Abstract
Objective
The use of antithyroid drug (ATD) therapy in patients with Graves’ disease (GD) hyperthyroidism has been increasing, but ATD therapy is associated with a higher relapse rate. We aimed to evaluate clinical factors for predicting relapse of GD after ATD therapy.
Methods
Patients (n = 149) with newly diagnosed GD who achieved remission of hyperthyroidism after ATD therapy (≥6 months) were followed up for >18 months after ATD withdrawal. We evaluated the predictive factors of relapse during a median of 6.9 years of follow-up.
Results
Disease relapse occurred in 52 patients (34.9%). By multivariate analyses, a duration of the minimum maintenance dose therapy (MMDT) of <6 months was a significant factor in disease relapse (hazard ratio [HR], 2.58; 95% confidence interval [CI], 1.47–4.52; p < 0.001), and a T3/free T4 (fT4) ratio > 120 at ATD withdrawal was significantly more frequent in patients with relapse (HR 2.43; 95% CI, 1.36–4.34; p = 0.002). In the prediction-of-relapse model, the likelihood of relapse was greater in the high-risk group, which had a short MMDT duration and a T3/fT4 ratio ≥120 (HR, 5.81; 95% CI, 2.52–13.39; p < 0.001) and the intermediate-risk group, which had a short MMDT duration or a T3/fT4 ratio < 120 (HR, 2.77; 95% CI, 1.26–6.13; p < 0.001), than in the low-risk group, which had a long MMDT duration and a T3/fT4 ratio < 120.
Conclusion
An MMDT longer than 6 months and a high T3/fT4 ratio at ATD withdrawal were independent predictors of relapse in patients who achieved initial remission after ATD for GD. These factors could be used to determine the optimal time to withdraw ATD during the treatment of GD hyperthyroidism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Graves’ disease (GD) is the most common cause of hyperthyroidism [1, 2] and is generally treated with antithyroid drugs (ATDs), radioactive iodine (RAI) ablation, or surgery [3]. The preference for the initial treatment modality of GD hyperthyroidism varies according to geographical region. ATD therapy is preferred in Europe and Asia, while RAI therapy is preferred in the United States of America (USA) [4]. However, the selection of ATDs as the initial treatment modality has been increasing in the USA because it is readily accepted by patients and is the favorable choice in those with thyroid-associated orbitopathy (TAO) [5]. Although RAI easily and effectively results in remission, it may lead to permanent hypothyroidism and other complications, including radiation exposure and deterioration of TAO [4,5,6]. Despite this, RAI has been recommended, as it is the most cost-effective method to control hyperthyroidism, particularly in countries where medical costs are high. However, in countries where medical costs are lower, the differences among treatment modalities are insignificant [7].
The main concern with ATD therapy is the higher risk of relapse [8, 9]. A review of 26 randomized clinical trials involving 3388 GD patients reported that the 1-year relapse rates after ATD therapy were 51 and 54%, in the block-and-replace group and dose-titration group, respectively [10]. A study performed in an iodine-sufficient area, northern Sweden, also reported a long-term remission rate of 56.5% in patients treated with ATDs [8]. Therefore, it is important to elucidate risk factors related to relapse during therapy with ATDs. Efforts to identify risk factors associated with relapse after ATD withdrawal are ongoing. Multiple risk factors for relapse after ATD therapy have been reported, including young age [11, 12], smoking [13,14,15], severe TAO [16] or large goiter [15], high titers of thyrotropin (TSH) receptor antibodies (TRAb) at diagnosis [17,18,19,20] or at the time of ATD withdrawal [17, 19], the total duration of ATD therapy [9], and pregnancy/postpartum [21]. However, the attribution of reported risk factors varies between studies, likely as a result of differences in the ethnic backgrounds of study participants, treatment strategies, or follow-up periods [8, 22].
The use of ATDs has gradually increased worldwide despite the relatively higher incidence of relapse or persistent disease [4]. It would be valuable to determine the optimal strategy by which to discontinue ATDs and the markers that accurately reflect disease activity to determine the most appropriate timing of ATD discontinuation to minimize relapse. We attempted to retrospectively elucidate predictive markers for relapse in patients with Graves’ hyperthyroidism who were treated with ATDs using a dose-titration regimen and achieved remission in our center. A previous study suggested that disappearance of TRAb might not guarantee long-term remission because reemergence of TRAb may occur when the disease recurs in some patients with GD [23]. Therefore, in addition to reported predictive markers, we included the serum T3/free T4 (fT4) ratio at the discontinuation of ATD therapy. A study reported that an increased TSH level was associated with an increased fT3/fT4 ratio [24]. This phenomenon could be explained by increased deiodination of T4 to T3 by TSH. Therefore, we hypothesized that the serum T3/fT4 ratio could reflect the degree of stimulation of the TSH receptor in thyrocytes in vivo and that the T3/fT4 ratio might be a more sensitive marker for activities of stimulating antibodies in vivo than the TRAb titer measured in vitro.
