Abstract
Most pediatric bone diseases result either from mutations of the essential genes for bone development or from abnormalities of mineral homeostasis. With an increase in non-invasive techniques to measure bone mineral density, the number of children with apparent low bone mineral density is rising. Furthermore, a new classification system proposed by the International Society for Clinical Densitometry now considers osteoporosis a valid diagnosis in children. Osteoporosis is a particular problem among children with conditions such as muscular dystrophy, immobilization, and chronic liver diseases and those who received a prolonged course of glucocorticoids. Pharmacologic agents for treatment of osteoporosis were developed primarily to prevent fragility fractures in postmenopausal women, and studies of their efficacy and safety in children are limited. Recent advances have seen new therapies for bone diseases in children; some of these conditions were deemed incurable in the past. This article reviews data regarding mechanism of action, safety, and efficacy of four bone drugs in pediatric patients. These are (1) zoledronic acid, a long-acting bisphosphonate; (2) denosumab, a RANKL inhibitor; (3) asfotase alfa, a synthetic alkaline phosphatase; and (4) burosumab, a monoclonal antibody against FGF23.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone disorders in children compresses into two groups: (1) bone disorders caused by gene mutations that disrupt normal bone development and (2) metabolic bone disorders related to chronic illness or disuse osteopathy. The first group of bone disorders is further classified into dysostoses, skeletal dysplasias, and osteolysis syndromes [1]. Dysostoses result from mutations of genes expressed during skeletal organogenesis. Examples of these diseases include Holt-Oram (TBX5 mutation) and Cousin syndrome (TBX15 mutation). Disruptions of genes expressed during both organogenesis and in postnatal life are responsible for skeletal dysplasias. These conditions are further divided into primary and secondary skeletal dysplasias [1]. In primary skeletal dysplasias, the formation of skeletal tissues is disrupted due to the mutations of genes that are expressed in these tissues, while the abnormalities of external factors such as mineral homeostasis cause secondary skeletal dysplasias [1, 2]. Osteogenesis imperfecta (OI) is the best-known example of primary skeletal dysplasias. Hypophosphatasia and hypophosphatemic rickets are examples of secondary skeletal dysplasias [1, 2]. The third group of genetic syndromes, termed osteolysis, is characterized by normal skeletal development, but bone resorption ensues and eventually leads to disappearance of skeletal tissues. Winchester-Torg syndrome (MMP2 mutation) is one of the most severe forms of osteolysis syndromes [1].
Many children with genetic bone disease suffer from limited mobility related to bone pain and progressive deformity which in turn further accelerates a decline in bone mineral density (BMD). Although advances in molecular diagnosis, particularly whole-exome sequencing, have increased knowledge of mutations responsible for genetic bone disease [3, 4], nonetheless, medical treatment for the majority of these disorders is not available and orthopedic procedures continue to be the mainstay for correction of deformity and alleviation of pain. OI is the most common form of skeletal dysplasia having an incidence of around 1 in 10,000 births [5]. Vertebral compression fractures also occur frequently in skeletal dysplasias, particularly among children with OI. In one cohort, all but one out of 79 children with OI sustained vertebral compression fractures [6]. Hence, considerable attention has focused on development of treatment for OI.
In 2019, the International Society for Clinical Densitometry (ISCD) established a definition of osteoporosis in children and screening by dual-energy X-ray absorptiometry (DXA) of children who are at risk for skeletal fractures [7]. The establishment of normative data for BMD in children has allowed wider and more accurate assessment of bone mineral density in chronic medical conditions in children [8, 9].
Anti-resorptive agents, including zoledronic acid and denosumab, have been used to reduce fracture risk. Initially, these agents did not have approval by the US Food and Drug Administration (FDA) for use in children, and their use has been based on a compassionate care [10]. However, advancement in protein pharmaceuticals has led to the development of two new drugs, asfotase alfa and burosumab, that specifically target the mechanism underlying bone disease. Asfotase alfa (Strensiq ®) is a synthetic alkaline phosphatase enzyme which was approved by the FDA in 2015 for treating hypophosphatasia. This was followed in 2018 by the approval for burosumab (Crysvita ®), a monoclonal antibody against FGF-23, for treatment of X-linked hypophosphatemia. This review examines efficacy and safety data of four drugs used now for the treatment of bone disease in children: zoledronic acid, denosumab, asfotase alfa, and burosumab.
Zoledronic Acid
Pharmacology and Biological Activities
Zoledronic acid (ZA) is a member of the bisphosphonate group. It is the most potent agent among its class and is approximately 850 times more potent than pamidronate. After the intravenous administration, it is cleared rapidly from the plasma, and mostly sequestrated in bones with a 100-fold difference in concentration between bone and plasma [11]. Like other bisphosphonates, ZA then undergoes endocytosis by osteoclasts. There, it disrupts osteoclast functions by interfering with post-translational modification of small GTPases such as Ras. These molecules are important regulators of osteoclast cellular processes including apoptosis. By disrupting these molecules, ZA increases apoptosis of osteoclasts and subsequently diminishes bone break down [12]. Due to its long half-life, zoledronic acid can be given once per year. Together with short infusion time (15–30 min), it has become an attractive option for treating osteoporosis in children.
Zoledronic Acid Therapy in Children
The number of reports on the use of ZA in pediatric patients has markedly increased in recent years. However, all of these reports were based on open-labeled studies, and outcomes were compared with baseline data. Only one study had a placebo-controlled group [13].
Osteogenesis Imperfecta
The greatest number of reports on the use of ZA has been in the treatment of OI. The doses of ZA ranged from 0.025–0.1 mg/kg/dose every 3–6 months, depending on the study [14,15,16,17]. Despite the differences in the dose, most studies indicated both favorable outcomes in bone mineral density and reduction in fracture frequency. In one report, the administration of ZA over 2 years in 25 children with OI type III and 8 children with OI type IV significantly reduced the number of fractures and saw an increase in the median (IQR) lumbar spine BMD-Z score from − 1.5 (− 2.1 to − 1.3) to − 0.8 (− 1.0 to − 0.7) [16]. Another study examined changes in mobility among children with OI type I, III, or IV [18]. The authors used the modified Bleck score, a scale ranging from 1 (wheelchair-bound or bedridden) to 9 (able to sprint and participate in sports), to assess the mobility of 14 children with OI type I, III, or IV after ZA infusion. The duration of treatment varied among subjects, but overall, the average modified Bleck score significantly improved from 4 (range 1–9) before treatment to 6 (range 1–9) after treatment [18].
The effect of ZA on the vertebral shape of OI patients with vertebral compression fracture has also been examined [19]. A significant improvement in vertebral column height, determined by morphometric measurements of lumbar spine X-rays, was observed in children with OI types I, III, and IV (average age 8.9 years) 1 year after ZA (Reclast ®) treatment (5 mg annually), and the effect was sustained after 2 years of treatment. Lumbar spine BMD Z-score was also determined in that study. It also improved from − 3.9 ± 1.8 to 0.2 ± 2.1 [19]. Fever and transient hypocalcemia were the only side effects despite high dose of ZA infusion in this study [19]. In a 4-year retrospective study of 31 patients with OI types I, III, IV, V, VI, and VII, discontinuation of ZA treatment after the completion of growth in OI patients resulted neither in a decline in lumbar spine BMD nor an increase in the rate of vertebral compression fractures [20].
