Abstract
In the past decades, dietary guidelines focused on reducing saturated fat as the primary strategy for cardiovascular disease prevention, neglecting the many other potential effects of diet on health, in particular the harmful effects of sugar. A greater intake of soft drinks (sugar-sweetened beverages), for example, is associated with a 44% increased prevalence of metabolic syndrome, a higher risk of obesity, and a 26% increased risk of developing diabetes mellitus. Carbohydrates comprise around 55% of the typical western diet, ranging from 200 to 350 g/day in relation to a person’s overall caloric intake. For long-term weight gain, food rich in refined grains, starches, and sugar appear to be major culprits. Low-carbohydrate diets restrict daily carbohydrates between 20 and 50 g, as in clinical ketogenic diets. The results of controlled trials show that people on ketogenic diets (a diet with no more than 50 g carbohydrates/day) tend to lose more weight than people on low-fat diets. Moreover, there is no good evidence for recommending low-fat diets, as low-carbohydrate diets lead to significantly greater weight loss (1.15 kg) than did low-fat interventions. However, the magnitude of such a benefit is small. As the quality of ingested carbohydrates seems more important than the quantity for health outcomes, people with metabolic disorders should avoid or substantially reduce low-fiber, rapidly digested, refined grains, starches, and added sugars. So, the consumption of the right carbohydrates (high-fiber, slowly digested, and whole grains), in a moderately lower amount (between 40 and 50% of daily energy content), is compatible with a state of good health and may represent a scientifically-based and palatable choice for people with metabolic disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“Too much of a good thing” may be toxic (Anonymous)
In the last decades, dietary recommendations have mainly focused on dietary fat, blood cholesterol, or total calories, hiding the many other potential effects of diet on health. We now know that diet can influence not only glucose and lipid levels, but also other cardiometabolic risk factors, such as oxidative stress, inflammation, and endothelial health, hardly considered before to be diet-linked [1, 2]. We also know that diets focused on isolated nutrient targets, such as low-fat diets, produce little clinical benefit on cardiovascular (CV) disease, diabetes mellitus, or insulin resistance [3]. By contrast, healthy dietary patterns, such as Mediterranean diet patterns, are consistently associated with lower risk of clinical events [4,5,6,7]. And finally, we know that the quality of foods affect weight homeostasis in the long-term, in such a way that all calories are not equal for long-term adiposity.
The carbohydrates are not all the same
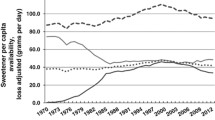
By 1967, both sugar and saturated fat were identified as mortality risk factors [8]. Mortality rates in the US at that time were one of the highest in the world, with about 820 deaths per 100,000 persons per year, and were the same for both sugar consumption (130 pounds per year) and saturated fat (33% of total daily calories). In Italy, mortality rates were eight-fold lower (about 100 per 100,000 persons per year) and were associated with a saturated fat consumption of 10% of total daily calories, and sugar consumption of 40 pounds per year. Despite this evidence, for decades following those data, dietary guidelines focused on reducing saturated fat as the primary strategy for CV disease prevention.
When consumed in excess, both sugars and saturated fat are markers of Western dietary patterns associated with increased chronic disease risk [9]. Carbohydrate-rich foods bring about half or more of all calories in most diets. However, it has become clear that not all carbohydrates are the same and that the quality of carbohydrate-rich foods is linked to risk. Foods rich in dietary fiber and whole grain contents (such as fruits, legumes, vegetables, and whole grains) are protective, whereas foods rich in refined grains (such as white bread, white rice, cereal, crackers, and bakery desserts), starches (potatoes), and added sugars (sugar-sweetened beverages, candy) are harmful. As it happens for total fat, the cardiometabolic effects of total carbohydrate are modified by the quality of the carbohydrate.
The added sugar: a threaten to cardiometabolic health
Despite decades of dietary guidelines promoting low-fat eating, obesity has continued to strike at an alarming rate. A greater intake of soft drinks (sugar-sweetened beverages, SSBs) is associated with a 44% increased prevalence of metabolic syndrome [10], a higher risk of obesity [11], and a 26% increased risk of developing diabetes mellitus [12]. The association of soft drink consumption with obesity and higher insulin resistance has been attributed to multiple factors, including greater caloric intake, its high fructose content, less satiety, and a positive general effect of consuming refined carbohydrates [13].
