Abstract
Introduction
Pasireotide, a multi-somatostatin receptor (SSTR)-ligand with high affinity for SSTR5 was recently approved for acromegaly treatment.
Patients and methods
A retrospective multicenter study investigating the efficacy and safety of long-acting (LAR) pasireotide treatment in 35 patients (20 males) with active acromegaly (28 macroadenomas).
Results
Mean baseline insulin-like growth factor-1 (IGF-1) at diagnosis was 3.1 ± 1.3 × ULN. All but five patients have undergone pituitary surgery and six received sellar radiotherapy. All remained with active acromegaly despite first-generation somatostatin analogue (SSA) treatment. Immediately before pasireotide-LAR initiation, eighteen patients were under SSA monotherapy and one with pegvisomant. The remaining patients received combination therapy with SSA and pegvisomant, n = 9 (two received cabergoline also); SSA and cabergoline, n = 4; pegvisomant and cabergoline, n = 1. Two were untreated. Mean IGF-1 was 1.76 ± 0.9 ULN before pasireotide. Pasireotide-LAR starting dose was 40 mg/4 weeks in most patients. IGF-1 normalized in 19 patients, IGF-1 between 1-1.2 × ULN was reached in five, and in additional two patients IGF-1 was significantly suppressed. No effect was seen in nine patients. Pasireotide dose was reduced by 20 mg in six patients with excellent response, with preserved IGF-1 control in five. Severe headaches in six patients disappeared or improved with pasireotide. Side effects consisted of symptomatic cholelithiasis in one patient and deterioration of glucose control in 22 patients, requiring initiation or intensification of antidiabetic treatment in seventeen. One patient developed diabetic ketoacidosis.
Conclusions
In the real-life scenario ~54% of patients with acromegaly resistant to first-generation SSA, may normalize IGF-1 with pasireotide; however, 63% experienced glucose control deterioration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acromegaly is a rare condition caused by elevated circulating growth hormone (GH) and insulin-like growth factor-1 (IGF-1) levels. The disease is secondary to GH over-secretion from a pituitary adenoma in almost all cases [1]. Uncontrolled acromegaly is associated with high morbidity and mortality rates [2]. However, treatment mediated normalization of GH and IGF-1 levels may restore mortality rates of patients with acromegaly to those of the healthy population [2]. Transsphenoidal surgery by an experienced neurosurgeon is recommended as first-line therapy in most cases [3], but up to 50% of operated patients will experience persistent or recurrent disease, requiring medical treatment to achieve hormonal remission [4].
Long-acting somatostatin analogues (SSAs) are considered first-line medical treatment following unsuccessful surgery, or when surgery is not suitable [3]. Somatostatin analogues have been shown to normalize GH and IGF-1 in approximately 50% of patients, in addition to tumor volume reduction, with consequent improvement of cardiovascular and metabolic comorbidities [5]. However, half of the patients fail to achieve biochemical control with the first-generation SSAs, octreotide, or lanreotide [6], with high affinity for SSTR2. The GH-receptor antagonist, pegvisomant, may be given to patients who remain uncontrolled with SSA, as monotherapy or in combination with SSA. Pegvisomant given as daily injection normalized IGF-1 levels in 63% of patients treated in a real-life scenario [7]. Consistent with its mechanism of action, pegvisomant does not control tumor volume and GH secretion.
Pasireotide, a second-generation somatostatin receptor ligand, has higher affinity for SSTR5 than SSTR2, and moderate binding to SSTR1, and SSTR3 [8]. In two large, randomized, controlled phase III studies (RCT), long-acting pasireotide (LAR) was superior to long-acting octreotide and lanreotide in providing hormonal control in both medically naïve [9] and SSA resistant acromegaly patients [10]. Pasireotide was approved by the FDA and EMA in 2014 for the treatment of patients with active acromegaly.
We present herein results of a retrospective multicenter study that investigated the efficacy and safety of pasireotide-LAR treatment given in a clinical setting to patients resistant to SSA.
