Abstract
Purpose
To evaluate the epidemiology, presentation and management of hypoparathyroidism in Canada. Hypoparathyroidism is associated with significant morbidity and poor quality of life. We present baseline results from the Canadian National Hypoparathyroidism Registry, a prospective observational study evaluating hypoparathyroidism in Canada.
Methods
Our study enrolled 130 patients with hypoparathyroidism. Patients were followed every 6 months with clinical and lab assessments. We present baseline data in this manuscript.
Results
Seventy percent (91/130) of patients had postsurgical hypoparathyroidism, 30% (39/130) of patients had nonsurgical hypoparathyroidism due to autoimmune, genetic or idiopathic causes, and a molecular diagnosis was confirmed in 11 of these 39 patients. Pseudohypoparathyroidism was confirmed in 4/39 patients, DiGeorge syndrome in 2/39 patients, Barakat syndrome with a mutation in the GATA3 gene in 1/39, and activating mutations of the CASR gene in 3/39 patients with nonsurgical hypoparathyroidism. Renal complications with nephrocalcinosis or nephrolithiasis were present in 27% (14/52) of patients with postsurgical disease and 17% (4/24) of patients with nonsurgical hypoparathyroidism. Basal ganglia calcification was noted on imaging in 15% (n = 5/34) of patients with postsurgical hypoparathyroidism and 37% (n = 7/19) of patients with nonsurgical hypoparathyroidism.
Conclusions
Hypercalciuria was more commonly seen in those with renal complications of nephrocalcinosis, nephrolithiasis or CKD, and hyperphosphatemia was more commonly seen in those with basal ganglia calcification. Hospitalization occurred in 28% of those with postsurgical hypoparathyroidism and 46% of those with nonsurgical hypoparathyroidism. Hypoparathyroidism is associated with significant morbidity. Effective strategies to reduce the short-and long-term complications of hypoparathyroidism need to be developed and evaluated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoparathyroidism is a rare endocrine disorder characterized by low serum calcium in the presence of a low or inappropriately normal parathyroid hormone (PTH) level. This occurs usually in association with hyperphosphatemia and relative hypercalciuria [1,2,3,4]. The most common cause of hypoparathyroidism is neck surgery (~75% of cases) resulting in injury to the parathyroid glands or their blood supply [1, 4,5,6,7]. Surgeries which may result in hypoparathyroidism include neck dissection (5%), parathyroidectomy (21%), and thyroidectomies (partial and/or total) (47%) [8]. Hypoparathyroidism is considered to be permanent if hypocalcemia persists for more than 6 months following surgery and it is estimated that 7.6% of patients develop hypoparathyroidism following surgery, of whom 25% are chronic and 75% are transient [8].
Non-surgical causes of hypoparathyroidism account for ~25% of cases and include autoimmune and genetic variants resulting in destruction or abnormal formation, function or agenesis of the parathyroid glands. Infiltrative causes of hypoparathyroidism include granulomatous disease (sarcoidosis, amyloidosis), metastatic cancer and mineral deposition (copper or iron). Hypomagnesemia or hypermagnesemia, radiation destruction, and mitochondrial disorders can also result in hypoparathyroidism [1]. PTH resistant states (pseudohypoparathyroidism), characterized by target organ resistance to PTH, present with a similar biochemical profile as hypoparathyroidism with low serum calcium, high serum phosphate and normal vitamin D levels, but PTH levels are elevated. We included patients with pseudohypoparathyroidism in the nonsurgical causes of hypoparathyroidism.
The presentation of hypoparathyroidism is dependent on the severity, duration and rate of onset of the hypocalcemia [1]. Classical symptoms include numbness and tingling in the hands, feet or face as well as muscle twitching or cramping [1]. Depressed mood, confusion, irritability as well as cognitive impairment may also be present. Seizures may develop with significant hypocalcemia and pulmonary complications such as bronchospasm and/or laryngospasm may develop [1]. Cardiac complications include bradyarrthymia due to prolonged QT interval as well as congestive heart failure, which can result due to depressed systolic function [3, 4].
