Abstract
Extracellular vesicles (EVs) shed from kidney mesenchymal stem cells (KMSCs) show protective effects against acute kidney injury and progressive kidney fibrosis via mRNA transfer. Previous studies report improvement of renal anemia following administration of genetically modified MSCs or peritoneal mesothelial cells that secrete erythropoietin (EPO). Here, we determined whether EPO-secreting KMSC-derived EVs (EPO(+)-EVs) can improve renal anemia in mouse models of chronic kidney disease (CKD). The mouse CKD and renal anemia model was induced by electrocoagulation of the right renal cortex and sequential left nephrectomy. At six weeks post-nephrectomy, we observed significantly lower hemoglobin (10.4 ± 0.2 vs. 13.2 ± 0.2 g/dL) and significantly higher blood urea nitrogen and serum creatinine levels in CKD mice relative to controls (60.5 ± 0.5 and 0.37 ± 0.09 mg/dL vs. 19.9 ± 0.5 and 0.12 ± 0.02 mg/dL, respectively). Genetically engineered EPO(+)–KMSCs secreted 71 IU/mL EPO/106 cells/24 h in vitro, and EPO(+)–EVs isolated by differential ultracentrifugation expressed EPO mRNA and horizontally transferred EPO mRNA into target cells in vitro and in vivo. Furthermore, at two weeks post-injection of EPO(+)–KMSCs or EPO(+)-EVs into CKD mice with renal anemia, we observed significant increases in hemoglobin levels (11.7 ± 0.2 and 11.5 ± 0.2 vs. 10.1 ± 0.2 g/dL, respectively) and significantly lower serum creatinine levels at eight weeks in comparison to mice receiving vehicle control (0.30 ± 0.00 and 0.23 ± 0.03 vs. 0.43 ± 0.06 mg/dL, respectively). These results demonstrate that intraperitoneal administration of EPO(+)-EVs significantly increased hemoglobin levels and renal function in CKD mice, suggesting the efficacy of these genetically engineered EVs as a promising novel strategy for the treatment of renal anemia.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Decreased production of erythropoietin (EPO) by the failing kidney is the predominant cause of anemia in patients with chronic kidney disease (CKD) [1, 2]. Therefore, therapy with recombinant human EPO (rhEPO) has been the mainstay of management of renal anemia in patients with CKD and end-stage renal failure [3–6].
The strategy of combining cell and gene therapy to develop and implant genetically engineered mesenchymal stem cells (MSCs) secreting EPO appears promising for the treatment of renal anemia; however, poor long-term cellular viability and maldifferentiation of infused MSCs, as well as possible suppression of EPO production by uremic toxins, limit cell-based therapy. Additionally, potential induction of anti-EPO antibodies limits widespread use of cell-based anemia treatment [6, 7].
Extracellular vesicles (EVs) are submicron-sized vesicles that result from plasma-membrane remodeling of stimulated cells. EVs contain microRNAs, mRNAs, proteins, and other genetic materials involved in cell signaling [8–11]. Moreover, EVs function as vectors of intercellular communication and can effectively transfer biological information to target cells. Early studies demonstrated improvement of renal injury following administration of MSC-derived EVs, with the regenerative effects mediated by transfer of mRNA into target cells [12, 13]. Our previous studies showed benefits of treating the injured kidney with EVs derived from kidney MSCs (KMSCs) for acute kidney injury and unilateral ureteral obstruction kidneys. Administration of KMSC-derived EVs not only improved the regeneration of tubular epithelial cells but also inhibited endothelial-to-mesenchymal transition (EMT) to ameliorate renal fibrosis [14, 15]. Furthermore, in contrast to cell-based therapy, EVs have a superior safety profile, including a lower propensity to trigger immune responses and an inability to differentiate into tumor cells [12, 16]. Moreover, EVs can be stored for long periods without losing their function [17], making them potentially ideal as an off-the-shelf cell therapy product.
This study reports the functional changes of KMSCs in the uremic environment, generation of genetically engineered KMSCs to express EPO (EPO(+)–KMSCs), and isolation of EPO(+)–KMSC-derived EVs (EPO(+)-EVs). Additionally, we investigated whether administration of EPO(+)–KMSCs and EPO(+)-EVs can correct anemia and renal dysfunction in mouse models of CKD.
Materials and Methods
In Vitro Indoxyl Sulfate (IS) and p-cresol Treatment and Cell Viability Assay
To mimic uremic conditions, EPO(+)–KMSCs were treated with serial concentrations of IS and p-cresol. Cells were seeded at 1 × 104 cells/well onto tissue-culture plates before treatment (IS: 0.25, 1.0, and 2.5 mM; p-cresol: 0.05, 0.1, 0.25, and 0.5 mM) and incubated for 24 h in alpha-minimum essential medium (alpha-MEM) with serum restriction.
Cell viability was determined using an EZ-Cytox cell proliferation assay kit (Daeil Lab Service Co, Seoul, the Republic of Korea) according to manufacturer’s instructions. Briefly, 20 µL of EZ-Cytox kit reagent was added to each well of a 96-well microplate and then incubated at 37°C in a humidified CO2 incubator for 3 h. After incubation, the optical density at 450 nm was measured using a microplate reader (BioTek Instruments, Inc., Winooski, VT, USA).
Generation of Mouse KMSCs Engineered to Express EPO and EV Isolation
KMSCs previously isolated and cloned from a fibroblast-like cell line from the kidney of an adult FVB/N Tie-2/green fluorescent protein (GFP) mouse were cultured on gelatin-coated dishes in alpha-MEM with 10 % horse serum (Gem Biotech, Woodland, CA, USA) to 80 % confluence, as previously described [18]. For generation of EPO(+)–KMSCs, plasmids encoding EPO mRNA were generated by inserting human EPO cDNA into a lentiviral vector co-expressing GFP. HEK293T cells were co-transfected with the lentiviral expression vector and packaging construct to generate lentiviral supernatant, as described previously [19]. After transduction of the KMSCs with lentiviral supernatant, EPO(+)–KMSCs were identified by GFP expression using fluorescence microscopy and reverse transcription polymerase chain reaction (RT-PCR) with primers targeting human EPO mRNA. EPO secretion was measured in the supernatant of the EPO(+)–KMSCs by an enzyme-linked immunosorbent assay (ELISA) specific for human EPO (Quantikine; R&D Systems, Minneapolis, MN, USA).