In order to limit their consumption, it has been proposed adding taxes to processed foods that contain any form of added sugars, defined as any sweetener containing the molecule fructose added to food in processing. This would include carbonated soft drinks, sports drinks, and energy drinks. Currently, a US citizen consumes an average of 216 L of soda per year, of which 58% contains sugar: translating in calories, this means about >600 calories per person per day [14]. The US does not have a nationwide soda tax, but a few of its cities have passed their own tax. The first US sugar tax on SSBs introduced in Berkeley, California, has been associated with soft drink sales fall by almost 10% [15]. Whether these taxes ultimately improve health outcomes remains unknown. However, when the consumption of harmful foods has been prohibited or regulated by law, there has been an improvement of health outcome.
For example, New York City was the first large metropolitan area in the US to restrict transfatty acids, recognized as non-safe by FDA on June 16 2015, in eateries (restaurants, bakeries, cafeterias, senior-meal programs, mobile food-vending units, soup kitchens, park concessions, street-fair food booths). A retrospective observational pre-post study [16] of residents in counties with trans-fatty acids restrictions versus counties without restrictions demonstrated a 4.5% reduction in CV mortality in counties within 1 year after restrictions, which translated to 13 fewer CV deaths per 100,000 persons per year.
Obesity, metabolic syndrome, and type 2 diabetes
The results from the Global Burden of Disease obtained in 195 Countries over 25 years show that a total of 107.7 million children and 603.7 million adults were obese [17]. Around 40% of US adults and 19% of US children are now obese; moreover, more than half of today’s children are expected to be obese by age 35 years [18]. More than 29 million US adults have diabetes [19]; without major changes, as many as 1 in 3 US adults could have diabetes by 2050. By 2012, more than one-third (34–35%) of all US adults met the criteria for metabolic syndrome, with the highest burden being among adults with low socioeconomic status [20]. Metabolic syndrome is not driven solely by the rising prevalence of obesity among US adults, as its prevalence was constant over time even among the nonobese people. Prevalence of metabolic syndrome increases with age: given the demographic trend in the western population of increasing age, a further increase in metabolic syndrome prevalence is to be expected, associated with a concomitant increase in related chronic diseases and conditions.
Low-carbohydrate (carb) diets
Carbohydrates comprise around 55% of the typical western diet, ranging from 200 to 350 g/day in relation to a person’s overall caloric intake. Low-carb diets restrict daily carbs between 20 and 50 g, as in clinical ketogenic diets. Given the variable reduction of sugars and starches, the body reduces insulin secretion and switches to burning fat, and this happens primarily on the very low-carb diet. In this metabolic state—i.e., nutritional ketosis— the liver converts fatty acids into ketone bodies that provide fuel to the body’s tissues; moreover, ketone bodies can penetrate the blood-brain barrier and are used by the brain as a fuel.
Confirming the results of earlier systematic reviews [21, 22], a more recent meta-analysis [23] of 13 randomized controlled trials show that people on ketogenic diets (a diet with no more than 50 g carbohydrates/day) tend to lose more weight than people on low-fat diets. Tobias et al. [24] did a systematic review and meta-analysis of randomized trials comparing the long-term effect (≥1 year) of dietary interventions on weight loss. According to their main conclusion, there is no good evidence for recommending low-fat diets, as the difference in weight loss was just 0.36 kg when low-fat weight loss diets were compared with various other higher-fat weight loss diets. In fact, low-carbohydrate diets led to significantly greater weight loss than did low-fat interventions.
However, the magnitude of such a benefit is small: participants prescribed low-carbohydrate diets lost only about 1 kg (1.15 kg) of additional weight after 1 year compared with those advised to consume low-fat diets. Although statistically significant, this difference is likely without clinical meaning [25]. Furthermore, irrespective of the diet prescription, the overall average weight loss in trials testing interventions designed to reduce body weight is limited (about 3.75 kg). This is in line with the results of large randomized clinical trials with long-term dietary interventions for weight loss showing that individuals under intensive lifestyle interventions can lose about 4.8 kg [26].
One calorie is not always one calorie
The supposed beneficial effect of a low or very-low carb diets on body weight may be due to the modulation of resting energy expenditure. Under isoenergetic conditions, Ebbeling et al. [27] found that a carbohydrate-restricted diet is better than a low-fat diet for retaining an individual’s basal metabolic rate. In other words, the quality of calories consumed may affect the number of calories burned: metabolism slowed by more than 400 kcal/day on a low-fat diet while there was no significant decline in metabolic rate on a very low-carb diet. On the other hand, long-term diet adherence is low, irrespective of whether low-fat or other diets, such as low-carbohydrate diets, are prescribed [28].
