Abstract
In recent years, umbilical cord blood (UCB) has been widely used as an alternative source to bone marrow (BM) for transplantation of hematopoietic stem and progenitor cells (HSPCs) in a variety of hematological and non-hematological disorders. Nevertheless, the insufficient number of UCB-HSPCs for graft represents a major challenge. HSPCs ex vivo expansion prior to transplantation is a valid strategy to overcome this limit. Several attempts to optimize the expansion conditions have been reported, including the use of mesenchymal stromal cells (MSCs) as feeder layer. Wharton’s Jelly (WJ), the main component of umbilical cord (UC) matrix, is especially rich in MSCs, which are considered ideal candidates for feeder layer in co-culture systems. In fact, they can be easily harvested and grow robustly in culture, producing a confluent monolayer in a short time. Similarly to bone marrow-mesenchymal stromal cells (BM-MSCs), WJ-derived MSCs (WJ-MSCs) have been used to support hematopoiesis in vitro and in vivo. Here, we review the rationale for using MSCs, particularly WJ-MSCs, as a feeder layer for UCB-HSPCs ex vivo expansion. In addition, we report the main findings attesting the use of these MSCs as a support in hematopoiesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The umbilical cord (UC) is an extra-embryonic formation which links the developing fetus to the placenta. Recently it has emerged that the tissues within the UC are a reliable source of both hematopoietic stem/progenitor cells (HSPCs), derived from umbilical cord blood (UCB), and mesenchymal stromal cells (MSCs), derived from the perivascular tissues. The UC is a perinatal tissue, easily accessible with no risks for the donor and causing no ethical concerns. UCB is considered an alternative source of HSPCs for hematopoietic stem cells transplantation (HSCT) with respect to bone marrow (BM) and peripheral blood, because of the easy availability, tolerance of HLA-mismatch, and low incidence of graft versus host disease (GVHD) [1]. Moreover, UCB-derived HSPCs have a higher frequency of progenitors with greater clonogenic potential compared to their adult counterpart [2, 3]. Unfortunately, the yield of UCB-HSPCs from a single unit is insufficient for the transplant in adult patients. Therefore, several attempts have been made to expand these cells in vitro by using multiple combinations of specific media, cytokines, growth factors and more recently also mesenchymal stromal cells (MSCs) as feeder layers. The rationale behind the use of MSCs as a stromal support in in vitro settings is based on the physiological role of these cells in BM, where they act as a natural scaffold for HSPCs growth. A wealth of evidence exists showing that MSCs influence HSPCs homing, retention, proliferation and differentiation by means of two mechanisms: cell-to-cell contact and paracrine factors secretion [4]. Many preclinical and clinical studies have demonstrated that the co-transplantation of UCB-HSPCs with BM-MSCs enhances the hematopoietic cell engraftment and accelerates platelet and neutrophil recovery after transplantation [5]. Wharton’s jelly-MSCs (WJ-MSCs) isolated from UC-matrix may be an ideal candidate for the stromal feeder layer in co-culture systems, in that they are easily harvested and can readily be expanded to reach a confluent monolayer in a short time [6]. Conversely to BM-MSCs, only a limited number of studies have investigated the role of WJ-MSCs in supporting ex vivo expansion of HSPCs. In this review, we discuss the rationale for using MSCs, in particular WJ-MSCs, as a feeder layer in HSPCs ex vivo expansion and we report the main results obtained in this field.
Human Umbilical Cord Tissue: a Source of Mesenchymal Stromal Cells and Hematopoietic Cells
The umbilical cord is essential for fetal development since it contains the umbilical vessels that provide the blood flow between the developing fetus and the placenta during pregnancy. The histological organization of human UC reveals the presence of multiple tissue layers. Externally the UC consists of an umbilical epithelium, also known as amniotic epithelium. Beneath which, a thick layer of mucous connective tissue, named Wharton’s jelly (WJ), embeds the umbilical vessels (two arteries and one vein). The main physiological function of Wharton’s Jelly is to prevent compression, torsion and bending of the vessels during pregnancy. WJ contains an abundant extracellular matrix which is particularly rich in glycosaminoglycans (GAGs), mainly hyaluronic acid (HA) and proteoglycans. The fibrillar component is less abundant and contains several types of collagen molecules of either a fibril- or non-fibril-forming types. The cells residing in WJ have been the object of studies in past years, and were classically identified as either myofibroblasts or atypical fibroblasts [reviewed in 7]. Several authors have demonstrated that the most of cells contained in the stromal compartment exhibit the vast majority of features typical of mesenchymal stromal cells [7, 8]. UCB is a hematopoietic tissue which contains a heterogeneous population of hematopoietic cells, either stem or progenitor cells capable of self-renewal and of generating all blood cell types, respectively [9]. Phenotypically, HSPCs are identified by the expression of CD34 surface glycophosphoprotein, [10] and by the absence of all lineage specific markers (Lin negative). In UCB, this primitive population represents about 0.1–0.4 % of total nucleated cells (TNCs). Within the Lin−/CD34+ cell population, the CD38 marker is used to differentiate multipotent progenitors (CD38-), and committed progenitors (CD38+). The subpopulation Lin−/CD34+/CD38- represents about 10 % of HSPCs in UCB [11, 12]. The co-expression of CD90 or CD133 on CD34+/CD38- cells defines the hematopoietic stem cells with long-term repopulating ability [12, 13]. Compared to adult HSPCs, UCB-derived HSPCs are easily available at birth and have higher in vitro proliferation capacity with superior in vitro clonogenic potency and in vivo engraftment capacity, and therefore they can enhance BM-reconstitution after transplantation [14–16]. These features make UCB grafts as elective choice for HSCT in patients with hematological diseases and other disorders such as lysosomal storage disorders (LSD) [17]. Unfortunately, the yield of UCB-HSPCs from a single unit is often insufficient for transplant in an adult patient. Therefore, different strategies have been employed to increase the number of UCB-HSPCs while maintaining their repopulating capacity. In this regard, the feeder co-culture system with mesenchymal stromal cells, derived from bone marrow or perinatal tissues, represents an optimal approach to overcome this limit.
WJ-MSCs: Main Features and Mechanisms of Interactions with Hematopoietic Cells
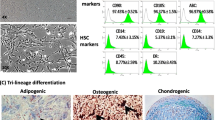
WJ-MSCs fulfill all the criteria proposed by the International Society for Cellular Therapy (ISCT) to define a MSC population: expression of markers, cellular morphology, multipotency, ability to self-renew, and plastic adherence [18]. WJ-MSCs have some traits in common and some distinctive traits with respect to BM-MSCs [6, 19]. Due to their relative “youth”, WJ-MSCs, as well as other perinatal cells, have a higher expansion ability with faster population doubling time than the adult MSCs. The expansion capability is linked to a high telomerase activity typical of stem cells [20]. WJ-MSCs are considered a therapeutic tool for regenerative medicine applications thanks to their ability to trans-differentiate into multiple mature cell types in vitro and in vivo [20–29]. Apart from the classical markers that identify the MSC population according to ISCT criteria (CD73, CD90, CD105), a few recent papers have reported other markers expressed by WJ-MSCs and BM-MSCs. Surface antigens such as CD10, CD13, CD44, CD49e, and CD166 are now recognized as part of their phenotype [20, 27–34] (Table 1). Intriguingly, recent papers have also highlighted that WJ-MSCs express several other molecules which may further help to characterize their phenotype in vitro and elucidate some of the possible interaction pathways with HSPCs and/or mature blood cells. For example, CD117 (c-kit), the receptor for the stem cells factor (SCF) harboured by HSPCs, has been repeatedly detected in WJ-MSCs and little is known about the role of this interaction [27]. Nilsson and co-workers were the first to show that WJ-MSCs express the osteopontin gene [35], while Raio et al. found that WJ-MSCs are able to secrete hyaluronic acid [36]. Interestingly, both these molecules are among the main constituents of the HSPCs niche. In particular, osteopontin is a critical regulator of HSPCs localization and proliferation [35]. WJ-MSCs as well as other MSCs express CXCL12 (CXC-Chemochine-ligand-12, also known as SDF-1α, stromal derived factor-1), an important regulator of hematopoiesis and HSPCs homing. This chemokine, by interacting with its receptor CXCR4 (CXC-Chemokine-receptor 4) localized on HSPCs surface, plays a role in the cyclical HSPCs mobilization and homing from and to the BM vascular niche [37–39]. Most of the cytokines involved in hematopoiesis regulation known to be expressed by BM-MSCs are also secreted by WJ-MSCs (see Table 1). Key examples are interleukin (IL)-6, SCF, Fms-related-tyrosine kinase-3 ligand (Flt-3 ligand), and macrophage-colony stimulating factor (M-CSF). Conversely, unique to WJ-MSCs is the ability to secrete further molecules associated with HSPC proliferation, such as granulocyte-colony stimulating factor (G-CSF) and granulocyte-macrophage -colony stimulating factor (GM-CSF) [40, 41]. All this evidence supports the idea of using these cells as feeder layers for HSPCs expansion. With the growing number of reports adding new information on WJ-MSCs secretome and basic biology, it can be expected that their ability to interact with HSPCs will be further confirmed in the near future. Moreover, further research needs to be done in order to clarify the role of WJ-MSCs in the microenvironment in supporting fetal hematopoiesis, and confirm the use of these cells as feeder layers for the expansion of hematopoietic progenitors. In addition to the hematopoietic-supportive function, MSCs are used in transplantation settings to constrain the immune response of recipient to donor cells, thus limiting graft rejection [42]. MSCs exert this immunosuppressive function via modulation of both cellular and innate immune pathways [43, 44]. WJ-MSCs derive from a naturally immune-privileged tissue and, by maintaining a positional memory of their features, may have a selective advantage to escape the immune system also in an immunocompetent environment, more than their adult counterpart [45]. Extended characterization of WJ-MSCs immune molecules has revealed the expression of non-classical class Ib MHC molecules such as HLA-G (both the membrane-located molecule and its soluble form HLA-G5), HLA-F, HLA-E, together with other molecules, such as the Early Pregnancy Factor (EPF) which is a secreted molecule currently undergoing investigation [46–49]. All of these factors have a key role in the induction of tolerance of the mother’s immune system toward the semi-allogeneic embryo, in particular for maternal NK cells [46]. Several mechanisms have been proposed to explain the hypoimmunogenicity and immune-modulation caused by WJ-MSCs [50–52], however this field needs to be extensively explored in order to improve their clinical application.
