Abstract
Ovarian cancer is considered the most lethal among all gynecological malignancies due to its early metastatic dissemination, extensive spread, and malignant ascites. The current standard of care for advanced ovarian cancer involves a combination of cytoreductive surgery and chemotherapy utilizing platinum-based and taxane-based agents. Although initial treatment yields clinical remission in 70–80% of patients, the majority eventually develop treatment resistance and tumor recurrence. A growing body of evidence indicates the existence of cancer stem cells within diverse solid tumors, including ovarian cancer, which function as a subpopulation to propel tumor growth and disease advancement by means of drug resistance, recurrence, and metastasis. The presence of ovarian cancer stem cells is widely considered to be a significant contributor to the unfavorable clinical outcomes observed in patients with ovarian cancer, as they play a crucial role in mediating chemotherapy resistance, recurrence, and metastasis. Ovarian cancer stem cells possess the capacity to reassemble within the entirety of the tumor following conventional treatment, thereby instigating the recurrence of ovarian cancer and inducing resistance to treatment. Consequently, the creation of therapeutic approaches aimed at eliminating ovarian cancer stem cells holds great potential for the management of ovarian cancer. These cells are regarded as one of the most auspicious targets and mechanisms for the treatment of ovarian cancer. There is a pressing need for a comprehensive comprehension of the fundamental mechanisms of ovarian cancer’s recurrence, metastasis, and drug resistance, alongside the development of effective strategies to overcome chemoresistance, metastasis, and recurrence. The implementation of cancer stem cell therapies may potentially augment the tumor cells’ sensitivity to existing chemotherapy protocols, thereby mitigating the risks of tumor metastasis and recurrence, and ultimately improving the survival rates of ovarian cancer patients.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is typically classified into three primary types based on cell origin: epithelial cancer (90%), sex cord-stromal cancer (7%), and germ cell cancer (3–7%) [1]. Epithelial ovarian cancer is the leading cause of death among women and has the highest mortality rate of all gynecological malignancies [2]. It ranks fifth globally in cancer-related deaths among women [3]. High-grade serous ovarian carcinoma (HGSOv) is the most prevalent form of epithelial ovarian cancer, accounting for 60–80% of cases [4]. The absence of precise detection techniques during the initial stages of ovarian Cancer results in an estimated 75% of patients being diagnosed at stage III or IV. The corresponding survival rates for patients with stage III and IV disease are 39% and 17%, respectively. At the time of diagnosis, over 80% of ovarian cancer patients exhibit peritoneal metastasis and significant ascites, which accounts for the demise of 90% of ovarian cancer patients [5,6,7]. Research findings indicate that ovarian cancer presents a five-year overall survival rate of 40%, while epithelial ovarian cancer exhibits a survival rate in close proximity to 30% [8, 9]. The life expectancy of individuals diagnosed with this condition ranges from 6 to 18 months [10]. The resistance of chemotherapy and the consequent recurrence of tumors render ovarian cancer the most fatal gynecologic malignancy [11].
Undoubtedly, surgical resection and platinum or taxane chemotherapy have proven to be efficacious treatments for the majority of patients. As per the literature, nearly 80% of patients exhibit success with these treatments [12], while approximately 70% of patients experience end-stage disease, recurrent disease, and chemotherapy resistance [13]. Furthermore, conventional chemotherapy, such as platinum and paclitaxel, can enhance short-term survival rates. Chemotherapy resistance may ensue following multiple treatment cycles, as evidenced by several studies that have identified various mechanisms underlying this phenomenon, including inadequate intracellular drug accumulation, heightened activation of antioxidant and anti-apoptotic signals, and enhanced DNA repair efficiency [14]. The emergence of chemotherapy resistance and disease recurrence can significantly impede long-term survival outcomes [15, 16]. Over the past four decades, there has been minimal progress in the long-term survival rates of patients diagnosed with advanced ovarian cancer [17]. The decision to employ multiple chemotherapeutic agents with varying biological mechanisms, either in combination or as monotherapy, in the treatment of recurrent ovarian cancer is left to the discretion of the clinician and is dependent on the patient’s systemic therapy and platinum-free interval [17]. It is crucial to acknowledge, however, that despite treatment, recurrent ovarian cancer remains incurable [18]. Several genetic abnormalities, such as P53 and BRCA1/2 mutations, RB1 and NF1 inhibition, and MDR1 overexpression, are implicated in the development of chemotherapy resistance in ovarian cancer. To overcome this challenge, various platinum- and paclitaxel-free treatments have been developed, including VEGF inhibitors and PARP inhibitors, which have demonstrated improved overall survival in ovarian cancer patients. However, their use is constrained by their high costs and toxic side effects. Despite the development of several treatment options, ovarian cancer remains associated with a high recurrence rate. Despite a decade of concerted efforts to develop novel treatment strategies for ovarian cancer, there has been no significant improvement in long-term clinical outcomes [19]. Furthermore, approximately 70–75% of patients who undergo optimal treatment will experience tumor recurrence, and the survival rate for those with recurrent ovarian cancer is poor due to increased resistance to conventional treatment methods [20]. The cumulative toxic effects of chemotherapy, cross-resistance to chemotherapy, and the diminished quality of life experienced by ovarian cancer patients represent significant clinical challenges.
Cancer stem cells are a distinct subset of cells present within tumors that possess the capacity for self-renewal and the ability to generate heterogeneous cancer cell lineages [21, 22]. Stem cells, contingent upon the tumor microenvironment, can undergo division and produce daughter cells that maintain the full differentiation potential and self-renewal capacity of their parent stem cells. Upon culturing under specific conditions, these daughter cells can further differentiate. Recent research indicates that cancer stem cells, which possess the capacity to differentiate into all cell types present in particular tumors, are prevalent in diverse solid tumors and exert a pivotal influence on tumorigenesis, progression, metastasis, recurrence, angiogenesis, and drug resistance. Notably, ovarian cancer is characterized by a significant subpopulation of cancer stem cells within the tumor tissue, which may contribute to the high incidence of metastasis and recurrence [23,24,25,26,27,28,29,30,31,32]. Research has indicated that cancer stem cells exhibit greater resistance to conventional chemotherapy regimens and possess the capacity to initiate tumorigenesis, thereby constituting a significant factor in disease recurrence. The prevailing therapeutic approaches primarily target differentiated and rapidly proliferating tumor cells, leaving behind quiescent tumor stem cells that subsequently lead to tumor recurrence and metastasis. Furthermore, recent investigations have established that cancer stem cells display a high degree of resistance to established chemotherapy and radiotherapy, which represents a major contributor to the failure of cancer treatment [33]. The inability to eradicate cancer stem cells effectively is a significant contributing factor to the recurrence of ovarian cancer following chemotherapy, as evidenced by multiple sources [34,35,36]. These cells are typically in the G0 phase of the cell cycle and possess elevated levels of telomerase activity, DNA repair proficiency, and anti-apoptotic activity, enabling them to evade the cytotoxic effects of chemotherapy. Consequently, novel therapeutic strategies aimed at inhibiting cancer stem cells hold promise for achieving comprehensive suppression of tumor growth, metastasis, drug resistance, and recurrence. In order to address the constraints of ovarian cancer treatment, novel therapeutic strategies are required to impede the emergence of relapsing and chemotherapy-resistant neoplasms by selectively targeting cancer stem cells. This approach holds promise for extending the survival of individuals afflicted with ovarian cancer(refer to Fig. 1).
While traditional chemotherapy can partially reduce tumor cells, it has limited efficacy against cancer stem cells. During treatment, the continuous production of new tumor cells by cancer stem cells poses a challenge to complete tumor eradication. The elimination of cancer stem cells is therefore crucial in preventing the generation of new tumor cells and gradual tumor regression. Combining both treatment modalities can yield a significant reduction in tumor volume during the early stages of treatment and improve patient prognosis
Cancer Stem Cells
Basic Concepts of Cancer Stem Cells
Cancer stem cells (CSCs), also referred to as tumor-initiating cells (TICs), are a limited population of tumor cells that exhibit stem-like characteristics within neoplasms. These cells possess the capacity for self-renewal and differentiation, enabling them to sustain the hierarchical organization of the tumor [37]. CSCs have been detected and isolated in various tumors, including ovarian cancer [37], breast cancer [38], pancreatic cancer [39], colon cancer [40], and acute myeloid leukemia [41]. This particular subset of stem cells sustains the progression and maturation of tumor cells [42], and possesses inherent resistance to therapeutic measures targeting rapidly proliferating cells [43,44,45,46].
The hypothesis of cancer stem cells suggests that tumors exhibit a hierarchical organization, wherein subpopulations of cancer cells possess self-replicating properties. Additionally, this population, which is infrequent in tumor tissue, obtains or maintains stem-like characteristics, such as the capacity to produce differentiated daughter cells, resistance to drugs, and inherent or acquired DNA repair capability [47, 48]. These features collectively contribute to the advancement, preservation, or recurrence of the disease [49,50,51]. The theory of cancer stem cells has recently integrated the notion of plasticity, whereby these particular cellular subsets possess the capacity to undergo dedifferentiation in either direction or differentiate into a spectrum of stem-like characteristics when exposed to environmental stressors [29, 52,53,54].
Isolation and Enrichment of Cancer Stem Cells and Model Establishment
In 2005, Bapat et al. initially isolated ovarian cancer stem cells from the ascites of a patient with advanced ovarian cancer [55]. Subsequent investigations employed varying experimental techniques and selected distinct tumor markers to isolate cancer stem cells from ovarian tumors or ascites specimens. These studies revealed that between 0.25% and 12% of cells in tumor tissues exhibit cancer stem cell properties [56, 57]. Despite their minority status within the overall tumor tissue, these cells exert a dominant influence on the development and progression of ovarian cancer.
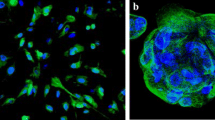
In recent times, various groups have endeavored to establish novel models of human cancer stem cells [58, 59]. Presently, the process of enrichment involves the collection of cells that express markers of tumor stem cells [60, 61] or relies on the assessment of aldehyde dehydrogenase (ALDH) activity [62]. Successful identification and isolation of ovarian cancer stem cells have been achieved through the utilization of cell surface markers such as CD44, CD117, and CD133. The identification of cancer stem cells has been widely facilitated by the assessment of ALDH1 activity. Cells that exhibit high levels of ALDH1 expression can be identified through the ALDEFLUOR assay and isolated through the use of ALDH1 antibody [63]. Currently, the isolation of ovarian cancer stem cells predominantly relies on the utilization of CD44, CD133, CD24, CD117 (c-Kit), and ALDH 1A1 markers, often in combination [64,65,66,67,68,69]. Tumor spheroid formation is a frequently employed technique in cancer stem cell culture [70, 71]. A viable method for enriching cancer stem cells involves the utilization of transformed ovarian cancer cell lines that generate tumor spheres or undergo epithelial-mesenchymal transition (EMT) [72]. These cell lines express alternative cancer stem cell markers and exhibit potential tumorigenic properties in vivo. This model has proven to be instrumental in identifying compounds that selectively target cancer stem cells [73].
