Abstract
Mast cells secrete a wide spectrum of stored or newly synthesized pro-inflammatory, anti-inflammatory, and/or immunosuppressive mediators and express several costimulatory and inhibitory surface molecules. Mast cells finely tune activities of T cells, B cells, and regulatory cells and effectively contribute to the development of different T cell-associated responses by influencing their recruitment, activation, proliferation, and differentiation. The interaction between mast cells and T cells, with regard to cellular functionality and immune responses, can be assessed in both activating and inhibitory regulations. While Th2 cytokines, including IL-5 and IL-9, stimulate stem cell factor (SCF)-dependent proliferation of mast cells, Th1 cytokine IFN-γ suppresses SCF-mediated differentiation of mast cell progenitors. Mast cell mediators such as CCL5 have a role in the recruitment of CD8+ T cells to viral infection sites where their ability in clearance of viral reservoirs is needed. The capacity of mast cells in presenting antigens by classes I and II MHC molecules to CD4+ and CD8+ T cells respectively is considered one of the main antigen-dependent interactions of mast cells with T cells. Interestingly, Tregs recruit mast cells to different sites through secretion of IL-9, while the OX40L (expressed on mast cell)-OX40(expressed on T cell) interaction inhibits the extent of the mast cell degranulation. Recently, the capability of exosomes to carry regulatory receptors of the mast cell surface and their role in T cell activation has been investigated. Functional interplay between mast cells and T cell subsets has been suggested primarily by investigating their co-localization in inflamed tissues and involvement of mast cells in autoimmune diseases. In this review, the interactions of mast cells with T cells are reviewed in cell-to-cell, cytokine, and exosome categories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
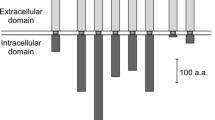
Mast cells (MCs) are CD34+/CD117+ innate immune cells derived from multipotent hematopoietic progenitor cells of bone marrow origin. The progenitors migrate through blood to tissues where differentiation and maturation of MCs under the influence of local growth factors, mainly stem cell factor (SCF) and IL-3 occur [1,2,3]. FcεRI, for IgE activation, and c-kit (CD117), the receptor of the SCF, serve as fingerprints in MC characterization [4, 5]. Cross-linking of the MCs surface-bound FcεRI upon binding to antigen activates multiple signaling pathways which results in degranulation, de novo synthesis of arachidonic acid metabolites, and production of various cytokines and chemokines [6]. The MC cytoplasm contains 50–200 large granules that store inflammatory mediators, cytokines, chondroitin sulfate, and neutral proteases [7]. MCs play a key role in host defense through expressing receptors that belong to the five main families of pathogen recognition receptors (PRR) namely toll-like receptors, C-type lectin-like receptors, scavenger receptors, NOD-like receptors, and RIG-I-like receptors [8]. Interestingly, while expression of TLR1-9 has been reported on human MCs, still there is no report of TLR-5 expression on murine MCs [9] (Fig. 1a). Traditionally, they are best known for their detrimental impact on allergic reactions, especially anaphylaxis. Additionally, they have also been implicated in damaging responses in a large variety of disorders, including atherosclerosis, cancer, and arthritis. However, MCs have numerous functions that are beneficial to the host, in particular, in bacterial infection and protection against envenomation [2]. In this review, the direct (cell-cell interaction) and indirect interaction (secreted factors) of MCs with CD4+ T helper cells, including Th1, Th2, and regulatory T cells, and CD8+ T cells will be summarized and discussed. CD4+ T cells are crucial for directing appropriate immune responses against harmful microorganisms and found to be detrimental in the pathogenesis of inflammatory or autoimmune diseases and allergic disorders [10]. Naïve CD4+ T cells are activated after interaction with antigen-MHC complex and under influence of cytokines differentiate into specific subtypes. Development of naïve CD4+ T to Th1 and Th2 cells requires cytokines and transcription factors. For instance, cytokines including IL12, IFNγ, and transcription factors such as T bet, STAT1, STAT4, Runx 3, Eomes, and H1x are needed to induce Th1 development while cytokines IL4, IL2, and transcription factors including GATA3, STAT6, STAT5, STAT3, Gfi-1, c-Maf, and IRF4 are needed to induce Th2 development [11]. Commitment to the Th1 lineage inhibits Th2 development and vice versa. IFNγ production by Th1 cells inhibits production of Th2 cytokines. Likewise, IL-4 produced by Th2 cells inhibits the production of IFNγ and IL-12, preventing differentiation of naïve CD4+ T cells to the Th1 lineage [12]. Mast cells are capable of promoting vasodilation, plasma extravasation, and most importantly, recruitment and activation of granulocytes, T cells, B cells, and dendritic cells. However, upon appropriate activation, they release products possessing anti-inflammatory or immunosuppressive properties, including IL-10 and TGF-β [13]. The ability of MCs to activate T cells is mostly appreciated due to their capability of acting as antigen presenting cells (APCs). MHC class II molecules play a central role in peptide presentation to CD4+ T cells during initiation of the adaptive immune response. The constitutive expression of MHC class II molecules is confined to professional APCs including dendritic cells, macrophages, and B cells [14]. However, the ability of MCs to interact with T cells is not confined to class II MHC molecule as MCs process bacterial antigens and was found to present epitopes through class I MHC molecules to cultivated T cell after phagocytic uptake of live bacteria in vitro [15]. MCs through releasing a wide range of chemotactic factors for different CD4+ T cell subsets: CCL3, CCL4, CXCL9, and CXCL10 for Th1; CCL5(RANTES [16]) and CCL11 for Th2; CCL2(MIP-1α [16]) and CCL20 for Th17 are able to recruit T cell subsets [17]. MCs promote in vivo T cell migration to inflammatory sites by rapidly activating endothelial cells under influence of histamine and TNF-α, followed by secreting lymphotactin and IL-16 to act as chemoattractant [18, 19] (Fig. 1b). Additionally, MCs express several costimulatory molecules including CD40L, OX40L, CD86, and CD80 by which tune T and B cells by either enhancing or inhibiting their responses [17]. MCs owing to their mediators participate in polarization of Th cell responses of CD4+ lymphocytes such as IL-12 and IFNγ for Th1, IL-4 for Th2, IL-6 and TGFβ1 for Th17, and IL-6 and TNF-α for Th22 [17, 20]. MCs and activated T cells interact directly via ICAM-1 (CD54) and LFA-1 (CD11a) molecules [21].