Rationale for UCB-HSPCs Ex Vivo Expansion
Unrelated UCB transplantation has become one of the standard therapeutic options for pediatric patients with hematological malignancies and various genetic, hematological or immunological disorders [reviewed in 53–55]. Compared to BM grafts, the UCB graft offers substantial advantages such as greater availability of banked cryopreserved UCB units, with consequently shorter time to UCBT (a median of 25–36 days earlier compared to BM); a wider donor pool due to tolerance of 1–2 HLA mismatches out of 6 (higher HLA mismatch is associated with lower probability of engraftment); lower risk of transmitting infections by latent viruses; and lower incidence and severity of GVHD without compromising graft versus leukemia/lymphoma (GvL) effects [56]. The lower incidence and severity of GVHD in UCB recipients is the direct consequence of the biological properties displayed by UCB lymphocytes: reduced proliferation, cytokine production, and cytotoxicity to alloantigens [57]. Despite these logistical and clinical advantages, the UCBT in adult patients is limited by the low number of progenitors present in UCB unit. This limit causes a slower engraftment time with consequent slightly higher risk of disease relapse and mortality from bacterial infections due to delayed immune system recovery [56, 57]. To overcome these drawbacks and increase the number of transplantable HSPCs, two main strategies have been investigated: infusion of two UCB units, and ex-vivo expansion of UCB-HSPCs [58, 59]. Although the co-transplantation of two un-manipulated UCB units led to significant improvements over the single unit infusion, the hematopoietic recovery remains often suboptimal [60]; this has been correlated with the observation that only cells from one UCB ultimately predominated in the reconstituted BM [61]. Therefore, recently, efforts have been focused on the development of ex vivo expansion technologies to increase the total number of UCB-HSPCs while preserving their stemness and capacity to differentiate in all blood cell types [62, 63].
UCB-HSPCs Expansion Conditions
Various protocols have been developed to promote UCB-HSPCs ex-vivo expansion by using different media, growth factors and cytokines [reviewed in 63]. Most of them converge on the supplementation of three early hematopoietic cytokines: SCF, thrombopoietin (TPO), and Flt-3, known to be important for the growth and maintenance of hematopoietic cell stemness and pluripotency. Further attempts have been made to optimize HSPCs ex vivo expansion rate with the addition of other cytokines, IL-3, IL-6, IL-11 and G-CSF, known to be involved in the maintenance of primitive progenitors. However, the cytokine-mediated expansion methods generated only moderate increases in the number of progenitor cells with consequently modest improvement in neutrophil and platelet recovery after transplantation [62, 64–66]. For this reason, the need to improve expansion conditions led to the use of other growth factors known to enhance cell proliferation, such as angiopoietin-like proteins (Angptl-protein) [67], pleiotrophin [68] and insulin-like growth factor-binding protein-2 (IGFBP-2) [69, 70]. Apart from peptides and proteins, also small molecules and chemical compounds have also been investigated for their ability to promote progenitor cells expansion [71]. This was the case of tetraethylenepentamine (TEPA, a copper chelator) [72], StemRegenin 1, identified as aryl hydrocarbon receptor antagonist (SR1) [73], and nicotinamide (NAM), a potent inhibitor for both NAD + −dependent enzymes and sirtuin-1-inhibitor [74]. All these molecules enhanced the hematopoietic stem cells proliferation and differentiation. Another chemical compound, UM171, in cooperation with SR1, has been demonstrated to increase the number of long-term hematopoietic progenitors and inhibits differentiation toward erythroid and megakaryocytic lineages [75]. One of the most potent molecules that promotes ex vivo HSPCs amplification is Notch ligand [76] which plays a critical role in self-renewal, survival, proliferation and differentiation of stem and progenitor cells in vitro and in enhancing engraftment in vivo [77]. Since most of these studies confirm that the cytokine-driven expansion conditions are accompanied by concomitant cell differentiation, in recent years the use of stromal cells has been suggested as a more natural approach to augment the number of UCB-derived HSPCs [78].
Rationale of MSCs as a Feeder Layer to Enhance UCB-HSPCs Expansion
The long-term fate of HSPCs depends on migration, adhesion to the niche, and subsequent regulation of self-renewal versus differentiation state [79]. All these properties are regulated by cues provided in vivo by the niche cellular microenvironment. MSCs, together with endosteal cells, vascular cells and pericytes, form the BM niche and play a key role in supporting both maintenance and differentiation of the stem cell pool [80–84]. Therefore, this supportive interaction could be mimicked by an in vitro model where HSPCs are co-cultured in the presence of MSCs as stromal support [85, 86]. Although numerous studies have demonstrated the capacity of MSCs as a feeder to maintain the undifferentiated state of HSPCs with different degrees of efficacy [87–89], little is known about the precise cellular and molecular mechanisms involved in these interactions. It has been suggested that MSCs could support hematopoiesis by two mechanisms: direct cell-to-cell contact and secretion of specific factors [37, 78]. Some reports demonstrated that cell-to-cell contact is crucial to promote expansion of stem cell progenitors [38] and some authors even highlighted after expansion, two hematopoietic cell populations with different phenotypic and biological characteristics: one adherent to the stromal layer and the other floating in the medium [90]. The notion that the contact with MSCs influences the hematopoietic cell behavior and fate is supported by microscopical observations. The hematopoietic cells form pseudopodia-like protrusions and acquire high motility when co-cultured in the presence of a MSC monolayer [91]. Moreover, in the co-culture system it is possible to observe clusters of tightly packed cells, referred to as a cobblestone areas, composed of hematopoietic progenitors that adhere to the stromal cells [92]; the ability of HSPCs to form cobblestone areas is currently used as an in vitro test, (cobblestone area-forming cells assay, CAFC), to assess the frequency of long-term BM-reconstitution HSCs.
It is not definitely known whether the interaction between MSC and HSPCs, resulting in HSC proliferation, is mediated by diffusible factors crossing over from the MSCs to HSPCs during cell-to cell contact or through secretion of them by the MSCs into the microenvironment where HSPCs are located [91]. Different reports have highlighted that soluble factors released by MSCs are sufficient to promote hematopoietic cells expansion [86, 93]. Among these, some growth factors, chemokines and cytokines such as tumor necrosis factor-alpha (TNF-α), transforming growth factor-beta1 (TGF-β1), leukemia inhibitory factor (LIF), CXCL12, SCF, M-CSF, IL-3, IL-6, TPO and Flt-3 ligand have been implicated in the regulation of either survival, proliferation, homing or differentiation of HSPCs [37]. In particular, elevated levels of CXCL12 in the co-culture system have resulted in down-regulation of a number of cytokines and chemokines that promotes HSPCs differentiation and restrains self-regeneration [38, 94]. The enhanced engraftment reported in in vivo studies after co-transplantation of MSCs and HSPCs is probably related to the production by MSCs of cytokines and growth factors, such as SDF-1α, that promotes the homing and expansion of the transplanted HSPCs [95, 96]. In this context, an extended characterization of the intrinsic properties of stromal cells as feeder will be mandatory to better understand their potentiality as a tool for HSPCs expansion.