Extra-weight effects
Individuals with metabolic syndrome, insulin resistance associated with obesity, and type 2 diabetes (all diseases of carbohydrate intolerance) are likely to see improvements in biomarkers of disease risk with well-formulated low or very-low carbohydrate diet. Glucose control improves [29] as a consequence of both less glucose introduction, and improved insulin sensitivity. Beyond reducing weight and insulin resistance, low-carb diets may also affect lipid levels, and associate with improvements in triglycerides and high-density lipoprotein (HDL) cholesterol levels, as well as a shift from more harmful small, dense LDL particles to less-harmful large, nondense particles; however, low-density lipoprotein (LDL) cholesterol levels may show an increase on the diet [30].
Dietary factors and cardiometabolic deaths
In the US, an estimated 45.4% of all cardiometabolic deaths (n = 318,656 due to heart disease, stroke, and type 2 diabetes) were associated with suboptimal intakes of 10 dietary factors in 2012 [31]. Among individual dietary components, the largest estimated mortality was associated with high sodium (9.5%), followed by low nuts/seeds (8.5%), high processed meats (8.2%), low seafood omega-3 fats (7.8%), low vegetables 7.6%), low fruits (7.5%), and high sugar-sweetened beverages (7.4%), while the lowest estimated mortality burdens were associated with low polyunsaturated fats (2.3%) and high unprocessed red meats (0.4%). Between 2002 and 2012, the total number of US cardiometabolic deaths associated with BBSs declined by 14.5%. In addition to direct harms, low-quality carbohydrates such as refined grains, certain potatoes, SSBs, and sweets may increase cardiometabolic risk by displacing other, healthier foods in the diet, e.g., fruits, vegetables, nuts, legumes, and minimally processed whole grains.
The optimal diet for metabolic disorders
Meal planning should be individualized for individuals with metabolic disorders, as it has been suggested for the diabetic patient [32]. Moreover, the ideal percentage of calories from macronutrients (carbohydrate, protein, and fat) may be not the same for all people. A variety of eating patterns are acceptable [33, 34], including Mediterranean [35, 36], dietary approaches to stop hypertension (DASH) [37, 38], and plant-based diets [39, 40]. All they are examples of healthful eating patterns, although individualized meal planning should focus on personal preferences, needs, and goals.
Dietary patterns that have demonstrated beneficial outcomes share many characteristics, including increased consumption of minimally processed foods such as fruits, nuts/seeds, vegetables (excluding potatoes), legumes, whole grains, seafood, yogurt, and vegetable oils (olive oil in the Mediterranean diet); and fewer consumption of red meats, processed (sodium-preserved) meats, and foods rich in refined grains, starches, and added sugars. Such diets are higher in natural antioxidants, fiber, vitamins, minerals, phenolics, and unsaturated (monounsaturated and polyunsaturated) fats, and lower in glycemic load, glycemic index, salt, and trans fat.
Mediterranean diet produces significant cardiometabolic benefits in people with metabolic disturbances [41, 42]. Increased consumption of high-quality foods cools down inflammation, ameliorates endothelial dysfunction, and reduces oxidative stress [43]. This in turn may improve insulin sensitivity in the peripheral tissues, acting as a barrier to the metabolic syndrome and type 2 diabetes.
Conclusions
The optimal percentages of carbohydrates in a daily diet should be individualized for people with metabolic disorders, such as obesity, metabolic syndrome, and type 2 diabetes. As the quality of ingested carbohydrates seems more important than the quantity for health outcomes, people with metabolic disorders should avoid or substantially reduce low-fiber, rapidly digested, refined grains, starches, and added sugars. For long-term weight gain, foods rich in such carbohydrates appear to be major culprits. In a more general sense, the dietary patterns that have demonstrated cardiovascular [4, 5, 44, 45] or metabolic [35, 36] benefits in people at higher risk for cardiovascular disease, including the diabetic patient, present a carbohydrate content lower than 50% of daily energy content. So, the consumption of the right carbohydrates (high-fiber, slowly digested, and whole grains), in a moderately lower amount (between 40 and 50% of daily energy content) is compatible with a state of good health and may represent a scientifically-based and palatable choice for people with metabolic disorders. Reducing refined grains, starches, and added sugars is a major dietary priority for cardiometabolic health [46, 47]. However, patient education remains a cornerstone of therapy, to improve long-term adherence and hence to magnify the beneficial effects of diet [48].