Childhood Osteoporosis
A summary of published data on treatment protocols of ZA in pediatric bone disease is presented in Table 1. Among these conditions, treatment of ZA in Duchenne muscular dystrophy comprised the greatest number of reports [53]. The combination of limited mobility and glucocorticoid use put these patients at high risk for long bone and vertebral compression fracture. The effect of ZA on BMD in Duchenne muscular dystrophy is subject of two small reports consisting of 5 and 9 patients per cohort respectively. In one study, patients received ZA at 0.1 mg/kg every 6 months [22], whereas the dose of 0.04 mg/kg every 4 months was used in another report [23]. Both studies indicated modest improvement of lumbar spine BMD Z-score. In the study using the ZA dose of 0.04 mg/kg every 4 months, the vertebral height ratios of patients who had a history of vertebral fractures stabilized or improved in some patients after receiving ZA [22].
The benefits of ZA therapy in patients with spinal muscular atrophy (SMA), another neurodegenerative disease that results in immobilization, has also been reported [24]. Although BMD Z-score at the lateral distal femur did not change, the average number of fractures significantly decreased from 1.4 per year to 0.1 per year after 2 years of treatment of SMA patients with ZA [24].
The only randomized, double-blinded, placebo-controlled study of ZA in childhood osteoporosis was in patients with Crohn’s disease who had received a prolonged course of glucocorticoids. Seven patients were treated with ZA. Six patients served as controls. After a single infusion of 0.066 mg/kg of ZA, lumbar spine BMD Z-score was significantly better at 6 and 12 months after the therapy compared with that of controls [13]. Figure 1a and b indicates a marked improvement in vertebral compression fractures in a patient who received ZA for 1 year after a prolonged course of glucocorticoid therapy at the author’s institution. More extensive studies are needed to establish a benefit from the use of ZA to treat childhood osteoporosis.
a Lateral spine radiogram of a 13-year-old male showing vertebral compression fractures due to a prolonged course of glucocorticoids. b Spine radiogram of the same patient 1 year after a single dose of zoledronic acid infusion at 0.05 mg/kg. Vertebral column height increased particularly in the lumbar region (arrow heads). c Knee radiogram of a 3-year-old boy with childhood hypophosphatasia showing poor mineralization and tongue-shaped radiolucency. d After 18 months of asfotase alfa therapy, bone mineralization improved significantly. The tongue-shaped radiolucent areas are now replaced with mineralized tissue
Safety of Zoledronic Acid in Children
Serious side effects of ZA such as atypical fracture or osteonecrosis of the jaw have not been reported in children. Common side effects include acute phase reactions and abnormalities of serum calcium or phosphorus. Hypophosphatemia occurred in 25.2% of patients in a cohort of 80 pediatric patients who received ZA infusion (a total of 204 infusions) for treatment of various bone diseases [21]. The dose of ZA ranged from 0.0125 to 0.05 mg/kg. Sixteen percent of patients in the study developed hypocalcemia although all patients received calcium and calcitriol before the first dose of ZA and in the subsequent infusions. Acute-phase reactions (fever, myalgia, bone pain, or headache) also occurred in 19% of patients. Two patients developed symptomatic hypocalcemia that required intravenous calcium infusion. The frequency of all adverse effects significantly declined with subsequent infusions [21]. Adverse effects were also less frequent in patients who had previously received other bisphosphonates [21]. Similar adverse effects such as acute phase reactions, hypophosphatemia, and hypocalcemia that were transient and responded well to treatments have also been reported in other smaller studies [14, 16,17,18, 22, 23].
Denosumab
Pharmacology and Biological Activities
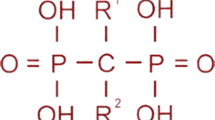
Denosumab is a human monoclonal antibody that binds to the receptor activator of NF-κB ligand (RANKL). RANKL is expressed in osteoblasts, osteocytes, bone marrow stromal cells, and activated T cells. Binding of RANKL to RANK present on osteoclast precursor cells induces osteoclastogenesis [54]. Osteoprotogerin (OPG), secreted by osteoblasts, osteocytes, and T and B cells, binds to RANKL and inhibits RANK-RANKL activation. The ratio of RANKL to OPG is an important indicator of bone homeostasis. High RANKL/OPG ratio, observed in several bone diseases such as osteoporosis, favors osteoclastogenesis and bone resorption [54]. Similar to OPG, denosumab inhibits the RANK-RANKL binding, suppresses osteoclastogenesis, and decreases bone resorption [55].
The Fracture Reduction Evaluation of Denosumab (FREEDOM) study was the first large-scale randomized placebo-controlled study that showed the effectiveness of denosumab in the reduction of fracture in osteoporotic women [54]. Following the publication of the FREEDOM studyin 2010, the FDA approved denosumab for a treatment of osteoporosis in postmenopausal women and men with high risk of fracture, and for treatment of bone metastases from solid tumors. The pharmacokinetics of denosumab has been extensively studied in groups of patients. Denosumab exerts a dose-dependent effect after the subcutaneous administration. The effective inhibition of RANKL was achieved at a dose of 60 mg every 6 months in women with osteoporosis regardless of the weight. More than 97% occupancy of RANKL is achieved at a dose of 120 mg every 4 weeks in cancer patients with bone metastases [56, 57]. The current regimens of denosumab are based on these studies. Pharmacokinetic studies of denosumab in children have not been published and are lacking, and there is currently no FDA-approved indication for pediatric use. Reports on the use of denosumab in children have been done under research protocols.
Denosumab Use in Children
Fibrous Dysplasia
Bone cells in fibrous dysplasia lesion highly express RANKL, and this makes denosumab an appealing choice of treatment in this condition. The first report on the use of denosumab in children was in a 9-year-old boy with fibrous dysplasia from McCune-Albright syndrome [25]. The patient received monthly injection of denosumab starting at 1 mg/kg with an incremental increase of 0.25 mg/kg every 3 months. Seven months after the beginning of treatment, there was a substantial reduction in pain, and a decline in bone turnover markers and tumor growth rate. Treatment was discontinued at the seventh month because patient sustained a fracture related to traumatic injury. Rebound hypercalcemia and an increase in the level of bone turnover markers occurred after the discontinuation of the treatment [25]. In a separate study, denosumab, 60 mg every 3 months, was effective in reducing pain in a 20-year-old patient who was diagnosed with monostotic fibrous dysplasia of the left mandible at 11 years of age [26]. Although no prospective study in children with fibrous dysplasia has been published, a recent prospective study on the use of denosumab in adult patients with fibrous dysplasia showed promising results. Twelve patients (28–68 years of age) who had not responded to bisphosphonate therapy received 60 mg of denosumab every 3 months. Four patients had McCune-Albright syndrome, seven patients had polyostotic, and one had monostotic fibrous dysplasia. After 15 months of treatment, the levels of bone turnover markers significantly reduced, and ten patients reported a significant reduction in pain [27].
Osteogenesis Imperfecta
Children with OI (type I, III, and IV) had higher serum RANKL level compared with healthy controls [58]. The number of immature osteoblasts in the skeleton of transgenic mice with OI phenotypes (oim/oim) was greater than wild-type littermates. The immature osteoblasts also expressed a higher level of RANKL/OPG ratio, and co-culture of these cells with bone marrow–derived non-adherent monocytes resulted in increased osteoclast differentiation [59]. Both studies suggest that the activation of RANK-RANKL system attributes to higher bone resorption observed in OI, and therefore, the inhibition of RANKL by denosumab may provide clinical improvement in OI patients.