Mast Cell Interaction with CD4 Helper Cells
Direct Interaction of MC-TCD4 Cells
MCs require three key components to mediate their unique role in the pathogenesis of an allergic disease: environmental antigens, antigen-specific IgE and MC activation/hyperplasia. The latter two components can be affected by Th2-secreted cytokines, including IL-4 and IL-10. In this regard, IL-4 acts primarily as MC proliferative factor; additionally, it promotes Ig class switching in B cells from IgM to IgE, while IL-10 induces MC proliferation and differentiation [22]. Allergic airway inflammation demonstrates a complicated scene of crosstalk between variety of immune cells including MCs, DCs, regulatory T cells (Tregs), B cells, eosinophils, and neurons. Respiratory DCs process the allergens and present it to naïve Th0 cells by which drive them toward Th2 phenotype. Th2-secreted IL-4 and IL-13 activate B cells to produce allergen-specific IgE. Th2-released IL-5 induces proliferation and recruitment of eosinophils to the site of inflammation. Upon allergen/antigen IgE cross-linking, MCs degranulate and secrete histamine and pro-inflammatory mediators and cytokines including IL-4 and IL-13. Epithelial and smooth muscle cell functions are under autonomous control of nerves. The latter cells are potent to modulate MC responses by releasing neuropeptides including neurokinin A, substance P (SP). ATP and other nucleotides stimulate different P2 receptors on the surface of immune cells including MCs and mediate IgE-induced degranulation. ATP induces expression and release of many pro-inflammatory mediators from MCs, including IL-4 and IL-13. Tregs degrade ATP owing to expressing ATP-converting enzymes (CD39 and CD73) inhibit Th2-mediated response. MCs have a role in the downregulation of the allergic response by secreting inhibitory cytokines such as IL-10 or mediators that shift the Th1/Th2 balance to Th1 (IFNγ and IL-12) [23] (Fig. 2). Th1-secreted IFNγ and Th2-secreted IL-4 and IL-5 alter MC population using several different mechanisms. Investigations showed that IFN-γ inhibits early progenitor cell division, IL-4 downregulates early CD117 expression, and IL-5 blocks later cell division. IL-4 and IFN- γ exert their suppressive effects on degranulation and FcεRI expression. Additionally, IL-4 induces division and potentiates FcεRI-mediated degranulation [24]. Yeatman et al. investigated the early and late phases of apoptosis in a cell culture model and showed that combined stimulation with IL-4 and IL-10 induces apoptosis of IL-3-dependent BMMCs. They applied FITC-coupled annexin V staining for detecting the early stages of apoptosis. Moreover, fragmentation of the cell’s DNA by its own nucleases was investigated in late stage apoptosis through assessment of subdiploid DNA content [22] (Fig. 3).
ATP released by neurons of airway is sensed by mast cell P2X and P2Y receptors. Activation of receptors results in IL-4 and IL-13 release which act on B cell population. Moreover, Th2-released IL-4 and IL-13 activate B lymphocytes to produce allergen-specific IgE. Th2-secreted IL-5 induces proliferation and recruitment of eosinophils. Tregs inhibit Th2-mediated response after sensing ATP through receptors CD39 and CD73
To investigate the role of IL-4 and IL-10 in MC apoptosis, BMMCs were cultured in IL-3 alone (not shown) or in IL-3 with IL-4 and/or IL-10. High contents of phosphatidylserine on the outer membrane and higher subdiploid DNA content showed that BMMCs in the presence of IL-3, IL-4, and IL-13 were subjected to apoptosis
Antigen Presentation
Human MCs interact with T cells which results in enhanced expression of HLA class II molecules on MCs via release of IFN-γ by T cells. The expression of HLA class II molecules enables them to present both peptide and entire protein antigens to CD4+ T cells [25]. Additionally, cytokines such as IL-4 and GM-CSF (also known as CSF2) enhance the capacity of MCs to act as APC [26]. MCs owing to constitutively expressing Notch1 and Notch2 and their stimulation with Notch ligand Dll1(delta-like1) express MHC class II molecules [14]. Additionally, Dll1/notch signaling augments FcεRI-mediated IL-4, IL-6, IL-13, and TNF production by BMMCs [27]. Some investigations provide a line of evidence on ability of CD1d-expressing MCs to act as APCs for iNKT cells and exacerbate airway inflammation and remodeling through upregulating IgE production via B cell Ig class switching [28]. For investigation of MCs capacity to activate polyclonal T cells rather than cloned T cells, researchers generated CD4+ bulk T cells expanded with pooled tetanus toxoid, tuberculin, and Candida albicans. Incubation of autologous MCs with these antigens to use them as APCs for polyclonal bulk T cells showed their capacity of activating autologous polyclonal CD4+ T cells [25].
MCs Interaction with Th-17
Th17 cells are CD4 T cells which require the pleiotropic cytokine TGF-β and IL-6 to develop and characterized by the production of effector cytokines including IL-17 (or IL-17A), IL-17F, and IL-6 [29,30,31]. MCs contribute to Th17 cell responses through both indirect effect on dendritic cells and an OX40-mediated crosstalk with regulatory T cells [32]. The T cell ability of cytokine production, expansion, and survival was enhanced by the OX40 costimulatory signals. OX40 is not expressed on naïve or memory T cells but is transiently induced upon activation with corresponding antigens [33]. Supernatant of activated MCs could increase the number of IL-17-producing T cells due to effect of MC-secreted IL-1β [32]. Moreover, it has been demonstrated that IL-33 acts directly on MCs to generate IL-1β and IL-6, thereby enhancing Th17 differentiation. Such interaction may result in neutrophil-dominant OVA-induced airway inflammation in response to OVA rechallenge [34].
Indirect Interaction of MC-TCD4 Cells
Indirect interaction of MC-TCD4 cells occurs when exogenous antigens are uptaken by activated MCs, then transferred to DCs to be processed and presented to T cells. Carroll-Portillo et al. activated α-DNP-IgE-primed MC/9 MCs by DNP-OVA and incubated them with immature DCs (imDCs) for 1 h before adding OTII T cell line to the co-culture. After 16 h of co-culture, the T cells were found to have significant upregulation of CD25, as a marker of T cell activation. Removing DCs from protocol led to no detectable CD25 upregulation [35] (Fig. 4). Crosstalk between peritoneal cultured MCs (PCMCs) and DCs showed that PCMC-primed DCs are able to alter CD4+ T cell maturation in favor of Th1 and Th17 subsets. One of the studies reported that PCMCs establish direct cell-to-cell contacts with imDCs which result in DC maturation and releasing T cell modulating cytokines. Furthermore, T cells stimulated by PCMC-primed DCs secrete IFN-γ and IL-17 [36].
Direct interaction between MC and T cell through presenting antigen by MC results in T cell activation. Indirect MC-T cell interaction occurs when MCs internalize the antigen and transfer it to DCs to be processed and presented to T cells. In this model, based on investigation of Carroll-Portillo et al., activated α-DNP-IgE-primed MC/9 MCs after incubation with immature DCs (iDCs) transfer the antigen to iDCs to be presented to OTII T cells. The latter cells activate and consequently upregulate CD25 as activation marker. Removing DCs from protocol led to no detectable CD25 upregulation
MC-Th2 Regulation
