Abstract
HIV infection continues to be a serious health issue with an alarming global spread, owing to the fact that attempts at developing an effective vaccine or a permanent cure remains futile. So far, the only available treatment for the clinical management of HIV is the combined Anti-Retroviral Therapy (cART), but the long-term cART is associated with metabolic changes, organ damages, and development and transmission of drug resistant HIV strains. Thus, there is a need for the development of one-time curative treatment for HIV infection. The allogeneic transplantation with the Hematopoietic Stem and Progenitor cells (HSPCs) having 32 bp deletion in Chemokine receptor 5 gene (CCR5 Δ32) demonstrated successful HIV remission in the Berlin and London patients, and highlighted that transplantation of CCR5 null HSPCs is a promising approach for a long- term HIV remission. The advent of gene editing technologies offers a new choice of generating ex vivo CCR5 ablated allogeneic or autologous HSPCs for stem cell transplantation into HIV patients. Many groups are attempting CCR5 disruption in HSPCs using various gene-editing strategies. At least two such studies, involving CCR5 gene editing in HSPCs have entered the clinical trials. This review aims to outline the strategies taken for CCR5 gene editing and discuss the challenges associated with the development of CCR5 manipulated HSPCs for the gene therapy of HIV infection.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Human Immunodeficiency Virus-1 (HIV-1) infection was identified in 1983 as the causative retrovirus of Acquired Immunodeficiency Syndrome (AIDS), and it still remains as an incurable immune disease in spite of decades of dedicated research. Moreover, the clinical management of the deadly HIV-1 infection grows more challenging due to generation or resistant strains and the stable latent HIV-1 reservoirs in various tissues and hematopoietic cells.
The ART is the current standard of care for HIV-1 positive patients in which antagonists against one or different steps of HIV-1 infection such as entry and propagation are administered. This includes reverse transcriptase inhibitors, protease inhibitors and integrase inhibitors. In 1987, zidovudine (AZT) was developed as the first anti-retroviral drug, which reduced the perinatal transmission of HIV [1]. The availability of saquinavir, a protease inhibitor drug, opened the possibility of Highly Activated Anti-retroviral therapy (HAART) in which multiple drugs are administered in combination to suppress the virus propagation [2]. HAART was acknowledged as an advanced treatment for HIV-1 infection. Anti-retroviral therapy is functional in lowering the patient’s total burden of HIV-1 by continuously removing the detectable levels of virus from the system, thereby delaying the progression to AIDS and prolonging the lives of individuals. Though an effective treatment strategy, ART does not provide a permanent cure since the risk from latent viral reservoirs persists. Recent findings indicate that HIV-1 also infects the HSPCs. The HIV-1 integrates its entire genome into the host cells and persist without producing infectious viruses, which is known as latency [3]. Latency enables the infected cells from evading immune recognition and clearance, which can lead to the establishment of reservoirs in the HSPCs. As the infected HSPCs self-renew and differentiate into hematopoietic lineages throughout their lifetime, it results in the retention of viremia in the patient. The other drawback is that, though the cART keeps the HIV-1 RNA levels undetectable in HIV-1 infected patients, it does not eliminate the latent proviral DNA. The patients are dependent on cART for lifetime to suppress the HIV-1 replication from the latent proviral DNA as the interruption of cART leads to viral rebound [4]. Also, long-term cART exposure is associated with the development of drug resistant strains of HIV-1 and metabolic changes in the host cells resulting in organ damages [5].
Many attempts to develop vaccines against the HIV proved futile with very few reaching the clinical trials and none of the studies producing sufficient therapeutic effect. The RV144 trial of 2009 was the only recorded vaccine clinical trial demonstrating an appreciable efficacy of 31.2% [6]. Even a fairly recent HIV-1 vaccine trial HVTN702, conducted among the South African individuals by National Institute of Health (USA), was discontinued due to its ineffectiveness [7].
The identification of HIV-1 viral tropism and the essential co-receptors, CCR5 and CXCR4, mediating the HIV-1 entry, resulted in the emergence of co-receptor targeted treatment as an alternative for cART or as an additive treatment along with the cART [8]. The inhibition of CCR5 with maraviroc, a small molecule that selectively blocks CCR5, led to the restriction of HIV-1 entry into the immune cells and showed a significant level of viral suppression and improved CD4 cell count at 48 weeks follow up [9]. Maraviroc has now been approved by the FDA for the treatment of HIV-1. The inhibition of CXCR4 with AMD3100 or both the CCR5 and CXCR4 with AMD3541 are the other options available. Thus, co-receptor targeted treatment is an exciting approach towards HIV treatment [10]. The cure for HIV could be the sterilizing cure (complete elimination of virus), functional cure (suppression of viral load) or remission (undetectable viral load). In this review, we will focus on various gene editing strategies and challenges associated with genetic ablation of CCR5 receptor in HSPCs for HIV-1 gene therapy.
The CCR5 and CXCR4 Co-Receptor Mediated HIV Infection
HIV-1 enters the immune cells through CD4 receptors and it establishes infection by the following steps; 1) Fusion with the cell membrane 2) Reverse transcription of its RNA to DNA 3) Integration of viral DNA in the host DNA 4) transcription and translation of viral DNA 5) Viral assembly and destruction of host cell, leading to immune cell depletion. The major depletion of immune cells eventually results in AIDS (Fig. 1).
Co-receptor mediated HIV infection: 1. R5 HIV-1 finds CD4 expressing cells (Macrophages and T-cells) 2. Establishment of interaction with CD4 receptor and gp120 of HIV 3. Recruitment of CCR5 co-receptor and binding of co-receptor for fusion 4. HIV starts releasing viral Capsid into target cells 5. Released capsid in target cells 6. Release of viral RNA into the target cells 7. Reverse transcription of viral RNA into cDNA. 8. Proviral DNA integration into host genome
The chemokine receptors, CCR5 and CXCR4 play a critical role as co-receptors for HIV-1 infection. CCR5 belongs to G protein coupled receptor family encoded in the short arm of chromosome 3 and it is expressed on the immune cells such as CD4 T cells, macrophages and dendritic cells. The CXCR4 encoded in the chromosome 2 is expressed on the cell surface of hematopoietic cells and are specific for stromal cell-derived factor-1. The HIV-1 envelope glycoprotein(gp) is composed of spikes formed from trimers of gp120-gp41 heterodimers. During infection, the gp120 external subunit binds to the CD4 receptor by acting as a chemokine mimic, followed by a conformational change in the envelope proteins, that exposes the gp41 transmembrane subunit. Gp41 now interacts with either CCR5 or CXCR4, the choice of which determines the viral tropism, thereby fusing with the target cell membrane to deliver the viral capsid. There are mainly 3 HIV-1 tropisms based on co-receptor usage for host cell entry– R5 (CCR5 utilizing), X4 (CXCR4 utilizing) and R5X4 (utilizing both the receptors) [11]. R5 HIV tropism initiates the early stage of infection and at later stages, toward the progression of AIDS, the more virulent X4 tropism becomes prevalent [12, 13].
HIV-1 Remission through CCR5 Δ32 Allogenic Haematopoietic Stem Cell Transplantation
Approximately, 1% of European population have a homozygous CCR5∆32 genotype that leads to the absence of CCR5 expression, imparting natural HIV-1 resistance [14]. Allogeneic stem cell transplantation with the HSPCs harvested from such CCR5 ∆32 donors have shown promising results against R5 tropic HIV-1 infection.