This study assessed the clinical outcomes in GD patients treated with ATDs who had achieved remission and had been followed up for more than 6 years, thereby defining the clinical factors for predicting relapse after remission. Additionally, we aimed to develop an appropriate strategy to reduce the relapse rate after ATD therapy.
Materials and methods
Patients
This historical cohort study screened patients who were newly diagnosed with GD and had been treated at Asan Medical Center, Seoul, Korea, between 2005 and 2012. Patients who achieved remission after ATD therapy for at least 6 months and then had been followed up for more than 18 months after ATD withdrawal were included. A total of 149 patients were eligible for this study. GD was diagnosed based on a high serum fT4 level with a suppressed TSH level, an increased serum TRAb titer, increased uptake on a 99m-technetium (Tc) thyroid scan with or without the presence of TAO, and diffuse goiter [25]. TAO was defined as an inflammatory eye disease associated with autoimmune thyroid disorder [26]. It was classified by disease activity and severity as mild, moderate, or severe [27, 28]. A goiter was categorized according to the World Health Organization goiter classification system (grade 0: no goiter; grade 1: thyroid palpable but not visible; grade 2: thyroid visible with neck in normal position) via physical examination by a physician [29]. This study was approved by the Institutional Review Board of Asan Medical Center, Seoul, Korea.
Treatment and follow-up
ATD therapy was administered using a dose titrating regimen described previously [25]. Most patients were initially treated with methimazole (MMI) (15–30 mg/day) or carbimazole (20–40 mg per day), and some were prescribed with propylthiouracil (PTU) because of minor adverse events. ATD therapy was discontinued based on the following criteria: (1) the levels of TSH, fT4, and TRAb were normalized or (2) a euthyroid state was maintained over 6 months with the minimum maintenance dose of ATDs regardless of the presence of TRAb (MMI = 2.5 mg/day, carbimazole = 5 mg/day, and PTU = 25 mg/day) [25, 30, 31]. Euthyroid state was defined as keeping free T4 and TSH within the normal reference ranges. Serum fT4, total T3, TSH, and TRAb were regularly measured during the follow-up period. These parameters were tested at 3, 9, and 15 months from the time of ATD withdrawal and every 6 months thereafter. RAI therapy was considered when patients failed to achieve euthyroidism despite treatment with ATDs or when serious adverse effects occurred as a result of ATD therapy.
Laboratory measurements
Serum TSH levels were determined using the TSH-CTK-3a radioimmunoassay (RIA; DiaSorin SpA, Saluggia, Italy) with a functional sensitivity of 0.07 mIU/L, as described previously [32]. Serum fT4 levels were measured using the fT4 RIA (Immunotech, Prague, Czech Republic), and serum total T3 levels were measured by RIA using T3-CTK (DiaSorin SpA). The reference ranges of TSH, fT4, and total T3 were 0.4–4.5 mIU/L, 0.80–1.90 ng/dL, and 151–277 ng/dL, respectively. TRAb was measured using a competitive thyrotropin-binding inhibitory immunoglobulin (TBII) assay by the B·R·A·H·M·S TRAK human RIA (B·R·A·H·M·S GmbH, Hennigsdorf/Berlin, Germany) according to the manufacturer’s instructions [33]. TBII titers ≥1.5 IU/L were considered positive with an analytical sensitivity of 0.3 IU/L and a functional assay sensitivity of 1.0 ± 0.2 IU/L.
Definitions of clinical outcomes
Remission was defined as euthyroid status with normal TSH, fT4, and total T3 maintained for more than 1 year after ATD withdrawal. Relapse was defined as low TSH with or without increased fT4 during follow-up after remission. Upon identifying relapse, a second course of ATD therapy or RAI therapy was considered.
Statistical analyses
R® version 3.0 and the R libraries “survival,” “Hmisc,” “Cairo,” “prodliman,” and “pROC” were used to analyze data (R Foundation for Statistical Computing, www.R-project.org). Continuous variables were described as means with standard deviations or medians with interquartile ranges (IQRs) and were analyzed using the Student’s t test. Categorical variables were examined by the chi-square test and presented as frequencies with percentages. We performed receiver operating characteristic curve analysis and determined the ability of optimal cutoff values for the T3/fT4 ratio at diagnosis and ATD withdrawal, and the duration of minimum maintenance dose therapy (MMDT), to predict relapse. A Cox proportional hazard model was used to identify predictive variables, including age, sex, goiter size, the presence of TAO, thyroid function test at diagnosis and ATD withdrawal, 99m-Tc scan uptake at diagnosis, duration of ATD therapy, and serum TBII titer. Relapse-free survival (RFS) curves were calculated using the Kaplan–Meier method and compared using the log-rank test. A Cox proportional hazard model was applied to evaluate risk factors for relapse of GD, which were presented as hazard ratios (HRs), 95% confidence intervals (CIs), and p values. The multivariate analysis included age, sex, goiter size, the presence of TAO, thyroid function test and TBII at diagnosis and ATD withdrawal, 99m-Tc scan uptake at diagnosis, and treatment duration of any ATDs. All p-values were two-sided with values < 0.05 considered statistically significant.