Ovarian Cancer Stem Cell Markers
By identifying predictive biomarkers for ovarian cancer, personalized prediction, prevention, and precision medicine can be achieved, ultimately leading to improved survival rates for patients with invasive ovarian cancer. While biomarkers such as carbohydrate antigen 125 (CA125), human epididymis protein 4 (HE4), breast cancer 1 (BRCA1), and human chorionic gonadotropin (HCG) have been utilized in the diagnosis of ovarian cancer, their effectiveness as common biomarkers remains suboptimal [74]. Several omics techniques, such as transcriptomics and proteomics, have been employed to expedite the implementation of predictive, preventive, and personalized medicine (PPPM), thereby enhancing the precision of efficacy forecasting [75,76,77].
The identification of ovarian cancer stem cells is based on the expression of certain molecular markers. Over the years, several biomarkers have been discovered that are specifically or co-expressed in these cells, and their distinct roles in tumorigenesis have been extensively investigated. The overexpression of biomarkers such as CD44, CD133, CD117, LGR5, or ALDH has been used to identify cancer stem cells [66, 78,79,80]. The identification of ovarian cancer stem cell characteristics, including the quantification of cancer stem cell population [37] and the evaluation of CD44 expression [81], has been suggested as a means of predicting disease progression in ovarian cancer and facilitating the selection of appropriate treatment strategies.
Epithelial ovarian cancer has been found to possess over 10 cancer stem cell markers, such as side population (SP), CD133, ALDH1/2, LY6A, LGR5, EpCAM, CD133, CD44, CD34, CD24, CD117, MyD88, and CDH1. Research has demonstrated that CD133 can sustain the functional characteristics and tumorigenesis of ovarian cancer stem cells by stimulating cell survival signaling pathways, thus rendering it a promising candidate for targeted therapy aimed at ovarian cancer stem cells [82].The cell surface markers CD105, CD44, and CD106 exhibit potential as cancer stem cell-related markers, prognostic indicators, and therapeutic targets for ovarian cancer, as suggested by previous research [83].
Ovarian Cancer Stem Cell-related Signaling Pathways and Key Transcription Factors
Research has demonstrated that the dynamic interplay among cancer stem cells, tumor cells, and their microenvironment triggers distinct pathways that facilitate the proliferation and advancement of tumor cells. Certain pathways are responsible for conferring stemness upon tumor cells. The identification of the cellular pathways implicated in the interplay of genes involved in these mechanisms is crucial for advancing our comprehension of the molecular underpinnings of cancer stem cells and their association with tumor cells.
Research has demonstrated that the signaling pathways of Wnt, SONIC Hedgehog (SHH), NOTCH, PI3K/PTEN, MAPK, and NF-κB are associated with epithelial ovarian cancer stem cells [82, 84]. Furthermore, aberrant signaling pathways in cancer stem cells encompass Hedgehog, Notch, Wnt/β-catenin pathways, PI3K/AKT, TGF-β, EGFR, JAK/STAT, NF-κB, and other oncogenic cascade pathways [34]. Recent research has indicated that cellular signaling pathways, including Notch, Sonic Hedgehog (SHH), Wnt/β-catenin, PTEN, TGF-β, and Bmi-1, which are crucial for stem cell self-renewal, also play a role in regulating cancer stem cell maintenance [85, 86]. Additionally, several transcription factors, such as NANOG, HOXB7, MITF, FOXM1, and c-JUN, have been identified as key regulators. Furthermore, certain transcriptional regulators, including Myc, β-Catenin, NFκB, STAT, RUNX, and NOTCH/CSL, have emerged as potential therapeutic targets for cancer stem cells [87].
Ovarian Cancer Stem Cells and Microenvironment
Tumor heterogeneity is frequently associated with cancer stem cells, and the plasticity of tumor cells can shape cancer stem cell-related heterogeneity in response to the tumor microenvironment. The insufficient comprehension of the molecular behavior of these cancer stem cells and the consequent inadequate targeting of these cells within tumor tissue may significantly contribute to the low overall survival rates observed in ovarian cancer patients, as well as the development of drug resistance and recurrence in this population.Currently, there is a prevailing belief that the various alterations occurring within the cancer stem cell microenvironment (TME) are primarily accountable for the emergence of cancer stem cells and their involvement in tumorigenesis. The TME, which comprises non-cancer stem cell tumor cells (CCs) [88] and neighboring stroma, is actively modulated by these CCs to facilitate the preservation and propagation of the cancer stem cell niche [89]. The reciprocal transformation between cancer stem cells (CSCs) and tumor cells (CCs) is a dynamic process, whereby CSCs have the ability to induce CCs to undergo dedifferentiation and acquire tumor initiation properties [90]. Consequently, the intricate interplay between CSCs and CCs within the CSC niche in the tumor microenvironment (TME) has stimulated research into the similarities in gene expression patterns between these cell states and their impact on the shared regulatory circuitry. Furthermore, research endeavors have endeavored to discern the principal regulators within the co-regulatory network linking CSCs and CCs. These alterations facilitate the advancement of tumors towards a more malignant phenotype and confer resistance to chemotherapy. Identification of these pivotal regulators may facilitate the development of therapeutic interventions aimed at targeting CSCs, which could potentially be utilized in the management of ovarian cancer.
In this review, we summarize six therapeutic approaches for cancer stem cells, including targeting the signaling pathways of cancer stem cells, targeting the surface molecular markers of cancer stem cells, using miRNA to regulate drug resistance genes of cancer stem cells, using lncRNA to regulate drug resistance genes of cancer stem cells, and epigenetically changing the characteristics of cancer stem cells to induce cell differentiation. This is outlined in detail below
Targeted Therapy of Ovarian Cancer Stem Cells(refer to Fig. 2)
Targeting Ovarian Cancer Stem Cell-related Signaling Pathways
The activation of the AKT-GSK3β-β-catenin signaling axis by TRIB2 has been found to stimulate cancer stem cell-like properties [91]. Recent research indicates that TRIB2 may hold potential as a target for the treatment of ovarian cancer. In vitro investigations have demonstrated that targeting tumor stem cell-related factors can enhance the sensitivity of cancer stem cell-enriched tumor spheres to platinum drugs, thereby presenting a novel therapeutic approach for patients with platinum-resistant ovarian cancer [92].
The regulation of ovarian cancer stem cells is significantly influenced by the NANOG-miR-424/503-WEE1 signal axis, which has been demonstrated to be modulated by atorvastatin in certain studies. The combination of WEE1 inhibitor and conventional DNA damage drug chemotherapy holds promise for preventing the recurrence of ovarian cancer, as suggested by research findings [93].
The enrichment of cancer stem cells in ovarian cancer stem cells, which is dependent on cisplatin, is primarily attributed to the activation of multiple stemness-related pathways, notably the Notch signaling pathway [94]. Notably, genetic modifications in Notch pathway genes have been identified in approximately 22% of all ovarian tumors [95]. Recent investigations have demonstrated the critical involvement of the Notch pathway in cancer stem cell self-renewal, chemotherapy resistance, proliferation and maintenance, and evasion of cytotoxic drugs.Consequently, the inhibition of the Notch pathway to target cancer stem cells holds significant therapeutic potential. Recent research has identified ZIP4 as a novel cancer stem cell marker and a promising therapeutic target for high-grade serous ovarian cancer. Furthermore, investigations have demonstrated the involvement of a novel ZIP4-Notch3 axis in the regulation of tumor stem cell activity, encompassing the formation of sphere cells and colonies in vitro, as well as the development of tumor tissues and ascites in vivo [96]. This axis presents a viable approach for the targeting of ovarian cancer stem cells through the modulation of ZIP4. The activation of the stem-like transformation of ovarian tumor cells through the Notch1/c-Myc pathway by SNORA72 has been demonstrated in previous research [97]. This finding suggests that SNORA72 may be a viable therapeutic target for the eradication of cancer stem cells. Further studies have shown that a sequential combination therapy of cisplatin and eugenol may effectively eliminate drug-resistant cancer stem cells by targeting the Notch-Hes1 pathway [98]. Therefore, the Notch signaling pathway holds promise as a therapeutic target for ovarian cancer patients.
S100B, a calcium-binding protein with an efr-hand motif, exhibits aberrant expression in various cancer types, such as melanoma, colon cancer, and ovarian cancer [99]. Notably, S100B is highly expressed in ovarian cancer stem cells, thereby facilitating self-renewal and tumorigenicity of these cells. The stemness properties of ovarian cancer stem cells are regulated by S100B through its modulation of p53 [100]. Furthermore, S100B can deactivate p53, elevate the expression of MDR1 and MRP1, and confer resistance to cisplatin in ovarian cancer stem cells [101]. Several small-molecule inhibitors that target the S100B-p53 interaction have been studied for their potential in cancer therapy [102]. In the future, these inhibitors may be utilized in conjunction with chemotherapy to treat ovarian cancer.
The SNAI1/let-7 axis has been identified as the principal mechanism of epithelial-mesenchymal transition (EMT) that facilitates stemness. Furthermore, empirical evidence has demonstrated that SNAI1 can serve as a viable therapeutic target for directing cancer stem cells [103].
In vitro experiments conducted by Ping Chen and colleagues have shown that the extracts of two medicinal plants, namely Pao and Rau, exhibit significant inhibition of ovarian cancer stem cells. The joint inhibition of ovarian cancer stem cells by Pao and Rau may be attributed to their ability to inhibit the Wnt/β-catenin pathway. However, the veracity of this mechanism requires further validation through appropriate animal models [104].
The activation of the Notch3 pathway by NR2F6 has been demonstrated to induce cisplatin resistance and promote the stem-like phenotype in ovarian cancer cells. As a result, NR2F6 may represent a promising therapeutic target for the treatment of ovarian cancer, as suggested by previous research [105].
Eukaryotic initiation factor 5A2 (EIF5A2) is a putative oncogene situated on human chromosome 3q26, a genomic region that is frequently amplified in diverse tumors [106]. A growing body of evidence indicates that EIF5A2 exerts a crucial function in promoting anchorage-independent growth, xenograft tumor growth, augmenting cancer cell metastasis, and enhancing treatment resistance via various pathways [107]. The E2F1/KLF4 pathway is implicated in the positive regulation of ovarian cancer stem cell stemness by EIF5A2, suggesting a promising avenue for targeted therapy of this disease [108].
In pursuit of the objective of eliminating cancer stem cells, natural products have garnered considerable interest due to their enduring impact and comparatively minimal adverse effects [81]. Research has demonstrated that baicalin impedes the stemness of ovarian tumor cells by repressing RASSF6 at the transcriptional level, thereby diminishing YAP activity. This discovery highlights baicalin’s potential as a novel YAP inhibitor and a promising anti-tumor medication for eradicating ovarian cancer stem cells [109].
Recent findings indicate that brucine D exhibits a synergistic effect in paclitaxel-based chemotherapy for epithelial ovarian cancer, whereby its tumor suppressive properties are attributed to heightened apoptosis and clearance of cancer stem cells. Mechanistic investigations have further elucidated the involvement of JNK and STAT3 signaling pathways in the synergistic effect of brucine D in taxol-based chemotherapy for ovarian cancer [110].
N-butylphthalide (BP) is a naturally occurring compound that is derived from A. sinensis. The findings of the study indicate that BP effectively suppressed the proliferation of ovarian cancer stem cells in both in vitro and in vivo settings. Additionally, BP exhibited inhibitory effects on the migration and invasion of ovarian cancer stem cells. The mechanism of action of BP involves the activation of the apoptosis signaling pathway, which leads to the induction of apoptosis in ovarian cancer stem cells. Furthermore, BP was found to enhance the cytotoxicity of chemotherapy drugs such as cisplatin and paclitaxel against ovarian cancer stem cells [63].
