Abstract
To examine the effects of a structured group-based education programme, patient empowerment programme (PEP), compared with usual care on 2-year changes in patient-reported outcomes (PRO) in patients with diabetes mellitus (DM). A prospective observational study of 715 patients (PEP/non-PEP: 390/325) was conducted to complete the baseline PRO survey and followed up for 2 years. Health-related quality of life (HRQOL) was measured using the short-form 12 at baseline and annually at two follow-up assessments, which yielded physical and mental component summary and SF-6D preference-based scores. Perceived control over diabetes and general health status were measured using the patient enablement instrument (PEI) and global rating scale (GRS) at follow-ups. When compared with non-PEP, PEP participants significantly reported improvement in health condition (GRS score > 0; 24.55 % vs 10.16 %; odds ratio = 2.502; P = 0.018) in 2 years and enabled the self-perceived control over diabetes (PEI score > 0; 72.20 % vs 38.40 %; odds ratio = 3.25; P < 0.001) in 1-year follow-up but no sustained effects in year 2 (52.65 % vs 39.04 %; odds ratio = 1.366; P = 0.265). There were no significant differences between PEP and non-PEP groups in the changes in quality of life scores (all P > 0.05) at 1 year. Although HRQOL scores deteriorated over 2-year period in both groups, PEP participants reported similar changes in HRQOL scores to that of non-PEP. PEP for DM patients preserved self-perceived disease control and health condition, whereas PEP participants perceived their HRQOL similar to that of non-PEP participants. Findings of PRO should be considered alongside clinical outcomes when evaluating the overall benefits of PEP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is one of the most common chronic diseases, with an increased prevalence worldwide [1]. To halt the diabetes epidemic, a growing body of literature on comparative effectiveness research has quantified the benefits and harms of emerging interventions for diabetes, primarily on pharmacological interventions [2–4], to inform judicious decision-making about which alternate intervention is more effective when compared to usual care through synthesis of evidence.
Systematic reviews [5, 6] and meta-analyses [7–9] concluded that diabetes education and self-management interventions had heavily relied on conventional lifestyle modifications and clinical outcomes reflected by metabolic control, but had less turned to outcomes from patients’ perspective. In recognition of need for data on patients’ perspective, information collected using patient-reported outcomes (PRO) based on subjective data provided by patients or patient proxies [10] is considerably integrated with clinical data for comparative effectiveness research. Thus, recommendation of the adopted use of PRO within comparative effectiveness research was warranted by Patient-Centred Outcomes Research Institute (PCORI) [11], Agency for Healthcare Research and Quality (AHRQ) [12] and professional societies like International Society of Quality of Life Research (ISOQOL) [13]. Given that diabetes self-management education is the patient-centred process of facilitating the exchange of knowledge, skill and ability necessary for diabetes self-care [14], several desirable PRO [15] refer to the measurement of constructs including health-related quality of life (HRQOL), diabetes knowledge, self-management/behaviour change and perceived control.
Different constructs of PRO data are available alongside the clinical data in comparative effectiveness research for diabetes education interventions in the United States [16] and United Kingdom [17–19]. Due to heterogeneity of HRQOL effects across studies in a meta-analysis [20], strength of evidence on HRQOL effects reported in self-management education interventions of diabetes was insufficient to make valid conclusions on whether the HRQOL outcomes following interventions were improved or not. Moreover, there is a paucity of PRO data for comparative effectiveness research in Hong Kong context. The implementation of patient empowerment programme (PEP), a structured diabetes education programme in Hong Kong primary care setting, was evaluated in a study design of prospective comparative effectiveness research. Up to 3 years of follow-up, more diabetic patients in PEP group in comparison with non-PEP group were associated with better metabolic control [21], reduced all-cause mortality [22], cardiovascular complications [22, 23], microvascular complications [23, 24], hospitalization and emergency department visits [25]. The effects of PEP on PROs were evaluated in an interim analysis of a before-and-after study design [26]. Despite improvement in role emotional (RE) and bodily pain (BP) as a result of PEP, the lacking in a comparison group (control or usual care group) would limit the implication of whether PEP (compared with non-PEP) was associated with improved HRQOL and PRO at large.
