Abstract
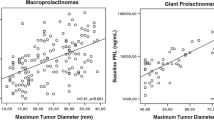
Giant prolactinomas are rare tumors characterized by their large size, compressive symptoms, and extremely high prolactin secretion. The aim of this study is to describe our experience with a series of 16 giant prolactinomas cases in terms of clinical presentation, therapeutic decisions, and final outcomes. Retrospective analysis of adult patients diagnosed with giant prolactinomas at the endocrine departments of three university tertiary hospitals. We included 16 patients (43.7 % women); mean age at diagnosis: 42.1 ± 21 years. The most frequent presentation was compressive symptoms. The delay in diagnosis was higher in women (median of 150 months vs. 12 in men; p = 0.09). The mean maximum tumor diameter at diagnosis was 56.9 ± 15.5 mm, and mean prolactin levels were 10,995.9 ± 12,157.8 ng/mL. Dopamine agonists were the first-line treatment in 11 patients (mean maximum dose: 3.9 ± 3.2 mg/week). Surgery was the initial treatment in five patients and the second-line treatment in six. Radiotherapy was used in four cases. All patients but one, are still with dopamine agonists. After a mean follow-up of 9 years, prolactin normalized in 7/16 patients (43.7 %) and 13 patients (81 %) reached prolactin levels lower than twice the upper limit of normal. Mean prolactin level at last visit: 79.5 ± 143 ng/mL. Tumor volume was decreased by 93.8 ± 11.3 %, and final maximum tumor diameter was 18.4 ± 18.8 mm. Three patients are actually tumor free. Giant prolactinomas are characterized by a large tumor volume and extreme prolactin hypersecretion. Multimodal treatment is frequently required to obtain biochemical and tumor control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Giant prolactinomas (GP) are low-prevalence pituitary adenomas representing 0.5–4.4 % of all pituitary tumors, more commonly affecting men. GPs are defined by their size, which is larger than 40 mm; their extrasellar invasiveness; their frequent symptoms derived from local mass effect; and an extremely high prolactin (PRL) concentration (usually >1000 ng/mL) without growth hormone (GH) or adrenocorticotropic hormone (ACTH) co-secretion. A variable degree of hypopituitarism is usually present [1–3]. Dopamine agonists (DA), especially cabergoline (CAB), are the first-line treatment for these tumors, decreasing PRL concentration and tumor size, even after a few days of treatment [1, 4]. However, the optimum treatment regimen for patients with GP is not well defined, and this represents a challenge for clinicians. The large tumor and the extreme hyperprolactinemia may require combined or sequential treatments, using CAB together with decompressive surgery, RT or even temozolomide, to improve compressive symptoms and to achieve hormonal control [2, 5–7]. The aim of this report is to describe our experience with a series of 16 GP cases followed up to 9 years after diagnosis, with special attention to clinical presentation, therapeutic decisions, and final outcomes.
Materials and methods
Patients
We performed a retrospective analysis of all adult patients diagnosed with GP with regular follow-up (with at least one medical visit during the last 2 years) at the endocrine departments of three university tertiary hospitals in Spain. An ethics committee approved the study and an informed consent was obtained from all patients before inclusion. All diagnostic and therapeutic procedures were performed as a part of the normal clinical care. Inclusion criteria were (1) pituitary macroadenoma larger than 4 cm in diameter, (2) PRL level higher than 1000 ng/mL, and (3) significant extrasellar invasion. Clinical records were reviewed for demographic and clinical characteristics, PRL levels, pituitary function, tumor size, and invasiveness at first evaluation and during follow-up. The therapeutic approach was evaluated in terms of efficacy (control of PRL hypersecretion and tumor size) and safety (adverse events, surgical complications and changes in pituitary function).
