Abstract
Purpose
Previous studies revealed that high serum uric acid (SUA) levels correlated with increased triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio. However, evidence is lacking regarding whether TG/HDL-C is an independent risk factor or just a simple marker of hyperuricemia. We aimed to investigate the relationship between TG/HDL-C and the risk of hyperuricemia in Chinese population.
Methods
This retrospective cohort study involved 15,198 subjects (43.14 ± 13.13 years, 54.9% men) who were free of hyperuricemia at baseline. The association between TG/HDL-C and the risk of hyperuricemia, in the total sample and stratified by subgroups, was examined by multiple logistic regression analyses.
Results
During 4 years follow-up, hyperuricemia occurred in 2365 (15.6%) participants. The cumulative incidence of hyperuricemia was significantly elevated with increasing TG/HDL-C quartiles (5.9, 10.8, 18.4, and 27.5%, respectively). After multivariate adjustment, the odds ratio for hyperuricemia in the highest compared with the lowest quartile of TG/HDL-C was 1.80 (95% confidence interval [CI] 1.49, 2.18), and each SD increment of TG/HDL-C ratio caused a 10% additional risk for hyperuricemia. Moreover, subgroup analyses showed that the association between TG/HDL-C and the risk of hyperuricemia was more pronounced in women and normal-weight adults. The results were consistent when analyses were restricted to participants without metabolic syndrome.
Conclusions
TG/HDL-C ratio was positively related to the risk of hyperuricemia in Chinese population, particularly in women and normal-weight individuals. These findings suggested the potential of TG/HDL-C ratio to serve as an independent risk indicator in the prevention of hyperuricemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperuricemia is a condition characterized by abnormally elevated levels of serum uric acid (SUA) and it has become a great challenge to public health concerns worldwide [1]. Hyperuricemia is a common metabolic disease in Europe and the United States, affecting more than 20% of the general population [2, 3]. In China, the prevalence of hyperuricemia ranged from 13% to 25%, and it will continue to increase because of the alteration in diet, lifestyle and population age structure [4, 5]. Hyperuricemia has long been recognized as the major etiologic factor in gout, an excruciatingly painful inflammatory arthritis [6]. Moreover, accumulating evidence suggests that hyperuricemia is closely related to the presence and severity of multiple comorbidities that affect longevity and well-being, such as cardiovascular disease, type 2 diabetes mellitus (T2DM), chronic kidney disease, non-alcoholic fatty liver disease and cancer [7,8,9,10]. Accordingly, identifying and managing the risk factors of hyperuricemia may be a promising strategy to prevent and delay adverse outcomes of hyperuricemia.
It is well established that lipid abnormalities, especially increased triglycerides (TG) levels together with decreased high-density lipoprotein cholesterol (HDL-C) levels, are commonly presented in hyperuricemia patients [11,12,13,14]. On the other hand, compelling evidence indicated that hyperuricemia is closely linked to insulin resistance [15, 16]. Since the ratio of triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) not only contained pivotal components of hyperlipidemia, but also formulated as a proxy for insulin resistance [17, 18], we hypothesized that TG/HDL-C ratio may potentially associate with the development of hyperuricemia. However, it has yet to be elucidated whether the TG/HDL-C ratio could serve as a risk indicator to optimize the prevention of hyperuricemia. In addition, multiple related risk factors, such as gender, drinking, and body mass index (BMI), could affect the ratio of TG/HDL-C as well as the risk of hyperuricemia [5, 19]. Therefore, we conducted a retrospective cohort study to investigate the relationship between TG/HDL-C and hyperuricemia, and to evaluate whether this association was modified by other related factors.
Methods
Study design and study subjects
This single-center, retrospective cohort study was conducted based on the population who participated in their physical examination in the Health Management Center of the Third Xiangya Hospital (Changsha, China). All of the data were obtained from the database of the Third Xiangya Hospital, and we have previously published studies using this database [20,21,22]. In the present study, we included 19,795 subjects between 20 and 85 years old whose data were available at 2012 and 2016. If the subjects in this study had more than one annual exam, we only used the first record of that year to avoid double counts. Subjects who met the following criteria were excluded: (1) no available data on key variables, including SUA, TG and HDL-C (n = 277); (2) with hyperuricemia at baseline (n = 2094); (3) taking lipid-lowering drugs (n = 125); (4) with chronic kidney disease (n = 2101). Finally, a total of 15,198 subjects were included in the present study (Fig. 1).
Ethics approval for the study protocol and analysis of the data was obtained from the Medical Ethics Committee of Third Xiangya Hospital. All of the work has been carried out in accordance with the Declaration of Helsinki, and informed written consent was obtained from all subjects.