The first use of denosumab in OI was reported in patients with OI type VI, a rare autosomal recessive form of OI caused by mutation of the SERPINF1 gene [28]. Children with OI type VI respond poorly to bisphosphonate because the large amount of unmineralized osteoid provides a poor docking site for the bisphosphonate molecule [60]. Four children with OI type VI received denosumab at the dose of 1 mg/kg every 3 months. All patients tolerated the injection without any side effects, and bone resorption markers normalized after each injection. However, bone resorption markers returned to the pre-treatment level at around 6–8 weeks. Despite this, in the follow-up report, there was a significant increase in the vertebral column height in segments with a compression fracture at baseline after 2 years of treatment. In addition, all patients had improvement in mobility score and a reduction in the number of fractures [29]. Nonetheless, other studies have questioned the efficacy of denosumab in OI type VI. In a case-series of 13 patients with OI type VI, when treatment was changed from bisphosphonate to denosumab (1 mg/kg every 3 months) in four patients, there were no clear benefits of denosumab after a follow-up period of 3 years. In particular, the median number of femur and tibia fractures in the last 2 years of treatment was similar in bisphosphonate and denosumab treatments [30]. With respect to the pharmacodynamics, two studies reported that the duration of action of denosumab in children with OI type VI was shorter than 3 months, much shorter than the duration of action in postmenopausal women. In one report, the number of osteoclasts in the iliac bone biopsy specimen of a patient with OI type VI began to increase 3 months after the last dose of denosumab [31]. In the second report, a rapid decline in lumbar spine BMD Z-score was noted in two patients with OI type VI whose denosumab injection was switched from every 3 to every 6 months [61].
With respect to treatment of other types of OI with denosumab, ten patients with OI type I, III, or IV prospectively received denosumab (1 mg/kg) every 12 week months for 36 weeks. Although the average lumbar spine BMD Z-score significantly increased from − 2.2 to − 1.27, the treatment did not result in an improvement in the mobility scores [62].
In light of the limited number of studies and their conflicting results, it is difficult to draw a conclusion of the effectiveness of denosumab as a single agent for treatment of OI. Additional large-scale and long-term studies are needed [63].
Giant Cell–Rich Lesions
This group of disease consists of giant cell tumor of the bone, aneurysmal bone cyst, and central giant cell granuloma. Although each of these tumors has distinct histological features, they have in common the presence of osteoclast-like giant cells. These cells express high-level RANKL suggesting a possible benefit of denosumab therapy. In 2013, the FDA approved the use of denosumab in giant cell tumor of the bone in adults and skeletally mature adolescents [64]. The peak incidence of giant cell tumor among adolescents is between 13 and 19 years of age, and common sites are the proximal tibia, vertebra, and pelvis [32]. The growth of tumor can result in pain, nerve compression, and fractures. Although surgical removal of the lesion is the principal treatment, denosumab has been used in patients with metastatic, recurrence, or unresectable tumor. Case-series reports have described the use of denosumab in seven adolescents with giant cell tumor of the bone [32,33,34,35,36]. Three patients had pulmonary metastasis [34, 35]. In all reports, the initial dose was 120 mg weekly for 1 month and followed by 120 mg every 4 weeks. Denosumab treatment resulted in a significant decrease in the tumor size and the disappearance of giant cells [32,33,34,35,36]. Pulmonary metastatic nodules decreased in size in all three patients, and in one patient, some nodules disappeared [34, 35].
Aneurysmal bone cyst is a benign bone tumor that presents as a single lesion with internal septations. Most patients present before 20 years of age, common sites are long bones, vertebra, and pelvis [40]. Surgical resection is the mainstay of the therapy but may not be possible in some patients due to the location of the tumor. Similar to giant cell tumor of the bone, aneurysmal bone cyst contains large number of osteoclast-like giant cells [40]. The first use of denosumab in two children with aneurysmal bone cyst was reported in 2013 [41]. Three additional case-series reports with a total of 19 affected children were later published [40, 42, 43]. In three of these reports, the dose of denosumab was 70 mg/m2 with a maximum dose 120 [40, 41, 43], whereas one study used a fixed dose of 120 mg [42]. Patients received a weekly injection during the first month, and then monthly injections. The duration of treatment ranged from 4 months to 2 yearsdepending on the clinical response. Treatment relieved pain in all patients and significantly improved neurological symptoms among four patients who had nerve compression. Tumor reduced in size in ten patients. However, the lesion recurred in four patients after the discontinuation of the treatment [40,41,42,43].
Central giant cell granuloma is another giant cell–rich bone tumor. It occurs mainly in the maxilla or mandible. Reports of three patients (4, 9, and 12 years old) with central giant cell granuloma who received denosumab have been published [37,38,39]. The dose of denosumab used was similar to the other two types of giant cell-rich tumors. Two patients were treated with denosumab because they had a poor response to other medical treatments. One patient received denosumab as a primary therapy. Tumor size significantly reduced in all patients, and none of them required surgery [37,38,39].
Juvenile Paget’s disease is a rare debilitating bone disease caused by an inactivating mutation of TNFRSF11B gene encoding OPG. Lack of OPG causes unregulated bone turnover and subsequently severe and progressive bone deformities [65]. In a single report, an 8-year-old girl with juvenile Paget’s disease received two doses of denosumab (0.5 mg/kg) 7 weeks apart. Bone turnover markers, including serum bone-specific alkaline phosphatase, osteocalcin, and urine N-telopeptides, rapidly declined after the injections [44]. The treatment was discontinued after the second dose due to severe hypercalcemia. However, the effect of denosumab on bone deformities could not be determined because of the short course of therapy [44].
Safety of Denosumab in Children
Although hypocalcemia can occur, it is less frequent in children who received denosumab than it is in children who received zoledronic acid. By contrast, hypercalcemia occurred in many patients who received denosumab, and was often severe and necessitated the bisphosphonate therapy [25, 31, 34, 40, 42, 62, 66, 67]. Although sometimes found during treatment [61], hypercalcemia typically occurred after the discontinuation possibly due to rebound osteoclastic activities in highly active bones of pediatric patients [55]. Denosumab may exert only cytostatic effect on bone cells, and when RANKL becomes immediately available after the discontinuation of denosumab, osteoclastogenesis resumes swiftly causing the rebound effects [54]. Hypercalcemia was also more common in patients with giant cell–rich lesions who received higher dose and more frequent injections of denosumab [39, 66, 67]. It was also suggested that a gradual spacing out of the denosumab injections before discontinuing the treatment may prevent rebound hypercalcemia [39]. For these reasons, serum calcium should be closely monitored in patients who receive denosumab. Osteonecrosis of the jaw was reported in a 19-year-old patient who received denosumab for 4 years for giant cell tumor of the bone [36].
Concern about the lasting effects of denosumab on the growth plates has been raised because of its inhibitory effects on growth plates of rodents and primates, and the finding of dense sclerotic bands in the metaphyseal areas in children who received denosumab [55, 68]. However, a histological exam of the sclerotic bands revealed that these were calcified cartilage derived from unresorbed primary spongiosa. The bands also migrated away from the growth plates after the treatment was stopped indicating that the linear bone growth had resumed [69].
Asfotase Alfa
Pharmacology and Biological Activities
Asfotase alfa is a human recombinant tissue non-specific alkaline phosphatase (TNSALP) fusion protein. It consists of the catalytic domain of TNSALP, the Fc portion of human IgG and a deca-asparatate oligopeptide domain [70]. The addition of deca-aspartate oligo domain increases the binding affinity of the protein for hydroxyapatite in the bones [70]. In vitro study indicated that the binding affinity of asfotase alfa to hydroxyapatite is 32-fold greater than the native enzyme [71]. The main function of TNSALP is the hydrolysis of inorganic pyrophosphate into organic phosphate needed for bone mineralization. TNSALP is also necessary for metabolism of vitamin B6. Mutations in the TNSALP gene (also named ALPL) cause hypophosphatasia, a condition marked by a subnormal level of serum alkaline phosphatase and defective bone mineralization [72]. Asfotase alfa was approved by the FDA in 2015 as a treatment of hypophosphatasia, and currently, it is the only treatment for hypophosphatasia.
Asfotase alfa exerts linear pharmacokinetics after subcutaneous injection, and the average elimination half-life of asfotase alfa is 2.3 days. Bodyweight affects the volume of distribution and clearance, and therefore the current dosing regimen is based on patient’s weight [70, 73].