Results
Baseline characteristics of patients and clinical course
The baseline characteristics of 149 patients with GD are presented in Table 1. The mean age was 45.17 ± 12.11 years, and 28.9% were males. Eight-one patients (54.4%) had a goiter, and 11 (7.4%) showed clinically evident TAO. Fifty-four patients (36.3%) were treated with MMI, and 89 (59.7%) were treated with carbimazole. The median level of TSH at diagnosis was 0.04 mIU/L (IQR 0.04–0.07 mIU/L), and the median fT4 level was 3.15 ng/dL (2.60–3.80 ng/dL). The initial titer of serum TBII was 10.65 IU/L (5.60–18.65 IU/L).
The median follow-up duration was 6.9 years (IQR 4.91–9.19 years). The median duration of ATD therapy to remission was 22.03 months (IQR 15.31–41.12 months), and the median duration of MMDT among total ATD therapy was 6.72 months (Table 1). The median titer of TBII at ATD withdrawal was 1.10 IU/L (0.61–1.80 IU/L), and the median T3/fT4 ratio was 116.2 (104.4–130.3). When patients had been followed up for a median of 3.92 years (IQR 2.79–6.14 years) after ATD withdrawal, 52 out of 149 patients (34.9%) experienced relapse. The median duration from ATD withdrawal to relapse was 32.56 months (IQR 17.71–48.98 months). Six (11.5%) of 52 relapsed patients underwent RAI therapy, and 1 patient (1.9%) was treated with total thyroidectomy. The remaining patients underwent a second course of ATD therapy after relapse.
Clinical characteristics related to the relapse of Graves’ disease
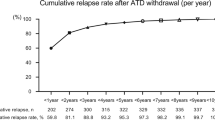
After withdrawal of the initial ATD, 52 (34.9%) of 149 patients experienced relapse. We compared the clinical features of patients in the remission group (n = 97) with those of patients who had relapsed (n = 52) to identify the clinical features associated with relapse of hyperthyroidism. In univariate analysis, a short duration of MMDT ( <6 months) was significantly associated with relapse (HR, 3.33; 95% CI, 1.54–7.20; p < 0.001; Table 2), and this association remained significant in multivariate analysis (HR, 2.58; 95% CI, 1.47–4.52; p < 0.001; Table 2). When we compared RFS according to the duration of MMDT, patients with a shorter duration of MMDT showed significantly shorter RFS (p < 0.001; Fig. 1a). A high total T3/fT4 ratio ( ≥120) at ATD withdrawal was associated with relapse (HR, 2.29; 95% CI, 1.31–3.97; p = 0.003; Table 2), and it was independently associated with relapse in multivariate analysis (HR, 2.43; 95% CI, 1.36–4.34; p = 0.002; Table 2). Patients who had a high T3/fT4 ratio at ATD withdrawal demonstrated significantly shorter RFS (p = 0.006, Fig. 1b). There were no significant associations between GD relapse and age, sex, the presence of TAO, the degree of goiter, 99m-Tc uptake on thyroid scans, total ATD therapy duration, initial thyroid function test, or titer of TBII at ATD withdrawal.
Comparison of relapse-free survival (RFS) in patients with GD who underwent antithyroid drug (ATD) treatment and achieved initial remission after ATD withdrawal. a The RFS curves according to the duration of minimum maintenance dose therapy. b The RFS curves according to the T3/freeT4 ratio at ATD withdrawal
Prediction of relapse by risk stratification
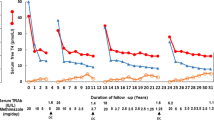
In multivariate analysis with a Cox proportional hazard model, the duration of MMDT (<6 months) and the T3/fT4 ratio at ATD withdrawal were significantly correlated with relapse of GD (Table 2). The duration of MMDT and the T3/fT4 ratio at ATD withdrawal were combined to stratify the patients into four groups as follows: low-risk group, longer duration of MMDT (≥6 months) and low T3/fT4 ratio < 120; intermediate-risk group 1, longer duration of MMDT (≥6 months) and high T3/fT4 ratio ≥ 120; intermediate-risk group 2, shorter duration of MMDT (<6 months) and low T3/fT4 ratio < 120; and high-risk group, shorter duration of MMDT (<6 months) and high T3/fT4 ratio ≥ 120. The likelihood of relapse was greater in the high-risk group (HR, 5.81; CI, 2.52–13.40; p < 0.001), intermediate group 1 (HR, 2.46; CI, 1.02–5.94; p = 0.04), and intermediate group 2 (HR, 3.19; CI, 1.32–7.70; p = 0.01) than in the low-risk group (Table 3). There was a significant difference in RFS between the four groups (p < 0.001; Fig. 2a); however, only a modest difference was observed between intermediate groups 1 and 2 (HR, 2.46; CI, 1.02–5.94; p = 0.04 and HR, 3.19; CI, 1.32–7.70; p = 0.01, respectively). We considered it reasonable to reclassify patients into three groups according to the numbers of the two risk factors. Consequently, among the three groups, the intermediate-risk (HR, 2.77; CI, 1.26–6.13; p < 0.001) and high-risk (HR, 5.81; CI, 2.52–13.40; p < 0.001) groups showed a significantly higher risk of relapse than the low-risk group (Table 3). There was also a significant difference in RFS between the three groups (p < 0.001; Fig. 2b).