Data collection and measurements
All subjects were interviewed by trained interviewers using questionnaires to collect information on age, sex, education level, cigarette smoking, drinking habits and medical history. Smoking status was classified as a current smoker (smoking in the past 6 months) and non-smoker (cessation of smoking for more than 6 months or never smoking). The same rules were implemented to define drinking status. Anthropometric measurements were performed with the subjects wearing light clothing. Waist circumference (WC) was measured at umbilical level in a standing position with light expiration. Body weight and height were measured in a standing position using calibrated weighing scales, and BMI was calculated as weight (kg) divided by height (m) squared. Blood pressure (BP) was measured twice on the right arm with a mercury sphygmomanometer while the subjects were in a seated position after at least 10 min of rest. The final BP value was obtained by averaging the values of the measurements. Blood samples were collected from the antecubital vein after an overnight fasting and stored at −20 °C until analyzed. Fasting blood glucose (FBG), total cholesterol (TC), TG, low-density lipoprotein cholesterol (LDL-C), HDL-C, SUA, albumin (ALB), creatinine (SCr) and alanine aminotransferase (ALT) were determined using standard laboratory methods and tested using an auto-analyzer (Hitachi 7600-110; Hitachi, Tokyo, Japan). Renal function was estimated by calculated glomerular filtration rate (eGFR) using a modified Chinese equation based on inulin clearance as follows: eGFR (mL/min/1.73 m2) = 175 × (Scr in enzymatic method)−1.234 × age− 0.287 (× 0.79, if female) [23].
Definitions of obesity, hypertension, diabetes, metabolic syndrome, and hyperuricemia
Participants with a BMI ≥ 25.0 kg/m2 were defined as overweight/obesity according to the World Health Organization (WHO) criteria [24]. Hypertension was defined on the basis of the Joint National Committee 7 report as systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg, or individuals who were on antihypertensive medications or a prior diagnosis of hypertension [25]. T2DM was diagnosed according to the American Diabetes Association diagnostic criteria in subjects with FBG ≥7.0 mmol/L, or using hypoglycemic drugs or a previous diagnosis of diabetes [26]. Modified NCEP-ATPIII guideline that specifically applied for Asians was used for classification of metabolic syndrome [27]. Participants with three or more of these criteria were considered to have metabolic syndrome: (1) TG ≥ 1.7 mmol/L or lipid-lowering drugs; (2) SBP ≥ 130 mmHg or DBP ≥ 85 mmHg or antihypertensive drugs; (3) FBG ≥ 5.6 mmol/L or medications for diabetes; (4) HDL-C < 1.04 mmol/L for men or <1.29 mmol/L for women; and (5) WC ≥ 90 cm in men or ≥80 cm in women. Hyperuricemia was defined as SUA ≥ 420 mmol/L in men or ≥360 mmol/L in women, or any treatment for hyperuricemia [4]. Subjects who were free of hyperuricemia in 2012 but received a diagnosis of hyperuricemia in 2016 were defined as incident hyperuricemia cases.
Statistical analysis
The entire study population was divided into four groups according to their quartiles of baseline TG/HDL-C ratio (Q1: < 0.459, Q2: 0.459~0.753, Q3: 0.754~1.296, Q4: > 1.296), and the parameters were compared between these four groups. The data were presented as numbers with percentages for categorical variables, and as means ± standard deviation or as medians (25th and 75th percentile) values for continuous variables. The analysis of one-way analysis of variance (ANOVA) or a post hoc analysis of the least significant difference (LSD) was used to compare the means of the normally distributed continuous variables, otherwise, the Kruskal–Wallis test was used. The Chi-square test was used for categorical variables. The odds ratios (ORs) and 95% confidence intervals (CIs) for hyperuricemia were calculated using the logistic regression model after adjustment for multiple confounders. Model 1 was adjusted for age and sex. In Model 2, the analysis was adjusted for age, sex, education status, smoking, drinking, overweight/obesity, hypertension, and diabetes. In addition to the confounders analyzed in Model 2, Model 3 included admission of TC, LDL-C, eGFR, ALB, and ALT. Model 4 added baseline SUA based on Model 3. We also estimated the risk of hyperuricemia associated with TG/HDL-C as continuous variables in all models. In addition, sensitivity analyses were conducted to assess the robustness of the results by rerunning all the models in participants without metabolic syndrome at baseline (N = 12,813). Further stratification analyses were conducted to obtain ORs and 95% CIs for incident hyperuricemia in various subgroups. All analyses were performed using IBM SPSS version 22.0 (IBM Corp., Armonk, NY, USA) and two-tailed P values of <0.05 were considered statistically significant.
Results
Demographic data and clinical characteristics
The baseline demographic and clinical characteristics of the study participants are summarized in Table 1. The mean age of 15,198 subjects was 43.14 ± 13.13 years and 54.9% of participants were men. The median TG/HDL-C ratio was 0.75 (0.46–1.28). Compared with lower TG/HDL-C levels, subjects who had higher TG/HDL-C levels were more likely to be older and males. Subjects with higher TG/HDL-C levels also had a tendency to have higher BMI, WC, BP, FBG, TG, TC, LDL-C, SUA, SCr, ALT, and ALB. Besides, the frequencies of overweight/obesity, hypertension, diabetes, current smoking or drinking habit also increased with TG/HDL-C levels. On the other hand, there was an inverse association between HDL-C, eGFR as well as levels of education and TG/HDL-C ratio.
