Abstract
Purpose
The appropriate cosyntropin dose during cosyntropin stimulation tests remains uncertain. We conducted a prospective, randomized pilot study to compare 1 μg IV low dose cosyntropin test, 25 μg IM medium dose cosyntropin test, and 250 μg IM standard dose cosyntropin test to evaluate secondary adrenal insufficiency. Insulin tolerance test was used as the gold standard.
Method
The study included patients with hypothalamic/pituitary disease (n = 10) with at least one pituitary axis deficiency other than ACTH deficiency and controls (n = 12). All tests were done in random order. Sensitivity and specificity were calculated for total cortisol and serum free cortisol cut-off levels during cosyntropin stimulation tests.
Results
The median (range) age and F/M sex ratios for patients and controls were 54 years (23–62), 2/8, and 33 years (21–51), 6/6, respectively. The best total cortisol cut-off during low dose cosyntropin test, medium dose cosyntropin test, 30 min and 60 min standard dose cosyntropin test were 14.6 μg/dL (100% sensitivity & specificity), 18.7 μg/dL (100% sensitivity, 88% specificity), 16.1 (100% sensitivity & specificity), and 19.5 μg/dL (100% sensitivity & specificity), respectively. There was no difference in the ROC curve for cortisol values between the cosyntropin stimulation tests (p > 0.41). Using a cortisol cut-off of 18 μg/dL during cosyntropin stimulation tests, only cortisol level at 30 min during standard dose cosyntropin test provided discrimination similar to insulin tolerance test. The best peak free cortisol cut-off levels were 1 μg/dL for insulin tolerance test, 0.9 μg/dL for low dose cosyntropin test, 0.9 μg/dL for medium dose cosyntropin test, and 0.9 μg/dL and 1.3 μg/dL for 30 min and 60 min standard dose cosyntropin test, respectively.
Conclusion
All cosyntropin stimulation tests had excellent correlations with insulin tolerance test, when appropriate cut-offs were used. This pilot study does not suggest an advantage in using 25 μg cosyntropin dose during the cosyntropin stimulation test. A serum free cortisol cut-off of 0.9 μg/dL may be used as pass criterion during low dose cosyntropin test, standard dose cosyntropin test cosyntropin test, and 30 min standard dose cosyntropin test.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The optimal test to diagnose secondary adrenal insufficiency (AI) remains a matter of debate [1, 2]. Both, the low dose (1 µg) and the standard dose (250 µg) cosyntropin tests have been used for evaluation of adrenal function, and have their own proponents and critics, although several studies show similar diagnostic performance [1, 3, 4]. Oelkers et al reported a subcutaneous cosyntropin dose of 20–30 µg producing near maximum concentrations of cortisol over 1 h and Adrenocorticotropic hormone (ACTH) levels in the 200–350 pg/ml range [5]. This range of ACTH closely resembles levels achieved during the Insulin Tolerance Test (ITT) and Metyrapone tests [6, 7]. Accordingly, we had been using 25 µg cosyntropin dose IM for Cosyntropin Stimulation Tests (CST) in most patients in our Neuroendocrine clinic since 2004.
There have been many studies exploring the value of serum total cortisol during CSTs, however there are only a handful studies looking at the value of serum free cortisol measurement in an outpatient setting to assess secondary AI [8, 9].
We conducted a randomized, prospective pilot trial comparing the serum total and free cortisol responses of three different cosyntropin doses; 1 μg IV low dose cosyntropin test (LDCT), 25 μg IM medium dose cosyntropin test (MDCT), and 250 μg IM standard dose cosyntropin test (SDCT) to evaluate secondary AI. We used the results of ITT as our laboratory gold standard and assessed the total and free cortisol cut-off values during the CSTs and ITT. Since some studies suggest that the same cortisol cut-off cannot be used at 30 min and 60 min time points during the SDCT [10,11,12], we investigated the cut-offs at both time points separately for the SDCT.