Subjects and methods
Patients and study design
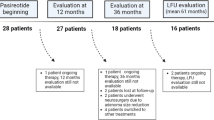
Patients with acromegaly treated with at least two consecutive monthly injections of pasireotide-LAR were identified in seven medical centers in Israel. Patients with clinical, biochemical, and hormonal data available before and during pasireotide treatment were included in the study. A retrospective analysis including patients starting pasireotide treatment since 2016, as part of the national health system in Israel, was conducted. Patients previously treated with pasireotide as part of the randomized phase III clinical studies [9, 10] or under a compassionate treatment program were excluded. The study was conducted according to best clinical practice directives after being approved by the local ethical review board. The cohort included 35 patients, who were resistant or partially resistant to the commercially available SSAs, octreotide-LAR, or lanreotide autogel. Thus, when treated for 6 months or longer with SSAs as monotherapy, they did not achieve IGF-1 normalization. Nine of these patients continued with SSA injections, while pegvisomant treatment was added, some achieved now hormonal remission. Pasireotide was started following SSA and pegvisomant discontinuation. Pasireotide initiation and dose adjustments were performed at the treating endocrinologist’s discretion. Antidiabetic medications were introduced or augmented as required, according to current antidiabetic treatment recommendations of the American Diabetes Association.
Information on pituitary imaging, laboratory tests at diagnosis and during treatment with acromegaly directed therapeutic modalities, and starting date, dose, hormonal response, adverse events, and glycemic control during pasireotide treatment were collected from clinical records by the treating endocrinologist in each participating center.
GH and IGF-1 evaluation
Serum GH and IGF-1 levels were measured in the morning following an overnight fast, using chemiluminescent immunometric assays (Immulite 2000; Siemens) in most patients. The GH assay has a sensitivity of 0.05 ng/ml, an intra-assay coefficient of variation (CV) of 4.6% for a GH concentration of 3.7 ng/ml and an inter-assay CV of 5.7%. The intra-assay and inter-assay CVs for an IGF-1concentration of 380 ng/ml are 2.9% and 7.4%, respectively. Some patients had their IGF-1 levels measured by the Liaison chemiluminescence immunoassay (DiaSorin, Italy). IGF-1 levels are presented based on the upper limit of normal range (ULN; IGF-1 value divided by the sex-specific and age-specific upper normal limit), comparing values along the follow-up of each patient. Hormonal levels were measured by the same laboratory using the same hormonal assay before and during pasireotide-LAR treatment in each patient.
Hormonal control
Hormonal control under pasireotide-LAR treatment was defined by achieving normal sex and age adjusted IGF-1 levels throughout the follow-up treatment. Patients were considered partially controlled if IGF-1 levels under treatment were between 1-1.2 × ULN. Patients were considered to have pasireotide associated improvement when IGF-1 levels decreased ≥50% relative to baseline levels, but not below 1.2 × ULN. As only random morning GH levels were available before and while on pasireotide treatment, GH levels were not used to define remission.
Statistical analysis
Descriptive analysis was performed and results are expressed as mean ± SD and median, as appropriate. Mann–Whitney test was used to analyze hormonal and biochemical parameters prior and subsequent to pasireotide treatment initiation. A p-value < 0.05 was considered of statistical significance.
Results
Patients’ characteristics
The study cohort consisted of 35 patients (20 males, 15 females) with acromegaly treated in seven medical centers in Israel. Mean age was 40.8 ± 13.3 years (median, 39 years; range, 20–71) at diagnosis (Table 1), and 48.7 + 14.1 years (median, 46 years; range, 25–81) at the start of pasireotide therapy. There were 28 macroadenomas, three microadenomas, one patient with McCune-Albright syndrome and two adenomas with unknown size. Mean IGF-1 at diagnosis was 3.1 ± 1.3 × ULN (median; 2.93 × ULN) for age and gender (Table 1). Two patients presented with PRL co-secretion and two with TSH co-secretion. All patients except five underwent pituitary surgery, while six have previously undergone sellar radiotherapy (one patient, 3 months following pasireotide initiation; the others, 10–47 months before pasireotide). All patients were resistant to SSA treatment, up to octreotide LAR doses of 30 mg every 3 or 4 weeks, and lanreotide autogel 120–160 mg every 4 weeks or 120 mg every 3 weeks (Table 1). Pegvisomant and cabergoline doses reached up to 30 mg/day and 2 mg/week respectively, alone or in combination. Immediately before pasireotide-LAR initiation, eighteen patients were under SSA monotherapy and one subject was treated with pegvisomant. The remaining patients received combination therapy with SSA and pegvisomant, n = 9 (two of them received also cabergoline); SSA and cabergoline, n = 4; pegvisomant and cabergoline, n = 1. Two patients were untreated immediately before pasireotide initiation (Table 1), but were found resistant to SSA in the past. Thirty patients were uncontrolled under their respective medical regiments. Five patients had normal IGF-1 levels under combined treatment of SSA and pegvisomant before pasireotide, but four of them continued to experience severe headaches unresponsive to several pain management strategies. Their treatment was modified to explore if pasireotide could be more effective in headache control. Mean IGF-1 was 1.76 ± 0.9 × ULN (median, 1.59 × ULN) before switching to pasireotide-LAR. Mean HBA1C was 6.1% (median, 5.9%) and the prevalence of diabetes mellitus was 31.4% before pasireotide initiation.