Hütter et al., (2009) reported the first breakthrough case of HIV remission, famously known as the Berlin patient [15]. The Berlin patient was diagnosed as HIV-1 positive and underwent HAART for 4 years. In 2006, he was diagnosed with Acute Myeloid Leukemia (AML). Stem cell transplantation was carried out from an HLA matched (10/10) donor with the homozygous CCR5∆32 genotype. This patient underwent a rigorous conditioning regimen with the total body irradiation (TBI) and cyclophosphamide. Due to AML relapse after the first transplantation, he underwent second stem cell transplantation from the same donor. Long-term follow-up of Berlin patient showed 100% chimerism having CCR5 ∆32 Homozygous genotype with no detectable viral load in his Lymph nodes, gut, brain and CD4 cells [16].
Recently, a second patient popularly termed as the London patient achieved HIV-1 remission through the same approach. Similar to the first case, he underwent HSPC transplantation from a.
HLA matched (9/10) donor with homozygous ∆32 genotype and ART was discontinued 16 months post transplantation [17]. Viral rebound was not observed even after 30 months of ART withdrawal. The HIV-1 reservoir, analyzed with a highly sensitive assay, indicated no detectable viral load in body fluids such as semen, plasma as well as lymphoid organs, rectum, caecum, sigmoid colon and terminal ileum. However, low levels of viral load were observed in CD4 Central memory T cells and lymph node tissues and the positive signal for LTR and env indicated that the sterilizing cure might require a longer time.
Further HIV-1 related illnesses have not appeared in both the Berlin and London patients even after ART withdrawal for 12 years and 30 months respectively. These results provided the evidence for a successful HIV-1 remission using CCR5 null HSPCs. The clinical outcomes of the Berlin and London patients are listed in Table 1. The sterilizing cure in these patients is still unknown as low levels of HIV-1 viral RNA and proviral DNA were detected in some tissues of both the patients on long term follow up. Low copy of HIV-1 RNA was detected in Plasma and Rectum in Berlin patient which was negative in London patient whereas, defective proviral DNA of HIV-1 was detected in both the Berlin and London patients. Noteworthy, Env and LTR sequences of the viral genome were detected in the lymph node of the London patient but Integrase and Ψ were absent, which led to the inability to produce infectious HIV-1 particle [18].
Whether the eradication of previously established HIV-1 reservoirs in Berlin patient was due to the allogenic HSCT or the intense conditioning regimen involving total body irradiation, remains unclear. The SHIV infected monkeys which received total body irradiation were observed to have a rapid depletion of peripheral blood CD4 cells than CD4 cells in lymphoid tissues such as spleen and axillary lymph nodes. Only 30 to 40% of CD4 cells were depleted in spleen, indicating that the residual HIV-1 infected cells could still persist in lymphoid tissues and TBI may not be sufficient to eliminate the viral reservoirs [19]. In line with this, another study demonstrated an effective reduction of HIV-1 reservoirs in lymphoid tissues in the HIV-1 infected monkeys which were transplanted with CCR5 modified autologous stem cells. These findings suggest that the CCR5 modified stem cells but not the total body irradiation eliminate the viral reservoirs on long term [20]. This notion is further strengthened by the remission of the London patient who did not undergo total body irradiation. The undetectable levels of reservoir in most of the tissue samples and peripheral blood samples in both London and Berlin patients proved that CCR5 null HSPC transplantation will eradicate the tissue resident HIV-1 latent reservoirs. This is further proved by the failure of the usage of allogenic stem cells with the wild type CCR5 or heterozygous CCR5∆32 genotype in HIV infected patients to cease viral rebound upon ART withdrawal [21].
Overall, Allogenic stem cell transplantation from donor harboring ∆32 genotype is a promising approach to achieve HIV-1 remission.
Remission against R5 Tropic Virus by CCR5 Disruption
Drug Mediated CCR5 Inhibition Improves CD4 Cell Count
After the pioneering work of Cocchi et al., demonstrating CCR5 as an essential coreceptor utilized by R5 tropic HIV-1 virus for the entry into T-cells and macrophages, it has been validated and established as a standard therapeutic target against HIV-1.
Several CCR5 antagonists were identified by high throughput pharmacological screening and these antagonists stabilize the inactive CCR5 protein thus restricting the binding of chemokines and gp120 [22]. Maraviroc, a CCR5 antagonist showed promising results in the clinical trials with minimal toxicity, low HIV-1 RNA copies and improved CD4 cell count [23, 24]. .Maraviroc binds to the extracellular loop of CCR5 protein and induces the confirmational change there by it prevents the HIV-1 interaction with the CCR5 receptor. Subsequently, several other chemokine drugs such as Vicriviroc and aplaviroc potentially supressed HIV-1 for 24 months, but eventually led to the development of malignancies [25], and hepatotoxicity [26]. Resistance against CCR5 targeting drugs were also reported, thereby challenging its long-term efficacy.
Disruption of CCR5 Gene Using Genome Editing Approaches
Recently developed gene editing tools like Zing Finger Nucleases (ZFN), Transcription Activator like Effector nucleases (TALEN) and Clustered Regularly Interspaced Short palindromic repeats (CRISPR-Cas9) allows scientists to knockout CCR5 protein by inducing DNA double strand breaks (DSB) at the open reading frame of CCR5 in immune cells as well as hematopoietic stem cells.
B.1 ZFN Mediated CCR5 Disruption
ZFNs are artificially created heterodimers synthesized by fusing Zing finger DNA binding domain and DNA cleaving domain. DNA binding domain consists of two zinc finger modules which allow recognition of unique hexamer sequence in the genome. DNA cleavage domain comprises FokI endonuclease, which upon dimerization at the recognition of DNA binding domain, cleaves the DNA leading to the formation of DSBs at the target locus. The DNA repair, by the non-homologous end joining repair pathway, leads to incorporation/substitution/deletion of nucleotides preventing the expression of a functional protein. Several studies have demonstrated CCR5 disruption using ZFN in CD4 cells and HSPCs.
Adenovirus mediated transient expression of ZFN targeting the first transmembrane domain of CCR5 protein in human CD4 cells induced CCR5 disruption to a mean frequency of 50%. The CCR5 disrupted CD4 cells displayed R5-HIV-1 resistance in vitro as well as in vivo. The engraftment studies in NOG mice showed a reduced viral load and increased CD4 cell count with 3-fold selective enrichment of CCR5 negative cells upon HIV-1 infection [27]. Sangamo therapeutics carried out a clinical trial with 12 HIV-1 infected individuals who were under ART. The autologous CD4 cells were collected from the patients. CCR5 was edited with ZFN and infused back into the patients. During ART interruption, the wildtype CD4 cells started declining whereas CCR5 modified CD4 T cells remained stable. Although ZFN mediated CCR5 edited CD4 cells were safe in human subjects, complete HIV-1 remission was not observed, possibly due to the low gene editing efficiency and persistence of reservoir in other tissues [28]. Simultaneous editing of CCR5 and CXCR4 in human CD4 cells provided protection against X4 and R5 tropic virus in mice [29, 30].
.