Materials and methods
Patients and controls
The study had two groups of patients 18 to 65 years of age. The first group (n = 10) included patients with hypothalamic/pituitary disease with at least one pituitary axis deficiency other than ACTH deficiency (see electronic supplementary material for diagnoses and exclusion criteria). The second group (n = 12) comprised healthy volunteers. The three CSTs and ITT were done in random order. A minimum and maximum time interval of 48 h and 3 months were allowed in the study protocol to accommodate participants’ schedule.
Cortisol levels were measured at 30 and 60 min during CSTs. A peak cortisol cut-off of 18 μg/dL was used as the pass criterion during ITT. The result of total cortisol levels during ITT were used to determine free cortisol cut-offs during CSTs and ITT. None of the patients had pituitary surgery within 6 weeks prior to enrollment and none of the women were on estrogen. Patients had to be on at least 3 months of stable hormone replacement for hormone deficiencies. All controls had normal TSH, free T4 and prolactin levels. All premenopausal women in the control group had a history of regular, age appropriate menses and none took birth control pills within 3 months of study entry. Postmenopausal subjects had appropriately elevated FSH concentration. All men in the control group had normal FSH and total testosterone levels.
Study procedures
All participants were instructed to fast for 12 h prior to testing. Six patients were on glucocorticoid replacement and were instructed to hold their medication for 24 h prior to their testing. All the tests were conducted at the Clinical Research Unit on site at the Cleveland Clinic. The study was approved by the Cleveland Clinic Institutional Review Board. All subjects signed an informed consent.
Cosyntropin Stimulation Tests and ITT : see electronic supplementary material for procedure details.
Assays
The total and free cortisol were analyzed at Quest Diagnostics Nichols Institute, San Juan Capistrano, CA 92675, USA. Both serum free and total cortisol levels were measured using an isotope dilution mass spectrophotometric method. Briefly, total cortisol and serum free cortisol (from dialysate after separation by equilibrium dialysis) were directly measured using a two-dimensional separation system, including on-line extraction by high turbulence liquid chromatography followed by analytical liquid chromatography separation and detection by a tandem mass spectrometer. The limit of quantitation (LOQ) for the serum free cortisol was 0.03 µg/dL; intra-assay variation (CV) was 7.4 and 9.3 % at serum free cortisol of 0.36 and 2.20 µg/dL, respectively; inter-assay CV was 9.4 and 9.8% at serum free cortisol of 0.36 and 2.17 µg/dL, respectively. For total cortisol the LOQ was 0.1 µg/dL; intra-assay CV was 3.0 and 4.6% at total cortisol of 15.9 and 202.7 µg/dL, respectively; inter-assay CV was 7.9 and 6.6% at total cortisol of 15.2 and 189.9 µg/dL, respectively. Of 21 common steroid compounds tested for interference, at 200 µg/dL, only 20 alpha-dihydroxycortisol and 20 beta-hydroxycortisone were detected at 1.4 and 1.4%, respectively.
Statistical analysis
Patient groups were compared on categorical factors using Pearson χ 2 tests and Fisher exact tests. Continuous measures were evaluated using Wilcoxon rank sum tests. Sensitivity (SE) and specificity (SP) for each of the CSTs were estimated using optimal cut-offs from ROC curves, with respect to ITT as the gold standard. Youden’s Index, which identifies the largest combination of SE and SP for each test was used to identify the optimal cut-off for each test. Tests were compared on SE and SP using McNemar’s test. Pearson’s correlation coefficient was used to measure the strength of association of peak cortisol levels among pairs of testing methods. Ninety-five percent confidence intervals were produced for all the correlation, SE, and SP estimates. Comparisons of the correlations were performed using the methods by Meng, Rosenthal, and Rubin (1992) to compare the correlations and calculate 95% confidence intervals for the difference among the tests [13]. Lower bounds of these intervals above a zero value was considered statistically significant evidence that the 25-µg test is a better test, while lower bounds at least as high as −0.15 was used to determine non-inferiority at those respective margins. Analyses were performed using R software (version 3.1; Vienna, Austria) and SAS software (version .3; Cary, NC).