Response to pasireotide
Pasireotide-LAR starting dose was 60 mg/4 weeks in six patients and 40 mg/4 weeks in the remaining cohort. IGF-1 normalization was achieved in 19 patients (54%), partial control (IGF-1 between 1-1.2 × ULN) was reached in five (in four of them, <1.05 ULN), and two additional patients experienced significant improvement in disease control (IGF-1 suppression ≥50% but still above 1.2 × ULN) (Fig. 1a). Biochemical response to pasireotide was based on repeated normal IGF-1 measurements (median, 3 measurements of normal IGF-1/patient). Pasireotide had no effect in nine patients (Figs. 1a and 2). Altogether, 26 out of 35 patients (74%) in the cohort benefited from pasireotide treatment. Out of four uncontrolled patients under combined SSA/ pegvisomant treatment, pasireotide normalized IGF-1 in three (Fig. 1b). Three other patients switched from combination SSA/pegvisomant therapy to pasireotide experienced a significant biochemical deterioration (Fig. 1b). The exclusion of five patients controlled by combination therapy did not change the overall results of the study (IGF-1 normalized in 17/30 uncontrolled patients, 56.6%). Among patients who normalized IGF-1 with pasireotide and after excluding 11 patients who received pagvisomant (with or w/o SSA), median random GH before pasireotide was 1.9 ng/ml. Three of the responders continued with cabergoline. Baseline IGF-1 level at diagnosis of acromegaly or IGF-1 before pasireotide initiation did not predict biochemical responsiveness, as 6/13 patients with severe disease and IGF-1 above 3 × ULN at diagnosis and 4/9 patients with ≥2 × ULN before being switched to pasireotide achieved remission.
IGF-1 levels presented as IGF-1 × ULN before (black bars) and following pasireotide treatment (gray bars): a in each of the 35 patients included in this study. *patients treated with SSA combined with pegvisomant before being switched to pasireotide; b in 9 patients on combination SSA with pegvisomant (black bars) and after being switched to pasireotide (gray bars). IGF-1 normal range, ≤1 × ULN; partial control, IGF-1 ≤ 1.2 × ULN
Six patients had severe headaches that resolved (n = 4) or significantly improved (n = 2) with pasireotide. Four of them achieved IGF-1 normalization, one had partial control, but in one patient IGF-1 levels rose. Irrespective of their hormonal response to pasireotide treatment, there was a significant decrease in headache frequency and intensity in all of them.
In six patients with excellent response to starting dose of pasireotide, monthly dose could be reduced by 20 mg with continuous IGF-1 control in five (Fig. 3). Importantly, IGF-1 normalization could be already detected in responding patients as early as after one or two pasireotide injections.
Two patients with mixed GH-TSH co-secreting adenomas normalized IGF-1 with pasireotide. However, one of them remained with elevated thyroid hormone levels when switched to pasireotide.
Currently six, nine, and three patients are well controlled with pasireotide doses of 20 mg, 40 mg, and 60 mg respectively. One of the responders discontinued treatment due to symptomatic cholelithiasis. Among patients partially controlled, three continue with 40 and two with 60 mg. Twenty six of the 35 patients included in this cohort continue with pasireotide injections (mean treatment interval, 13.1 ± 5.3 months; median, 12 months), and seven discontinued due to inefficacy.
