Abstract
Increasing number of patients with thyroid carcinoma, especially young female patients, prefer to choose endoscopic thyroidectomy with bilateral central neck dissection (ETBC) for perfect cosmetic effects. However, the incidence of hypoparathyroidism after ETBC has not been well studied. Ninety six patients with papillary thyroid carcinoma were enrolled. All patients, including 49 ETBC and 47 open surgery patients, underwent total thyroidectomy with bilateral central neck dissection (CND). Some patients also underwent lateral neck dissection simultaneously. The incidence of hypoparathyroidism and parathyroid hormone (PTH) level were examined. Patients in the open surgery group had more advanced lesions, with larger tumor (p = 0.000), older age (p = 0.000), and more serious local involvement. The dissection extent of the open group was significantly larger than that of the ETBC group (p = 0.006). In contrast, the ETBC group with less dissection extent showed a significantly higher incidence of transient hypoparathyroidism than the open group (59.2 vs. 29.6 %, p = 0.004). The average PTH decline of the ETBC group was significantly higher than that of the open group on postoperative day 1 (POD1) (32.1 vs. 21.6 pg/ml, p = 0.010). Furthermore, the ETBC group had a significantly higher portion of patients with a PTH <10 pg/ml on POD1 (p = 0.001). One patient in the ETBC group developed permanent hypoparathyroidism. Autotransplantation and inadvertent removal rates of parathyroid did not differ between the two groups. Although generally considered a safe method for patients with thyroid carcinoma, ETBC may increase the risk of transient hypoparathyroidism compared with conventional open surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma has become an increasingly common thyroid malignancy, with a female-to-male incidence ratio of 5–1 [1, 2]. The prevalence of ultrasound (US) has profoundly facilitated the detection and thus surgical treatment of papillary thyroid carcinomas, especially micro-carcinomas [3]. Hypocalcemia, mostly due to inadvertent devascularization or removal of parathyroid glands, is the most frequent complication after total thyroidectomy [4–6]. Although the majority of iatrogenic hypoparathyroidism is transient, 3–4 % PTC patients may develop a permanent hypoparathyroidism after thyroidectomy plus neck dissection [2]. Some studies even reported an incidence of 10 % [7].
Scarless in the neck endoscopic thyroidectomy has cosmetic advantage over conventional open surgery [8]. Following the first report by Gangner [9], various endoscopic thyroidectomy techniques have been developed [10]. Accumulating clinical studies have confirmed this technique as a safe procedure with similar clinical effect as open surgery. Exploited initially at benign thyroid diseases like goiter and adenoma, surgical indications of endoscopic thyroidectomy have been markedly extended along with the progress on surgical skills and instruments [11, 12]. Nowadays, endoscopic surgery of small thyroid carcinoma could be safely accomplished at certain high-volume medical institutes in China and Korea [12].
Previous studies have shown that postoperative hypoparathyroidism is correlated to the extent of resection and surgical technique, based mostly on open surgery studies [4, 13–15]. There have been some reports on hypocalcemia after endoscopic thyroidectomy with similar incidence [16–20]. Nevertheless, the surgical extents in those reports were not consistent. Patients who underwent unilateral lobectomy, subtotal thyroidectomy, or total thyroidectomy were often included simultaneously. Besides, most patients with thyroid carcinoma just underwent ipsilateral central neck dissection (CND) in those studies. Moreover, a large portion of benign lesions, which did not need neck dissection, were also included [19]. It is conceivable that with the enlargement of surgical extent on thyroidectomy plus lymph node dissection, the risk of postoperative hypoparathyroidism by endoscopic approach could be underappreciated. We report herein for the first time that endoscopic thyroidectomy with bilateral CND could increase the risk of hypoparathyroidism than conventional open surgery.