ZFNs are also being used to edit the CCR5 in the HSPCs. Ad5/F35-mediated delivery of ZFN into HSPCs can edit the cells, but with the low efficiency of 5% indels. They were able to increase the editing frequency up to 30% with Protein Kinase C activators. The PKC activators work through the ERK/MEK pathway to improve the gene editing efficiency. The CCR5 modified adult HSPCs retained multilineage potential in NSG mice and exhibited R5-tropic HIV-1 resistance [31, 32].
To overcome the toxicities associated with plasmid DNA or the Ad5/F35, ZFN encoding mRNA was delivered through electroporation which helped to achieve maximum of 50% gene editing efficiency with minimal toxicity [33]. This approach has reached the clinical trial (#NCT02500849).
To achieve an efficiency of 100% manipulation of CCR5 locus, ZFN mRNA was electroporated with AAV6 donor template encoding green fluorescent protein into the adult mobilized peripheral blood HSPCs. This strategy allows the selection of CCR5 edited cells for the transplantation by sorting the GFP positive cells [34]. .However, clinical translation of such a strategy will be challenging. Other approaches employed to enrich gene modified stem cells in the mice include over-expression of the aldehyde dehydrogenase-1 or the mutant drug resistant Methylguanine methyltransferse in HSPCs using lentiviral vectors which provide cellular resistance against cytotoxic agents such as cyclophosphamide and temozolomide. By using this approach they observed a significant increase in the number of gene modified cells in the mice and non-human primate models [35, 36].
Disruption of CCR5 gene in autologous HSPCs from monkeys were also reported. These studies showed 64% modification in ex vivo and 40% in vivo after transplantation. CCR5 disrupted HSPCs retained engraftment and multi lineage potential in a large animal model [37]. Also, CCR5 modified immune cells were found in the gut and lymph nodes, where HIV-1 infected latent reservoirs are usually predominant, indicating a successful replacement of HIV-1 infected reservoir cells by CCR5 modified cells. The protected CCR5 modified cells had the potential to eradicate the viral reservoirs through graft versus HIV-1 effect. However, long term follow up results from the same monkeys showed reduction in the frequency of CCR5 modification from 40% to 4%, which may not be sufficient for long-term ART free viral remission [20].
B.2 TALEN Mediated CCR5 Disruption
TALE was identified as a natural protein in the plant pathogenic bacteria Xanthomonas Species. It is artificially engineered to fuse Fok1 nuclease at C-terminus of TALE and used for targeted genome editing. Plasmids encoding variants of TALENs were transfected into HEK293T cells to obtain 45% gene editing of CCR5 locus with better viability and less off-targets than ZFN [38]. Delivery of TALEN into the cells in plasmid form is associated with severe cytotoxicity. To overcome this barrier, another study showed fusion of cell penetrating peptide TAT with TALEN which demonstrated a 5% modification frequency of CCR5 locus in human iPSCs (induced pluripotent cells) [39]. Subsequently, TALEN encoding mRNA transfection in PM1 cell line and Human primary T cells showed an increased editing frequency of about 90% and 50% respectively [40]. In addition, Shi et al screened 28 novel TALENs in GHOST-CCR5-CXCR4 cell line and Human Primary CD4 cells. They observed that the TALEN mediated CCR5 disrupted cells confer HIV-1 resistance with low cytotoxicity than ZFN [41].
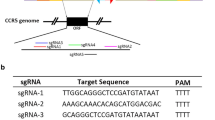
B.3 CRISPR/Cas9 Mediated CCR5 Ablation
CRISPR/Cas9 is the bacterial innate immune system which destroys the invading viruses. The locus targeting is achieved through sgRNA which is made up of CRISPR RNA and trans-acting RNA while the target cleavage is achieved by Cas nuclease.
Initially, CRISPR/Cas9 was delivered as plasmids and expressed under the Pol III promoter which resulted in lower gene editing efficiency [42]. Recent advancements simplified two RNA into single synthetic guide RNA and increased the stability by incorporating phosphothiorate modifications, thus improving the targeting and cleavage activity [43,44,45,46]. Similar to ZFNs and TALENS, CRISPR/Cas9 has also shown to disrupt the CCR5 in both CD4 T cells and in human HSPCs with an efficiency of 42% and 34% respectively [47]. .Comparative studies with TALEN and CRISPR/Cas9 targeting CCR5 gene in HEK293T cells showed enhanced editing with CRISPR/Cas9 [48].
AAV mediated delivery of individual CRSIPR/Cas9 components into CD4 cells led to the ablation of CCR5 protein up to 30% [49] Packing of both Cas9 and sgRNA components into a single AAV construct could increase the efficiency but the size of spCas9 prevents the feasibility of such efforts. In an alternative approach to overcome size restrictions, a smaller Cas9 isolated from Staphylococcus aureus was used and this resulted in successful modification of CCR5 gene in primary CD4 cells and HSPCs [50]. CRISPR/Cas9 mediated CCR5 ablation in human fetal liver derived HSPCs exhibited engraftment and multilineage potential. Immune cells derived from the CCR5 ablated HSPCs displayed HIV-1 resistance in NPG mice [51].
Lentiviral vector encoding CRISPR/Cas9 against CCR5 locus were transduced into monkey HSPCs to ablate CCR5 gene. GFP expressing lentiviral vector was used as control. Before infusion, GFP expression was found to be 70% and after 8 months of infusion it went down to 6.5%. Notably, CCR5 modified cells were increased upto 3-fold upon ART withdrawal after 8 months of transplantation but SIV remission was not achieved due to lower editing frequency [52].
In addition, early data presented in 5’th conference on cell and gene therapy for HIV-1 cure 2019 indicated that the ZFN mediated CCR5 modified autologous hematopoietic stem and progenitor cells were engrafted in HIV-1 patients with successful establishment of multilineage reconstitution potential in two different cohorts. Several clinical trials with the aim of HIV cure using various gene therapy approaches are listed in Table 2.
Challenges Associated with CCR5 Editing in HSPCs
Despite the extensive studies on the HIV-1 infection throughout the years, successful HIV remission has been attained only in two cases. The time duration between the Berlin and London cases are almost a decade, which indicates that CCR5∆32 homozyogous transplantation is restricted by multiple factors including donor availability, viral rebound and transplantation- associated risks. Some of these factors may also hamper the progress of HSPCs gene editing therapy (Fig. 2).
Failure of HSPCs Mobilization in HIV-1 Patients
The minimum cell dose of at least 5 × 106 HSPCs per kg of patient is recommended for manipulation and subsequent autologous or allogenic transplantation. While such collection can be achieved in healthy donors with the mobilization reagents like G-CSF and Plerixafor, the feasibility of such a harvest in the HIV-1 infected persons are unclear. The London patient initially underwent CXCR4 based mobilization reagents for the stem cell harvest which was a failure. Another study showed G-CSF mobilization failure in 27% of the study population consisting of 155 HIV-1 patients. This frequency is relatively high when compared with the healthy individuals where the mobilization failure rates are around 5% [53, 54]. Recently City of Hope with Sangamo therapeutics attempted two rounds of mobilization in HIV infected individuals using both Plerixafor and G-CSF to harvest 7.5 × 106 HSPCs/kg. The reasons for poor mobilization with available mobilizing agent in HIV infected individuals are largely unknown.