Apart from being the master cells in allergic reactions, MCs play a role in immune tolerance during aberrant Th2 responses. The mechanisms of action include increasing the expression of Bcl-6 in Th2 cells under influence of mouse mast cell protease-6 (mMCP-6). Increased Bcl-6 inhibits GATA-3 expression in Th2 cells, while increases forkhead box P3 (FOXP3) which consequently results in reducing Th2 cytokines. Results of Liu et al. suggest that the increase in Bcl-6 may be involved in the conversion of antigen-specific CD4+ T cells to Foxp3+ Tregs [37]. Some studies have provided evidence on regulatory role of Th2-type cytokines on MC viability, functionality, and hemostasis by negative regulation of the surface expression of the SCF receptor, (CD117). For example, it has been reported that MCs stimulated with IL-3 and IL-4 demonstrated a 50% reduction in CD117 expression, although with unchanged CD117 mRNA levels. Moreover, IL-4 and IL-10 have been shown to possess inhibitory effects on FcεRI levels in the presence of IL-3 on murine BMMC [38]. Th2 cells through their released cytokines influence MC functions for instance, IL-4 inhibits expression of the high affinity IgE receptor (FcεRI) and CD117 on cultured MCs, and combined with Th2 cytokine IL-10 elicit MC apoptosis [39, 40]. IL-4 in a dose-dependently manner suppresses IFN-γ-mediated survival and differentiation of MCs from mouse splenic precursors [39, 41]. One interesting aspect of the interaction between MC-T cells has been traced in lymph nodes, where MCs have been reported to have a role in recruitment of T cells. Related studies consistently suggest that MCs may play a key role in induction of primary and/or local memory T cell responses [25]. Within minutes of bacterial challenge, MCs secrete TNF, as they are the only cell type capable of storing TNF within peripheral tissues [42, 43]. The presence of TNF in lymph node and induced hyper cellularity due to accumulation of T cells has been studied by McLachlan and colleagues. In their mouse model, animals were injected by E. coli into the footpads, and related nodes were monitored due to accumulation of T cells, MC population, and their released mediators. Flow cytometric analysis of the nodes revealed a marked increase in T and B lymphocytes. Using MC granule-specific stain toluidine blue, they observed significant local MC degranulation when compared with control. A significant difference in the node cellularity after bacterial challenge in wild type and MC-deficient W/Wv mice, and then restoring the hypocellularity in MC-repleted W/Wv mice provided evidence that MCs play a role in accumulation of T cells. They reported that injection of TNF into the footpad could increase lymph node hypertrophy when compared with control. Applying TNF-neutralizing Abs could significantly reduce the T cell population. As the last step, they repleted footpads of W/Wv mice with BMMCs from TNF-deficient mice or their age-matched control counterparts. W/Wv mice repleted with TNF-deficient MCs portrayed significantly less hypertrophy than either WT mice or W/Wv mice repleted with WT-MCs [43]. Nakae et al. reported that MCs stimulated via the FcεRI enhanced the activation of T cell subsets including CD4+, CD8+, Th1, Th2, Tc1, Tc2, γδTCR+, and CD4+CD62L− T cells. Furthermore, MC-derived TNF was shown to enhance both CD4+ and CD8+ proliferation in T cell-MC cocultures. This group of researchers using neutralizing Ab to either TNFRI or TNFRII concluded that signaling from both TNFRI and TNFRII contributes to optimal enhancement of T cell proliferation by IgE/Ag-stimulated MCs [44]. Most recently, a study aimed to investigate the contribution of MCs in boosting the Th17 axis in mucosal immunity. In this study, supernatant of activated MCs could increase the number of IL-17-producing T cells due to MC-secreted IL-1β. Secretion of the latter mediator was caspase-independent, indicating that Th17 cell expansion by MC occurred through inflammasome-independent IL-1β [32]. Researches aimed to study the interactions of MCs and T cells within tumor microenvironment suggest that MC infiltrating into tumor upon recruiting by SCF produced by tumor cells results in the suppression of T lymphocytes and NK cells. The mechanism of action may include adenosine releasing by activated MCs. Studies based on intravenous injection of MCs into mice reported decreased IL-2 and increased IL-10, TGF-β, and Foxp3 mRNAs in the tumor microenvironment. Consistent with cytokine changes, the percentage of Treg cells in total T cells in the tumor was increased [45]. MC-derived histamine, chemokines, LTB4, and TNF-α promote dendritic cell migration and lymphocyte recruitment, leading to hypertrophy of antigen-draining lymph nodes. MC expresses costimulatory molecules of the B7 family including CD80 and CD86, members of the TNF and TNF receptor families, CD28, and CD40 ligands. Activated MCs release Th2 cytokines such as IL-4, IL-5, IL-9, and IL-13 that are capable of polarizing T and B cell responses [46]. Interestingly, MC-derived histamine has both positive and negative immunomodulatory effects in which it can promote Th1 cell activation through H1 receptors while conversely can suppress both Th1 and Th2 cell activation through H2 receptors [47]. The presence of MCs around the tumor cells leads to depletion of serotonin, the mediator with a key role in T cell proliferation and activation. MCs by expressing serotonin-specific transporters take up and store serotonin. Consequently, they contribute to create an environment unfavorable for T cell activation and proliferation [48].
Mast Cell Interaction with Treg
Recent investigations showed that CD25+ Tregs owing to OX40/OX40L interaction with MCs are capable of inhibiting MC degranulation and anaphylaxis. Surface-bound Treg-derived TGF-β has been reported to enhance MC production of IL-6 which has a role in bacterial clearance and host survival [49]. CD4+/CD25+ Treg cells expressing FOXP3 have been documented in skin allografts where their interaction with MCs is essential for Treg cell-dependent peripheral tolerance. Such Treg subset actively participates in recruitment and activation of MCs by secreting IL-9. Since IL-9 is considered as a growth factor for MCs, its neutralization accelerates allograft rejection in tolerant mice. OX40L-OX40 interaction has been reported to inhibit the extent of MC degranulation in vitro and of the immediate hypersensitivity response in vivo [50]. In tumor microenvironment, Tregs are recruited by MC-released adenosine, and their interaction dictates the level of cancer-associated inflammation and influences the enhancement or suppression of tumor growth. Tregs derived from healthy mice suppress the expansion and differentiation of MC progenitors and MC degranulation. MC-derived histamine IL-6 and IL-23 together with OX40 engagement on Treg abolish suppressive functions of Tregs. Additionally, MC is able to inhibit expression of IL-10 by Treg through OX40L–OX40 interaction [46, 51, 52]. Another crosstalk occurs in tumor microenvironment among MCs, Tregs, and myeloid-derived suppressor cells (MDSCs). MCs have been reported to mobilize the infiltration of MDSCs to tumor by regulating the expressions of CCL2 and Th2 cytokines. MDSCs released IL-17 attracts Treg cells. In return, recruited Tregs produce IL-9 which strengthens the survival and protumor effects of MCs in tumor microenvironment [53, 54]. Moreover, Treg-derived IL-9 promotes recruitment of MCs into transplanted allografts; thus, it is important for maintaining allograft tolerance [49]. Considering that MCs produce TGF-β which is necessary for in vivo and ex vivo expansion of Tregs, it is tempting to speculate that thymic MCs, influence the development of this population [55]. MC-derived IL-6 and TNF acting with Treg-derived TGF-β are capable to skew T effector cells (CD4+ CD25−) to a pro-inflammatory Th17 phenotype [56]. Investigations aimed to reveal the immunologic basis of allergen-specific immunotherapy (AIT) in individuals with bee venom allergy showed that Treg-secreted IL-10 and TGF-β suppress MCs in addition to basophils and eosinophils [57]. Treg cells inhibit allergic inflammation by different modes of action including MC suppression. In this regard, Treg-derived IL-10 inhibits MC activation and cytokine production, and Treg-derived TGF-β inhibits expression of FcεRI [58].