Long term renal complications of hypoparathyroidism include renal impairment with development of chronic kidney disease as well as nephrolithiasis or nephrocalcinosis. Hypercalciuria, hyperphosphatemia and recurrent episodes of hypercalcemia appear to be associated with an increased risk of renal complications [1, 9]. An increased risk of basal ganglia calcification, seizures, and cataracts has also been observed in patients with hypoparathyroidism. In a longitudinal cohort study in the US, renal calcification was seen in 31% of patients who had undergone renal imaging, and basal ganglia calcification was seen in 52% of patients [10]. CKD was significantly more prevalent amongst individuals with hypoparathyroidism in comparison to eucalcemic healthy age-matched controls. Non-surgical hypoparathyroidism patients are at an increased risk of hospitalization secondary to seizures in comparison to postsurgical hypoparathyroidism. (nonsurgical hypoparathyroidism HR 10.05 (95% CI 5.39–18.72) vs. postsurgical hypoparathyroidism HR 3.82 (95% CI 2.15–6.79)), cataracts (HR 4.21 (95% CI 2.13–8.34)) and ischemic heart disease (HR 2.01(95% CI 1.31–3.09)) [11, 12]. An increased risk of neuropsychiatric illness has also been demonstrated in both nonsurgical and surgical hypoparathyroidism patients (HR 2.45(95% CI 1.78–3.35)). No overall increase in mortality or fracture risk has been reported in a Danish study [12]. Patients with hypoparathyroidism have been noted to have an increased risk of epilepsy (HR 1.65 (95% CI 1.12–2.44) [13]. Hypercalcemia has been associated with renal failure and death as noted in the Scottish population-based study [13].
Prospective longitudinal data comprehensively evaluating etiology, presentation, complications, and management of patients with hypoparathyroidism is currently limited with only published abstract data from our study in the Canadian population. In this paper, we present the baseline results of our prospective study of adults with hypoparathyroidism in Canada.
Canadian national hypoparathyroidism registry
The Canadian National Hypoparathyroidism Registry (CNHR) was established in 2014 following approval by the Hamilton Integrated Research Ethics Board (HiREB) and is the first registry designed to collect data on Canadian patients with chronic hypoparathyroidism. The registry was developed with the following objectives:
-
1.
Evaluate the etiology and presenting symptoms of patients with hypoparathyroidism.
-
2.
Evaluate current treatment practices in Canada.
-
3.
Assess differences in presentation based on etiology of the disease.
-
4.
Evaluate the association of biochemical data and the risk of developing short- and long-term complications of hypoparathyroidism including nephrolithiasis, nephrocalcinosis or basal ganglia calcification in comparison to those without complications.
-
5.
Assess fracture risk in Canadian patients with hypoparathyroidism.
-
6.
Evaluate mortality in patients with hypoparathyroidism.
Currently there is limited data available on the epidemiology of chronic hypoparathyroidism in Canada, including prevalence, management, treatment and mortality. The CNHR was established to fill this knowledge gap and obtain a greater understanding of the natural course of hypoparathyroidism in Canada.
Methods
Patients
We recruited male and female adults at or above the age of 18 years with chronic hypoparathyroidism (defined as a low serum calcium in the presence of low or inappropriately normal PTH levels for at least 6 months prior to enrolment) and patients that were receiving conventional therapy (calcium supplements and active vitamin D metabolites) for at least 6 months prior to enrollment, conventional therapy and PTH(1–34), PTH(1–34) alone, PTH(1–84) plus conventional therapy or PTH(1–84) alone. In Canada PTH(1–84) is currently not available. We have been evaluating PTH (1–84) in clinical trials. Following completion of the clinical trial with PTH (1–84) we were able to obtain PTH (1–84) for 3 of our patients with hypoparathyroidism with approval by Health Canada. These patients on PTH (1–84) have been included in our CNHR. Patients with either postsurgical or nonsurgical hypoparathyroidism were included as well as patients with pseudohypoparathyroidism. We excluded patients with transient hypoparathyroidism (hypoparathyroidism which resolved within 6 months of surgery) and subjects unable to provide informed consent. This study was approved by the McMaster University ethics review board HiREB in October 2014.
Recruitment centres
The primary center for patient assessment and data analysis was the Calcium Disorders Clinic at McMaster University, which is a tertiary care referral center for parathyroid disease in Canada. Patients were also recruited from McMaster University, Western University, University of Toronto as well as specialized academic as well as community centers from across Canada.
Design
This is a prospective observational registry designed to follow patients with chronic hypoparathyroidism. We report on the baseline data from this prospective observational study in Canadian patients with hypoparathyroidism.
