Abstract
Purpose
Proglucagon is expressed in both pancreatic alpha cells and intestinal epithelial L cells and is cleaved into glucagon and glucagon-like peptide-1 (GLP-1) by different prohormone convertases (PCs). Recent studies have shown that α-cells can also secrete GLP-1, which may improve islet function. However, little is known about the factors influencing GLP-1 secretion by α cells. In this study, we investigated whether insulin promotes GLP-1 secretion by α cells, as well as the mechanisms underlying this phenomenon.
Methods
We cultured the alpha-cell line In-R1-G9 in low- or high-glucose medium in the presence or absence of insulin to determine the influence of glucose concentrations on the actions of insulin. We also treated In-R1-G9 cells with insulin for different times and at different doses. Then GLP-1 and glucagon protein expression levels were estimated. Moreover, ERK and phosphatidylinositol-3-kinase/AKT (PI3K/AKT) pathway activity levels and prohormone convertase expression levels were evaluated to elucidate the mechanism underlying the effects of insulin on GLP-1 secretion by α-cells.
Results
Insulin promoted GLP-1 secretion in a time- and dose-dependent manner under high-glucose conditions. Inhibiting the PI3K/AKT pathway with LY294002 and the Ras/mitogen-activated protein kinase (RAS/MAPK) pathway with PD98059 reduced GLP-1 secretion, respectively, in inhibitor-treated cells compared with insulin-treated cells. Moreover, insulin increased prohormone convertase 1/3 expression levels in the corresponding group of IN-R1-G9 cells compared with the control group of cells.
Conclusion
Insulin facilitates GLP-1 secretion by pancreatic alpha cells by inducing PC1/3 expression under high-glucose conditions, a phenomenon that may be associated mainly with PI3K/AKT pathway activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insulin-secreting β-cells and glucagon-secreting α-cells play critical roles in maintaining sugar balance. Under normal physiological conditions, α-cells and β-cells interact to maintain blood glucose levels within an appropriate range [1,2,3]. According to the theory regarding the involvement of “double-hormones” in diabetes, which was proposed by Unger and Orci over 40 years ago, simultaneous relative or absolute hypoinsulinemia and hyperglucagonemia result in the development of type 2 diabetes mellitus (T2DM) [4]. The role of α-cells in the development of T2DM has historically been neglected. However, in recent years, the findings of some major studies regarding pancreatic α-cells have improved our understanding of the roles of these cells in the maintenance of normal pancreatic function and diabetes. The most important of these findings was noted in a study in which α-cells were found to transform into to β-cells in cases in which β-cells are massively damaged, their numbers are significantly reduced [5,6,7,8] or the expression levels of some transcription factors associated with their effects change [9, 10]. α-cell proliferation and glucagon-like peptide-1 (GLP-1) expression can be induced by high blood glucose, pregnancy, and streptozotocin injections, and GLP-1 plays a critical role in maintaining β-cell function and facilitating β-cell proliferation [11, 12]. These findings suggest that the pancreas may have evolved an intrinsic mechanism to compensate for β-cell damage.
Previous studies on L cells have shown that GLP-1 secretion by α cells is affected by many factors in addition to nutrients, such as neurotransmitters, cytokines, and insulin [13]. SDF-1 [14, 15] and interleukin-6 [16,17,18] have been shown to participate in α-cell hyperplasia and GLP-1 secretion. α-cells and β-cells are in close contact with each other, and insulin suppresses glucagon secretion in a paracrine manner; however, whether insulin secretion affects GLP-1 production by pancreatic α-cells is unclear. Thus, in this study, we investigated the role of insulin in GLP-1 secretion by pancreatic α-cells.
Materials and methods
Cell culture and treatments
In-R1-G9 cells were grown in RPMI-1640 (HyClone, USA) supplemented with 10% heat-inactivated fetal bovine serum (FBS) (Gibco, USA), 10 mg/ml penicillin and streptomycin at 37 °C with 5% CO2 and 95% air.