Association between TG/HDL-C and the risk of hyperuricemia
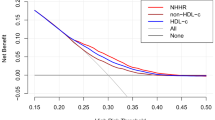
During 4 years follow-up, hyperuricemia occurred in 2365 (15.6%) participants. Figure 2 A depicts that the incidence of hyperuricemia increased from 5.9% to 27.5% from the lowest TG/HDL-C quartile to the highest in all subjects. Table 2 illustrates the multiple adjusted associations between TG/HDL-C and incident hyperuricemia. In all four models of the statistical analysis, the ORs for hyperuricemia increased across the TG/HDL-C quartiles. After adjusting for age and sex (Model 1), the OR for hyperuricemia in the comparison between the highest and lowest quartiles of TG/HDL-C was 4.37 (95% CI 3.71–5.16). After further adjusting for all confounders (Model 4), the association between TG/HDL-C and incident hyperuricemia was also significant. Compared with the first quartile, the ORs for hyperuricemia in the second, third and fourth TG/HDL-C quartiles were 1.25 (95% CI 1.04–1.50), 1.60 (95% CI 1.33–1.92), and 1.80 (95% CI 1.49–2.18), respectively. Moreover, the OR of hyperuricemia per 1-SD increase in the TG/HDL-C was 1.10 (95% CI, 1.05–1.16). In addition, we tried a broader diagnostic criterion (SUA levels ≥360 mmol/L) [28, 29] to reevaluate the association between TG/HDL-C ratio and incident hyperuricemia, and our results indicated that TG/HDL-C ratio was also positively related to the risk of hyperuricemia (Supplemental Fig. 1 and Table S1).
To completely rule out the impact of metabolic syndrome on the relationship between TG/HDL-C and hyperuricemia, we reevaluate the relationship between TG/HDL-C and hyperuricemia in participants without metabolic syndrome (N = 12,813). Figure 2b displays that the cumulative incidence of hyperuricemia was significantly elevated with increasing TG/HDL-C quartiles (5.6, 9.4, 15.5, and 24.0%, respectively). Table 3 manifests the OR for hyperuricemia in the highest compared with the lowest quartile of TG/HDL-C was 1.70 (95% CI 1.38–2.10), and each SD increment of TG/HDL-C ratio caused a 18% additional risk for hyperuricemia in people without metabolic syndrome after adjusting for all confounders (Model 4).
Subgroup analyses
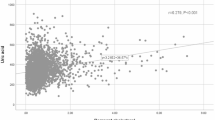
The associations between quartiles of TG/HDL-C and hyperuricemia were further investigated among subgroups. We found that the association differed significantly according to gender (P = 0.001) and BMI categories (P = 0.006) in all participates. However, no heterogeneity was observed with age (P = 0.186), smoking (P = 0.110), drinking (P = 0.747), diabetes (P = 0.701) and hypertension (P = 0.612). The subgroup analyses to assess the relationship between TG/HDL-C quartiles and hyperuricemia according to sex and BMI categories in all subjects were presented in Fig. 3a. After multivariate adjustment (Model 4), a stronger association was observed among women and normal-weight individuals than in men and overweight/obesity subjects.
Subgroup Analyses for TG/HDL-C and incident hyperuricemia in a all subjects (N = 15,198) and b subjects without metabolic syndrome (N = 12,813). *adjusted for sex, age, education status, smoking, drinking, overweight/obesity, diabetes, hypertension, total cholesterol, low-density lipoprotein cholesterol, albumin, alanine aminotransferase, estimated glomerular filtration rate and serum uric acid
Similarly, no heterogeneity was observed with age (P = 0.459), smoking (P = 0.277), drinking (P = 0.444), diabetes (P = 0.805) and hypertension (P = 0.520) in subjects without metabolic syndrome (N = 12,813). After excluded subjects with metabolic syndrome, Fig. 3b depicts that TG/HDL-C ratio is also more strongly associated with incident hyperuricemia in women and in normal-weight individuals.
Discussion
The primary findings supported our hypothesis that people with high TG/HDL-C ratio are at an increased risk of developing hyperuricemia among Chinese adults. After adjusted for all the potential confounding factors, subjects in the highest quartile of TG/HDL-C were nearly 1.8-fold more likely to develop hyperuricemia compared with those in the lowest quartile, and each SD increment of TG/HDL-C ratio caused a 10% additional risk for hyperuricemia. In addition, the association between TG/HDL-C ratio and the risk of hyperuricemia was more pronounced in women and normal-weight subjects. To the best of our knowledge, this is the first population-based cohort study that evaluated whether TG/HDL-C ratio was an independent risk factor of hyperuricemia.