The plasticity of the EPO(+)–KMSCs was tested by differentiation into mesenchymal lineages, such as osteogenic, adipogenic, and endothelial differentiation. EPO(+)–KMSCs were differentiated into osteocytes using a commercial kit (Gibco; Life Technologies, Carlsbad, CA, USA), and Alizarin Red S was used to stain calcium in the mineralized extracellular matrix. Adipogenic differentiation was induced in cultures grown in medium with insulin, dexamethasone, and indomethacin for 2 weeks, and Oil Red O was used for lipid-droplet staining. In vitro tube formation on EPO(+)–KMSCs seeded on growth-factor-reduced Matrigel (BD Biosciences, Franklin Lakes, NJ, USA) was used. Cells were observed under an inverted microscope (Nikon, Kanagawa, Japan) during 24 h incubation at 37°C [20]. To confirm endothelial differentiation of EPO(+)–KMSCs, immunofluorescence analysis and western blot analysis were performed using anti-CD31 antibody (Abcam).
To generate EVs [EPO(+)-EVs], EPO(+)–KMSCs were cultured in serum-free alpha-MEM in < 1 % O2 using a controlled atmospheric chamber and O2 analyzer (Thermo Fisher Scientific, Marietta, OH, USA) for 24 h. Cell debris was removed by centrifugation at 2,000 ×g for 10 min, and the cell-free supernatants were centrifuged at 50,000 ×g (Optima L-90 K ultracentrifuge; Beckman Coulter, Brea, CA, USA) for 2 h at 4°C before being washed in phosphate-buffered saline (PBS) and centrifuged again under the same conditions [14, 21].
Nanoparticle‐tracking and Flow‐cytometric Analyses
Size distribution and enumeration of EVs were performed by nanoparticle-tracking analysis (NTA) using a NanoSight NS 300 instrument (NanoSight Limited, Amesbury, UK) equipped with NTA 2.3 software [21]. EPO(+)-EVs were examined by flow cytometry (BD Canto II; BD Biosciences) after rinsing the instrument with particle-free rinse solution for 15 min to eliminate background. Beads (1 µm; Sigma-Aldrich, St. Louis, MO, USA) were used as size markers for fluorescence-activated cell sorting (FACS) analysis as previously described [12, 22, 23] using the following allophycocyanin (APC)- or phycoerythrin (PE)-conjugated antibodies: anti-Annexin V (Biolegend, San Diego, CA, USA); anti-CD29 and anti-CD44 (BD Biosciences); and anti-CD73 and anti-α4, -α5, and -α6 integrins (Biolegend). Mouse APC- or PE-conjugated non-immune isotypic IgG was used as a control.
Quantitative PCR
PCR was performed using total RNA extracted from cells and EVs. First-strand cDNA was produced from total RNA using a cDNA synthesis kit (SuperScript III first-strand synthesis system; Invitrogen, Carlsbad, CA, USA). Briefly, 1 µg to 2 µg RNA, 2 µL RT buffer, 1 µM to 10 mM dNTP mixture, 1 µM of random hexamer, 2 µM to 0.1 M DTT, 1 µL reverse transcriptase, and nuclease-free water were used for synthesis. The following PCR primers were used for amplification: human EPO forward, 5’-ACTGTCCCAGACACCAAAGT-3’ and reverse, 5’-ATGTGGATAAAGCCGTCAGT-3’; mouse EPO forward, 5’-GACAGTCGAGTTCTGGAGAG-3’ and reverse, 5’-GAACAGGCCATAGAAGTTTG-3’. Reactions were performed in triplicate for each sample to analyze gene expression, which was normalized against β-actin or 18S ribosomal RNA levels. Negative cDNA controls were cycled in parallel with each run.
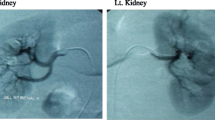
Generation of a Mouse Model of CKD
The animal study protocol was performed in accordance with guidelines for laboratory animals and approved by the Institutional Animal Care and Use Committee, Department of Laboratory Animal Medicine, Medical Research Center, Yonsei University College of Medicine (2010-0226-1). FVB/N mice (5–6-weeks old) were purchased from Orientbio (Gyeonggi-Do, the Republic of Korea) and maintained under temperature-controlled conditions and a 12-/12-h light/dark cycle, with access to water and food ad libitum. Mice were anesthetized by mask inhalation of isoflurane (~ 1–3 %), and all efforts were made to minimize suffering. A murine model of CKD and renal anemia was induced by electrocoagulation, as previously described [24]. Direct injury to the cortex was induced by electrocoagulation of the entire right kidney surface sparing the hilum, followed by contralateral left nephrectomy 10 to 12 days later. No significant difference in post-surgical survival of CKD mice was observed during the six-week follow-up in sham-operated control animals in a previous study, and severe anemia occurred after six weeks of renal failure [24]. Similarly, in the present study, mice received an intraperitoneal injection of EPO(+)–KMSCs (1 × 106/mouse) and EPO(+)-EVs (2 × 107/mouse) in 150 µL saline, with saline alone used as vehicle control six weeks after contralateral nephrectomy. The number of injected EVs was derived from our previous study investigating the antifibrotic effects of KMSC-derived EVs. For each group, mice were sacrificed 2 weeks after intraperitoneal administration of EPO(+)–KMSCs and EPO(+)-EVs (n = ~ 4–6 mice/group). CKD and anemia were confirmed via assessment of renal histology, as well as measurement of blood urea nitrogen (BUN), serum creatinine, and hemoglobin levels. Serum EPO levels in CKD mice treated with vehicle control and EPO(+)-EVs were measured using ELISA specific for human EPO (Quantikine; R&D Systems, Minneapolis, MN, USA).
Morphologic Studies
For histologic confirmation of CKD, kidney sections were stained with Masson’s trichrome stain. Tubular injury was semiquantitatively scored by an independent investigator who was blinded to the study design. Scoring was determined by assessing the cortex and corticomedullary junction, as follows: 0, none; 1+, < 25 %; 2+, 25–50 %; and 3+, > 50 % of tubules. Twenty fields randomly selected from the cortex and corticomedullary junction on each slide section were examined at ×400 magnification, as previously described [25, 26].