Comparison of the RFS curves between the risk-stratified groups according to the duration of minimum maintenance dose therapy (MMDT) and the T3/free T4 (fT4) ratio. a Four-group stratification: Low risk, patients with an MMDT duration of ≥6 months and a T3/fT4 ratio <120; Intermediate-risk 1, patients with an MMDT duration of ≥6 months and a T3/fT4 ratio ≥120; Intermediate-risk 2, patients with an MMDT duration of <6 months and a T3/fT4 ratio <120; High risk, patients with an MMDT duration of < 6 months and a T3/fT4 ratio ≥120. b Three-group stratification: Low risk, patients with an MMDT duration of ≥ 6 months and a T3/fT4 ratio <120; Intermediate risk, patients with an MMDT duration of ≥6 months and aT3/fT4 ratio <120 or vice versa; High risk, patients with an MMDT duration of <6 months and a T3/fT4 ratio ≥120
Eight of 51 patients (15.7%) in the low-risk group relapsed. Only three of them had positive TBII titers at the time of ATD withdrawal and the remaining five patients relapsed despite negative TBII titers at withdrawal. In high-risk group, 18 patients (64.3%) relapsed with GD. Eleven of these patients had positive TBII titers at the time of ATD withdrawal, but seven patients relapsed despite negative TBII titers at withdrawal.
Discussion
This study evaluated the clinical outcomes of 149 GD patients who achieved remission after treatment with ATDs during a median of 6 years follow-up. About 35% of patients experienced GD relapse after ATD withdrawal. We demonstrated that a prolonged MMDT (≥6 months) was associated with a lower relapse rate after ATD therapy. Furthermore, we found that the T3/fT4 ratio at ATD withdrawal was significantly lower in patients without relapse, which suggested that a higher T3/fT4 ratio at the time of ATD withdrawal might be indicative of active GD. Our findings suggested that the T3/fT4 ratio at ATD discontinuation was a more sensitive marker for the activity of stimulating antibodies than the TRAb titer. Our risk stratification using these two risk factors may be useful when physicians are making a decision regarding ATD withdrawal to minimize the recurrence of GD.
The selection of first-line treatment for GD remains controversial. The recent American Thyroid Association (ATA) guidelines recommend that physicians select treatment options among ATD therapy, RAI ablation, and surgery, taking into account availability and cost [1]. Several studies suggested that ATD therapy might be useful for the treatment of hyperthyroidism [9, 34]. Recently, the effectiveness of ATDs was proven by favorable clinical outcomes in relapsed patients during a second course of ATD therapy [22]. However, 50% of reported relapses occurred within 1 year of ATD withdrawal, and more than 90% of relapses occurred within 4 years [8, 22]. Higher relapse rates were reported for ATD therapy compared with RAI ablation; therefore, it is valuable to predict and make efforts to decrease the relapse rate in patients treated with ATDs [5]. Based on previous data, multiple risk factors for relapse have been suggested, including young age, male sex, large goiter, TAO, and TBII titer at diagnosis and ATD withdrawal; however, we were unable to find a significant association between several clinical factors and relapse in this study.
In general, the optimal duration of ATD therapy is reported to be between 12 and 18 months [1, 10]. However, the total duration of ATD was not a significant factor predicting relapse of GD in our study. Only longer duration (≥6 months) of MMDT showed a marked association with a lower relapse rate. This finding is in agreement with that of a previous Japanese study involving 107 GD patients [31]. Another study where the minimum dose of ATD (methimazole 2.5–7.5 mg) was maintained over 5 years showed that long-term maintenance of the minimum dose of ATDs was more effective than RAI therapy [5]. Based on these results, prolonged maintenance of the minimum dose of ATDs in patients with normal thyroid function may be associated with low activity of GD [31]. In addition, Laurberg et al. hypothesized that remission of GD during ATD therapy may be linked to the recovery of immunologic regulation with restoration of the euthyroid state [35]. Therefore, extended maintenance of the minimum dose of ATDs could be helpful to achieve remission by prolonging a euthyroid state.