Asfotase Alfa Use in Children
Perinatal and Infantile Hypophosphatasia
Hypophosphatasia is classified into five types based on the age of onset and severity [72]. Mutations that severely affect enzyme functions result in the perinatal and infantile forms, most of the cases being inherited in a recessive form [74]. Patients with the perinatal form frequently die from respiratory failure or vitamin B6–dependent seizures [75]. Patients with the infantile form usually present before 6 months of age with rickets, failure to thrive, hypotonia, epilepsy, and craniosynostosis [72]. Patients with the infantile form can also experience deterioration of respiratory status and die of respiratory insufficiency [45].
The first clinical trial of asfotase alfa was investigated in 11 patients, ranging from 2 weeks to 3 years of age, with the perinatal and infantile form of hypophosphatasia [45]. Subjects received the first dose intravenously at 2 mg/kg followed by subcutaneous injection at 1 mg/kg three times per week. Skeletal mineralization significantly improved by 24 weeks of treatment and continued to improve until the end of the observation period at 48 weeks. Ten patients were receiving ventilatory support. At the end of the study, six patients no longer required respiratory support because of marked improvement in the mineralization of the thoracic skeleton [45]. Motor function also improved in all patients who were able to complete the functional assessments. One patient who withdrew from the study had a substantial demineralization of ribs 14 months after the discontinuation of treatment. Biochemical analysis indicated a significant reduction in serum pyridoxal 5′-phosphate (PLP) and inorganic pyrophosphate, the direct substrates of TNSALP following treatment with asfotase alfa [45]. As inorganic pyrophosphate inhibits mineralization, its reduction has been a factor in bone healing [72]. On the basis of this study, asfotase alfa was approved by the FDA in 2015 for treatment of hypophosphatasia.
The study continued after FDA approval of the medication. After 7 years of treatment, the skeletal healing was sustained. None of the nine patients who completed the study required reinitiation of ventilatory support. Treatment with asfotase alfa had only a modest effect on height. Baseline median height Z-score was − 3.72, and the median height Z-score in the third year increased to − 2.33 but then decreased to − 3.02 at the end of the study [46].
A comparative study published in 2016 further supported the effect of asfotase alfa on the survival of patients with the perinatal and infantile form of hypophosphatasia [47]. In this study, the clinical outcomes of 37 patients with perinatal and infantile hypophosphatasia who received asfotase alfa were compared with the history controls consisting of 48 patients with similar chronological age and the disease characteristics [47]. The survival rate at 1 and 5 years of age was 95 and 84% respectively in the treatment group compared with only 42 and 27% in the historical control group. Furthermore, 76% of the patients in the treatment group who initially required ventilatory support survived compared with only 5% of the patients in the control group [47]. Another large multinational clinical trial which enrolled 69 patients with hypophosphatasia whose diagnosis was made before 6 months showed similar efficacy of asfotase alfa in improving bone mineralization and respiratory status [76]. Forty-six percent of patients who required respiratory support at the start of trial no longer required it after a median duration treatment of 2 years. Patients who did not respond to the treatment had a higher rate of developing neutralizing antibody to asfotase alfa [76].
Childhood Hypophosphatasia
Patients with this form of hypophosphatasia often present after 6 months. The clinical manifestations include premature loss of deciduous teeth, rickets, bowed legs, and craniosynostosis. Radiographic studies of long bones often reveal bone hypomineralization and tongue-shaped radiolucency extending from physes into metaphyses [72, 77]. Decreased muscle strength and the delay in walking are also common [72, 77]. The functional analysis of ALPL gene mutations in this group of patients indicated that the mutated protein retained some residual activities [74]. Childhood hypophosphatasia inherits in a dominant fashion in 46 to 66% of patients compared with only 3 to 5% perinatal and infantile hypophosphatasia [77, 78].
Asfotase alfa treatment of childhood hypophosphatasia was first tried in 13 children ranging from 6 to 12 years of age [48]. Bone mineralization significantly increased after 6 months of treatment. Improvements in motor functions, strength, and agility, and reduction in pain were also noted as early as 6 months of treatment and sustained throughout the five-year duration of the study [48]. Seven out of 13 children (64%) in the extension study report also developed craniosynostosis, which was thought to be a complication of hypophosphatasia, and treatment with asfotase alfa could not prevent it [46]. Figure 1c and d illustrate the knee radiograms of a 3-year-old patient with hypophosphatasia, who is followed at the author’s institution, showing marked improvement of bone mineralization after asfotase alfa treatment for 18 months.
The therapeutic effects of asfotase alfa in adolescents with hypophosphatasia were also reported in a trial consisting of six patients between 13 and 18 years of age. The study also included 13 adult patients [49]. The patients received asfotase alfa at 2.1–3.5 mg/kg/week during the first 6 months, followed by 0.5 mg/kg/week for six more months. The dose was later increased to 1 mg/kg/week after the first year. At the end of the study, only four adolescents completed the study. Serum PLP and inorganic pyrophosphate were significantly reduced after the first 6 months of treatment and sustained throughout the 5-year duration of study. Transiliac bone biopsy also indicated a decrease in mineralization lag time at 1 year after the start of treatment. The total distance on the 6-min walking test also increased significantly and indicated functional improvement [49]. However, the study did not perform a subgroup analysis among adolescent patients. Rapid demineralization of long bones was also reported in an adolescent with hypophosphatasia after the patient stopped the treatment for 1 year [79].
Safety of Asfotase Alfa in Children
Asfotase alfa is well-tolerated in most patients in all reports. Severe allergic reactions that led to the discontinuation of the therapy occurred in a single case in each of the two studies [46, 49]. The most common side effect of asfotase alfa was injection site reactions; erythema, hematoma and hypertrophy, all of which were mild and improved when the injection site was switched [46, 48, 49]. Acute phase reactions such as pyrexia, flu-like symptoms, vomiting, and diarrhea were more common among young patients, but most of these reactions occurred during the original study when asfotase alfa was given intravenously [46].
Ectopic calcifications particularly nephrocalcinosis and ocular calcifications also occurred in some patients, and the latter was more common among children and adolescents. None of the patient developed renal insufficiency or visual impairment during the study [46, 49]. One patient developed soft tissue calcification at the injection sites, which resolved after the location of injection was changed [46]. The current guidelines of the treatment with asfotase alfa recommend a renal ultrasound and ophthalmologic examination to screen for these two complications [80]. Closed monitoring of serum calcium in perinatal and infantile hypophosphatasia is also recommended although severe hypocalcemia from asfotase alfa treatment has not been reported [80].
Burosumab
Pharmacology and Biological Activities
Burosumab is a fully human recombinant IgG1 monoclonal antibody that binds and neutralizes fibroblast growth factor 23 (FGF23) [81]. FGF23 is produced by osteocytes and plays an essential role in phosphate homeostasis. The expression of sodium-phosphate co-transporters in the renal tubules is inhibited by FGF23, leading to an increase in renal phosphate excretion. FGF23 also suppresses 1-alpha hydroxylase and therefore suppresses the formation of calcitriol, an important factor for intestinal phosphate absorption [82]. Hereditary conditions that lead to an elevated serum FGF23 level will result in hypophosphatemia, rickets, osteomalacia, and skeletal deformities. Burosumab was created to antagonize the circulating FGF23 in X-linked hypophosphatemia (XLH), the most common form of hereditary renal phosphate wasting disorders [50].