Research has demonstrated that ovarian cancer stem cells exhibit a significant expression of ERβ1, and the utilization of ERβ agonizts may induce apoptosis in these cells while simultaneously decreasing their stemness through the up-regulation of FDXR and CDKN1A. It has been postulated that the ERβ agonist LY500307 may hold potential as a therapeutic agent for the management of ovarian cancer [111].
The activation of p70S6 kinase (p70S6K), which is an effector of the phosphatidylinositol 3 kinase /Akt pathway, has garnered considerable interest due to its frequent occurrence in ovarian cancer [112]. A rational approach involving the design of small interfering RNA (siRNA) targeting p70S6K in cancer stem cells, coupled with the delivery of siRNA through dendrimer nanotechnology, led to a noteworthy decrease in cancer stem cell proliferation, while exhibiting minimal cytotoxicity towards normal ovarian surface epithelial cells. The findings indicate that p70S6K holds potential as a therapeutic target for ovarian cancer. Moreover, when coupled with the administration of siRNA via nanotechnology, it presents a novel strategy for molecularly targeted cancer treatment in the context of metastatic ovarian cancer [113].
Research has indicated that the overexpression of XIST can augment the responsiveness of ovarian cancer stem cells to paclitaxel, with its impact potentially linked to the upregulation of KMT2C. The miR-93-5p/XIST/KMT2C signaling axis has been identified as a promising therapeutic target and may hold significant implications for the management of ovarian cancer, as per a study [114].
In an ovarian cancer mouse model, the utilization of a small molecule inhibitor of Fn14 to obstruct the TWEAK-Fn14-RelB signaling cascade resulted in an extension of patient survival following carboplatin chemotherapy. These findings provide insight into a signaling axis that may be employed in the treatment of ovarian cancer progression [115].
Calcitriol, a steroid hormone and active metabolite of vitamin D, has been shown to effectively eliminate ovarian cancer stem cells that exhibit ALDH positive, CD44 positive, and CD117 positive characteristics. This is achieved through the inhibition of the Wnt signaling pathway, which ultimately impedes the growth of xenograft tumors [116]. Simultaneously, the inhibition of ovarian cancer stem cell traits is facilitated by 1, 25 (OH)2D3 through the upregulation of VDR expression, the promotion of β-catenin expression in the cytoplasm, and the downregulation of CD44 expression. These discoveries offer novel perspectives on the contribution of vitamin D in diminishing the stemness of cancer stem cells [117].
The co-administration of paclitaxel and molotinib has been observed to effectively decrease tumor burden by suppressing paclitaxel-induced JAK2/STAT3 activation and the growth of tumor stem cells. These preliminary results hold significant potential for the advancement of a “maintenance therapy” following chemotherapy, utilizing the effectiveness of molotinib treatment for patients with ovarian cancer [118].
The GLI family of transcription factors, comprising GLI1, GLI2, and GLI3, are integral components of the Hedgehog (Hh) signaling pathway. GLI1 functions as a potent activator of target genes, and Hh signaling is essential for embryonic development [119]. Studies have demonstrated that inhibition of GLI1 transcription factor activity can effectively reverse cancer stem cell-like characteristics that exacerbate chemotherapy resistance and impede ovarian tumor cell migration. Targeting GLI1 may therefore represent a promising therapeutic strategy for enhancing the clinical outcomes of ovarian cancer patients with chemotherapy resistance and tumor metastasis [120].
Ovarian cancer cells have been found to express various estrogen receptor subtypes, such as ERα and ERβ [121]. Recent studies have shown that ERβ exhibits anti-tumor properties [122]. Phytoestrogens, namely genistein and daidzein, present in soybean have a strong affinity for ERβ. Additionally, Erβ-041, a highly effective selective ERβ agonist, has been identified.The compounds Genistein, daidzein, and ERβ-041 have been observed to decrease the migration, invasion, proliferation, and sphere formation of ovarian cancer cells, as well as induce cell cycle arrest and apoptosis. These effects are achieved through the modulation of the FAK, PI3K/AKT/GSK signaling pathway, and p21/cyclin D1 expression. These findings suggest that these compounds possess the ability to inhibit the stem-like properties of ovarian tumors and may serve as a viable therapeutic option for individuals afflicted with ovarian cancer [123].
The inhibition of self-renewal, invasion, and migration of ovarian cancer stem cells by SB525334 through the blockade of the TGF-β/Smad/EMT pathway presents a promising avenue for clinical diagnosis and therapeutic intervention in the context of ovarian cancer stem cell-mediated tumor metastasis and recurrence, as suggested by recent research [124].
The combination of a Yangplum diet and proanthocyanidin leaves has been found to effectively reduce the stem cell characteristics of ovarian cancer chemotherapy resistance. This is achieved through the induction of G1 phase cell cycle arrest, which targets the Wnt/β-catenin signaling pathway, as evidenced by research conducted by [125].
The up-regulation of PHBY259 phosphorylation in the lipid raft domain through c-Kit binding to PHB has been shown to activate the Notch3-PBX1 and β-catenin-ABCG2 signaling pathways, ultimately leading to an increase in ovarian cancer stemness. Consequently, targeting c-Kit and PHBY259 through intervention strategies presents an opportunity to screen and develop novel therapeutic drugs for the treatment of advanced ovarian cancer and related ailments [126].
The activation of the Fos/Jun pathway by LCC promotes the terminal differentiation of ovarian cancer cells and heightens their susceptibility to paclitaxel. This mechanism presents a promising avenue for targeting cancer stem cells and augmenting the efficacy of chemotherapy in treating ovarian cancer. Consequently, the combination of LCC and chemotherapy drugs holds significant potential as a therapeutic approach for ovarian cancer, warranting further investigation and development [127].
Research has indicated that PFKFB3 has the potential to regulate the inhibitor of apoptosis protein and NF-kB signaling pathways, thereby facilitating the stemness of ovarian tumors. This finding suggests that PFKFB3 could serve as a viable therapeutic target for individuals afflicted with ovarian cancer [128].
Research has demonstrated that the down-regulation of MYPT1 (PPP1R12A), which encodes myosin phosphatase target subunit 1, in ovarian tumors is linked to reduced patient survival, heightened tumorigenesis, and resistance to platinum-based chemotherapy drugs. Additionally, the overexpression of miR-30b targeting MYPT1 led to the augmentation of stem cell properties in ovarian tumors, which was found to be associated with Hippo pathway activation. The inhibition of the Hippo pathway transcriptional coactivator YAP has been found to impede platinum resistance that is induced by low expression of MYPT1 or overexpression of miR-30b. This discovery establishes a connection between chemotherapy resistance in ovarian tumors and the activation of Hippo pathway target genes following the downregulation of MYPT1, which enhances tumor stemness. The combined use of cisplatin and YAP inhibitors has been shown to effectively inhibit MYPT1-induced chemotherapy resistance, indicating the potential efficacy of this therapy for patients with low MYPT1 expression who may be resistant to platinum-based therapy [129].
The induction of the CSF2/p-STAT3 signaling pathway by myeloid-derived suppressor cells (MDSCs) has been found to enhance the stemness of ovarian tumor cells. As such, targeting MDSCs or CSF2 may prove to be a viable strategy for improving the efficacy of conventional treatment, as suggested by previous research [130].
The up-regulation of circ_0000745 by IGF2BP2 has been found to promote the invasion and stemness of ovarian tumor cells through the miR-3187-3p/ERBB4/PI3K/AKT axis. This discovery suggests that circ_0000745 may serve as a promising therapeutic target for the treatment of ovarian cancer [131].
Recent research has identified a novel mechanism through which HIF-2a governs the resistance of ovarian cancer stem cells to chemotherapy by directly stimulating BCRP. Furthermore, investigations have demonstrated that HIF-2a represents a crucial target for reversing the chemotherapy resistance mediated by ovarian cancer stem cells, and the combination of HIF-2a inhibitors with conventional chemotherapy is anticipated to enhance the therapeutic efficacy for patients with ovarian cancer [132] (refer to Table 1).
Targeting Molecular Markers of Ovarian Cancer Stem Cells
ALDH activity has been established as a functional marker of cancer stem cells in ovarian cancer, with high expression of ALDH1A1 observed in ovarian cancer stem cells [133]. Patients with elevated levels of ALDH1A1 in tumors have been found to exhibit poor survival [134, 135]. Consequently, targeting ALDH1A1 has been identified as a potentially effective strategy to impede tumor stemness and recurrence. In this regard, CM37 has been shown to inhibit ALDH1A1, leading to a rise in intracellular ROS accumulation, which, in turn, resulted in increased DNA damage and decreased viability of ovarian tumor cells. The efficacy of a novel small molecule inhibitor targeting ALDH1 A1 has been demonstrated in ovarian cancer models that exhibit a high concentration of cancer stem cells. The refinement of this class of small molecules presents a promising avenue for the development of a targeted therapeutic approach to address the challenge of refractory ovarian cancer [136].
The transcriptional repressor, DNA damage binding protein 2 (DDB2), has been found to impede the conversion of non-cancer Stem Cells Internationalo cancer stem cells by suppressing the transcription of Aldh1A1. Additionally, DDB2 has the ability to eliminate the traits of ovarian cancer stem cells by down-regulating the expression of ALDH1A1 [137]. A novel ALDH1A1 inhibitor, 974, has been discovered and has demonstrated efficacy in reducing the quantity of ovarian cancer stem cells by targeting ALDH1A1.The combination of small molecule inhibitors that target ALDH1A1 with chemotherapy presents a promising strategy for preventing the recurrence of ovarian cancer, with potential for clinical translation [138]. Various inhibitors have been developed to selectively target cancer stem cells by inhibiting ALDH1A1 or by utilizing a pan-ALDH1A inhibition approach. The latter approach offers the advantage of simultaneously targeting multiple ALDH isoforms. The compound 673 A, which inhibits pan-ALDH1A, induces apoptosis via programmed necrosis in ovarian cancer stem cells, leading to a reduction in tumorigenesis and a significant synergistic effect with chemotherapy agents. Additionally, Thea-saponin E has been shown to inhibit the proliferation and sphere formation of ALDH+ stem cells.
Disulfiram (DSF) is a well-known drug utilized for the treatment of alcoholism, which has demonstrated considerable potential for anticancer activity. Its mechanism of action involves the inhibition of enzymatic activity of ALDH isoforms and ROS generation, which can be further enhanced by Cu2+ regulation. DSF can be employed as a novel adjuvant chemotherapy drug in combination with cisplatin for the treatment of ovarian cancer. It can effectively inhibit ALDH activity and augment the sensitivity of cisplatin-resistant ALDH-positive cancer stem cells to cisplatin, as evidenced by previous research [139]. Subsequent investigations have revealed that ALDH contributes to oxidative stress, metabolism, and energy turnover in ALDH-associated cisplatin-resistant ovarian cancer stem cells. To summarize, this study has established the crucial involvement of ALDH-associated cisplatin-resistant cancer stem cells and has identified a rational DSF regimen as a promising therapeutic adjunct through quantitative in vitro assessment. This finding will aid in addressing ALDH-related cisplatin resistance and furnish a pragmatic foundation for the formulation of novel chemotherapy protocols [140].