Data collection
A standardized form was used to extract patient information from medical records. Baseline characteristics including demographics (age, age of onset, gender, and duration of disease), etiology and current pharmacologic therapy were obtained. The primary outcome of this registry is to evaluate the biochemical profile in patients with hypoparathyroidism including albumin-corrected serum calcium, ionized calcium, serum phosphate, serum magnesium, 24 h urine calcium excretion and 25 dihydroxy vitamin D as well as the prevalence and incidence of short-and long-term complications of hypoparathyroidism. Laboratory tests were obtained every 6 months. Secondary outcomes include the proportion of patients with complications of hypoparathyroidism including renal, neurologic, ocular and skeletal complications including fractures. Hospitalization rates, morbidity, and mortality are secondary outcomes. Data on hypoparathyroidism-related hospitalization was collected every 6 months. Renal complications were evaluated by lab profile as well as renal ultrasound. Soft tissue calcification in the brain was evaluated by either computed tomography (CT) scan or magnetic resonance imaging (MRI). Fracture risk was evaluated by the Canadian Association of Radiologists and Osteoporosis Canada (CAROC) tool [14, 15].
Statistical analysis
Descriptive summaries are presented as mean ± standard deviation (SD) or as median and intervals for continuous variables and counts and percentage (%) for categorical data. Measures of correlation were explored between renal and basal ganglia calcification and laboratory profile. A t-test was used to determine if there was a significant difference in the biochemical profile of patients with and without renal and basal ganglia calcification. Clinical laboratory tests were summarized. Statistical analysis was conducted using Microsoft Excel 2010 (Microsoft, Redmond, WA, USA) and statistical significance was determined if p < 0.05.
Results
Patient characteristics
We enrolled 130 patients with chronic hypoparathyroidism from October 2014 to January 2020. The mean age was 54 (range 21–97) yrs and the average age of onset of hypoparathyroidism was 42 yrs. The mean duration of hypoparathyroidism was 12 yrs with 76% of participants being female (N = 99). Ninety-one patients (70%) had postsurgical hypoparathyroidism with the most common indication for neck surgery (55%, n = 50/91) being thyroid cancer (Table 1). Non-surgical hypoparathyroidism was seen in 30% of patients (N = 39). Amongst patients with nonsurgical hypoparathyroidism, 26% (10/39) of cases had autoimmune hypoparathyroidism, 10% (4/39) had pseudohypoparathyroidism, 5% (2/39) had DiGeorge syndrome, 3/39 (8%) had activating mutations of the calcium sensing receptor (CASR) gene, 1/39 (3%) (had Barakat Syndrome with a mutation in the GATA 3 gene, and 46% (18/39) of patients had idiopathic hypoparathyroidism.
Medications
All 130 patients were on calcium supplements, 85% were on calcitriol (N = 111), 2% were on alphacalcidiol (N = 2) and 70% were on vitamin D2 or D3 therapy (N = 91). Approximately 26% were on magnesium supplements (N = 34) and 30% were on hydrochlorothiazide (N = 39). A total of 33 patients were on PTH therapy, 30 patients were on PTH(1–34) and 3 patients were on PTH(1–84) (Table 2).
Biochemical profile
Among patients with chronic hypoparathyroidism the mean albumin-corrected serum calcium was 2.11 ± 0.17 (range 1.52–2.58) mmol/L, ~42% of patients had serum calcium levels in the normal reference range (2.15 and 2.60 nmol/L) and 58% of patients has serum calcium levels below 2.15 mmol/L. The mean ionized serum calcium was 1.13 ± 0.09 (range 0.75–1.41) mmol/L. The mean serum phosphate level was in the upper range of normal at 1.34 ± 0.3 (0.9–1.45) mmol/L and ~29% of patients had elevated serum phosphate levels (>1.45 mmol/L). The mean calcium-phosphate product was in the normal reference range at 2.88 ± 0.53 (1.76–6.41) mmol2/L2. The calcium-phosphate product was elevated (above 5.5 mmol2/L2) in only one patient (0.9%). The mean serum magnesium level was normal at 0.79 ± 0.08 (0.53–0.99) mmol/L and 12% of patient had serum magnesium levels below 0.7 mmol/L. Approximately 16% of patients had serum 25 hydroxy vitamin D levels <75 nmol/L with the mean 25 hydroxy vitamin D being in the normal reference range at 101.6 ± 28.2 (49–179) nmol/L. The mean eGFR was 77.4 ± 22.1 (32–118) mL/min and ~23% had stage 3 chronic kidney disease with an eGFR <60 mL/min. Hypercalciuria was defined as a 24 h urine calcium excretion >7.5 mmol/day and was observed in 36% of participants with hypoparathyroidism. The mean 24 h urine calcium was 6.05 ± 3.36 mmol/d (Table 3).
