfare, Japan and was approved by the Ethics Committee of the National Center for Global Health and Medicine as the project-leading center and by the institutional ethics committees of the participating centers.
Results
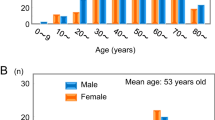
A total of 500 PPGL patients were analyzed in the present study: 106 from the ACPA-J study and 394 from the PHEO-J study. Their baseline characteristics are summarized in Table 1. The prevalence of PPGL patients with negative results for urinary metanephrines was 6.2%. The prevalence of patients with a family history of PPGL was 6.4%. Extra-adrenal PPGLs were observed in 16.2% of patients. The prevalence of patients with metastatic PPGL was 6.7%.
In a univariate logistic regression analysis, we found that extra-adrenal PPGL was positively associated with negative results for urinary metanephrines (OR 6.58, 95% CI 3.03–14.3, p < 0.001). The presence of metastasis was also positively associated with negative results for urinary metanephrines (OR 4.22, 95% CI 1.58–11.3, p = 0.004). The prevalence of MIBG positivity was negatively associated with negative results for urinary metanephrines (OR 0.15, 95% CI 0.03–0.77, p = 0.023). Other parameters, including sex, age at the time of the first diagnosis, and family history did not differ significantly between PPGL patients with negative results for urinary metanephrines and those with a catecholamine-producing PPGL. These results are summarized in Table 2.
We next assessed the metabolic parameters in patients with PPGL. The baseline metabolic parameters in PPGL patients in the ACPA-J study are shown in Table 3. The percentages of patients with hypertension, glucose intolerance, and dyslipidemia were 64.8%, 42.3%, and 39.4%, respectively. A comparison between the metabolic parameters in patients with negative results for urinary metanephrines and catecholamine-producing PPGL patients in the ACPA-J cohort is summarized in Table 4. The prevalence of hypertension and glucose intolerance were significantly lower in PPGL patients with negative results for urinary metanephrines (35.7% vs. 69.2%, p = 0.015, 15.4% vs. 46.2%, p = 0.036). Fasting blood sugar and HbA1c were also significantly lower in PPGL patients with negative results for urinary metanephrines (89 mg/dL vs. 115 mg/dL, p < 0.001, 5.6% vs. 6.1%, p = 0.007). BMI did not significantly differ between patients with negative results for urinary metanephrines and catecholamine-producing PPGL patients.
Discussion
Our study demonstrated that extra-adrenal PPGL and metastasis are positively associated with negative results for urinary metanephrines, while MIBG positivity is negatively associated with negative results for urinary metanephrines
We found that the prevalence of PPGL patients with negative results for urinary metanephrines was 6.2% in our cohort. Based on earlier spectrophotometry, Lenders et al. reported that 26 of 114 (22.8%) patients were negative for urinary total metanephrines. Based on an HPLC analysis, they also reported that only 3 of 105 (2.9%) patients showed negative results for urinary fractionated metanephrines [7]. A more recent study showed that the prevalence of PPGL patients with negative results for urinary deconjugated metanephrines was 16 of 226 patients (7.1%) [8]. In that study, the prevalence of patients with negative results for plasma-free metanephrines was lower than urinary levels (3.4% vs. 7.1%). If plasma-free metanephrines had been measured instead of urinary fractionated metanephrines in our study, the prevalence of patients with negative results for metanephrines in our cohort may have been lower than the present result. Heavner et al. reported that 7 of 78 (8.9%) PPGL patients were negative for serum biomarkers (4 patients were negative for urinary metanephrine, 2 were negative for plasma metanephrine, and 1 was negative for plasma catecholamine). In contrast to our results, there were no extra-adrenal or metastatic tumors in PPGL patients negative for catecholamines and their metabolites, whereas there were 6 extra-adrenal and 9 metastatic cases in patients with catecholamine-producing PPGL [5].