Kidney sections were stained with Masson’s trichrome for analysis of kidney fibrosis. Areas positive for Masson’s trichrome were evaluated in relation to the unit area and expressed as a percentage using MetaMorph microscopy image analysis software (Molecular Devices, CA, USA). Microscopy assessment was carried out in a blinded manner, and 20 randomly selected fields from each slide section were examined at ×400 magnification. Immunohistochemistry using anti-F4/80 (Abcam) was performed to evaluate macrophage infiltration. The quantification of F4/80-positive cells was expressed as the number of cells per high-power field (HPF) [15].
Madin–Darby Canine Kidney (MDCK) and Mouse Peritoneal Mesothelial Cell (PMC) Culture and Treatment with EPO(+)-EVs
We used MDCK cells purchased from the Korean Cell Line Bank (Seoul, the Republic of Korea) to assess the in vitro effects of EPO(+)-EVs. MDCK cells were seeded at 5 × 104 cells/well onto 6-well culture plates and incubated at 37°C under 5 % CO2 for 48 h in Dulbecco’s modified Eagle medium supplemented with 10 % fetal bovine serum (FBS) (Gibco; Life Technologies), penicillin G (100 U/mL), and streptomycin (100 U/mL).
Mouse PMCs were isolated and cultured, as previously described [27]. Briefly, mouse PMCs were obtained from adult FVB mice and seeded onto 75-cm2 Falcon tissue flask plates and incubated at 37°C under 5 % CO2 for 48 h in alpha-MEM supplemented with 10 % FBS. Cells were cultured for 6 to 8 days until confluent, and monoclonal mouse anti-cytokeratin (Sigma-Aldrich) was used to confirm the presence of cells by immunofluorescence staining (Supplemental Figure S1). Incorporation of EPO(+)-EVs into the target cell cytoplasm was demonstrated by detecting red fluorescence from CellTracker-labeled EVs by fluorescence microscopy.
Statistical Analysis
Data are expressed as the mean ± standard error of the mean. Differences between groups were analyzed by a Mann–Whitney U test or Kruskal–Wallis test using SPSS (v.20.0; IBM Corp., Armonk, NY, USA). A P < 0.05 was considered statistically significant.
Results
In Vitro Effect of Uremic Condition on KMSCs
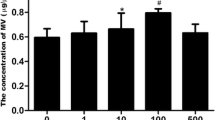
To investigate the effects of in vitro uremic conditions, cultured KMSCs were treated with IS and p-cresol, which inhibited cell proliferation over the course of 24 h relative to vehicle control (Fig. 1a). Additionally, we observed that cell viability following exposure to various IS concentrations (0.25, 1.0, and 2.5 mM) decreased in a dose-dependent manner (by 6.5 %, 11.7 %, and 23.1 %, respectively) as compared with vehicle control (P = 0.054, P = 0.001, and P < 0.001, respectively). In addition, p-cresol treatment decreased the cell viability in a dose-dependent manner (0.05 mM by 3.3 %, 0.1 mM by 8.8 %, and 0.25 mM 21.7 %, and 0.5 mM by 37.6 %) as compared with vehicle control (P = 0.234, P = 0.007, P < 0.001, and P < 0.001, respectively) (Fig. 1b). RT-PCR analysis revealed significant decreases in mouse EPO mRNA levels following IS and p-cresol treatment relative to vehicle control (mouse EPO/β-actin: IS, 0.57 ± 0.05 vs. 1.22 ± 0.08, P = 0.002; p-cresol, 0.58 ± 0.14 vs. 1.00 ± 0.13, P = 0.004) (Fig. 1c).
Viability and erythropoietin (EPO) mRNA levels in kidney-derived mesenchymal stem cells (KMSCs) under uremic conditions. a Cell proliferation of KMSCs treated with either vehicle control or indoxyl sulfate (IS) according to microscopy analysis. b Relative cell viability of KMSCs according to IS and p-cresol concentrations. c EPO mRNA levels in vehicle control cells relative to those treated with IS or p-cresol, respectively. Results represent the mean ± standard error of the mean of three independent experiments. *P < 0.05 vs. vehicle control, Krukal–Wallis test
Characterization of Mouse KMSCs Engineered to Express Human EPO
Lentiviral transduction of KMSCs with a vector expressing human EPO-GFP resulted in GFP expression as confirmed by fluorescence microscopy and FACS analysis. We observed an average transduction rate of ~ 98.9 % according to FACS (Fig. 2a, left), with most KMSCs verified as expressing GFP according to florescence microscopy (Fig. 2a, right). Following confirmation of human EPO mRNA expression in EPO(+)–KMSCs by RT-PCR (Fig. 2b), we measured human EPO secretion in vitro into 24-h conditioned-culture supernatant by ELISA. Although wild-type KMSCs showed no secretion of detectable levels of human EPO, we detected 71.1 ± 3.7 IU/mL of secreted human EPO from EPO(+)–KMSCs (Fig. 2c).
Characterization of erythropoietin (EPO)-expressing kidney-derived mesenchymal stem cells (KMSCs). a (GFP) expression was confirmed by flow-cytometric analysis (left) and florescence microscopy (right). b RT-PCR confirmation of the presence of human EPO mRNA in EPO(+)–KMSCs. c EPO protein was detected in EPO(+)–KMSC culture supernatant by enzyme-linked immunosorbent assay. GFP, Green fluorescent protein; DAPI, 4’,6-diamidino-2-phenylindole
To determine whether EPO(+)–KMSCs maintained the multilineage-differentiation potential of KMSCs, cells from passages 10 to 15 were cultured on gelatin-coated dishes with cytokines known to induce cell differentiation and labeled with phenotype-specific markers. Undifferentiated cells maintained a dendritic cell-like morphology along with extension of numerous filopodia (Fig. 3a). At 2 weeks after induction of the adipocyte lineage, Oil Red O+ cells were detected (Fig. 3a, upper right), and osteogenesis differentiation was confirmed by presence of Alizarin Red S+ cells (Fig. 3a, lower right). Additionally, in vitro endothelial capillary tube formation by EPO(+)–KMSCs was observed on growth-factor-reduced Matrigel with light microscopy (Fig. 3b). To confirm endothelial differentiation, EPO(+)–KMSCs with tube formation on growth-factor-reduced Matrigel were evaluated by CD31-positive staining and fluorescence objective lens (Fig. 3c). Moreover, CD31 protein expression was observed using western blot analysis (Fig. 3d).