After subcutaneous injection, burosumab is absorbed slowly with time to maximum concentration between 8 to 10 days. The serum concentration of burosumab also shows a linear relationship with the dose. The terminal half-life is approximately 19 days. Burosumab is most likely broken down in the body without direct excretion [81]. In adults, a single injection every 4 weeks sufficiently maintained the pharmacologic effects of burosumab [83]. However, the results of the phase 2 clinical trial in children indicated that serum phosphorus levels are less fluctuated in patients who received burosumab every 2 weeks [50]. Burosumab received approval by the FDA in April 2018. The current regimen in children younger than 18 years is 0.8 mg/kg (minimum of 10 mg and maximum of 90 mg) every 2 weeks [81].
Burosumab Use in Children
Burosumab is approved for the treatment of XLH in patients who are 1 year and older [81]. Inactivating mutations of phosphate-regulating endopeptidase homolog X-linked (PHEX) gene cause an elevation of serum FGF23 level, which results in hypophosphatemia and eventually leads to rickets and bone deformities. Other common problems include poor growth, delayed motor skills, skull abnormalities (dolicocephaly, frontal bossing, and craniosynostosis), joint pain, excessive dental caries, and tooth abscesses [82, 84]. Serum chemistry analysis typically shows hypophosphatemia, elevated alkaline phosphatase, normal calcium, normal parathyroid hormone, and low or normal 1,25-dihydoxyvitamin D [82]. Nephrocalcinosis occurs frequently and is thought to be a complication of conventional therapy with phosphorus supplement and calcitriol [84].
The first clinical trial of burosumab in children with XLH was published in 2018 [50]. Fifty-two children between 5 and 12 years of age with XLH, who previously received conventional therapy, were randomly assigned to receive burosumab every 2 or every 4 weeks for 64 weeks. The dose was gradually escalated in the first 16 weeks to achieve optimal fasting serum phosphorus and then continued for an additional 48 weeks [50]. A decrease in the Thacher rickets severity score, assessed by radiographic studies, was apparent at the 40th week compared with that of the baseline in both regimens. Significant increase in serum phosphorus, renal tubular reabsorption, and serum 1,25-dihydroxyvitamin D, and reduction in serum alkaline phosphatase from the baseline were also observed at the 40th week. However, burosumab injection every 2 weeks resulted in a higher and less fluctuating serum phosphorus level [50]. The height Z-score, physical functions, and pain score modestly improved from the baseline at the end of the study period [50].
Based on the data from the first trial, the subsequent study of younger children with XLH used the dosing regimen of 0.8 mg/kg every 2 weeks with an increment to 1–2 mg/kg every 2 weeks if serum phosphorus prior to the next dose remained below the lower limit of normal range. Thirteen children between 1 and 4 years of age were enrolled in the study, which continued for a total of 64 weeks. Similar to the first trial in older children, Thacher rickets severity score significantly decreased at the 40th-week assessment. The average serum phosphorus normalized at the 40th week and sustained until the end of the study. Serum 1,25-dihydroxyvitamin D and alkaline phosphatase also normalized at the same time-point. However, there was no significant increase in height Z-score at the end of trial [51].
The results of the multinational phase 3 study comparing the efficacy of burosumab to the conventional treatment with oral phosphate and calcitriol or alfacalcidiol were published in 2019 [52]. Children between 1 and 12 years of age with XLH who were previously treated with conventional therapy were randomly assigned to continue with the conventional therapy or to switch to burosumab (0.8 mg/kg every 2 weeks) for a duration of 64 weeks. Thirty-two patients in conventional therapy group and 29 patients in the burosumab group completed the study. At baseline, the average Thacher rickets severity scores were similar in both groups. The scores significantly decreased among patients who received burosumab compared with those among patients in the conventional therapy group at the 40th and 64th week of therapy [52]. Significantly lower serum alkaline phosphatase level in the burosumab group was achieved at the 16th week, and the level normalized at the 40th week of the study. Serum phosphorus significantly increased in the burosumab group at the 4th week of treatment and maintained throughout the duration of the study. The changes in height Z-score and 6-min walking test distance from baseline were also significantly greater among patients who received burosumab compared with that of the conventional group [52]. Despite the remarkable outcomes of this study, several arguments regarding the trial design were raised. At the start of the trial, rickets was moderate to severe in all patients despite receiving conventional therapy, and it was likely that the continuation of this regimen would not change the outcomes. The average doses of phosphate and active vitamin D in the conventional group also varied considerably, and this could have an impact on the healing of rickets [85].
Safety of Burosumab in Children
The most common adverse events from these three trials were acute phase reactions to the injection: pyrexia, headache, cough, nasal congestion, vomiting, and diarrhea [50,51,52]. These reactions were self-limited and were more common among young children [52]. Injection site reactions, such as erythema, pain rash, and swelling, were also common but resolved spontaneously and did not lead to the discontinuation of the treatment [50,51,52]. Several patients had nephrocalcinosis at the start of the trial, but the condition did not worsen in any patient, and none of the patients developed new lesion at the end of the study. Ectopic calcification was also not detected during the study period [50, 52].
Dental complications, caries, and abscess occurred between 31 and 54% patients who received burosumab [51, 52]. Interestingly, the incidence of these dental complications was higher among patients who received burosumab than those who received conventional therapy in the phase 3 trial [52]. The exact reasons of this finding are uncertain, but it is hypothesized that there might be other biologically active peptides that were elevated due to PHEX deficiency, and their levels will not be affected by burosumab treatment. It also suggested that conventional therapy might have direct dental benefits [85]. Although both dental caries and abscess are not a contraindication for the treatment, particular attention should be made to detect these common dental complications among XLH patients who are receiving burosumab.
Conclusions
Novel therapies are now available to treat rare pediatric bone diseases. Many of these drugs are synthetic protein molecules that specifically target the underlying mechanism of the disease, and because of this reason, survival or healing of deformities is now possible in certain conditions such as perinatal lethal hypophosphatasia or XLH. Although currently available data indicate that certain drugs, such asfotase alfa and burosumab, are effective in treating its specific condition, others, such as zoledronic acid or denosumab, show somewhat modest efficacy in treating childhood osteoporosis. One of the possible explanations is the lack of randomized placebo-controlled trials with uniformed regimens to produce reliable results. Physicians who treat childhood osteoporosis are still required to use careful judgment when deciding on the choice and the dose of treatment. Newer biologic agents are also being developed to treat genetic bone diseases. Four different pharmaceutical companies are currently developing a C-type natriuretic peptide analog that antagonizes FGFR3 signaling as a treatment for achondroplasia. Romosozumab, a neutralizing monoclonal antibody against sclerostin, was recently approved for treating postmenopausal osteoporosis. Sclerostin is an inhibitor of Wnt/β-catenin signaling, a central pathway in bone formation, and the neutralization of sclerostin leads to an increase in bone mass. Because romosozumab can modulate bone formation, it can potentially become a new therapeutic option for genetic bone diseases with low bone mineral density. These were a few examples of the recent advancements in bone drug developments. We can certainly expect to see the surge in the number of new drugs for treating bone diseases in the near future.
References
Spranger JW, Brill PW, Nishimura G, Superti-Furga A, Unger S. Introduction. In: Spranger JW, Brill PW, Nishimura G, Superti-Furga A, Unger S, editors. Bone dysplasias. New York: Oxford University Press; 2012.
Geister KA, Camper SA. Advances in skeletal dysplasia genetics. Annu Rev Genomics Hum Genet. 2015;16(1):199–227. https://doi.org/10.1146/annurev-genom-090314-045904.
Dubail J, Brunelle P, Baujat G, Huber C, Doyard M, Michot C, et al. Homozygous loss-of-function mutations in CCDC134 are responsible for a severe form of osteogenesis imperfecta. J Bone Miner Res. 2020. https://doi.org/10.1002/jbmr.4011.
Rafati M, Mohamadhashem F, Hoseini A, Hoseininasab F, Ghaffari SR. A novel ACVR1 mutation detected by whole exome sequencing in a family with an unusual skeletal dysplasia. Eur J Med Genet. 2016;59(6–7):330–6. https://doi.org/10.1016/j.ejmg.2016.05.007.