Methods
Biochemical and hormonal assays were performed, and samples were collected after an overnight fast, at baseline and at different follow-up times. The use of drugs potentially associated with hyperprolactinemia was ruled out in all patients. Serum hormone levels were measured in local laboratories using two-site immunoradiometric or chemiluminometric assays. When necessary, blood samples were obtained by the use of a venous catheter to obtain two or three blood samples at 15–20 min intervals to avoid traumatic venipuncture. Serum samples were diluted in all cases except two to allow the proper measure of PRL concentration. Pituitary, thyroid, adrenal, and gonadal functions were evaluated in all patients. GH and ACTH co-secretion were discarded. Tumor characteristics were locally evaluated with a similar pituitary-magnetic resonance imaging (MRI) protocol (with sagittal, coronal, and axial planes) at baseline and during follow-up at least once per year. An extrasellar tumor growth was considered significant in those cases with compression of the optic chiasm, frontal or temporal lobe, or with invasion of cavernous sinus, sphenoid sinus, clivus, skull base, or nasopharynx [1]. Tumor volume was calculated by the DiChiro and Nelson formula [8, 9]. Changes in tumor size larger than 30 % (diameter) or larger than 65 % (volume) were considered significant [3]. Ophthalmologic evaluation was performed in all cases.
Statistical analysis
Statistical analysis was performed using SPSS version 22. Results were expressed as mean and standard deviation in variables with normal distribution and as median and range in those with no normal distribution. Gender differences were analyzed with t Student test in variables with normal distribution and with Mann–Whitney test in those with no normal distribution. Correlation between quantitative characteristics was calculated with Spearman test. A p value <0.05 was considered significant.
Results
Patients
We included 16 patients in this study: seven women and nine men. They were followed during a mean time of 9 ± 5.3 years (22 months to 18 years) from diagnosis. The main characteristics of the whole group and treatments are described in Tables 1 and 2. Mean age at diagnosis was 42.1 ± 21 years old. There was no case of hereditary pituitary adenoma or associated endocrinopathy. An AIP mutations study was performed in case 16 with negative results. The duration of symptoms before diagnosis varied greatly, ranging from a few days to 36 years, with a median of 12 months. The delay in diagnosis was higher in women than in men (median of 150 months in women vs. 12 in men; p = 0.09) (Table 3).
The reasons for the initial medical consultation were compressive symptoms in 11 cases (mainly visual impairment), symptoms related to hyperprolactinemia and hypogonadism in two patients (amenorrhea and galactorrhea) and both types of symptoms (visual impairment and erectile dysfunction) in one patient. Despite the fact that the tumors were large, the diagnosis was incidental in two cases (Table 1). No patient presented with symptoms of GH, thyroid-stimulating hormone (TSH), or ACTH deficiency.
The mean maximum tumor diameter at diagnosis was 56.9 ± 15.5 mm, and the mean initial volume was 46.9 ± 40.6 cm3. In all cases, a pituitary tumor caused significant compression or invasion of adjacent structures (Fig. 1): cavernous sinus invasion in 14 (87.5 %), compression of optic chiasm in 12 (75 %), sphenoidal sinus invasion in 7 (43.7 %), clivus or skull base invasion in 7 (43.7 %), carotid artery encasement in 3 (18.7 %), nasopharynx invasion in 2 (12.5 %), midbrain invasion in 1 (6.2 %), and middle cerebral artery encasement in 1 (6.2 %).
MRI studies from cases 2 (a/b) and 7 (c/d): Case 2: a Extensive skull base invasion at diagnosis; b significant reduction in tumor size after 6 months of medical treatment. Case 7: c at diagnosis, with cavernous sinus, sphenoidal sinus, and clivus (skull base) invasion. d After 22 months of medical treatment and RT
Mean serum PRL concentration at diagnosis (excluding cases 13 and 14 in which serum dilution was not performed) was 10,995.9 ± 12,175.8 ng/mL (range: 1011–45,440 ng/mL). All patients had hypopituitarism at diagnosis, with follicle-stimulating hormone/Luteinizing hormone (FSH/LH) deficiency in 100 % of cases, TSH deficiency in 9 out of 16 (56 %), ACTH deficiency in 7 out of 16 (43 %), and GH deficiency in 3 of the 6 patients in which this axis was specifically assessed by means of a dynamic test. Two patients were diagnosed with GH deficiency during adolescence (Table 1). In case 11, parental heights were not available, and the patient grew 11 cm during follow-up on gonadal substitution, reaching a final height of 165 cm. In case 16, and according to mean parental height, growth was not affected.