In a retrospective study from the Mayo Clinic, plasma or urinary metanephrines/catecholamines levels within the reference ranges were found in 51 of 248 (20.6%) patients with metastatic PPGL patients [9]. Similarly, PPGL patients with negative results for urinary metanephrines accounted for 18.8% (6/32) of PPGL patients with metastasis in our cohort. The proportion of patients with negative results for urinary metanephrines was higher among those with metastatic PPGL than among all PPGL patients. This implies an association between negative results for metanephrines and metastatic PPGL. In catecholamine-producing PPGL, catecholamines and their metabolites are higher in patients with metastatic PPGL than in those with non-metastatic PPGL. For example, Feng compared the clinical characteristics of 136 PPGL patients and showed that urinary metanephrine and normetanephrine were significantly higher in patients with metastatic than non-metastatic PPGL [10]. In their study, all PPGL patients exhibited elevation of catecholamines or their metabolites, whereas our study included PPGL patients with negative results for urinary metanephrines and catecholamines. We presume this discrepancy is attributable to differences in the characteristics of the enrolled patients between our study and theirs.
The clinical characteristics of PPGL patients with SDHx mutations were recently reported. The frequency of metastatic PPGL is reportedly higher among patients with SDHB mutations than among those without them [11, 12]. In addition, PPGL with SDHB mutations sometimes lacks tyrosine hydroxylase, which results in biochemically silent PPGL [13]. More recently, Dreijerink et al. similarly showed that SDHD mutations are associated with biochemically silent PPGL [14]. Neumann et al. found that the prevalence of extra-adrenal PPGL was significantly higher among patients with SDHB/SDHD mutations than among those without these mutations [15], while Timmers et al. showed that the sensitivity of MIBG scintigraphy was lower in patients with SDHB/SDHD mutations [16]. In the present study, PPGLs with negative results for urinary metanephrines were significantly associated with extra-adrenal PPGL, negative MIBG scintigraphy findings, and the presence of metastatic lesions. Considering the characteristics of SDHx-related PPGL, patients with SDHx mutations may account for a significant portion of the patients with negative results for urinary metanephrines in our cohort.
Park et al. assessed urinary excretion of catecholamines and their metabolites per tumor diameter and found that the amount of excreted vanillylmandelic acid per tumor diameter was significantly lower in patients who developed metastatic PPGL than in those who did not develop metastatic PPGL [17]. In addition, Grouzmann showed that tumoral catecholamines and metanephrine levels were lower in patients with extra-adrenal than adrenal PPGL [18]. Eisenhofer reported that PPGL patients with SDHB mutations showed lower tumoral catecholamines levels than did other tumors [19]. Eisenhofer et al. also reported that tumoral catecholamine content had a positive relationship with tumor-derived increases in metanephrine [20]. We suggest the higher proportion of negative results for urinary metanephrines in patients with metastatic PPGL may reflect the lower tumoral catecholamine content in patients with SDHB mutations or extra-adrenal PPGL, which are more prone to metastasis than other tumors.
The sensitivity of MIBG scintigraphy ranged between 85 and 88% in adrenal PPGL [4]. However, the sensitivity of MIBG scintigraphy is reportedly lower in other settings. It ranged between 56 and 75% in extra-adrenal PPGL [4], 50-59% in metastatic PPGL [16, 21, 22], and 45% in PPGL arising from SDHx mutations [16]. In the present study, we found that MIBG positivity was negatively associated with negative results for urinary metanephrines. This may be associated with a higher proportion of metastatic PPGL and extra-adrenal PPGL in patients with negative results for urinary metanephrines.
In the present study, the prevalence of metastatic PPGL was 6.7%, which is lower than in previous reports. For example, Eisenhofer et al. reported 35 of 365 (9.6%) PPGL patients were diagnosed with metastatic PPGL at the time of initial presentation. They also reported that another 70 patients were diagnosed with metastatic PPGL during their follow-up [19]. Another report conducted in South Korea showed that while 94 of 1048 (9.0%) patients had metastatic PPGL at the time of diagnosis, an additional 91 patients were diagnosed with metastatic PPGL during their follow-up period [23]. Considering that metastatic lesions often become apparent several years after the initial diagnosis, the lower prevalence of metastatic PPGL in our cohort is likely due in part to the lack of follow-up data in the present study. It may also partly derive from the lower sensitivity of MIBG scintigraphy for detecting metastatic lesions.