Materials and methods
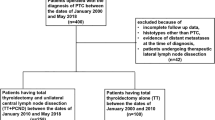
Patients
The study design and protocol were approved by the Ethics Committee of Second Affiliated Hospital, Zhejiang University College of Medicine. From January 2014 to December 2014, 49 consecutive patients undergoing endoscopic thyroidectomy with bilateral central neck dissection (ETBC) were included for this study. Forty seven consecutive patients who underwent open thyroidectomy and bilateral CND in the same period were selected as the control group. All patients included in this study met the following criteria: all received total thyroidectomy, node dissection extent contained bilateral central neck compartments at least, none had previously undergone thyroid operation, and all had an adequate medical history available. Six patients in the ETBC group and 17 patients in the open surgery group showed signs of lateral neck metastases by preoperative US. A simultaneous selective lateral neck dissection (LND) was performed for the 23 patients. Seven patients in the open surgery group showed signs of strap muscle involvement. No patient showed signs of vocal cord involvement. Indications for the ETBC operation included: (1) differentiated thyroid carcinoma with a maximum tumor size <2.5 cm; (2) 15–50 years old; and (3) the patients had a cosmetic requirement. The exclusion criteria were as follows: (1) male; (2) fat (BMI >30); (3) short neck; (4) previous neck or chest surgical history; (5) metastatic lymph nodes in level V or metastatic lymph nodes occurred below the sternoclavicular joint; (6) metastatic lymph nodes were fused with each other or fixed in the neck; and (7) metastatic lymph nodes invade surrounding tissue, such as trachea, esophagus, and recurrent laryngeal nerve. Preoperative diagnoses for thyroid nodules were made by ultrasound and ultrasound-guided fine-needle aspiration biopsy. Informed consent was obtained after informing surgical methods, possible complications, and possibility of conversion from endoscopic to open surgery.
Surgical procedures
For open surgery, 10 patients showed signs of central neck metastases by US with an average node diameter of 0.7 cm (range 0.5–0.9 cm). 17 patients showed signs of lateral neck metastases by US with an average node diameter of 1.1 cm (range 0.9–2.3 cm). Bilateral CND was performed for all enrolled patients. CND was performed cranially to both superior thyroid arteries and the pyramidal lobe, caudally to the innominate vein, laterally to the carotid sheaths, and dorsally to the prevertebral fascia. A selective LND including level II to IV was performed for patients with suspicious lateral nodes.
As to the ETBC group, four patients showed signs of central neck metastases by US with an average node diameter of 0.6 cm (range 0.5–0.7 cm). Six patients showed signs of lateral neck metastases by US with an average node diameter of 0.9 cm (range 0.7–1.3 cm). Prophylactic bilateral CND was performed for all enrolled patients. A selective endoscopic LND was performed for patients with suspicious lateral nodes. The ETBC procedure was described similarly in our previous publications [21, 22]. In the present study, all incisions were made around two areolas to make the scar more covert. Briefly, two incisions were made along the upper margin of right mammary areolas at opposite positions. One 10-mm trocar and another 5-mm trocar were inserted through the above incisions separately. Furthermore, a 5-mm incision was made along the upper margin of left mammary areola (Fig. 1). All the ETBC operations were performed with 5-mm ultrasonic coagulation device (Harmonic Scalpel, HS; Ethicon Endosurgery, USA). All devascularized parathyroid glands were routinely autografted in the sternocleidomastoid.
Hospitalization and postoperative follow-up
Parathyroid hormone (PTH) levels were routinely obtained 1 day before surgery. A serum PTH level was obtained on the morning of postoperative day 1 (POD1). Symptomatic hypocalcemia was defined as any patient who reported symptoms of perioral or digital numbness/tingling, or muscle cramps in the upper or lower extremities.
At the first postoperative clinic visit, patients were evaluated for symptoms of hypocalcemia. Serum calcium and PTH levels were obtained only for those patients started on calcium supplementation and/or calcitriol supplementation, or if persistent symptoms of hypocalcemia were reported after discharge.