Results
The median (range) age for patients and volunteers was 54 (23–62) and 33 (21–51), respectively (p = 0.021). The F/M sex ratio for patients and volunteers were 2/8 and 6/6, respectively (p = 0.20). The time interval between two consecutive tests was 10 days (2–48 days). While, one participant had 64 day interval between the first and last test, 80% of patient group and 84% of control group had all four tests completed within 30 days.
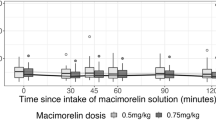
The peak total cortisol levels during ITT in patients and controls were 16.6 μg/dL (1.1–26.1) and 23.2 μg/dL (20.2–25.9), respectively. The peak total cortisol levels for patients and controls during the CSTs were as following: LDCT 14.5 μg/dL (2.2–28.4) and 23.4 μg/dL (16.7–31.9); MDCT 17.4 μg/dL (2.0–24.9) and 22.0 μg/dL (16.4–28.6); 30 min SDCT 16.1 μg/dL(1.8–25.8) and 22.3 μg/dL (18.8–27.8); 60 min SDCT 19.1 μg/dL (2.4–29.4) and 25.0 μg/dL (21.9–31.5), respectively (Fig. 1).
Boxplots show the relationships, by test, between patient groups on total cortisol. The thick line in the middle of the boxes reflects the median, while the box edges are the quartiles (interquartile range). Whiskers extend to the smallest and largest values within 1.5 times the interquartile range above the third quartile and below the first quartile
The best total cortisol cut-offs for diagnosis of secondary AI were 14.6 μg/dL (100% SE & SP) for LDCT, 18.7 μg/dL (100% SE, 88% SP) for MDCT, 16.1 μg/dL (100% SE & SP) for 30 min SDCT and 19.5 μg/dL (100% SE & SP) for 60 min SDCT. There was no difference in the ROC curve for cortisol values between the CSTs (p > 0.41). Using a cortisol cut-off of 18 μg/dL as the pass criteria during CSTs, only the cortisol level at 30 min during SDCT provided discrimination similar to ITT.
All subjects had peak total cortisol at 60 min during the SDCT. During MDCT and LDCT, 81% and 50% of subjects had peak cortisol at 30 min, respectively. Pearson correlations for peak cortisol levels between the ITT and the CSTs is shown in Fig 1 in electronic supplementary material. Peak cortisol level during SDCT correlated better with ITT compared to MDCT (p = 0.044). Among CSTs, LDCT had the lowest correlation with ITT, and was significantly lower than the SDCT (p = 0.005), but not the MDCT (p = 0.32).
The peak free cortisol levels during ITT in patients and controls were 0.95 μg/dL (0.06–2.2) and 1.9 μg/dL (1.2–2.7), respectively. The peak free cortisol levels for patients and controls during CSTs were as following: LDCT 0.77 μg/dL (0.07–2.2) and 1.9 μg/dL (1.0–3.7); MDCT 0.91 μg/dL (0.05–1.7) and 1.8 μg/dL (0.74–3.0); 30 min SDCT 0.89 μg/dL (0.06–2.2) and 1.8 μg/dL (1.1–3.1); 60 min SDCT 1.3 μg/dL (0.06–2.6) and 2.3 μg/dL (1.7–3.8), respectively (Fig. 2).