Hyperuricemia has emerged as a major public health concern because of its increasing prevalence and significant impact on various clinical disorders [1,2,3, 7]. In this 4-year follow-up study of 15,198 subjects (43.14 ± 13.13 years, 54.9% men), we observed that 15.6% of Chinese adults developed hyperuricemia. Cao et al. conducted a large prospective cohort study of 58,542 Chinese people (44.0 ± 13.36 years for men and 42.0 ± 12.26 years for women, 59.75% men), the incidence of hyperuricemia was 12.1% with a median of 2.5 years of follow-up. In another prospective cohort study in China, Zhang et al. found that hyperuricemia occurred in 25.9% of participants after 6 years [30]. Strikingly, in the Atherosclerosis Risk in Communities Study of 9451 American who usually consumption of high-fructose corn syrup such as sugar-sweetened soda, 34.8% of them developed hyperuricemia during 6-year follow-up [31]. Since Chinese people have experienced drastic changes in dietary habits with the rapid westernization of lifestyle, the prevalence of hyperuricemia will continue increase in China, leading to serious adverse health outcomes. Thus, exploring of the risk factors that identify those who are prone to develop hyperuricemia is beneficial to early prevention and treatment of the cardiovascular diseases and subsequent gouty arthritis.
The ratio of TG/HDL-C has been recognized as a simple and convenient marker of atherogenic dyslipidemia and insulin resistance [17, 18]. Although the TG/HDL-C ratio has been suggested as a potential tool to identify patients at increased risk of cardiovascular diseases, T2DM, fatty liver and chronic kidney disease [32,33,34,35], limited data were available regarding the association between TG/HDL-C and hyperuricemia. Peng et al. utilized the data of the Third National Health and Nutrition Examination Survey (NHANES III), which demonstrated that TG/HDL-C ratio was significantly associated with increased SUA level [11]. Similarly, in a cross-sectional study of 3518 individuals, Tanya et al. observed that high SUA levels were associated with increased TG/HDL-C ratio even after controlling for traditional cardiovascular disease risk factors and confounders including obesity and metabolic syndrome [12]. Besides, SUA levels were also found to be positively related to TG/HDL-C ratio in children [36]. Nevertheless, it is remains unclear whether TG/HDL-C ratio is a causative risk factor or merely a simple marker of hyperuricemia, because the cross-sectional design limited the interpretation of causality between TG/HDL-C and hyperuricemia. In this cohort study, we found that TG/HDL-C ratio was positively correlated with increased risk of hyperuricemia, which extended previous studies by confirming the causative effect of TG/HDL-C on the development of hyperuricemia. These findings were also confirmed when using a more extensive criterion to identify hyperuricemia [28, 29]. Moreover, it is well established that metabolic syndrome is a major contributor to the development of hyperuricemia [37, 38], which may cause a spurious association between TG/HDL-C and hyperuricemia. In this case, we reevaluated whether elevated TG/HDL-C ratio is still related to the increased risk of hyperuricemia in subjects without metabolic syndrome, and our data showed that the relationship between TG/HDL-C and incident hyperuricemia was still robust regardless of the presence of metabolic syndrome. Furthermore, the association between TG/HDL-C and the risk of hyperuricemia remained significant even after adjusted for multiple confounders included baseline SUA, suggesting the potential of TG/HDL-C ratio to serve as an independently risk indicator of hyperuricemia in clinical practice.
Several potential mechanisms could be proposed to explain TG/HDL-C as a risk factor for the development of hyperuricemia. First, elevated TG level may contribute to the overproduction of uric acid through free fatty acids metabolic pathways. More specifically, hypertriglyceridemia caused more free fatty acid production and utilization, and the synthesis of fatty acids in the liver is associated with the de novo synthesis of purines, thereby accelerating uric acid production [39, 40]. Second, low HDL-C level was independently associated with a decreased eGFR and increased risk of renal impairment, which may result in decreased excretion of uric acid [41,42,43] Third, TG/HDL-C is a surrogate marker of insulin resistance [18], which also involved in the development of hyperuricemia. Insulin resistance is able to enhance renal urate reabsorption via stimulation of the uric acid transporter 1 (URAT1) [44] and/or the Na-dependent anion co-transporter in brush border membranes of the renal proximal tubule [45, 46]. Moreover, insulin resistance could lead to accelerated rate of lipolysis and decreased adipose tissue lipoprotein lipase activity [47], in turn, caused hyperlipemia and the subsequent overproduction of uric acid.
Interestingly, accumulating evidence suggested that hyperuricemia, hyperlipidemia and insulin resistance reflect the common lifestyles and dietary habits such as lack of physical activity, alcohol consumption and high-fructose diet [48, 49]. In addition, some lipid-lowering drugs such as fenofibrate, atorvastatin and simvastatin could play a possible role in decreasing the concentration of SUA via an enhanced urinary excretion of uric acid [50, 51]. Similarly, drug treatments for improving insulin sensitivity were also demonstrated to reduce SUA levels [52, 53]. Hence, appropriate management of high TG/HDL-C levels, through dietary, exercise or pharmacological interventions, may be helpful in preventing progression of hyperuricemia.