The Un-Optimized Conditioning Regimen
The conditioning regimen plays a critical role in the success of the gene therapy as poor conditioning may dilute the frequency of CCR5 edited HSPCs fraction. The Berlin patient was subjected to high intensity conditioning with TBI and cyclophosphamide whereas the London patient received just the cyclophosphamide treatment. Cyclophosphamide with TBI was used in Chinese clinical trial where HLA matched allogenic HSPCs were edited for CCR5 using CRISPR/Cas9 and transplanted (NCT03164135.) The ongoing clinical trial by City of Hope with Sangamo therapeutics tested two doses of busulphan in two cohorts and they observed an increased CD4 T cell reconstitution in the cohorts which received high dose of busulphan (NCT02500849). There are not many studies, testing the optimal conditioning regimen for the transplantation of CCR5 modified HSPCs. The conditioning regimen may reduce the viral load which may have beneficial effect during the engraftment of gene edited HSPCs.
Graft Versus Host Disease
Autologous HSPCs are the optimal candidates for CCR5 gene editing as they don’t provoke GVHD. However, HIV infected patients having following issues such as 1) haematological malignancies 2) Poor HSPC mobilization 3) Poor quality of HSPCs, need CCR5 manipulation only in allogenic HSPCs from HLA matched donors. While this could be an interesting strategy, there is a risk of GVHD associated with this approach. Such GVHD was reported in a patient with HIV who received ex vivo CCR5 manipulated allogenic HSPCs from fully matched HLA matched donor [55]. This warns GVHD is a critical factor during stem cell transplantation.
The Low-Frequency of Gene Edited Cells In Vivo
The first-in-human case report with CRISPR/Cas9 mediated CCR5 gene edited HSPCs transplantation proved to be safe but showed poor efficacy against HIV-1 infection. The editing efficiency of the infused product was 17.8% which was considerably low and this declined to 2.5% in vivo. Similar to this trial, preliminary results from the City of Hope with Sangomo trial showed that the editing frequency of pre-infusion product was about 23% and 28% in cohort 1 and cohort 2 respectively. But only 4% of the engrafted CD4 T cells retained the gene modification after 800 days of transplantation (NCT02500849). This may be due to the following reasons; 1) The frequency of long-term re-populating stem cells or gene editing in the long-term re-populating stem cells is very low 2) The heterozygous CCR5 editing may not provide resistance against HIV, as the edited cells are eliminated by the infection, causing a reduction in the frequency of these cells 3) Purity of CD34+ HSPCs used for the manipulation is low. The Chinese trial had only 71% of cells positive for the CD34 marker (NCT03164135). 4) The gene-manipulation procedure needs further optimization. The Chinese study used the research scale electroporation for repeated electroporations to manipulate a large dose of HSPCs. This may result in variation in the gene editing frequency. A clinical scale electroporation would be preferable to avoid variations in the gene editing.
The Pre-Existing X4-Tropic Virus
Similar to the Berlin and London patients, the Essen patient was transplanted with CCR5Δ32/Δ32 HSPCs in an allogenic setup. However, unlike the previous cases, a viral rebound was observed in the Essen patient on long term follow-up. The findings showed the presence of a minor fraction of X4- tropic viruses before the transplantation and these viruses infected the engrafted CCR5Δ32/Δ32 HSPCs using CXCR4 receptor. Furthermore, patient screening data from the City of Hope with Sangamo therapeutics showed that 40% of the individuals had X4-tropic HIV. The pre-existing X4-tropic HIV could still infect the CCR5 gene edited cells and cause failure of gene therapy. While CCR5 disruption is a feasible approach in HSPCs, the disruption of CXCR4 in HSPCs may lead to defects in the homing and engraftment potential of gene edited HSPCs in the bone marrow [56].
Cell to Cell Transmission of HIV
Cell to cell transmission of HIV-1 is higher than cell free receptor dependent viral infections. The formation of viral synapses between the infected and non-infected T cells and the phagocytosis of infected, dying and dead T-cells by macrophages are observed to be the mechanism of cell to cell transmission of HIV-1 [57]. Both R5 and X4 tropic viruses can be transmitted through this mechanism. Blocking cell to cell transmission of HIV-1 is deemed more challenging, both with broadly neutralizing antibodies and cART. Whether the genetic ablation of CCR5 could prevent such cell-to-cell transmission of HIV is yet to be explored.
Co-culturing of macrophages harvested from homozygous ∆32 individuals, with CCR5 positive peripheral blood nuclear cells, renders conversion of CCR5-ve cells to CCR5+ve cells and make them susceptible to R5-tropic HIV-1 infection. The study proved that the CCR5 protein is transferred from positive cells to negative cells through micro vesicles. The inhibition of extracellular vesicle formation blocks the CCR5 transfer. The transfer of CCR5 protein from peripheral mononuclear cells to endothelial cells during trans-endothelial migration is also observed, which suggests that, CCR5-ve cells can also be infected by HIV through acquired CCR5 receptor from CCR5+ve cells [58]. Another study proved that even the truncated CCR5 protein retains its functional properties in HEK293T cells [59]. .All these findings recommend for the validation of CCR5 null CD4 T cells and macrophages against cell to cell transmission of HIV-1.
HSPCs Harbouring HIV DNA
All subpopulations of T-cells carry similar levels of intact HIV-1 proviral DNA and the infectious virus can be formed from any of these subpopulations [60]. .Several studies have proved that HIV-1 infects the hematopoietic progenitor cells, leading to haematological abnormalities and cytotoxicity. HSPCs isolated from HIV-1 infected individuals with high viral load showed gag induction on culturing with GM-CSF and TNF-α This indicates that the HSPCs harbour HIV-1 proviral DNA [61, 62]. However, HIV-1 infection in the subpopulations of HSPCs and the induction of virus formation during lineage differentiation are poorly understood. About 1% of HSPCs express CD4/CCR5 receptors and 2.5% of HSPCs express CD4/CXCR4 receptors possibly causing the R5 and X4 tropic HIV-1 infection leading to establishment of latent reservoirs in them [63]. HSPCs are heterogenous in nature and certain subpopulations contribute to long term engraftment. Hence, HIV-1 infectivity and inducibility among different population of HSPCs needs to be extensively validated with large number of donors.
CCR5 and CXCR4 Independent HIV-1 Infections
Extracellular vesicles and HIV-1 particles are relatively same in size and composition and they are surrounded by lipid bilayer with glycoproteins. Megakaryocytes derived extracellular vesicles (EV) are shown to be endocytosed by the HSPCs [64].Recent studies also indicated that the HIV-1 infected dendritic cells and macrophages release exosome particles with HIV-1 proteins and RNA molecules which might be endocytosed by the HSPCs. This process may establish HIV-1 infection in CD4 null primitive HSPCs [65]. .The in vitro demonstrations of EV mediated HIV-1 infection of HSPCs is hugely impaired by limitations such as lysis of HSPCs on treatment with HIV-1 core proteins. This concept needs to be tested with a robust platform [66].
Conclusion and Future Perspectives
The whole-exome sequencing along with the whole-genome genotyping has demonstrated that there are no increased mortality risks for the ∆32 CCR5 homozygous individuals compared to CCR5 positive individuals. Henceforth, generating CCR5 null genotype has been a primary goal in the HIV gene therapy field. Various gene editing tools and strategies are being employed to create CCR5 edited HSPCs. The key challenges in translating this approach appear to be the presence of X4 tropic virus, mobilisation of HSPCs, quality of the cells for manipulation and the gene editing efficiency. Careful selection of patients who are just started with ART may avoid issues associated with CXCR4 tropic viral rebound. Mobilisation of HSPCs and the quality of mobilised product can be a hurdle but the infusion of even the low doses of CCR5 edited HSPCs could still provide benefits as these cells will not be cleared by the virus. Recent reports suggest that pre-existing HIV-1 infection does not affect the engraftment potential of the Hematopoietic stem cells in mice [67] CCR5 gene editing in allogenic stem cell transplantation could be another strategy to circumvent the mobilisation issues and poor quality of HSPCs in these patients.