In vitro differentiation of erythropoietin (EPO)-expressing kidney-derived mesenchymal stem cells (KMSCs). a Confirmation of the multilineage-differentiation potential of KMSCs by Oil-Red O (upper right) and Alizarin Red S (lower right) staining. b In vitro identification of endothelial capillary tube formation by EPO(+)–KMSCs on growth-factor-reduced Matrigel at baseline and after 6 h. c FITC-green fluorescent CD31-positive cells in fluorescence microscopy analysis. d CD31 protein expression in western blotting analysis. DAPI, 4’,6-diamidino-2-phenylindole; FITC, fluorescein isothicyanate
EPO(+)-EVs Characterization
To assess the properties of EPO(+)-EVs, they were isolated from culture media and characterized by NTA and FACS analysis. NTA revealed that cultured EPO(+)-EVs were distributed with a mean size of 225.5 ± 19.2 nm (Fig. 4a), with human EPO expression confirmed by PCR (Fig. 4b). Human EPO mRNA expression of EPO(+)–KMSCs was used as a positive control (Fig. 4b). Flow-cytometric analysis revealed EPO(+)-EVs mainly detected at a region below the forward-scatter signal corresponding to the 1-µm beads used as internal standards (Fig. 4c, upper left). Moreover, we confirmed that EPO(+)-EVs were positive for Annexin V (86 %) and expressed CD44, CD73, CD29, and α4/α5/α6 integrin (Fig. 4c), which were also expressed on the surface of KMSCs except α5 integrin (Fig. 4d).
Nanoparticle-tracking analysis (NTA) and fluorescence-activated cell sorting. a NTA showing the distribution of microparticle (MP) size and number from erythropoietin (EPO)(+)–kidney-derived mesenchymal stem cells (KMSCs). b Human EPO mRNA levels in EPO(+)–KMSCs and EVs. c Flow cytometry analysis of Annexin V, CD44, CD73, CD29, and α4/α5/α6 integrin surface expression on EPO(+)–KMSC-derived EVs and EPO(+)–KMSC d. Black lines indicate isotypic controls
Effect of EPO(+)-EVs on Anemia and Renal Function in CKD Mice
The mouse model of CKD was induced by electrocoagulation of the unilateral renal cortex followed by contralateral nephrectomy after two weeks. Six weeks after nephrectomy, hemoglobin levels were significantly lower in CKD mice as compared with normal mice (10.4 ± 0.2 vs. 13.2 ± 0.2 g/dL; P < 0.05), whereas and BUN and serum creatinine levels were elevated (60.5 ± 0.5 and 0.37 ± 0.09 mg/dL vs. 19.9 ± 0.5 and 0.12 ± 0.02 mg/dL, respectively; P < 0.05) (Supplemental Figure S2A and S2B). Examination of kidney sections stained with Masson’s trichrome and semiquantitative injury scoring revealed extensive fibrotic lesions in the cortex and corticomedullary junction (Supplemental Figure S3A) and significantly increased scores in the kidney with CKD mice after 6 and 9 weeks compared to that of control, respectively (Supplementary Figure S3B).
We then investigated the in vivo beneficial effects of EPO(+)–KMSCs or EPO(+)-EVs on renal anemia in CKD mice. As shown in Fig. 5a, administration of EPO(+)–KMSCs or EPO(+)-EVs to CKD mice significantly increased hemoglobin levels relative to mice treated with vehicle control (11.7 ± 0.2 and 11.5 ± 0.2 g/dL vs. 10.1 ± 0.2 g/dL, respectively; P < 0.05). Additionally, assessment of the in vivo renoprotective effects of EPO(+)–KMSCs or EPO(+)-EVs administration demonstrated that both significantly lowered serum creatinine levels relative to vehicle control (0.30 ± 0.00 and 0.23 ± 0.03 mg/dL vs. 0.43 ± 0.03 mg/dL, respectively; P < 0.05). Moreover, BUN levels following EPO(+)-EVs administration showed significant decreases relative to vehicle control (54.9 ± 1.3 mg/dL vs. 68.6 ± 3.6 mg/dL; P < 0.05) (Fig. 5b), and CKD mice treated with EPO(+)–KMSCs also showed lower BUN levels (60.1 ± 2.3 mg/dL vs. 68.6 ± 3.6 mg/dL; P = 0.058) (Fig. 5b).
Effect of erythropoietin (EPO)(+)–kidney-derived mesenchymal stem cell (KMSC)-derived extracellular vesicles (EPO(+)-EVs) on anemia and renal function in mouse models of chronic kidney disease (CKD). a Hemoglobin levels in CKD mice treated with EPO(+)–KMSCs and EPO(+)-EVs relative to vehicle control. b Blood urea nitrogen levels (BUN) and serum creatinine (Cr) levels in CKD mice treated with EPO(+)–KMSCs and EPO(+)-EVs relative to vehicle control. *P < 0.05 vs. vehicle control, Krukal–Wallis test
In CKD mice treated with vehicle, Masson’s trichrome staining of kidney tissue showed more fibrotic lesions compared with those of EPO(+)–KMSCs or EPO(+)-EVs injected mice (55.05 ± 2.1 vs. 30.0 ± 0.9, 19.7 ± 0.9 % of total tubulointerstitial area, respectively, *P < 0.05) (Fig. 6a and b). Immunohistochemistry for macrophages using F4/80 antibody showed increased macrophage infiltration in the tubulointerstitial area in the kidney of CKD mice treated with vehicle control. In contrast, the F4/80-positive cells were significantly decreased in the kidney of mice treated with EPO(+)–KMSCs or EPO(+)-EVs (59.3 ± 1.5 vs. 32.2 ± 2.0, 22.4 ± 3.0 per field, respectively, *P < 0.05) (Fig. 6a and b).