In-R1-G9 cells were cultivated in medium containing 5.2 mM or 25 mM glucose for 72 h. The cells were then incubated in RPMI-1640 without FBS for an additional 6 h, after which the supernatant was discarded, and the cells in the treatment group were treated with KRBS with 10-7 M insulin, and the cells in control group were treated with the same amount of PBS. Both groups of cells were treated with 0.5% BSA (Sigma, USA) and 0.1% DiprotinA (Biovision, USA, a specific dipeptidyl peptidase IV inhibitor), as described previously [19]. The cells were treated with the indicated reagents for 6 h, after which their supernatants were collected to measure GLP-1 and glucagon levels. To determine whether different insulin stimulation times and concentrations affected GLP-1 and glucagon secretion, we serum-starved the cells for 6 h, after which we stimulated them with 10-7 M insulin for different times (2, 6, and 24 h) or treated them with various concentrations of insulin (10−11 to 10−6 M) for 2 h under high-glucose (25 mM glucose) conditions. To confirm the effects of insulin resistance on In-R1-G9 cells, we incubated In-R1-G9 cells with 10−7 M insulin for 24 h to establish an insulin resistance model and then treated the cells with different concentrations of insulin to compare their responses to treatment with those of non-insulin resistant cells. Excess culture media were collected and frozen until needed for analysis.
Biochemical analyses
Total GLP-1 expression levels were assessed by ELISA (Millipore, USA). The antibody pair used in this assay measures GLP-17-36 and GLP-19-36 expression and has no significant cross-reactivity with glucagon, GLP-2, GIP, or oxyntomodulin. Glucagon levels were also measured by ELISA (Bluegene, CHN). The results of the assay were accepted when all of its quality control (QC) values fell within their excepted ranges.
Insulin signaling pathway in In-R1-G9 cells
To determine the effects of insulin on phosphatidylinositol-3-kinase/AKT (PI3K/AKT) and Ras/mitogen-activated protein kinase (RAS/MAPK) pathway activity and confirm the successful establishment of the insulin resistance cell model, we extracted total protein to measure phosphotyrosine (Abcam, USA), insulin receptor (β-subunit, Santa, USA), phospho-Akt (Ser473, Santa, USA), Akt (Santa, USA), phospho-ERK1/2 (Thr202/Tyr204, Abcam, USA), ERK1/2 (Abcam, USA), and GADPH (Cell Signaling Technology, USA) protein expression levels by western blotting, as previously described [20].
The cells were then pretreated with 50 μM LY294002 (Biovision, USA), a PI3K/AKT pathway inhibitor, or 50 μM PD98059 (Biovision, USA), a RAS/MAPK pathway inhibitor, for 15 min before being stimulated with 10−7 M insulin for 2 h, after which the supernatants were collected to detect GLP-1 and glucagon levels. Total protein was then extracted, and western blotting was performed as described above.
Mechanism responsible for insulin-induced GLP-1 secretion
Cellular proteins were extracted, and western blotting was performed as described above to measure prohormone convertase 1/3 (PC1/3) and prohormone convertase 2 (PC2) expression levels, as described in a previous study [19].
Statistical analysis
All data are expressed as the mean ± standard error of the mean (SEM). The data were analyzed by Student’s t-test or ANOVA with SPSS 22.0 software (SPSS Inc., Chicago, USA); however, some of the data were first ln or log10 transformed to normalize variance. p < 0.05 was considered statistically significant.
Results
Effects of different glucose concentrations on GLP-1 and glucagon secretion by In-R1-G9 cells
To determine the direct effects of glucose on GLP-1 and glucagon secretion by In-R1-G9 cells, as well as the optimum glucose concentration with which to simulate GLP-1 and glucagon secretion, we measured GLP-1 and glucagon levels in culture media. We found that that there was no significant difference in GLP-1 secretion between the low-glucose + insulin and low-glucose control groups; however, contrasting results were observed in the experiments in which glucagon secretion was measured. GLP-1 secretion was significantly increased in the high-glucose control group compared with the low-glucose control group, as GLP-1 levels were 277.27% higher in the former group than in the latter group [(136.12 ± 12.38) pM vs. (36.08 ± 3.16) pM, p < 0.001]. GLP-1 secretion was significantly increased in the high-glucose + insulin group compared with the low-glucose + insulin group, as GLP-1 levels were 56.82% higher in the former group than in the latter group [(213.80 ± 15.39) pM vs. (136.12 ± 12.38) pM, p < 0.05] (Fig. 1a). However, glucagon levels were significantly decreased in both insulin-treated groups compared with the corresponding control groups, and the difference in glucagon levels between the insulin-treated and control groups was larger in the low-glucose group than in the high-glucose group (Fig. 1b). Insulin and glucagon exerted contrasting effects on the GLP-1/glucagon ratio (Fig. 1c).