References
D. Giugliano, A. Ceriello, K. Esposito, The effects of diet on inflammation: emphasis on the metabolic syndrome. J. Am. Coll. Cardiol. 48, 677–685 (2006)
K. Esposito, D. Giugliano, Diet and inflammation: a link to metabolic and cardiovascular diseases. Eur. Heart J. 27, 15–20 (2006)
R. Micha, D. Mozaffarian, Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: a fresh look at the evidence. Lipids 45, 893–905 (2010)
R. Estruch, E. Ros, J. Salas-Salvado, M.I. Covas et al., Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 368, 1279–1290 (2013)
K. Esposito, D. Giugliano, Mediterranean diet for primary prevention of cardiovascular disease. N. Engl. J. Med. 369, 674–675 (2013)
M.I. Maiorino, G. Bellastella, P. Chiodini et al., Primary prevention of sexual dysfunction with Mediterranean diet in type 2 diabetes: the MÈDITA randomized trial. Diabetes Care 39, e143–144 (2016)
M.I. Maiorino, G. Bellastella, M. Petrizzo, L. Scappaticcio, D. Giugliano, K. Esposito, Anti-inflammatory effect of Mediterranean diet in type 2 diabetes is durable: 8-year follow-up of a controlled trial. Diabetes Care 39, e44–45 (2016)
R.B. McGandy, D.M. Hegsted, F.J. Stare, Dietary fats, carbohydrates and atherosclerotic vascular disease. N. Engl. J. Med. 277, 186–192 (1967)
M. Nestle, Food industry funding of nutrition research. The relevance of history for current debates. JAMA Intern. Med. 176, 1685–1686 (2016)
R. Dhingra, L. Sullivan, P.F. Jacques et al., Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 116, 480–488 (2007)
M.B. Schulze, J.E. Manson, D.S. Ludwig, Sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 292, 927–934 (2004)
V. Malik, B.M. Popkin, G.A. Bray, J.P. Després, W.C. Willett, F.B. Hu, Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 33, 2477–2483 (2010)
A. Drewnowski, F. Bellisle, Liquid calories, sugar, and body weight. Am. J. Clin. Nutr. 85, 651–661 (2007)
R.H. Lustig, L.A. Schmidt, C.D. Brindis, The toxic truth about sugar. Nature 48, 27–29 (2012)
J. Falbe, H.R. Thompson, C.M. Becker, N. Rojas, C.E. McCulloch, K.A. Madsen, Impact of the Berkeley excise tax on sugar-sweetened beverage consumption. Am. J. Public. Health 106, 1865–1871 (2016)
E.J. Brandt, R. Myerson, M.C. Perraillon, T.S. Polonsky, Hospital admissions for myocardial infarction and stroke before and after the trans-fatty acid restrictions in New York. JAMA Cardiol. 2, 627–634 (2017)
The GBD 2015 Obesity Collaborators, Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377, 13–27 (2017)
NCHS, National Health and Nutrition Examination Survey, 2015–2016. NCHSData Brief, No. 288, October 2017 https://www.cdc.gov/nchs/data/databriefs/db288.pdf Accessed 23 Jan 2018
National Center for Chronic Disease Prevention and Health Promotion. At a glance 2016 diabetes. https://www.cdc.gov/chronicdisease/resources/publications/aag/pdf/2016/diabetes-aag.pdf Accessed 23 Jan 2018
J.X. Moore, N. Chaudhary, T. Akinyemiju, Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Prev. Chronic Dis. 14, 160287 (2017)
M. Hession, C. Rolland, U. Kulkarni et al., Systematic review of randomized controlled trials of low-carbohydrate vs. low-fat/low-calorie diets in the management of obesity and its comorbidities. Obes. Rev. 10, 36–50 (2009)
A.J. Nordmann, A. Nordmann, M. Briel et al., Effects of low-carbohydrate vs. low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch. Intern. Med. 166, 285–293 (2006)
N.B. Bueno, I.S. de Melo, S.L. de Oliveira, A. da Rocha, Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br. J. Nutr. 110, 1178–1187 (2013)
D.K. Tobias, M. Chen, J.E. Manson, D.S. Ludwig, W. Willett, F. Hu, Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 3, 968–979 (2015)
American College of Physicians, Primer on statistical significance and P values. Eff. Clin. Pract. 4, 183–184 (2001)
T.A. Wadden, S. Volger, D.B. Sarwer et al., A two-year randomized trial of obesity treatment in primary care practice. N. Engl. J. Med. 365, 1969–1979 (2011)
C.B. Ebbeling, J.F. Swain, H.A. Feldman et al., Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA 307, 2627–2634 (2012)
K.D. Hall, Prescribing low-fat diets: useless for long-term weight loss? Lancet Diabetes Endocrinol. 3, 920–921 (2015)