Marini JC, Forlino A, Bachinger HP, Bishop NJ, Byers PH, Paepe A, et al. Osteogenesis imperfecta. Nat Rev Dis Primers. 2017;3(1):17052. https://doi.org/10.1038/nrdp.2017.52.
Lindahl K, Kindmark A, Rubin CJ, Malmgren B, Grigelioniene G, Soderhall S, et al. Decreased fracture rate, pharmacogenetics and BMD response in 79 Swedish children with osteogenesis imperfecta types I, III and IV treated with pamidronate. Bone. 2016;87:11–8. https://doi.org/10.1016/j.bone.2016.02.015.
The International For Clinical Densitometry. 2019 ISCD Official Positions – Pediatric. 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-pediatric/.
Bachrach LK, Gordon CM, Section on Endocrinology. Bone densitometry in children and adolescents. Pediatrics. 2016;138(4). https://doi.org/10.1542/peds.2016-2398.
Zemel BS, Leonard MB, Kelly A, Lappe JM, Gilsanz V, Oberfield S, et al. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J Clin Endocrinol Metab. 2010;95(3):1265–73. https://doi.org/10.1210/jc.2009-2057.
Klein GL. Introduction. In: Klein GL, editor. Bone drugs in pediatrics. New York: Springer; 2014.
Biggin A, Munns CF. Bisphosphonates in osteogenesis imperfecta. In: Klein GL, editor. Bone drug in pediatrics. New York: Springer; 2014.
Russell RG. Bisphosphonates: the first 40 years. Bone. 2011;49(1):2–19. https://doi.org/10.1016/j.bone.2011.04.022.
Sbrocchi AM, Forget S, Laforte D, Azouz EM, Rodd C. Zoledronic acid for the treatment of osteopenia in pediatric Crohn’s disease. Pediatr Int. 2010;52(5):754–61. https://doi.org/10.1111/j.1442-200X.2010.03174.x.
Barros ER, Saraiva GL, de Oliveira TP, Lazaretti-Castro M. Safety and efficacy of a 1-year treatment with zoledronic acid compared with pamidronate in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab. 2012;25(5–6):485–91. https://doi.org/10.1515/jpem-2012-0016.
Bowden SA, Mahan JD. Zoledronic acid in pediatric metabolic bone disorders. Transl Pediatr. 2017;6(4):256–68. https://doi.org/10.21037/tp.2017.09.10.
Otaify GA, Aglan MS, Ibrahim MM, Elnashar M, El Banna RA, Temtamy SA. Zoledronic acid in children with osteogenesis imperfecta and Bruck syndrome: a 2-year prospective observational study. Osteoporos Int. 2016;27(1):81–92. https://doi.org/10.1007/s00198-015-3216-9.
Panigrahi I, Das RR, Sharda S, Marwaha RK, Khandelwal N. Response to zolendronic acid in children with type III osteogenesis imperfecta. J Bone Miner Metab. 2010;28(4):451–5. https://doi.org/10.1007/s00774-009-0149-4.
Constantino CS, Krzak JJ, Fial AV, Kruger KM, Rammer JR, Radmanovic K, et al. Effect of bisphosphonates on function and mobility among children with osteogenesis imperfecta: a systematic review. JBMR Plus. 2019;3(10):e10216. https://doi.org/10.1002/jbm4.10216.
Li LJ, Zheng WB, Zhao DC, Yu W, Wang O, Jiang Y, et al. Effects of zoledronic acid on vertebral shape of children and adolescents with osteogenesis imperfecta. Bone. 2019;127:164–71. https://doi.org/10.1016/j.bone.2019.06.011.
Robinson ME, Trejo P, Palomo T, Glorieux FH, Rauch F. Osteogenesis imperfecta: skeletal outcomes after bisphosphonate discontinuation at final height. J Bone Miner Res. 2019;34(12):2198–204. https://doi.org/10.1002/jbmr.3833.
George S, Weber DR, Kaplan P, Hummel K, Monk HM, Levine MA. Short-term safety of zoledronic acid in young patients with bone disorders: an extensive institutional experience. J Clin Endocrinol Metab. 2015;100(11):4163–71. https://doi.org/10.1210/jc.2015-2680.
Sbrocchi AM, Rauch F, Jacob P, McCormick A, McMillan HJ, Matzinger MA, et al. The use of intravenous bisphosphonate therapy to treat vertebral fractures due to osteoporosis among boys with Duchenne muscular dystrophy. Osteoporos Int. 2012;23(11):2703–11. https://doi.org/10.1007/s00198-012-1911-3.
Lim A, Zacharin M, Pitkin J, de Valle K, Ryan MM, Simm PJ. Therapeutic options to improve bone health outcomes in Duchenne muscular dystrophy: zoledronic acid and pubertal induction. J Paediatr Child Health. 2017;53(12):1247–8. https://doi.org/10.1111/jpc.13692.
Nasomyont N, Hornung LN, Wasserman H. Intravenous bisphosphonate therapy in children with spinal muscular atrophy. Osteoporos Int. 2020;31(5):995–1000. https://doi.org/10.1007/s00198-019-05227-9.
Boyce AM, Chong WH, Yao J, Gafni RI, Kelly MH, Chamberlain CE, et al. Denosumab treatment for fibrous dysplasia. J Bone Miner Res. 2012;27(7):1462–70. https://doi.org/10.1002/jbmr.1603.
Eller-Vainicher C, Rossi DS, Guglielmi G, Beltramini GA, Cairoli E, Russillo A, et al. Prompt clinical and biochemical response to denosumab in a young adult patient with craniofacial fibrous dysplasia. Clin Cases Miner Bone Metab. 2016;13(3):253–6. https://doi.org/10.11138/ccmbm/2016.13.3.253.
Majoor BCJ, Papapoulos SE, Dijkstra PDS, Fiocco M, Hamdy NAT, Appelman-Dijkstra NM. Denosumab in patients with fibrous dysplasia previously treated with bisphosphonates. J Clin Endocrinol Metab. 2019;104(12):6069–78. https://doi.org/10.1210/jc.2018-02543.
Semler O, Netzer C, Hoyer-Kuhn H, Becker J, Eysel P, Schoenau E. First use of the RANKL antibody denosumab in osteogenesis imperfecta type VI. J Musculoskelet Neuronal Interact. 2012;12(3):183–8.
Hoyer-Kuhn H, Netzer C, Koerber F, Schoenau E, Semler O. Two years’ experience with denosumab for children with osteogenesis imperfecta type VI. Orphanet J Rare Dis. 2014;9(1):145. https://doi.org/10.1186/s13023-014-0145-1.
Trejo P, Palomo T, Montpetit K, Fassier F, Sato A, Glorieux FH, et al. Long-term follow-up in osteogenesis imperfecta type VI. Osteoporos Int. 2017;28(10):2975–83. https://doi.org/10.1007/s00198-017-4141-x.
Ward L, Bardai G, Moffatt P, Al-Jallad H, Trejo P, Glorieux FH, et al. Osteogenesis imperfecta type VI in individuals from Northern Canada. Calcif Tissue Int. 2016;98(6):566–72. https://doi.org/10.1007/s00223-016-0110-1.
Federman N, Brien EW, Narasimhan V, Dry SM, Sodhi M, Chawla SP. Giant cell tumor of bone in childhood: clinical aspects and novel therapeutic targets. Paediatr Drugs. 2014;16(1):21–8. https://doi.org/10.1007/s40272-013-0051-3.