Among metabolic parameters, those associated with blood pressure and glucose intolerance were significantly worse in patients with catecholamine-producing PPGL. This is to be expected, considering the effects of catecholamines on blood pressure and glucose metabolism [24, 25]. A previous study showed the effects of catecholamines on body weight throughout a hypermetabolic and proinflammatory state [26]. Heavner et al. compared the clinical characteristics between patients with negative results for catecholamines and their metabolites and catecholamine-producing PPGLs [5]. They reported that BMIs were significantly higher in patients who were negative for catecholamines or their metabolites, though the prevalence of glucose intolerance did not significantly differ between the two groups. Our results are inconsistent with these results. This may reflect differences in the prevalence of obesity and glucose intolerance between Japan and the United States of America.
Limitations
There are several limitations to this study. The most important limitation is that genetic testing was not performed in our cohort. Second, the degree to which consanguinity was investigated was not uniform among the participating institutions. Third, no MIBG scintigraphy data were available in the PHEO-J registry. Fourth, according to the 4th edition of the WHO classification of endocrine tumors, all PPGLs may have metastatic potential. In the present study, however, a diagnosis of metastatic PPGL was based on radiological findings at the time of initial diagnosis [27, 28]. Fifth, this is a retrospective study. Sixth, we defined PPGL patients as negative for urinary metanephrines when both urinary metanephrine and normetanephrine did not exceed the upper reference limits. However, the definition of PPGL with negative results for metanephrines has not been unified in previous reports. Seventh, we did not have an adequate method for detecting dopamine-producing tumors. Although data on urinary dopamine were collected in the study, nearly all urinary dopamine is synthesized within the renal tubules from circulating DOPA through tubular DOPA-decarboxylase activity. Consequently, urinary dopamine is not an adequate indicator of dopamine-producing tumors. Eighth, the methods for measuring tumor size differed in the ACPA-J and PHEO-J studies. In the ACPA-J study, tumor size was determined by radiological imaging, whereas it was determined by measuring pathological specimens in the PHEO-J study. This made it impossible to include tumor size in the analysis. Finally, it is impossible to distinguish PPGL that did not produce catecholamines from tumors classified as PPGL with negative results for urinary metanephrines.
Conclusion
Our study revealed that PPGL patients without excessive catecholamines were more likely to have extra-adrenal lesions and metastatic disease. Because PPGL with negative results for urinary metanephrines was associated with negative MIBG scintigraphy findings, whole-body imaging other than MIBG scintigraphy is important for accurate localization PPGLs and for diagnosis of metastasis. In addition, these patients should be closely followed up and monitored for the emergence of metastatic lesions, even when there was no metastasis at the time of the first diagnosis.
Data availability
The data sets used or analyzed during the study are available from the corresponding author on reasonable request.
References