W.S. Yancy Jr, E.C. Westman, J.R. McDuffie et al., A randomized trial of a low-carbohydrate diet vs orlistat plus a low-fat diet for weight loss. Arch. Intern. Med. 170, 136–145 (2010)
J.S. Volek, M.J. Sharman, C.E. Forsythe, Modification of lipoproteins by very low-carbohydrate diets. J. Nutr. 135, 1339–1342 (2005)
R. Micha, J.L. Peñalvo, F. Cudhea, F. Imamura, C.D. Rehm, D. Mozaffarian, Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA 317, 912–924 (2017)
American Diabetes Association, 4. Lifestyle management: standards of medical care in diabetes—2018. Diabetes Care 41(Supplement 1), S38–S50 (2018)
J. MacLeod, M.J. Franz, D. Handu et al., Academy of Nutrition and Dietetics Nutrition practice guideline for type 1 and type 2 diabetes in adults: nutrition intervention evidence reviews and recommendations. J. Acad. Nutr. Diet. 117, 1637–1658 (2017)
L. Schwingshackl, C. Schwedhelm, G. Hoffmann et al., Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 105, 1462–1473 (2017)
K. Esposito, M.I. Maiorino, M. Ciotola et al., Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann. Intern. Med. 151, 306–314 (2009)
K. Esposito, M.I. Maiorino, M. Petrizzo, G. Bellastella, D. Giugliano, The effects of Mediterranean diet on need for diabetes drugs and remission of newly diagnosed type 2 diabetes: follow up of a randomized trial. Diabetes Care 37, 1824–1830 (2014)
E.M. Cespedes, F.B. Hu, L. Tinker et al., Multiple healthful dietary patterns and type 2 diabetes in the Women’s Health Initiative. Am. J. Epidemiol. 183, 622–633 (2016)
S.H. Ley, O. Hamdy, V. Mohan, F.B. Hu, Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 383, 1999–2007 (2014)
S. Rinaldi, E.E. Campbell, J. Fournier, C. O’Connor, J. Madill, A comprehensive review of the literature supporting recommendations from the Canadian Diabetes Association for the use of a plant-based diet for management of type 2 diabetes. Can. J. Diabetes 40, 471–477 (2016)
R. Pawlak, Vegetarian diets in the prevention and management of diabetes and its complications. Diabetes Spectr. 30, 82–88 (2017)
K. Esposito, M.I. Maiorino, G. Bellastella, D.B. Panagiotakos, D. Giugliano, Mediterranean diet for type 2 diabetes: cardiometabolic benefits. Endocrine 56, 27–32 (2017)
K. Esposito, C. Di Palo, M.I. Maiorino, et al., Long-term effect of mediterranean-style diet and calorie restriction on biomarkers of longevity and oxidative stress in overweight men. Cardiol. Res. Pract. 2011, 293916 (2010).
J.D. Smith, T. Hou, D.S. Ludwig, et al., Changes in intake of protein foods, carbohydrate amount and quality, and long-term weight change: results from 3 prospective cohorts. Am. J. Clin. Nutr. 101, 1216–1224 (2015).
M.I. Maiorino, G. Bellastella, M. Petrizzo, L. Scappaticcio, D. Giugliano, K. Esposito, Mediterranean diet cools down the inflammatory milieu in type 2 diabetes: the MÉDITA randomized controlled trial. Endocrine 54, 634–641 (2016)
M.I. Maiorino, G. Bellastella, M. Petrizzo et al., Effect of a Mediterranean diet on endothelial progenitor cells and carotid intima-media thickness in type 2 diabetes: follow-up of a randomized trial. Eur. J. Prev. Cardiol. 24, 399–408 (2017)
Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. 2015. http://www.health.gov/dietaryguidelines/2015-scientific-report/. Accessed 25 Jan 2018
D. Mozaffarian, Dietary and policy priorities for cardiovascular disease, diabetes, and obesity. A comprehensive review. Circulation 133, 187–225 (2016)
C. Gazzaruso, M. Fodaro, A. Coppola, Structured therapeutic education in diabetes: is it time to re-write the chapter on the prevention of diabetic complications? Endocrine 53, 347–349 (2016)
Funding
This study was supported in part by Associazione Salute con Stile.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
These authors contributed equally: Dario Giugliano, Maria Ida Maiorino, Giuseppe Bellastella and Katherine Esposito.
Rights and permissions
About this article
Cite this article
Giugliano, D., Maiorino, M.I., Bellastella, G. et al. More sugar? No, thank you! The elusive nature of low carbohydrate diets. Endocrine 61, 383–387 (2018). https://doi.org/10.1007/s12020-018-1580-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1580-x