Boxplots show the relationships, by test, between patient groups on free cortisol. The thick line in the middle of the boxes shows the median, while the box edges are the quartiles (interquartile range). Whiskers extend to the smallest and largest values within 1.5 times the interquartile range above the third quartile and below the first quartile. Responses outside these ranges are plotted as individual circles and represent potential outliers
The best peak free cortisol cut-offs were 1 μg/dL for ITT, 0.9 μg/dL for LDCT (100%SE and 100%SP), 0.9 μg/dL for MDCT (100%SE and 94%SP), and 0.9 μg/dL (100%SE and 100%SP) and 1.3 μg/dL (100%SE and 100%SP) for 30 min and 60 min SDCT, respectively. Pearson correlations for peak free cortisol levels between the ITT and the CSTs is shown in Fig 2 in electronic supplementary material. There was no difference in the area under the ROC curve for free cortisol values between the CSTs (p = 0.36).
Discussion
We compared total and free cortisol levels during CSTs using three different doses of cosyntropin with ITT as the gold standard test in a randomized, prospective pilot trial. All CSTs performed well compared to ITT as long as appropriate cut-offs were used. Specifically, we did not find any advantage for using 25 μg cosyntropin dose compared to 1 and 250 μg doses.
Over the years, several different tests have been proposed to evaluate patients for secondary AI. The dilemma for an ideal test has been discussed in detail by Grossman in a review article [14]. The CST is used routinely to assess secondary AI, compared to ITT, since it is safe and relatively convenient. We found here, in patients with established hypothalamic pituitary pathology, CSTs correlated well with the ITT.
250 μg CST (SDCT)
One critique of the SDCT is that 250 µg of cosyntropin produces supraphysiologic ACTH levels in the 1000–60,000 pg/ml range [6, 15]. The concern is that adrenal cortex is maximally stimulated leading to false negative results in partial AI [16,17,18,19,20,21]. Case reports have been published with patients having AI based on clinical symptoms and abnormal ITT, who responded normally to the 250 µg dose [22, 23].
There is significant variability in the reported cut-off levels of serum cortisol during SDCT ranging from 18.1 µg /dL to 22.4 µg /dL [2, 3, 11, 24]. The limitations of the traditional cut-offs of SDCT in pregnant women have been discussed by Yuen et al. and higher cut-offs are recommended for that population [25]. Almost always, patients achieve higher cortisol levels at 60 min and therefore there is little evidence for the use of the same cortisol cut- off for both 30 and 60 min time points. In our study, both time points provided excellent diagnostic accuracy as long as appropriate cortisol cut-offs were used. In addition, a cortisol level of 18 μg /dL at 30 min during SDCT provided discrimination similar to the ITT. Accordingly, one may argue that 30 min cortisol value may be adequate during the SDCT. This is similar to the findings in the series of 200 patients which suggested to use the 30 min time point during the SDCT [10].
1 μg CST (LDCT)
The proponents of the 1 µg cosyntropin dose reported higher sensitivity in patients on chronic glucocorticoid treatment [16]. This has been supported by other investigators [1, 24, 26,27,28,29]. However, some studies have reported lower specificity with the 1 µg cosyntropin dose [30,31,32]. Fleseriu et al found abnormal cortisol levels in 23 out of 26 patients during the LDCT who had passed the SDCT. These patients were asymptomatic, without any glucocorticoid coverage, during a follow-up period that lasted as long as 2 years [33]. In addition, there is a concern for the reproducibility of 1 µg dose at different times of the day. Nieman et al reported 20 and 63% false positive results with LDCT in healthy volunteers who underwent the test at 0800 h or 1600 h, respectively [34].
Furthermore, the 1 µg cosyntropin is not available as a commercial preparation. It is prepared by diluting 250 µg vials, with the potential for dosing errors. Lower doses of cosyntropin stored in glass tubes have been shown to be unstable; and therefore, plastic tubes are recommended [16]. However, longer plastic tubing has also been reported as a factor for the lower specificity of LDCT due to loss of ACTH in the walls of the tubing [34].
Similar to SDCT, LDCT has been reported with wide variations in cut-off, ranging from 17 to 22 µg/dL (470–600 nmol/l) [2, 24, 32]. In the current study, LDCT provided 100% sensitivity and specificity as long as a lower cortisol cut-off of 14.6 µg /dL was used as the pass criterion, which suggests that the higher false positive results in some studies may be related to the use of a cortisol cut- off of 18 µg /dL, which is generally used as the pass criteria for the LDCT [32].