Mast Cell Interaction with CD8 Tcells
MCs are capable to sense and respond to microbial components owing to express a full repertoire of PRRs including TLRs which their engagement results in recruiting effector CD8+ T cells by secreting CCL5 [59]. McAlpine et al. to provide a line of evidence to MC capability of CD8+ T cell recruitment in viral infection examined supernatants of reovirus-infected cord blood MCs (CBMCs) for chemotaxis assays. Virus-infected CBMCs were found capable to recruit CD8 T cells and CD3CD56 T cells by producing CCL3, CCL4, and CCL5. Furthermore, CD56+ T cell migration was inhibited by pertussis toxin and met-RANTES as CCR1/CCR5 antagonists [60]. MCs are permissive for MCMV infection, and in the course of a lytic viral replication, cycle-infected MCs degranulate and release CCL5. CCL5 binds to CCR5 upregulated on CD8+ T cells and its gradient attracts the CD8+ T cells in an initially antigen-independent manner to infected tissues [61]. Most recently, a novel crosstalk between CD8+ T cells and MC during immune defense against CMV was reported by Ebert and colleagues. They investigated the role of MC-derived CCL5 in CD8+ T cell recruitment in a murine model of CMV and reported that CD8 T+ cells of C57BL/6 mice could be successfully recruited to the mCMV-infected lungs when compared with MC-deficient KitW-sh/W-sh controls. Reversing the impaired recruitment in MC deficient mice by BMMC reconstitution verified the role of MCs in viral immunity through recruitment of CD8 T cells [62]. Ott et al. used transwell migration assays to assess the activated MCs capability of induction chemotaxis of effector, but not central memory, CD8+ T cells through releasing leukotriene B4 (LTB4) in vivo. For this purpose, they sensitized (BMMCs) with IgE and placed them to the lower wells of the migration chamber. BMMCs were then stimulated with F(ab′)2 fragments of rabbit antibody to mouse IgG to induce degranulation thus, releasing LTB4. They immediately added CD8+ T cells to the upper wells and applied flow cytometry to assess the CD8+ T cells migration after incubating the chambers for 3 h at 37 °C. Surprisingly, three to fourfold more CD8+ T cells migrated toward activated BMMCs than toward resting BMMCs or those sensitized with IgE alone [63] (Fig. 5a). The interactions between MCs and CD8+ T cells include but not limited to chemokine-induced recruitment. Indeed, MC ability of processing bacterial Ags for presentation through MHC class I molecules to T cells implies on the existence of a cell-cell plus costimulatory interactions between MCs and CD8+ T cells [59]. Stelekati et al. studied MCs for their potential of taking up exogenous peptides, generating peptide-MHC class I molecules, and finally expressing them on the cell surface. They could successfully recognize the specific complexes of OT-I (transgenic CD8+ T cells) peptides and MHC class I molecules using 25-D1.16 antibodies on the surface of BMMCs after preincubation with the model antigenic peptide (OVA257–264). These researchers cocultured OVA257–264-loaded BMMCs with T cell receptor− (TCR−) transgenic (OT-I) for 48 h, then CD8+ T cell activation was analyzed by flow cytometry for the assessment of CD69, CD25, and CD44 as T cell activation markers. To explore the observed effect of MHC class I, they benefited from a model including BMMCs derived from beta-2-microglobulin (b2m)-deficient (B2m−/−) mice. As expected, the B2m−/− MCs induced only a minimal activation of CD8+ T cells (Fig. 5b). Interestingly, the interaction between MCs and CD8+ T cells could increase intracellular granzyme B (Gzmb) expression in CD8+ T cells accompanied with enhanced exocytosis. The latter effect was assessed through measuring lysosomal-associated membrane protein-1 (LAMP-1) [64].
a Sensitized BMMCs with IgE placed in lower chamber in transwell migration assays were able to induce the CD8+ T cells migration by releasing LTB4. b Stelekati et al. to show BMMCs ability to present exogenous antigens via MHC class I molecules to OT I CD8+ T cells loaded BMMCs with OVA257-264 and cocultured with OT I cells and then investigated the expression of activation markers CD44, CD69, and CD25. Applying beta-2-microglobulin (b2m)-deficient (B2m−/−) mice revealed that BMMCs could effectively activate CD8+ T cells through presenting antigen by MHC class I molecules
Role of Mast-Cells in Chronic Inflammatory Diseases
The number of MCs in the synovial tissues and fluids of patients with rheumatoid arthritis (RA) is found to be increased [65]. MC-specific proteinases, mainly tryptase and chymase, are capable of degrading various matrix components, and activating the zymogen forms of the matrix metalloproteinases prostromelysin and procollagenase [66]. MC-derived histamine, VEGF, leukotrienes, and prostaglandins are associated with increased vascular permeability and angiogenesis. Fibroblast activation and hyperplasia observed in RA is attributed to histamine, IL-1, IL-6, PDGF, and IL-13. MCs contribute to differentiation and activation of osteoclasts by releasing heparin, MIP-1α, TNF-α, IL-1, histamine, and RANKL. MCs play a role in recruitment of leukocytes to RA synovia by releasing mediators mainly TNF-α, MCP-6, IL-8, and leukotrienes (Fig. 6a). MCs in RA, in addition to have pro-inflammatory roles, may act as immunomodulatory cells. In this regard, they suppress DC migration, maturation, and activation by releasing histamine and IL-10. Moreover, MC-derived IL-10 and TGF-β induce and maintain Tregs. They can inhibit Th1 activation by releasing IL-4 and TGF-β or inhibit fibroblasts by production of IL-13 [67, 68]. B cell recruitment and activation through interaction of the CD40L on the MCs surface with CD40 on B cells induces the release of anti-CCP IgE with high affinity for the mast cell FcεRI receptor, which perpetuates their activation [69]. In Alzheimer’s disease, MCs following activation by amyloid beta clusters that bind to TLRs release pro-inflammatory cytokines such as IL-1, IL-18, IL-32, TNF, and arachidonic acid products, such as the PGD2 [70]. MCs activate P2 purinergic receptors in microglia by releasing ATP which provokes the secretion of IL-33. This cytokine acts through ST2 receptors on MCs and causes the release of IL-6, IL-13, and monocyte chemoattractant protein-1 (MCP-1). Moreover, MC-derived tryptase facilitates the release of reactive oxygen species (ROS) and pro-inflammatory cytokine mediators such as TNF-α and IL-6 (Fig. 6b) [71, 72]. In asthmatic patients, antigen-stimulated MCs release sphingosine-1-phosphate (S1P) which in return leads to MCs chemotaxis (through S1PR1) and degranulation (through S1PR2). This mediator affects eosinophil infiltration of the airway wall and stimulates the contractions of airway smooth muscle (ASM) [73]. KIT inhibition by Imatinib in patients with severe refractory asthma showed decreased airway hyper-responsiveness, MC counts, and tryptase release and provided a line of evidence to MC contribution in asthma pathogenesis [74]. MCs are involved in the liver’s fibrotic response to chronic inflammation. MC tryptase induces proliferation, migration, and type I collagen synthesis by fibroblasts in human liver and has similar effects on hepatic fat-storing cells mainly, stellate cells, and the major matrix-producing cells in liver fibrosis. MC hyperplasia during the development of liver fibrosis could be due to SCF produced by hepatic fibroblasts [75] (Fig. 6c). MC degranulation due to unknown triggers occurs in the mucosa of the ileum and colon of patients with inflammatory bowel disease (IBD) and elevated levels of mediators including TNF-α, IL-16, substance P, histamine, and tryptase are observed [76]. MC can be activated by stress via eosinophil-derived CRH, IgE, or ATP and release mediators, including proteases, histamine, chemokines, and cytokines, leading to the attraction of inflammatory cells, changes in barrier function, and tissue remodeling [77].
Role of Mast-Cells in Autoimmune Diseases
There is a growing body of evidence that MCs are involved in the exacerbation of several autoimmune diseases. Interplay between MCs and T cells at sites of autoimmunity is documented by marked increase in MC number and co-localization of MCs and T cells. Here, we list the contributory role of MCs in autoimmune diseases. Having insight into involved MC mediators and their mechanism of action in pathogenesis of each autoimmune disease could help to target MCs activation, degranulation, and released mediators for possible therapeutic purposes. For instance, treatment with inhibitors of MC degranulation may be a good way to inhibit MS. Moreover, MCs can be inhibited through the action of an Fcε–Fcγ fusion protein engineered to engage human FcγRIIb with high affinity. Interestingly, tyrosine kinase inhibitors including Masitinib, which are capable of inhibiting the survival, migration, and activity of MCs, have been reported promising in treatment of patients with progressive MS [51]. Recently, disodium cromoglycate was reported promising in blocking injurious MC degranulation specifically without affecting the immunomodulatory role of these cells in treatment of autoimmune anti-myeloperoxidase glomerulonephritis in mice [78] (Table 1).