Effects of different glucose concentrations on GLP-1 and glucagon secretion by IN-R1-G9 cells. In-R1-G9 cells were divided into low-glucose and high-glucose groups, which were subsequently subdivided into control (white bars) and insulin groups (black bars). The low- and high-glucose groups were cultivated in 1640 medium containing 5.2 mM and 25 mM glucose, respectively. The cells in the insulin-treated subgroups were treated with 10-7 M, while the cells in the control subgroups were treated with the same amount of PBS. The cells were treated for 6 h, after which the cell supernatants were collected to measure GLP-1 and glucagon levels. *p < 0.05, **p < 0.01 compared with untreated control group that received the same glucose concentration; ###p < 0.001 compared with untreated control group that received low glucose
Effects of different insulin stimulation times on GLP-1 and glucagon secretion by In-R1-G9 cells
The level of GLP-1 secreted by IN-R1-G9 cells increased significantly, namely, by 70.54% [(262.58 ± 16.12) pM vs. (153.97 ± 12.91) pM, p < 0.01], in the experimental group compared with the control group after 2 h of treatment with insulin. The level of GLP-1 secreted by IN-R1-G9 cells increased significantly, namely, by 64.98% [(284.66 ± 14.88) pM vs. (172.54 ± 12.73) pM, p < 0.05], in the experimental group compared with the control group after 6 h of treatment with insulin. The level of GLP-1 secreted by IN-R1-G9 cells increased significantly, namely, by 60.25% [(327.98 ± 14.01) pM vs. (204.67 ± 11.28) pM, p < 0.05], in the experimental group compared with the control group after 24 h of treatment with insulin. The most significant difference in GLP-1 secretion between the experimental and control groups was noted after 2 h of treatment with insulin (Fig. 2a). Thus, 2 h was chosen as the optimum insulin stimulation time for subsequent experiments. However, the level of glucagon secreted by IN-R1-G9 cells was inversely correlated with the duration of insulin treatment (Fig. 2b).
Effect of different insulin stimulation times on GLP-1 and glucagon secretion by IN-R1-G9 cells. Under high-glucose conditions (25 mM glucose), IN-R1-G9 cells were stimulated with 10-7 M insulin (black bars) for 2, 6, and 24 h, after which the supernatants were collected to measure GLP-1 and glucagon levels, as previously described. *p < 0.05, **p < 0.01, ***p < 0.001 compared with untreated control group (white bars)
Effects of different insulin dosages and insulin resistance on GLP-1 and glucagon secretion by In-R1-G9 cells
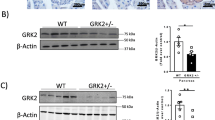
To investigate the ability of different insulin concentrations and differences in insulin sensitivity to influence GLP-1 and glucagon secretion by α-cells, we treated IN-R1-G9 cells with high concentrations of insulin (10−7 M) for 24 h to establish an insulin resistance model. To determine whether the model was successfully established, we evaluated phosphotyrosine, insulin receptor, phospho-Akt, total Akt, phospho-ERK1/2, total ERK1/2, and GAPDH protein expression levels by western blotting, the results of which showed that treatment with high concentrations of insulin-induced increases in the expression levels of the proteins mentioned above. However, insulin-induced insulin receptor phosphorylation levels and total insulin receptor protein expression levels decreased by 31.39 and 51.43% in pretreated IN-R1-G9 cells compared with control cells (Fig. 3a, b), while Akt and ERK1/2 phosphorylation levels decreased significantly in pretreated IN-R1-G9 cells compared with control cells (Fig. 3c, d).