Postoperative hypoparathyroidism was defined as permanent when parathyroid hormone was subnormal, or calcium with or without calcitriol supplementation exceeded 6 months postoperatively to treat clinical symptoms of hypocalcemia. Otherwise, the case was considered as transient hypoparathyroidism.
Statistics
Statistical analysis was performed using SPSS 17.0, Chicago, IL, USA. Frequencies were compared using Pearson χ 2 test. Continuous variables between two groups were compared using Mann–Whitney U test. A p value <0.05 was considered statistically significant.
Results
Demographics
There were 90 female (94 %) and 6 male (6 %) patients in total with a mean age at diagnosis of 40.4 years (range 17–80 years). Patients in the ETBC group were significantly younger than the open group (34.2 vs. 46.9 years, p = 0.000) (Table 1).
The average tumor diameter was 0.77 cm in the ETBC group and 1.24 cm in the open surgery group (p = 0.000). 78 % of patients (38/49) in the ETBC group had a largest tumor diameter ≤1 cm. In the open surgery group, 53 % of patients (25/47) had a largest tumor diameter ≤1 cm. 40.8 % of patients (20/49) in the ETBC group had central neck metastases, while 85.1 % of patients (40/47) in the open surgery group had central neck metastases. The difference was significant between the two groups (p = 0.024). As to the lateral compartment, 50 % of patients (3/6) in the ETBC group and 71 % of patients (12/17) in the open surgery group had lateral neck metastases by final pathology examination.
The open surgery group included more advanced lesions than the ETBC group. To be specific, tumors were significantly larger (1.24 vs. 0.77 cm, p = 0.000) and the incidence of multifocality was significantly higher in the open surgery group (78.7 vs. 53.1 %, p = 0.008). Besides, there were more lesions with extracapsular invasion and extrathyroid extension in the open surgery group (Table 1).
Surgery
Of the 49 patients in the ETBC group, 43 patients underwent total thyroidectomy with bilateral CND. Another six patients also underwent selective LND simultaneously. Of the 47 patients in the open surgery group, 30 patients underwent total thyroidectomy with bilateral CND. Another 17 patients underwent selective LND simultaneously. The dissection extent of the open group was significantly larger than that of the ETBC group (p = 0.006, Table 1).
The mean operation time of the ETBC group was significantly longer than that of the open surgery group (187 vs. 135 min, p = 0.000), although more patients underwent LND in the open surgery group. The node yield after neck dissection was not different between the two groups (Table 1).
Hypoparathyroidism and PTH decline
The average PTH decline of the ETBC group was significantly higher than that of the open group on POD1 (p = 0.01). More patients’ PTH level in the ETBC group dropped below the minimum reference of 15 pg/ml on POD1. The difference was significant between the two groups (p = 0.001). Furthermore, more patients in the ETBC group had a PTH <10 pg/mL on POD1. The difference was significant between the two groups (p = 0.001, Table 2).
The incidence of transient hypoparathyroidism in the ETBC group was 59.2 %, which was significantly higher than 29.8 % in the open group (p = 0.004). Of all the 96 patients, only one patient in the ETBC group developed permanent hypoparathyroidism (Table 2).
Fifteen patients in the ETBC group (30.6 %) and 11 patients (23.4 %) in the open surgery group underwent autotransplantation of the parathyroid gland. The difference was not significant between the two groups (p = 0.427). In the present study, inadvertently removed parathyroid glands referred to the resected ones found in the specimen during final pathology examination. Inadvertent removal of the parathyroid gland was observed in four patients in the ETBC group (8.2 %) and three patients (6.4 %) in the open surgery group, separately. The difference was not significant between the two groups (p = 0.737, Table 2).
Follow-up
Of the 43 patients who developed transient hypoparathyroidism, 40 patients recovered within 1 month postoperatively. The other three patients recovered within 2–3 months postoperatively, and they were all in the ETBC group. As to other complications, each group had one case of chyle leakage. No case of postoperative bleeding was observed. Two cases of transient vocal palsy were observed in the ETBC group. No case of permanent vocal palsy was observed (Table 1).