Type of initial treatment
Dopamine agonist
DAs were the first-line treatment in 11 patients (68.7 %): ten were treated with CAB and one case was treated with bromocriptine (BMC). The mean initial CAB dose was 1.37 ± 0.88 mg/week, and the mean maximum dose was 3.9 ± 3.2 mg/week (range 1–7.5 mg/week). Patient on BMC therapy was treated initially with 7.5 mg/day to a maximum dose of 21.25 mg/day. Dose tritation was performed according to biochemical and tumor response to the maximum tolerated dose. Echocardiographic studies were performed in 11 patients without significant findings. One patient developed a pneumoencephalus secondary to CAB treatment.
Only four patients of this group did not receive further treatment on follow-up (Table 2) and only two of them achieved normal PRL concentrations. Six patients required surgical treatment as second-line therapy. Surgery was indicated for persistent visual or compressive symptoms (cases 12 and 15); pituitary apoplexy (case 13); development of a pneumoencephalus (case 6); and for partial resistance to DA (cases 5 and 14). Case 5 showed a poor tumor response to high dose CAB treatment, and surgery was indicated after the development of focal seizures secondary to tumor compression. In case 14, the biochemical response was poor (PRL baseline 2331 ng/mL to 971/861) and the tumor response was absent with a maximum tolerated CAB dose of 2.5 mg per week. A small (11 mm) supra-selar tumor persisted after surgery with severe hyperprolactinemia, which was again resistant to medical therapy requiring RT. RT was used as second-line therapy in case 7 (Fig. 1), for an unresectable tumor with partial response to medical therapy. As third-line treatment, two cases (12 and 13) required a second surgery and another two (cases 14 and 15) were irradiated for visual worsening and persistence of tumor remnants that were poorly responsive to DA.
Pituitary surgery
Decompressive pituitary surgery was the first treatment in five patients (31.25 %). Indications for surgery were severe visual deterioration in three patients (cases 10, 11, and 16), intratumoral hematoma (case 9) and patient’s preference (pregnancy desire) in case 8. All surgically first-line-treated patients showed amelioration of local symptoms but all required medical treatment for persistent disease, and in one patient (case 16), RT was necessary as third-line therapy for tumor progression on follow-up.
Treatment of hypopituitarism
FSH/LH, ACTH, and TSH deficiencies were adequately treated in all patients. Dynamic tests of GH secretion were not systematically performed in this series because, in Spain, GH replacement is not accepted for patients with hypersecreting pituitary adenoma requiring specific treatment. No patient in this series was treated with GH.
Long-term outcome of multimodal treatment
All patients of this series were treated with DA. Four patients (cases 1, 2, 3, and 4) were treated exclusively with DA. Although two of them (cases 1 and 2) showed a partial biochemical response, further treatment was considered not necessary (Table 2). Most patients required combined or multimodal therapy. Six patients (cases 5, 7, 13, 14, 15, and 16) showed an insufficient response to DA requiring additional treatment (3 required surgical procedures, and 4 required pituitary irradiation). Only in one case was the discontinuation of DA treatment possible (Table 2).