BM-MSCs Support Hematopoiesis
The ability of BM-MSCs to support hematopoiesis has been reported in both pre-clinical and clinical studies. The pathways through which the hematopoietic supportive function of stromal cells is exerted are not fully elucidated. Some authors have provided evidence that the direct cell-to-cell contact is crucial to promote HSPCs growth [97, 98] and to preserve their stemness [99], while others suggest that the contact is more essential for the regulation of mature blood cells production [100, 101]. Conversely, some papers pointed out that the secreted paracrine soluble factors are key players in hematopoiesis [84, 102]. Different studies have attempted to establish the optimal combination and concentration of different cytokines to expand HSPC in culture in presence of BM-MSCs, with divergent results [5, 78, 103–106]. The addition of two epigenetic regulators, namely 5-aza-deoxycytidine (aza-D) and trichostatin A (TSA), to the culture medium was found to enhance BM-MSCs feeder action to maintain the UCB-HSPCs stemness [107]. Another strategy to strengthen the BM-MSCs function as feeder layers is their genetic manipulation in order to induce the secretion of crucial factors for HSPCs growth such as angiopoietin-like 5, [108] or the expression of human telomerase reverse transcriptase (hTERT) [109]. More recent studies focused on miming the BM niche in vitro by seeding the MSCs on three-dimensional (3D) collagen or fibrin scaffolds together with HSPCs. An increased migration of HPSCs toward MSCs was observed and, in addition, higher levels of molecules involved in the maintenance of a quiescent pool of HSPCs were detected [110]. Moreover, a synergic action between 3D scaffolds and MSCs to increase the proliferation of HSPCs retaining a more primitive phenotype has been reported [110, 111]. The supportive functions of BM-MSCSs have been proved in mouse models where the co-transplantation of BM-MSCs with UCB-HSPCs resulted in higher hematopoietic engraftment versus UCB-HSPCs transplantation alone [41, 112, 113]. All these successful in vitro and in vivo findings opened the way to clinical translation. De Lima and co-workers transplanted 31 myeloablated patients affected by hematologic malignancies with two UCB units, one un-manipulated and one expanded for 14 days on BM-MSCs layers in the presence of SCF, TPO, Flt-3 ligand and G-CSF. This protocol significantly improved engraftment compared to that of using un-manipulated double UCB units as a graft. However, long-term follow-up showed that only the cells derived from the un-manipulated UCB unit ultimately contributed to long-term donor-derived hematopoiesis. The authors attributed the positive engraftment results to the increased numbers of committed progenitors in the expanded cells that accelerated the hematopoietic recovery [114]. The long time needed to expand a sufficient number of BM-MSCs is unfortunately a logistical problem correlated to the use of these cells as a feeder layer for HSPCs ex vivo expansion, since the progression of some hematological diseases, such as leukemia, sometimes has a fast clinical course. For this reason, MSCs derived from alternative sources, in particular UC-matrix derived MSCs, have been employed for their prompt availability and great proliferation capacity.
State of the Art on the Use of WJ-MSCs as a Feeder Layer for HSPCs Expansion
The amount of recent data coming from laboratories worldwide attests the use of WJ-MSCs as feeders for HSPCs growth and maintenance in vitro and as support for engraftment in vivo. In this regard, the advantages of using WJ-MSCs as stromal support, alternatively to BM-MSCs, can be summed up in the following key features: immediate availability, painless procedures to donors, lower risk of viral contamination, higher ex vivo expansion rate, and expression of specific cytokines and growth factors that are involved in the hematopoiesis. Several attempts have been made to define the role of WJ-MSCs to support ex vivo HSPCs expansion: the main findings are summarized in Table 2. In 2006, Lu and colleagues [40] were the first to establish a protocol to isolate abundant MSCs from UC tissue by an enzymatic procedure and to show their hematopoiesis supportive function. They found that UC-MSCs shared several phenotypic and molecular features with BM-MSCs but had higher in vitro colony–forming unit-fibroblast (CFU-F) potential and higher proliferation ability as demonstrated by a faster cell population doubling time. The authors highlighted in UC-MSCs the expression of cytokines and growth factors involved in hematopoiesis (SCF, LIF, Flt-3 ligand , IL-6, M-CSF , VEGF) as well as in the HSC engraftment (SDF-1). The levels of expression of these factors were comparable to those to BM-MSCs; additionally, the UC-MSCs also expressed GM-CSF and G-CSF, growth factors crucial to expand granulocyte and macrophage progenitors. The hematopoietic supportive function was assessed by co-culturing CD34+ cells from allogeneic cord blood with UC and BM-derived MSCs as feeder layers. After 5 weeks, the clonogenic potential of both co-cultured CD34+ cells was evaluated in a long-term CFU assay and no difference in the number of CFU-GEMM, BFU-E CFU-GM colonies generated from the most primitive progenitors was reported. In addition, the typical cobblestone areas generated by primitive hematopoietic stem cells were observed in both co-culture systems. Overall, these data highlighted a comparable hematopoietic-supportive potential between UC-and BM-MSCs. In this study, noteworthy was the low expression of the HLA-ABC molecule detected on UC-MSCs in addition to the absence of HLA-DR expression that is typical in MSCs populations. These findings, also reported for human umbilical cord perivascular stromal cells [115], strengthen the usefulness of UC-MSCs for allogeneic cell therapy in that the low expression of the HLA-ABC molecule would limit the host immune response. These promising findings have aroused interest to use UC-MSCs as feeders for ex vivo HSPCs expansion. The potential therapeutic application of WJ-MSCs, as stromal support for the growth and maintenance of UCB-derived hematopoietic stem cells in culture, comes also from the group of Bakhshi [116]. They showed that WJ-MSCs, similarly to BM-MSCs, effectively maintained UCB-CD34+ cells as demonstrated by the capability to form colonies in the long-term culture initiating cells (LTC-IC) assay. Friedman and co-workers [41] reported that UC-MSCs produced significant amounts of hematopoietic cytokines and growth factors and enhanced the hematopoietic engraftment in SCID mice. They observed a greater number of hematopoietic colonies, in particular CFU-GM, when the UCB-mononuclear cells (UCB-MNC) were plated in semisolid medium in the presence of a UC-MSCs monolayer. Moreover, NOD/SCID γcnull mice, when co-transplanted with a limited number of either unfractionated UCB-MNCs or selected UCB-CD34+ cells and UC-MSCs, showed a higher frequency of human CD45+ cells in both bone marrow and peripheral blood compared to mice transplanted with UCB cells alone. The authors suggested that this improvement was due to the capacity of co-injected UC-MSCs to provide an organized stroma essential for the hematopoietic cell engraftment; this function may be sustained by the numerous factors released by UC-MSCs. More recently, Magin and co-workers [117] compared the feeder potential of three primary cell types: BM-MSCs, WJ-MSCs and umbilical cord vein endothelial cells (HUVECs). They found that all these primary cells had a comparable potential to support UCB-CD34+ cells expansion, with WJ-MSCs even superior than the other two cell types. In co-culture systems with UCB and the three cell monolayers, MNC expansion was 30- to 60-fold, colony-forming cells expansion 20- to 40-fold, and cobblestone area-forming expansion 10- to 50-fold. Another study, carried out by Tipnis and co-workers [118], showed that UC-MSCs of autologous or allogenic origin were similarly able to sustain both fresh or cryopreserved UCB-CD34+ cells expansion in the presence of a very low concentration of exogenous cytokines (SCF, Flt-3, TPO, b-FGF). After 14 days of co-culture, both autologous and allogeneic UC-MSCs were able to increase the number of TNCs (about 27-fold), the number of CD34+ cells (24-fold), and the number of colonies developed in short-term CFU assay (more than 5-fold) compared to the uncultured UCB-CD34+ cells. In this study, the expansion potentiality of UC-MSCs of both origins was superior to that of BM-MSCs as a feeder. Even in this study it was ascertained that the UC-MSCs released high levels of SDF-1α, Flt-3, G-CSF, GM-CSF, TPO, angiogenin, HGF, LIF, and IL-6, all of which play an important role in CD34+ cells growth. In addition, the cell adhesion molecules CD29 and CD44, required for homing HSC to BM in vivo, were also expressed. Of note, the CD34+ cells expanded in contact with UC-MSCs became strongly positive for cell adhesion molecules, such as VLA-4 (very late antigen-4) and LFA-1 (lymphocyte function associated antigen-1), known to be involved in the maintenance of stemness. The results reviewed so far, while attesting the hematopoiesis-supportive role of WJ-MSCs, are elusive about the mechanisms underlying this function: cell-to-cell direct contact and/or soluble factors secretion. Fong and colleagues [91] addressed this issue by measuring the proliferation rate and the clonogenic potential of UCB-CD34+ cells when cultured either in direct contact with WJ-MSCs or in WJ-MSCs-conditioned medium (WJ-MSCs-CM) using UCB-CD34+ cells grown alone as control. After 9 days of culture, in a medium supplemented with early hematopoietic cytokines cocktail (SCF, TPO, Flt-3 ligand), a significant increase of CD34+ cells number and frequency was observed in both conditions, with WJ-MSC-CM condition even superior. Moreover, a more than 2-fold increase of colony numbers was found with respect to controls in the CFU-assay, when CD34+ cells were cultured in direct contact with MSCs or in the presence of conditioned medium. All the six morphological colony types were observed in all conditions suggesting a normal hematopoiesis process in vitro. These findings strengthen the use of conditioned medium, either un-fractionated or pre-fractionated, for future clinical applications, avoiding the possible side effects of harmful agents transmission from the stromal cells used as support for cell expansion. Interestingly, the authors observed that UCB-CD34+ cells, either in co-culture system or in the presence of CM, presented pseudopodia-like