Discussion
The prevalence of endoscopic approach on thyroidectomy and neck dissection also accompanies ensuing concerns and arguments of this technique over morbidity and mortality. Although there have been some reports on hypoparathyroidism incidence post endoscopic thyroidectomy [16–20, 23], correlation between endoscopic surgical extent and hypoparathyroidism incidence has not been well studied. The extent of thyroidectomy and neck dissection was not identical in those studies. Moreover, endoscopic lobectomy of benign lesions without neck dissection was frequently included in previous studies. Tae previously reported that the hypoparathyroidism rate did not differ between endoscopic and open surgery groups; however, most of the included patients underwent unilateral thyroidectomy and neck dissection [24]. In this study, we aimed to analyze the effect of endoscopic total thyroidectomy with bilateral CND on the incidence of hypoparathyroidism.
The most surprising finding of the present study is that the ETBC group demonstrated a significantly higher incidence of transient hypoparathyroidism than that of the open surgery group. Consistently, the ETBC group manifested a significantly higher average PTH decline than the open group on POD1. In addition, significantly more patients’ PTH level dropped below the minimum reference of 15 pg/ml in the ETBC group. Previous studies suggested that a single PTH <10 pg/ml obtained in the morning on POD1 was amenable to predict the risk for symptomatic hypocalcemia [25, 26]. In this study, 46.9 % of the ETBC group had a PTH <10 pg/ml on POD1, which was concordant with the high incidence of transient hypoparathyroidism in this group. Based on these results, we concluded that ETBC increased the risk of transient hypoparathyroidism compared to the open surgery.
In contrast to previous findings that postoperative hypoparathyroidism risk is correlated to the dissection extent, the ETBC group with less dissection extent showed a significantly higher incidence of transient hypoparathyroidism. In the present study, the rate of parathyroid autotransplantation was similar between two groups (30.6 vs 23.4 %, p = 0.427). Besides, the rate of inadvertent removal of parathyroid glands was similar (8.2 vs 6.4 %, p = 0.737). Inadvertently removed parathyroid glands were found on specimen during final pathology examination, rendering the autotransplantation infeasible. Generally, the location of the upper parathyroid is relatively fixed, making it easily identifiable and well preserved. In addition, area around the upper parathyroid is rarely involved by metastatic nodes, which spared the upper parathyroid from iatrogenic injury during dissection. Taken together, we speculate that harmonic scalpel-inflicted devascularization of parathyroid glands during node dissection, especially the lower parathyroid glands, could be the main cause to a higher incidence of transient hypoparathyroidism.
Unlike open surgery, endoscopic identification of the recurrent laryngeal nerve (RLN) is basically accomplished at the lower pole of the thyroid gland. Besides, retraction and exposure of the gland mainly depends on one separating plier controlled by the operator. It is known that the blood supply of lower parathyroid comes largely from the inferior thyroid artery, whereas the upper parathyroid could be supplied by both the superior and inferior thyroid arteries [27, 28]. During the RLN exposure process and node dissection, peripheral ligation of the inferior thyroid artery, which is essential to preserve the integrity of the parathyroidal branches [14], may not be completely guaranteed in ETBC. One important reason is that the retraction of the thyroid is very inconvenient in ETBC, and the exposure of RLN is more confined compared with open surgery. This may jeopardize the parathyroidal branches and lead to a high incidence of postoperative hypoparathyroidism. A fine retractor may better solve this problem. Recently, we exploited a MiniLap instrument (Stryker, San Jose, CA, USA) in the node dissection and found this instrument useful in yielding a better view of the inferior thyroid artery and RLN.