This comparative effectiveness research in observational study design aimed to evaluate the effect of PEP on PRO in the constructs of HRQOL, preference-based measure, transition rating in patient’s enablement and global health condition at and 2-year follow-up of PEP and non-PEP groups.
Methods
This analysis reflects the first 2-year PRO data derived from the evaluation of PEP as a tertiary-wide primary care service component in Hospital Authority of Hong Kong (HA). The PEP has been launched in 2010 for the purpose of quality of diabetes management enhancement in primary care in Hong Kong. A detailed description of the setting of PEP has been published previously [21, 22, 24].
In sequential roll-out design of PEP intervention, four out of seven local district clusters had implemented PEP interventions in 2010, while the remaining three joined in 2011. In brief, two non-government organizations (NGOs) highly experienced in community medical service and education were invited to participate in this programme in first phase. Subsequently, four NGOs in second phase and three NGOs in third phase were commissioned. They were required to deliver sessions on disease-specific knowledge and self-management skills, self-efficacy and lifestyle modifications. Each enrolled patients would receive generic self-efficacy enhancement and lifestyle modification components, and disease-specific knowledge and skills component sessions. Generic component sessions covered the importance of self-management and behaviour modification, healthy diet and regular exercise habit, goal setting and problem-solving skills, sharing on self-monitoring experience, stress coping management, psychosocial support and networking, communications with healthcare professionals. Disease-specific sessions, in total of 300 min or equivalent, would cover comprehensive information about diabetes, responsibility of self-care management, medications in diabetes control and contingency management on hypo-glycaemia and hyper-glycaemia.
Subjects
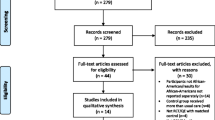
Subjects were eligible for the PRO analysis if we had successfully matched the patient identifier with HA administrative data to link with clinical data. Both PEP participants and controls were contacted for the baseline PRO survey by telephone interview within 1 month from the date of recruitment, and followed up for the 1 and 2-year assessments (Fig. 1 ). Since the PEP enrolment status was identified through administrative data and PRO survey, control subjects who enrolled in PEP after baseline date were dropped from the analysis.
For PRO analysis, both PEP participants and controls were administered with the socio-demographic questions and HRQOL instrument using the Chinese (Hong Kong) version of SF-12v2 at baseline assessment. The assessments on perceived control over diabetes and general health (GH) status using the patient enablement instrument (PEI) and global rating scale (GRS) were undertaken at 1 and 2-year follow-up by telephone. The retrospective measures of PEI and GRS were not required to be administered at baseline.
The PRO data were linked with the clinical data including anthropometric and biochemical information through clinical management system database of HA. The integration of PRO data with clinical data provided a comprehensive profile of patients’ health, and validated the diagnosis of type 2 diabetes with the primary care physician coding International Classification of Primary Care (ICPC-2) of T90 diabetes non-insulin dependent. We defined the subjects as having hypertension and the presence of diabetic complications according to the diagnosis coding system of International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) and ICPC-2 in HA administrative database. The information letter explained the study aim was explained, and the written informed consent was obtained in all PEP and non-PEP participants.
Ethics approval of this study was granted by institutional review board and clinical trial registry (HKCTR-1187).
Patient-reported outcomes
We identified four appropriate and validated PRO measures (SF-12v2, SF-6D, PEI and GRS) to capture relevant constructs by which the comparative effectiveness of PEP intervention was adequately evaluated and judged.
HRQOL measures
The Chinese (Hong Kong) SF-12 Health Survey has been validated [27] and normed [28] on the general Chinese population in Hong Kong, and thus was used to measure generic HRQOL in the same population with diabetes [26, 29]. It measures eight domains of HRQOL on physical functioning (PF), role physical (RP), BP, GH, vitality (VT), social functioning (SF), RE and mental health (MH) on a scale with theoretical range from 0 to 100. A higher score indicates better HRQOL. The eight domain scores were aggregated based on population-specific weights to calculate two summary scores, the physical component summary (PCS) and mental component summary (MCS).
By deriving the SF-6D preference-based score, seven out of twelve items from SF-12v2 has been selected to retain the minimum loss of descriptive information as described by Brazier and colleagues [30]. The theoretical range of SF-6D preference-based score ranged from 1 for full health to 0.315 for the worse possible health state according to Chinese Hong Kong population-specific scoring algorithm [31, 32]. The SF-12v2-derived SF-6D preference-based score was responsive to detect positive changes over time [33]. The SF-6D preference-based score is served as preference weighting input to quality-adjusted life-year outcomes in economic evaluation to inform health policy decision-making.