Anti-fibrotic and anti-inflammatory effects of EPO(+)–KMSC or EVs in the kidneys of CKD mice. Light-field microscopic analysis of Masson’s trichrome–stained sections of kidneys from CKD mice treated with vehicle control, EPO(+)–KMSC, or EVs (a). Quantitative analysis of tubulointerstitial fibrosis in Masson’s trichrome–stained sections using MetaMorph analysis (b, upper graph). Immunohistochemical study for F4/80 expression in the kidneys of CKD mice treated with vehicle control, EPO(+)–KMSC, or EVs (a). Quantification analysis of F4/80-positive cells per field (b, lower graph). Ten randomly selected high-power fields were quantified and averaged to obtain the value for each mouse (n = 6 for each experimental group). Results are expressed as the mean ± SE of three different experiments. Kruskal-Wallis test was performed; * P < 0.05 vs. vehicle control
In Vitro and In Vivo EPO(+) –KMSC-derived EV-mediated Horizontal EPO mRNA Transfer
To elucidate the underlying mechanism of improved renal anemia observed in CKD animal experiments, a separate set of in vitro experiments were conducted using MDCK cells and mouse PMCs. Following confirmation of the presence of red CellTracker™-labeled EVs in MDCK cells and mouse PMCs by immunofluorescence microscopy (Fig. 7a), we assessed horizontal transfer of EPO mRNA from EPO(+)-EVs into target cells, with cells in the presence of EPO(−)-EVs used as negative controls. RT-PCR analysis confirmed that MDCK cells and mouse PMCs incubated with EPO(+)-EVs for 3 and 5 days expressed human EPO mRNA, suggesting successful horizontal transfer of the human gene in vitro (Fig. 7b). Furthermore, we detected significant levels of human EPO in the supernatants of MDCK cells and mouse PMCs treated with EPO(+)-EVs (Fig. 7c).
Erythropoietin (EPO)(+)–kidney-derived mesenchymal stem cell (KMSC)-derived extracellular vesicles (EPO(+)-EVs) mediate horizontal EPO mRNA transfer into peritoneal mesothelial cells (PMCs) and tubular cells in vitro. a Immunofluorescence microscopy showing red CellTracker™ -labeled EVs in Madin–Darby canine kidney (MDCK) cells and mouse PMCs. b Human EPO mRNA levels in MDCK cells and mouse PMCs treated with EPO(+)-EVs, with EPO(−)-EVs used as negative controls. c Levels of human EPO protein secreted from EPO(+)-EVs-treated MDCK cells and mouse PMCs according to enzyme-linked immunosorbent assay
Next, we investigated in vivo EPO(+)-EVs-mediated horizontal transfer of human EPO mRNA into injured mice kidney tissue. RT-PCR analysis demonstrated that human EPO mRNA was expressed only in the kidney of CKD mice that received EPO(+)-EVs (Fig. 8a). Moreover, serum human EPO levels were detected in CKD mice treated with EPO(+)-EVs (23.6 ± 9.8 mIU/mL) (Fig. 8b).
Erythropoietin (EPO)(+)–kidney-derived mesenchymal stem cell (KMSC)-derived extracellular vesicles (EPO(+)-EVs) mediate horizontal EPO mRNA transfer into the kidney of CKD mice in vivo. a RT-PCR demonstrated human EPO mRNA in kidney tissue of CKD mice treated with EPO(+)-EVs. CKD mice treated with vehicle control failed to show any human EPO mRNA. EPO(+)–KMSC and normal kidney tissue was used as positive and negative control, respectively. b Serum levels of human EPO in CKD mice treated with vehicle control or EPO(+)-EVs determined using ELISA analysis
We also investigated in vitro EPO(+)-EVs-mediated horizontal transfer of EPO mRNA into human tubular epithelial cells (HK-2, ATCC®) and human podocytes (from Jun Oh, MD., University Medical Center Hamburg-Eppendorf, Germany). The presence of red CellTracker™-labeled EVs in HK-2 cells and human podocytes was observed using immunofluorescence microscopy (Supplementary Figure S4A). In particular, EPO mRNA was expressed only in cells treated with EPO(+)-EVs by RT-PCR (Supplementary Figure S4B).
Discussion
In this study, we demonstrated that genetically engineered EPO(+)–KMSCs effectively secreted EPO, and that administration of EPO(+)–KMSCs, as well as EPO(+)-EVs, to CKD mice significantly corrected renal anemia and renal dysfunction. Furthermore, the mechanism for improving renal anemia and renal dysfunction was related to horizontal transfer of EPO mRNA.
Renal anemia predominantly results from EPO deficiency; therefore, rhEPO treatment has been widely used to correct renal anemia in patients with advanced CKD [1, 2]. However, unlike physiological EPO levels observed in normal controls, current rhEPO-dosing regimens induce supraphysiological concentrations of EPO in patients with CKD. Such high doses of rhEPO are associated with increased vascular-access thrombosis and mortality in patients on dialysis [28], as well as worsened hypertension and increased progression of malignancy and death in cancer patients [2–4].
Preclinical studies show that cell-based therapy might be a promising therapeutic strategy to improve renal anemia. Induction of EPO expression into various cells types, such as fibroblasts, keratinocytes, and myoblasts, results in sustained EPO secretion and correction of renal anemia [29–31]. In particular, PMCs or MSCs that have been genetically engineered to secrete EPO have successfully corrected renal anemia in animal studies [6, 32]. A previous report showed that KMSCs produced increased amounts of the hypoxia-inducible growth factors vascular endothelial growth factor (VEGF) and EPO [18]; however, MSCs under uremic conditions were functionally incompetent [33, 34] and displayed decreased expression of proangiogenic factors, such as VEGF, as well as cellular senescence, defective migration, and decreased angiogenesis [33]. In the present study, we demonstrated that IS and p-cresol, well-known uremic toxins, decreased KMSC viability and suppressed murine EPO expression in a dose-dependent manner. These findings highlight further limitations of cell-based therapy in the setting of uremia and the need for novel cell-free strategies to treat renal anemia.