The issue as to when to withdraw ATD therapy remains unresolved. The ATA guidelines recommend that TRAb be measured prior to ATD withdrawal and that ATD should only be discontinued after confirmation of normal levels of TRAb [1]. GD is an autoimmune disorder in which TRAb stimulates the thyroid gland and causes hyperthyroidism [1, 25]. The titers of TRAb at diagnosis or ATD withdrawal are known to be indicative of disease activity in GD [12, 19]. However, the role of TRAb levels as a predictor of clinical outcomes of ATD therapy has been controversial. TRAb values in some patients who experienced recurrence of hyperthyroidism after ATD withdrawal remained high. This was supported by a study in mice that found that excessive autoantibody stimulation decreases the sensitivity of the thyroid gland to TRAb by downregulating TSH receptors [36]. This might be caused by a change in thyroid gland responsiveness to TRAb as a result of the progression of cell-mediated autoimmune destruction during the natural course of GD [19]. Another possible explanation is that the nature of the antibody is changed after long-term ATD therapy. Although these TRAbs were measurable, they are functionally different and not associated with clinical or biochemical hyperthyroidism [37]. On the contrary, some patients who relapsed with GD did not show TBII positivity. One explanation is that the sensitivity of second-generation TBII assays is still too low to identify minute amounts of antibodies. The second explanation is that the production of TRAb is still confined to the thyroid gland and adjacent lymph nodes without spill-over of antibodies into the circulation and, therefore, TRAbs are unmeasurable in serum [38]. Hence, TBII has limited value to predict GD relapse by seroconversion of TRAbs at the time of ATD discontinuation.
In the euthyroid state, around 80% of circulating T3 originates from peripheral deiodination from T4, but only 20% of circulating T3 is secreted by the thyroid gland [39]. Whereas, in the pathological state, a relatively higher fraction of T3 is secreted by the thyroid gland [40]. The mechanisms for this was proposed to be the higher T3 content in thyroglobulin [41], or the enhanced deiodination of T4 to T3 by iodothyronine deiodinase in the hyperactive thyroid gland [42]. In previous studies, the T3/T4 ratio at diagnosis was suggested to be a useful marker in the diagnosis of GD differentiating destructive thyrotoxicosis [43] and the ratio throughout treatment periods was significantly associated with clinical outcomes in GD [44]. In our study, the T3/fT4 ratio was a sensitive marker for the determination of disease activity, and a lower T3/fT4 ratio at ATD withdrawal was independently associated with a lower relapse rate after ATD therapy. This suggests that a low T3/fT4 ratio at the time of ATD withdrawal reflects lower disease activity of GD, leading to higher remission rates. Further studies are needed to determine the mechanism responsible; however, the TBII titer during the course of ATD therapy was not correlated with the clinical outcome in this study. The exclusion of patients with severe GD who did not achieve remission following ATD therapy from this study could be a cause of this discrepancy. Patients with a high titer of TBII might be treated by RAI or surgery. Therefore, our findings apply to specific clinical settings after the achievement of remission with ATD for Graves’ hyperthyroidism.
This study has some limitations as a result of its retrospective design and consequent dependence on medical records. First, the evaluation of variables such as goiter and TAO may be somewhat subjective as their description depends on the examining physician’s experience and background. The evaluation of goiter size by ultrasound or grading of TAO by validated scoring systems would provide more objective information. Second, the reproductive history during the follow-up period after ATD discontinuation was not available and the effect of pregnancy and postpartum on relapse could therefore not be evaluated. Third, we were unable to apply the fT3/fT4 ratio because our center measured only total T3 when evaluating thyroid function. Fourth, there might be selection bias because we included patients who maintained a euthyroid state for more than one year after ATD discontinuation to define risk factors for relapsing disease rather than persistent disease. Our study was therefore not representative of the whole spectrum of GD patients who were treated with ATDs.
This study was conducted in Korea which is a representative of an iodine-sufficient area. Previously, several studies suggested that increasing dietary iodine adversely influenced the effectiveness of ATDs [45, 46]. Although we did not evaluate the iodine intake of this study cohort, according to other recent reports, excessive iodine intake did not have an effect on the clinical outcomes of GD hyperthyroidism in an iodine-replete area [47, 48]. Therefore, the effect of excessive iodine intake on clinical outcomes in this study cohort would be negligible.
This study found that prolonged MMDT with ATDs for more than 6 months was associated with a lower rate of GD relapse. Moreover, the T3/fT4 ratio at ATD withdrawal was an independent predictor of GD relapse. On the basis of these results, it would be advisable for physicians to prolong the minimum dose of ATD and to confirm that the T3/fT4 ratio is low before ATD withdrawal to reduce the risk of relapse in GD patients who achieved initial remission after ATD therapy for hyperthyroidism.