Other doses of cosyntropin used for CST
More than 50 years ago, Landon et al. reported that a much lower dose of cosyntropin can produce maximal adrenal stimulation [35]. There have been dose-response studies highlighting that lower doses of synthetic ACTH produce peak cortisol levels similar to the 250 µg dose [5, 16, 36, 37]. Contreras et al. reported that mean serum cortisol concentrations 30 min after 25 µg and 250 µg ACTH IM were not different (p = 0.158) [38]. Similarly, Oelkers et al. showed that near maximum cortisol concentration is achieved following 20 to 30 µg (subcutaneous) cosyntropin administration [5]. Accordingly, we designed this pilot study to investigate whether the use of 25 µg cosyntropin dose would provide any advantage over 1 and 250 µg doses. We found that the peak cortisol level during SDCT correlated better with ITT compared to MDCT (p = 0.044). In summary, the MDCT did not provide an advantage over LDCT and SDCT.
Free cortisol during CST and ITT
There is a sound pathophysiological basis for measurement of serum free cortisol rather than total cortisol level in patients with low binding proteins such as advanced liver disease, nephrotic syndrome or critically ill patients, or in states associated with elevated binding proteins such as pregnancy and in women taking estrogen [9, 39]. However, due to limited number of studies a widely accepted cut-off for free cortisol during CSTs or ITT, in an outpatient setting has not been established.
In a cross-sectional study of 295 outpatients, a free cortisol of 0.9 and 1.2 µg/dL at 30 and 60 min during SDCT was suggested as the pass criteria for the diagnosis of AI [8]. In another study of 60 healthy volunteers and 21 patients with pituitary disease, free cortisol levels of 1.1 µg/dL, 1.2 and 1.5 µg/dL were suggested as the pass criteria during LDCT, and at 30 and 60 min time points during SDCT, respectively [9]. Our study found similar free cortisol cut-off values of 0.9 µg/dL for LDCT and 30 min time point during SDCT, and 1.3 µg/dL for 60 min time point during SDCT. The lack of wide availability and long turnaround time are limitations for free cortisol in clinical practice.
There may be clinically significant differences in cortisol cut-offs when different assays are used. Serum cortisol values in this study were measured using a LCMS assay. In one study the total cortisol levels were 12% lower when measured by immunoassay compared to LCMS [9]. One may expect similar differences in free cortisol assays measured by LCMS.
This is the first, prospective, randomized study to compare MDCT to SDCT, LDCT, and ITT. However, our study has limitations. The number of participants is small, which limits understanding of potential relationships between total and free cortisol levels and other factors, such as age or sex. We excluded patients who may benefit the most from measurement of free cortisol levels such as those with liver disease, nephrotic syndrome, or women on estrogen or those who were pregnant, so as to establish baseline values in patients with pituitary disease and in normal controls. Larger studies are needed to establish the suggested cut-off levels for serum free cortisol.
Conclusion
The current pilot study does not support an advantage of the use of 25 mcg cosyntropin during CST. All three dose-schedules of the CSTs performed well and had excellent correlation with ITT as long as appropriate cut-offs were used. A free cortisol cut-off of 0.9 μg/dL may be used as the pass criteria during the LDCT, MDCT, and at 30 min time point during SDCT. A higher free cortisol cut-off of 1.3 μg/dL is required for 60 min time point during SDCT.