Effects of different insulin concentrations and insulin resistance on GLP-1 and glucagon secretion by IN-R1-G9 cells. a–d IN-R1-G9 cells were pretreated without or with high-dose (10-7 M) insulin for 24 h to induce insulin resistance. After being washed thrice with Krebs-Ringer buffer, the cells were treated with 10−7 M insulin for 2 h, and then aliquots of cell lysates were subjected to western blot analysis to confirm that the model had been successfully established. *p < 0.05, **p < 0.01, ***p < 0.001 compared with untreated control group; #p < 0.05, ##p < 0.01 compared with pretreatment group. e–g GLP-1 and glucagon secretion levels and the GLP-1/glucagon ratio as a result of treatment with medium alone (control) or insulin (10−11 to 10−6 M) in the presence of high glucose in the non-insulin resistance group (white bars) and insulin resistance group (black bars). GLP-1 and glucagon secretion levels were determined by ELISA. *p < 0.05, **p < 0.01, ***p < 0.001 compared with untreated control group; #p < 0.05, ##p < 0.01 compared with insulin resistance group
We then treated IN-R1-G9 cells with media containing 10−11 to 10−6 M insulin. We found that as the insulin concentration increased, the level of GLP-1 secretion in each group initially increased and then decreased. The levels of GLP-1 secretion peaked in the non-insulin resistance and insulin resistance groups when the insulin concentrations in the media were 10−7 M and 10−8 M, respectively. Under these conditions, the levels of GLP-1 secretion in the indicated groups were 92.57% [(366.98 ± 9.85) pM vs. (190.57 ± 9.83) pM, p < 0.05] and 70.82% [(246.37 ± 11.56) pM vs. (144.23 ± 7.98) pM, p < 0.05] higher than the corresponding levels in the control group. We also found that insulin-induced GLP-1 levels were higher in the non-insulin resistance group than the insulin resistance group (Fig. 3e). The glucagon secretion level displayed a downward overall trend in the two groups (Fig. 3g), while the GLP-1/glucagon ratio displayed an upward trend that was consistent with the trend in the GLP-1 level. Insulin had no effect on the above ratio when administered at a concentration between 10−7 and 10−6 M in the non-insulin resistance group; however, insulin had a significant effect on the indicated ratio when administered at a concentration between 10-7 and 10-6 M in the insulin resistance group (Fig. 3f).
Effect of insulin signaling pathway inhibition on GLP-1 and glucagon secretion by In-R1-G9 cells
To determine whether insulin-induced AKT or ERK1/2 phosphorylation was associated with GLP-1 secretion, we performed AKT and ERK1/2 assays. Insulin significantly increased p-AKT and p-ERK1/2 expression by 843.80% (p < 0.001) and 260.14% (p < 0.01), respectively (Fig. 4a, b), in treated cells compared with control cells. However, when IN-R1-G9 cells were treated with the PI3K/AKT pathway inhibitor LY294002, AKT phosphorylation was inhibited, and GLP-1 secretion decreased by 55.95% [(158.31 ± 12.39) pM vs. (359.42 ± 31.92) pM, p < 0.01] in inhibitor-treated cells compared with insulin-treated cells. When IN-R1-G9 cells were treated with the RAS/MAPK pathway inhibitor PD98059, ERK1/2 phosphorylation was suppressed, and GLP-1 secretion decreased by 36.37% [(228.7 ± 12.52) pM vs. (359.42 ± 31.92) pM, p < 0.05] (Fig. 4a–c) in inhibitor-treated cells compared with insulin-treated cells. There was a significant difference in the degree to which GLP-1 secretion was inhibited between the LY294002- and PD98059-treated groups (p < 0.05). As expected, glucagon levels increased in both inhibitor-treated groups compared with the insulin-treated group (Fig. 4d), and LY294002 and PD98059 significantly suppressed insulin-induced increases in the GLP-1/glucagon ratio (Fig. 4f).
Effects of insulin signaling pathway inhibition on GLP-1 and glucagon secretion by IN-R1-G9 cells. In-R1-G9 cells were pretreated with or without the pharmacological inhibitors LY294002 (50 μM) or PD98059 (50 μM) for 15 min before being stimulated with or without 10-7 M insulin for 2 h. a, b Aliquots of cell lysates were subjected to western blot analysis. **p < 0.01, ***p < 0.001 compared with untreated control group; ###p < 0.001 compared with insulin + LY294002 or insulin + PD98059 group. c–e Samples of medium were collected for measurements of GLP-1 and glucagon expression by ELISA or kept frozen at –20 °C. *p < 0.05, **p < 0.01 compared with insulin group; #p < 0.05 as indicated
Effects of insulin on PC1/3 and PC2 levels
As PC1/3 and PC2 play important roles in GLP-1 synthesis [13], we investigated whether insulin and LY294002 or PD98059 affect PC1/3 and PC2 protein expression levels in this study. Under high-glucose conditions, PC1/3 expression levels were increased, and PC2 expression levels were decreased in insulin-stimulated cells compared with control cells. However, PC1/3 expression levels decreased significantly, and PC2 expression levels increased significantly when insulin-stimulated cells were pretreated with LY294002 or PD98059 compared with when they were treated with insulin alone (Fig. 5).