outgrowths and acquired higher motility. Time-lapse microscopy showed that these cellular protrusions helped the UCB-cells to migrate toward the MSC surface, suggesting that MSCs may favor HSPC homing to BM niche. Proteomic analysis of the WJ-MSC-CM revealed high levels of interleukins (IL-1a, IL-6, IL-7, IL-8), as well as SCF, HGF and ICAM-1, suggesting once again that they may be the agents involved in the UCB-CD34+ cells expansion. In a recent work, Milazzo and co-workers [119] proved the capability of WJ-MSCs to expand UCB-CD34+ cells in vitro and to improve their engraftment in NOD/SCID mice. The co-culture of purified-CD34+ cells with WJ-MSCs, without cytokines addition, increased the number of CD34+ cells by 2.0 and 7.0 times after 7 and 13 days respectively, compared to control (uncultured CD34+ cells at day 0). The authors observed, after 7 days of exposure to WJ-MSCs, the expansion of primitive hematopoietic progenitors (CD34+/CD90+ cells, 1.8-fold expansion, and CD34+/ CD33-, 27.4-fold expansion) as well as multipotent early progenitors (CD34+/CD38+, 4.1-fold expansion). The ability by WJ-MSCs to support early hematopoietic progenitors during co-culture was also demonstrated by the amplification of CD34+ cells with higher clonogenic potential (2.2 and 7.5 fold increase after 7 and 13 days, respectively) and higher frequency of ALDH+ cells (enzyme aldehyde dehydrogenase positive cells), in comparison to controls. ALDH is a stem cell marker involved in stem cells differentiation and proliferation [120]. Moreover, cells co-cultured for 7 days on WJ-MSCs migrated more efficiently (30 % higher migratory capacity) compared to CD34+ uncultured cells, in a trans-well migratory assay toward the stromal derived-factor 1α (SDF-1α). The efficacy of the WJ-MSCs to enhance the repopulating capacity of hematopoietic progenitors was evaluated. The expanded CD34+ cells, particularly at 7 days of co-culture, engrafted NOD/SCID mice more efficiently than the uncultured CD34+ cells (100 % versus 75 % transplantation success). The ability of WJ-MSCs and BM-MSCs to enhance engraftment of UCB-CD34+ cell transplanted in NOD/SCID mice was also evaluated by Van De Garde and co-workers [121]. They found that both MSCs populations promoted comparable enhanced recovery of human platelets and human CD45+ cells in mice peripheral blood and found 6-weeks after transplantation a 3-fold higher engraftment of human HSPCs in the BM, blood and spleen when compared to uncultured CD34+ cells. The authors also investigated the phenotypic and functional properties acquired by the UCB-CD34+ cells after direct contact for 10 days with the stromal cells, in the presence of the cytokine TPO. A significant increase of CD49d and CD49e expression was observed in addition to a slight rise of other adhesion molecules (CD11a, CD11b, CD184) associated with homing to or retention in the BM. No increase in the number of TNCs and CD34+ cells or changes in the ratio between different cell subpopulations were reported after co-culture with both WJ-and BM-MSCs. The authors suggested that the culture conditions used, absence of early hematopoietic cytokines and presence of only TPO, may explain the lack of TNCs and CD34+ cells expansion. These results are in agreement with TPO functioning to enhance the platelet repopulation in vivo and to retain the hematopoietic engraftment capacity in NOD/SCID mice [122, 123]. Interestingly, the HSPCs cultured on BM-MSCs stroma were able to generate more BFU-E colonies, while those cultured on WJ-MSCs gave rise to higher numbers of CFU-GEMM generated from the most primitive hematopoietic progenitors. In these studies, the immunosuppressive properties of both MSC populations were confirmed in experiments of T-cell proliferation inhibition of PBMC (peripheral blood mononuclear cells) stimulated with αCD3αCD28 beads. Klein and co-workers [124] compared the hematopoietic ability of WJ-MSCs with other MSCs derived from perinatal tissues including amniotic fluid, amnion, chorion, and cord blood, which were tested for the same tasks. They measured the expansion rates of CD34+ cells after co-culture of UCB-MNCs with MSCs feeders derived from all the above-mentioned perinatal sources, including WJ-MSCs and BM-MSCs. In particular, the fold increase of CD34+ and CD45+ cells was measured after 14 days of co-culture and the clonogenic potential of the cultured cells was determined in short-and long-term assays. The results showed in all the experiments comparable expansion rates of CD34+ and CD45+ cells, and high ability to form CFUs in the short-term assay, particularly when a low number of CD34+ cells (5 × 102 to 1 × 104) were cultured per cm2 of MSC-monolayer. Expansion of LTC-IC was partly detected in this experiment. However, the expansion of CD34+ cells was significantly more effective when co-cultured with MSCs from BM and amniotic fluid, compared to that observed in amnion, chorion and Wharton’s Jelly as feeders. In order to explain the very high expansion rate detected the authors revisited other data in the literature and found similar results when a low number of CD34+ cells and a high concentration of TPO were used. In particular, this cytokine is known to have an anti-apoptotic effect on HSPCs [125]. Of note, this work also reported that cryopreserved MSCs, compared with fresh ones, had a better capability to expand UCB-CD34+ cells. This result is important in a clinically-oriented interpretation of the data since banked cells are prompt to be employed for therapeutic approaches [124]. The ability of different MSCs to support UCB-CD34+ cells was also investigated by Kadekar and colleagues [126]. They performed a systematic comparison of placental-and cord-derived MSCs characteristics and found that these two cell types presented very a similar morphology, phenotype and potentiality to differentiate toward three cell lineages (osteoblasts, adipocytes and chondrocytes) but had differential ability to support the ex vivo expansion of UCB-CD34+ cells. In particular, placenta derived-MSCs (P-MSCs) resulted to be a better feeder similarly to BM-MSCs for ex vivo maintenance of primitive HSCs, with a higher engraftment potential than that of cells expanded on UC-MSCs layer. Precisely, CD34 + cells expanded on P-MSCs showed a higher percentage of primitive CD34+/CD38-cells, higher CFU and LTC-IC ability and better in vitro adhesion to fibronectin and migration ability toward SDF-1α. The NOD/SCID repopulation ability of HSPCs cultured in the presence of P-MSCs was enhanced compared to that of cells grown on UC-MSCs. After 10 days of co-culture, the authors found a significant 400-fold and 250-fold increase in the number of TNCs when UCB-CD34+ cells were in the presence, respectively, of P-MSCs and UC-MSCs, compared to the uncultured CD34+ cells. The massive expansion reported in the cells co-cultured with P-MSCs did not hinder the quiescent state of the expanded CD34+ cells, as revealed by the high percentage of cells found in G0/G1phase of cell cycle at the end of culture. A further 2.5-fold increase in immature hematopoietic progenitors cells CD34+/CD38-, a higher proportion of the most primitive CD34+/CD133+ cells, and a higher clonogenic potential was reported for CD34+ cells expanded on the P-MSC layer compared to UC-MSCs ones. In particular, there were 1.5 times more CFUs, a 4-fold increase in BFU-E and a 1.6-fold increase in CFU-GEMM. The in vivo studies demonstrated that CD34+ cells expanded in both feeder layers resulted in multi-lineage engraftment in NOD-SCID mice, with enhanced repopulation ability by CD34+ cells expanded on P-MSCs. These functional data correlated well with the different expression of molecules involved in stem cells self-renewal and maintenance by the two mesenchymal cell types. In particular, the authors argued that P-MSCs supported the expansion of functionally superior HSCs, with higher levels of Notch, Wnt and hepatic growth factor (HGF) expression. On the other hand, UC-MSCs facilitated more the expansion of committed progenitors by the secretion of pro-inflammatory cytokines, such as IL-1α, β, human monocyte chemotactic protein2 and 3 (MCP 2,3) and C-C motif chemokine 20 (CCL20, also known as MIP-3α), that drive HSCs differentiation processes [126].
Clinical Application of UC-MSCs and HSPCs Co-Transplantation
Up to now no clinical application of expanded UCB on UC-MSCs feeder layer has been documented. Nevertheless, the promising pre-clinical results of hematopoietic supportive function by UC-MSCs, here reviewed, have led researchers to co-infuse UC-MSCs with UCB-HSPCs to improve hematopoietic cells transplantation outcome. A pilot study carried out by Wu and co-workers [128] evaluated the safety and efficacy of co-transplantation of UC-MSCs with un-manipulated UCB unit. Five pediatric patients, three with non-malignant hematologic diseases and two with leukemia, received the co-transplant, while nine patients were engrafted with UCB alone. The intravenous co-infusion was feasible and no graft failure was reported. All 14 patients reached 100 % cellular chimerism on the 60th day of transplantation. The time needed to achieve neutrophil and platelet recovery was shorter in patients receiving the co-transplant compared to those receiving UCB alone. No transplant–related mortality was reported among the five patients receiving the co-transplant. By contrast, two of the nine patients receiving UCBT alone died for bacterial infections as result of prolonged neutropenia. The same authors reported analogous results in another study of UCBT in 32 patients with high risk of acute lymphoblastic leukemia in which 20 were co-transplanted with UC-MSCs and 12 transplanted with UCB alone [129].
In another study, Wu and colleagues co-transplanted UC-MSCs with adult haploidentical-HSPCs, derived from BM and mobilized peripheral blood, in patients with refractory/relapsed hematological malignancy They reported a fast hematopoietic engraftment and no adverse infusion-related reactions [130]. The same engraftment improvement in patients with severe aplastic anemia (SAA) was reported in other two studies of co-transplantation of UC-MSCs with HSPCs derived from adult sources [131, 132]. The concomitant infusion of MSCs and adult HSPCs seems to be particularly effective in patients with SAA since these patients have defective MSCs that compromise the engraftment of the allogeneic transplanted HSPCs [133, 134]. In this setting, the infusion of normal MSCs may play an important role in providing the specialized BM microenvironment to allow HSPCs engraftment.