References
N. Weintrob, E. Sprecher, Z. Josefsberg, C. Weininger, Y. Aurbach-Klipper, D. Lazard, M. Karp, A. Pertzelan, Standard and low-dose short adrenocorticotropin test compared with insulin-induced hypoglycemia for assessment of the hypothalamic-pituitary-adrenal axis in children with idiopathic multiple pituitary hormone deficiencies. J. Clin. Endocrinol. Metab. 83, 88–92 (1998)
T.A. Abdu, T.A. Elhadd, R. Neary, R.N. Clayton, Comparison of the low dose short synacthen test (1 microg), the conventional dose short synacthen test (250 microg), and the insulin tolerance test for assessment of the hypothalamo-pituitary-adrenal axis in patients with pituitary disease. J. Clin. Endocrinol. Metab. 84, 838–843 (1999)
J. Mayenknecht, S. Diederich, V. Bahr, U. Plockinger, W. Oelkers, Comparison of low and high dose corticotropin stimulation tests in patients with pituitary disease. J. Clin. Endocrinol. Metab. 83, 1558–1562 (1998)
I.E. Widmer, J.J. Puder, C. Konig, H. Pargger, H.R. Zerkowski, J. Girard, B. Muller, Cortisol response in relation to the severity of stress and illness. J. Clin. Endocrinol. Metab. 90, 4579–4586 (2005)
W. Oelkers, T. Boelke, V. Bahr, Dose-response relationships between plasma adrenocorticotropin (ACTH), cortisol, aldosterone, and 18-hydroxycorticosterone after injection of ACTH-(1-39) or human corticotropin-releasing hormone in man. J. Clin. Endocrinol. Metab. 66, 181–186 (1988)
P. Darmon, F. Dadoun, C. Frachebois, J.G. Velut, S. Boullu, A. Dutour, C. Oliver, M. Grino, On the meaning of low-dose ACTH(1-24) tests to assess functionality of the hypothalamic-pituitary-adrenal axis. Eur. J. Endocrinol. 140, 51–55 (1999)
J.J. Staub, B. Noelpp, J. Girard, J.B. Baumann, S. Graf, J.G. Ratcliffe, The short metyrapone test: comparison of the plasma ACTH response to metyrapone and insulin-induced hypoglycaemia. Clin. Endocrinol. 10, 595–601 (1979)
I. Bancos, D. Erickson, S. Bryant, J. Hines, T.B. Nippoldt, N. Natt, R. Singh, Performance of free versus total cortisol following cosyntropin stimulation testing in an outpatient setting. Endocr. Pract. 21, 1353–1363 (2015)
M.G. Burt, B.L. Mangelsdorf, A. Rogers, J.T. Ho, J.G. Lewis, W.J. Inder, M.P. Doogue, Free and total plasma cortisol measured by immunoassay and mass spectrometry following ACTH(1)(-)(2)(4) stimulation in the assessment of pituitary patients. J. Clin. Endocrinol. Metab. 98, 1883–1890 (2013)
J. Lindholm, H. Kehlet, Re-evaluation of the clinical value of the 30 min ACTH test in assessing the hypothalamic-pituitary-adrenocortical function. Clin. Endocrinol. 26, 53–59 (1987)
S.J. Hurel, C.J. Thompson, M.J. Watson, M.M. Harris, P.H. Baylis, P. Kendall-Taylor, The short Synacthen and insulin stress tests in the assessment of the hypothalamic-pituitary-adrenal axis. Clin. Endocrinol. 44, 141–146 (1996)
F. Kelestimur, A. Akgun, O. Gunay, A comparison between short synacthen test and depot synacthen test in the evaluation of cortisol reserve of adrenal gland in normal subjects. J. Endocrinol. Invest. 18, 823–826 (1995)
X. Meng, R. Rosenthal, D. Rubin, Comparing correlated correlation coefficients. Psychol. Bull. 111, 172–175 (1992)
A. Grossman, Assessment of the HPA axis: another new test? Endocrine 40, 268–269 (2015)
G.M.D. Dickstein, E.M.D. Arad, C.M.D. Shechner, Low-dose ACTH stimulation test. Endocrinologist. 7, 285–293 (1997)