J.W. Lenders, G. Eisenhofer, M. Mannelli, K. Pacak,, Pheochromocytoma. Lancet. 366, 665–675 (2005). https://doi.org/10.1016/S0140-6736(05)67139-5
A.M.A. Berends, E. Buitenwerf, R.R. de Krijger, N.J.G.M. Veeger, A.N.A. van der Horst-Schrivers, T.P. Links, M.N. Kerstens,, Incidence of pheochromocytoma and sympathetic paraganglioma in the Netherlands: a nationwide study and systematic review. Eur. J. Intern. Med. 51, 68–73 (2018). https://doi.org/10.1016/j.ejim.2018.01.015
G. Eisenhofer, H. Keiser, P. Friberg, E. Mezey, T.T. Huynh, B. Hiremagalur, T. Ellingson, S. Duddempudi, A. Eijsbouts, J.W. Lenders, Plasma metanephrines are markers of pheochromocytoma produced by catechol-O-methyltransferase within tumors. J. Clin. Endocrinol. Metab. 83(6), 2175–2185 (1998). https://doi.org/10.1210/jcem.83.6.4870
J.W. Lenders, Q.Y. Duh, G. Eisenhofer, A.P. Gimenez-Roqueplo, S.K.G. Grebe, M.H. Murah, M. Naruse, K. Pacak, W.F. Young Jr., Endocrine society. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99(6), 1915–1942 (2014). https://doi.org/10.1210/jc.2014-1498
M.G. Heavner, L.S. Krane, S.M. Winters, M. Mirzazadeh, Pheochromocytoma diagnosed pathologically with previous negative serum markers. J. Surg. Oncol. 112(5), 492–495 (2015). https://doi.org/10.1002/jso.24031
K.A. Vanderveen, S.M. Thompson, M.R. Callstrom, W.F. Young Jr, C.S. Grant, D.R. Farley, M.L. Richards, G.B. Thompson, Biopsy of pheochromocytomas and paragangliomas: potential for disaster. Surgery 146(6), 1158–1166 (2009). https://doi.org/10.1016/j.surg.2009.09.013
J.W. Lenders, K. Pacak, M.M. Walther, W.M. Linehan, M. Mannelli, P. Friberg, H.R. Keiser, D.S. Goldstein, G. Eisenhofer, Biochemical diagnosis of pheochromocytoma: which test is best? JAMA 287(11), 1427–1434 (2002). https://doi.org/10.1001/jama.287.11.1427
G. Eisenhofer, A. Prejbisz, M. Peitzsch, C. Pamporaki, J. Masjkur, N. Rogowski-Lehmann, K. Langton, E. Tsourdi, M. Pęczkowska, S. Fliedner, T. Deutschbein, F. Megerle, H.J.L.M. Timmers, R. Sinnott, F. Beuschlein, M. Fassnacht, A. Januszewicz, J.W.M. Lenders, Biochemical diagnosis of chromaffin cell tumors in patients at high and low risk of disease: plasma versus urinary free or deconjugated O-Methylated Catecholamine metabolites. Clin. Chem. 64(11), 1646–1656 (2018). https://doi.org/10.1373/clinchem.2018.291369
O. Hamidi, W.F. Young Jr, N.M. Iñiguez-Ariza, N.E. Kittah, L. Gruber, C. Bancos, S. Tamhane, I. Bancos, Malignant pheochromocytoma and paraganglioma:272 patients over 55 years. J. Clin. Endocrinol. Metab. 102(9), 3296–3305 (2017). https://doi.org/10.1210/jc.2017-00992
F. Feng, Y. Zhu, X. Wang, Y. Wu, W. Zhou, X. Jin, R. Zhang, F. Sun, Z. Kasoma, Z. Shen, Predictive factors for malignant pheochromocytoma: analysis of 136 patients. J. Urol. 185(5), 1583–1590 (2011). https://doi.org/10.1016/j.juro.2010.12.050
A.P. Gimenez-Roqueplo, J. Favier, P. Rustin, C. Rieubland, M. Crespin, V. Nau, P. Khau Van Kien, P. Corvol, P.F. Plouin, X. Jeunemaitre, COMETE network.: mutations in the SDHB gene are associated with extra-adrenal and/or malignant phaeochromocytomas. Cancer Res. 63(17), 5615–5621 (2003)
L. Amar, J. Bertherat, E. Baudin, C. Ajzenberg, B. Bressac-de Paillerets, O. Chabre, B. Chamontin, B. Delemer, S. Giraud, A. Murat, P. Niccoli-Sire, S. Richard, V. Rohmer, J.L. Sadoul, L. Strompf, M. Schlumberger, X. Bertagna, P.F. Plouin, X. Jeunemaitre, A.P. Gimenez-Roqueplo, Genetic testing in pheochromocytoma or functional paraganglioma. J. Clin. Oncol. 23(34), 8812–8818 (2005). https://doi.org/10.1200/JCO.2005.03.1484