We also conducted stratified analyses to explore whether the association between TG/HDL-C and hyperuricemia was affected by several established risk factors. Our study showed significant gender differences in the relation of TG/HDL-C ratio with hyperuricemia risk, and this association was significantly higher in women than in men. Intriguingly, similar pattern has been observed for the association between TG/HDL-C and risk of diabetes, chronic kidney disease and non-alcoholic fatty liver disease [33,34,35]. Although the underlying mechanism of such gender-specific differences remains unknown, one possible explanation might be due to sex hormones. Current literature supported a robust role of estrogen signaling through Estrogen Receptor alpha (ERα) to impact glucose and TG metabolism [19]. Thus, decline in estrogen levels after menopause may lead to dysregulation of lipid metabolism, which put women under greater risk of developing hyperuricemia. In addition, the association between TG/HDL-C levels and the presence of hyperuricemia was more pronounced in normal-weight individuals. It is possible that some additional mechanisms linked overweight/obesity to hyperuricemia may attenuate the association between TG/HDL-C and risk of hyperuricemia. A genome-wide association study found that hyperuricemia and genes mediating uric acid homeostasis are significantly associated with the overweight/obese state [54]. In addition, Bedir et al. proposed that leptin, secreted from adipose tissue, could be a pathogenic factor responsible for hyperuricemia in obese subjects [55]. Thus, it is important to identify women and normal-weight people with high TG/HDL-C levels as high-risk population of hyperuricemia, and further studies are required to validate and explicate these findings in our study.
The main strength of the current study was the retrospective cohort design with a relatively large sample size, which provided sufficient statistical power to reflect the authentic relationship between TG/HDL-C ratio and the risk of hyperuricemia. Nevertheless, several limitations also required consideration. As a retrospective, single-center study, selection bias is inevitable in our study. In fact, there were 62,748 subjects who underwent annual health checkup at our hospital in 2012. In this study we enrolled 19,795 subjects who came to the health management center both in 2012 and in 2016, however, the background demographics were almost same. The demographic data and clinical characteristics of all the subjects in 2012 and this cohort study subjects after using the same exclusion criteria showed no significant differences (Supplemental Table S2). Moreover, our study cannot rule out the possibility that both high TG/HDL and elevated SUA might be the result of the collinearity with other conditions instead of the consequence of a direct interaction, which has a limitation to reveal the causal relationship between TG/HDL-C and hyperuricemia. Furthermore, we did not get the data of insulin sensitivity of participants, because insulin sensitivity test is not a routine item for health examination population. However, a large body of evidence demonstrated that the TG/HDL-C ratio is a good marker of insulin resistance in Chinese people [56, 57]. In addition, some other factors that may influence SUA levels were not collected in our study, such as physical activity, diets rich in purine or fructose, menopausal status, and concomitant medication treatment. Finally, the study population is comprised of only Chinese. Thus, extrapolating the results to other ethnic population should be interpreted cautiously, especially for African descent with “TG paradox” [58]. Further prospective studies with multiethnic and more detailed information collection are needed to assess the value of TG/HDL-C ratio in prevention of hyperuricemia.
Conclusions
The present study indicated that elevated TG/HDL-C ratio increased future risk of hyperuricemia in Chinese population, especially in female and normal-weight individuals. From a clinical and public health perspective, clinicians should pay attention to the risk of hyperuricemia in individuals with high TG/HDL-C ratio and develop proper management to decrease the risk of hyperuricemia by improving TG/HDL-C levels.
References
T. Bardin, P. Richette, Impact of comorbidities on gout and hyperuricaemia: an update on prevalence and treatment options. BMC Med. 15(1), 123 (2017)