G. Dickstein, C. Shechner, W.E. Nicholson, I. Rosner, Z. Shen-Orr, F. Adawi, M. Lahav, Adrenocorticotropin stimulation test: effects of basal cortisol level, time of day, and suggested new sensitive low dose test. J. Clin. Endocrinol. Metab. 72, 773–778 (1991)
D.H. Streeten, G.H. Anderson Jr, M.M. Bonaventura, The potential for serious consequences from misinterpreting normal responses to the rapid adrenocorticotropin test. J. Clin. Endocrinol. Metab. 81, 285–290 (1996)
E. Reschini, A. Catania, G. Giustina, Plasma cortisol response to ACTH does not accurately indicate the state of hypothalamic-pituitary-adrenal axis. J. Endocrinol. Invest. 5, 259–261 (1982)
S.G. Soule, M. Fahie-Wilson, S. Tomlinson, Failure of the short ACTH test to unequivocally diagnose long-standing symptomatic secondary hypoadrenalism. Clin. Endocrinol. 44, 137–140 (1996)
S.K. Cunningham, A. Moore, T.J. McKenna, Normal cortisol response to corticotropin in patients with secondary adrenal failure. Arch. Intern. Med. 143, 2276–2279 (1983)
M. Schmiegelow, U. Feldt-Rasmussen, A.K. Rasmussen, M. Lange, H.S. Poulsen, J. Muller, Assessment of the hypothalamo-pituitary-adrenal axis in patients treated with radiotherapy and chemotherapy for childhood brain tumor. J. Clin. Endocrinol. Metab. 88, 3149–3154 (2003)
G.C. Borst, H.J. Michenfelder, J.T. O’Brian, Discordant cortisol response to exogenous ACTH and insulin-induced hypoglycemia in patients with pituitary disease. N. Engl. J. Med. 306, 1462–1464 (1982)
J. Landon, F.C. Greenwood, T.C. Stamp, V. Wynn, The plasma sugar, free fatty acid, cortisol, and growth hormone response to insulin, and the comparison of this procedure with other tests of pituitary and adrenal function. II. In patients with hypothalamic or pituitary dysfunction or anorexia nervosa. J. Clin. Invest. 45, 437–449 (1966)
K. Tordjman, A. Jaffe, Y. Trostanetsky, Y. Greenman, R. Limor, N. Stern, Low-dose (1 [mu]g) adrenocorticotrophin (ACTH) stimulation as a screening test for impaired hypothalamo-pituitary-adrenal axis function: sensitivity, specificity and accuracy in comparison with the high-dose (250 [mu]g) test. Clin. Endocrinol. 52, 633–640 (2000)
K.C. Yuen, L.E. Chong, C.A. Koch, Adrenal insufficiency in pregnancy: challenging issues in diagnosis and management. Endocrine 44, 283–292 (2013)
S. Rasmuson, T. Olsson, E. Hagg, A low dose ACTH test to assess the function of the hypothalamic-pituitary-adrenal axis. Clin. Endocrinol. 44, 151–156 (1996)
B. Ambrosi, L. Barbetta, T. Re, E. Passini, G. Faglia, The one microgram adrenocorticotropin test in the assessment of hypothalamic-pituitary-adrenal function. Eur. J. Endocrinol. 139, 575–579 (1998)
L.M. Thaler, L.S. Blevins, Jr: The low dose (1-microg) adrenocorticotropin stimulation test in the evaluation of patients with suspected central adrenal insufficiency. J. Clin. Endocrinol. Metab. 83, 2726–2729 (1998)
M. Magnotti, M. Shimshi, Diagnosing adrenal insufficiency: which test is best--the 1-microg or the 250-microg cosyntropin stimulation test? Endocr. Pract. 14, 233–238 (2008)
M. Maghnie, E. Uga, F. Temporini, N. Di Iorgi, A. Secco, C. Tinelli, A. Papalia, M.R. Casini, S. Loche, Evaluation of adrenal function in patients with growth hormone deficiency and hypothalamic-pituitary disorders: comparison between insulin-induced hypoglycemia, low-dose ACTH, standard ACTH and CRH stimulation tests. Eur. J. Endocrinol. 152, 735–741 (2005)