H.J. Timmers, K. Pacak, T.T. Huynh, M. Abu-Asab, M. Tsokos, M.J. Merino, B.E. Baysal, K.T. Adams, G. Eisenhofer, Biochemically silent abdominal paragangliomas in patients with mutations in the succinate dehydrogenase subunit B gene. J. Clin. Endocrinol. Metab. 93(12), 4862–4832 (2008). https://doi.org/10.1210/jc.2008-1093
K.M.A. Dreijerink, J.A. Rijken, C.J. Compaijen, H.J.L.M. Timmers, A.N.A. van der Horst-Schrivers, R.S. van Leeuwaarde, P.S. van Dam, C.R. Leemans, E.W.C.M. van Dam, C. Dickhoff, C.J. Dommering, P. de Graaf, G.J.C. Zwezerijnen, P. van der Valk, C.W. Menke-Van der Houven van Oordt, E.F. Hensen, E.P.M. Corssmit, E.M.W. Eekhoff, Biochemically silent sympathetic paraganglioma, pheochromocytoma, or metastatic disease in SDHD mutation carriers. J. Clin. Endocrinol. Metab. 104(11), 5421–5426 (2019). https://doi.org/10.1210/jc.2019-00202
H.P. Neumann, C. Pawlu, M. Peczkowska, B. Bausch, S.R. McWhinney, M. Muresan, M. Buchta, G. Franke, J. Klisch, T.A. Bley, S. Hoegerle, C.C. Boedeker, G. Opocher, J. Schipper, A. Januszewicz, C. Eng; European-American Paraganglioma Study Group, Distinct clinical features of paraganglioma syndromes associated with SDHB and SDHD gene mutations. JAMA 292(8), 943–951 (2004). https://doi.org/10.1001/jama.292.8.943
H.J. Timmers, C.C. Chen, J.A. Carrasquillo, M. Whatley, A. Ling, G. Eisenhofer, K.S. King, J.U. Rao, R.A. Wesley, K.T. Adams, K. Pacak, Staging and functional characterization of pheochromocytoma and paraganglioma by 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography. J. Natl. Cancer Inst. 104(9), 700–708 (2012). https://doi.org/10.1093/jnci/djs188
J. Park, C. Song, M. Park, S. Yoo, S.J. Park, S. Hong, B. Hong, C.S. Kim, H. Ahn, Predictive characteristics of malignant pheochromocytoma. Korean J. Urol. 52(4), 241–246 (2011). https://doi.org/10.4111/kju.2011.52.4.241
E. Grouzmann, O. Tschopp, F. Triponz, M. Matter, S. Bilz, M. Brändle, T. Drechser, S. Sigrist, H. Zulewski, C. Henzen, S. Fischli, K. Abid, Catecholamine metabolism in paraganglioma and pheochromocytoma: similar tumors in different sites? PLoS ONE 10(5), e0125426 (2015). https://doi.org/10.1371/journal.pone.0125426
G. Eisenhofer, J.W. Lenders, G. Siegert, S.R. Bornstein, P. Friberg, D. Milosevic, M. Mannelli, W.M. Linehan, K. Adams, H.J. Timmers, K. Pacak, Plasma methoxytyramine: a novel biomarker of metastatic pheochromocytoma and paraganglioma in relation to established risk factors of tumour size, location and SDHB mutation status. Eur. J. Cancer 48(11), 1739–1749 (2012). https://doi.org/10.1016/j.ejca.2011.07.016
G. Eisenhofer, M.M. Walther, T.T. Huynh, S.T. Li, S.R. Bornstein, A. Vortmeyer, M. Mannelli, D.S. Goldstein, W.M. Linehan, J.W. Lenders, K. Pacak, Pheochromocytomas in von Hippel-Lindau syndrome and multiple endocrine neoplasia type 2 display distinct biochemical and clinical phenotypes. J. Clin. Endocrinol. Metab. 86(5), 1999–2008 (2001). https://doi.org/10.1210/jcem.86.5.7496
H.J.L.M. Timmers, C.C. Chen, J.A. Carrasquillo, M. Whatley, A. Ling, B. Havekes, G. Eisenhofer, L. Martiniova, K.T. Adams, K. Pacak, Comparison of 18F-Fluoro-L-DOPA, 18F-Fluoro-Deoxyglucose, and 18F-Fluorodopamine PET and 123I-MIBG Scintigraphy in the localization of pheochromocytoma and paraganglioma. J. Clin. Endocrinol. Metab. 94(12), 4757–4767 (2009). https://doi.org/10.1210/jc.2009-1248