A.U.A. Kumar, L.D. Browne, X. Li, F. Adeeb, F. Perez-Ruiz, A.D. Fraser, A.G. Stack, Temporal trends in hyperuricaemia in the Irish health system from 2006-2014: a cohort study. PLoS ONE 13(5), e0198197 (2018)
M. Chen-Xu, C. Yokose, S.K. Rai, M.H. Pillinger, H.K. Choi, Contemporary prevalence of gout and hyperuricemia in the United States and decadal trends: the national health and nutrition examination survey, 2007–2016. Arthritis Rheumatol. 71(6), 991–999 (2019)
R. Liu, C. Han, D. Wu, X. Xia, J. Gu, H. Guan, Z. Shan, W. Teng, Prevalence of hyperuricemia and gout in mainland China from 2000 to 2014: a systematic review and meta-analysis. BioMed. Res. Int. 2015, 762820 (2015)
Z. Miao, C. Li, Y. Chen, S. Zhao, Y. Wang, Z. Wang, X. Chen, F. Xu, F. Wang, R. Sun, J. Hu, W. Song, S. Yan, C.Y. Wang, Dietary and lifestyle changes associated with high prevalence of hyperuricemia and gout in the Shandong coastal cities of Eastern China. J. Rheumatol. 35(9), 1859–1864 (2008)
J.A. Singh, S.G. Reddy, J. Kundukulam, Risk factors for gout and prevention: a systematic review of the literature. Curr. Opin. Rheumatol. 23(2), 192–202 (2011)
H. Wang, H. Zhang, L. Sun, W. Guo, Roles of hyperuricemia in metabolic syndrome and cardiac-kidney-vascular system diseases. Am. J. Transl. Res. 10(9), 2749–2763 (2018)
T. Wang, Y. Bi, M. Xu, Y. Huang, Y. Xu, X. Li, W. Wang, G. Ning, Serum uric acid associates with the incidence of type 2 diabetes in a prospective cohort of middle-aged and elderly Chinese. Endocrine 40(1), 109–116 (2011)
K. Wijarnpreecha, P. Panjawatanan, N. Lekuthai, C. Thongprayoon, W. Cheungpasitporn, P. Ungprasert, Hyperuricaemia and risk of nonalcoholic fatty liver disease: a meta-analysis. Liver Int 37(6), 906–918 (2017)
Y. Xie, P. Xu, K. Liu, S. Lin, M. Wang, T. Tian, C. Dai, Y. Deng, N. Li, Q. Hao, L. Zhou, Z. Dai, Hyperuricemia and gout are associated with cancer incidence and mortality: a meta-analysis based on cohort studies. J. Cell. Physiol. 234(8), 14364–14376 (2019)
T.C. Peng, C.C. Wang, T.W. Kao, J.Y. Chan, Y.H. Yang, Y.W. Chang, W.L. Chen, Relationship between hyperuricemia and lipid profiles in US adults. BioMed. Res. Int. 2015, 127596 (2015)
T. Keenan, M.J. Blaha, K. Nasir, M.G. Silverman, R. Tota-Maharaj, J.A. Carvalho, R.D. Conceicao, R.S. Blumenthal, R.D. Santos, Relation of uric acid to serum levels of high-sensitivity C-reactive protein, triglycerides, and high-density lipoprotein cholesterol and to hepatic steatosis. Am. J. Cardiol. 110(12), 1787–1792 (2012)
M.J. Stelmach, N. Wasilewska, L.I. Wicklund-Liland, A. Wasilewska, Blood lipid profile and BMI-Z-score in adolescents with hyperuricemia. Ir. J. Med. Sci. 184(2), 463–468 (2015)
J. Vekic, Z. Jelic-Ivanovic, V. Spasojevic-Kalimanovska, L. Memon, A. Zeljkovic, N. Bogavac-Stanojevic, S. Spasic, High serum uric acid and low-grade inflammation are associated with smaller LDL and HDL particles. Atherosclerosis 203(1), 236–242 (2009)
G.M. Reaven, The kidney: an unwilling accomplice in syndrome X. Am. J. Kidney Dis. 30(6), 928–931 (1997)
E. Bonora, B. Capaldo, P.C. Perin, S. Del Prato, G. De Mattia, L. Frittitta, S. Frontoni, F. Leonetti, L. Luzi, G. Marchesini, M.A. Marini, A. Natali, G. Paolisso, P.M. Piatti, A. Pujia, A. Solini, R. Vettor, R.C. Bonadonna, Hyperinsulinemia and insulin resistance are independently associated with plasma lipids, uric acid and blood pressure in non-diabetic subjects. The GISIR database. Nutr. Metab. Cardiovasc. Dis. 18(9), 624–631 (2008)
M.Dobiasova, J.Frohlich, The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL). Clin. Biochem. 34(7), 583–588 (2001)
D. Lin, Y. Qi, C. Huang, M. Wu, C. Wang, F. Li, C. Yang, L. Yan, M. Ren, K. Sun, Associations of lipid parameters with insulin resistance and diabetes: a population-based study. Clin. Nutr. 37(4), 1423–1429 (2018)
B.T. Palmisano, L. Zhu, J.M. Stafford, Role of estrogens in the regulation of liver lipid metabolism. Adv. Exp. Med. Biol. 1043, 227–256 (2017)
H. Dai, W. Wang, R. Chen, Z. Chen, Y. Lu, H. Yuan, Lipid accumulation product is a powerful tool to predict non-alcoholic fatty liver disease in Chinese adults. Nutr. Metab. 14, 49 (2017)
H. Dai, W. Wang, X. Tang, R. Chen, Z. Chen, Y. Lu, H. Yuan, Association between homocysteine and non-alcoholic fatty liver disease in Chinese adults: a cross-sectional study. Nutr. J. 15(1), 102 (2016)