Complications of hypoparathyroidism
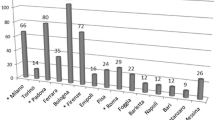
Of the 130 patients, 58% (n = 76) completed renal imaging of whom 52 patients (68%) had postsurgical hypoparathyroidism and 24 patients (32%) had nonsurgical hypoparathyroidism). Nephrocalcinosis or nephrolithiasis was observed in 27% (n = 14/52) of the patients with postsurgical disease and 17% (n = 4/24) of the patients with nonsurgical hypoparathyroidism. Fifty-three patients (41%) completed brain imaging with either CT or MRI scan of whom 34 patients (64%) had postsurgical hypoparathyroidism and 19 patients (36%) had nonsurgical hypoparathyroidism (n = 19). Basal ganglia calcification was observed in 15% (5 of 34) patients with postsurgical hypoparathyroidism and 37% (7 of the 19) patients with nonsurgical hypoparathyroidism (Fig. 1).
We evaluated the association between biochemical parameters and long-term complications of hypoparathyroidism (nephrolithiasis, nephrocalcinosis, and basal ganglia calcification) (Table 4). Amongst patients with renal complications (nephrocalcinosis or nephrolithiasis) hypercalciuria was more commonly seen in those with renal complications (24 h urine calcium of 7.50 ± 4.9 mmol/d) in comparison to patients without renal complications (6.18 ± 3.9 mmol/d, p = 0.18). Albumin-corrected serum calcium levels (p = 0.21), ionized calcium (p = 0.16) and serum phosphate (p = 0.37) were not significantly associated with nephrocalcinosis or nephrolithiasis. There was no difference in the calcium-phosphate product between patients with and those without renal calcification. The mean calcium-phosphate product was 2.71 ± 0.5 mmol2/L2 in patients with nephrocalcinosis or nephrolithiasis and was 2.71 ± 0.48 mmol2/L2 in patients without nephrocalcinosis or nephrolithiasis). The calcium-phosphate product was also not different between patients with basal ganglia calcification (2.68 ± 0.69 mmol2/L2) and patients without basal ganglia calcification (2.68 ± 0.45 mmol2/L2). Phosphate levels were numerically higher however in those with basal ganglia calcification with mean serum phosphate level of 1.38 ± 0.3 mmol/L in comparison to 1.27 ± 0.2 mmol/L in patients without basal ganglia calcification, however this was not statistically significant p = 0.10). Albumin-corrected serum calcium (p = 0.07) was not significantly associated with basal ganglia calcification.
Skeletal health
Out of the 65 patients for whom fracture risk was calculated (using the CAROC tool) ~81% of patients were at low risk (N = 53), 5% were at moderate risk (N = 3) and 14% were at high risk (N = 9).
Hospitalization
Forty-four patients (34%) required hospitalization. Patients with nonsurgical disease were twice as likely to be hospitalized than those with postsurgical disease with 46% (n = 18/39) non-surgical and 28% (n = 26/91) postsurgical being hospitalized. Multiple hospitalization for hypoparathyroidism-related symptoms occurred in eight patients (8/44). The remaining 36 patients had only 1 hospitalization each. Three patients (3/44) were hospitalized twice, two patients (2/44) were hospitalized three times, 1 patient (1/44) was hospitalized four times, 1 patient (1/44) was hospitalized six times, and 1 patient (1/44) was hospitalized eight times.
Among patients with nonsurgical hypoparathyroidism, common causes for hospitalization were symptomatic hypocalcemia (28%, n = 11), seizure (17%, n = 3), infection (5%, n = 2), cardiovascular disease (5%, n = 2), hypercalcemia (3%, n = 1), tetany (3%, n = 1) and renal surgery (3%, n = 1) (Fig. 2).
In patients with postsurgical hypoparathyroidism the most common causes for hospitalization were hypocalcemia (15%, n = 14), hypercalcemia (7%, n = 6), cardiovascular disease (4%, n = 4), kidney stone (2%, n = 2), infection (2%, n = 2), cancer (1%, n = 1), and seizure (1%, n = 1).
Discussion
The baseline data from the prospective CNHR in 130 patients with chronic hypoparathyroidism provides valuable insights into the etiology, pharmacologic management, biochemical profile, and complications of hypoparathyroidism. The prospective nature of our study is unique compared to previously published studies which have been limited in sample size (given the rarity of this disease), duration or design being retrospective.