Patient enablement instrument
The Patient Enablement Instrument (PEI) is a retrospective measure of patient’s enablement in perceived control and coping with the illness [34]. The PEI was originally developed by Howie and colleagues [35] to measure patient’s enablement, translated into traditional Chinese version and shown to be valid and reliable in Chinese patients [36]. It has six items (1. able to cope with life, 2. able to understand your illness, 3. able to cope with your illness, 4. able to keep yourself healthy, 5. confident about your health and 6. able to help yourself) each rated on a 3-point (0 = the same or less; 1 = slightly improved/increased; 2 = greatly improved/increased). The summation of six-item score provides the PEI score ranging from 0 to 12, with a higher score indicating better self-perceived enablement.
Global rating scale
The GRS is a single retrospective item assessing the subject’s global perception of any change in the overall health condition on a 7-point scale (−3 = much worse to 3 = much improved) over the last 12 months. The GRS questionnaire, developed by Jaeschke et al. in 1987 [37], has been commonly used as the external criterion of subjective change in global health condition.
Data analysis
Descriptive statistics were used to calculate the baseline characteristics of socio-demographic and clinical data in PEP and non-PEP groups. Differences in baseline characteristics between PEP and non-PEP were tested using independent t-test for continuous variables and χ 2 test for categorical variables.
As the HRQOL scores by SF-12v2 were the only PRO measured at baseline and follow-up, we assessed the effects of PEP on HRQOL over time while accounting for within-subject correlation with repeated measurement. Unadjusted analyses on the changes in HRQOL scores at follow-up from baseline between PEP and non-PEP groups were tested using paired t-test. The linear mixed effect model including patients as a random effect, with the adjustment of baseline characteristics, was constructed to undertake the adjusted analysis on the effect of PEP on SF-12v2, SF-6D scores. Multiple logistic regression was used for PEI > 0 and GRS > 0 at 1 and 2-year follow-up between PEP and non-PEP group. Adjusted analysis controlled for both socio-demographic (gender, age, marital status, drinking, educational level, smoking, regular exercise and household monthly income) and clinical (blood pressure, HbA1c, lipid profile, body mass index (BMI), estimated glomerular filtration rate (eGFR), duration of DM, comorbidity and treatment modalities) characteristics.
All statistical analyses were performed using STATA Version 13.0. All significant tests were two-tailed and those with a P-value less than 0.05 were considered as statistically significant.
Results
After exclusion of those who failed to give consent and match with the administrative data, 1188 patients (569 PEP participants and 619 controls) were eligible for the PRO analysis. Subsequently, 390 (response rate: 68.5 %) PEP participants and 325 (response rate: 52.5 %) controls completed the baseline PRO survey, respectively.
Table 1 shows the comparison of the socio-demographic, clinical characteristics, SF-12v2 and SF-6D between PEP participants and control patients at baseline. For the socio-demographic characteristics, there were no significant differences between groups in terms of gender, regular exercise, household monthly income, marital and smoking status. However, we found that PEP participants were generally younger, more likely to be non-drinkers and with higher education. For clinical characteristics, PEP group significantly had higher diastolic blood pressure, HbA1c, low-density lipoprotein-cholesterol, total cholesterol to high-density lipoprotein-cholesterol ratio and eGFR than those of the control group, while the differences in SBP, triglyceride and BMI were not significant. For disease characteristics, the duration of DM of PEP group was significantly shorter and the proportion of family history of DM was significantly lower than those of the control group. For co-morbidity, PEP group significantly had lower proportion of having hypertension and higher eGFR than those of the control group, while there were no significant differences in the history of cardiovascular event, coronary heart disease, heart failure and stroke. For treatment modalities, the use of anti-hypertensive drugs in control group was significantly higher than that of PEP group, while there were no significant differences in the use of insulin, oral drugs and lipid-lowering agents. For the SF-12v2 scores, PEP group generally had higher scores in each of the domains than those of the control group. The differences in SF-12v2 scores between groups were generally significant, especially in the domains of PF, RP, BP, SF, RE and PCS scores. Finally, for the SF-6D score, PEP group significantly had a higher score than that of control group.