Y. Lu, M. Lu, H. Dai, P. Yang, J. Smith-Gagen, R. Miao, H. Zhong, R. Chen, X. Liu, Z. Huang, H. Yuan, Lifestyle and risk of hypertension: follow-up of a young pre-hypertensive cohort. Int. J. Med. Sci. 12(7), 605–612 (2015)
Y.C. Ma, L. Zuo, J.H. Chen, Q. Luo, X.Q. Yu, Y. Li, J.S. Xu, S.M. Huang, L.N. Wang, W. Huang, M. Wang, G.B. Xu, H.Y. Wang, Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J. Am. Soc. Nephrol. 17(10), 2937–2944 (2006)
World Health Orgnization, Physical status: the use and interpretation of ant hropometry. Report of a WHO Expert Committee. World Health Organ. Technical Report Series no. 854, 1–452 (1995)
C. Lenfant, A.V. Chobanian, D.W. Jones, E.J. Roccella, Seventh report of the joint national committee on the prevention, detection, evaluation, and treatment of high blood pressure (JNC 7): resetting the hypertension sails. Hypertension 41(6), 1178–1179 (2003)
P.H. Marathe, H.X. Gao, K.L. Close, American diabetes association standards of medical care in diabetes 2017. J. Diabetes 9(4), 320–324 (2017)
K.G. Alberti, R.H. Eckel, S.M. Grundy, P.Z. Zimmet, J.I. Cleeman, K.A. Donato, J.C. Fruchart, W.P. James, C.M. Loria, S.C. Smith Jr., Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16), 1640–1645 (2009)
T. Bardin, Hyperuricemia starts at 360 micromoles (6 mg/dL). Jt. Bone Spine 82(3), 141–143 (2015)
G. Desideri, G. Castaldo, A. Lombardi, M. Mussap, A. Testa, R. Pontremoli, L. Punzi, C. Borghi, Is it time to revise the normal range of serum uric acid levels? Eur. Rev. Med. Pharm. Sci. 18(9), 1295–1306 (2014)
Y. Zhang, F. Wei, C. Chen, C. Cai, K. Zhang, N. Sun, J. Tian, W. Shi, M. Zhang, Y. Zang, J. Song, Y. He, J. Feng, Q. Zhou, M. Li, P. Bai, S. Feng, W.D. Li, Higher triglyceride level predicts hyperuricemia: a prospective study of 6-year follow-up. J. Clin. Lipidol. 12(1), 185–192 (2018)
A.S. Bomback, V.K. Derebail, D.A. Shoham, C.A. Anderson, L.M. Steffen, W.D. Rosamond, A.V. Kshirsagar, Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int. 77(7), 609–616 (2010)
Q.W. Deng, S. Li, H. Wang, L. Lei, H.Q. Zhang, Z.T. Gu, F.L. Xing, F.L. Yan, The short-term prognostic value of the triglyceride-to-high-density lipoprotein cholesterol ratio in acute ischemic stroke. Aging Dis. 9(3), 498–506 (2018)
Y.L. Wang, W.P. Koh, M. Talaei, J.M. Yuan, A. Pan, Association between the ratio of triglyceride to high-density lipoprotein cholesterol and incident type 2 diabetes in Singapore Chinese men and women. J. Diabetes 9(7), 689–698 (2017)
C.I. Ho, J.Y. Chen, S.Y. Chen, Y.W. Tsai, Y.M. Weng, Y.C. Tsao, W.C. Li, Relationship between TG/HDL-C ratio and metabolic syndrome risk factors with chronic kidney disease in healthy adult population. Clin. Nutr. 34(5), 874–880 (2015)
Y. Fukuda, Y. Hashimoto, M. Hamaguchi, T. Fukuda, N. Nakamura, A. Ohbora, T. Kato, T. Kojima, M. Fukui, Triglycerides to high-density lipoprotein cholesterol ratio is an independent predictor of incident fatty liver: a population-based cohort study. Liver Int. 36(5), 713–720 (2016)
D.Ozalp Kizilay, S. Sen, B. Ersoy, Associations between serum uric acid concentrations and cardiometabolic risk and renal injury in obese and overweight children. J. Clin. Res Pediatr. Endocrinol. 11(3), 262–269 (2019)
K. Chaudhary, K. Malhotra, J. Sowers, A. Aroor, Uric acid - key ingredient in the recipe for cardiorenal metabolic syndrome. Cardiorenal Med. 3(3), 208–220 (2013)
S.P. Juraschek, L.C. Kovell, E.R. Miller, A.C. Gelber, Dose-response association of uncontrolled blood pressure and cardiovascular disease risk factors with hyperuricemia and gout. PLoS ONE 8(2), e56546 (2013)
F. Matsuura, S. Yamashita, T. Nakamura, M. Nishida, S. Nozaki, T. Funahashi, Y. Matsuzawa, Effect of visceral fat accumulation on uric acid metabolism in male obese subjects: visceral fat obesity is linked more closely to overproduction of uric acid than subcutaneous fat obesity. Metabolism 47(8), 929–933 (1998)
T. Balasubramanian, Uric acid or 1-methyl uric acid in the urinary bladder increases serum glucose, insulin, true triglyceride, and total cholesterol levels in Wistar rats. TheScientificWorldJournal 3, 930–936 (2003)
K. Kawachi, H. Kataoka, S. Manabe, T. Mochizuki, K. Nitta, Low HDL cholesterol as a predictor of chronic kidney disease progression: a cross-classification approach and matched cohort analysis. Heart Vessels 34(9), 1440–1455 (2019)