Safety
Mean fasting glucose levels were 109 ± 28 mg/dl before and 138 ± 37 mg/dl after pasireotide initiation (p < 0.0001). Mean HBA1C levels increased from 6.1 ± 1.1% (median, 5.9%) to 6.7 ± 1.3% (median 6.35%) (p = 0.07) while on pasireotide treatment. Eleven patients with normal glucose metabolism did not experience deterioration and two others with mild impaired fasting glucose improved without specific treatment. Seventeen patients required initiation or intensification of antidiabetic treatment among the twenty-two who experienced worsening of hyperglycemia. In four patients HBA1C levels rose over 9%, requiring the addition of insulin to the treatment regimen in two of them. Both responding and non-responding patients developed hyperglycemia attributable to pasireotide. A 32-year-old McCune–Albrigth female patient with previous normal glucose levels, developed diabetes under pasireotide treatment. Despite having interrupted the medication due to inefficacy, she developed diabetic ketoacidosis two months later, requiring hospitalization. It is possible that pasireotide mediated inhibition of insulin secretion in this patient was profound and prolonged, contributing to this unexpected and unusual complication. Patients who had their pasireotide dose decreased due to excellent IGF-1 response tended to experience some improvement in glucose control. Development of hyperglycemia/diabetes mellitus did not lead to pasireotide discontinuation in any patient. One patient developed symptomatic cholelithiasis, and another had cholecystectomy due to cholelithiasis diagnosed previously while on lanreotide autogel treatment.
Discussion
The results of this retrospective study suggest that a considerable number of acromegaly patients resistant to first-generation SSA may benefit from treatment with monthly injections of pasireotide. In this cohort over 50% of patients achieved normalization of IGF-1 levels. Furthermore, 83% of responders were well controlled with low dose pasireotide (20-40 mg monthly injections). Interestingly, six patients exhibited over-responsiveness to pasireotide, with suppression of IGF-1 levels below the lower limit of normal range or to the lower range, thus requiring dose reduction that did not compromise disease control in most of them. The phenomenon of hormonal over-response to pasireotide has been previously reported in patients naïve to SSA treatment [9] and also after switching patients from octreotide to pasireotide therapy [11].
The rate of IGF-1 normalization found in our study is higher than previously reported. In a large, phase III RCT, patients with acromegaly naïve to medical treatment were assigned to receive either octreotide-LAR (n = 182) or pasireotide-LAR (n = 176) for twelve months [9]. Patients given pasireotide achieved a higher rate of IGF-1 normalization compared to those treated with octreotide (38.6% versus 23.6%). This could reflect the higher affinity of pasireotide for SSTR5, but the pituitary-directed effect of pasireotide and octreotide evaluated as GH reduction, was comparable in this study [9]. Other factors, such as a reduction of IGF-1 levels mediated by a stronger inhibition of insulin secretion by pasireotide compared to octreotide may partially explain these clinical findings. Patients with inadequate biochemical control at the end of the core study were eligible to switch from octreotide-LAR to pasireotide-LAR. IGF-1 normalization was achieved in 27% of these patients [12]. Another 24-week, phase III RCT (PAOLA) evaluated the efficacy of pasireotide-LAR treatment (40 or 60 mg/4 weeks; n = 65, in each group) in patients resistant to first-generation SSA. The control group consisted of patients that continued treatment with octreotide-LAR or lanreotide autogel (active control group; n = 68) despite being inadequately controlled by these analogues [10]. As expected, no patients in the active control group achieved IGF-1 normalization, compared with 25% of pasireotide treated patients [10]. In a phase II study with pasireotide-LAR (20–60 mg) conducted in 33 Japanese patients with acromegaly, medically naïve, or inadequately controlled by SSA or dopamine agonists, 27% of patients achieved normal IGF-1 levels after 12 months of treatment [13].