Effects of insulin on PC1/3 and PC2 expression levels. In-R1-G9 cells were cultured under the same conditions as those described in Fig. 4. Cellular proteins were extracted, and western blotting was performed to measure PC1/3, PC2, and GAPDH expression. *p < 0.05, **p < 0.01 compared with untreated control group; #p < 0.05, ##p < 0.01 compared with insulin-treated group
Discussion
In pancreatic islets, the ratio of of β-cells to α-cells is approximately 4:1-3:1 [21]. The two types of cells are interconnected and exchange signaling molecules to reciprocally regulate the secretion activity of their counterparts [2, 3]. Pancreatic α-cells are generally considered glucagon-secreting cells [22]. Both GLP-1 and glucagon are eventually synthesized as a result of transcription and translation of the glucagon gene [23, 24]. Pancreatic α-cells have also been found to secrete GLP-1 [6]. However, the mechanism through which this process occurs remains unclear. We investigated the effects of insulin on GLP-1 secretion using glucagon-secreting IN-R1-G9 cells as a pancreatic α-cell model. The results showed that insulin could affect GLP-1 secretion by α-cells and have shed more light on the mechanisms governing the interactions between pancreatic α- and β-cells.
The α-cell line used in this study was the glucagon-secreting IN-R1-G9 cell line, which was derived from the rat insulinoma IN-111-R1 cell line by single-cell cloning. The biological characteristics of this cell line are similar to those of primary α-cells and enable the cells in question to produce glucagon. No insulin was detected in the cell supernatant by radioimmunoassay (RIA). The cell line also reacted properly to stimuli, such as glucose and arginine, and has been considered a good model for studies on glucagon [25]. Most of the studies on GLP-1 secretion by α cells have utilized primary pancreatic islet cells and αTC1-6 cells, and few studies have reported whether IN-R1-G9 cells can produce GLP-1. In this study, we found that IN-R1-G9 cells can produce a small amount of GLP-1 under low-glucose conditions (5.2 mM); however, GLP-1 secretion levels increased significantly in cells cultured under high-glucose conditions (25 mM). These results were consistent with those of previous investigations on vivo pancreatic islets and αTC1-6 cells [26] and indicated that GLP-1 release is dependent on glucose concentrations.
Insulin plays an important role in the interaction between β-cells and α-cells; thus, we focused on the effects of insulin on GLP-1 secretion by α-cells. After IN-R1-G9 cells were treated with 10−7 M insulin in high-glucose medium for 6 h, the GLP-1 concentration in the corresponding supernatant increased by 96.54%; however, no such increase in GLP-1 levels occurred in cells cultured in low-glucose medium. Thus, we concluded that the effects of insulin on GLP-1 secretion by α-cells were glucose concentration-dependent. Furthermore, we also found that the effects of insulin on GLP-1 secretion by IN-R1-G9 cells were time- and concentration-dependent. We also successfully established cell models of insulin resistance by pretreating IN-R1-G9 cells with insulin at high concentrations, as previously described [27]. We found that pretreatment with insulin impaired the sensitivity of the indicated cells to insulin. These results signified the importance of combating insulin resistance.
What are the mechanisms underlying these phenomena? IN-R1-G9 cells have been shown to have insulin receptors (IRs) on their surfaces (approximately 2.0 × 104/cell) [28]; thus, we investigated whether the classical insulin signaling pathways, namely, the PI3K/AKT (PKB) and RAS/MAPK pathways, participated in insulin-mediated GLP-1 secretion. Insulin signaling is mediated by a complex signaling network involving several pathways and hundreds of molecules. Of these, the PI3K/AKT (PKB) and RAS/MAPK pathways are the major pathways underlying insulin-induced GLP-1 secretion. The former pathway participates in insulin metabolism, and the latter pathway regulates gene expression and cooperates with the PI3K pathway to regulate cell proliferation and differentiation [24, 29]. The PI3K inhibitor LY294002 and the MEK inhibitor PD98059 were used to investigate the effects of the pathways on insulin-mediated GLP-1 secretion. Both inhibitors attenuated the effects of insulin on GLP-1 secretion. Specifically, they reduced insulin-mediated GLP-1 secretion by 55.95% and 36.37%, respectively, which suggested that the PI3K/AKT and RAS/MAPK pathways may both participate in insulin-induced GLP-1 secretion.