In various solid tumors, the properties of cancer stem cells and resistance to chemotherapy have been observed to be inhibited by retinoic acid. The combination of cisplatin and retinoic acid has been shown to increase the sensitivity of platinum-based chemotherapeutic agents in ovarian cancer stem cells. The suppression of Nrf2 has been found to significantly reduce the tumor stem cell-like properties of ALDH-H cells, including high tumor stem cell markers, chemotherapy resistance, colony or sphere formation, and tumor growth [141]. In addition, it was observed that the expression of ALDH1 and activation of NRF2 were suppressed by all-trans retinoic acid (ATRA), leading to a decrease in the cancer stem cell-like characteristics of ALDH-H cells, while no such effect was observed in ALDH-L cells. These findings elucidate the underlying molecular mechanisms of Aldh1a1-mediated cancer stem cell-like properties and indicate the potential therapeutic application of ATRA in ovarian cancer stem cells with elevated Aldh1a1 expression [142].
Trimebutine maleate (TM) exhibits enhanced selectivity towards ovarian cancer stem cells through the inhibition of stemness-related transcription factors, namely OCT3/4 and SOX2, as well as the blockade of calcium and BKCa channels. In the case of advanced ovarian cancer patients with amplification of KCNMA1 gene and calcium channel subunit genes (CACNA1D, CACNA1F, and CACNA1H), BKCa and calcium channels may serve as viable drug targets for the management of recurrent and resistant ovarian cancer.Further experimentation and clinical verification are necessary to determine whether these genes serve as common tumor stem cell markers or represent specific subsets, and whether the combination of TM and conventional chemotherapy can enhance the survival rate of patients exhibiting high expression of these genes [143].
Several studies have demonstrated that the concomitant administration of bozotinib and nimaidipine can exert a synergistic effect in impeding the formation and viability of ovarian cancer stem cell spheres. Furthermore, the combined treatment of these pharmaceutical agents has been observed to significantly diminish the expression of cancer stem cell markers CD133, KLF4, and NANOG, as well as stemness-related signaling molecules such as phosphorylated stat5, phosphorylated akt, phosphorylated erk, and Wnt/β-catenin. Additionally, the dual drug regimen has been shown to induce apoptosis of ovarian cancer stem cells to a significant degree [144].
According to research findings, KLF12 has the potential to serve as a therapeutic target for the management of cisplatin-resistant ovarian cancer. This is achieved through the regulation of ISG15 expression, which effectively inhibits the cancer stem cell phenotype [145].
Research has demonstrated that the up-regulation of PIK3R3 in ovarian cancer stem cells can be mitigated by inhibiting PIK3R3, resulting in a reduction in the size of ovarian cancer stem cell spheroids. Furthermore, ROC curve analysis of drug response has suggested that PIK3R3 may serve as a promising predictive biomarker for Avastin®-mediated ovarian tumor therapy [146].
The efficacy of 4-MU in suppressing the expression of cancer stem cell markers, specifically ALDH1A1 and ABCG2, has been demonstrated. This has led to the proposition that 4-MU holds potential as a therapeutic approach to impede the activation of cancer stem cells and enhance the survival rates of patients. Additionally, 4-MU has been observed to hinder the proliferation and invasion of drug-resistant ovarian cancer cells by inducing apoptosis and inhibiting the activation of cancer stem cells [147].
The presence of the carbohydrate component Sialic acid Thomson neoantigen (STn) has been identified on protein biomarkers of pancreatic, colonic, and gastric cancer stem cells. Research has revealed that human ovarian cancer cell lines exhibit varying levels of STn and the ovarian cancer stem cell marker CD133. STn-positive cells have been found to possess cancer stem cell properties, indicating that targeted therapies against STn may prove to be a viable clinical approach for eliminating STn-positive cancer stem cells and STn-positive non-cancer stem cell populations in ovarian tumors [148] (refer to Table 2).
To Use miRNA to Regulate Drug Resistance Genes in Ovarian Cancer Stem Cells
Research has demonstrated that miR-600 facilitates the stemness, proliferation, and metastasis of ovarian cancer cells by directly suppressing KLF9. Consequently, reducing the expression of miR-600 may represent a novel therapeutic approach for ovarian cancer in the future [149].
Research has demonstrated that let-7i possesses the ability to impede the migration and invasion of tumor cells, as well as stimulate apoptosis by suppressing the stemness of tumor cells. In instances where BRCA mutations are absent, the overexpression of let-7i has been observed to heighten the sensitivity of tumor cells to the PARP inhibitor olaparib. These findings have established a sound basis for the utilization of let-7i as a therapeutic agent in the management of ovarian cancer patients [150].
The expression of miR-139-5p/SDC4 through WDFY3-AS2 has the potential to alter the cisplatin resistance of ovarian cancer cells both in vitro and in vivo, thereby offering a promising therapeutic avenue for addressing drug resistance in ovarian cancer [151].
The findings of a study indicate that the estrogen-mediated E2F6 ceRNA network, epigenetics, and competitive inhibition of microRNA-193a activity contribute to the promotion of stemness and tumorigenesis in ovarian cancer. Consequently, inhibiting estrogen production in vivo may have therapeutic implications for ovarian cancer [152].
LncRNA Regulates Drug Resistance Genes of Ovarian Cancer Stem Cells
Taurine upregulated gene 1 (TUG1) is a lengthy non-coding RNA situated on chromosome 22q12.2 [153]. The long non-coding RNA TUG1 has the potential to enhance the proliferation, invasion, and stemness of ovarian tumor cells. Research has demonstrated that TUG1 exerts a tumorigenic effect in ovarian cancer by modulating the stemness of ovarian tumor cells.The direct targeting of miR-186-5p by TUG1 leads to the up-regulation of ZEB1, ultimately promoting the proliferation, invasion, and stemness of ovarian tumor cells. As such, TUG1 presents itself as a potential therapeutic target for the treatment of ovarian cancer. These findings offer a novel perspective on the pathogenesis of ovarian cancer and provide a foundation for improved diagnosis and treatment strategies [154].
Epigenetic Changes in Stemness of Ovarian Tumor Cells
The negative regulatory function of STON2 in ovarian tumor cells has been observed through DNMT1/MUC1-mediated epigenetic mechanisms. As such, STON2 is implicated in the biological processes of ovarian cancer stem cells and presents a promising target for novel therapeutic interventions aimed at eradicating ovarian cancer [155].
Induction of Differentiation to Treat Ovarian Cancer Stem Cells
Inducing differentiation is a crucial approach for effectively eradicating cancer stem cells and mitigating drug resistance [87]. This can be achieved through various mechanisms, including morphogenesis-driven signaling cascades and epigenetic differentiation therapies [156]. Commonly used differentiation inducers, such as all-trans retinoic acid (ATRA), a metabolic intermediate of vitamin A, have been shown to induce differentiation of breast cancer stem cells, reduce cell invasion and migration, and enhance sensitivity to tumor therapy in clinical settings [157].Research has indicated that photoflavin, a derivative of riboflavin, has the ability to decrease drug resistance in cancer stem cells within the OVCAR-3 cell lines (CSCs/DDP) of ddresistance ovarian cancer. Additionally, it has been found to augment the efficacy of cisplatin (DDP) chemotherapy on cancer stem cells by inducing differentiation of the tumor stem cell phenotype [158].
Other Methods Treat Ovarian Cancer Stem Cells
Epidemiological and scientific studies have provided evidence indicating the significant involvement of hormones in the development and occurrence of ovarian tumors. Several studies have demonstrated the participation of the androgen receptor AR in the progression of multiple malignant tumors, such as prostate cancer, bladder cancer, liver cancer, kidney cancer, and lung cancer [159, 160]. In recent times, the association between polycystic ovary syndrome, obesity, and a heightened risk of ovarian cancer has been established, leading to the AR signaling axis becoming a research focal point [161]. The mounting evidence suggests that AR is commonly expressed in diverse subtypes of ovarian cancer, particularly epithelial ovarian cancer, and its elevated expression is linked to unfavorable prognosis of ovarian cancer [162, 163]. Furthermore, androgens have the potential to stimulate the stemness traits of ovarian cancer cells through the activation of the Nanog promoter. This discovery necessitates further investigation, as it could offer novel insights into the hormonal regulatory pathways of ovarian cancer stem cells, thereby prompting a reevaluation of the therapeutic approaches for ovarian cancer stem cells [164].
Salinomycin is a monocarboxylic polyether ionophore isolated from Streptomyces albus. As a inonophore with strict selectivety for alkali ions and a strong preference for potassium, salinomycin interferes with transmembrane potassium potential and promotes the efflux of K+ ions from mitochondria and cytoplasm [165]. It exerts a range of effects on cancer stem cells, such as apoptosis induction, autophagy, oxidative stress, and inhibition of tumor cell proliferation, angiogenesis, and stemness [166,167,168]. Nevertheless, its clinical application as an anticancer agent is restricted due to its low water solubility and high toxicity to healthy tissues at elevated doses. We proposed a therapeutic strategy aimed at reducing the adverse reactions of salinomycin and improving its clinical benefits by constructing tumor targeting vectors that mimic high-density lipoprotein (HDL) and synthesizing salinomycin-loaded high-density lipoprotein (S-HDL) [169].
The Plasma Activation Medium (PAM) exhibits selective targeting of a diverse range of malignant tumor cells, thereby demonstrating its potential as an anticancer drug [70, 71]. Research has shown that PAM effectively diminishes the properties of ovarian cancer stem cells and exhibits a synergistic antitumor effect when combined with cisplatin [170].
Cantrixil is a newly developed third-generation benzopyrun molecule. Initial examination of stem cell markers has demonstrated that IP Cantrixil has the potential to trigger apoptosis of ovarian cancer stem cells and enhance the sensitivity of cells to conventional chemotherapy treatments. This finding is significant and warrants further investigation for potential early clinical implementation, with the aim of providing greater benefits to individuals afflicted with ovarian cancer [171].
For a considerable period, molecular hydrogen has been regarded as an inactive gas. However, Ohsawa et al. have documented that hydrogen exhibits antioxidant properties and restrains brain damage resulting from ischemia-reperfusion, thereby signifying its therapeutic potential [172]. Numerous researchers have similarly documented the therapeutic potential of hydrogen molecules in various ailments, such as ischemia-reperfusion injury (I/R), metabolic syndrome, neurodegeneration, mitochondrial diseases, and inflammation. Despite the commonly held belief that the antioxidant properties of hydrogen molecules are responsible for their beneficial effects, the precise molecular mechanisms underlying these effects remain elusive [173]. The study indicates that hydrogen molecules possess the ability to impede the growth of cancer stem cells and associated angiogenesis, thereby proposing their potential utility in the management of ovarian cancer [174].
Chromatin target protein arginine methyltransferase (CHTOP) is a crucial intracellular protein that exhibits high expression levels in ovarian cancer. Its close association with the malignant phenotype of epithelial ovarian cancer cells, including metastasis, chemotherapy resistance, and stemness, indicates its potential as a targeted therapy for ovarian cancer. Inhibition of stemness-related signaling pathways has been shown to decrease the stemness of epithelial ovarian cancer cells [175].
COX-2, a prostaglandin synthase responsible for the conversion of arachidonic acid to PGH2, has been found to be significantly overexpressed in ovarian cancer patients, potentially contributing to the progression of the disease [176]. Additionally, 5-LOX, also known as 5-lipoxygenase, has been linked to the promotion of hypoxic response and inflammation in ovarian epithelial cells [177]. The compound licofelone, a dual COX/LOX inhibitor, has been shown to reverse the stemness of ovarian multicellular tumor spheres (MCTS) and increase their sensitivity to the first-line chemotherapy drug paclitaxel [178].