Conclusions and Future Perspectives
MSCs play an important role in modulating the BM microenvironment and supporting hematopoiesis. The hematopoietic environment of patients who receive HSCT is often damaged by chemotherapy, irradiation or by the malignant hematological disease per se [135, 136]. For this reason, as well as to induce immune tolerance, the co-transplantation of BM-MSCs with HSPCs is widely used to reconstitute the damaged stroma and to provide all the hematopoietic cytokines ligands and stem cell factors needed to promote HSPCs homing and engraftment [137, 138]. The co-infusion with MSCs, including WJ-MSCs, at the time of HSPCs has effectively been of benefit in HSCT, in particular in UCBT where the limited number of hematopoietic cells is associated with high graft failure.
As regards their supportive function, MSCs have been exploited as a feeder layer in the co-culture system to increase the number of UCB-derived HSPCs. MSCs isolated from Wharton Jelly appear to offer greater clinical utility compared to BM-MSCs, due to their higher efficiency of recovery coupled with a painless isolation procedure, minimal ethical concerns, higher rate of expansion and lower immunogenicity. A further intriguing feature is their origin from a perinatal tissue. On one hand, this enables WJ-MSCs to interact with hematopoietic and immune cells by means of both cell-cell contact and secetion of paracrine factors. On the other hand, it may be supposed that the common anatomical localization of WJ-and UCB-HSPCs should favor a more efficient cross-talk between the two cell types. Considering the striking differences between the bone marrow stem cells niche and the Wharton’s jelly one, more research is needed in this field to ascertain the multiple unknown in vivo roles of WJ-MSCs.
The results of pre-clinical studies reported here attest that the WJ-MSCs are optimal feeders for ex vivo expansion of UCB-HSPCs. The co-culture strategy is more attractive than the cytokine-driven culture condition which still has some constraints that delay the clinical translation: (i) the difficulty to establish the optimal culture conditions to expand and maintain stemness of hematopoietic cells, (ii) the expensive cost of cytokines for large-scale culture and the heterogeneous potency between commercial lots of active culture compounds, and (iii) the cytotoxicity due to the use of non-physiological concentrations. The use of UC-MSCs as a feeder layer overcomes most of the limits of cytokine-driven culture systems. On the other hand, the co-culture condition needs to be also worked out to improve its effectiveness and safety. In particular, protocols of UC-MSCs expansion have to be well defined as regards the type of culture media, the number of cell passages, and the risk of pathogens transmission from cell-to-cell. Moreover, the mechanisms underlying hematopoietic supportive function by UC-MSCs need to be further investigated since several questions are still open. The first is whether or how cell-to-cell contact and/or secretion of soluble factors influence the entire process and if both mechanisms are needed to achieve maximum efficacy. A comprehensive knowledge of the secreted molecules of WJ-MSCs, through exploiting secretomic approaches, and the design of mechanistic studies aimed to isolate single factors to gain the same effect of using the cells are the next targets in this fascinating field of research. The second aspect which warrants further research is to define the intrinsic functional properties of the expanded UCB-HSPCs, and also to well clarify which sub-populations of HSPCs are generated at different culture conditions in the presence of MSCs. Only with a full knowledge of factors and pathways involved in the process of HSPCs expansion in vitro, optimal protocols can be established to further improve the existing clinical application.
References
Cohen, Y., & Nagler, A. (2004). Umbilical cord blood transplantation-how, when and for whom? Blood Reviews, 18(3), 167–179.
Mayani, H., & Lansdorp, P. M. (1998). Biology of human umbilical cord blood derived hematopoietic stem/progenitor cells. Stem Cells, 16, 153–165.
Kita, K., Lee, J. O., Finnerty, C. C., & Herndon (2011). Cord blood-derived hematopoietic stem/progenitor. Cells: Current challenges in Engraftment, Infection, and Ex vivo expansion. Stem cells International. doi:10.4061/2011/276193.
Zhang, Y., Chai, C., Jiang, X. S., Teoh, S. H., & Leong, K. W. (2006). Co-culture of umbilical cord blood CD34+ cells with human mesenchymal stem cells. Tissue Engineering, 12, 2161–2170.
Robinson, S. N., Simmons, P. J., Yang, H., Alousi, A. M., de Lima, J. M., & Shpall, E. J. (2011). Mesenchymal stem cells in ex vivo cord blood expansion. Best Practice & Research. Clinical Haematology, 24, 83–92.
Troyer, D. L., & Weiss, M. L. (2007). Concise review: Wharton’s jelly-derived cells are a primitive stromal cell population. Stem Cells, 26, 591–599.
Corrao, S., La Rocca, G., Lo Iacono, M., Corsello, T., Farina, F., & Anzalone, R. (2013). Umbilical cord revisited: from Wharton’s jelly myofibroblasts to mesenchymal stem cells. Histology and Histopathology, 28, 1235–1244.
Anzalone, R., Farina, F., Zummo, G., & La Rocca, G. (2011). Recent patents and advances on isolation and cellular therapy applications of mesenchymal stem cells from human umbilical cord Wharton’s jelly. Recent Patents on Regenerative Medicine, 1, 216–227.
D’Arena, G., Musto, P., Cascavilla, N., et al. (1996). Human umbilical cord blood: immunophenotypic Heterogeity of CD34 + hematopoietic progenitor cells. Hematologica, 81, 404–409.
Civin, C. I., & Gore, S. D. (1993). Antigenic analysis of hematopoiesis: a review. Journal of Hematotherapy, 2, 137–144.
Piacibello, W., Sanavio, F., & Garetto, L. (1997). Extensive amplification and self-renewal of human primitive hematopoietic stem cells from cord blood. Blood, 89(8), 2644–2653.
Chotinantakul, K., Prasajak, P., & Leeanansaksiri, W. (2013). Wnt1 accelerates an ex vivo expansion of human cord blood CD34(+)CD38(-) cells. Stem Cells International, 2013, 909812. doi:10.1155/2013/909812 .Epub 2013 Aug 20
Mosaad, Y. M. (2014). Hematopoietic stem cells: an overview. Transfusion and Apheresis Science, 51, 68–82.
Wynter, E. A., Emmerson, A. J. B., & Testa, N. G. (1999). Properties of peripheral blood and cord blood stem cells. Bailliere’s Clinical Hematology, 12, 1–17.
Leung, W., Ramirez, M., Novelli, E. M., et al. (1998). In vivo engraftment potential of clinical hematopoietic grafts. Journal of Investigative Medicine, 46(6), 303–311.
Lewis, I., & Verfaillie, C. M. (2000). Multi-lineage expansion potential of primitive hematopoietic progenitors. Superiority of umbilical cord blood compared to mobilized peripheral blood. Experimental Hematology, 28(9), 1087–1095.
Aldenhoven, M., & Kurtzberg, J. (2015). Cord blood is the optimal graft source for the treatment of pediatric patients with lysosomal storage diseases: clinical outcomes and future directions. Cytotherapy, 17(6), 765–774. doi:10.1016/j.jcyt.2015.03.609 .Epub 2015 Mar 31
Dominici, M., Le Blanc, K., Mueller, I., et al. (2006). Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy, 8, 315–317.
Huang, Y. C., Parolini, O., La Rocca, G., & Deng, L. (2012). Umbilical cord versus bone marrow-derived mesenchymal stromal cells. Stem Cells and Development, 21, 2900–2903.
La Rocca, G., Anzalone, R., Corrao, S., et al. (2009). Isolation and characterization of Oct-4+/HLA-G+ mesenchymal stem cells from human umbilical cord matrix: differentiation potential and detection of new markers. Histochemistry and Cell Biology, 131, 267–282.
Batsali, A. K., Kastrinaki, M. C., Papadaki, H. A., & Pontikoglou, C. (2013). Mesenchymal stem cells derived from Wharton’s jelly of the umbilical cord: biological properties and emerging clinical applications. Current Stem Cell Research & Therapy, 8, 144–155.
Anzalone, R., Lo Iacono, M., Loria, T., et al. (2011). Wharton’s jelly mesenchymal stem cells as candidates for beta cells regeneration: extending the differentiative and immunomodulatory benefits of adult mesenchymal stem cells for the treatment of type 1 diabetes. Stem Cell Reviews and Reports, 7, 342–363.
Lo Iacono, M., Anzalone, R., Corrao, S., et al. (2011). Perinatal and Wharton’s jelly derived mesenchymal stem cells in cartilage regenerative medicine and tissue engineering strategies. The Open Tissue Engineering and Regenerative Medicine Journal, 4, 72–81.
Corrao, S., La Rocca, G., Lo Iacono, M., et al. (2013). New frontiers in regenerative medicine in cardiology: the potential of Wharton’s jelly mesenchymal stem cells. Current Stem Cell Research & Therapy, 8, 39–45.
Anzalone, R., Farina, F., Zummo, G., & La Rocca, G. (2011). Recent patents and advances on isolation and cellular therapy applications of mesenchymal stem cells from human umbilical cord Wharton’s jelly. Recent Patents on Regenerative Medicine, 1, 216–227.
De Bruyn, C., Najar, M., Raicevic, G., et al. (2011). A rapid, simple, and reproducible method for the isolation of mesenchymal stromal cells from Wharton’s jelly without enzymatic treatment. Stem Cells and Development, 20, 547–557.