Posttranslational modifications of the glucagon gene are tissue specific, as the modifications are catalyzed by different prohormone convertases found in different tissues [30]. In intestinal L cells, GLP-1, GLP-2, glicentin, and oxyntomodulin are synthesized through a reaction catalyzed by PC1/3. In α-cells, PC2 facilitates glucagon synthesis [23]. In this study, we investigated PC1/3 and PC2 expression at the protein level in IN-R1-G9 cells. The results indicated that insulin enhanced PC1/3 expression and inhibited PC2 expression, effects that were attenuated by LY294002 and PD98059. These data suggested that insulin could affect PC1/3 and PC2 expression through the PI3K/AKT and RAS/MAPK pathways in IN-R1-G9 cells.
The study showed that the regulatory effects of insulin on GLP-1 and glucagon secretion by pancreatic α-cells contrasted with each other and varied according to the conditions in which the cells were cultured. Therefore, the GLP-1/glucagon ratio was measured to determine proglucagon-derived peptide production levels in pancreatic α-cells. The results showed that the GLP-1/glucagon ratio increased in response to treatment with insulin under high-glucose conditions mimicking diabetes, indicating that insulin could significantly increase the ratio and that high glucose and insulin could stimulate the compensatory functions of pancreatic α-cells.
Collectively, the results of our study suggested that insulin boosted GLP-1 secretion by increasing PC1/3 expression in pancreatic α-cells under high-glucose conditions. Both the PI3K/AKT and RAS/MAPK pathways were involved in this process. The above phenomenon may represent a new mechanism by which pancreatic α-cells and β-cells interact, especially in hyperglycemia.
References
E. Mannucci, F. Tesi, G. Bardini et al. Effects of metformin on glucagon-like peptide-1 levels in obese patients with and without Type 2 diabetes. Diabetes Nutr. Metab. 17, 336–342 (2004)
C. Over, D.M. Berman, N.S. Kenyon et al.The unique cytoarchitecture of human pancreatic islets has implications for islet cell function. Proc. Natl Acad. Sci. USA 103, 2334–2339 (2006)
D.J. Steiner, A. Kim, K. Miller, M. Hara Pancreatic islet plasticity: Interspecies comparison of islet architecture and composition. Islets 2, 135–145 (2010)
R.H. Unger, L. Orci, The essential role of glucagon in the patho-genesis of diabetes mellitus. Lancet 1, 14–16 (1975)
J.S. Moon, K.C. Won, Pancreatic α-cell dysfunction in type 2 diabetes: old kids on the block. Diabetes Metab. J. 39, 1–9 (2015)
F. Thorel, V. Népote, I. Avril et al. Conversion of adult pancreatic alpha-cells to beta-cells after extreme beta-cell loss. Nature 464, 1149–1154 (2010)
C.H. Chung, E. Hao, R. Piran et al. Pancreatic beta cell neogenesis by direct conversion from mature alpha cells. Stem Cells 28, 1630–1638 (2010)
L. Ye, M.A. Robertson, D. Hesselson, D.Y. Stainier, R.M. Anderson, Glucagon is essential for alpha cell transdifferentiation and beta cell neogenesis. Development 142, 1407–1417 (2015)
P. Collombat, X. Xu, P. Ravassard et al. The ectopic expression of Pax4 in the mouse pancreas converts progenitor cells into alpha and subsequently beta cells. Cell 138, 449–462 (2009)
Y.P. Yang, F. Thorel, D.F. Boyer, P.L. Herrera, C.V. Wright, Context-specific alpha-to-beta-cell reprogramming by forced Pdx1 expression. Genes Dev. 25, 1680–1685 (2011)
R.D. Wideman, I.L. Yu, T.D. Webber et al. Improving function and survival of pancreatic islets by endogenous production of glucagon-like peptide 1. Proc. Natl Acad. Sci. USA 103, 13468–13473 (2006)
G.E. Fava, E.W. Dong, H. Wu, Intra-islet glucagon-like peptide 1. J. Diabetes Complicat. 30, 1651 (2016)