Table 2 shows the comparison of SF-12v2 scores, SF-6D, PEI and GRS between groups at baseline, post-12 months and post-24 months. A majority of PEP group (72.20 %) reported being ‘more enabled’ and 32.49 % reported global improvement in health after 12 months, and 52.65 % of PEP group reported being ‘more enabled’ and 24.55 % reported global improvement in health after 24 months, which were significantly higher than those reported by the control group. The difference in changes in PEI and GRS scores between groups were 2.08 and 0.46 after 12 months and 0.79 and 0.45 after 24 months, respectively, indicating better perceived disease control and global improvement in health for PEP participants. On the other hand, there were no significant differences in the changes in SF-12v2 and SF-6D scores between groups at 12 or 24 months. However, it should be noted that both groups reported significant reductions within group in the PCS, MCS and SF-6D at 24 months, suggesting worsening in HRQOL among these DM patients.
Table 3 shows the adjusted analysis on the effects of PEP on SF-12v2, SF-6D, PEI and GRS score. Adjusted analyses at 12 months or 24 months follow-up were not significant in PCS, MCS and SF-6D, indicating the effect of PEP with time on SF-12v2 and SF-6D scores were insignificant at 12 or 24 months. On the other hand, the effect of PEP with time on PEI > 0 was significantly positive (odds ratio = 3.250) at 12 months, while the effect of PEP with time on GRS > 0 was significantly positive (odds ratio = 2.502) at 24 months.
Discussions
This comparative effectiveness research assessed the important PRO at 2 years of the PEP in real-world primary care setting. A structured diabetes education intervention to promote self-management and empowerment of patients with diabetes was associated with significantly improved perceived control over diabetes at 1 year and GH status at 2 years, and with a non-significant improvement in the physical, mental and preference-based HRQOL at 2 years. Differences of the change in patient’ enablement and GH status outcomes between two groups favoured the PEP participants. Nevertheless, the lack of significant differences in physical, mental and preference-based HRQOL at 1 year echoed the findings from previous randomized controlled studies that the structured group-based education programme, the US Diabetes Conversation Map programme [16] and the UK Expert Patient Education (X-PERT) programme [17] showed no significantly better improvement in physical, mental aspect and overall HRQOL specific to diabetes when compared to usual care. Furthermore, comparative effectiveness research in diabetes education and self-management programme (DESMOND), a rigorously designed cluster randomized controlled trial, produced similar patterns of HRQOL changes at 1 and 3 years [18, 19]. Consistent finding of statistical insignificance could be in part due to low sensitivity of HRQOL instruments for diabetes education evaluation. When compared to retrospective ‘transition’ [38] measures of patient’ enablement and GH status, pre-/post-measure of HRQOL change might be a less insensitive PRO through the collection of generic [16, 18, 19] and diabetes-specific tools [17]. Although the achievable goal of diabetes education may be a managed deterioration or stability in HRQOL outcomes, insensitive measures could lead to a lesser variation in outcomes among diabetes educators and NGOs, rising concerns on the adoption of HRQOL outcomes for monitoring and assessing quality of care for PEP intervention.
Changes in HRQOL and preference-based measures over time were similar in PEP and non-PEP groups. There were no significant changes in the physical and mental aspect of HRQOL from baseline to 1-year follow-up, in line with findings from our interim analysis of HRQOL data after PEP participation [26]. At 2-year follow-up, both the PEP and non-PEP participants were not effective in sustaining physical and mental aspect of HRQOL, dropping with 1.68–2.07 points and 4.22–4.68 points, respectively. Unlike the HRQOL outcomes, the GH condition sustained significant improvement to 2 years, while the PEP enabled the patients’ perceived control over diabetes at 1 year but did not sustain until 2 years. As significant changes were detected after PEP intervention, this study highlighted the importance of measuring the patient’s enablement and health status as quality indicators of diabetes education interventions. Provided that the PEP was associated with reduced diabetic complications [22–24], such reductions may be in part contributed by the benefits of improved PRO. However, further analyses are warranted to ascertain that PRO mediates the association between PEP and diabetic complication.