The results indicate that the utilization of clinically feasible NAMPT inhibitors, such as FK866, in conjunction with platinum-based chemotherapy, to target NAMPT, is a potentially effective therapeutic approach in the suppression of treatment-induced aging-related cancer stem cells [179].
The anti-malarial drug, Atovaquone, which has received approval from the FDA, has been demonstrated to impede the proliferation of ovarian cancer stem cells by inhibiting mitochondrial electron transport, as evidenced by research findings [180].
A set of GA(glycyrrhetinic acid) derivatives, which incorporate a CA moiety with either piperazine or ethylenediamine (EDA) as a linker, were synthesized and designed. These semisynthetic derivatives were subjected to in vitro testing to determine their inhibitory activity against ovarian tumor cell growth. Compound 7c exhibited the highest inhibitory activity and selectivity among the tested derivatives.The study demonstrated that compound 7c effectively decreased the colony formation and sphere formation capacity of SKOV3 and OVCAR3 cells, while also significantly reducing the proportion of CD44 + , CD133 + , and ALDH+ subsets in both cell lines. These findings suggest that compound 7c possesses strong potential in eradicating ovarian cancer stem cells [181].
Numerous studies have indicated that the persistence of ALDH+ cells subsequent to chemotherapy is the primary cause of ovarian cancer recurrence [182]. It has been established that cisplatin administration to ovarian cancer cells leads to an elevation in mitochondrial membrane potential. Both in vitro and in vivo investigations have demonstrated that the co-administration of OXPHOS inhibitors and platinum effectively impedes platinum-induced enrichment of ALDH+ cells. The aforementioned discovery underscores the necessity for additional preclinical and clinical investigations focused on the utilization of OXPHOS inhibitors to prolong the reappearance of ovarian cancer and enhance the longevity of individuals afflicted with ovarian cancer [183].
Recent research has indicated that EZH2 plays a crucial role in the promotion of T cell differentiation [184]. Consequently, it is imperative to carefully evaluate the appropriate dosage of EZH2 inhibitors in the treatment of ovarian cancer so as not to compromise T cell functionality.
Several studies have indicated that piperine exhibits potential as an anticancer agent, as it can mitigate the stemness of ovarian tumor cells, thereby enhancing the efficacy of chemotherapy in cancer patients [185].
The preclinical efficacy of Saracatinib (AZD0530), a potent Src family kinase inhibitor, in high-grade serous ovarian cancer has been established [186]. Additionally, Selumetinib (AZD6244), a noncompetitive MEK1/2 inhibitor, has demonstrated clinical activity in low-grade ovarian cancer by inhibiting serous and clear cell ovarian cancer xenografts [187]. Furthermore, the combined treatment of Saracatinib and Selumetinib has been shown to target ovarian cancer stem cells, resulting in reduced ovarian cancer proliferation and induction of cell death [188].
The elimination of cancer stem cells in ovarian cancer can be achieved through the application of combination therapy involving thioredihydroquinazolines and cisplatin. The potential for more effective treatment of cisplatin-resistant metastatic ovarian cancer can be realized through the continued development of thioxdihydroquinazolinone small molecules, as suggested by previous research [189].
Research has demonstrated that the overexpression of Survivin is a significant contributor to the chemoresistance of ovarian cancer stem cells. CPE-1347, a mixed lineage kinase inhibitor that has been deemed safe for human use, selectively targets the expression of Survivin in ovarian cancer stem cells. By acting as a sensitizer to conventional chemotherapy for ovarian cancer, CEP-1347 presents a viable and practical approach to improving the treatment of this disease [190].
AS602801 has been identified as a potential anti-cancer stem cell agent that can enhance the responsiveness of ovarian cancer stem cells to paclitaxel and carboplatin therapy by downregulating the expression of the anti-apoptotic protein survivin. Research findings indicate that AS602801 may augment the sensitivity of ovarian cancer stem cells to paclitaxel by suppressing the expression of MDR1 [36].
Solanum solanum extract containing the active ingredient (SR-T100) can induce cell apoptosis by up-regulating the expression of tumor necrosis factor receptor and activating the mitochondrial apoptosis pathway, and has a therapeutic effect on actinic keratosis. There are studies evaluating new molecular mechanisms of SR-T100-regulated stemness and chemoresistance. The concentration of SR-T100 inhibiting 50% cell viability (IC50) in ovarian cancer cells was lower than that in non-malignant cells. The IC50 of SR-T100 in resistant cells was similar to that in sensitive cells. In addition, SR-T100 increased the sensitivity of drug-resistant cells to cisplatin and paclitaxel. SR-T100 can down-regulate the expression of stem cell markers aldehyde dehydrogenase 1 (ALDH1), Notch1 and FoxM1 in ovarian cancer cells, and reduce the formation of ovarian cancer cell spheres. Using microarray analysis, immunoblotting, luciferase activity and chromatin immunoprecipitation (ChIP) analysis, we found that SR-T100 inhibited the expression and promoter activity of c/EBPβ and COL11A1 in the resistant cells but not in the sensitive cells. The SR - T100, paclitaxel and cisplatin can restrain the growth of the A2780CP70 cells in nude mice transplanted tumor, and cisplatin and SR - T100 combined inhibition of the superior to the application. The SR - T100 may be potential adjuvant treatment of ovarian cancer chemotherapy drug [191].
Aldehyde dehydrogenase 1 (ALDH1) is a marker of cancer stem cell-like cells (CSC) in human cancers. However, the specific ALDH1 regulatory function and the underlying signaling pathways have not been fully elucidated. Studies ALDH1 adjust function and its potential signal transduction, and tested all trans retinoic acid (ATRA) can inhibit ALDH1 regulating tumor behavior of ovarian cancer cells. By using flow cytometry and exogenous expression of enrichment of low or knock out the expression of ALDH1 found ALDH1 activity and the drying of ovarian cancer cells were positively correlated, according to the formation and the expression of CSC marker balloon and tumor xenograft model in mice. ALDH1 directly regulates the function of ovarian cancer cells. Also found ALDH1 can regulate the expression of FoxM1 and Notch 1, while the FoxM1 and Notch 1 participated in the downstream of ALDH1 mediated the biological function of signal transduction. Silk bacterium element sulfur chain (Thiostrepton) inhibition of FoxM1 and DAPT Notch1 inhibition can be cut cells into the ball skills. ATRA can reduce the expression of ALDH1, inhibit the tumorigenic ability of ovarian cancer cells, and inhibit the sphere formation, cell migration and invasion of ovarian cancer cells. Above all cut ALDH1 FoxM1 / ATRA Notch1 signaling pathway and inhibition of ovarian cancer cell tumor formation [192].
Summary and Prospect
The cellular state of the cancer stem cell phenotype has been acknowledged for a considerable period of time as a mechanism that replenishes a substantial quantity of tumor cells via self-renewal, exhibiting a high capacity for tumor initiation and resistance to treatment. In recent times, numerous research groups have formulated novel therapeutic approaches to eliminate tumors and forestall disease recurrence by focusing on this minute cohort of cells. The resistance exhibited by ovarian cancer stem cells has been attributed to several factors, including decreased intracellular drug accumulation, heightened DNA repair, and the quiescent nature of these cells. In recent years, various approaches have been explored to overcome drug resistance in ovarian cancer by targeting cancer stem cells. These strategies include targeting surface markers of cancer stem cells, inhibiting drug efflux transporters, regulating pathways of cell self-renewal and differentiation, and inducing apoptosis [166]. In the context of ovarian cancer stem cells, the inhibition of Notch activity through the use of gamma-secretase inhibitors (GSI), Aurora A kinase, or DNA methyltransferase inhibitors has demonstrated efficacy in targeting epigenetic processes [10, 167, 168]. Additionally, several prominent transcriptional regulators including Myc, β-Catenin, NFκB, STAT, RUNX, and NOTCH/CSL have emerged as potential therapeutic candidates for the targeting of cancer stem cells [87]. The aggregation of data indicates that modifications in lipid and fatty acid-associated signaling pathways play a crucial role in the preservation of cancer stem cells [35, 36]. Current empirical data proposes that the regulation of cancer stem cell maintenance and differentiation is governed by extracellular matrix mechanics. The interplay between cells and extracellular matrix is a fundamental factor in the establishment and preservation of stem cells [156, 193].Cancer stem cells have the ability to diminish and evade natural killer (NK) cells by suppressing the expression of NK cell-activating ligands, including major histocompatibility I peptide-related sequence A (MICA) and histocompatibility I peptide-related sequence B (MICB), thereby evading immune surveillance [157].
Cancer stem cells typically comprise a minor proportion of the overall cancer cell population. Consequently, high-throughput screening drugs that are selectively targeted rely on the in vitro proliferation of a stable and highly enriched population of cancer stem cells. Various techniques exist for isolating ovarian cancer stem cells, however, the mechanisms through which ovarian cancer stem cells originating from distinct pathways facilitate tumor progression are dissimilar. Currently, the fundamental signaling pathways that regulate ovarian cancer stem cells remain indeterminate.Recent research has demonstrated that cancer stem cells exhibit heightened activity, and that the anomalous activation of transcriptional regulators associated with the cancer stem cell phenotype may impart a significant degree of cellular plasticity [194]. Hence, the identification of molecular regulators that govern distinct functions, namely self-renewal, differentiation, and chemotherapy resistance, in cancer stem cells is of paramount importance. These cells are not only indispensable for the initiation and progression of tumors, but also contribute significantly to treatment resistance and disease relapse owing to their capacity to counteract drug efficacy [195].
Chemotherapy is a primary and all-encompassing therapeutic approach aimed at impeding the advancement of tumors and extending the survival time of patients after surgery [196]. In general, patients diagnosed with advanced ovarian cancer exhibit a favorable response to a combination of taxane and platinum chemotherapy. However, the presence of chemoresistant tumor cells in metastatic sites may persist, resulting in a state of dormancy for an extended period following initial treatment, ultimately culminating in tumor recurrence [197]. Over the past few decades, there have been persistent endeavors to advance surgical techniques and intensive combination chemotherapy for the treatment of advanced ovarian cancer. However, despite these efforts, the long-term clinical outcomes for patients have not exhibited significant improvement [198]. Notably, ovarian cancer stem cells have been observed to endure conventional chemotherapy, thereby posing a clinical challenge. In this context, while the mechanisms linked to ovarian cancer stem cells remain incompletely understood, empirical evidence has shown that a minor subset of tumor cells exhibiting chemotherapy resistance may possess cancer stem cell attributes, thereby contributing significantly to disease relapse [199]. Consequently, there is a pressing need to explore novel therapeutic interventions that target cancer stem cells. Such interventions could involve the direct targeting of stem-cell surface biomarkers, the modulation of stem-cell signaling pathways, or other approaches aimed at eradicating cancer stem cells. Numerous clinical trials investigating targeted therapy have yielded unfavorable outcomes [4], indicating significant challenges in the development of therapeutic drugs targeting cancer stem cells. In order to gain a deeper understanding of disease progression and drug resistance mechanisms in tumors, in vivo and in vitro biological tests are necessary to facilitate the development of drugs targeting cancer stem cells [200].