References
D.S. Ross, H.B. Burch, D.S. Cooper, M.C. Greenlee, P. Laurberg, A.L. Maia, S.A. Rivkees, M. Samuels, J.A. Sosa, M.N. Stan, 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 26(10), 1343–1421 (2016)
J.P. Brito, S. Schilz, N. Singh Ospina, R. Rodriguez-Gutierrez, S. Maraka, L.R. Sangaralingham, V.M. Montori, Antithyroid drugs—the most common treatment for Graves’ disease in the United States: a nationwide population-based study. Thyroid 26(8), 1144–1145 (2016)
E. Mohlin, H.F. Nyström, M. Eliasson, Long-term prognosis after medical treatment of Graves’ disease in a northern Swedish population 2000-2010. Eur. J. Endocrinol. 170, 419–427 (2013)
H.B. Burch, K.D. Burman, D.S. Cooper, A 2011 survey of clinical practice patterns in the management of Graves’ disease. J. Clin. Endocrinol. Metab. 97(12), 4549–4558 (2012)
D. Villagelin, J.H. Romaldini, R.B. Santos, A.B. Milkos, L.S. Ward, Outcomes in relapsed Graves’ disease patients following radioiodine or prolonged low dose of methimazole treatment. Thyroid 25(12), 1282–1290 (2015)
K.H. Yi, J.H. Moon, I.-J. Kim, H.-S. Bom, J. Lee, W.Y. Chung, J.H. Chung, Y.K. Shong, The diagnosis and management of hyperthyroidism consensus-report of the Korean Thyroid Association. J. Korean Thyroid Assoc. 6(1), 1–11 (2013)
S. Yamashita, N. Amino, Y.K. Shong. The American Thyroid Association and American Association of Clinical Endocrinologists hyperthyroidism and other causes of thyrotoxicosis guidelines: viewpoints from Japan and Korea. (Mary Ann Liebert, Inc, 140 Huguenot Street, 3rd Floor New Rochelle, NY 10801 USA), 2011)
E. Mohlin, H. Filipsson Nystrom, M. Eliasson, Long-term prognosis after medical treatment of Graves’ disease in a northern Swedish population 2000-2010. Eur. J. Endocrinol. 170(3), 419–427 (2014). https://doi.org/10.1530/eje-13-0811
F. Azizi, L. Ataie, M. Hedayati, Y. Mehrabi, F. Sheikholeslami, Effect of long-term continuous methimazole treatment of hyperthyroidism: comparison with radioiodine. Eur. J. Endocrinol. 152(5), 695–701 (2005)
P. Abraham, A. Avenell, S. McGeoch, L.F. Clark, J.S. Bevan, Antithyroid drug regimen for treating Graves’ hyperthyroidism. Cochrane Database Syst. Rev. CD003420 (2010)
A. Allahabadia, J. Daykin, R.L. Holder, M.C. Sheppard, S.C. Gough, J.A. Franklyn, Age and gender predict the outcome of treatment for Graves’ hyperthyroidism. The. J. Clin. Endocrinol. Metab. 85(3), 1038–1042 (2000)
P. Vitti, T. Rago, L. Chiovato, S. Pallini, F. Santini, E. Fiore, R. Rocchi, E. Martino, A. Pinchera, Clinical features of patients with Graves’ disease undergoing remission after antithyroid drug treatment. Thyroid 7(3), 369–375 (1997)
T. Chowdhury, P. Dyer, Clinical, biochemical and immunological characteristics of relapsers and non‐relapsers of thyrotoxicosis treated with anti‐thyroid drugs. J. Intern. Med. 244(4), 293–297 (1998)
D. Glinoer, P. De Nayer, M. Bex, Effects of l-thyroxine administration, TSH-receptor antibodies and smoking on the risk of recurrence in Graves’ hyperthyroidism treated with antithyroid drugs: a double-blind prospective randomized study. Eur. J. Endocrinol. 144(5), 475–483 (2001)
B. Nedrebo, P.I. Holm, S. Uhlving, J. Sorheim, S. Skeie, G.E. Eide, E.S. Husebye, E.A. Lien, S. Aanderud, Predictors of outcome and comparison of different drug regimens for the prevention of relapse in patients with Graves’ disease. Eur. J. Endocrinol. 147(5), 583–589 (2002)