Impact of administration modes on PRO results should be recognized. Mode of administration for this study was telephone interview deserving advantages of greater convenience and literacy to completing questionnaires [39]. Besides the advantages, the telephone interview disabled the direct patient–clinician communication on PRO results in tabulated and graphic presentations. In spite of substantial start-up and maintenance costs for electronic PRO collection, we urged the advocacy of electronic platform [40–42] to efficiently collect high-quality PRO data in routine assessments at intake enrolment and follow-up.
Limitations
Several limitations in this study should be acknowledged. First, the research method of PEP was designed based on a quasi-experimental, observational study rather than a pragmatic randomized controlled trial eliminating patient selection and confounding bias. Meanwhile, such study design observed real-world evidence of PEP effects in primary care setting. Second, many patients were excluded due to eligibility of data integration. Specifically, 1103 patients (PEP/non-PEP: 365/738) were excluded from analysis due to the failure to link PRO data with HA administrative data. Of those eligible to join the study, 206 patients (PEP/non-PEP: 112/94) were excluded due to their refusal to consent for integrating PRO data with clinical data. To minimize the waste of resource, collection of PRO data in routine practice was highly recommended to facilitate data integration. Finally, this prospective study focusing on Chinese population may not be generalizable to other non-Chinese population.
Conclusions
In a 2-year prospective study, PEP for patients with DM preserved self-perceived disease control and health condition, whereas PEP participants perceived their quality of life similar to non-PEP. This study underlined the importance of PRO integration, especially patient enablement and global health status, with clinical outcomes when evaluating the overall benefits of structured diabetes education intervention.
Abbreviations
- DM:
-
diabetes mellitus
- PEP:
-
patient empowerment programme
- PRO:
-
patient-reported outcomes
- PCS:
-
physical component summary
- MCS:
-
mental component summary
- PEI:
-
patient enablement instrument
- GRS:
-
global rating scale
- PCORI:
-
Patient-Centred Outcomes Research Institute
- AHRQ:
-
Agency for Healthcare Research and Quality
- ISOQOL:
-
International Society of Quality of Life Research
- HRQOL:
-
health-related quality of life
- NGOs:
-
non-government organizations
- PF:
-
physical functioning
- RP:
-
role physical
- BP:
-
bodily pain
- GH:
-
general health
- VT:
-
vitality
- SF:
-
social functioning
- RE:
-
role emotional
- MH:
-
mental health
References
L. Chen, D.J. Magliano, P.Z. Zimmet, The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat. Rev. Endocrinol. 8(4), 228–236 (2012). doi:10.1038/nrendo.2011.183
W.L. Bennett, N.M. Maruthur, S. Singh, J.B. Segal, L.M. Wilson, R. Chatterjee, S.S. Marinopoulos, M.A. Puhan, P. Ranasinghe, L. Block, W.K. Nicholson, S. Hutfless, E.B. Bass, S. Bolen, Comparative effectiveness and safety of medications for type 2 diabetes: an update including new drugs and 2-drug combinations. Ann. Intern. Med. 154(9), 602–613 (2011). doi:10.7326/0003-4819-154-9-201105030-00336
C.L. Roumie, A.M. Hung, R.A. Greevy, C.G. Grijalva, X. Liu, H.J. Murff, T.A. Elasy, M.R. Griffin, Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Ann. Intern. Med. 157(9), 601–610 (2012). doi:10.7326/0003-4819-157-9-201211060-00003
H.C. Yeh, T.T. Brown, N. Maruthur, P. Ranasinghe, Z. Berger, Y.D. Suh, L.M. Wilson, E.B. Haberl, J. Brick, E.B. Bass, S.H. Golden, Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann. Intern. Med. 157(5), 336–347 (2012). doi:10.7326/0003-4819-157-5-201209040-00508