Given these limitations, a strategy using MSC-derived EVs rather than MSCs alone might be useful, as EVs can circumvent concerns regarding extensive expansion or maldifferentiation of genetically modified MSCs in target tissues [35]. In the present study, we established genetically engineered KMSCs capable of expressing human EPO and isolated EVs enriched with human EPO mRNA. These KMSCs were lentivirally engineered to secrete high levels of human EPO independent of hypoxic stimuli and without altering the mesenchymal phenotype or plasticity. We showed that EPO(+)–KMSCs secreted ~ 71 IU/mL EPO/106 cells/day, which greatly exceeds basal levels of serum EPO (5 ~ 25 mIU/L) [36]. Therefore, it is unsurprising that administration of 1 × 106 EPO(+)–KMSCs resulted in substantial increases in hemoglobin levels in CKD mice. Compared to a previous study demonstrating genetically engineered bone marrow MSCs secreting human EPO [6], the EPO(+)–KMSCs in the present study secreted ~ 10-fold higher levels of human EPO. Interestingly, serum levels of human EPO were detected in the CKD mice treated with EPO(+)-EVs at two weeks after treatment. Intraperitoneal administration of EPO(+)-EVs to CKD mice also resulted in significant increases in hemoglobin levels that were comparable to those observed by EPO(+)–KMSCs. Previous examples of gene therapy using a single intraperitoneal administration of adenoviruses containing rhEPO resulted in in vivo gene transfer to mouse peritoneal mesothelium, with northern blot analysis confirming human EPO cDNA expression in peritoneal tissue, and mesothelial cell-culture supernatants containing rhEPO protein. Moreover, they showed that mice administered adenoviruses containing rhEPO demonstrated increases in serum rhEPO levels, as well as marked increase in hemoglobin levels for up to 40 days [37].
In the present study, in vitro treatment of MDCK cells and murine PMCs with EPO(+)-EVs demonstrated horizontal transfer of EPO mRNA into target cells, with large amounts of human EPO protein detected in the conditioned supernatants of these EPO(+)-MP-treated cells. Moreover, in vivo intraperitoneal administration of EPO(+)-EVs also mediated horizontal mRNA transfer into the injured kidney of CKD mice. These in vitro and in vivo results support possible use of EPO(+)-EVs as a novel therapeutic strategy for treating renal anemia and renal dysfunction. We previously demonstrated that KMSCs are capable of homing to injured kidney in animal models of ischemic-reperfusion injury and unilateral ureteral obstruction [14, 15]. The exact mechanism of homing and engraftment of EVs into injured kidney tissues of CKD mice has not been elucidated in the present study. Nevertheless, surface molecules and adhesion molecules expressed on EVs such as CD44, CD29, α4-, α5-, and α6-integrins are likely to be involved [14].
In addition to increased hemoglobin levels, intraperitoneal administration of EPO(+)-EVs to CKD mice resulted in significant decreased in serum creatinine and BUN levels as compared with mice treated with vehicle control. The improved renal function observed agrees with accumulating evidence that MSC-derived EVs exert renoprotective effects in animal models of renal injury [12, 16]. A previous report also demonstrated that KMSC-derived EVs improve renal tubular regeneration and inhibit peritubular capillary rarefaction in ischemic kidneys via delivery of proangiogenic factors [14]. Additionally, KMSC-derived EVs exhibited antifibrotic effects by ameliorating EMT in a model of kidney unilateral ureteral obstruction [15]. Notably, the dose of EPO(+)-EVs administered in the present study was same as that in previous studies. Therefore, these results suggest that EPO(+)-EVs are capable of exerting renoprotective effect in a murine model of CKD and anemia.
Several previous studies revealed that MSC-derived EVs modulate immune responses and facilitate organ repair [24, 38]. Interestingly, Wang et al. showed that relative to PBS-treated MSC-derived microvesicles (MSC-MVs), EPO-treated MSC-MVs showed better restorative effects following transforming growth factor-β1-induced fibrosis in vitro and in vivo [39]. In addition to hematopoietic effect, the genetically engineered EPO(+)-EVs described in the present study might confer greater protection against renal damage. Moreover, F4/80 immunochemical staining showed decreased macrophage infiltration in the tubulointerstitial area of kidney in CKD mice treated with EPO(+)–KMSCs or EPO(+)-EVs compared to that of vehicle control. The present study could not unveil the exact mechanisms underlying the renoprotective immune modulation in the CKD mice model, and therefore further studies should be performed to clarify the issue.
There are a few limitations to this study. First, the fate of intraperitoneally administered EPO (+)-EVs is not fully described. A previous study describing administration of adenovirus containing human EPO cDNA intraperitoneally examined the peritoneal mesothelium and demonstrated successful gene transfer and induction of EPO synthesis in the peritoneal cells [37]. In the present study, we did not isolate mouse peritoneum or investigate other intraperitoneal organs for EPO expression. Many of these EVs and their genetic contents can be taken up by peritoneal macrophages, thereby rendering them inactive and administered EPO(+)-EVs could have been absorbed into systemic circulation. Furthermore, EPO (+)-EVs should be investigated in CKD mice using other administration routes for a potential clinical application. Nevertheless, our data showed that EPO(+)-EVs successfully transferred EPO mRNA into target cells in vitro and injured kidney tissue in vivo to promote overt EPO synthesis. Second, human EPO levels were not measured in the serum of CKD mice. Our in vitro data revealed that EPO(+)-EVs transferred to MDCK cells and murine PMCs resulted in significant increases in hemoglobin; therefore, this suggests that administration of EPO(+)-EVs promoted increased hematopoiesis in CKD mice. Third, the model of CKD and renal anemia induced by electrocoagulation of the renal cortex can potentially demonstrate inconsistent degrees of histological changes; however, our data showed persistent and significant decreases in hemoglobin levels and impaired renal function (serum creatinine and BUN levels) post-nephrectomy relative to normal mice. Moreover, the survival rate of CKD mice was > 90 % during the follow-up period (data not shown). Finally, isolation and characterization of EPO(+)-EVs should be investigated following Current Good Manufacturing Practice regulations for clinical applications in a future study.
Conclusions
In summary, we showed that EPO(+)–KMSCs and EPO(+)–KMSC-derived EVs showed comparable renoprotective effects, as well as induced increases in hemoglobin levels, in CKD mice. These results suggest the efficacy of genetically induced EPO(+)-EVs as a potential therapeutic strategy for treating renal anemia in CKD.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
KDOQI; National Kidney Foundation (2006). KDOQI clinical practice guidelines and clinical practice recommendations for anemia in chronic kidney disease. American Journal of Kidney Diseases, 47(5 Suppl 3), S11–S145.
Babitt, J. L., & Lin, H. Y. (2012). Mechanisms of anemia in CKD. Journal of the American Society of Nephrology, 23(10), 1631–1634.