G.E. Lim, P.L. Brubaker, Glucagon-like peptide 1 secretion by the L-cell: the view from within. Diabetes 55, S70 (2006)
P. Marchetti, R. Lupi, M. Bugliani et al. A local glucagon-like peptide 1 (GLP-1) system in human pancreatic islets. Diabetologia 55, 3262–3272 (2012)
Z. Liu, V. Stanojevic, S. Avadhani, T. Yano, J.F. Habener, Stromal cell-derived factor-1 (SDF-1)/chemokine (C-X-C motif) receptor 4 (CXCR4) axis activation induces intra-islet glucagon-like peptide-1 (GLP-1) production and enhances beta cell survival. Diabetologia 54, 2067–2076 (2011)
H. Ellingsgaard, I. Hauselmann, B. Schuler et al. Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and alpha cells. Nat. Med. 17, 1481–1489 (2011)
K. Timper, E. Dalmas, E. Dror et al. Glucose-dependent insulinotropic peptide stimulates glucagon-like peptide 1 production by pancreatic islets via interleukin-6, produced by α cells. Gastroenterology 151, 165 (2016)
R.D. Wideman, I.L. Yu, T.D. Webber et al. Improving function and survival of pancreatic islets by endogenous production of glucagon-like peptide 1 (GLP-1). Proc. Natl Acad. Sci. USA 103, 13468–13473 (2006)
S. Piro, L.G. Mascali, F. Urbano et al. Chronic exposure to GLP-1 increases GLP-1 synthesis and release in a pancreatic alpha cell line (α-TC1): evidence of a direct effect of GLP-1 on pancreatic alpha cells. PLoS ONE 9, e90093 (2014)
G.E. Lim, G.J. Huang, N. Flora et al. Insulin regulates glucagon-like peptide-1 secretion from the enteroendocrine L cell. Endocrinology 150, 580–591 (2008)
B. Domenico, A. Mathieu, M. Philippe et al. Unique arrangement of alpha- and beta-cells in human islets of Langerhans. Diabetes 59, 1202–1210 (2010)
P.J. Lefèbvre, Early milestones in glucagon research. Diabetes Obes. Metab. 13(Suppl. 1), 1–4 (2011)
S. Dhanvantari, N.G. Seidah, P.L. Brubaker, Role of prohormone convertases in the tissue-specific processing of proglucagon. Mol. Endocrinol. 10, 342–355 (1996)
S. Vasu, R.C. Moffett, N.H. McClenaghan, P.R. Flatt, Differential molecular and cellular responses of GLP-1 secreting L-cells and pancreatic alpha cells to glucotoxicity and lipotoxicity. Exp. Cell Res. 336, 100–108 (2015)
R. Takaki, J. Ono, M. Nakamura et al. Isolation of glucagon-secreting cell lines by cloning insulinoma cells. In Vitr. Cell. Dev. Biol. 22, 120–126 (1986)
N.M. Whalley, L.E. Pritchard, D.M. Smith et al. Processing of proglucagon to GLP-1 in pancreatic α-cells: is this a paracrine mechanism enabling GLP-1 to act on β-cells? J. Endocrinol. 211, 99–106 (2011)
S. Muntoni, S. Muntoni, Insulin resistance: pathophysiology and rationale for treatment. Ann. Nutr. Metab. 58, 25–36 (2011)
K. Kisanuki, H. Kishikawa, E. Araki et al. Expression of insulin receptor on clonal pancreatic alpha cells and its possible role for insulin-stimulated negative regulation of glucagon secretion. Diabetologia 38, 422–429 (1995)
C.M. Taniguchi, B. Emanuelli, C.R. Kahn, Critical nodes in signalling pathways: insights into insulin action. Nat. Rev. Mol. Cell Biol. 7, 85–96 (2006)
Y. Anini, P.L. Brubaker, Muscarinic receptors control glucagon-like peptide 1 secretion by human endocrine L cells. Endocrinology 144, 3244–3250 (2003)
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 81670706 and 81770818), National Special Scientific Research Fund of Public Welfare Profession (No. 201502007), National Key Research and Development Plan (No. 2016YFC0901204).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Liu, P., Song, J., Liu, H. et al. Insulin regulates glucagon-like peptide-1 secretion by pancreatic alpha cells. Endocrine 62, 394–403 (2018). https://doi.org/10.1007/s12020-018-1684-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1684-3