A.K. Eckstein, H. Lax, C. Lösch, D. Glowacka, M. Plicht, K. Mann, J. Esser, N.G. Morgenthaler, Patients with severe Graves’ ophthalmopathy have a higher risk of relapsing hyperthyroidism and are unlikely to remain in remission. Clin. Endocrinol. 67(4), 607–612 (2007)
C. Cappelli, E. Gandossi, M. Castellano, C. Pizzocaro, B. Agosti, A. Delbarba, I. Pirola, E. De Martino, E.A. Rosei, Prognostic value of thyrotropin receptor antibodies (TRAb) in Graves’ disease: a 120 months prospective study. Endocr. J. 54(5), 713–720 (2007)
P. Laurberg, G. Wallin, L. Tallstedt, M. Abraham-Nordling, G. Lundell, O. Tørring, TSH-receptor autoimmunity in Graves’ disease after therapy with anti-thyroid drugs, surgery, or radioiodine: a 5-year prospective randomized study. Eur. J. Endocrinol. 158(1), 69–75 (2008)
C. Carella, G. Mazziotti, F. Sorvillo, M. Piscopo, M. Cioffi, P. Pilla, R. Nersita, S. Iorio, G. Amato, L. Braverman, Serum thyrotropin receptor antibodies concentrations in patients with Graves’ disease before, at the end of methimazole treatment, and after drug withdrawal: evidence that the activity of thyrotropin receptor antibody and/or thyroid response modify during the observation period. Thyroid 16(3), 295–302 (2006)
H.S. Choi, W.S. Yoo, Free thyroxine, anti-thyroid stimulating hormone receptor antibody titers, and absence of goiter were associated with responsiveness to methimazole in patients with new onset Graves’ disease. Endocrinol. Metab. 32(2), 281–287 (2017)
M. Rotondi, C. Cappelli, B. Pirali, I. Pirola, F. Magri, R. Fonte, M. Castellano, E.A. Rosei, L. Chiovato, The effect of pregnancy on subsequent relapse from Graves’ disease after a successful course of antithyroid drug therapy. J. Clin. Endocrinol. Metab. 93(10), 3985–3988 (2008). https://doi.org/10.1210/jc.2008-0966
Y.A. Kim, S.W. Cho, H.S. Choi, S. Moon, J.H. Moon, K.W. Kim, D.J. Park, K.H. Yi, Y.J. Park, B.Y. Cho, The second antithyroid drug treatment is effective in relapsed Graves’ disease patients: a median 11-year follow-up study. Thyroid 27(4), 491–496 (2017)
U. Feldt-Rasmussen, H. Schleusener, P. Carayon, Meta-analysis evaluation of the impact of thyrotropin receptor antibodies on long term remission after medical therapy of Graves’ disease. J. Clin. Endocrinol. Metab. 78(1), 98–102 (1994)
D. Strich, G. Karavani, S. Edri, D. Gillis, TSH enhancement of FT4 to FT3 conversion is age dependent. Eur. J. Endocrinol. 175, 49–54 (2016). EJE-16-0007
H. Kwon, W.G. Kim, E.K. Jang, M. Kim, S. Park, M.J. Jeon, T.Y. Kim, J.-S. Ryu, Y.K. Shong, W.B. Kim, Usefulness of measuring thyroid stimulating antibody at the time of antithyroid drug withdrawal for predicting relapse of Graves disease. Endocrinol. Metab. 31(2), 300–310 (2016)
E. Peterson, P. De, R. Nuttall, BMI, diet and female reproductive factors as risks for thyroid cancer: a systematic review. PLoS ONE 7(1), e29177 (2012). https://doi.org/10.1371/journal.pone.0029177
M.P. Mourits, M.F. Prummel, W.M. Wiersinga, L. Koornneef, Clinical activity score as a guide in the management of patients with Graves’ ophthalmopathy. Clin. Endocrinol. 47(1), 9–14 (1997)
L. Bartalena, L. Baldeschi, A.J. Dickinson, A. Eckstein, P. Kendall-Taylor, C. Marcocci, M.P. Mourits, P. Perros, K. Boboridis, A. Boschi, Consensus statement of the European group on Graves’ orbitopathy (EUGOGO) on management of Graves’ orbitopathy. Thyroid 18(3), 333–346 (2008)
World Health Organization, Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers (Geneva: World Health Organization, 2007).