Winearls, C. G., Oliver, D. O., Pippard, M. J., Reid, C., Downing, M. R., & Cotes, P. M. (1986). Effect of human erythropoietin derived from recombinant DNA on the anaemia of patients maintained by chronic haemodialysis. Lancet, 2(8517), 1175–1178.
Eschbach, J. W., Egrie, J. C., Downing, M. R., Browne, J. K., & Adamson, J. W. (1987). Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. The New England Journal of Medicine, 316(2), 73–78.
Macdougall, I. C. (2001). Present and future strategies in the treatment of renal anaemia. Nephrology, Dialysis, Transplantation, 16(Suppl 5), 50–55.
Eliopoulos, N., Gagnon, R. F., Francois, M., & Galipeau, J. (2006). Erythropoietin delivery by genetically engineered bone marrow stromal cells for correction of anemia in mice with chronic renal failure. Journal of the American Society of Nephrology, 17(6), 1576–1584.
Chiang, C. K., Tanaka, T., Inagi, R., Fujita, T., & Nangaku, M. (2011). Indoxyl sulfate, a representative uremic toxin, suppresses erythropoietin production in a HIF-dependent manner. Laboratory Investigation, 91(11), 1564–1571.
Schorey, J. S., & Bhatnagar, S. (2008). Exosome function: from tumor immunology to pathogen biology. Traffic, 9(6), 871–881.
Camussi, G., Deregibus, M. C., Bruno, S., Cantaluppi, V., & Biancone, L. (2010). Exosomes/microvesicles as a mechanism of cell-to-cell communication. Kidney International, 78(9), 838–848.
Morel, O., Toti, F., Hugel, B., & Freyssinet, J. M. (2004). Cellular microparticles: a disseminated storage pool of bioactive vascular effectors. Current Opinion in Hematology, 11(3), 156–164.
Ratajczak, J., Miekus, K., Kucia, M., et al. (2006). Embryonic stem cell-derived microvesicles reprogram hematopoietic progenitors: evidence for horizontal transfer of mRNA and protein delivery. Leukemia, 20(5), 847–856.
Bruno, S., Grange, C., Deregibus, M. C., et al. (2009). Mesenchymal stem cell-derived microvesicles protect against acute tubular injury. Journal of the American Society of Nephrology, 20(5), 1053–1067.
Gatti, S., Bruno, S., Deregibus, M. C., et al. (2011). Microvesicles derived from human adult mesenchymal stem cells protect against ischaemia-reperfusion-induced acute and chronic kidney injury. Nephrology, Dialysis, Transplantation, 26(5), 1474–1483.
Choi, H. Y., Moon, S. J., Ratliff, B. B., et al. (2014). Microparticles from kidney-derived mesenchymal stem cells act as carriers of proangiogenic signals and contribute to recovery from acute kidney injury. PLoS One, 9(2), e87853.
Choi, H. Y., Lee, H. G., Kim, B. S., et al. (2015). Mesenchymal stem cell-derived microparticles ameliorate peritubular capillary rarefaction via inhibition of endothelial-mesenchymal transition and decrease tubulointerstitial fibrosis in unilateral ureteral obstruction. Current Stem Cell Research & Therapy, 6, 18.
Cantaluppi, V., Gatti, S., Medica, D., et al. (2012). Microvesicles derived from endothelial progenitor cells protect the kidney from ischemia-reperfusion injury by microRNA-dependent reprogramming of resident renal cells. Kidney International, 82(4), 412–427.
Satheesh Madhav, N. V. (2011). Review on microparticulate drug delivery system. International Journal of PharmTech Research, 3(3), 1242–1254.
Plotkin, M. D., & Goligorsky, M. S. (2006). Mesenchymal cells from adult kidney support angiogenesis and differentiate into multiple interstitial cell types including erythropoietin-producing fibroblasts. American Journal of Physiology. Renal Physiology, 291(4), F902–F912.
Skalamera, D., Dahmer, M., Purdon, A. S., et al. (2012). Generation of a genome scale lentiviral vector library for EF1alpha promoter-driven expression of human ORFs and identification of human genes affecting viral titer. PLoS One, 7(12), e51733.
Arnaoutova, I., & Kleinman, H. K. (2010). In vitro angiogenesis: endothelial cell tube formation on gelled basement membrane extract. Nature Protocols, 5(4), 628–635.
Dragovic, R. A., Gardiner, C., Brooks, A. S., et al. (2011). Sizing and phenotyping of cellular vesicles using Nanoparticle Tracking Analysis. Nanomedicine: the Official Journal of the American Academy of Nanomedicine, 7(6), 780–788.
Deregibus, M. C., Cantaluppi, V., Calogero, R., et al. (2007). Endothelial progenitor cell derived microvesicles activate an angiogenic program in endothelial cells by a horizontal transfer of mRNA. Blood, 110(7), 2440–2448.
Baj-Krzyworzeka, M., Szatanek, R., Weglarczyk, K., et al. (2006). Tumour-derived microvesicles carry several surface determinants and mRNA of tumour cells and transfer some of these determinants to monocytes. Cancer Immunology, Immunotherapy, 55(7), 808–818.
Gagnon, R. F., & Gallimore, B. (1988). Characterization of a mouse model of chronic uremia. Urological Research, 16(2), 119–126.
Yamada, K., Miwa, T., Liu, J., Nangaku, M., & Song, W. C. (2004). Critical protection from renal ischemia reperfusion injury by CD55 and CD59. Journal of Immunology, 172(6), 3869–3875.
Kang, D. H., Kim, Y. G., Andoh, T. F., et al. (2001). Post-cyclosporine-mediated hypertension and nephropathy: amelioration by vascular endothelial growth factor. American Journal of Physiology. Renal Physiology, 280(4), F727–F736.
Bot, J., Whitaker, D., Vivian, J., Lake, R., Yao, V., & McCauley, R. (2003). Culturing mouse peritoneal mesothelial cells. Pathology Research and Practice, 199(5), 341–344.
Streja, E., Park, J., Chan, T. Y., et al. (2016). Erythropoietin dose and mortality in hemodialysis patients: marginal structural model to examine causality. International Journal of Nephrology 2016, 6087134.
Naffakh, N., Henri, A., Villeval, J. L., et al. (1995). Sustained delivery of erythropoietin in mice by genetically modified skin fibroblasts. Proceedings of the National Academy of Sciences of the United States of America, 92(8), 3194–3198.