E. Loveman, G.K. Frampton, A.J. Clegg, The clinical effectiveness of diabetes education models for type 2 diabetes: a systematic review. Health Technol. Assess. 12(9), 1–116 (2008)
A. Coppola, L. Sasso, A. Bagnasco, A. Giustina, C. Gazzaruso, The role of patient education in the prevention and management of type 2 diabetes: an overview. Endocrine (2015). doi:10.1007/s12020-015-0775-7
S.L. Norris, J. Lau, S.J. Smith, C.H. Schmid, M.M. Engelgau, Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 25(7), 1159–1171 (2002)
A. Steinsbekk, L.O. Rygg, M. Lisulo, M.B. Rise, A. Fretheim, Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus: a systematic review with meta-analysis. BMC Health Serv. Res. 12, 213 (2012). doi:10.1186/1472-6963-12-213
L. Fan, S. Sidani, Effectiveness of diabetes self-management education intervention elements: a meta-analysis. Can. J. Diabetes 33(1), 18–26 (2009)
C. Acquadro, R. Berzon, D. Dubois, N.K. Leidy, P. Marquis, D. Revicki, M. Rothman, P.R.O.H. Group, Incorporating the patient’s perspective into drug development and communication: an ad hoc task force report of the patient-reported outcomes (pro) harmonization group meeting at the Food and Drug Administration, February 16, 2001. Value Health 6(5), 522–531 (2003). doi:10.1046/j.1524-4733.2003.65309.x
Methodology Committee of the Patient-Centered Outcomes Research Institute (PCORI): Methodological standards and patient-centeredness in comparative effectiveness research: the PCORI perspective. J. Am. Med. Assoc. 307(15), 1636–1640 (2012). doi:10.1001/jama.2012.466
J. Slutsky, D. Atkins, S. Chang, B.A. Collins Sharp, AHRQ series paper 1: comparing medical interventions: AHRQ and the effective health-care program. J. Clin. Epidemiol. 63(5), 481–483 (2010). doi:10.1016/j.jclinepi.2008.06.009
B.B. Reeve, K.W. Wyrwich, A.W. Wu, G. Velikova, C.B. Terwee, C.F. Snyder, C. Schwartz, D.A. Revicki, C.M. Moinpour, L.D. McLeod, J.C. Lyons, W.R. Lenderking, P.S. Hinds, R.D. Hays, J. Greenhalgh, R. Gershon, D. Feeny, P.M. Fayers, D. Cella, M. Brundage, S. Ahmed, N.K. Aaronson, Z. Butt, ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual. Life Res. 22(8), 1889–1905 (2013). doi:10.1007/s11136-012-0344-y
M.A. Powers, J. Bardsley, M. Cypress, P. Duker, M.M. Funnell, A. Hess Fischl, M.D. Maryniuk, L. Siminerio, E. Vivian, Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care 38(7), 1372–1382 (2015). doi:10.2337/dc15-0730
R. Colagiuri, C.A. Eigenmann, A national consensus on outcomes and indicators for diabetes patient education. Diabetic Med. 26(4), 442–446 (2009). doi:10.1111/j.1464-5491.2009.02700.x
J. Sperl-Hillen, S. Beaton, O. Fernandes, A. Von Worley, G. Vazquez-Benitez, E. Parker, A. Hanson, J. Lavin-Tompkins, P. Glasrud, H. Davis, K. Adams, W. Parsons, C.V. Spain, Comparative effectiveness of patient education methods for type 2 diabetes: a randomized controlled trial. Arch. Intern. Med. 171(22), 2001–2010 (2011). doi:10.1001/archinternmed.2011.507
T.A. Deakin, J.E. Cade, R. Williams, D.C. Greenwood, Structured patient education: the diabetes X-PERT programme makes a difference. Diabetic Med. 23(9), 944–954 (2006). doi:10.1111/j.1464-5491.2006.01906.x
K. Khunti, L.J. Gray, T. Skinner, M.E. Carey, K. Realf, H. Dallosso, H. Fisher, M. Campbell, S. Heller, M.J. Davies, Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. Br. Med. J. 344, e2333 (2012). doi:10.1136/bmj.e2333
M.J. Davies, S. Heller, T.C. Skinner, M.J. Campbell, M.E. Carey, S. Cradock, H.M. Dallosso, H. Daly, Y. Doherty, S. Eaton, C. Fox, L. Oliver, K. Rantell, G. Rayman, K. Khunti, E. Diabetes, Self Management for, O., Newly Diagnosed, C.: Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. Br. Med. J. 336(7642), 491–495 (2008). doi:10.1136/bmj.39474.922025.BE