In our study the prevalence of postsurgical and nonsurgical hypoparathyroidism was consistent with published international data [10, 11, 13]. Despite treatment with calcium, activated vitamin D and hydrochlorothiazide as well as PTH (in 26% of patients), hypocalcemia was still present in a significant number of patients and was the most common cause of hospitalization in both the postsurgical and nonsurgical hypoparathyroidism patient populations. This illustrates the fact that hypocalcemia is still not well controlled and is unfortunately relatively common in patients despite being on drug therapy for hypoparathyroidism. Hospitalizations were more commonly noted in patients with nonsurgical disease in comparison to postsurgical disease. This may be due to the fact that patients with nonsurgical disease may also have significant comorbidity in association with hypoparathyroidism such as adrenal insufficiency or type 1 diabetes mellitus in those with autoimmune polyendocrine syndrome 1 and other conditions such as cardiac disease in DiGeorge syndrome or renal complications in those with HDR syndrome (hypoparathyroidism, sensorineural deafness, renal dysplasia) due to GATA binding protein 3 gene mutation.
Individuals with postsurgical hypoparathyroidism may also be identified with the condition earlier then their nonsurgical counterparts. An earlier diagnosis may be possible post-surgery as the possibility of hypoparathyroidism is considered in these patients as a complication of surgery. Whereas in those with nonsurgical hypoparathyroidism the diagnosis may not be considered and may be delayed resulting in presentation at an advanced stage with more complications and more frequent hospitalizations. Infections were noted in both groups and may be due to deficiency in 1,25dihydroxyvitamin D levels as a result of low or inadequate PTH. Vitamin D has important effects on the immune response and vitamin D deficient states may be associated with a higher number of infections. Vitamin D deficiency reduces the ability of white blood cells to mature and to produce antigens necessary to prevent infections and appears to have an important role in the immune response [16, 17]. Standard of care treatment with calcitriol may lower the risk of infection as noted by other investigators [9], but this needs further evaluation.
Renal and intracranial calcification are long-term complications of chronic hypoparathyroidism [4]. In our study, nephrocalcinosis or nephrolithiasis was seen in 27% of patients with postsurgical hypoparathyroidism and in 17% of patient with nonsurgical hypoparathyroidism in whom renal imaging was completed. A significant number of patients had renal complications and this supports the findings of other international studies including the Danish patient registry in whom renal complications were noted to be significantly more prevalent with a HR 3.67 (95% CI 2.41–5.59) in comparison to eucalcemic controls [11].
In our study basal ganglia calcification was present in 15% of patients with postsurgical hypoparathyroidism and 37% of patients with nonsurgical hypoparathyroidism in whom brain imaging was completed. The prevalence of basal ganglia calcification is less than the findings from the US chart review, which identified basal ganglia calcification in 52% of patients with hypoparathyroidism having with brain imaging with CT [10]. In a retrospective registry-based study of 537 patients with chronic hypoparathyroidism, cerebral calcification was seen in 75% of patients with imaging completed. The prevalence of cerebral calcification in this retrospective study is significantly higher than what has been reported in the literature [10, 11, 18, 19]. The exact cause of basal ganglia calcification is not known, however elevated calcium-phosphate product is thought to be a contributing factor [20,21,22]. In our study, basal ganglia calcification was seen in fewer patients with hypoparathyroidism and this may reflect the fact that the mean calcium phosphate product in almost all of our patients was in the normal reference range. We still had patients with basal ganglia calcification despite a calcium phosphate product (55 mg2/dL2 (4.4 mmol2L2)) in the reference range. This suggests that the ideal calcium-phosphate product may actually be lower than has been suggested and needs to be reconsidered. We did note that serum phosphate was numerically higher in patients with basal ganglia calcification 1.38 ± 0.3 in comparison to those without basal ganglia calcification 1.27 ± 0.2 however this difference was not statistically significant (p = 0.10). Prospective evaluation in a larger patient population is required to further evaluate the relationship between serum phosphate and intracranial calcification.