Descamps, V., Blumenfeld, N., Beuzard, Y., & Perricaudet, M. (1996). Keratinocytes as a target for gene therapy. Sustained production of erythropoietin in mice by human keratinocytes transduced with an adenoassociated virus vector. Archives of Dermatology, 132(10), 1207–1211.
Dalle, B., Payen, E., Regulier, E., et al. (1999). Improvement of mouse beta-thalassemia upon erythropoietin delivery by encapsulated myoblasts. Gene Therapy, 6(2), 157–161.
Einbinder, T., Sufaro, Y., Yusim, I., et al. (2003). Correction of anemia in uremic mice by genetically modified peritoneal mesothelial cells. Kidney International, 63(6), 2103–2112.
Noh, H., Yu, M. R., Kim, H. J., et al. (2012). Uremia induces functional incompetence of bone marrow-derived stromal cells. Nephrology, Dialysis, Transplantation, 27(1), 218–225.
Wang, W., Liu, X., Wang, W., et al. (2016). The effects of indoxyl sulfate on human umbilical cord-derived mesenchymal stem cells in vitro. Cellular Physiology and Biochemistry, 38(1), 401–414.
Ratajczak, J., Wysoczynski, M., Hayek, F., Janowska-Wieczorek, A., & Ratajczak, M. Z. (2006). Membrane-derived microvesicles: important and underappreciated mediators of cell-to-cell communication. Leukemia, 20(9), 1487–1495.
Lappin, T. R., Maxwell, A. P., & Johnston, P. G. (2002). EPO’s alter ego: erythropoietin has multiple actions. Stem Cells, 20(6), 485–492.
Osada, S., Ebihara, I., Setoguchi, Y., Takahashi, H., Tomino, Y., & Koide, H. (1999). Gene therapy for renal anemia in mice with polycystic kidney using an adenovirus vector encoding the human erythropoietin gene. Kidney International, 55(4), 1234–1240.
Allan, D., Tieu, A., Lalu, M., & Burger, D. (2020). Mesenchymal stromal cell-derived extracellular vesicles for regenerative therapy and immune modulation: Progress and challenges toward clinical application. Stem Cells Translational Medicine, 9(1), 39–46.
Wang, Y., Lu, X., He, J., & Zhao, W. (2015). Influence of erythropoietin on microvesicles derived from mesenchymal stem cells protecting renal function of chronic kidney disease. Stem Cell Research & Therapy, 6, 100.
Funding
This study was supported by a faculty research grant from Yonsei University College of Medicine (6-2014-0042), a research grant from CHA Bundang Medical Center (2015 − 0301), and the Basic Science Research Program through the National Research Foundation of Korea (2012R1A1A2009345) funded by the Ministry of Education of the Republic of Korea.
Author information
Authors and Affiliations
Contributions
Conceptualization: Hoon Young Choi and Hyeong Cheon Park; Methodology: Hoon Young Choi, Hyeong Cheon Park, Tae Yeon Kim, Mirae Lee, Soo Hyun Kim, and Jong Hyun Jhee; Formal analysis and investigation: Hoon Young Choi, Tae Yeon Kim, Mirae Lee, Soo Hyun Kim, and Hyung Jong Kim; Writing - original draft preparation: Hoon Young Choi and Hyeong Cheon Park; Writing - review and editing: Hoon Young Choi, Yong Kyu Lee, Hyung Jong Kim, and Hyeong Cheon Park; Funding acquisition: Yong Kyu Lee, Hyung Jong Kim, and Hyeong Cheon Park; Supervision: Hyung Jong Kim, Jong Hyun Jhee ,and Hyeong Cheon Park.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interests.
Ethics Approval
The animal study protocol was performed in accordance with guidelines for laboratory animals and approved by the Institutional Animal Care and Use Committee, Department of Laboratory Animal Medicine, Medical Research Center, Yonsei University College of Medicine (2010-0226-1).
Consent for Publication
Not applicable.
Consent to Participate
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the Topical Collection: Special Issue on Exosomes and Microvesicles: from Stem Cell Biology to Translation in Human Diseases
Guest Editor: Giovanni Camussi
Supplementary Information
Supplemental Figure S1
Immunofluorescence staining of cytokeratin in mouse peritoneal mesothelial cells (PMCs). Immunofluorescence microscopy showing cytokeratin-labeled (red) mouse PMCs. DAPI, 4’,6-diamidino-2-phenylindole. (PNG 315 kb)
Supplemental Figure S2
Anemia and renal function in normal mice and mouse models of chronic kidney disease (CKD). (A) Hemoglobin levels and (B) blood urea nitrogen levels (BUN) and serum creatinine (Cr) levels in normal and CKD mice. *P < 0.05 vs. vehicle control, Kruskal–Wallis test. (PNG 60 kb)
Supplemental Figure S3
Masson’s trichrome staining of tissue from mouse models of chronic kidney disease (CKD). (A) Extensive fibrotic lesions were present in the cortex and corticomedullary junction of kidney sections from CKD mice after 6 and 9 weeks. (B) Semiquantitative injury scoring of the cortex and corticomedullary junction of kidney sections from CKD mice after 6 and 9 weeks. (PNG 2399 kb)
Supplement Figure S4
Erythropoietin (EPO)(+)–kidney-derived mesenchymal stem cell (KMSC)-derived extracellular vesicles (EPO(+)-EVs) mediate horizontal EPO mRNA transfer into human tubular cells (HK-2) and human podocytes in vitro. (A) Immunofluorescence microscopy showing red CellTracker™ -labeled EVs in human tubular cells (HK-2) and human podocytes. (B) EPO mRNA levels in HK-2 and human podocytes treated in vitro with EPO(+)-EVs. EPO(−)-EVs were used as negative controls.(PNG 413 kb)
Rights and permissions
About this article
Cite this article
Choi, H.Y., Kim, T.Y., Lee, M. et al. Kidney Mesenchymal Stem Cell‐derived Extracellular Vesicles Engineered to Express Erythropoietin Improve Renal Anemia in Mice with Chronic Kidney Disease. Stem Cell Rev and Rep 18, 980–992 (2022). https://doi.org/10.1007/s12015-021-10141-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-021-10141-x