F. Wang, J. Zheng, P. Ye, L. Luo, Y. Bai, R. Xu, L. Sheng, T. Xiao, H. Wu, Association of high-density lipoprotein cholesterol with the estimated glomerular filtration rate in a community-based population. PLoS ONE 8(11), e79738 (2013)
A.F. Wright, I. Rudan, N.D. Hastie, H. Campbell, A ‘complexity’ of urate transporters. Kidney Int. 78(5), 446–452 (2010)
A. Enomoto, H. Kimura, A. Chairoungdua, Y. Shigeta, P. Jutabha, S.H. Cha, M. Hosoyamada, M. Takeda, T. Sekine, T. Igarashi, H. Matsuo, Y. Kikuchi, T. Oda, K. Ichida, T. Hosoya, K. Shimokata, T. Niwa, Y. Kanai, H. Endou, Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature 417(6887), 447–452 (2002)
E. Muscelli, A. Natali, S. Bianchi, R. Bigazzi, A.Q. Galvan, A.M. Sironi, S. Frascerra, D. Ciociaro, E. Ferrannini, Effect of insulin on renal sodium and uric acid handling in essential hypertension. Am. J. Hypertension 9(8), 746–752 (1996)
F. Perez-Ruiz, M.A. Aniel-Quiroga, A.M. Herrero-Beites, S.P. Chinchilla, G.G. Erauskin, T. Merriman, Renal clearance of uric acid is linked to insulin resistance and lower excretion of sodium in gout patients. Rheumatol. Int. 35(9), 1519–1524 (2015)
P. Bjornstad, R.H. Eckel, Pathogenesis of lipid disorders in insulin resistance: a brief review. Curr. Diabetes Rep. 18(12), 127 (2018)
Y. Kim, J. Kang, G.T. Kim, Prevalence of hyperuricemia and its associated factors in the general Korean population: an analysis of a population-based nationally representative sample. Clin. Rheumatol. 37(9), 2529–2538 (2018)
G.E. Thottam, S. Krasnokutsky, M.H. Pillinger, Gout and metabolic syndrome: a tangled web. Curr. Rheumatol. Rep. 19(10), 60 (2017)
G. Derosa, P. Maffioli, Ž. Reiner, L.E. Simental-Mendía, A. Sahebkar, Impact of statin therapy on plasma uric acid concentrations: a systematic review and meta-analysis. Drugs 76(9), 947–956 (2016)
G. Derosa, P. Maffioli, A. Sahebkar, Plasma uric acid concentrations are reduced by fenofibrate: a systematic review and meta-analysis of randomized placebo-controlled trials. Pharmacol. Res. 102, 63–70 (2015)
S. Tsunoda, K. Kamide, J. Minami, Y. Kawano, Decreases in serum uric acid by amelioration of insulin resistance in overweight hypertensive patients: effect of a low-energy diet and an insulin-sensitizing agent. Am. J. Hypertens. 15(8), 697–701 (2002)
D.N. Kiortsis, T.D. Filippatos, M.S. Elisaf, The effects of orlistat on metabolic parameters and other cardiovascular risk factors. Diabetes Metab. 31(1), 15–22 (2005)
A. Kottgen, E. Albrecht, A. Teumer, V. Vitart, J. Krumsiek, C. Hundertmark, G. Pistis, D. Ruggiero, C.M. O’Seaghdha, T. Haller, Q. Yang, T. Tanaka, A.D. Johnson, Z. Kutalik, A.V. Smith, J. Shi et al. Genome-wide association analyses identify 18 new loci associated with serum urate concentrations. Nat. Genet. 45(2), 145–154 (2013)
A. Bedir, M. Topbas, F. Tanyeri, M. Alvur, N. Arik, Leptin might be a regulator of serum uric acid concentrations in humans. Jpn. Heart J. 44(4), 527–536 (2003)
D. Gasevic, J. Frohlich, G.B. Mancini, S.A. Lear, The association between triglyceride to high-density-lipoprotein cholesterol ratio and insulin resistance in a multiethnic primary prevention cohort. Metabolism. 61(4), 583–589 (2012)
T. Du, G. Yuan, M. Zhang, X. Zhou, X. Sun, X. Yu, Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc. Diabetol. 13, 146 (2014)
S.S. Yu, D.C. Castillo, A.B. Courville, A.E. Sumner, The triglyceride paradox in people of African descent. Metab. Syndr. Relat. Disord. 10(2), 77–82 (2012)
Acknowledgements
We gratefully acknowledge all the participants in this study along with the clinical staff of the Third Xiangya Hospital for their assistance in collecting and examining the biochemical samples.
Funding
This study was funded by the National Key Technology Research and Development Program (No. 2016YFC0900802), and the Postgraduate Innovation Project of Central South University (No. 2014zzts089).
Author contributions
All authors were responsible for drafting the manuscript and revising it critically for constructive intellectual content. All authors approved the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consents were obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, XY., Wu, QY., Chen, ZH. et al. Elevated triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio increased risk of hyperuricemia: a 4-year cohort study in China. Endocrine 68, 71–80 (2020). https://doi.org/10.1007/s12020-019-02176-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-02176-5