Subtotal surgery was performed 13 times in 11 patients (5 first-line treatments, 6 second-line treatments with 2 surgeries in 2 cases). The goal of surgery was to resolve compressive symptoms or to debulk the tumor to achieve a better response to DA therapy. Surgery was successful to resolve or ameliorate pituitary hematoma, apoplexy and compressive symptoms in all cases but one. In case 5, tumor resection was not possible due to the presence of a very fibrous, hard, and vascularized tumor after long-term CAB therapy. Significant debulking of pituitary adenoma in case 14 (partially resistant to CAB) was not followed by a better response to treatment. No patient was cured by surgery. Three patients who were operated on (cases 14, 15 and 16) required RT for tumor control during follow-up. There was no major or permanent surgical complication. Only one patient (case 13) presented postsurgical cerebrospinal fluid leakage requiring lumbar drainage. Pathological and immunohistochemical studies were available in 12 samples and were consistent with a monohormonal PRL tumor.
Pituitary irradiation was used in four patients (one as second-line and three as third-line treatment) for tumor control. All irradiated patients showed decreased PRL concentration, and two cases developed new pituitary deficiencies during follow-up.
PRL levels
After a mean follow-up of 9 years, PRL reached normal values (<29 ng/mL) in 7/16 patients (43.7 %) and 13 out of 16 (81 %) showed PRL levels lower than twice the upper limit of normal (ULN) (Table 2). The mean PRL level at last visit was 79.5 ± 143 ng/mL with a decrease of 98.1 ± 4 % (p < 0.05) from diagnosis. Biochemical response to treatments was not influenced by gender, type of first-line treatment or DA dose. Three out of four irradiated patients achieved a normal PRL concentration, and the remaining case reached a PRL concentration lower than 2 × ULN (Table 2). Only in one irradiated case was the discontinuation of DA treatment possible.
Tumor size
Tumor size decreased significantly in all but one patient (case 11) (Table 1). The final maximum tumor diameter was 18.4 ± 18.8 mm and final tumor volume was 4.8 ± 12.3 cm3 (1). Tumor volume after treatments decreased by 93.8 ± 11.3 %. At the last visit, 13 patients (81.2 %) had tumor remnants; three (treated with DA, surgery and two cases with RT) are tumor free. We did not find any significant difference in patients with or without tumor remnants regarding initial tumor volume (56.43 vs. 42.67 cm3, p = 0.1), baseline PRL level (10987 ± 12657 vs. 7023 ± 8752, p = 0.65) or initial treatment with surgery or DA (p = 0.75). Patients with tumor eradication received RT therapy more frequently than those with tumor persistence (66.67 vs. 15.3 %; p = 0.02). Men showed a statistically non-significant trend to a higher rate of tumor persistence than women (88.8 vs. 42.8 %) (Table 3). In no case, giant prolactinoma evolved aggressively to pituitary carcinoma.
Pituitary function and visual defects
Four patients (25 %) recovered pituitary function during follow-up: one patient recovered gonadal axis, two patients recovered corticotropic axis and one patient recovered gonadal and corticotropic axis. Five patients developed new pituitary deficiencies (2 FSH/LH, 3 ACTH, 2 TSH). Among 12 patients with chiasm compression at baseline, four patients showed a complete recovery, four improved partially and, in the last four, visual defects remained stable.
Discussion
Prolactinomas are prevalent tumors affecting women more frequently, especially as microprolactinomas [10]. The gold standard of treatment is well established [11]. CAB treatment exhibits a high efficacy rate for normalizing PRL, reversing hypogonadism and infertility and decreasing tumor size [2]. Although BMC has been employed as first-line treatment in the past [12, 13], nowadays is used for patients who are intolerant or resistant to CAB. Surgery is usually reserved for symptomatic patients who are resistant to or unable to tolerate the required dose of CAB. RT is rarely used and is restricted for aggressive or malignant prolactinoma. In contrast, GPs are a low-prevalence disease that are more frequent in men and defined by very large tumors with compressive symptoms and extreme PRL hypersecretion [10, 14–16]. The optimum treatment for these patients is not well defined. It is well known that the response to a dopamine agonist is worse in men (perhaps due to lower tumor expression of the estrogen receptor alpha [17]) and in patients with larger tumors or higher PRL concentration [11, 18].