A recent Dutch study explored the therapeutic yield of switching acromegaly patients who were well controlled (IGF-1 ≤ 1.2 × ULN) by combined first-generation SSA and pegvisomant treatment, to pasireotide [14]. According to their response to an initial reduction in pegvisomant dose, patients were assigned to pasireotide monotherapy (60 mg/4 weeks) or combined with pegvisomant. It is not stated whether these patients were initially resistant to SSA monotherapy. Although 73.8% of patients were controlled after 12 weeks of the assigned treatment, and pegvisomant dose could be reduced by 66%, one cannot conclude from this study the efficacy of pasireotide alone.
Taken together, approximately 39% of naïve and 25% of patients resistant to SSA achieved disease control with pasireotide treatment in previous studies. A higher rate of pituitary surgery in our cohort may be one of the explanations for this difference in disease control rates. In the present study, 86% had undergone previous pituitary surgery, in comparison to only 40% in the head to head study comparing octreotide-LAR with pasireotide-LAR in acromegaly patients naïve to medical treatment [9]. After stratification, disease control was 50.7% and 30.5% in naïve patients with or without previous pituitary surgery, respectively [9]. Taken that our cohort comprised of patients resistant to previous treatment, the more appropriate comparison is with the PAOLA study that showed a 25% IGF-1 normalization under pasireotide-LAR 60 mg/4 weeks, of which only 63% had undergone previous surgery [10]. Thus, less patients in these two large prospective RCTs had the benefit of prior surgical debulking that has been shown to increase responsiveness to medical therapy [15].
Moreover, mean IGF-1 level before starting pasireotide was 1.76 ± 0.9 × ULN in the current study, compared to 2.6-2.8 × ULN in the PAOLA study [10].
Another possible explanation for the variable rates of medical remission in these cohorts may stem from the inherent different design of RCTs and retrospective studies. The advantages of RCTs may be compromised by the fact that the study population is highly selected by various inclusion and exclusion criteria. Therefore, it is possible that results obtained by highly controlled studies cannot be translated to the real-life scenario. Although our study was retrospective, this disadvantage may be, at least partially, remediated by the fact that it included most, if not all pasireotide treated acromegaly patients in Israel, since its registration in 2016. Because the medication is reimbursed by the national health system as second-line medical treatment for uncontrolled acromegaly patients resistant to SSA, and consequently largely available, the possibility of selection bias is minimal. In addition, the exclusion of patients previously treated with pasireotide in phase III studies or as part of a compassionate treatment program may be considered also as a potential selection bias. Previous radiation therapy is an additional factor that could potentially affect response rates to treatment. In contrast with the RCTs, in which previous radiation therapy was an exclusion criterion, six patients included in our cohort had received this treatment modality. Although three of them entered medical remission, it seems improbable that previous radiation therapy could explain the very early response of IGF-1 to pasireotide. The rapid IGF-1 suppression, as early as after one or two injections of pasireotide, has been recently reported by others [14]. This early response in not characteristic of first-generation SSA, in which, maximal therapeutic effect is expected only after 3–6 months of therapy.
An important, and to the best of our knowledge, as yet unreported observation was the beneficial effect of pasireotide in patients complaining of severe headaches, despite treatment with SSA. The effect was no less than dramatic, as patients previously incapacitated or with severely impaired functioning reported complete resolution or significant improvement in frequency and intensity of headaches, shortly after pasireotide initiation, with a consequent remarkable improvement in their quality of life. A similar analgesic effect has been previously reported with octreotide treatment, but the mechanism underlying this effect is unknown [16]. It can be speculated, that at least in these patients, signaling through SSTR5 is superior to SSTR2 in relieving headache associated with acromegaly.
In line with the known deleterious effect of pasireotide on glucose metabolism [9, 10, 13, 17], 63% of patients in this cohort experienced worsening of hyperglycemia and 49% required initiation or addition of antidiabetic treatment including insulin. This rate of glucose control deterioration is higher compared to the reported efficacy rate of 54%. However, treatment intensification resulted in good diabetes control in most patients. Thorough investigations conducted to underpin the underlying mechanisms mediating pasireotide-induced hyperglycemia implicate reduction of insulin secretion through binding to SSTR5 expressed on islet cells [18], as well as inhibition of incretin secretion by pasireotide [19]. Symptomatic colelithiasis that developed in two patients is a well-known side effect of SSA treatment. As our patients were not routinely referred for abdominal imaging, the true prevalence of asymptomatic cholelithiasis in our cohort is unknown.