I. Ilias, C.C. Chen, J.A. Carrasquillo, M. Whatley, A. Ling, K.T. Adams, S. Perera, K. Pacak, Comparison of 6-18F-Fluorodopamine PET with 123I-Metaiodobenzylguanidine and 111In-Pentetreotide scintigraphy in localization of nonmetastatic and metastatic pheochromocytoma. J. Nucl. Med. 49(10), 1613–1619 (2008). https://doi.org/10.2967/jnumed.108.052373
J.H. Kim, H. Moon, J. Noh, J. Lee, S.G. Kim, Epidemiology and prognosis of pheochromocytoma/paraganglioma in Korea: a nationwide study based on the national health insurance service. Endocrinol. Metab. 35(1), 157–164 (2020). https://doi.org/10.3803/EnM.2020.35.1.157
S.M. Zuber, V. Kantorovich, K. Pacak, Hypertension in pheochromocytoma: characteristics and treatment. Endocrinol. Metab. Clin. North Am. 40(2), 295–311 (2011). https://doi.org/10.1016/j.ecl.2011.02.002
H. Komada, Y. Hirota, A. So, T. Nakamura, Y. Okuno, H. Fukuoka, G. Iguchi, Y. Takahashi, K. Sakaguchi, W. Ogawa, Insulin secretion and insulin sensitivity before and after surgical treatment of pheochromocytoma or paraganglioma. J. Clin. Endocrinol. Metab. 102(9), 3400–3405 (2017). https://doi.org/10.1210/jc.2017-00357
O. Petrák, D. Haluzíková, P. Kaválková, B. Štrauch, J. Rosa, R. Holaj, A. Brabcová Vránková, D. Michalsky, M. Haluzík, T. Zelinka, J. Widimsky Jr., Changes in energy metabolism in pheochromocytoma. J. Clin. Endocrinol. Metab. 98(4), 1651–1658 (2013). https://doi.org/10.1210/jc.2012-3625
R.V. Lloyd, R.Y. Osamura, G. Kloppel, J. Rosai, WHO classification of tumours: pathology and genetics of tumours of endocrine organs. 4th ed. (IARC, Lyon), 2017)
A.K. Lam, Update on adrenal tumours in 2017 World Health Organization (WHO) of endocrine tumours. Endocr. Pathol. 28(3), 213–227 (2017). https://doi.org/10.1007/s12022-017-9484-5
Acknowledgements
We thank the PHEO-J and ACPA-J study members for their collaboration.
Authors’ contributions
Akiyuki Kawashima analyzed the data and drafted the manuscript. Masakatsu Sone devised the concept and design of this study and revised the manuscript. Nobuya Inagaki, Mitsuhide Naruse, and Akiyo Tanabe contributed to the interpretation of data and revised the manuscript. Kentaro Okamoto, Mika Tsuiki, Shoichiro Izawa, Michio Otsuki, Shintaro Okamura, Takamasa Ichijo, Takuyuki Katabami, Yoshiyu Takeda, Takanobu Yoshimoto contributed to the acquisition of data.
Funding
This study was funded as a part of the JRAS by a Research Grant from the Japan Agency for Medical Research and Development (AMED) under Grant Numbers JP17ek0109122 and JP20ek0109352, and the National Center for Global Health and Medicine, Japan (27-1402 and 30-1008). PHEO-J was supported by a Health Labour Sciences Research Grant for Research on Measures for Intractable Diseases from the Ministry of Health, Labour, and Welfare in Japan (H23-Nanchi-ippan-099).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All studies analyzed in the present study were in accordance with the Declaration of Helsinki and the guidelines for clinical studies published by the Ministry of Health and Labour, Japan and were approved by the Ethics Committee of the National Hospital Organization Kyoto Medical Center as the project-leading center and by the institutional ethics committees of the participating centers.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kawashima, A., Sone, M., Inagaki, N. et al. Pheochromocytoma and paraganglioma with negative results for urinary metanephrines show higher risks for metastatic diseases. Endocrine 74, 155–162 (2021). https://doi.org/10.1007/s12020-021-02816-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02816-9