Anzalone, R., Lo Iacono, M., Corrao, S., et al. (2010). New emerging potentials for human Wharton’s jelly mesenchymal stem cells: immunological features and hepatocyte-like differentiative capacity. Stem Cells and Development, 19(4), 423–437.
Weiss, M. L., Medicetty, S., Bledsoe, A. R., et al. (2006). Human umbilical cord matrix stem cells: preliminary characterization and effect of transplantation in a rodent model of Parkinson’s disease. Stem Cells, 24, 781–792.
Anzalone, R., Corrao, S., Lo Iacono, M., et al. (2013). Isolation and characterization of CD276+/HLA-E+ human subendocardial mesenchymal stem cells from chronic heart failure patients: analysis of differentiative potential and immunomodulatory markers expression. Stem Cells and Development, 22, 1–17.
Karahuseyinoglu, S., Cinar, O., Kilic, E., et al. (2007). Biology of stem cells in human umbilical cord stroma: in situ and in vitro surveys. Stem Cells, 25, 319–331.
Tondreau, T., Lagneaux, L., Dejeneffe, M., et al. (2004). Bone marrow-derived mesenchymal stem cells already express specifi c neural proteins before any differentiation. Differentiation, 72, 319–326.
Hung, S. C., Chen, N. J., Li, H.-S., Ma, H.-L., & Lo, W.-H. (2002). Isolation and characterization of size-sieved stem cells from human bone marrow. Stem Cells, 20, 249–258.
Turnovcova, K., Ruzickova, K., Vanecek, V., Sykova, E., & Jendelova, P. (2009). Properties and growth of human bone marrow mesenchymal stromal cells cultivated in different media. Cytotherapy, 25, 1–12.
Karaoz, E., Aksoy, A., Ayhan, S., Sarıboyacı, A. E., Kaymaz, F., & Kasap, M. (2009). Characterization of mesenchymal stem cells from rat bone marrow: ultrastructural properties, differentiation potential and immunophenotypic markers. Histochemistry and Cell Biology, 132, 533–546.
Nilsson, S. K., Johnston, H. M., Whitty, G. A., et al. (2005). Osteopontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood, 106, 1232–1239.
Raio, L., Cromi, A., Ghezzi, F., et al. (2005). Hyaluronic content of wharton’s jelly in healthy and down syndrome foetuses. Matrix Biology, 2005(24), 166–174.
Li, Tian, and Wu, Y. (2001). Paracrine molecules of mesenchymal stem cells for hematopoietic stem cell niche. Bone marrow research, ID353878, 8 doi:10.1155/2011/353878.
Mishima, S., Nagai, A., & Abdullah, S. (2010). Effective ex vivo expansion of hematopoietic stem cells using osteoblast-differentiated mesenchymal stem cells is CXCL12 dependent. European Journal of Haematology, 84(6), 538–546.
Sugiyama, T., Kohara, H., Noda, M., & Nagasawa, T. (2006). Maintenance of hematopoietic stem cell pool by CXCL12-CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity, 25(6), 977–988.
Lu, L. L., Liu, Y. J., & Yang, S. G. (2006). Isolation and characterization of human umbilical cord mesenchymal stem cells with hematopoiesis-supportive function and other potentials. Haematologica, 91(8), 1017–1026.
Friedman, R., Betancur, M., Boissel, L., Tuncer, H., Cetrulo, C., Klingermann, H. (2007). Umbilical Cord mesenchymal Stem Cells: Adjuvants for Human Cell Transplantation, 13, 1477–1486.
Ke, Z., & Liu, Q. (2016). The clinical application of mesenchymal stromal cells in hematopoietic stem cell transplantation. Journal of Hematology & Oncology, 9, 46.
Alma, J., Nauta, W., & Fibbe, E. (2007). Immunomodulatory properties of mesenchymal stromal cells. Blood, 110, 3499–3506.
Aggarwal, S., & Pittenger, M. F. (2005). Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood, 105, 1815–1818.
Chan, C. K., Wu, K. H., Lee, Y. S., et al. (2012). The comparison of interleukin-6-associated immunosuppressive effect of human ESCs, fetal type-MSCs, and adult-type MSCs. Transplantation, 94, 132.
La Rocca, G., Corrao, S., Lo Iacono, M., Corsello, T., Farina, F., & Anzalone, R. (2012). Novel immunomodulatory markers expressed by human WJ-MSC: an updated review in regenerative and reparative medicine. The Open Tissue Engineering and Regenerative Medicine Journal, 5, 50–58.
Corrao, S., Campanella, C., Anzalone, R., et al. (2010). Human Hsp10 and early pregnancy factor (EPF) and their relationship and involvement in cancer and immunity: current knowledge and perspectives. Life Sciences, 86, 145–152.
Corrao, S., Anzalone, R., Lo Iacono, M., et al. (2014). Hsp10 nuclear localization and changes in lung cells response to cigarette smoke suggest novel roles for this chaperonin. Open Biology, 4(10). doi:10.1098/rsob.140125.
Fanchin, R., Galiot, V., Rouas-Freiss, N., Frydman, R., & Carosella, E. D. (2009). Implication of HLA-G in human embryo implantation. Human Immunology, 68, 259–263.
Weiss, M. L., Anderson, C., Medicetty, S., et al. (2008). Immune properties of human umbilical cord Wharton’s jelly-derived cell. Stem Cells, 26, 2865–2874.
Valencic, E., Piscianz, E., Andolina, A., Ventura, A., & Tommasini, A. (2010). The immunosuppressive effect of Wharton’s jelly sromal cells depends on the timing of their licensing and on lymphocyte activation. Cytotherapy, 12, 154–160.
Tipnis, S., Viswanathan, C., & Majumdar, A. S. (2010). Immunosuppressive properties of human umbilical cord derived mesenchymal stem cells: role of B7-H1 and IDO. Immunology and Cell Biology, 88, 795–806.
Gluckman, E. (2000). Current status of umbilical cord blood hematopoietic stem cell transplantation. Experimental Hematology, 28, 1197–1205.
Broxmeyer, H. E. (2010). Umbilical cord transplantation: epilogue. Seminars in Hematology, 3, 272–283.
Ballen, K., Gluckman, E., & Broxmeyer, H. E. (2013). Umbilical cord blood transplantation: the first 25 years and beyond. Blood, 122, 491–498.
Gluckman, E., Rocha, V., Arcese, W., et al. (2004). Factors associated with outcomes of unrelated cord blood transplant: guidelines for donor choice. Experimental Hematology, 32(4), 397–407.
Brown, J., & Boussiotis, V. A. (2009). Umbilical cord blood transplantation: basic biology and clinical challenges to immune reconstitution. Clinical Immunology 2008, 127(3), 286–297. doi:10.1016/j.clim.2008.02.008.
Gluckman, E., Rocha, V., Boyer-Chammard, A., et al. (1997). Outcome of cord-blood transplantation from related and unrelated donors. Eurocord transplant group and the European blood and marrow transplantation group. New England Journal of Medicine, 337, 373–381.
Norkin, M, Lazarus, H.M., Wingard, J.R. (2013). Umbilical cord blood graft enhancement strategies: has the time come to move these into the clinic?. Bone Marrow Transplantation 48, 884–889.
Sideri, A., Neokleous, N., De La Brunet Grange, P., et al. (2011). An overview of the progress on double umbilical cord blood transplantation. Haematologica, 96, 1213–1220.
Barker, J. N., Weisdorf, D. J., De For, T. E., et al. (2005). Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood, 105, 1343–1347.
Dahlberg, A., Delaney, C., & Bernstein, I. D. (2011). Ex vivo expansion of human hematopoietic stem and progenitor cells. Blood, 117, 6083–6090.
Bari, S., Seah, K. K., Poon, Z., et al. (2015). Expansion and homing of umbilical cord blood hematopoietic stem and progenitor cells for clinical transplantation. Biology of Blood and Marrow Transplantation, 21, 1008–1019.
Shpall, E. J., Quinones, R., Giller, R., et al. (2002). Transplantation of ex vivo expanded cord blood. Biology of Blood and Marrow Transplantation, 8(7), 368–376.
de Lima, M., Mc Mannis J.D., Saliba, R., et al. (2008). Double cord blood transplantation (CBT) with and without ex-vivo expansion (EXP): a randomized, controlled study [abstract]. Blood, 112 Abstract 154.
Jaroscak, J., Goltry, K., Smith, A., et al. (2003). Augmentation of umbilical cord blood (UCB) transplantation with ex vivo-expanded UCB cells: results of a phase I trial using the Aastrom Replicell system. Blood, 101(12), 5061–5067.
Zhang, C. C., Kaba, M., Ge, G., et al. (2006). Angiopoietin-like proteins stimulate ex vivo expansion of hematopoietic stem cells. Nature Medicine, 12, 240–245.
Himburg, H. A., Muramoto, G. G., Daher, P., et al. (2010). Pleiotrophin regulates the expansion and re generation of hematopoietic stem cells. Nature Medicine, 16, 475–482.
Celebi, B., Mantovan, D., & Pineault, N. (2012). Insulin-like growth factor binding protein-2 and neurotrophin 3 synergize together to promote the expansion of hematopoietic cells ex vivo. Cytokine, 58, 327–331.