Role of Exosomes in MC-T Cell Interplay
The role of exosomes, the nanovesicles released by different cell types including MCs, has been documented in interaction between MCs and T cells. Exosomes are being generated from multivesicular bodies (MVB) released into extracellular space via exocytosis [87]. MVBs are formed after membranes of vacuolar endosomes bud inwards and pinch off into the lumen of the vesicle [88]. Exosomes released from cells circulate in the blood, suggesting that they play an important role in intercellular communications [89]. Structurally, they contain membrane transport and fusion proteins as well as tetraspanins. Li et al. investigated the role of exosomes in differentiation of naïve CD4 T cells and developed BMMCs from bone marrow cells of bronchoalveolar lavage (BALB)/c mice cultured with rIL-3. Assessments revealed a purity of 98% after toluidine blue staining and confirming FcεRI expression. The cells were cultured for 72 h with rIL-3 in RPMI 1640. Supernatant after subjecting to centrifugation for removing the cells and debris underwent filtration, and ultracentrifugation and exosomes were isolated. Exosomes were then coincubated with naive CD4+ T cells in the presence of IL-4. Researchers found out that the presence of MC exosomes had resulted in differentiation of naive CD4+ T cells to Th2 cells comparing to control. Using fluorescent dyes, they showed that the exosomes were attached to CD4+ T cells. They presumed based on the similar studies on other immune cells that ligation of OX40L present on exosomes and OX40 expressed on T cells was responsible for the observed differentiation effect. Finally, to investigate the molecular mechanism of action, they applied anti-mouse OX40L mAb to block OX40L. The inhibition of OX40L resulted in lower number of differentiated CD4+ T cells [90]. Interestingly, OX40–OX40L interaction in interplay between MCs and B cells influences the capacity of B cells in producing IgE and IgA [91,92,93] (Fig. 7).
Li et al. to investigate the role of exosomes in T cell differentiation developed BMMCs from mice bone marrow cells. For the purpose of obtaining exosomes, the cells underwent ultracentrifugation and filtration. Applying anti-mouse OX40L mAb, exosomes were found to have a key role in differentiation of naive CD4+ T cells to Th2 cells via OX40-OX40L interaction
Discussion and Conclusion
The interplay between MCs and T cells is believed to be multi-faceted, as they have been shown to contribute to both a pro- or anti-inflammatory response, depending on the immunological setting [94]. MCs display a wide range of functionality depending on the tissue in which they differentiate and reside. Their distribution within the skin and internal organs permits them to be among the first cells of the immune response, along with dendritic cells and tissue macrophages, to interact with environmental antigens and allergens and invading pathogens. Additionally, MCs are equipped with TLRs and cytokines and chemokines receptors to sense tissue microenvironment. As part of the innate immunity, MCs interact and direct the following immune response through several activation pathways including by cell-cell interactions and secreted immunomodulatory factors. In return, T cells provide signals required for MC activation and mediator release. Interestingly, the expression and release of mediators including MMP-9 and histamine were also induced when MCs incubated with cell membranes isolated from activated T cells [95]. The ability of Ag presenting through MHC class II molecules makes MCs unique immune cells with multiple capabilities. However, this ability should be investigated deeply, as the exact role of MC surface receptors in Ag presentation remains unknown. For instance, it is reported that only surface FcεRIhi MCs expressing surface MHC II could effectively involve in Ag presentation [96]. A wide variety of cells secrete exosomes, and the presence of exosomes in many biological fluids, such as urine, saliva, BAL fluid, and plasma has been reported. MC-derived exosomes have 200 to 400 different proteins most of which are not identified; thus, their possible activating or inhibitory effects on crosstalk between MCs and T cells should be considered [88]. Some of these proteins are able to effectively shape the outcome of indirect crosstalk such as MHCII molecules loaded on the MC-derived exosomes. More investigation should be focused to determine the role of such molecules. Undoubtedly, having deep insights of interactions between MCs and T cells on both molecular and cellular levels will shed lights on discovering and developing novel therapies for some diseases. In this regard, Nahum et al. characterized a novel MC activation pathway initiated by contact with activated T cells through phosphorylation of the mitogen-activated protein kinases (MAPKs) extracellular signal-regulated kinase and p38. According to their investigation on Ras, a GTP-binding protein acts as upstream regulator of the MAPK system, they concluded that targeting the Ras pathway could be a possible treatment option for conditions in which MCs interact with T cells, such as sarcoidosis, rheumatoid arthritis, and graft tolerance [97].
Abbreviations
- RANKL:
-
Receptor activator of NF-κB ligand
- LTs:
-
Leukotrienes
- PGs:
-
Prostaglandins
- PAF:
-
Platelet activating factor
- MCs:
-
Mast cells
- iDCs:
-
Immature DCs
References
Gri G, Frossi B, D'Inca F, Danelli L, Betto E, Mion F, Sibilano R, Pucillo C (2012) Mast cell: an emerging partner in immune interaction. Front Immunol 3:120. https://doi.org/10.3389/fimmu.2012.00120
Wernersson S, Pejler G (2014) Mast cell secretory granules: armed for battle. Nat Rev Immunol 14(7):478–494. https://doi.org/10.1038/nri3690
Kalesnikoff J, Galli SJ (2008) New developments in mast cell biology. Nat Immunol 9(11):1215–1223. https://doi.org/10.1038/ni.f.216
Migalovich-Sheikhet H, Friedman S, Mankuta D, Levi-Schaffer F (2012) Novel identified receptors on mast cells. Front Immunol 3:238. https://doi.org/10.3389/fimmu.2012.00238
Komi DEA, Rambasek T, Wohrl S (2017) Mastocytosis: from a molecular point of view. Clin Rev Allergy Immunol. https://doi.org/10.1007/s12016-017-8619-2
Okayama Y, Kawakami T (2006) Development, migration, and survival of mast cells. Immunol Res 34(2):97–115. https://doi.org/10.1385/ir:34:2:97
Krystel-Whittemore M, Dileepan KN, Wood JG (2015) Mast cell: a multi-functional master cell. Front Immunol 6:620. https://doi.org/10.3389/fimmu.2015.00620