Bardakhchyan S, Kager L, Danielyan S, Avagyan A, Karamyan N, Vardevanyan H, et al. Denosumab treatment for progressive skull base giant cell tumor of bone in a 14 year old female - a case report and literature review. Ital J Pediatr. 2017;43(1):32. https://doi.org/10.1186/s13052-017-0353-0.
Karras NA, Polgreen LE, Ogilvie C, Manivel JC, Skubitz KM, Lipsitz E. Denosumab treatment of metastatic giant-cell tumor of bone in a 10-year-old girl. J Clin Oncol. 2013;31(12):e200–2. https://doi.org/10.1200/JCO.2012.46.4255.
Reddy K, Ramirez L, Kukreja K, Venkatramani R. Response to denosumab in 2 children with recurrent giant cell tumor of the bone with pulmonary metastasis. J Pediatr Hematol Oncol. 2019;Publish Ahead of Print. https://doi.org/10.1097/MPH.0000000000001654.
Uday S, Gaston CL, Rogers L, Parry M, Joffe J, Pearson J, et al. Osteonecrosis of the jaw and rebound hypercalcemia in young people treated with denosumab for giant cell tumor of bone. J Clin Endocrinol Metab. 2018;103(2):596–603. https://doi.org/10.1210/jc.2017-02025.
Bredell M, Rordorf T, Kroiss S, Rucker M, Zweifel DF, Rostetter C. Denosumab as a treatment alternative for central giant cell granuloma: a long-term retrospective cohort study. J Oral Maxillofac Surg. 2018;76(4):775–84. https://doi.org/10.1016/j.joms.2017.09.013.
Naidu A, Malmquist MP, Denham CA, Schow SR. Management of central giant cell granuloma with subcutaneous denosumab therapy. J Oral Maxillofac Surg. 2014;72(12):2469–84. https://doi.org/10.1016/j.joms.2014.06.456.
Upfill-Brown A, Bukata S, Bernthal NM, Felsenfeld AL, Nelson SD, Singh A, et al. Use of denosumab in children with osteoclast bone dysplasias: report of three cases. JBMR Plus. 2019;3(10):e10210. https://doi.org/10.1002/jbm4.10210.
Kurucu N, Akyuz C, Ergen FB, Yalcin B, Kosemehmetoglu K, Ayvaz M et al. Denosumab treatment in aneurysmal bone cyst: evaluation of nine cases. Pediatr Blood Cancer. 2018;65(4). https://doi.org/10.1002/pbc.26926.
Lange T, Stehling C, Frohlich B, Klingenhofer M, Kunkel P, Schneppenheim R, et al. Denosumab: a potential new and innovative treatment option for aneurysmal bone cysts. Eur Spine J. 2013;22(6):1417–22. https://doi.org/10.1007/s00586-013-2715-7.
Durr HR, Grahneis F, Baur-Melnyk A, Knosel T, Birkenmaier C, Jansson V, et al. Aneurysmal bone cyst: results of an off label treatment with denosumab. BMC Musculoskelet Disord. 2019;20(1):456. https://doi.org/10.1186/s12891-019-2855-y.
Raux S, Bouhamama A, Gaspar N, Brugieres L, Entz-Werle N, Mallet C, et al. Denosumab for treating aneurysmal bone cysts in children. Orthop Traumatol Surg Res. 2019;105(6):1181–5. https://doi.org/10.1016/j.otsr.2019.04.028.
Grasemann C, Schundeln MM, Hovel M, Schweiger B, Bergmann C, Herrmann R, et al. Effects of RANK-ligand antibody (denosumab) treatment on bone turnover markers in a girl with juvenile Paget’s disease. J Clin Endocrinol Metab. 2013;98(8):3121–6. https://doi.org/10.1210/jc.2013-1143.
Whyte MP, Greenberg CR, Salman NJ, Bober MB, McAlister WH, Wenkert D, et al. Enzyme-replacement therapy in life-threatening hypophosphatasia. N Engl J Med. 2012;366(10):904–13. https://doi.org/10.1056/NEJMoa1106173.
Whyte MP, Simmons JH, Moseley S, Fujita KP, Bishop N, Salman NJ, et al. Asfotase alfa for infants and young children with hypophosphatasia: 7 year outcomes of a single-arm, open-label, phase 2 extension trial. Lancet Diabetes Endocrinol. 2019;7(2):93–105. https://doi.org/10.1016/S2213-8587(18)30307-3.
Whyte MP, Rockman-Greenberg C, Ozono K, Riese R, Moseley S, Melian A, et al. Asfotase alfa treatment improves survival for perinatal and infantile hypophosphatasia. J Clin Endocrinol Metab. 2016;101(1):334–42. https://doi.org/10.1210/jc.2015-3462.
Whyte MP, Madson KL, Phillips D, Reeves AL, McAlister WH, Yakimoski A, et al. Asfotase alfa therapy for children with hypophosphatasia. JCI Insight. 2016;1(9):e85971. https://doi.org/10.1172/jci.insight.85971.
Kishnani PS, Rockman-Greenberg C, Rauch F, Bhatti MT, Moseley S, Denker AE, et al. Five-year efficacy and safety of asfotase alfa therapy for adults and adolescents with hypophosphatasia. Bone. 2019;121:149–62. https://doi.org/10.1016/j.bone.2018.12.011.
Carpenter TO, Whyte MP, Imel EA, Boot AM, Hogler W, Linglart A, et al. Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med. 2018;378(21):1987–98. https://doi.org/10.1056/NEJMoa1714641.
Whyte MP, Carpenter TO, Gottesman GS, Mao M, Skrinar A, San Martin J, et al. Efficacy and safety of burosumab in children aged 1-4 years with X-linked hypophosphataemia: a multicentre, open-label, phase 2 trial. Lancet Diabetes Endocrinol. 2019;7(3):189–99. https://doi.org/10.1016/S2213-8587(18)30338-3.
Imel EA, Glorieux FH, Whyte MP, Munns CF, Ward LM, Nilsson O, et al. Burosumab versus conventional therapy in children with X-linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet. 2019;393(10189):2416–27. https://doi.org/10.1016/S0140-6736(19)30654-3.
Bell JM, Shields MD, Watters J, Hamilton A, Beringer T, Elliott M, et al. Interventions to prevent and treat corticosteroid-induced osteoporosis and prevent osteoporotic fractures in Duchenne muscular dystrophy. Cochrane Database Syst Rev. 2017;1:CD010899. https://doi.org/10.1002/14651858.CD010899.pub2.
Faienza MF, Chiarito M, D’Amato G, Colaianni G, Colucci S, Grano M, et al. Monoclonal antibodies for treating osteoporosis. Expert Opin Biol Ther. 2018;18(2):149–57. https://doi.org/10.1080/14712598.2018.1401607.
Boyce AM. Denosumab: an emerging therapy in pediatric bone disorders. Curr Osteoporos Rep. 2017;15(4):283–92. https://doi.org/10.1007/s11914-017-0380-1.
Gibiansky L, Sutjandra L, Doshi S, Zheng J, Sohn W, Peterson MC, et al. Population pharmacokinetic analysis of denosumab in patients with bone metastases from solid tumours. Clin Pharmacokinet. 2012;51(4):247–60. https://doi.org/10.2165/11598090-000000000-00000.
Sutjandra L, Rodriguez RD, Doshi S, Ma M, Peterson MC, Jang GR, et al. Population pharmacokinetic meta-analysis of denosumab in healthy subjects and postmenopausal women with osteopenia or osteoporosis. Clin Pharmacokinet. 2011;50(12):793–807. https://doi.org/10.2165/11594240-000000000-00000.
Brunetti G, Papadia F, Tummolo A, Fischetto R, Nicastro F, Piacente L, et al. Impaired bone remodeling in children with osteogenesis imperfecta treated and untreated with bisphosphonates: the role of DKK1, RANKL, and TNF-alpha. Osteoporos Int. 2016;27(7):2355–65. https://doi.org/10.1007/s00198-016-3501-2.