In this study, the most frequent clinical presentation was a young or middle-age patient with compressive symptoms (visual field defects and headaches). Indeed, 7 out of 16 cases showed skull base invasion (Fig. 1) with atypical presentations (hearing loss, poor general health) and an incidental diagnosis in some cases. This presentation has been described [19], suggesting that GP should be considered in the differential diagnosis of skull base tumors.
Symptoms of hyperprolactinemia and hypopituitarism were often absent or very limited and were considered to be insignificant by the patients themselves. The percentage of women affected was slightly higher in this series than previously described (10–37.5 %) [13, 14]. Notably, women showed a relevant delay from first symptoms to diagnosis compared to men. This delay may be related to a misinterpretation of symptoms as a consequence of minor gynecological problems or menopause either by the patient or by the physician, similarly to what has recently been described in acromegaly [20]. On the other hand, we did not find differences in PRL concentration, tumor size or final outcome between males and females. Although tumor persistence was more frequent in men, this difference was not statistically significant.
Regarding therapy, GP patients frequently show a fairly good response to DA with large reductions in PRL concentration and tumor volume. Nevertheless, the large tumor burden and extreme hyperprolactinemia often prevent PRL normalization from being reached. In a previous study, baseline PRL was higher in those cases without PRL normalization or tumor persistence after treatments [6]. In a recent review, CAB achieved PRL normalization in 60 % of GP cases, significant tumor size reduction in 74 %, and improved visual field defects in 96 % [3]. In this study, only four patients were exclusively treated with DA, and only two of them reached a normal PRL concentration. Partial resistance to DA justified three second-line and four third-line treatments. Perhaps the efficacy of DA could have increased with higher DA doses; however, the mean dose used in this study was similar to previous studies [1, 14] and was higher than the dose used in non-giant prolactinoma patients [21].
First-line surgery is rarely curative for GP [3, 22, 23]. However, tumor debulking may be necessary to improve acute compressive symptoms and may be followed by better response to DA therapy [3, 24–26]. In this study, decompressive surgery was performed at any time in 11 out of 16 cases. Surgery was successful in all but one case in terms of resolution of local complications but was not followed by PRL normalization. The indication of surgical treatment for GP is variable in recent studies, ranging between 13 [21] and 50 % [24]. The more frequent use of surgery in this study may relate to some characteristics of this series such as date of diagnosis, tumor size, local symptoms, and intolerance or partial resistance to DA; it could also relate to local healthcare practices based on the availability of skilled neurosurgical teams. Surgical complications in this series were almost negligible. Additionally, four patients were treated with RT for tumor remnants with partial resistance to DA or for tumor progression after surgery and during CAB treatment.
As a result of combined treatments and after a mean follow-up of 9 ± 5.3 years, PRL concentration decreased by more than 95 %. Although PRL normalization was only reached in less than half of the patients, most cases had at final visit a PRL concentration lower than 2 × ULN with little or no clinical impact. Only in one case was the discontinuation of DA possible. Tumor size decreased by more than 90 % from the baseline, but tumor eradication was rarely achieved. Most tumor remnants were small and well tolerated. Visual defects improved or resolved in two-thirds of affected patients and pituitary function improved in four cases. The final outcome (PRL levels and tumor persistence) did not relate to gender, clinical presentation, PRL levels, tumor size or invasiveness, type of first treatment or DA dose. Only pituitary irradiation was related to a higher rate of tumor eradication. Adverse events related with treatments were rare: one case of pneumoencephalus secondary to CAB (as described in literature [27]); one case of postsurgical cerebrospinal fluid; and four cases of new pituitary deficiencies (two after pituitary irradiation and two after surgery).