The effect of hypoparathyroidism on skeletal health is currently not well characterized. A decrease in bone remodeling, bone formation and cortical porosity has been associated with hypoparathyroidism [1, 23]. Bone mineral density appears to be well maintained and cortical porosity is reduced on evaluation by HRpQCT [24]. A decrease in the risk of upper extremity fracture was noted in patients with postsurgical hypoparathyroidism [25]. Other investigators have noted increased vertebral deformities in patients with postsurgical hypoparathyroidism despite normal BMD [26]. Similar findings were noted with a higher prevalence of vertebral fractures in those with hypoparathyroidism in comparison to eucalcemic controls [27].
In our study fracture risk was calculated for 65 patients using the CAROC tool. We found that the majority of patients (N = 53, ~81%) were at low risk (<10% risk of a major osteoporotic fracture over the next 10 years.) A small number (N = 3, 5%) were at moderate fracture risk (10–20% fracture risk over the next 10 years) and 14% (N = 9) were at high risk. Patients at moderate or high risk of fracture had other important risk factors for fracture including steroid use or early menopause. The impact of hypoparathyroidism on bone strength is not well understood at this time. Further prospective evaluation of skeletal health in patients with hypoparathyroidism utilizing imaging modalities evaluating the quality of bone with trabecular bone score, vertebral fracture assessment and HRpQCT will enhance our understanding of the impact of hypoparathyroidism on bone strength.
The majority of our patients (89%) were receiving standard of care with calcium, vitamin D, activated vitamin D and hydrochlorothiazide. In our study 26% of patients were on PTH therapy and the majority of patients were on PTH(1–34) as PTH(1–84) is currently not approved in Canada. PTH therapy has been evaluated in patients with hypoparathyroidism and PTH replacement therapy enables reductions in the doses of calcium and active vitamin D while maintaining serum calcium in the normal reference range [1, 28,29,30]. Reduction in serum phosphate levels and improvement in quality of life have also been observed [1, 28, 31]. This registry will prospectively evaluate the effects of pharmacologic therapy on the biochemical profile and risk of renal and skeletal complications.
Conclusion
Hypoparathyroidism is associated with a significant disease burden and may lead to hospitalization in a large number of patients. Renal complications of nephrocalcinosis and nephrolithiasis were present in 22% of treated patients despite maintenance of a calcium phosphate product in the desired reference range (<4.4 mmol2/L2). In our study basal ganglia calcification was noted in fewer patients then has been reported previously (15% of the postsurgical hypoparathyroidism patients and 37% of the nonsurgical hypoparathyroidism patient population) and this may be a reflection of the fact that our patients did have a mean calcium phosphate product which was in the normal reference range. However we still noted this complication in a significant number of patients. This suggests that the ideal calcium phosphate product needs to be reconsidered. Given the proportion of patients with complications of hypoparathyroidism it is important to monitor patients and optimize pharmacologic therapy with the goal of maintaining serum calcium levels in the low-normal reference range, avoiding hyperphosphatemia, hypercalcemia, hypercalciuria and renal and extraskeletal calcification. Fracture risk was low in the absence of traditional osteoporosis risk factors amongst patients with hypoparathyroidism.
Data availability
Data available upon request.
References
A.A. Khan, C. Koch, S.H.M. Van Uum, J.P. Baillargeon, J. Bollerslev, M.L. Brandi, C. Marcocci, L. Rejnmark, R. Rizzoli, M.Z. Shrayyef, R.V. Thakker, B.O. Yildiz, B. Clarke, Standards of Care for Hypoparathyroidism in Adults. Eur. J. Endocrinol. 180(3), P1–P22 (2019)
M.L. Brandi, J.P. Bilezikian, D. Shoback, R. Bouillon, B.L. Clarke, R.V. Thakker, A.A. Khan, J.T. Potts, Management of hypoparathyroidism: summary statement and guidelines. J. Clin. Endocrinol. Metab. 101, 2273–2283 (2016)
H. Al-Azem, A.A. Khan, Hypoparathyroidism. Best Pract. Res: Clin. Endocrinol. Metab. 26, 517–522 (2012)
J.P. Bilezikian, A. Khan, J.T. Potts Jr, M.L. Brandi, B.L. Clarke, D. Shoback, H. Jüppner, P. D’Amour, J. Fox, L. Rejnmark, L. Mosekilde, M.R. Rubin, D. Dempster, R. Gafni, M.T. Collins, J. Sliney, J. Sanders, Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J. Bone Miner. Res. 26(10), 2317–2337 (2011)
D. Shoback, Clinical practice. Hypoparathyroidism. N. Engl. J Med. 359, 391–403 (2008)
D.M. Shoback, J.P. Bilezikian, A.G. Costa, D. Dempster, H. Dralle, A.A. Khan, R.Bouillon, Presentation of hypoparathyroidism: etiologies and clinical features. J. Clin. Endocrinol. Metab. 101, 2300–2312 (2016).