Li H, Jiang X, Delaney J, Franceschetti T, Bilic-Curcic I, Kalinovsky J, et al. Immature osteoblast lineage cells increase osteoclastogenesis in osteogenesis imperfecta murine. Am J Pathol. 2010;176(5):2405–13. https://doi.org/10.2353/ajpath.2010.090704.
Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley PJ, Travers R. Osteogenesis imperfecta type VI: a form of brittle bone disease with a mineralization defect. J Bone Miner Res. 2002;17(1):30–8. https://doi.org/10.1359/jbmr.2002.17.1.30.
Trejo P, Rauch F, Ward L. Hypercalcemia and hypercalciuria during denosumab treatment in children with osteogenesis imperfecta type VI. J Musculoskelet Neuronal Interact. 2018;18(1):76–80.
Hoyer-Kuhn H, Franklin J, Allo G, Kron M, Netzer C, Eysel P, et al. Safety and efficacy of denosumab in children with osteogenesis imperfect--a first prospective trial. J Musculoskelet Neuronal Interact. 2016;16(1):24–32.
Li G, Jin Y, Levine MAH, Hoyer-Kuhn H, Ward L, Adachi JD. Systematic review of the effect of denosumab on children with osteogenesis imperfecta showed inconsistent findings. Acta Paediatr. 2018;107(3):534–7.
Lipplaa A, Dijkstra S, Gelderblom H. Challenges of denosumab in giant cell tumor of bone, and other giant cell-rich tumors of bone. Curr Opin Oncol. 2019;31(4):329–35. https://doi.org/10.1097/CCO.0000000000000529.
Polyzos SA, Cundy T, Mantzoros CS. Juvenile Paget disease. Metabolism. 2018;80:15–26. https://doi.org/10.1016/j.metabol.2017.10.007.
Gossai N, Hilgers MV, Polgreen LE, Greengard EG. Critical hypercalcemia following discontinuation of denosumab therapy for metastatic giant cell tumor of bone. Pediatr Blood Cancer. 2015;62(6):1078–80. https://doi.org/10.1002/pbc.25393.
Setsu N, Kobayashi E, Asano N, Yasui N, Kawamoto H, Kawai A, et al. Severe hypercalcemia following denosumab treatment in a juvenile patient. J Bone Miner Metab. 2016;34(1):118–22. https://doi.org/10.1007/s00774-015-0677-z.
Kobayashi E, Setsu N. Osteosclerosis induced by denosumab. Lancet. 2015;385(9967):539. https://doi.org/10.1016/S0140-6736(14)61338-6.
Wang HD, Boyce AM, Tsai JY, Gafni RI, Farley FA, Kasa-Vubu JZ, et al. Effects of denosumab treatment and discontinuation on human growth plates. J Clin Endocrinol Metab. 2014;99(3):891–7. https://doi.org/10.1210/jc.2013-3081.
Scott LJ. Asfotase alfa in perinatal/infantile-onset and juvenile-onset hypophosphatasia: a guide to its use in the USA. BioDrugs. 2016;30(1):41–8. https://doi.org/10.1007/s40259-016-0161-x.
Yadav MC, de Oliveira RC, Foster BL, Fong H, Cory E, Narisawa S, et al. Enzyme replacement prevents enamel defects in hypophosphatasia mice. J Bone Miner Res. 2012;27(8):1722–34. https://doi.org/10.1002/jbmr.1619.
Whyte MP. Hypophosphatasia - aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol. 2016;12(4):233–46. https://doi.org/10.1038/nrendo.2016.14.
Scott LJ. Asfotase alfa: a review in paediatric-onset hypophosphatasia. Drugs. 2016;76(2):255–62. https://doi.org/10.1007/s40265-015-0535-2.
Mornet E. Hypophosphatasia. Metabolism. 2018;82:142–55. https://doi.org/10.1016/j.metabol.2017.08.013.
Whyte MP, Leung E, Wilcox WR, Liese J, Argente J, Martos-Moreno GA, et al. Natural history of perinatal and infantile hypophosphatasia: a retrospective study. J Pediatr. 2019;209:116–24 e4. https://doi.org/10.1016/j.jpeds.2019.01.049.
Hofmann CE, Harmatz P, Vockley J, Hogler W, Nakayama H, Bishop N, et al. Efficacy and safety of asfotase alfa in infants and young children with hypophosphatasia: a phase 2 open-label study. J Clin Endocrinol Metab. 2019;104(7):2735–47. https://doi.org/10.1210/jc.2018-02335.
Rush ET. Childhood hypophosphatasia: to treat or not to treat. Orphanet J Rare Dis. 2018;13(1):116. https://doi.org/10.1186/s13023-018-0866-7.
Mornet E. Genetics of hypophosphatasia. Arch Pediatr. 2017;24(5S2):5S51–5S6. https://doi.org/10.1016/S0929-693X(18)30014-9.
Bowden SA, Adler BH. Reappearance of hypomineralized bone after discontinuation of asfotase alfa treatment for severe childhood hypophosphatasia. Osteoporos Int. 2018;29(9):2155–6. https://doi.org/10.1007/s00198-018-4613-7.
Kishnani PS, Rush ET, Arundel P, Bishop N, Dahir K, Fraser W, et al. Monitoring guidance for patients with hypophosphatasia treated with asfotase alfa. Mol Genet Metab. 2017;122(1–2):4–17. https://doi.org/10.1016/j.ymgme.2017.07.010.
Lyseng-Williamson KA. Burosumab in X-linked hypophosphatemia: a profile of its use in the USA. Drugs Ther Perspect. 2018;34(11):497–506. https://doi.org/10.1007/s40267-018-0560-9.
Imel EA, Biggin A, Schindeler A, Munns CF. FGF23, hypophosphatemia, and emerging treatments. JBMR Plus. 2019;3(8):e10190. https://doi.org/10.1002/jbm4.10190.
Zhang X, Peyret T, Gosselin NH, Marier JF, Imel EA, Carpenter TO. Population pharmacokinetic and pharmacodynamic analyses from a 4-month intradose escalation and its subsequent 12-month dose titration studies for a human monoclonal anti-FGF23 antibody (KRN23) in adults with X-linked hypophosphatemia. J Clin Pharmacol. 2016;56(4):429–38. https://doi.org/10.1002/jcph.611.
Beck-Nielsen SS, Mughal Z, Haffner D, Nilsson O, Levtchenko E, Ariceta G, et al. FGF23 and its role in X-linked hypophosphatemia-related morbidity. Orphanet J Rare Dis. 2019;14(1):58. https://doi.org/10.1186/s13023-019-1014-8.
Gordon RJ, Levine MA. Burosumab treatment of children with X-linked hypophosphataemic rickets. Lancet. 2019;393(10189):2364–6. https://doi.org/10.1016/S0140-6736(19)31054-2.
Availability of Data and Material
The data that support this article are available from the corresponding author upon reasonable request.
Code Availability
Not applicable
Author information
Authors and Affiliations
Contributions
Supamit Ukarapong designed the concepts of the article, performed the literature search, drafted and revised the manuscript, and approved the version to be published. Tossaporn Seeherunvong performed the literature search, drafted and revised the manuscript, and approved the version to be published. Gary Berkovitz critically revised the manuscript and approved the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethics Approval
The article does not contain any studies with human or animal subjects performed by any of the authors.
Consent to Participate
Not applicable
Consent for Publication
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ukarapong, S., Seeherunvong, T. & Berkovitz, G. Current and Emerging Therapies for Pediatric Bone Diseases. Clinic Rev Bone Miner Metab 18, 31–42 (2020). https://doi.org/10.1007/s12018-020-09272-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12018-020-09272-5