J. Cochran, V.S. Conn, Meta-analysis of quality of life outcomes following diabetes self-management training. Diabetes Educ. 34(5), 815–823 (2008). doi:10.1177/0145721708323640
C.K.H. Wong, W.C.W. Wong, C.L.K. Lam, Y.F. Wan, W.H.T. Wong, K.L. Chung, D. Dai, E.L.H. Tsui, D.Y.T. Fong, Effects of patient empowerment programme (PEP) on clinical outcomes and health service utilization in type 2 diabetes mellitus in primary care: an observational matched cohort study. PLoS ONE 9(5), e95328 (2014). doi:10.1371/journal.pone.0095328
C.K.H. Wong, W.C.W. Wong, Y.F. Wan, A.K.C. Chan, K.L. Chung, F.W.K. Chan, C.L.K. Lam, Patient empowerment programme in primary care reduced all-cause mortality and cardiovascular diseases in patients with type 2 diabetes mellitus: a population-based propensity-matched cohort study. Diabetes Obes. Metab. 17(2), 128–135 (2015). doi:10.1111/dom.12397
C.K.H. Wong, W.C.W. Wong, E.Y.F. Wan, A.K.C. Chan, F.W.K. Chan, C.L.K. Lam, Macrovascular and microvascular disease in obese patients with type 2 diabetes attending structured diabetes education program: a population-based propensity-matched cohort analysis of patient empowerment programme (PEP). Endocrine. 53(2), 412–422 (2016). doi:10.1007/s12020-015-0843-z
C.K.H. Wong, W.C.W. Wong, Y.F. Wan, A.K.C. Chan, F.W.C. Chan, C.L.K. Lam, Patient empowerment programme (PEP) and risk of microvascular diseases among patients with type 2 diabetes mellitus in primary care: a population-based propensity matched cohort study. Diabetes Care 38(8), e116–117 (2015). doi:10.2337/dc14-2213
C.K.H. Wong, W.C.W. Wong, E.Y.F. Wan, A.K.C. Chan, F.W.K. Chan, C.L.K. Lam, Effect of a structured diabetes education programme in primary care on hospitalizations and emergency department visits among people with type 2 diabetes mellitus: results from the patient empowerment programme. Diabetic Med. (2015). doi:10.1111/dme.12969
C.K.H. Wong, W.C.W. Wong, E. Wan, W. Wong, F.W.K. Chan, C.L.K. Lam, Increased number of structured diabetes education attendance was not associated with the improvement in patient-reported health-related quality of life: results from patient empowerment programme (PEP). Health Qual. Life Outcomes 13(1), 126 (2015). doi:10.1186/s12955-015-0324-3
C.L.K. Lam, E.Y.Y. Tse, B. Gandek, Is the standard SF-12 health survey valid and equivalent for a Chinese population? Qual. Life Res. 14(2), 539–547 (2005)
C.L.K. Lam, C.K.H. Wong, E.T.P. Lam, Y.Y.C. Lo, W.W. Huang, Population norm of Chinese (HK) SF-12 health survey_version 2 of Chinese adults in Hong Kong. HK Practitioner 32(2), 77–86 (2010)
C.K.H. Wong, Y.Y.C. Lo, W.H.T. Wong, C.S.C. Fung, The associations of body mass index with physical and mental aspects of health-related quality of life in Chinese patients with type 2 diabetes mellitus: results from a cross-sectional survey. Health Qual. Life Outcomes 11(1), 142 (2013). doi:10.1186/1477-7525-11-142
J.E. Brazier, J. Roberts, The estimation of a preference-based measure of health from the SF-12. Med. Care 42(9), 851–859 (2004)
S.M. McGhee, J. Brazier, C.L.K. Lam, L.C. Wong, J. Chau, A. Cheung, A. Ho, Quality-adjusted life years: population-specific measurement of the quality component. Hong Kong Med. J. 17(Suppl 6), 17–21 (2011)
C.L.K. Lam, J. Brazier, S.M. McGhee, Valuation of the SF-6D health states is feasible, acceptable, reliable, and valid in a Chinese population. Value Health 11(2), 295–303 (2008). doi:10.1111/j.1524-4733.2007.00233.x
C.K.H. Wong, B. Mulhern, Y.-F. Wan, C.L.K. Lam, Responsiveness was similar between direct and mapped SF-6D in colorectal cancer patients who declined. J. Clin. Epidemiol. 67(2), 219–227 (2014). doi:10.1016/j.jclinepi.2013.08.011