In the present study, all patients in the ETBC group were performed bilateral CND, although controversy exists about routine prophylactic CND for patients with papillary carcinoma, especially low-risk micro-carcinomas [29, 30]. One major concern is the recurrence in the central neck area. Female patients prefer the endoscopic approach for its cosmetic advantage to avoid the neck scar. However, a re-operation due to recurrence will undo this cosmetic effect and could also cause further complications [31, 32]. To keep the recurrence risk to the minimum, we performed central neck dissection meticulously for each patient. However, consensus on the rationality of ETBC could not be drawn yet. More perspective studies with a large number of patients and long-term follow-up are needed to better address this controversy.
In the present study, LND was performed for six patients without a fine-needle aspiration (FNA) preoperatively in the ETBC group. Although FNA is the golden standard for a suspicious node, some nodes with micro-metastases may not be amenable for FNA. Besides, a negative FNA could not completely rule out the possibility of metastasis. For the same concern as the prophylactic CND, we prefer to remove any suspicious lateral compartment nodes for patients undergoing ETBC. In addition, many patients in our hospital are reluctant to take further node biopsy besides the primary thyroid lesions. Nevertheless, we are incorporating FNA as a routine procedure for suspicious lymph nodes.
Our hospital represents a high-volume medical institute for the treatment of thyroid carcinomas, and around 300 endoscopic thyroid surgeries are performed each year. Of note, all the operations in this study were accomplished by two senior surgeons highly skilled in endoscopic techniques (Zhiyu Li and Ping Wang) [8, 21, 22, 33]. It is well known that the endoscopic thyroidectomy has a relatively long learning curve. Therefore, the risk of hypoparathyroidism could be greatly increased, once the ETBC is performed by less-experienced hands in a low-volume institution. Furthermore, although most symptoms of hypocalcemia could be relieved within months, some may persist for years or even lifetime, which would seriously jeopardize patients’ life quality. Because patients choosing the endoscopic approach are largely young females, ETBC should be precautiously recommended and performed, especially when heavy lymph node involvement is detected preoperatively.
There are limitations to this study. First, although the follow-up time was sufficient to identify patients with permanent hypoparathyroidism, it was not long enough to observe recurrence. Therefore, we could not analyze the long-term clinical outcome, which is crucial to evaluate a new technique. Second, the number of enrolled patients was not large enough. In fact, most cases of ETBC were carried out within the last 2 years in our institution. However, we did observe a marked difference between the ETBC and open surgery groups.
Conclusion
Although ETBC is generally considered as a safe procedure for patients with thyroid carcinoma, this approach may increase the risk of transient hypoparathyroidism compared with conventional open surgery. We recommend that ETBC should be performed with caution, especially in the case of heavy lymph node involvement.
Abbreviations
- CND:
-
Central neck dissection
- LND:
-
Lateral neck dissection
- ETBC:
-
Endoscopic thyroidectomy with bilateral central neck dissection
- PTH:
-
Parathyroid hormone
- POD1:
-
Postoperative day 1