Conclusion
Consider revising the sentence as follows: Significant advancements have been achieved in the investigation of ovarian cancer stem cells in the past. Through the collaborative endeavors of pertinent specialists, cancer stem cells have been effectively isolated and cultured, and potential therapeutic targets and molecular markers for ovarian cancer stem cells have been identified. Nevertheless, these findings remain insufficient, and further exploration is required to elucidate the precise mechanism of action and targeted therapy. The primary objective is to persist in identifying and evaluating particular cancer stem cell markers and associated signaling pathways in ovarian cancer. This pursuit aims to enable earlier and more precise detection of tumors, facilitate targeted therapy, eradicate cancer stem cells, and establish novel avenues for the precise treatment of patients with ovarian cancer. Nevertheless, substantial impediments exist in the elimination of cancer stem cells. Initially, it is observed that these cells demonstrate heightened resistance to conventional cytotoxic drugs, and the administration of standard chemotherapy may inadvertently facilitate disease progression by promoting the selection of cancer stem cells. Additionally, the utilization of non-targeted cytotoxic drugs to eliminate cancer stem cells may result in severe side effects due to their inherent drug resistance and limited quantity. Consequently, the safe dosages of conventional cytotoxic drugs employed in clinical practice are inadequate for the eradication of cancer stem cells. Regrettably, conclusive clinical evidence supporting the efficacy of targeted therapies aimed at cancer stem cells in preventing tumor recurrence and metastasis remains elusive. Consequently, additional in vitro and in vivo trials are imperative to ensure the development of drugs targeting cancer stem cells, thereby enhancing the prognosis of patients afflicted with ovarian cancer.
References
Shanmugasundaram, G., Sundaramoorthy, E., & Sudalaiandi, S., et al. (2015). Double pathology: Malignant epithelial ovarian tumor and germ cell tumor (choriocarcinoma), a rare coexistence. World Journal of Clinical Oncology, 6, 421–425.
Siegel, R. L., Miller, K. D. & Jemal, A. (2020). Cancer statistics. CA: A Cancer Journal for Clinicians, 70, 7–30. https://doi.org/10.3322/caac.21590.
Karnezis, A. N., Cho, K. R., & Gilks, C. B., et al. (2017). The disparate origins of ovarian cancers: pathogenesis and prevention strategies. Nature Reviews Cancer, 17(1), 65–74. https://doi.org/10.1038/nrc.2016.113.
Chen, V. W., Ruiz, B., Killeen, J. L., Cote, T. R., Wu, X. C., & Correa, C. N. (2003). Pathology and classifification of ovarian tumors. Cancer, 97, 2631–2642.
Li, S. S., Ma, J., & Wong, A. S. T. (2018). Chemoresistance in ovarian cancer: exploiting cancer stem cell metabolism. Journal of Gynecologic Oncology, 29, e32 https://doi.org/10.3802/jgo.2018.29.e32.
Torre, L. A., Bray, F., Siegel, R. L., Ferlay, J., Lortet-Tieulent, J., & Jemal, A. (2012). Global cancer statistics. CA: A Cancer Journal for Clinicians, 65, 87–108.
Bachmayr-Heyda, A., Auer, K., Sukhbaatar, N., Aust, S., Deycmar, S., Reiner, A. T., Polterauer, S., Dekan, S., & Pils, D. (2016). Small RNAs and the competing endogenous RNA network in high grade serous ovarian cancer tumor spread. Oncotarget, 7, 39640–39653.
Stewart, C., Ralyea, C., & Lockwood, S. (2019). Ovarian cancer: An integrated review. Seminars in Oncology Nursing, 35(2), 151–156. https://doi.org/10.1016/j.soncn.2019.02.001.
Torre L., Trabert B., DeSantis C., et al. (2018) Ovarian cancer statistics. CA. 68(4):284–296. https://doi.org/10.3322/caac.21456
Vargas-Hern´ andez, V. M., Moreno-Eutimio, M. A., Acosta-Altamirano, G., & Vargas-Aguilar, V. M. (2014). Management of recurrent epithelial ovarian cancer. Gland Surgery, 3(3), 198–202.
Cornelison, R., Llaneza, D. C., & Landen, C. N. (2017). Emerging therapeutics to overcome chemoresistance in epithelial ovarian cancer: a mini-review. International Journal of Molecular Sciences, 18(10), 2171.
Kim, J. Y., Cho, C. H., & Song, H. S. (2017). Targeted therapy of ovarian cancer including immune check point inhibitor. Korean Journal of Internal Medicine, 32(5), 798–804. https://doi.org/10.3904/kjim.2017.008.
Ffrench, B., Gasch, C., O’Leary, J. J., & Gallagher, M. F. (2014). Developing ovarian cancer stem cell models: Laying the pipeline from discovery to clinical intervention. Molecular Cancer, 13, 262 .
Bai, X., Chen, Y., Hou, X., Huang, M., & Jin, J. (2016). Emerging role of NRF2 in chemoresistance by regulating drug-metabolizing enzymes and efflux transporters. Drug Metabolism Reviews, 48, 541–567.
McGuire, W. P., Hoskins, W. J., & Brady, M. F., et al. (1996). Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. The New England Journal of Medicine, 334, 1–6.
Vergote, I., Tropé, C. G., & Amant, F., et al. (2010). Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. The New England Journal of Medicine, 363, 943–953.
Davis, A., Tinker, A. V., & Friedlander, M. (2014). Platinum resistant” ovarian cancer: What is it, who to treat and how to measure benefit? Gynecologic Oncology, 133, 624–631.
Foley, O. W., Rauh-Hain, J. A., & del Carmen, M. G. (2013). Recurrent epithelial ovarian cancer: an update on treatment. Oncology, 27(4), 288.
Dao, F., Schlappe, B. A., & Tseng, J., et al. (2016). Characteristics of 10-year survivors of high-grade serous ovarian carcinoma. Gynecologic Oncology, 141(2), 260–263. https://doi.org/10.1016/j.ygyno.2016.03.010.
Kim, S., Han, Y., Kim, S. I., Kim, H. S., Kim, S. J., & Song, Y. S. (2018). Tumor evolution and chemoresistance in ovarian cancer. NPJ Precision Oncology, 2, e20 .
Rich, J. N. (2016). Cancer stem cells: Understanding tumor hierarchy and heterogeneity. Medicine, 95, S2–S7.
Clarke, M. F., Dick, J. E., Dirks, P. B., Eaves, C. J., Jamieson, C. H. M., Jones, D. L., Visvader, J., Weissman, I. L., & Wahl, G. M. (2006). Cancer stem cells-perspectives on current status and future directions: AACR Workshop on cancer stem cells. Cancer Research, 66, 9339–9344.
Ajani, J. A., Song, S., Hochster, H. S., & Steinberg, I. B. (2015). Cancer stem cells: the promise and the potential. Seminars in Oncology, 42, S3–S17.
Nishi, M., Akutsu, H., Kudoh, A., Kimura, H., Yamamoto, N., Umezawa, A., Lee, S. W., & Ryo, A. (2014). Induced cancer stem-like cells as a model for biological screening and discovery of agents targeting phenotypic traits of cancer stem cell. Oncotarget, 5, 8665–8680.
Visvader, J. E., & Lindeman, G. J. (2008). Cancer stem cells in solid tumours: Accumulating evidence and unresolved questions. Nature Reviews Cancer, 8, 755–768.
Alison, M. R., Lim, S. M., & Nicholson, L. J. (2011). Cancer stem cells: Problems for therapy? The Journal of Pathology, 223, 147–161.
Bao, B., Ahmad, A., Azmi, A., Ali, S., & Sarkar, F. (2013). Overview of cancer stem cells (CSCs) and mechanisms of their regulation: Implications for cancer therapy. Current Protocols in Pharmacology, 61, 14 .
Shibue, T., & Weinberg, R. A. (2017). EMT, CSCs, and drug resistance: The mechanistic link and clinical implications. Nature Reviews Clinical Oncology, 14, 611–629.
Batlle, E., & Clevers, H. (2017). Cancer stem cells revisited. Nature Medicine, 23, 1124–1134.
Chang, J. C. (2016). Cancer stem cells: Role in tumor growth, recurrence, metastasis, and treatment resistance. Medicine, 95, S20–S25.
Lytle, N. K., Barber, A. G., & Reya, T. (2018). Stem cell fate in cancer growth, progression and therapy resistance. Nature Reviews Cancer, 18, 669–680. https://doi.org/10.1038/s41568-018-0056-x.
Chen, D., Wu, M., Li, Y., Chang, I., Yuan, Q., & Ekimyan-Salvo, M., et al. (2017). Targeting BMI1(+) cancer stem cells overcomes chemoresistance and inhibits metastases in squamous cell carcinoma. Cell Stem Cell, 20, 621–634.e626. https://doi.org/10.1016/j.stem.2017.02.003.
Vinogradov, S., & Wei, X. (2012). Cancer stem cells and drug resistance: the potential of nanomedicine. Nanomed, 7, 597–615.
Keyvani, V., Farshchian, M., Esmaeili, S.-A., Yari, H., Moghbeli, M., & Nezhad, S.-R. K., et al. (2019). Ovarian cancer stem cells and targeted therapy. Journal of Ovarian Research, 12(1), 1–11. https://doi.org/10.1186/s13048-019-0588-z.
Liang, D. H., Choi, D. S., Ensor, J. E., Kaipparettu, B. A., Bass, B. L., & Chang, J. C. (2016). The autophagy inhibitor chloroquine targets cancer stem cells in triple negative breast cancer by inducing mitochondrial damage and impairing DNA break repair. Cancer Letters, 376(2), 249–258. https://doi.org/10.1016/j.canlet.2016.04.002.
Yamamoto, M., Suzuki, S., Togashi, K., Sanomachi, T., Seino, S., & Kitanaka, C., et al. (2019). AS602801 sensitizes ovarian cancer stem cells to paclitaxel by down-regulating MDR1. AntiCancer Research, 39(2), 609–617. https://doi.org/10.21873/anticanres.13154.
Nassar, D., & Blanpain, C. (2016). Cancer stem cells: basic concepts and therapeutic implications. Annual Review of Pathology, 11, 47–76. https://doi.org/10.1146/annurev-pathol-012615-044438.
Pal, D., Kolluru, V., Chandrasekaran, B., Baby, B. V., Aman, M., Suman, S., Sirimulla, S., Sanders, M. A., Alatassi, H., & Ankem, M. K., et al. (2017). Targeting aberrant expression of Notch-1 in ALDH (+) cancer stem cells in breast cancer. Molecular Carcinogenesis, 56, 1127–1136.
Li, C., Heidt, D. G., Dalerba, P., Burant, C. F., Zhang, L., Adsay, V., Wicha, M., Clarke, M. F., & Simeone, D. M. (2007). Identification of pancreatic cancer stem cells. Cancer Research, 67, 1030–1037.
O’Brien, C. A., Pollett, A., Gallinger, S., & Dick, J. E. (2007). A human colon cancer cell capable of initiating tumour growth in immunodeficient mice. Nature, 445, 106–110.
Bonnet, D., & Dick, J. E. (1997). Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nature Medicine, 3, 730–737.
He Q. Z., Luo X. Z., Wang K., Zhou Q., Ao H., Yang Y., Li S. X., Li Y., Zhu H. T., Duan T., (2014) Cellular physiology and biochemistry. International Journal of Experimental Cellular Physiology, Biochemistry and Pharmacology 33,173–184.
Dalerba, P., Cho, R. W., & Clarke, M. F. (2007). Cancer stem cells: models and concepts. Annual Review of Medicine, 58, 267–284.
Jordan, C. T., Guzman, M. L., & Noble, M. (2007). Cancer stem cells. The New England Journal of Medicine, 355, 1253–1261.
Reya, T., Morrison, S. J., Clarke, M. F., & Weissman, I. L. (2001). Stem cells, cancer, and cancer stem cells. Nature, 414, 105–111.