M. McAllister, G. Dunn, K. Payne, L. Davies, C. Todd, Patient empowerment: the need to consider it as a measurable patient-reported outcome for chronic conditions. BMC Health Serv. Res. 12(1), 157 (2012). doi:10.1186/1472-6963-12-157
J.G. Howie, D.J. Heaney, M. Maxwell, J.J. Walker, A comparison of a patient enablement instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam. Pract. 15(2), 165–171 (1998). doi:10.1093/fampra/15.2.165
C.L. Lam, N.Y. Yuen, S.W. Mercer, W. Wong, A pilot study on the validity and reliability of the patient enablement instrument (PEI) in a Chinese population. Fam. Pract. 27(4), 395–403 (2010). doi:10.1093/fampra/cmq021
R. Jaeschke, J. Singer, G.H. Guyatt, Measurement of health status: ascertaining the minimal clinically important difference. Control Clin. Trials 10(4), 407–415 (1989)
G.H. Guyatt, G.R. Norman, E.F. Juniper, L.E. Griffith, A critical look at transition ratings. J. Clin. Epidemiol. 55(9), 900–908 (2002). doi:10.1016/S0895-4356(02)00435-3
C.F. Snyder, N.K. Aaronson, A.K. Choucair, T.E. Elliott, J. Greenhalgh, M.Y. Halyard, R. Hess, D.M. Miller, B.B. Reeve, M. Santana, Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Qual. Life Res. 21(8), 1305–1314 (2012). doi:10.1007/s11136-011-0054-x
S. Ahmed, R.A. Berzon, D.A. Revicki, W.R. Lenderking, C.M. Moinpour, E. Basch, B.B. Reeve, A.W. Wu, on behalf of the International Society for Quality of Life Research: The use of patient-reported outcomes (PRO) within comparative effectiveness research: implications for clinical practice and health care policy. Med. Care 50(12), 1060–1070 (2012). doi:10.1097/MLR.0b013e318268aaff
A.W. Wu, C. Snyder, C.M. Clancy, D.M. Steinwachs, Adding the patient perspective to comparative effectiveness research. Health Aff. 29(10), 1863–1871 (2010). doi:10.1377/hlthaff.2010.0660
A.W. Wu, H. Kharrazi, L.E. Boulware, C.F. Snyder, Measure once, cut twice—adding patient-reported outcome measures to the electronic health record for comparative effectiveness research. J. Clin. Epidemiol. 66(8, Supplement), S12–S20 (2013). doi:10.1016/j.jclinepi.2013.04.005
Acknowledgments
We would like to thank the programme teams at HA head office (including Ms. Margaret Tay, Dr. Alexander Chiu, Dr. K. L. Chung, Dr. Alan Y. L. Kwok, Ms. Michelle Wong, Mr. Gary Ching and Ms. Bonnie Fok), and all cluster representatives and clinical staff in the patient empowerment programme for working with our team in this evaluation. Furthermore, we would like to thank Dr. S. V. Lo and the staff of the Statistics & Workforce Planning Department in the Hospital Authority Strategy and Planning Division for their help in coordinating the development of the evaluation frameworks and site visits and facilitating the data collection. This study has been funded by the Hong Kong Hospital Authority (Ref. no: 8011014157) and the Commissioned Study on Enhanced Primary Care, Food and Health Bureau, HKSAR (Ref. no EPC-HKU-2). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author contribution
Carlos K. H. Wong is the guarantor of the study. C. K. H. W. wrote the manuscript and researched data. F. W. K. C. contributed to acquisition of data and reviewed/edited the manuscript. W. C. W. W. and C. L. K. L. contributed to study design. Y. F. W., A. K. C. C and P. C. H. reviewed/edited the manuscript, contributed to statistical analysis and interpretation of results. W. C. W. W. and C. L. K. L. reviewed/edited the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Wong, C.K.H., Lam, C.L.K., Wan, E.Y.F. et al. Evaluation of patient-reported outcomes data in structured diabetes education intervention: 2-year follow-up data of patient empowerment programme. Endocrine 54, 422–432 (2016). https://doi.org/10.1007/s12020-016-1015-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1015-5