Ventura, F. M. S., Labude, N., Walenda, G., et al. (2013). Ex vivo expansion of cord blood-cd34(+) cells using IGFBP2 and Angptl-5 impairs short-term lymphoid repopulation in vivo. Journal of Tissue Engineering and Regenerative Medicine, 7, 944–954.
Zhang, Y., & Gao, Y. (2016). Novel chemical attempts at ex vivo hematopoietic stem cell expansion. International Journal of Hematology, 103(5), 519–529. doi:10.1007/s12185-016-1962-x.
De Lima, M., McMannis, J., Gee, A., et al. (2008). Transplantation of ex vivo expanded cord blood cells using the copper chelator tetraethylene-pentamine: a phase I/II clinical trial. Bone Marrow Transplantation, 41, 771–778.
Boitano, A. E., Wang, J., Romeo, R., et al. (2010). Aryl hydrocarbon receptor antagonists promote the expression of human hematopoietic stem cells. Science, 329, 1345–1348.
Peled, T., Shoham, H., Aschengrau, D., et al. (2012). Nicotinamide, a SRT1 inhibitor, inhibits differentiation and facilitates expansion of hematopoietic progenitor cells with enhanced bone marrow homing and engraftment. Experimental Hematology, 40(342–355), e1.
Fares, I., ChagraOUI, J., Gareau, S., et al. (2014). Cord blood expansion. Pyrimidoindole derivatives are agonists of human hematopoietic stem cell renewal. Science, 345, 1509–1512.
Bigas, A., & Espinosa, L. (2012). Hematopoietic stem cells: to be or notch to be. Blood, 119, 3226–3235.
Mayani, H. (2010). Notch signaling: from stem cell expansion to improving cord blood transplantation. Expert Review of Hematology, 3(4), 401–404.
Fajardo-Orduna, G. R., Mayani, H., & Montesinos, J. J. (2015). Hematopoietic support capacity of mesenchymal stem cells: biology and clinical potential. Archives of Medical Research, 46, 589–596.
Wagner, W., Weina, F., Roderburga, C., et al. (2007). Adhesion of hematopoietic progenitor cells to human mesenchymal stem cells as a model for cell-to-cell interaction. Experimental Hematology, 35, 314–325.
Oh, I. H., & Kwon, K. R. (2010). Concise review: multiple niches for hematopoietic stem cell regulation. Stem Cells, 28(7), 1243–1249.
Morrison, S. J., & Scadden, D. T. (2014). The bone marrow niche for hematopoietic stem cells. Nature, 505, 327–334.
Wilson, A., & Trumpp, A. (2006). Bone marrow hematopoietic stem cells niches. Nature Reviews. Immunology, 6, 93–106.
Zhang, J., & Li, L. (2008). Stem cell niche: microenvironment and beyond. Journal of Biological Chemistry, 283(15), 9499–9503.
Ehninger, A., & Trump, A. (2011). The bone marrow stem cell niche grows up: mesenchymal stem cells and macrophages move in. The Journal of Experimental Medicine, 208, 421–428.
Kohler, T., Plettig, R., Wetzstein, W., et al. (1999). Defining optimum conditions for the ex vivo expansion of human umbilical cord blood cells. Influences of progenitor enrichment, interference with feeder layers, early acting cytokines and agitation of culture vessels. Stem Cells, 17, 19–24.
Wagner, W., Roderburg, C., Wein, F., et al. (2007). Molecular and secretary profiles of human mesenchymal stromal cells and their abilities to maintain primitive hematopoietic progenitors. Stem Cells, 25, 2638–2647.
Dexter, T. M., Allen, T. D., & Lajtha, L. G. (1977). Conditions controlling the proliferation of haemopoietic stem cells in vitro. Journal of Cellular Physiology, 91, 335–344.
Kadereit, S., Deeds, L. S., Haynesworth, S. E., et al. (2002). Expansion of LTC-ICs and maintenance of p 21 and BCL-2 expression in cord blood CD34(þ)/CD38(−) early progenitors cultured over human MSCs as a feeder layer. Stem Cells, 20, 573–582.
Yamaguchi, M., Hirayama, F., Murahashi, H., et al. (2002). Ex vivo expansion of human UC blood primitive hematopoietic progenitors and transplantable stem cells using human primary BM stromal cells and human AB serum. Cytotherapy, 4, 109–118.
Alakel, N., Jing, D., Muller, K., Borhauser, M., Ehninger, G., & Ordemann, R. (2009). Direct contact with mesenchymal stromal cells affects migratory behaviour and gene expression profile of CD133+ hematopoietic stem cells during ex vivo expansion. Experimental Hematology, 37, 504–513.
Fong, C. Y., Gauthaman, S., Cheyyatraivendran, S., Lin, H. D., Biswas, A., & Bongso, A. (2012). Human umbilical cord Wharton’s jelly stem cells and its conditioned medium support hematopoietic stem cell expansion ex vivo. Journal of Cellular Biochemistry, 113, 658–668.
de Haan, G., Ploemache, R., The Cobblestone-Area-Forming Cell Assay. Hematopoietic Stem Cell Protocols, Volume 63 of the series Methods in Molecular Medicine pp 143–151.
Majumdar, M. K., Thiede, M. A., & Haynesworth, S. E. (2000). Human marrow-derived mesenchymal stem cells (MSCs) express hematopoietic cytokines and support long-term hematopoiesis when differentiated toward stromal and osteogenic lineages. Hematotherapy Stem Cell Research, 9, 841–848.
Itkin, T., & Lapidot, T. (2001). SDF-1 keeps HSC quiescent at home. Blood, 117, 373–374.
Bennaceur-Griscelli, A., Pondarre, C., Schiavon, V., Vainchenker, W., & Coulombel, L. (2001). Stromal cells retard the differentiation of CdD4(+)CD38(low/neg) human primitive progenitors exposed to cytokines independent of their mitotic history. Blood, 97, 435–441.
Dao, M. A., Pepper, K. A., & Nolta, J. A. (1997). Long-term cytokine production from engineered primary human stromal cells influences human hematopoiesis in an in vivo xenograft model. Stem Cells, 78, 110–117.
Gottschling, S., Saffrich, R., Seckinger, A., et al. (2007). Human mesenchymal stromal cells regulate initial self-renewing division of hematopoietic progenitor cells by beta-1-integrin dependent mechanism. Stem Cells, 25, 798–806.
Freund, D., Bauer, N., Boxberger, S., et al. (2006). Polarization of hematopoietic progenitors during contact with multipotent mesenchymal stromal cells: effects on proliferation and clonogenecity. Stem Cells and Development, 15(6), 815–829.
Breems, D. A., Blokland, E. A., Siebel, K. E., et al. (1998). Stroma contact prevents loss of hematopoietic stem cell quality during ex vivo expansion of CD34+ mobilized peripheral blood stem cells. Blood, 91(1), 111–117.
Lewis, I. D., Almeida-Porada, G., Du, J., et al. (2001). Umbilical cord blood cells capable of engrafting in primary, secondary, and tertiary, xenogenic hosts are preserved after ex vivo culture in a noncontact system. Blood, 97(11), 3441–3449.
Verfaillie, C. M. (1992). Direct contact between human primitive hematopoietic progenitors and bone marrow stroma is not required for long-term in vitro hematopoiesis. Blood, 79(11), 2821–2826.
da Silva, C. L., Goncalves, R., Cranpnell, K. B., et al. (2005). A human stromal-based serum-free system supports ex vivo expansion/mantainance of bone maroow and cord blood hematopoietic stem/progenitor cells. Experimental Hematology, 33(7), 828–835.
Flores-Guzman, P., Flores-Figueroa, E., Montesinos, J. J., et al. (2009). Individual and combined effects of mesenchymal stromal cells and recombinant stimulatory cytokines on the in vitro growth of primitive hematopoietic cells from human umbilical cord blood. Cytotherapy, 11, 886–896.
Rodriguez-Pardo, V. M., & Vernot, J. P. (2013). Mesenchymal stem cells promote a primitive phenotype CD34 + c-kit + in human cord blood-derived hematopoietic stem cells during ex vivo expansion. Cellular & Molecular Biology Letters, 18, 11–33. doi:10.2478/s11658-012-0036.
McNiece, I., Harrington, J., Turney, J., Kellner, J., & Shpall, E. J. (2004). Ex vivo expansion of cord blood mononuclear cells on mesenchymal stem cells. Cytotherapy, 6(4), 311–317.
Walenda, T., Bork, S., Horn, et al. (2010). Co-culture with mesenchymal stromal cells increases proliferation and maintenance of haematopoietic progenitor cells. Journal of Cellular and Molecular Medicine, 14, 337–350.
Koh, S. H., Choi, H. S., Park, E. S., Kang, H. J., Ahn, H. S., & Shin, H. Y. (2005). Co-culture of human Cd34+ cells with mesenchymal stem cells increases the survival of Cd34+ cells against the 5-aza-deoxycytidine or trichostatin A-induced cell death. Biochemical and Biophysical Research Communications, 329(3), 1039–1045.
Khoury, M., Drake, A., Chen, Q., et al. (2011). Mesenchymal stem cells secreting angiopoietin-like-5 support efficient expansion of human hematopoietic stem cells without compromising their repopulating potential. Stem Cells and Development, 20, 1371–1381.