Recent clinical trial report of gene edited autologous HSPCs for Sickle cell disease and β-thalassemia demonstrated the engraftment and multilineage potential of gene edited HSPCs. The efficacy in terms of functional hemoglobin production is superior in the gene editing study than the reports shown from lentiviral gene therapy studies. The adverse events were mainly associated with the conditioning regimens. This indicates CRISPR/Cas9 modification in autologous HSPCs is a feasible approach and this can be done for HIV patients [68]. The major concern in CRISPR/Cas9 editing is an unintended off target cleavage. Several techniques such as Whole genome sequencing, GUIDE-Seq and DISCOVER-Seq are now available to detect the off-targets [69]. The extensive off-target analysis by two different techniques is critical to ensure that the selected sgRNA is devoid of any unwarranted site binding. Also, the acceptable frequencies of off-target edits is yet to be identified. With the emergence of expansion protocols for cord blood HSPCs using small molecules like SR-1 and UM-171, it would be beneficial to edit the CCR5 in cord blood HSPCs and expand them for transplantation. The Hematopoietic progenitor cells derived from iPSCs are yet to demonstrated for its stemness and differentiation potential. The development of engraftable HSPCs from iPSCs would be an ideal system for HSPC gene therapy as the haplotype characterized iPSCs would be the donor for many patients and it could be off-the-shelf product.
The recent advances in the gene editing field such as non-viral delivery of Cas9 ribonucleo proteins, incorporation of 3X-nuclear localization signal to spCas9 and use of HiFi Cas9 with chemically modified sgRNAs can be combined with the recent advances in the transplantation field such as the targeted conditioning of HSPCs with AMG-191 monoclonal antibody which binds to CD117 (c-Kit), the fully closed- automated platforms for HSPCs purification and gene editing and the Intra-bone administration of gene modified HSPCs [70]. Another, strategy for reducing the cost of gene therapy is by infusing low dose of gene modified primitive HSPC fractions marked by CD34 + CD90 + CD45RA-,which can engraft better as shown in preclinical animal studies in non-human primates and mice [71,72,73] .This could be a potential way forward for the development of an efficient gene editing therapy for HIV.
Data Availability
Not applicable.
Abbreviations
- cART:
-
combined Anti-Retroviral Therapy
- HSPCs:
-
Hematopoietic Stem and Progenitor cells
- CCR5:
-
Chemokine receptor 5
- HIV-1:
-
Human Immunodeficiency Virus-1
- AIDS:
-
Acquired Immunodeficiency Syndrome
- AZT:
-
zidovudine
- HAART:
-
Highly Activated Anti-retroviral therapy
- AML:
-
Acute Myeloid Leukemia
- TBI:
-
Total body irradiation
- R5:
-
CCR5 utilizing HIV virus
- X4:
-
CXCR4 utilizing HIV virus
- gp:
-
glycoprotein
References
Fischl MA, Richman DD, Grieco MH, Gottlieb MS, Volberding PA, Laskin OL, et al. The efficacy of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. The New England Journal of Medicine [Internet]. 1987 Jul 23 [cited 2019 May 22];317(4):185–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3299089.
Collier AC, Coombs RW, Schoenfeld DA, Bassett RL, Timpone J, Baruch A, et al. Treatment of human immunodeficiency virus infection with saquinavir, zidovudine, and zalcitabine. The New England Journal of Medicine [Internet]. 1996 Apr 18 [cited 2019 May 22];334(16):1011–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8598838.
Wiegand A, Spindler J, Hong FF, Shaoc W, Cyktor JC, Cillo AR, et al. Single-cell analysis of HIV-1 transcriptional activity reveals expression of proviruses in expanded clones during ART. Proceedings of the National Academy of Sciences of the United States of America [Internet]. 2017 May 2 [cited 2020 Apr 21];114(18):E3659–68. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28416661.
Bertrand L, Cho HJ, Toborek M. Blood-brain barrier pericytes as a target for HIV-1 infection. [cited 2020 Apr 21]; Available from: https://academic.oup.com/brain/article-abstract/142/3/502/5298568
Montessori V, Press N, Harris M, Akagi L, Montaner JSG. 20040120S00033P229 Sudah. 2004;170(2):229–38.
Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, et al. Vaccination with ALVAC and AIDSVAX to Prevent HIV-1 Infection in Thailand. N Engl J Med [Internet]. 2009 Dec 3 [cited 2020 Apr 21];361(23):2209–20. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa0908492
Adepoju P. Moving on from the failed HIV vaccine clinical trial. Lancet HIV [Internet]. 2020 Mar 1 [cited 2020 Apr 21];7(3):e161. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2352301820300473
Coakley, E., Petropoulos, C. J., & Whitcomb, J. M. (2005). Assessing chemokine co-receptor usage in HIV. Current Opinion in Infectious Diseases, 18(1), 9–15.
Gulick RM, Lalezari J, Goodrich J, Clumeck N, DeJesus E, Horban A, et al. Maraviroc for Previously Treated Patients with R5 HIV-1 Infection. The New England Journal of Medicine [Internet]. 2008 Oct 2 [cited 2020 Apr 21];359(14):1429–41. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa0803152
Zhang, H., Kang, D., Huang, B., Liu, N., Zhao, F., Zhan, P., et al. (2016). Discovery of non-peptide small molecular CXCR4 antagonists as anti-HIV agents: Recent advances and future opportunities. European Journal of Medicinal Chemistry. Elsevier Masson SAS, 114, 65–78.
Berger, E. A., Murphy, P. M., & Farber, J. M. (1999). Chemokine receptors AS HIV-1 coreceptors: Roles in viral entry, tropism, and disease. Annual Review of Immunology, 17(1), 657–700.
Arif MS, Hunter J, Léda AR, Zukurov JPL, Samer S, Camargo M, et al. Pace of coreceptor tropism switch in HIV-1-infected individuals after recent infection. Journal of Virology [Internet]. 2017 Oct 1 [cited 2020 Nov 3];91(19). Available from: https://doi.org/10.1128/JVI.00793-17
Castagna A, Monno L, Carta S, Galli L, Carrara S, Fedele V, et al. Switch of predicted HIV-1 tropism in treated subjects and its association with disease progression. In: Medicine (United States) [Internet]. Lippincott Williams and Wilkins; 2016 [cited 2020 Nov 3]. Available from: /pmc/articles/PMC5591117/?report=abstract
Solloch U V., Lang K, Lange V, Böhme I, Schmidt AH, Sauter J. Frequencies of gene variant CCR5-Δ32 in 87 countries based on next-generation sequencing of 1.3 million individuals sampled from 3 national DKMS donor centers. Hum Immunol [Internet]. 2017 Nov 1 [cited 2019 May 16];78(11–12):710–7. Available from: https://www.sciencedirect.com/science/article/pii/S0198885917305104
Hütter G, Nowak D, Mossner M, Ganepola S, Müßig A, Allers K, et al. Long-Term Control of HIV by CCR5 Delta32/Delta32 Stem-Cell Transplantation. N Engl J Med [Internet]. 2009 Feb 12 [cited 2019 Apr 27];360(7):692–8. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa0802905
Hütter, G., & Thiel, E. (2011). Allogeneic transplantation of CCR5-deficient progenitor cells in a patient with HIV infection: An update after 3 years and the search for patient no. 2. Aids., 25(2), 273–274.