In conclusion, GP are a particular type of secreting pituitary tumor characterized by a large tumor volume, extreme PRL hypersecretion and good sensitivity to DA treatment. However, even when using high doses of DA, the response is often insufficient in terms of biochemical and tumor control. Frequently, GP patients will require a greater number of treatments and nevertheless would not achieve similar therapeutic goals to those obtained in patients with non-GP. Goals of treatment should be individualized and must include the following: resolving acute compressive symptoms, eradicating or reducing tumor mass while avoiding local compression, decreasing PRL concentration to a level that does not have significant clinical consequences and preserving pituitary function. DA should be the first choice of treatment except in patients with acute compressive symptoms or when pituitary apoplexy is suspected. An insufficient response to a high dose of DA may require decompressive or debulking surgery, especially if compressive symptoms are present. RT is rarely necessary for proliferative tumors that are resistant to other treatment modalities. Patients with GP will frequently require multimodal therapy including chronic treatment with DA, and most of them will achieve good (or at least enough) hormonal and tumor control without significant adverse events.
References
A.B. Moraes, C.M. Dos Santos Silva, L. Vieira Neto, M.R. Gadelha, Giant prolactinomas: the therapeutic approach. Clin. Endocrinol. (Oxf.) 79(4), 447–456 (2013)
I. Shimon, C. Benbassat, M. Hadani, Effectiveness of long-term cabergoline treatment for giant prolactinoma: study of 12 men. Eur. J. Endocrinol. 156(2), 225–231 (2007)
D. Maiter, E. Delgrange, Therapy of endocrine disease: the challenges in managing giant prolactinomas. Eur. J. Endocrinol. 170, 13–27 (2014)
S. Dash, A.K. Annamalai, H.L. Simpson, N. Sarkies, N.M. Antoun, R. Mannion, Acute shrinkage of a giant prolactinoma, masquerading as an erosive skull base tumour. QJM. 106, 85 (2013)
R.K. Shrivastava, M.S. Arginteanu, W.A. King, K.D. Post, Giant prolactinomas: clinical management and long-term follow up. J. Neurosurg. 97(2), 299–306 (2002)
S.M. Corsello, G. Ubertini, M. Altomare, R.M. Lovicu, M.G. Migneco, C.A. Rota, C. Colosimo, Giant prolactinomas in men: efficacy of cabergoline treatment. Clin. Endocrinol. (Oxf.) 58(5), 662–670 (2003)
M.E. Molitch, M.O. Thorner, C. Wilson, Management of prolactinomas. J. Clin. Endocrinol. 82, 996–1000 (1997)
G. Di Chiro, K.B. Nelson, The volume of the sella turcica. Am. J. Roentgenol Radium Ther. Nucl. Med. 87, 989–1008 (1962)
P. Lundin, F. Pedersen, Volume of pituitary macroadenomas: assessment by MRI. J. Comput. Assist. Tomogr. 16, 519–528 (1992)
A. Ciccarelli, A.F. Daly, A. Beckers, The epidemiology of prolactinomas. Pituitary 8, 3–6 (2005)
S. Melmed, F.F. Casanueva, A.R. Hoffman, D.L. Kleinberg, V.M. Montori, J.A. Schlechte, J.A. Wass, Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96(2), 273–288 (2011)
Z.B. Wu, C.J. Yu, Z.P. Su, Q.C. Zhuge, J.S. Wu, W.M. Zheng, Bromocriptine treatment of invasive giant prolactinomas involving the cavernous sinus: results of a long-term follow up. J. Neurosurg. 104(1), 54–61 (2006)