- RLN:
-
Recurrent laryngeal nerve
- FNA:
-
Fine-needle aspiration
References
J. Jin, R. Phitayakorn, S.M. Wilhelm, C.R. McHenry, Advances in management of thyroid cancer. Curr. Probl. Surg. 50(6), 241–289 (2013)
D.S. Cooper, G.M. Doherty, B.R. Haugen, R.T. Kloos, S.L. Lee, S.J. Mandel, E.L. Mazzaferri, B. McIver, F. Pacini, M. Schlumberger, S.I. Sherman, D.L. Steward, R.M. Tuttle, Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11), 1167–1214 (2009)
L. Davies, H.G. Welch, Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 295(18), 2164–2167 (2006)
S. Chindavijak, Prediction of hypocalcemia in postoperative total thyroidectomy using single measurement of intra-operative parathyroid hormone level. J. Med. Assoc. Thail. 90(6), 1167–1171 (2007)
L. Yip, M.N. Nikiforova, J.Y. Yoo, K.L. McCoy, M.T. Stang, M.J. Armstrong, K.J. Nicholson, N.P. Ohori, C. Coyne, S.P. Hodak, R.L. Ferris, S.O. LeBeau, Y.E. Nikiforov, S.E. Carty, Tumor genotype determines phenotype and disease-related outcomes in thyroid cancer: a study of 1510 patients. Ann. Surg. 262(3), 519–525 (2015)
T. Reeve, N.W. Thompson, Complications of thyroid surgery: how to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J. Surg. 24(8), 971–975 (2000)
G. Agarwal, V. Aggarwal, Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review. World J. Surg. 32(7), 1313–1324 (2008)
H. Yan, Y. Wang, P. Wang, Q. Xie, Q. Zhao, “Scarless” (in the neck) endoscopic thyroidectomy (SET) with ipsilateral levels II, III, and IV dissection via breast approach for papillary thyroid carcinoma: a preliminary report. Surg. Endosc. 29(8), 2158–2163 (2015)
M. Gagner, Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br. J. Surg. 83(6), 875 (1996)
C.M. Song, Y.H. Cho, Y.B. Ji, J.H. Jeong, D.S. Kim, K. Tae, Comparison of a gasless unilateral axillo-breast and axillary approach in robotic thyroidectomy. Surg. Endosc. 27(10), 3769–3775 (2013)
W.T. Ng, Endoscopic thyroidectomy in China. Surg. Endosc. 23(7), 1675–1677 (2009)
K.N. Park, S.H. Cho, S.W. Lee, Nationwide multicenter survey for current status of endoscopic thyroidectomy in Korea. Clin Exp Otorhinolaryngol 8(2), 149–154 (2015)
B. Abboud, Z. Sargi, M. Akkam, F. Sleilaty, Risk factors for postthyroidectomy hypocalcemia. J. Am. Coll. Surg. 195(4), 456–461 (2002)
O. Thomusch, A. Machens, C. Sekulla, J. Ukkat, M. Brauckhoff, H. Dralle, The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: a multivariate analysis of 5846 consecutive patients. Surgery 133(2), 180–185 (2003)
H.O. El Malki, R. Abouqal, Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia (Br J Surg 2014; 101: 307-320). Br. J. Surg. 101(7), 883 (2014)
B.H. Lang, M.P. Chow, A comparison of surgical outcomes between endoscopic and robotically assisted thyroidectomy: the authors’ initial experience. Surg. Endosc. 25(5), 1617–1623 (2011)
H. Yoo, B.J. Chae, H.S. Park, K.H. Kim, S.H. Kim, B.J. Song, S.S. Jung, J.S. Bae, Comparison of surgical outcomes between endoscopic and robotic thyroidectomy. J. Surg. Oncol. 105(7), 705–708 (2012)
J. Lee, J.H. Lee, K.Y. Nah, E.Y. Soh, W.Y. Chung, Comparison of endoscopic and robotic thyroidectomy. Ann. Surg. Oncol. 18(5), 1439–1446 (2011)
J.Y. Choi, K.E. Lee, K.W. Chung, S.W. Kim, J.H. Choe, H. Koo do, S.J. Kim, J. Lee, Y.S. Chung, S.K. Oh, Y.K. Youn, Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc 26(4), 948–955 (2012)
S.W. Kang, J.J. Jeong, J.S. Yun, T.Y. Sung, S.C. Lee, Y.S. Lee, K.H. Nam, H.S. Chang, W.Y. Chung, C.S. Park, Gasless endoscopic thyroidectomy using trans-axillary approach; surgical outcome of 581 patients. Endocr. J. 56(3), 361–369 (2009)