Gupta RK, Abdul-Jawad S, McCoy LE, Mok HP, Peppa D, Salgado M, et al. HIV-1 remission following CCR5Δ32/Δ32 haematopoietic stem-cell transplantation. Nature [Internet]. 2019 Apr 5 [cited 2019 May 22];568(7751):244–8. Available from: http://www.nature.com/articles/s41586-019-1027-4
Gupta, R. K., Peppa, D., Hill, A. L., Gálvez, C., Salgado, M., Pace, M., et al. (2020). Evidence for HIV-1 cure after CCR5Δ32/Δ32 allogeneic haemopoietic stem-cell transplantation 30 months post analytical treatment interruption: A case report. Lancet HIV, 1(20), 1–8.
Peterson CW, Benne C, Polacino P, Kaur J, McAllister CE, Filali-Mouhim A, et al. Loss of immune homeostasis dictates SHIV rebound after stem-cell transplantation. JCI Insight [Internet]. 2017 Feb 23 [cited 2020 Nov 3];2(4):91230. Available from: https://doi.org/10.1172/jci.insight.91230
Peterson, C. W., Wang, J., Deleage, C., Reddy, S., Kaur, J., Polacino, P., et al. (2018). Differential impact of transplantation on peripheral and tissue-associated viral reservoirs: Implications for HIV gene therapy. PLoS Pathogens, 14(4), 1–22.
Henrich, T. J., Hanhauser, E., Marty, F. M., Sirignano, M. N., Keating, S., Lee, T., et al. (2014). Antiretroviral-free HIV-1 remission and viral rebound following allogeneic stem cell transplantation: A report of two cases. Annals of Internal Medicine, 161(5), 319–327.
Dorr, P., Westby, M., Dobbs, S., Griffin, P., Irvine, B., Macartney, M., Mori, J., Rickett, G., Smith-Burchnell, C., Napier, C., Webster, R., Armour, D., Price, D., Stammen, B., Wood, A., & Perros, M. (2005). Maraviroc (UK-427,857), a potent, orally bioavailable, and selective small-molecule inhibitor of chemokine receptor CCR5 with broad-spectrum anti-human immunodeficiency virus type 1 activity. Antimicrobial Agents and Chemotherapy, 49(11), 4721–4732.
Fätkenheuer G, Nelson M, Lazzarin A, Konourina I, Hoepelman AIM, Lampiris H, et al. Subgroup analyses of maraviroc in previously treated R5 HIV-1 INFECTION. N Engl J Med [Internet]. 2008 Oct 2 [cited 2019 May 8];359(14):1442–55. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa0803154
Miao, M., De Clercq, E., & Li, G. (2020). Clinical significance of chemokine receptor antagonists. Expert Opin Drug Metab Toxicol [internet], 16(1), 11–30. Available from:. https://doi.org/10.1080/17425255.2020.1711884.
Gulick RM, Su Z, Flexner C, Hughes MD, Skolnik PR, Wilkin TJ, et al. Phase 2 study of the safety and efficacy of vicriviroc, a CCR5 inhibitor, in HIV-1–infected, treatment-experienced patients: AIDS clinical trials group 5211. The Journal of Infectious Diseases [Internet]. 2007 Jul 15 [cited 2019 May 8];196(2):304–12. Available from: https://academic.oup.com/jid/article-lookup/doi/10.1086/518797
Nichols WG, Steel HM, Bonny T, Adkison K, Curtis L, Millard J, et al. Hepatotoxicity observed in clinical trials of aplaviroc (GW873140). Antimicrob Agents Chemother [Internet]. 2008 Mar 1 [cited 2019 May 8];52(3):858–65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18070967.
Perez EE, Wang J, Miller JC, Jouvenot Y, Kim KA, Liu O, et al. Establishment of HIV-1 resistance in CD4+ T cells by genome editing using zinc-finger nucleases. Nat Biotechnol [Internet]. 2008 Jul 29 [cited 2019 May 7];26(7):808–16. Available from: http://www.nature.com/articles/nbt1410
Tebas, P., Stein, D., Tang, W. W., Frank, I., Wang, S. Q., Lee, G., Spratt, S. K., Surosky, R. T., Giedlin, M. A., Nichol, G., Holmes, M. C., Gregory, P. D., Ando, D. G., Kalos, M., Collman, R. G., Binder-Scholl, G., Plesa, G., Hwang, W. T., Levine, B. L., & June, C. H. (2014). Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV. The New England Journal of Medicine, 370(10), 901–910.
Yu, S., Yao, Y., Xiao, H., Li, J., Liu, Q., Yang, Y., Adah, D., Lu, J., Zhao, S., Qin, L., & Chen, X. (2018). Simultaneous knockout of CXCR4 and CCR5 genes in CD4+ T cells via CRISPR/Cas9 confers resistance to both X4- and R5-tropic human immunodeficiency virus type 1 infection. Human Gene Therapy, 29(1), 51–67.
Didigu CA, Wilen CB, Wang J, Duong J, Secreto AJ, Danet-Desnoyers GA, et al. Simultaneous zinc-finger nuclease editing of the HIV coreceptors ccr5 and cxcr4 protects CD4+ T cells from HIV-1 infection. Blood [Internet]. 2014 Jan 2 [cited 2019 may 22];123(1):61–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24162716.
Li, L., Krymskaya, L., Wang, J., Henley, J., Rao, A., Cao, L. F., Tran, C. A., Torres-Coronado, M., Gardner, A., Gonzalez, N., Kim, K., Liu, P. Q., Hofer, U., Lopez, E., Gregory, P. D., Liu, Q., Holmes, M. C., Cannon, P. M., Zaia, J. A., & DiGiusto, D. L. (2013 Jun 1). Genomic editing of the HIV-1 coreceptor CCR5 in adult hematopoietic stem and progenitor cells using zinc finger nucleases. Molecular Therapy, 21(6), 1259–1269.
Holt N, Wang J, Kim K, Friedman G. Zinc finger nuclease-mediated CCR5 knockout hematopoietic stem cell transplantation controls HIV-1 in vivo. Nat Biotechnol [Internet]. 2010 [cited 2020 May 7];28(8):839–47. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3080757/
DiGiusto, D. L., Cannon, P. M., Holmes, M. C., Li, L., Rao, A., Wang, J., et al. (2016 Mar 16). Preclinical development and qualification of ZFN-mediated CCR5 disruption in human hematopoietic stem/progenitor cells. Mol Ther - Methods Clin Dev, 3, 16067.
Yu S, Ou Y, Xiao H, Li J, Adah D, Liu S, et al. Experimental treatment of SIV-infected macaques via autograft of CCR5-disrupted hematopoietic stem and progenitor cells. Mol Ther - Methods Clin Dev [Internet]. 2020;17(June):520–31. Available from: https://doi.org/10.1016/j.omtm.2020.03.004, 2020.