Campillo-Navarro M, Chavez-Blanco AD, Wong-Baeza I, Serafin-Lopez J, Flores-Mejia R, Estrada-Parra S, Estrada-Garcia I, Chacon-Salinas R (2014) Mast cells in lung homeostasis: beyond type I hypersensitivity. Curr Respir Med Rev 10(2):115–123. https://doi.org/10.2174/1573398x10666141024220151
Sandig H, Bulfone-Paus S (2012) TLR signaling in mast cells: common and unique features. Front Immunol 3:185. https://doi.org/10.3389/fimmu.2012.00185
Hirahara K, Nakayama T (2016) CD4+ T-cell subsets in inflammatory diseases: beyond the Th1/Th2 paradigm. Int Immunol 28(4):163–171. https://doi.org/10.1093/intimm/dxw006
Luckheeram RV, Zhou R, Verma AD, Xia B (2012) CD4(+)T cells: differentiation and functions. Clin Dev Immunol 2012:925135. https://doi.org/10.1155/2012/925135
Caza T, Landas S (2015) Functional and phenotypic plasticity of CD4(+) T cell subsets. Biomed Res Int 2015:521957. https://doi.org/10.1155/2015/521957
Kalesnikoff J, Galli SJ (2011) Antiinflammatory and immunosuppressive functions of mast cells. Methods in molecular biology (Clifton, NJ) 677:207–220. https://doi.org/10.1007/978-1-60761-869-0_15
Nakano N, Nishiyama C, Yagita H, Koyanagi A, Ogawa H, Okumura K (2011) Notch1-mediated signaling induces MHC class II expression through activation of class II transactivator promoter III in mast cells. J Biol Chem 286(14):12042–12048. https://doi.org/10.1074/jbc.M110.138966
Malaviya R, Twesten NJ, Ross EA, Abraham SN, Pfeifer JD (1996) Mast cells process bacterial Ags through a phagocytic route for class I MHC presentation to T cells. J Immunol (Baltimore, Md : 1950) 156(4):1490–1496
Gilfillan AM, Beaven MA (2011) Regulation of mast cell responses in health and disease. Crit Rev Immunol 31(6):475–529
Cardamone C, Parente R, Feo GD, Triggiani M (2016) Mast cells as effector cells of innate immunity and regulators of adaptive immunity. Immunol Lett 178:10–14. https://doi.org/10.1016/j.imlet.2016.07.003
Valitutti S, Espinosa E (2010) Cognate interactions between mast cells and helper T lymphocytes. Self 1(2):114–122. https://doi.org/10.4161/self.1.2.11795
Gaudenzio N, Espagnolle N, Mars LT, Liblau R, Valitutti S, Espinosa E (2009) Cell-cell cooperation at the T helper cell/mast cell immunological synapse. Blood 114(24):4979–4988. https://doi.org/10.1182/blood-2009-02-202648
de Vries VC, Noelle RJ (2010) Mast cell mediators in tolerance. Curr Opin Immunol 22(5):643–648. https://doi.org/10.1016/j.coi.2010.08.015
Hershko AY, Rivera J (2010) Mast cell and T cell communication; amplification and control of adaptive immunity. Immunol Lett 128(2):98–104. https://doi.org/10.1016/j.imlet.2009.10.013
Yeatman CF 2nd, Jacobs-Helber SM, Mirmonsef P, Gillespie SR, Bouton LA, Collins HA, Sawyer ST, Shelburne CP, Ryan JJ (2000) Combined stimulation with the T helper cell type 2 cytokines interleukin (IL)-4 and IL-10 induces mouse mast cell apoptosis. J Exp Med 192(8):1093–1103
Bulanova E, Bulfone-Paus S (2010) P2 receptor-mediated signaling in mast cell biology. Purinergic signalling 6(1):3–17. https://doi.org/10.1007/s11302-009-9173-z
Kulka M, Metcalfe DD (2005) High-resolution tracking of cell division demonstrates differential effects of TH1 and TH2 cytokines on SCF-dependent human mast cell production in vitro: correlation with apoptosis and Kit expression. Blood 105(2):592–599. https://doi.org/10.1182/blood-2004-07-2838
Suurmond J, van Heemst J, van Heiningen J, Dorjee AL, Schilham MW, van der Beek FB, Huizinga TW, Schuerwegh AJ, Toes RE (2013) Communication between human mast cells and CD4(+) T cells through antigen-dependent interactions. Eur J Immunol 43(7):1758–1768. https://doi.org/10.1002/eji.201243058
Kambayashi T, Laufer TM (2014) Atypical MHC class II-expressing antigen-presenting cells: can anything replace a dendritic cell? Nat Rev Immunol 14(11):719–730. https://doi.org/10.1038/nri3754
Nakano N, Nishiyama C, Yagita H, Koyanagi A, Akiba H, Chiba S, Ogawa H, Okumura K (2009) Notch signaling confers antigen-presenting cell functions on mast cells. J Allergy Clin Immunol 123(1):74–81.e71. https://doi.org/10.1016/j.jaci.2008.10.040
Hong GU, Kim NG, Kim TJ, Ro JY (2014) CD1d expressed in mast cell surface enhances IgE production in B cells by up-regulating CD40L expression and mediator release in allergic asthma in mice. Cell Signal 26(5):1105–1117. https://doi.org/10.1016/j.cellsig.2014.01.029
Lee YK, Mukasa R, Hatton RD, Weaver CT (2009) Developmental plasticity of Th17 and Treg cells. Curr Opin Immunol 21(3):274–280. https://doi.org/10.1016/j.coi.2009.05.021
Weaver CT, Harrington LE, Mangan PR, Gavrieli M, Murphy KM (2006) Th17: an effector CD4 T cell lineage with regulatory T cell ties. Immunity 24(6):677–688. https://doi.org/10.1016/j.immuni.2006.06.002
Bi Y, Liu G, Yang R (2007) Th17 cell induction and immune regulatory effects. J Cell Physiol 211(2):273–278. https://doi.org/10.1002/jcp.20973
Suurmond J, Habets KL (2016) Expansion of Th17 cells by human mast cells is driven by inflammasome-independent IL-1beta. J Immunol 197(11):4473–4481
Ishii N, Takahashi T, Soroosh P, Sugamura K (2010) OX40-OX40 ligand interaction in T-cell-mediated immunity and immunopathology. Adv Immunol 105:63–98. https://doi.org/10.1016/s0065-2776(10)05003-0
Cho KA, Suh JW, Sohn JH, Park JW, Lee H, Kang JL, Woo SY, Cho YJ (2012) IL-33 induces Th17-mediated airway inflammation via mast cells in ovalbumin-challenged mice. Am J Physiol Lung Cell mol physiol 302(4):L429–L440. https://doi.org/10.1152/ajplung.00252.2011
Carroll-Portillo A, Cannon JL, te Riet J, Holmes A, Kawakami Y, Kawakami T, Cambi A, Lidke DS (2015) Mast cells and dendritic cells form synapses that facilitate antigen transfer for T cell activation. J Cell Biol 210(5):851–864. https://doi.org/10.1083/jcb.201412074
Dudeck A, Suender CA, Kostka SL, von Stebut E, Maurer M (2011) Mast cells promote Th1 and Th17 responses by modulating dendritic cell maturation and function. Eur J Immunol 41(7):1883–1893. https://doi.org/10.1002/eji.201040994
Liu ZQ, Song JP, Liu X, Jiang J, Chen X, Yang L, Hu T, Zheng PY, Liu ZG, Yang PC (2014) Mast cell-derived serine proteinase regulates T helper 2 polarization. Sci Rep 4:4649. https://doi.org/10.1038/srep04649
Shelburne CP, Ryan JJ (2001) The role of Th2 cytokines in mast cell homeostasis. Immunol Rev 179:82–93
Bailey DP, Kashyap M, Mirmonsef P, Bouton LA, Domen J, Zhu J, Dessypris EN, Ryan JJ (2004) Interleukin-4 elicits apoptosis of developing mast cells via a Stat6-dependent mitochondrial pathway. Exp Hematol 32(1):52–59
Yanagida M, Fukamachi H, Ohgami K, Kuwaki T, Ishii H, Uzumaki H, Amano K, Tokiwa T, Mitsui H, Saito H, Iikura Y, Ishizaka T, Nakahata T (1995) Effects of T-helper 2-type cytokines, interleukin-3 (IL-3), IL-4, IL-5, and IL-6 on the survival of cultured human mast cells. Blood 86(10):3705–3714