M. Mannstadt, J.P. Bilezikian, R.V. Thakker, F.M. Hannan, B.L. Clarke, L. Rejnmark, D.M. Shoback, Hypoparathyroidism. Nat. Rev. Dis. Primers 3, 17055 (2017)
J. Powers, K. Joy, A. Ruscio, H. Lagast, Prevalence and incidence of hypoparathyroidism in the United States using a large claims database. J. Bone Miner. Res. 28(12), 2570–2576 (2013)
L. Underbjerg, T. Sikjaer, L. Rejnmark, Long-Term Complications in Patients With Hypoparathyroidism Evaluated by Biochemical Findings: a Case-Control Study. J. Bone Miner. Res. 33(5), 822–831 (2018).
D.M. Mitchell, S. Regan, M.R. Cooley, K.B. Lauter, M.C. Vrla, C.B. Becker, M. Mannstadt, Long-term follow-up of patients with hypoparathyroidism. J. Clin. Endocrinol. Metab. 97, 4507–4514 (2012)
L. Underbjerg, T. Sikjaer, L. Mosekilde, L. Rejnmark, Cardiovascular and renal complications to postsurgical hypoparathyroidism: a Danish nationwide controlled historic follow-up study. J. Bone Miner. Res. 28, 2277–2285 (2013)
B.L. Clarke, E.M. Brown, M.T. Collins, H. Jüppner, P. Lakatos, M.A. Levine, M.M. Mannstadt, J.P. Bilezikian, A.F. Romanischen, R.V. Thakker, Epidemiology and Diagnosis of Hypoparathyroidism. J. Clin. Endocrinol. Metab. 101(6), 2284–2299 (2016)
T. Vadiveloo, P.T. Donnan, C.J. Leese, K.J. Abraham, G.P. Leese, Increased mortality and morbidity in patients with chronic hypoparathyroidism: a population-based study. Clin. Endocrinol. (Oxf) 90(2), 285–292 (2019)
K. Siminoski, W.D. Leslie, H. Frame, A. Hodsman, R.G. Josse, A. Khan, B.C. Lentle, J. Levesque, D.J. Lyons, G. Tarulli, J.P. Brown, Recommendations for bone mineral density reporting in Canada: a shift to absolute fracture risk assessment. J. Clin. Densitom. 10(2), 120–123 (2007)
B. Lentle, A.M. Cheung, D.A. Hanley, W.D. Leslie, D. Lyons, A. Papaioannou, S. Atkinson, J.P. Brown, S. Feldman, A.B. Hodsman, A.S. Jamal, R.G. Josse, S.M. Kaiser, B. Kvern, S. Morin, K. Siminoski, Scientific Advisory Council of Osteoporosis Canada. Osteoporosis Canada 2010 guidelines for the assessment of fracture risk. Can. Assoc. Radiol. J. 62(4), 243–250 (2011)
Y. Abu-Amer, Z. Bar-Shavit, Impaired bone marrow-derived macrophage differentiation in vitamin D deficiency. Cell Immunol. 151(2), 356–368 (1993)
C. Cui, P. Xu, G. Li, Y. Qiao, W. Han, C. Geng, D. Liao, M. Yang, D. Chen, P. Jiang, Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: role of renin-angiotensin system. Redox. Biol. 26, 101295 (2019 Sep)
M.R. Rubin, D.W. Dempster, H. Zhou, E. Shane, T. Nickolas, J. Sliney Jr, S.J. Silverberg, J.P. Bilezikian, Dynamic and structural properties of the skeleton in hypoparathyroidism. J. Bone Miner. Res. 23(12), 2018–2024 (2008)
R. Goswami, R. Sharma, V. Sreenivas, N. Gupta, A. Ganapathy, S. Das, Prevalence and progression of basal ganglia calcification and its pathogenic mechanism in patients with idiopathic hypoparathyroidism. Clin. Endocrinol. (Oxf). 77(2), 200–206 (2012)
J. Bollerslev, L. Rejnmark, C. Marcocci, D.M. Shoback, A. Sitges-Serra, W. Van Biesen, O.M. Dekkers, European Society of Endocrinology clinical guideline: treatment of chronic hypoparathyroidism in adults. Eur. J. Endocrinol. 173(2), G1–20 (2015)
J.P. Bilezikian, M.L. Brandi, N.E. Cusano, M. Mannstadt, L. Rejnmark, R. Rizzoli, J.T. Potts, Management of hypoparathyroidism: Present and future. J. Clin. Endocrinol. Metab. 101, 2313–2324 (2016)