Z.Y. Li, P. Wang, Y. Wang, S.M. Xu, L.P. Cao, R.S. Que, Endoscopic thyroidectomy via breast approach for patients with Graves’ disease. World J. Surg. 34(9), 2228–2232 (2010)
Z. Li, P. Wang, Y. Wang, S. Xu, L. Cao, R. Que, F. Zhou, Endoscopic lateral neck dissection via breast approach for papillary thyroid carcinoma: a preliminary report. Surg. Endosc. 25(3), 890–896 (2010)
A. Puzziello, L. Rosato, N. Innaro, G. Orlando, N. Avenia, G. Perigli, P.G. Calo, M. De Palma, Hypocalcemia following thyroid surgery: incidence and risk factors. A longitudinal multicenter study comprising 2631 patients. Endocrine 47(2), 537–542 (2014)
K. Tae, Y.B. Ji, S.H. Cho, K.R. Kim, D.W. Kim, D.S. Kim, Initial experience with a gasless unilateral axillo-breast or axillary approach endoscopic thyroidectomy for papillary thyroid microcarcinoma: comparison with conventional open thyroidectomy. Surg Laparosc Endosc Percutan Tech 21(3), 162–169 (2011)
C.P. Lombardi, M. Raffaelli, P. Princi, S. Santini, M. Boscherini, C. De Crea, E. Traini, A.M. D’Amore, C. Carrozza, C. Zuppi, R. Bellantone, Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery 136(6), 1236–1241 (2004)
A.A. Carr, T.W. Yen, G.G. Fareau, A.K. Cayo, S.M. Misustin, D.B. Evans, T.S. Wang, A single parathyroid hormone level obtained 4 hours after total thyroidectomy predicts the need for postoperative calcium supplementation. J. Am. Coll. Surg. 219(4), 757–764 (2014)
W.S. Halsted, H.M. Evans, The parathyroid glandules. Their Blood supply and their preservation in operation upon the thyroid gland. Ann. Surg. 46(4), 489–506 (1907)
M. Nobori, S. Saiki, N. Tanaka, Y. Harihara, S. Shindo, Y. Fujimoto, Blood supply of the parathyroid gland from the superior thyroid artery. Surgery 115(4), 417–423 (1994)
G. Conzo, D. Pasquali, G. Bellastella, K. Esposito, C. Carella, A. De Bellis, G. Docimo, M. Klain, S. Iorio, S. Napolitano, A. Palazzo, A. Pizza, A.A. Sinisi, E. Zampella, A. Bellastella, L. Santini, Total thyroidectomy, without prophylactic central lymph node dissection, in the treatment of differentiated thyroid cancer. Clinical retrospective study on 221 cases. Endocrine 44(2), 419–425 (2013)
J.A. Goddard, D.L. Steward, Prophylactic central lymph node dissection in differentiated thyroid cancer. Endocrine 44(2), 275–277 (2013)
M.R. Pelizzo, M. Variolo, C. Bernardi, M. Izuzquiza, A. Piotto, G. Grassetto, P.M. Colletti, B.I. Merante, Rubello D, Complications in thyroid resurgery: a single institutional experience on 233 patients from a whole series of 4,752 homogeneously treated patients. Endocrine 47(1), 100–106 (2014)
S.P. Balasubramanian, Iatrogenic/post-surgical hypoparathyroidism: where do we go from here? Endocrine 47(2), 357–359 (2014)
D. Xiang, L. Xie, Y. Xu, Z. Li, Y. Hong, P. Wang, Papillary thyroid microcarcinomas located at the middle part of the middle third of the thyroid gland correlates with the presence of neck metastasis. Surgery 157(3), 526–533 (2015)
Acknowledgments
This study was supported by Grants 2013C33134 and 2016C33141 from Science Technology Department of Zhejiang Province.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Xiang, D., Xie, L., Li, Z. et al. Endoscopic thyroidectomy along with bilateral central neck dissection (ETBC) increases the risk of transient hypoparathyroidism for patients with thyroid carcinoma. Endocrine 53, 747–753 (2016). https://doi.org/10.1007/s12020-016-0884-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-0884-y