Beard BC, Trobridge GD, Ironside C, McCune JS, Adair JE, Kiem HP. Efficient and stable MGMT-mediated selection of long-term repopulating stem cells in nonhuman primates. J Clin Invest [Internet]. 2010 Jul 1 [cited 2020 Nov 3];120(7):2345–54. Available from: https://pubmed.ncbi.nlm.nih.gov/20551514/
Ochoa Z, Chatterji U, Bobardt M, Mendicino M, Dybul M, Hardy WD. Wenshi Joseph Ramesh Spriha Increased Engraftment of Gene Modified HSPCs Overexpressing ALDH1 in vivo. 1(Figure 3):164.
Peterson, C. W., Wang, J., Norman, K. K., Norgaard, Z. K., Humbert, O., Tse, C. K., Yan, J. J., Trimble, R. G., Shivak, D. A., Rebar, E. J., Gregory, P. D., Holmes, M. C., & Kiem, H. P. (2016). Long-term multilineage engraftment of autologous genome-edited hematopoietic stem cells in nonhuman primates. Blood., 127(20), 2416–2426.
Mussolino, C., Morbitzer, R., Lütge, F., Dannemann, N., Lahaye, T., & Cathomen, T. (2011 Nov). A novel TALE nuclease scaffold enables high genome editing activity in combination with low toxicity. Nucleic Acids Research, 39(21), 9283–9293.
Ru R, Yao Y, Yu S, Yin B, Xu W, Zhao S, et al. Targeted genome engineering in human induced pluripotent stem cells by penetrating TALENs. Cell Regen. 2013 Jun 18;2(1):2:5.
Mock, U., MacHowicz, R., Hauber, I., Horn, S., Abramowski, P., Berdien, B., et al. (2015). mRNA transfection of a novel TAL effector nuclease (TALEN) facilitates efficient knockout of HIV co-receptor CCR5. Nucleic Acids Research, 43(11).
Shi B, Li J, Shi X, Jia W, Wen Y, Hu X, et al. TALEN-mediated knockout of CCR5 confers protection against infection of human immunodeficiency virus. JAIDS J Acquir Immune Defic Syndr [Internet]. 2017 Feb 1 [cited 2020 May 7];74(2):229–41. Available from: http://journals.lww.com/00126334-201702010-00018
Mali, P., Yang, L., Esvelt, K. M., Aach, J., Guell, M., DiCarlo, J. E., et al. (2013). RNA-guided human genome engineering via Cas9. Science (80- ), 339(6121), 823–826.
Vogel, P., Schneider, M. F., Wettengel, J., & Stafforst, T. (2014). Improving site-directed RNA editing in vitro and in cell culture by chemical modification of the guideRNA. Angewandte Chemie, International Edition, 53(24), 6267–6271.
Basila, M., Kelley, M. L., & Smith, A. V. B. (2017). Minimal 2’-O-methyl phosphorothioate linkage modification pattern of synthetic guide RNAs for increased stability and efficient CRISPR-Cas9 gene editing avoiding cellular toxicity. PLoS One, 12(11), 1–19.
Ling, X., Xie, B., Gao, X., Chang, L., Zheng, W., Chen, H., et al. (2020). Improving the efficiency of precise genome editing with site-specific Cas9-oligonucleotide conjugates. Science Advances, 6(15), 1–9.
Renaud, J. B., Boix, C., Charpentier, M., De Cian, A., Cochennec, J., Duvernois-Berthet, E., et al. (2016). Improved genome editing efficiency and flexibility using modified oligonucleotides with TALEN and CRISPR-Cas9 nucleases. Cell Reports, 14(9), 2263–2272.
Mandal, P. K., Ferreira, L. M. R., Collins, R., Meissner, T. B., Boutwell, C. L., Friesen, M., Vrbanac, V., Garrison, B. S., Stortchevoi, A., Bryder, D., Musunuru, K., Brand, H., Tager, A. M., Allen, T. M., Talkowski, M. E., Rossi, D. J., & Cowan, C. A. (2014 Nov 6). Efficient ablation of genes in human hematopoietic stem and effector cells using CRISPR/Cas9. Cell Stem Cell, 15(5), 643–652.
Nerys-Junior, A., Braga-Dias, L. P., Pezzuto, P., Cotta-de-Almeida, V., & Tanuri, A. (2018). Comparison of the editing patterns and editing efficiencies of TALEN and CRISPR-Cas9 when targeting the human CCR5 gene. Genetics and Molecular Biology, 41(1).
Li, C., Guan, X., Du, T., Jin, W., Wu, B., Liu, Y., et al. (2015). Inhibition of HIV-1 infection of primary CD4+ T-cells by gene editing of CCR5 using adenovirus-delivered CRISPR/Cas9. The Journal of General Virology, 96(8), 2381–2393.
Xiao, Q., Chen, S., Wang, Q., Liu, Z., Liu, S., Deng, H., et al. (2019). CCR5 editing by Staphylococcus aureus Cas9 in human primary CD4+ T cells and hematopoietic stem/progenitor cells promotes HIV-1 resistance and CD4+ T cell enrichment in humanized mice. Retrovirology [internet]. 2019;16(1):1–17. Available from. https://doi.org/10.1186/s12977-019-0477-y.
Xu L, Yang H, Gao Y, Chen Z, Xie L, Liu Y, et al. CRISPR/Cas9-Mediated CCR5 Ablation in Human Hematopoietic Stem/Progenitor Cells Confers HIV-1 Resistance In Vivo. Mol Ther [Internet]. 2017 Aug 2 [cited 2019 Mar 12];25(8):1782–9. Available from: https://www.sciencedirect.com/science/article/pii/S1525001617302137?via%3Dihub
Yu, S., Ou, Y., Xiao, H., Li, J., Adah, D., Liu, S., Zhao, S., Qin, L., Yao, Y., & Chen, X. (2020 Jun 12). Experimental treatment of SIV-infected macaques via autograft of CCR5-disrupted hematopoietic stem and progenitor cells. Mol Ther - Methods Clin Dev., 17, 520–531.
Re, A., Cattaneo, C., Skert, C., Balsalobre, P., Michieli, M., Bower, M., Ferreri, A. J. M., Hentrich, M., Ribera, J. M., Allione, B., Schommers, P., Montoto, S., Almici, C., Ferremi, P., Mazzucato, M., Gattillo, S., Casari, S., Spina, M., Diez-Martin, J. L., Tirelli, U., Rossi, G., & on the behalf of GECAT (Cooperative European Group on AIDS and Tumors). (2013). Stem cell mobilization in HIV seropositive patients with lymphoma. Haematologica., 98(11), 1762–1768.
Schooley, R. T., Mladenovic, J., Sevin, A., Chiu, S., Miles, S. A., Pomerantz, R. J., Campbell, T. B., Bell, D., Ambruso, D., Wong, R., Landay, A., Coombs, R. W., Fox, L., Kamoun, M., Jacovini, J., & AIDS Clinical Trials Group 285 Study Team. (2000). Reduced mobilization of CD34+ stem cells in advanced human immunodeficiency virus type 1 disease. The Journal of Infectious Diseases, 181(1), 148–157.