Pardal, R., Clarke, M. F., & Morrison, S. J. (2003). Applying the principles of stem-cell biology to cancer. Nature Reviews Cancer, 3, 895–902.
Gkountela, S., & Aceto, N. (2016). Stem-like features of cancer cells on their way to metastasis. Biology Direct, 11, e33 .
Maugeri-Sacca, M., Bartucci, M., & De Maria, R. (2012). DNA damage repair pathways in cancer stem cells. Molecular Cancer Therapeutics, 11, 1627–1636.
Phi, L. T. H., Sari, I. N., Yang, Y. G., Lee, S. H., Jun, N., Kim, K. S., Lee, Y. K., & Kwon, H. Y. (2018). Cancer Stem Cells (CSCs) in drug resistance and their therapeutic implications in cancer treatment. Stem Cells International, 2018, e5416923 .
Chow, E. K. (2013). Implication of cancer stem cells in cancer drug development and drug delivery. Journal of Laboratory Automation, 18, 6–11.
Abdullah, L. N., & Chow, E. K. (2013). Mechanisms of chemoresistance in cancer stem cells. Clinical and Translational Medicine, 2, e3 .
Deheeger, M., Lesniak, M. S., & Ahmed, A. U. (2014). Cellular plasticity regulated cancer stem cell niche: A possible new mechanism of chemoresistance. Cancer Cell Microenviron, 1, e295.
Doherty, M. R., Smigiel, J. M., Junk, D. J., & Jackson, M. W. (2016). Cancer stem cell plasticity drives therapeutic resistance. Cancers, 8, e8 .
Brown, R., Curry, E., Magnani, L., Wilhelm-Benartzi, C. S., & Borley, J. (2014). Poised epigenetic states and acquired drug resistance in cancer. Nature Reviews Cancer, 14, 747–753.
Bapat, S. A., Mali, A. M., Koppikar, C. B., & Kurrey, N. K. (2005). Stem and progenitor-like cells contribute to the aggressive behavior of human epithelial ovarian cancer. Cancer Research., 65, 3025–3029.
Vathipadiekal, V., Saxena, D., Mok, S. C., Hauschka, P. V., Ozbun, L., & Birrer, M. J. (2012). Identification of a potential ovarian cancer stem cell gene expression profile from advanced stage papillary serous ovarian cancer. PLoS ONE, 7, e29079
Kuroda, T., Hirohashi, Y., Torigoe, T., Yasuda, K., Takahashi, A., Asanuma, H., Morita, R., Mariya, T., Asano, T., Mizuuchi, M., Saito, T., & Sato, N. (2013). ALDH1-high ovarian cancer stem-like cells can be isolated from serous and clear cell adenocarcinoma cells, and ALDH1 high expression is associated with poor prognosis. PLoS ONE, 8, e65158
Scaffiffiffidi, P., & Misteli, T. (2011). In vitro generation of human cells with cancer stem cell properties. Nature Cell Biology, 13, 1051–1061.
Kao, C. Y., Oakley, C. S., Welsch, C. W., & Chang, C. C. (1997). Growth requirements and neoplastic transformation of two types of normal human breast epithelial cells derived from reduction mammoplasty. Cellular & Developmental Biology - Animal, 33, 282–288.
Al-Hajj, M., Wicha, M. S., Benito-Hernandez, A., Morrison, S. J., & Clarke, M. F. (2003). Prospective identifification of tumorigenic breast cancer cells. Proceedings of the National Academy of Sciences of the United States of America, 100, 3983–3988.
Singh, S. K., Clarke, I. D., Terasaki, M., Bonn, V. E., Hawkins, C., Squire, J., & Dirks, P. B. (2003). Identifification of a cancer stem cell in human brain tumors. Cancer Research, 63, 5821–5828.
Charafe-Jauffffret, E., Ginestier, C., Iovino, F., Wicinski, J., Cervera, N., Finetti, P., Hur, M. H., Diebel, M. E., Monville, F., & Dutcher, J., et al. (2009). Breast cancer cell lines contain functional cancer stem cells with metastatic capacity and a distinct molecular signature. Cancer Research, 69, 1302–1313.
Chang, Y., Wu, K., & Ding, D. (2021). The natural compound n-butylidenephthalide kills high-grade serous ovarian cancer stem cells by activating intrinsic apoptosis signaling pathways. Journal of Cancer, 12(11), 3126–3135.
Cannistra, S. A., DeFranzo, B., Niloff, J., & Ottensmeir, C. (1995). Functional heterogeneity of CD44 molecules in ovarian cancer cell lines. Clinical Cancer Research, 1, 333–342.
Ferrandina, G., Bonanno, G., Pierelli, L., Perillo, A., Procoli, A., & Mariotti, A., et al. (2008). Expression of CD133-1 and CD133-2 in ovarian cancer. International Journal of Gynecological Cancer, 18, 506–514.
Zhang, S., Balch, C., Chan, M. W., Lai, H. C., Matei, D., & Schilder, J. M., et al. (2008). Identification and characterization of ovarian cancer-initiating cells from primary human tumors. Cancer Research, 68, 4311–4320.
Curley, M. D., Therrien, V. A., Cummings, C. L., Sergent, P. A., Koulouris, C. R., & Friel, A. M., et al. (2009). CD133 expression defines a tumor initiating cell population in primary human ovarian cancer. Stem Cells, 27, 2875–2883.
Gao, M. Q., Choi, Y. P., Kang, S., Youn, J. H., & Cho, N. H. (2010). CD24+ cells from hierarchically organized ovarian cancer are enriched in cancer stem cells. Oncogene, 29, 2672–2680.
Koren, E., & Fuchs, Y. (2016). The bad seed: Cancer stem cells in tumor development and resistance. Drug Resistance Updates, 28, 1–12.
Thakur, B., & Ray, P. (2017). Cisplatin triggers cancer stem cell enrichment in platinumresistant cells through NF-κB-TNFα-PIK3CA loop. Journal of Experimental & Clinical Cancer Research, 36(1), 164.
Kaushik, N. K., Kaushik, N., Yoo, K. C., Uddin, N., Kim, J. S., Lee, S. J., & Choi, E. H. (2016). Low doses of PEG-coated gold nanoparticles sensitize solid tumors to cold plasma by blocking the PI3K/AKT-driven signaling axis to suppress cellular transformation by inhibiting growth and EMT. Biomaterials, 87, 118–130.
Mani, S. A., Guo, W., Liao, M.-J., Eaton, E. N., Ayyanan, A., Zhou, A. Y., Brooks, M., Reinhard, F., Zhang, C. C., & Shipitsin, M., et al. (2008). The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell, 133, 704–715.
Gupta, P. B., Önder, T., Jiang, G., Tao, K., Kuperwasser, C., Weinberg, R. A., & Lander, E. S. (2009). Identifification of selective inhibitors of cancer stem cells by high-throughput screening. Cell, 138, 645–659.
Li, N., & Zhan, X. (2019). Identification of clinical trait–related lncRNA and mRNA biomarkers with weighted gene co-expression network analysis as useful tool for personalized medicine in ovarian cancer. EPMA Journal, 10, 273–290.
Latifi, A., Luwor, R. B., Bilandzic, M., Nazaretian, S., Stenvers, K., Pyman, J., Zhu, H., Thompson, E. W., Quinn, M. A., Findlay, J. K., & Ahmed, N. (2012). Isolation and characterization of tumor cells from the ascites of ovarian cancer patients: molecular phenotype of chemoresistant ovarian tumors. PLoS ONE, 7(10), e46858 https://doi.org/10.1371/journal.pone.0046858.
Tan, D. S., Agarwal, R., & Kaye, S. B. (2006). Mechanisms of transcoelomic metastasis in ovarian cancer. The Lancet Oncology, 7(11), 925–934. https://doi.org/10.1016/S1470-2045(06)70939-1.
Kaku, T., Ogawa, S., Kawano, Y., Ohishi, Y., Kobayashi, H., Hirakawa, T., & Nakano, H. (2003). Histological classifification of ovarian cancer. Medical Electron Microscopy, 36, 9–17.
Baba, T., Convery, P. A., Matsumura, N., Whitaker, R. S., Kondoh, E., Perry, T., Huang, Z., Bentley, R. C., Mori, S., & Fujii, S., et al. (2009). Epigenetic regulation of CD133 and tumorigenicity of CD133+ ovarian cancer cells. Oncogene, 28, 209–218.
Yu, S., Mulero, M. C., Chen, W., Shang, X., Tian, S., Watanabe, J., Watanabe, A., Vorberg, T., Wong, C., & Gately, D., et al. (2021). Therapeutic targeting of tumor cells rich in LGR stem cell receptors. Bioconjugate Chemistry, 32, 376–384.
Landen, Jr, C. N., Goodman, B., Katre, A. A., Steg, A. D., Nick, A. M., Stone, R. L., Miller, L. D., Mejia, P. V., Jennings, N. B., & Gershenson, D. M., et al. (2010). Targeting aldehyde dehydrogenase cancer stem cells in ovarian cancer. Molecular Cancer Therapeutics, 9, 3186–3199.
Avila-Carrasco, L., Majano, P., & Sánchez-Toméro, J. A., et al. (2019). Natural plants compounds as modulators of epithelial-to-mesenchymal transition. Frontiers in Pharmacology, 10, 715 https://doi.org/10.3389/fphar.2019.00715.
Liu C. L., Chen Y. J., Fan M. H., et al. (2020) Characteristics of CD133-sustained chemoresistant cancer stem-like cells in human ovarian carcinoma. International Journal of Molecular Sciences, 21(18):6467.
Zhang, J., Yuan, B., Zhang, H., & Li, H. (2019). Human epithelial ovarian cancer cells expressing CD105, CD44 and CD106 surface markers exhibit increased invasive capacity and drug resistance. Oncology Letters, 17(6), 5351–5360. https://doi.org/10.3892/ol.2019.10221.
Fan, Q., Zhang, W., & Emerson, R. E., et al. (2020). ZIP4 Is a novel cancer stem cell marker in high-grade serous ovarian cancer. Cancers, 12(12), 3692.
Salem, M. L., El-Badawy, A. S., & Li, Z. (2014). Immunobiology and signaling pathways of cancer stem cells: Implication for cancer therapy. Cytotechnology, 67, 749–759.
Takebe, N., Miele, L., Harris, P. J., Jeong, W., Bando, H., Kahn, M. G., Yang, S. X., & Ivy, S. P. (2015). Targeting Notch, Hedgehog, and Wnt pathways in cancer stem cells: Clinical update. Nature Reviews Clinical Oncology, 12, 445–464.
Jin, X., Jin, X., & Kim, H. (2017). Cancer stem cells and differentiation therapy. Tumour Biology, 39, 1010428317729933.
Hanahan, D., & Coussens, L. M. (2012). Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell, 21, 309–322.
Fessler E., Dijkgraaf F. E., De Sousa E. M. F., Medema J. P., (2013) Cancer Letters. 341,97–104.
Li, Y., & Laterra, J. (2012). Cancer stem cells: distinct entities or dynamically regulated phenotypes? Cancer Research, 72, 576–580.
Kim, D. K., Kim, Y. N., Kim, Y. E., Lee, S. Y., Shin, M. J., Do, E. K., Choi, K. U., Kim, S. C., Kim, K. H., Suh, D. S., Song, P., & Kim, J. H. (2021). TRIB2 stimulates cancer stem-like properties through activating the AKT-GSK3β-β-catenin signaling axis. Molecular Cell, 44(7), 481–492. https://doi.org/10.14348/molcells.2021.0030.