Our study has several limitations. Its retrospective design did not allow for complete collection of relevant information, such as GH measurements and pituitary imaging during pasireotide treatment. Further, not all IGF-1 and GH measurements were performed using the same assay or conducted in a central laboratory, possibly compromising the accuracy of the results. Nevertheless, the use of ratios relative to age adjusted upper normal IGF-1 levels, and the fact that for each individual patient assays were performed in the same laboratory, may partially reduce the weight of this limitation. Another limitation is the relatively small number of patients in this cohort.
Still, this is the largest study assessing pasireotide-LAR efficacy as monotherapy in acromegaly patients resistant to SSA, since the registration trials.
In conclusion, in our “real life” retrospective study, we found that the majority of uncontrolled somatostatin resistant acromegaly patients benefited from pasireotide-LAR treatment, with a 54% rate of IGF-1 normalization, but with the tradeoff of glucose control deterioration in 63% of the cohort.
References
S. Melmed, Acromegaly. N. Engl. J. Med. 355, 2558–2573 (2006)
I.M. Holdaway, M.J. Bolland, G.D. Gamble, A meta-analysis of the effect of lowering serum levels of GH and IGF-I on mortality in acromegaly. Eur. J. Endocrinol. 159, 89–95 (2008)
L. Katznelson, E.R. Laws Jr., S. Melmed, M.E. Molitch, M.H. Murad, A. Utz, J.A. Wass; Endocrine Society, Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99, 3933–3951 (2014)
C. Schöfl, H. Franz, M. Grussendorf, J. Honegger, C. Jaursch-Hancke, B. Mayr, J. Schopohl; participants of the German Acromegaly Register, Long-term outcome in patients with acromegaly: analysis of 1344 patients from the German Acromegaly Register. Eur. J. Endocrinol. 168, 39–47 (2013)
A. Colao, R.S. Auriemma, M. Galdiero, G. Lombardi, R. Pivonello, Effects of initial therapy for five years with somatostatin analogs for acromegaly on growth hormone and insulin-like growth factor-I levels, tumor shrinkage, and cardiovascular disease: a prospective study. J. Clin. Endocrinol. Metab. 94, 3746–3756 (2009)
M.R. Gadelha, L.E. Wildemberg, M.D. Bronstein, F. Gatto, D. Ferone, Somatostatin receptor ligands in the treatment of acromegaly. Pituitary 20, 100–108 (2017)
A.J. van der Lely, B.M. Biller, T. Brue, M. Buchfelder, E. Ghigo, R. Gomez, J. Hey-Hadavi, F. Lundgren, N. Rajicic, C.J. Strasburger, S.M. Webb, M. Koltowska-Häggström, Long-term safety of pegvisomant in patients with acromegaly: comprehensive review of 1288 subjects in ACROSTUDY. J. Clin. Endocrinol. Metab. 97, 1589–1597 (2012)
C. Bruns, I. Lewis, U. Briner, G. Meno-Tetang, G. Weckbecker, SOM230: a novel somatostatin peptidomimetic with broad somatotropin release inhibiting factor (SRIF) receptor binding and a unique antisecretory profile. Eur. J. Endocrinol. 146, 707–716 (2002)
A. Colao, M.D. Bronstein, P. Freda, F. Gu, C.C. Shen, M. Gadelha, M. Fleseriu, A.J. van der Lely, A.J. Farrall, K. Hermosillo Reséndiz, M. Ruffin, Y. Chen, M. Sheppard; Pasireotide C2305 Study Group, Pasireotide versus octreotide in acromegaly: a head-to-head superiority study. J. Clin. Endocrinol. Metab. 99, 791–799 (2014)
M. Gadelha, M. Bronstein, T. Brue, M. Coculescu, M. Fleseriu, M. Guitelman, V. Pronin, G. Raverot, I. Shimon, K.K. Lievre, J. Fleck, M. Aout, A.M. Pedroncelli, A. Colao; Pasireotide C2402 Study Group, Superior efficacy of pasireotide versus continued treatment with octreotide or lanreotide in patients with inadequately controlled acromegaly: randomized prospective Phase III study. Lancet. Diabetes. Endocrinol 2, 875–884 (2014)