Xu, L., Wang, J., Liu, Y., Xie, L., Su, B., Mou, D., Wang, L., Liu, T., Wang, X., Zhang, B., Zhao, L., Hu, L., Ning, H., Zhang, Y., Deng, K., Liu, L., Lu, X., Zhang, T., Xu, J., Li, C., Wu, H., Deng, H., & Chen, H. (2019). CRISPR-edited stem cells in a patient with HIV and acute lymphocytic leukemia. The New England Journal of Medicine, 381(13), 1240–1247.
Nie, Y., Han, Y. C., & Zou, Y. R. (2008). CXCR4 is required for the quiescence of primitive hematopoietic cells. The Journal of Experimental Medicine, 205(4), 777–783.
Baxter, A. E., Russell, R. A., Duncan, C. J. A., Moore, M. D., Willberg, C. B., Pablos, J. L., Finzi, A., Kaufmann, D. E., Ochsenbauer, C., Kappes, J. C., Groot, F., & Sattentau, Q. J. (2014). Macrophage infection via selective capture of HIV-1-infected CD4+ T cells. Cell Host & Microbe, 16(6), 711–721.
Mack, M., Kleinschmidt, A., Brühl, H., Klier, C., Nelson, P. J., Cihak, J., Plachý, J., Stangassinger, M., Erfle, V., & Schlöndorff, D. (2000 Jul). Transfer of the chemokine receptor CCR5 between cells by membrane- derived microparticles: A mechanism for cellular human immunodeficiency virus 1 infection. Nature Medicine, 6(7), 769–775.
Qing R, Tao F, Chatterjee P, Schubert T, Blackburn C, Zhang S. Non-full-length Water-Soluble CXCR4 QTY and CCR5 QTY chemokine receptors: Implication for overlooked truncated but functional membrane receptors highlights Y2H screening reveals ligand interaction from truncated CXCR4 and CCR5 in QTY form. ISCIENCE [Internet]. 2020 [cited 2020 Oct 29];101670. Available from: https://doi.org/10.1016/j.isci.2020.101670.
Kwon, K. J., Timmons, A. E., Sengupta, S., Simonetti, F. R., Zhang, H., Hoh, R., et al. (2020). Different human resting memory CD4+ T cell subsets show similar low inducibility of latent HIV-1 proviruses. Science Translational Medicine, 12(528), 1–14.
Carter, C. C., McNamara, L. A., Onafuwa-Nuga, A., Shackleton, M., Riddell IV, J., Bixby, D., et al. (2011 Mar 17). HIV-1 utilizes the CXCR4 chemokine receptor to infect multipotent hematopoietic stem and progenitor cells. Cell Host & Microbe, 9(3), 223–234.
McNamara, L. A., Onafuwa-Nuga, A., Sebastian, N. T., Riddell, J., Bixby, D., & Collins, K. L. (2013). CD133+ hematopoietic progenitor cells harbor HIV genomes in a subset of optimally treated people with long-term viral suppression. The Journal of Infectious Diseases, 207(12), 1807–1816.
Sebastian, N. T., Zaikos, T. D., Terry, V., Taschuk, F., McNamara, L. A., Onafuwa-Nuga, A., et al. (2017). CD4 is expressed on a heterogeneous subset of hematopoietic progenitors, which persistently harbor CXCR4 and CCR5-tropic HIV proviral genomes in vivo. PLoS Pathogens, 13(7), 1–30.
Kao, C. Y., & Papoutsakis, E. T. (2018). Engineering human megakaryocytic microparticles for targeted delivery of nucleic acids to hematopoietic stem and progenitor cells. Science Advances, 4(11).
Olivetta, E., Chiozzini, C., Arenaccio, C., Manfredi, F., Ferrantelli, F., & Federico, M. (2020). Extracellular vesicle-mediated intercellular communication in HIV-1 infection and its role in the reservoir maintenance. Cytokine and Growth Factor Reviews. Elsevier Ltd, 51, 40–48.
Malhotra D, Fletcher AL, Turley SJ. Stromal and hematopoietic cells in secondary lymphoid organs: partners in immunity. Immunological Reviews [Internet]. 2013 Jan 1 [cited 2020 Apr 5];251(1):160–76. Available from: http://doi.wiley.com/10.1111/imr.12023
Suryawanshi, G. W., Khamaikawin, W., Wen, J., Shimizu, S., Arokium, H., Xie, Y., et al. (2020). The clonal repopulation of HSPC gene modified with anti-HIV-1 RNAi is not affected by preexisting HIV-1 infection. Science Advances, 6(30), 1–14.
Frangoul H, Altshuler D, Cappellini MD, Chen Y-S, Domm J, Eustace BK, et al. CRISPR-Cas9 gene editing for sickle cell disease and β-thalassemia. The New England Journal of Medicine [Internet]. 2021 Jan 21 [cited 2021 Feb 12];384(3):252–60. Available from: http://www.nejm.org/doi/10.1056/NEJMoa2031054
Zhang, X. H., Tee, L. Y., Wang, X. G., Huang, Q. S., & Yang, S. H. (2015). Off-target effects in CRISPR/Cas9-mediated genome engineering. Vol. 4, Molecular Therapy - Nucleic Acids. Nature Publishing Group, e264.
Agarwal, R., Dvorak, C. C., Kwon, H.-S., Long-Boyle, J. R., Prohaska, S. S., Brown, J. W., et al. (2019 Nov 13). Non-genotoxic anti-CD117 antibody conditioning results in successful hematopoietic stem cell engraftment in patients with severe combined immunodeficiency. Blood, 134(Supplement_1), 800–800.
Radtke, S., Adair, J. E., Giese, M. A., Chan, Y. Y., Norgaard, Z. K., Enstrom, M., et al. (2017). A distinct hematopoietic stem cell population for rapid multilineage engraftment in nonhuman primates. Science Translational Medicine, 9(414).
Humbert O, Radtke S, Samuelson C, Carrillo RR, Perez AM, Reddy SS, et al. Therapeutically relevant engraftment of a CRISPR-Cas9–edited HSC-enriched population with HbF reactivation in nonhuman primates. Science Translational Medicine [Internet]. 2019;11(503):eaaw3768. Available from: http://stm.sciencemag.org/lookup/doi/10.1126/scitranslmed.aaw3768
Radtke, S., Pande, D., Cui, M., Perez, A. M., Chan, Y.-Y., Enstrom, M., et al. (2020 Jan 21). Sort-purification of human CD34+CD90+ cells reduces target cell population and improves lentiviral transduction for gene therapy. bioRxiv, 850479.
Acknowledgements
This work was supported by Department of Biotechnology, Government of India. K.V.K is supported by fellowship from Department of Science and Technology- Innovation in Science Pursuit for Inspired Research - (IF180918) (DST-INSPIRE) and PB is supported by Junior Research Fellowship from Council of Scientific and Industrial Research (CSIR).
Funding
Department of Biotechnology, Ministry of Science and Technology, Government of India.
Author information
Authors and Affiliations
Contributions
K.V.K, P.B and ST drafted the study, executed the literature search and manuscript writing. This version of the manuscript is approved by all the three authors.
Corresponding author
Ethics declarations
Not applicable.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karuppusamy, K.V., Babu, P. & Thangavel, S. The Strategies and Challenges of CCR5 Gene Editing in Hematopoietic Stem and Progenitor Cells for the Treatment of HIV. Stem Cell Rev and Rep 17, 1607–1618 (2021). https://doi.org/10.1007/s12015-021-10145-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-021-10145-7