S.M. ChoBY, L. YiKH, M.H. KohCS, Evaluationofserum basalthyrotropinlevelsand thyrotopinreceptorantibodyactivitiesasprognostic markers for discontinuation of antithyroid drug treatmentinpatientswithGraves’ disease. Clin. Endocrinol. 36, 585–590 (1992)
T. Konishi, Y. Okamoto, M. Ueda, Y. Fukuda, I. Harusato, Y. Tsukamoto, N. Hamada, Drug discontinuation after treatment with minimum maintenance dose of an antithyroid drug in Graves’ disease: a retrospective study on effects of treatment duration with minimum maintenance dose on lasting remission. Endocr. J. 58(2), 95–100 (2011)
M.J. Jeon, W.G. Kim, E.K. Jang, Y.M. Choi, Y.-M. Lee, T.-Y. Sung, J.H. Yoon, K.-W. Chung, S.J. Hong, J.H. Baek, Thyroglobulin level in fine-needle aspirates for preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma: two different cutoff values according to serum thyroglobulin level. Thyroid 25(4), 410–416 (2015)
W.B. Kim, Clinical applications of thyrotropin binding inhibitor immunoglobulin (TBII) assays. J. Korean Endocr. Soc. 23(3), 174–178 (2008)
R.V. García-Mayor, C. Paramo, R.L. Cano, L.P. Mendez, J. Galofre, A. Andrade, Antithyroid drug and Graves’ hyperthyroidism. Significance of treatment duration and TRAb determination on lasting remission. J. Endocrinol. Investig. 15(11), 815–820 (1992)
P. Laurberg, Remission of Graves’ disease during anti-thyroid drug therapy. Time to reconsider the mechanism? Eur. J. Endocrinol. 155(6), 783–786 (2006)
T. Ando, R. Latif, T.F. Davies, Concentration-dependent regulation of thyrotropin receptor function by thyroid-stimulating antibody. J. Clin. Investig. 113(11), 1589–1595 (2004)
S. Costagliola, N.G. Morgenthaler, R. Hoermann, K. Badenhoop, J. Struck, D. Freitag, S. Poertl, W. Weglöhner, Jr.M. Hollidt, B: Quadbeck, Second generation assay for thyrotropin receptor antibodies has superior diagnostic sensitivity for Graves’ disease. J. Clin. Endocrinol. Metab. 84(1), 90–997 (1999)
X.G. Vos, N. Smit, E. Endert, J.G. Tijssen, W.M. Wiersinga, Frequency and characteristics of TBII-seronegative patients in a population with untreated Graves’ hyperthyroidism: a prospective study. Clin. Endocrinol. 69(2), 311–317 (2008). https://doi.org/10.1111/j.1365-2265.2008.03192.x
A.C. Bianco, D. Salvatore, B. Gereben, M.J. Berry, P.R. Larsen, Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr. Rev. 23(1), 38–89 (2002)
P. Laurberg, Mechanisms governing the relative proportions of thyroxine and 3, 5, 3′-triiodothyronine in thyroid secretion. Metabolism 33(4), 379–392 (1984)
P. Laurberg, Thyroxine and 3, 5, 3′-triiodothyronine content of thyroglobulin in thyroid needle aspirates in hyperthyroidism and hypothyroidism. J. Clin. Endocrinol. Metab. 64(5), 969–974 (1987).
P. Laurberg, H. Vestergaard, S. Nielsen, S.E. Christensen, T. Seefeldt, K. Helleberg, K.M. Pedersen, Sources of circulating 3, 5, 3′-triiodothyronine in hyperthyroidism estimated after blocking of type 1 and type 2 iodothyronine deiodinases. J. Clin. Endocrinol. Metab. 92(6), 2149–2156 (2007)
A. Carlé, N. Knudsen, I.B. Pedersen, H. Perrild, L. Ovesen, L.B. Rasmussen, P. Laurberg, Determinants of serum T4 and T3 at the time of diagnosis in nosological types of thyrotoxicosis: a population-based study. Eur. J. Endocrinol. 169(5), 537–545 (2013)
J. Takamatsu, K. Kuma, T. Mozai, Serum triiodothyronine to thyroxine ratio: a newly recognized predictor of the outcome of hyperthyroidism due to Graves’ disease. J. Clin. Endocrinol. Metab. 62(5), 980–983 (1986).
B.L. Solomon, J.E. Evaul, K.D. Burman, L. Wartofsky, Remission rates with antithyroid drug therapy: continuing influence of iodine intake?. Ann. Intern. Med. 107(4), 510–512 (1987).
F. Azizi, Environmental iodine intake affects the response to methimazole in patients with diffuse toxic goiter. J. Clin. Endocrinol. Metab. 61(2), 374–377 (1985).
S.M. Park, Y.Y. Cho, J.Y. Joung, S.Y. Sohn, S.W. Kim, J.H. Chung, Excessive iodine intake does not increase the recurrence rate of Graves’ disease after withdrawal of the antithyroid drug in an iodine-replete area. Eur. thyroid J. 4(1), 36–42 (2015)
T. Hiraiwa, M. Ito, A. Imagawa, J. Takamatsu, K. Kuma, A. Miyauchi, T. Hanafusa, Restriction of dietary Iodine does not ameliorate the early effect of anti-thyroid drug therapy for Graves’ disease in an area of excessive iodine intake. J. Endocrinol. Investig. 29(4), 380–384 (2006)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of Asan Medical Center, Seoul, Korea, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, S., Song, E., Oh, HS. et al. When should antithyroid drug therapy to reduce the relapse rate of hyperthyroidism in Graves’ disease be discontinued?. Endocrine 65, 348–356 (2019). https://doi.org/10.1007/s12020-019-01987-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01987-w