Hu ZQ, Zhao WH, Shimamura T, Galli SJ (2006) Interleukin-4-triggered, STAT6-dependent production of a factor that induces mouse mast cell apoptosis. Eur J Immunol 36(5):1275–1284. https://doi.org/10.1002/eji.200526275
Metz M, Maurer M (2007) Mast cells—key effector cells in immune responses. Trends Immunol 28(5):234–241. https://doi.org/10.1016/j.it.2007.03.003
McLachlan JB, Hart JP, Pizzo SV, Shelburne CP, Staats HF, Gunn MD, Abraham SN (2003) Mast cell-derived tumor necrosis factor induces hypertrophy of draining lymph nodes during infection. Nat Immunol 4(12):1199–1205. https://doi.org/10.1038/ni1005
Nakae S, Suto H, Iikura M, Kakurai M, Sedgwick JD, Tsai M, Galli SJ (2006) Mast cells enhance T cell activation: importance of mast cell costimulatory molecules and secreted TNF. J Immunol(Baltimore, Md : 1950) 176(4):2238–2248
Huang B, Lei Z, Zhang GM, Li D, Song C, Li B, Liu Y, Yuan Y, Unkeless J, Xiong H, Feng ZH (2008) SCF-mediated mast cell infiltration and activation exacerbate the inflammation and immunosuppression in tumor microenvironment. Blood 112(4):1269–1279. https://doi.org/10.1182/blood-2008-03-147033
Khazaie K, Blatner NR, Khan MW, Gounari F, Gounaris E, Dennis K, Bonertz A, Tsai FN, Strouch MJ, Cheon E, Phillips JD, Beckhove P, Bentrem DJ (2011) The significant role of mast cells in cancer. Cancer Metastasis Rev 30(1):45–60. https://doi.org/10.1007/s10555-011-9286-z
Galli SJ, Grimbaldeston M, Tsai M (2008) Immunomodulatory mast cells: negative, as well as positive, regulators of immunity. Nat Rev Immunol 8(6):478–486. https://doi.org/10.1038/nri2327
Wasiuk A, de Vries VC, Hartmann K, Roers A, Noelle RJ (2009) Mast cells as regulators of adaptive immunity to tumours. Clin Exp Immunol 155(2):140–146. https://doi.org/10.1111/j.1365-2249.2008.03840.x
Ganeshan K, Bryce PJ (2012) Regulatory T cells enhance mast cell production of IL-6 via surface-bound TGF-beta. J Immunol (Baltimore, Md : 1950) 188(2):594–603. https://doi.org/10.4049/jimmunol.1102389
Frossi B, Gri G, Tripodo C, Pucillo C (2010) Exploring a regulatory role for mast cells: ‘MCregs’? Trends Immunol 31(3):97–102. https://doi.org/10.1016/j.it.2009.12.007
Xu Y, Chen G (2015) Mast cell and autoimmune diseases. Mediat Inflamm 2015:246126. https://doi.org/10.1155/2015/246126
Piconese S, Gri G, Tripodo C, Musio S, Gorzanelli A, Frossi B, Pedotti R, Pucillo CE, Colombo MP (2009) Mast cells counteract regulatory T-cell suppression through interleukin-6 and OX40/OX40L axis toward Th17-cell differentiation. Blood 114(13):2639–2648. https://doi.org/10.1182/blood-2009-05-220004
Yang Z, Zhang B, Li D, Lv M, Huang C, Shen GX, Huang B (2010) Mast cells mobilize myeloid-derived suppressor cells and Treg cells in tumor microenvironment via IL-17 pathway in murine hepatocarcinoma model. PLoS One 5(1):e8922. https://doi.org/10.1371/journal.pone.0008922
Groot Kormelink T, Abudukelimu A, Redegeld FA (2009) Mast cells as target in cancer therapy. Curr Pharm Des 15(16):1868–1878
Christy AL, Brown MA (2007) The multitasking mast cell: positive and negative roles in the progression of autoimmunity. J Immunol (Baltimore, Md : 1950) 179(5):2673–2679
Walker ME, Hatfield JK, Brown MA (2012) New insights into the role of mast cells in autoimmunity: evidence for a common mechanism of action? Biochim Biophys Acta 1822(1):57–65. https://doi.org/10.1016/j.bbadis.2011.02.009
Akdis CA, Akdis M (2014) Mechanisms of immune tolerance to allergens: role of IL-10 and Tregs. J Clin Invest 124(11):4678–4680. https://doi.org/10.1172/jci78891
Palomares O, Martin-Fontecha M, Lauener R (2014) Regulatory T cells and immune regulation of allergic diseases: roles of IL-10 and TGF-beta. Genes Immun 15(8):511–520. https://doi.org/10.1038/gene.2014.45
Bulfone-Paus S, Bahri R (2015) Mast cells as regulators of T cell responses. Front Immunol 6:394. https://doi.org/10.3389/fimmu.2015.00394
McAlpine SM, Issekutz TB, Marshall JS (2012) Virus stimulation of human mast cells results in the recruitment of CD56(+) T cells by a mechanism dependent on CCR5 ligands. FASEB J : Off Publ Fed Am Soc Exp Biol 26(3):1280–1289. https://doi.org/10.1096/fj.11-188979
Podlech J, Ebert S, Becker M, Reddehase MJ, Stassen M, Lemmermann NA (2015) Mast cells: innate attractors recruiting protective CD8 T cells to sites of cytomegalovirus infection. Med Microbiol Immunol 204(3):327–334. https://doi.org/10.1007/s00430-015-0386-1
Ebert S, Becker M, Lemmermann NA, Buttner JK, Michel A, Taube C, Podlech J, Bohm V, Freitag K, Thomas D, Holtappels R, Reddehase MJ, Stassen M (2014) Mast cells expedite control of pulmonary murine cytomegalovirus infection by enhancing the recruitment of protective CD8 T cells to the lungs. PLoS Pathog 10(4):e1004100. https://doi.org/10.1371/journal.ppat.1004100
Ott VL, Cambier JC, Kappler J, Marrack P, Swanson BJ (2003) Mast cell-dependent migration of effector CD8+ T cells through production of leukotriene B4. Nat Immunol 4(10):974–981. https://doi.org/10.1038/ni971
Stelekati E, Bahri R, D'Orlando O, Orinska Z, Mittrucker HW, Langenhaun R, Glatzel M, Bollinger A, Paus R, Bulfone-Paus S (2009) Mast cell-mediated antigen presentation regulates CD8+ T cell effector functions. Immunity 31(4):665–676. https://doi.org/10.1016/j.immuni.2009.08.022
Li YS, Luo W, Zhu SA, Lei GH (2017) T cells in osteoarthritis: alterations and beyond. Front Immunol 8:356. https://doi.org/10.3389/fimmu.2017.00356
Woolley DE, Tetlow LC (2000) Mast cell activation and its relation to proinflammatory cytokine production in the rheumatoid lesion. Arthritis Res 2(1):65–74. https://doi.org/10.1186/ar70
Rivellese F, Nerviani A, Rossi FW, Marone G, Matucci-Cerinic M, de Paulis A, Pitzalis C (2017) Mast cells in rheumatoid arthritis: friends or foes? Autoimmun Rev 16(6):557–563. https://doi.org/10.1016/j.autrev.2017.04.001
Schuerwegh AJ, Dombrecht EJ, Stevens WJ, Van Offel JF, Bridts CH, De Clerck LS (2003) Influence of pro-inflammatory (IL-1 alpha, IL-6, TNF-alpha, IFN-gamma) and anti-inflammatory (IL-4) cytokines on chondrocyte function. Osteoarthr Cartil 11(9):681–687
Frenzel L, Hermine O (2013) Mast cells and inflammation. Joint, bone, spine : revue du rhumatisme 80 (2):141–145. doi:https://doi.org/10.1016/j.jbspin.2012.08.013
Shaik-Dasthagirisaheb YB, Conti P (2016) The role of mast cells in Alzheimer’s disease. Adv Clin Exp Med : Off Organ Wroclaw Med Univ 25(4):781–787. 10.17219/acem/61914
Folch J, Petrov D, Ettcheto M, Pedros I, Abad S, Beas-Zarate C, Lazarowski A, Marin M, Olloquequi J, Auladell C, Camins A (2015) Masitinib for the treatment of mild to moderate Alzheimer's disease. Expert Rev Neurother 15(6):587–596. https://doi.org/10.1586/14737175.2015.1045419