I. Shimon, W. Saeger, L.E. Wildemberg, M.R. Gadelha, Somatotropinomas inadequately controlled with octreotide may over-respond to pasireotide: the importance of dose adjustment to achieve long-term biochemical control. Hormones 16, 84–91 (2017)
M.D. Bronstein, M. Fleseriu, S. Neggers, A. Colao, M. Sheppard, F. Gu, C.C. Shen, M. Gadelha, A.J. Farrall, K. Hermosillo Reséndiz, M. Ruffin, Y. Chen, P. Freda; Pasireotide C2305 Study Group, Switching patients with acromegaly from octreotide to pasireotide improves biochemical control: crossover extension to a randomized, double-blind, Phase III study. BMC Endocr. Disord. 16, 16 (2016)
S. Tahara, M. Murakami, T. Kaneko, A. Shimatsu, Efficacy and safety of long-acting pasireotide in Japanese patients with acromegaly or pituitary gigantism: results from a multicenter, open-label, randomized, phase 2 study. Endocr. J. 64, 735–747 (2017)
A. Muhammad, A.J. van der Lely, P.J.D. Delhanty, A.H.G. Dallenga, I.K. Haitsma, J.A.M.J.L. Janssen, S.J.C.M.M. Neggers, Efficacy and safety of switching to pasireotide in acromegaly patients controlled with pegvisomant and first-generation somatostatin analogues (PAPE study). J. Clin. Endocrinol. Metab. 103, 586–595 (2018)
P. Petrossians, L. Borges-Martins, C. Espinoza, A. Daly, D. Betea, H. Valdes-Socin, A. Stevenaert, P. Chanson, A. Beckers, Gross total resection or debulking of pituitary adenomas improves hormonal control of acromegaly by somatostatin analogs. Eur. J. Endocrinol. 152, 61–66 (2005)
I. Donangelo, M. Rodacki, M.C. Peixoto, M. Vaisman, N.R. Caldas, M.R. Gadelha, Dependency and analgesia related to treatment with subcutaneous octreotide in patients with growth hormone-secreting tumors. Endocr. Pract. 10, 107–111 (2004)
M. Fleseriu, E. Rusch, E.B. Geer; ACCESS, Study Investigators Safety and tolerability of pasireotide long-acting release in acromegaly-results from the acromegaly, open-label, multicenter, safety monitoring program for treating patients who have a need to receive medical therapy (ACCESS) study. Endocrine 55, 247–255 (2017)
Y. Zambre, Z. Ling, M.C. Chen, X. Hou, C.W. Woon, M. Culler, J.E. Taylor, D.H. Coy, C. Van Schravendijk, F. Schuit, D.G. Pipeleers, D.L. Eizirik, Inhibition of human pancreatic islet insulin release by receptor-selective somatostatin analogs directed to somatostatin receptor subtype 5. Biochem. Pharmacol. 57, 1159–1164 (1999)
R.R. Henry, T.P. Ciaraldi, D. Armstrong, P. Burke, M. Ligueros-Saylan, S. Mudaliar, Hyperglycemia associated with pasireotide: results from a mechanistic study in healthy volunteers. J. Clin. Endocrinol. Metab. 98, 3446–3453 (2013)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I.S. has received research grants, consulting and lectureship fees from Novartis, Medison, and Pfizer. Y.G. received research grant from Pfizer, and research grant, travel support, and speaker fees from Novartis. The remaining authors declare that they have no conflict of interest.
Ethical approval
The study was conducted according to best clinical practice directives after being approved by the institutional ethical review board, with the 1964 Helsinki declaration and its later amendments.
Informed consent
Due to the retrospective design of the study, formal informed consent is not required. This article does not contain any studies with animals performed by any of the authors
Rights and permissions
About this article
Cite this article
Shimon, I., Adnan, Z., Gorshtein, A. et al. Efficacy and safety of long-acting pasireotide in patients with somatostatin-resistant acromegaly: a multicenter study. Endocrine 62, 448–455 (2018). https://doi.org/10.1007/s12020-018-1690-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1690-5