S. Soule, C. van Zyl Smit, G. Parolis, S. Attenborough, D. Peter, S. Kinvig, T. Kinvig, E. Coetzer, The low dose ACTH stimulation test is less sensitive than the overnight metyrapone test for the diagnosis of secondary hypoadrenalism. Clin. Endocrinol. 53, 221–227 (2000)
A.M. Suliman, T.P. Smith, M. Labib, T.M. Fiad, T.J. McKenna, The low-dose ACTH test does not provide a useful assessment of the hypothalamic–pituitary–adrenal axis in secondary adrenal insufficiency. Clin. Endocrinol. (Oxf). 56, 533–539 (2002)
M. Fleseriu, M. Gassner, C. Yedinak, L. Chicea, J.B. Delashaw Jr, D.L. Loriaux, Normal hypothalamic-pituitary-adrenal axis by high-dose cosyntropin testing in patients with abnormal response to low-dose cosyntropin stimulation: a retrospective review. Endocr. Pract. 16, 64–70 (2010)
M. Wade, S. Baid, K. Calis, H. Raff, N. Sinaii, L. Nieman, Technical details influence the diagnostic accuracy of the 1 microg ACTH stimulation test. Eur. J. Endocrinol. 162, 109–113 (2010)
J. LANDON, V.H. JAMES, R.J. CRYER, V. WYNN, A.W. FRANKLAND, Adrenocorticotropic effects of a synthetic polypeptide--beta 1-24-corticotropin--in man. J. Clin. Endocrinol. Metab. 24, 1206–1213 (1964)
M.L. Graybeal, V.S. Fang, Physiological dosing of exogenous ACTH. Acta Endocrinol. 108, 401–406 (1985)
S. Crowley, P.C. Hindmarsh, P. Holownia, J.W. Honour, C.G. Brook, The use of low doses of ACTH in the investigation of adrenal function in man. J. Endocrinol. 130, 475–479 (1991)
L.N. Contreras, A.L. Arregger, G.G. Persi, N.S. Gonzalez, E.M. Cardoso, A new less-invasive and more informative low-dose ACTH test: salivary steroids in response to intramuscular corticotrophin. Clin. Endocrinol. 61, 675–682 (2004)
A.H. Hamrahian, T.S. Oseni, B.M. Arafah, Measurements of serum free cortisol in critically ill patients. N. Engl. J. Med. 350, 1629–1638 (2004)
Acknowledgements
We want to thank Linda Heil and Robert McCoy who served as research coordinators and the nursing staff at Clinical Research Unit at Cleveland Clinic for their help with performing the Insulin Tolerance Tests and Cosyntropin Stimulation Tests.
Funding
This study was partly funded by a grant from Endocrine Fellows Foundation awarded to Dr Seenia Peechakara and by the Research Program Committee at Cleveland Clinic Foundation awarded to Dr Amir Hamrahian. Quest Diagnostics Inc analyzed the samples for free.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S.P., R.J.W., A.H.H., J.B., L.K., and P.R. report no conflicts of interests and have nothing to disclose. N.J.C., R.E.R., and M.J.M. are employees of Quest Diagnostics Inc and report no conflicts of interest. They were not involved in the trial design, data collection, and interpretation.
Ethical approval
All procedures performed in this study with human participants were in accordance with the ethical standards of the Cleveland Clinic institutional review board and with the 1964 Helsinki declaration and its later amendments. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Peechakara, S., Bena, J., Clarke, N.J. et al. Total and free cortisol levels during 1 μg, 25 μg, and 250 μg cosyntropin stimulation tests compared to insulin tolerance test: results of a randomized, prospective, pilot study. Endocrine 57, 388–393 (2017). https://doi.org/10.1007/s12020-017-1371-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1371-9