Kawano, Y., Kobune, M., Yamaguchi, M., et al. (2003). Ex vivo expansion of human umbilical cord hematopoietic progenitor cells using a coculture system with human telomerase catayitic subunit (hTERT)-transfected human stromal cells. Blood, 101, 532–540.
Leisten, I., Kramann, R., Ventura Ferreira, M. S., Bovi, et al. (2012). 3D co-culture of hematopoietic stem and progenitor cells and mesenchymal stem cells in collagen scaffold as a model of the hematopoietic niche. Biomaterials, 33, 1736–1747.
Ferreira, M. S., Jahnen-Dechenet, W., Labude, N., et al. (2012). Cord blood-hematopoietic stem cell expansion in 3D fibrin scaffolds with stromal support. Biomaterials, 33(29), 6987–6997.
Delalat, B., Pourfathollah, A. A., Soleimani, M., et al. (2009). Isolation and ex vivo expansion of human umbilical cord blood-derived Cd34+ stem cells and their cotransplantation with or without mesenchymal stem cells. Hematology, 14, 125–132.
Han, J. Y., Goh, R. H., Seo, S. Y., et al. (2007). Cotransplantation of cord blood hematopoietic stem cells and culture expanded and GM-CSF−/SCF-transfected mesenchymal stem cells in SCID mice. Journal of Korean Medical Science, 22, 242–247.
de Lima, M., McNiece, I., Robinson, S. N., et al. (2012). Cord-blood engraftment with ex vivo mesenchymal-cell culture. New England Journal of Medicine, 367(24), 2305–2315.
Saragusar, R., Lickorish, D., Baksh, D., Hosseini, M. M., & Davies, J. E. (2005). Human umbilical cord perivascular (HUCPV) cells: a source of mesenchymal progenitors. Stem Cells, 23, 220–229.
Bakhshi, T., Zabriskie, R. C., Bodie, S., et al. (2008). Mesenchymal stem cells from the Wharton’s jelly of umbilical cord segments provide stromal support for the maintenance of cord blood hematopoietic stem cells during long-term ex vivo culture. Transfusion, 48, 2638–2644.
Magin, A. S., Korfer, N. R., Pasrtenheimer, H., Lange, C., Zander, A., & Noll, T. (2009). Primary cells as feeder cells for coculture expansion of human hematopoietic stem cells from umbilical cord-blood a comparative study. Stem Cells and Development, 18(1). doi:10.1089/scd.2007.0273.
Tipnis, S., & Viswanathan, C. (2010). Umbilical cord matrix derived mesenchymal stem cells can change the cord blood transplant scenario. International Journal of Stem cells, 3(2), 103–118.
Milazzo, L., Vulcano, F., Barca, A., et al. (2014). Cord blood CD34+ cells expanded on Wharton’s jelly multipotent mesenchymal stromal cells improve the hematopoietic engraftment in NOD/SCID mice. European Journal of Haematology, 93(5), 384–391.
Mieog, J. S., de Kruijf, E. M., Bastiaannet, E., et al. (2012). Age determines the prognostic role of the cancer stem cell marker aldehyde dehydrogenase-1 in breast cancer. BMC Cancer, 12(42).
Van der Garde, M., van Pel, M., Millan, R. J. E., et al. (2015). Direct comparison of Wharton’s jelly and bone marrow-derived mesenchymal stromal cells to enhance engraftment of cord blood CD34+ transplants. Stem Cells and Development, 24(22). doi:10.1089/scd.2015.0138.
van der Garde, M., van Hensbergen, Y., Brand, A., Slot, M. C., de Graaf-Dijkstra, A., Mulder, A., Watt, S. M., & Zwaginga, J. J. (2015). Thrombopoietin treatment of one graft in a double cord blood transplant provides early platelet recovery while contributing to long-term engraftment in NSG mice. Stem Cells and Development, 24, 67–76.
van Hensbergen, Y., Schipper, L. F., Brand, A., Slot, M. C., Welling, M., Nauta, A. J., & Fibbe, W. E. (2006). Ex vivo culture of human CD34+ cord blood cells with thrombopoietin (TPO) accelerates platelet engraftment in a NOD/SCID mouse model. Experimental Hematology, 34, 943–950.
Klein, C., Strobel, J., Zingsem, J. et al. (2013). Ex vivo expansion of Hematopoietic Stem-and Progenitor Cells from Cord Blood in co-culture with Mesenchymal stroma cells from Amnion, Chorion, Wharton’s jelly, amniotic Fluid, Cord Blood, and Bone Marrow. Tissue Engineering Part. A, 19 (23and 24), 2577–2585.
Huang, G. P., Pan, Z. J., & Jia, B. B. (2007). Ex vivo expansion and transplantation of hematopoietic stem/progenitor cells supported by mesenchymal stem cells from human umbilical cord blood. Cell Transplantation, 16, 579.
Kedekar, D., Kale, V., & Limaye, L. (2015). Differential ability of MSCs isolated from placenta and cord as feeders for supporting ex vivo expansion of umbilical cord blood derived CD34+ cells. Stem Cell Research & Therapy, 6, 201.
Mayani, H., Little, M. T., Dragowska, W., Thornbury, G., & Lansdorp, P. M. (1995). Differential effects of the hematopoietic inhibitors MIP-1 alpha, TGF-beta, and TNF-alpha on cytokine-induced proliferation of subpopulations of CD34+ cells purified from cord blood and fetal liver. Experimental Hematology, 5, 422–427.
Wu, K. H., Sheu, J. N., Wu, H. P., et al. (2013). Co-transplantation of umbilical cord- derived mesenchymal stem cells promote hematopoietic engraftment in cord blood transplantation: a pilot study. Clinical and Translation Research, 95(5), 773–777.
Wu, K. H., Tsai, C., Wu, H. P., Sieber, M., Peng, C. T., & Chao, Y. H. (2013). Human application of ex-vivo expanded umbilical cord-derived mesenchymal stem cells: enhance hematopoiesis after cord blood transplantation. Cell Transplantation. doi:10.3727/096368913X663523.
Wu, Y. M., Wang, Z. H., Cao, Y. B., et al. (2013). Co-transplantation of haploidentical hematopoietic and umbilical cord mesenchymal stem cells with a myeloablative regimen for refractory/relapsed hematologic malignancy. Annals of Hematology. doi:10.1007/s00277-013--1831-0.
Chao, Y. H., Tsai, C., Peng, C. T., et al. (2011). Cotransplantation of umbilical cord MSCs to enhance engraftment of hematopoietic stem cells in patients with severe aplastic anemia. Bone Marrow Transplantation, 46(10), 1391–1392.
Wu, Y.C., Yongbin, L., Xiaohong et al. (2014). Cotransplantation of haploidentical hematopoietic and umbilical cord mesenchymal stem cells for severe aplastic anemia: successful engraftment and mild GVHD. Stem Cell Research, 12, 132–138.
Holmberg, L. A., Seidel, K., Leisenring, W., & Torok-Storb, B. (1994). Aplastic anemia: analysis of stromal cell function in long-term marrow cultures. Blood, 84, 3685–3690.
Chao, Y. H., Peng, C. T., Harn, H. J., Chan, C. K., & Wu, K. H. (2010). Poor potential of proliferation and differentiation in bone marrow mesenchymal stem cells derived from children with severe aplastic anemia. Annals of Hematology, 89, 715–723.
Arai, Y., Aoki, K., Takeda, J., et al. (2015). Clinical significance of high-dose cytarabine added to cyclophosphamide/total-body irradiation in bone marrow or peripheral blood stem cell transplantation for myeloid malignancy. Journal of Hematology & Oncology, 8, 102.
Chang, Y. J., Zhao, X. Y., Xu, L. P., et al. (2015). Donor-specific anti-human leukocyte antigen antibodies were associated with primary graft failure after unmanipulated haploidentical blood and marrow transplantation: a prospective study with randomly assigned training and validation sets. Journal of Hematology & Oncology, 8, 84.
Dazzi, F., Ramasamy, R., Glennie, S., Jones, S. P., & Roberts, I. (2006). The role of mesenchymal stem cells in haematopoiesis. Blood Reviews, 20(3), 161–171.
Zhao, K., & Liu, Q. (2016). The clinical application of mesenchymal stromal cells in hematopoietic stem cell transplantation. Journal of Hematology & Oncology, 9, 46.
Acknowledgements
This work was mainly supported by a grant from PO FESR 4.1.1.1 RIMEDRI (B75f1200150004), funds to SA via the Franco and Piera Cutino Foundation, Palermo. GLR and RA were supported by funding from the IEMEST. The funders had no role in study design, data collections and analysis, decision to publish, or preparation of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Giampiero La Rocca is member of the Scientific Board of Auxocell laboratories, Inc. The other authors declare no potential conflicts of interest.
Additional information
Melania Lo Iacono and Rita Anzalone contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Lo Iacono, M., Anzalone, R., La Rocca, G. et al. Wharton’s Jelly Mesenchymal Stromal Cells as a Feeder Layer for the Ex Vivo Expansion of Hematopoietic Stem and Progenitor Cells: a Review. Stem Cell Rev and Rep 13, 35–49 (2017). https://doi.org/10.1007/s12015-016-9702-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-016-9702-4