Xu D, Jiang HR, Kewin P, Li Y, Mu R, Fraser AR, Pitman N, Kurowska-Stolarska M, McKenzie AN, McInnes IB, Liew FY (2008) IL-33 exacerbates antigen-induced arthritis by activating mast cells. Proc Natl Acad Sci U S A 105(31):10913–10918. https://doi.org/10.1073/pnas.0801898105
Saluja R, Kumar A, Jain M, Goel SK, Jain A (2017) Role of Sphingosine-1-phosphate in mast cell functions and asthma and its regulation by non-coding RNA. Front Immunol 8:587. https://doi.org/10.3389/fimmu.2017.00587
Cahill KN, Katz HR, Cui J, Lai J, Kazani S, Crosby-Thompson A, Garofalo D, Castro M, Jarjour N, DiMango E, Erzurum S, Trevor JL, Shenoy K, Chinchilli VM, Wechsler ME, Laidlaw TM, Boyce JA, Israel E (2017) KIT inhibition by imatinib in patients with severe refractory asthma. N Engl J Med 376(20):1911–1920. https://doi.org/10.1056/NEJMoa1613125
Franceschini B, Ceva-Grimaldi G, Russo C, Dioguardi N, Grizzi F (2006) The complex functions of mast cells in chronic human liver diseases. Dig Dis Sci 51(12):2248–2256. https://doi.org/10.1007/s10620-006-9082-8
Bischoff SC (2016) Mast cells in gastrointestinal disorders. Eur J Pharmacol 778:139–145. https://doi.org/10.1016/j.ejphar.2016.02.018
Boeckxstaens G (2015) Mast cells and inflammatory bowel disease. Curr Opin Pharmacol 25:45–49. https://doi.org/10.1016/j.coph.2015.11.005
Gan PY, O'Sullivan KM, Ooi JD, Alikhan MA, Odobasic D, Summers SA, Kitching AR, Holdsworth SR (2016) Mast cell stabilization ameliorates autoimmune anti-myeloperoxidase glomerulonephritis. J Am Soc Nephrol : JASN 27(5):1321–1333. https://doi.org/10.1681/asn.2014090906
Elieh-Ali-Komi D, Cao Y (2017) Role of mast cells in the pathogenesis of multiple sclerosis and experimental autoimmune encephalomyelitis. Clin Rev Allergy Immunol 52(3):436–445. https://doi.org/10.1007/s12016-016-8595-y
Kolkhir P, Church MK, Weller K, Metz M, Schmetzer O, Maurer M (2017) Autoimmune chronic spontaneous urticaria: what we know and what we do not know. J Allergy Clin Immunol 139(6):1772–1781.e1771. https://doi.org/10.1016/j.jaci.2016.08.050
Rojanapremsuk T, Kasprowicz S, Schafer E, Story R, Clarke MS, Walls T, Snyder V, Gleason BC, Thomas AB, Cibull T (2015) Clinicopathologic findings in (anti-FcepsilonR1alpha) autoimmune-related chronic urticaria. J Cutan Pathol 42(5):329–332. https://doi.org/10.1111/cup.12471
Zebrowska A, Wagrowska-Danilewicz M (2014) Mediators of mast cells in bullous pemphigoid and dermatitis. Herpetiformis 2014:936545. https://doi.org/10.1155/2014/936545
Chen R, Ning G, Zhao ML, Fleming MG, Diaz LA, Werb Z, Liu Z (2001) Mast cells play a key role in neutrophil recruitment in experimental bullous pemphigoid. J Clin Invest 108(8):1151–1158. https://doi.org/10.1172/jci11494
Ujiie H, Nishie W, Shimizu H (2012) Pathogenesis of bullous pemphigoid. Immunol Allergy Clin N Am 32(2):207–215, v. https://doi.org/10.1016/j.iac.2012.04.001
Betto E, Usuelli V, Mandelli A, Badami E, Sorini C, Capolla S, Danelli L, Frossi B, Guarnotta C, Ingrao S, Tripodo C, Pucillo C, Gri G, Falcone M (2017) Mast cells contribute to autoimmune diabetes by releasing interleukin-6 and failing to acquire a tolerogenic IL-10+ phenotype. Clin Immunol (Orlando, Fla) 178:29–38. https://doi.org/10.1016/j.clim.2015.12.013
Conti P, Kempuraj D (2016) Important role of mast cells in multiple sclerosis. Mult sclerosis and Relat Disord 5:77–80. https://doi.org/10.1016/j.msard.2015.11.005
Kawikova I, Askenase PW (2015) Diagnostic and therapeutic potentials of exosomes in CNS diseases. Brain Res 1617:63–71. https://doi.org/10.1016/j.brainres.2014.09.070
Carroll-Portillo A, Surviladze Z, Cambi A, Lidke DS, Wilson BS (2012) Mast cell synapses and exosomes: membrane contacts for information exchange. Front Immunol 3:46. https://doi.org/10.3389/fimmu.2012.00046
Lenassi M, Cagney G, Liao M, Vaupotic T, Bartholomeeusen K, Cheng Y, Krogan NJ, Plemenitas A, Peterlin BM (2010) HIV Nef is secreted in exosomes and triggers apoptosis in bystander CD4+ T cells. Traffic (Copenhagen, Denmark) 11(1):110–122. https://doi.org/10.1111/j.1600-0854.2009.01006.x
Li F, Wang Y, Lin L, Wang J, Xiao H, Li J, Peng X, Dai H, Li L (2016) Mast cell-derived exosomes promote Th2 cell differentiation via OX40L-OX40 ligation. J Immunol Res 2016:3623898. https://doi.org/10.1155/2016/3623898
Grimbaldeston MA, Metz M, Yu M, Tsai M, Galli SJ (2006) Effector and potential immunoregulatory roles of mast cells in IgE-associated acquired immune responses. Curr Opin Immunol 18(6):751–760. https://doi.org/10.1016/j.coi.2006.09.011
Hong GU, Lim JY, Kim NG, Shin JH, Ro JY (2015) IgE and IgA produced by OX40-OX40L or CD40-CD40L interaction in B cells-mast cells re-activate FcepsilonRI or FcalphaRI on mast cells in mouse allergic asthma. Eur J Pharmacol 754:199–210. https://doi.org/10.1016/j.ejphar.2015.02.023
Hong GU, Park BS, Park JW, Kim SY, Ro JY (2013) IgE production in CD40/CD40L cross-talk of Band mast cells and mediator release via TGase 2 in mouse allergic asthma. Cell Signal 25(6):1514–1525. https://doi.org/10.1016/j.cellsig.2013.03.010
Mekori YA, Hershko AY (2012) T cell-mediated modulation of mast cell function: heterotypic adhesion-induced stimulatory or inhibitory effects. Front Immunol 3:6. https://doi.org/10.3389/fimmu.2012.00006
Mekori YA, Hershko AY, Frossi B, Mion F, Pucillo CE (2016) Integrating innate and adaptive immune cells: mast cells as crossroads between regulatory and effector B and T cells. Eur J Pharmacol 778:84–89. https://doi.org/10.1016/j.ejphar.2015.03.087
Gong J, Yang NS, Croft M, Weng IC, Sun L, Liu FT, Chen SS (2010) The antigen presentation function of bone marrow-derived mast cells is spatiotemporally restricted to a subset expressing high levels of cell surface FcepsilonRI and MHC II. BMC Immunol 11:34. https://doi.org/10.1186/1471-2172-11-34
Shefler I, Mekori YA, Mor A (2008) Stimulation of human mast cells by activated T cells leads to N-Ras activation through Ras guanine nucleotide releasing protein 1. J Allergy Clin Immunol 122(6):1222–1225. https://doi.org/10.1016/j.jaci.2008.07.024
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
I hereby state that none of the coauthors and the corresponding author of this paper have a conflict of interest, and it has been prepared for publication without using any funding. Moreover, the paper does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Elieh Ali Komi, D., Grauwet, K. Role of Mast Cells in Regulation of T Cell Responses in Experimental and Clinical Settings. Clinic Rev Allerg Immunol 54, 432–445 (2018). https://doi.org/10.1007/s12016-017-8646-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-017-8646-z