E. Delgrange, G. Raverot, M. Bex, P. Burman, B. Decoudier, F. Devuyst, U. Feldt-Rasmussen, M. Andersen, D. Maiter, Giant prolactinomas in women. Eur. J. Endocrinol. 170, 31–38 (2014)
M.H. Almalki, B. Buhary, S. Alzahrani, F. Alshahrani, S. Alsherbeni, G. Alhowsawi, N. Aljohani, Giant prolactinomas: clinical manifestations and outcomes of 16 Arab cases. Pituitary 3, 405–9 (2015)
A. Chattopadhyay, A. Bhansali, S.R. Masoodi, Long-term efficacy of bromocriptine in macroprolactinomas and giant prolactinomas in men. Pituitary 8(2), 147–154 (2005)
E.H. Cho, S.A. Lee, J.Y. Chung, E.H. Koh, Y.H. Cho, J.H. Kim, C.J. Kim, M.S. Kim, Efficacy and safety of cabergoline as first line treatment for invasive giant prolactinoma. J. Korean Med. Sci. 24(5), 874–878 (2009)
O. Cooper, A. Mamelak, S. Bannykh, J. Carmichael, V. Bonert, S. Lim, G. Cook-Wien, A. Ben-Shlomo, Prolactinoma ErbB receptor expression and targeted therapy for aggressive tumors. Endocrine 46(2), 318–327 (2014)
E. Delgrange, J. Trouillas, D. Maiter, J. Donckier, J. Tourniaire, Sex-related difference in the growth of prolactinomas: a clinical and proliferation marker study. J. Clin. Endocrinol. Metab. 82(7), 2102–2107 (1997)
G. Minniti, M.L. Jaffrain-Rea, A. Santoro, V. Esposito, L. Ferrante, R. Delfini, G. Cantore, Giant prolactinomas presenting as skull base tumors. Surg. Neurol. 57(2), 99–103 (2002)
I. Kreitschmann-Andermahr, S. Siegel, B. Kleist, J. Kohlmann, D. Starz, R. Buslei, M. Koltowska-Häggström, C.J. Strasburger, M. Buchfelder, Diagnosis and management of acromegaly: the patient’s perspective. Pituitary 19(3), 268–276 (2016)
E. Espinosa, E. Sosa, V. Mendoza, C. Ramírez, V. Melgar, M. Mercado, Giant prolactinomas: are they really different from ordinary macroprolactinomas? Endocrine 52(3), 652–659 (2016)
C. Yu, Z. Wu, J. Gong, Combined treatment of invasive giant prolactinomas. Pituitary 8(1), 61–65 (2005)
H.H. Oruçkaptan, O. Senmevsim, O.E. Ozcan, T. Ozgen, Pituitary adenomas: results of 684 surgically treated patients and review of the literature. Surg. Neurol. 53(3), 211–219 (2000)
I. Shimon, E. Sosa, V. Mendoza, Y. Greenman, A. Tirosh, E. Espinosa, V. Popovic, A. Glezer, M.D. Bronstein, M. Mercado, Giant prolactinomas larger than 60 mm in size: a cohort of massive and aggressive prolactin-secreting pituitary adenomas. Pituitary 19(4), 429–436 (2016)
V. Primeau, C. Raftopoulos, D. Maiter, Outcomes of transsphenoidal surgery in prolactinomas: improvement of hormonal control in dopamine agonist-resistant patients. Eur. J. Endocrinol. 166, 779–786 (2012)
L. Vroonen, M.L. Jaffrain-Rea, P. Petrossian, G. Tamagno, P. Chanson, L. Vilar, F. Borson-Chazot, L.A. Naves, T. Brue, B. Gatta, Prolactino-mas resistant to standard doses of cabergoline: a multicenter study of 92 patients. Eur. J. Endocrinol. 167, 651–662 (2012)
J.D. Machicado, J.M. Varghese, P.R. Orlander, Cabergoline-induced pneumocephalus in a medically treated macroprolactinoma. J. Clin. Endocrinol. Metab. 97(10), 3412–3413 (2012)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Andujar-Plata, P., Villar-Taibo, R., Ballesteros-Pomar, M.D. et al. Long-term outcome of multimodal therapy for giant prolactinomas. Endocrine 55, 231–238 (2017). https://doi.org/10.1007/s12020-016-1129-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1129-9