M.R. Rubin, N.E. Cusano, W.W. Fan, Y. Delgado, C. Zhang, A.G. Costa, S. Cremer, E. Dworakowski, J.P. Bilezikian, Therapy of hypoparathyroidism with PTH (1–84): a prospective six year investigation of efficacy and safety. J. Clin. Endocrinol. Metab. 101, 2742–2750 (2016)
M.R. Rubin, Skeletal Manifestations of Hypoparathyroidism. Bone. 120, 548–555 (2019)
N.E. Cusano, K.K. Nishiyama, C. Zhang, M.R. Rubin, S. Boutroy, D.J. McMahon, X.E. Guo, J.P. Bilezikian, Noninvasive Assessment of Skeletal Microstructure and Estimated Bone Strength in Hypoparathyroidism. J. Bone Miner. Res. 31(2), 308–316 (2016)
L. Underbjerg, T. Sikjaer, L. Mosekilde, L. Rejnmark, Postsurgical hypoparathyroidism-risk of fractures, psychiatric diseases, cancer, cataract, and infections. J. Bone Miner. Res. 29(11), 2504–2510 (2014)
M.L. Mendonça, F.A. Pereira, M.H. Nogueira-Barbosa, L.M. Monsignore, S.R. Teixeira, P.C. Watanabe, L.M. Maciel, F.J. de Paula, Increased vertebral morphometric fracture in patients with postsurgical hypoparathyroidism despite normal bone mineral density. BMC Endocr. Disord. 13, 1 (2013)
H. Chawla, S. Saha, D. Kandasamy, R. Sharma, V. Sreenivas, R. Goswami, Vertebral Fractures and Bone Mineral Density in Patients With Idiopathic Hypoparathyroidism on Long-Term Follow-Up. J. Clin. Endocrinol. Metab. 102(1), 251–258 (2017)
T. Sikjaer, L. Rejnmark, L. Rolighed, L. Heickendorff, L. Mosekilde, The effect of adding PTH (1–84) to conventional treatment of hypoparathyroidism: a randomized, placebo-controlled study. J. Bone Miner. Res. 26, 2358–2370 (2011)
T. Sikjaer, L. Rolighed, A. Hess, A. Fuglsang-Frederiksen, L. Mosekilde, L. Rejnmark, Effects of PTH(1–84) therapy on muscle function and quality of life in hypoparathyroidism: results from a randomized controlled trial. Osteoporos. Int. 25, 1717 (2014)
M. Mannstadt, B.L. Clarke, T. Vokes, M.L. Brandi, L. Ranganath, W.D. Fraser, P. Lakatos, L. Bajnok, R. Garceau, L. Mosekilde, H. Lagast, D. Shoback, J.P. Bilezikian, Efficacy and safety of recombinant human parathyroid hormone (1-84) in hypoparathyroidism (REPLACE): a double-blind, placebo-controlled, randomised, phase 3 study. Lancet Diabetes Endocrinol. 1(4), 275–283 (2013)
T.J. Vokes, M. Mannstadt, M.A. Levine, B.L. Clarke, P. Lakatos, K. Chen, R. Piccolo, A. Krasner, D.M. Shoback, J.P. Bilezikian, Recombinant Human Parathyroid Hormone Effect on Health-Related Quality of Life in Adults With Chronic Hypoparathyroidism. J. Clin. Endocrinol. Metab. 103(2), 722–731 (2018)
Funding
No funding was received for the development of the Canadian National Hypoparathyroidism Registry or for the analysis of the data. Research grants received for unrelated research projects: A.K.: Alexion, Amgen, Takeda, Ascendis, Chugai, Radius, Ultragenyx. A.M.: Merck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The ethical approval for the present study was obtained from the Hamilton Integrated Research Ethics Board HiREB (Project No: 14-664-D).
Informed consent
Informed consent was obtained from all participants per GCP guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khan, A.A., AbuAlrob, H., Punthakee, Z. et al. Canadian national hypoparathyroidism registry: an overview of hypoparathyroidism in Canada. Endocrine 72, 553–561 (2021). https://doi.org/10.1007/s12020-021-02629-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02629-w