Muñoz-Galván, S., Felipe-Abrio, B., García-Carrasco, M., Domínguez-Piñol, J., Suarez-Martinez, E., Verdugo-Sivianes, E. M., Espinosa-Sánchez, A., Navas, L. E., Otero-Albiol, D., Marin, J. J., Jiménez-García, M. P., García-Heredia, J. M., Quiroga, A. G., Estevez-Garcia, P., & Carnero, A. (2019). New markers for human ovarian cancer that link platinum resistance to the cancer stem cell phenotype and define new therapeutic combinations and diagnostic tools. Journal of Experimental & Clinical Cancer Research, 38(1), 234 https://doi.org/10.1186/s13046-019-1245-5.
Cho, J. G., Kim, S. W., Lee, A., Jeong, H. N., Yun, E., Choi, J., Jeong, S. J., Chang, W., Oh, S., Yoo, K. H., Lee, J. B., Yoon, S., Lee, M. S., Park, J. H., Jung, M. H., Kim, S. W., Kim, K. H., Suh, D. S., Choi, K. U., Choi, J., Kim, J., & Kwon, B. S. (2022). MicroRNA-dependent inhibition of WEE1 controls cancer stem-like characteristics and malignant behavior in ovarian cancer. Molecular Therapy-Nucleic Acids, 29, 803–822. https://doi.org/10.1016/j.omtn.2022.08.028.
Steg, A. D., Bevis, K. S., Katre, A. A., Ziebarth, A., Alvarez, R. D., & Zhang, K., et al. (2012). Stem cell pathway contribute to clinical chemoresistance in ovarian cancer. Clinical Cancer Research, 1, 869–881.
The Cancer Genomic Atlas Research Network. (2011). Integrated genomic analysis of ovarian carcinoma. Nature, 474, 609–615.
Eyvani, V., Farshchian, M., Esmaeili, S. A., Hadi, Y., Moghbeli, M., Nezhad, S.-R. K., & Abbaszadegan, M. R. (2019). Ovarian cancer stem cells and targeted therapy. Journal of Ovarian Research, 12, 120.
Zhang, L., Ma, R., Gao, M., Zhao, Y., Lv, X., Zhu, W., Han, L., Su, P., Fan, Y., Yan, Y., Zhao, L., Ma, H., Wei, M., & He, M. (2020). SNORA72 Activates the Notch1/c-Myc pathway to promote stemness transformation of ovarian cancer cells. Frontiers in Cell and Developmental Biology, 8, 583087 https://doi.org/10.3389/fcell.2020.583087.
Islam, S. S., & Aboussekhra, A. (2019). Sequential combination of cisplatin with eugenol targets ovarian cancer stem cells through the Notch-Hes1 signalling pathway. Journal of Experimental, Clinical Cancer Research : CR, 38, 382.
Huang, M. Y., Wang, H. M., Chang, H. J., Hsiao, C. P., Wang, J. Y., & Lin, S. R. (2012). Overexpression of S100B, TM4SF4, and OLFM4 genes is correlated with liver metastasis in Taiwanese colorectal cancer patients. DNA and Cell Biology, 31, 43–49.
Yang, T., Cheng, J., Yang, Y., Qi, W., Zhao, Y., Long, H., Xie, R., & Zhu, B. (2017). S100B mediates stemness of ovarian cancer stem-like cells through inhibiting p53. Stem Cells, 35, 325–336.
Yang, T., Cheng, J., You, J., Yan, B., Liu, H., & Li, F. (2018). S100B promotes chemoresistance in ovarian cancer stem cells by regulating p53. Oncology Reports, 40(3), 1574–1582. https://doi.org/10.3892/or.2018.6527.
Markowitz, J., & MacKerell, A. D. (2007). Jr and Weber DJ: A search for inhibitors of S100B, a member of the S100 family of calcium-binding proteins. Mini-Reviews in Medicinal Chemistry, 7, 609–616.
Wang H., Chirshev E., Hojo N., et al. (2021) The Epithelial-mesenchymal transcription factor SNAI1 represses transcription of the tumor suppressor miRNA let-7 in cancer. Cancers, 13(6):1469.
Chen, Q., Dong, R., & Chen, P. (2019). Extracts of the medicinal plants Pao Pereira and Rauwolfia vomitoria inhibit ovarian cancer stem cells in vitro. The FASEB Journal, 33(S1), 15347354221123019.
Li, H., Zhang, W., Niu, C., Lin, C., Wu, X., Jian, Y., Li, Y., Ye, L., Dai, Y., Ouyang, Y., Chen, J., Qiu, J., Song, L., & Zhang, Y. (2019). Nuclear orphan receptor NR2F6 confers cisplatin resistance in epithelial ovarian cancer cells by activating the Notch3 signaling pathway. International Journal of Cancer, 145, 1921–1934.
Guan, X. Y., Sham, J. S., Tang, T. C., Fang, Y., Huo, K. K., & Yang, J. M. (2001). Isolation of a novel candidate oncogene within a frequently amplified region at 3q26 in ovarian cancer. Cancer Research, 61, 3806–3809.
Cao, T. T., Lin, S. H., Fu, L., Tang, Z., Che, C. M., & Guan, X. Y., et al. (2017). Eukaryotic translation initiation factor 5A2 promotes metabolic reprogramming in hepatocellular carcinoma cells. Carcinogenesis, 38, 94–104.
Wang, K., Wang, Y., & Wang, Y., et al. (2021). EIF5A2 enhances stemness of epithelial ovarian cancer cells via a E2F1/KLF4 axis[J]. Stem Cell Research & Therapy, 12(1), 186.
Li, Y., Wang, D., & Liu, J., et al. (2020). BaicaliN Attenuates YAP activity to suppress ovarian cancer stemness. OncoTargets and Therapy, 13, 7151–7163.
Yan, Z., Jin, Z., & Sui, H., et al. (2022). Bruceine D sensitizes human ovarian cancer cells to paclitaxel through JNK and STAT3 signal regulation. Revista Brasileira de Farmacognosia, 32(2), 257–265.
He, Y., Alejo, S., Venkata, P. P., Johnson, J. D., Loeffel, I., Pratap, U. P., Zou, Y., Lai, Z., Tekmal, R. R., Kost, E. R., & Sareddy, G. R. (2022). Therapeutic targeting of ovarian cancer stem cells using estrogen receptor beta agonist. International Journal of Molecular Sciences, 23(13), 7159 https://doi.org/10.3390/ijms23137159.
Campbell, I. G., Russell, S. E., Choong, D. Y. H., Montgomery, K. G., Ciavarella, M. L., Hooi, C. S. F., Cristiano, B. E., Pearson, R. B., & Phillips, W. A. (2004). Mutation of the PIK3CA gene in ovarian and breast cancer. Cancer Research, 64, 7678–7681.
Ma, J., Kala, S., & Yung, S., et al. (2018). Blocking stemness and metastatic properties of ovarian cancer cells by targeting p70S6K with dendrimer nanovector-based siRNA delivery. Molecular Therapy, 26(1), 70–83.
Huang, R., Zhu, L., & Zhang, Y. (2020). XIST lost induces ovarian cancer stem cells to acquire taxol resistance via a KMT2C-dependent way. Cancer Cell Internationalernational, 20(1), 436.
Holmberg, R., Robinson, M., Gilbert, S. F., Lujano-Olazaba, O., Waters, J. A., Kogan, E., Velasquez, C. L. R., Stevenson, D., Cruz, L. S., Alexander, L. J., Lara, J., Mu, E. M., Camillo, J. R., Bitler, B. G., Huxford, T., & House, C. D. (2023). TWEAK-Fn14-RelB signaling cascade promotes stem cell-like features that contribute to post-chemotherapy ovarian cancer relapse. Molecular Cancer Research, 21(2), 170–186. https://doi.org/10.1158/1541-7786.MCR-22-0486.
Srivastava, A. K., Rizvi, A., Cui, T., Han, C., Banerjee, A., Naseem, I., Zheng, Y., Wani, A. A., & Wang, Q. E. (2018). Depleting ovarian cancer stem cells with calcitriol. Oncotarget, 9(18), 14481–14491. https://doi.org/10.18632/oncotarget.24520.
Ji, M., Liu, L., Hou, Y., & Li, B. (2019). 1α,25-Dihydroxyvitamin D3 restrains stem cell-like properties of ovarian cancer cells by enhancing vitamin D receptor and suppressing CD44. Oncology Reports, 41(6), 3393–3403. https://doi.org/10.3892/or.2019.7116.
Chan, E., Luwor, R., Burns, C., Kannourakis, G., Findlay, J. K., & Ahmed, N. (2018). Momelotinib decreased cancer stem cell associated tumor burden and prolonged disease-free remission period in a mouse model of human ovarian cancer. Oncotarget, 9(24), 16599–16618. https://doi.org/10.18632/oncotarget.24615.
Yanai, K., Nagai, S., Wada, J., Yamanaka, N., Nakamura, M., & Torata, N., et al. (2007). Hedgehog signaling pathway is a possible therapeutic target for gastric cancer. Journal of Surgical Oncology, 95, 55–62.
Zhao, Y., He, M., Cui, L., Gao, M., Zhang, M., Yue, F., Shi, T., Yang, X., Pan, Y. & Zheng, X. et al.(2020). Chemotherapy exacerbates ovarian cancer cell migration and cancer stem cell-like characteristics through GLI1. British Journal of Cancer, 122, 1638–1648.
Leung, Y. K., Mak, P., Hassan, S., & Ho, S. M. (2006). Estrogen receptor (ER)-beta isoforms: a key to understanding ER-beta signaling. Proceedings of the National Academy of Sciences of the United States of America, 103(35), 13162–13167.
Bossard, C., Busson, M., Vindrieux, D., Gaudin, F., Machelon, V., Brigitte, M., Jacquard, C., Pillon, A., Balaguer, P., & Balabanian, K., et al. (2012). Potential role of estrogen receptor beta as a tumor suppressor of epithelial ovarian cancer. PLoS ONE, 7(9), e44787.
Chan, K. K. L., Siu, M. K. Y., Jiang, Y. X., Wang, J. J., Leung, T. H. Y., & Ngan, H. Y. S. (2018). Estrogen receptor modulators genistein, daidzein and ERB-041 inhibit cell migration, invasion, proliferation and sphere formation via modulation of FAK and PI3K/AKT signaling in ovarian cancer. Cancer Cell International, 18, 65 https://doi.org/10.1186/s12935-018-0559-2.
Wen, H., Qian, M., He, J., Li, M., Yu, Q., & Leng, Z. (2020). Inhibiting of self-renewal, migration and invasion of ovarian cancer stem cells by blocking TGF-β pathway. PLoS ONE, 15(3), e0230230 https://doi.org/10.1371/journal.pone.0230230.
Zhang, Y., Chen, S., Wei, C., Rankin, G. O., Ye, X., & Chen, Y. C. (2018). Dietary compound proanthocyanidins from Chinese bayberry (Myrica rubra Sieb. et Zucc.) leaves attenuate chemotherapy-resistant ovarian cancer stem cell traits via targeting the Wnt/β-catenin signaling pathway and inducing G1 cell cycle arrest. Food & Function, 9(1), 525–533. https://doi.org/10.1039/c7fo01453h.
Fang, C. H., Lin, Y. T., Liang, C. M., & Liang, S. M. (2020). A novel c-Kit/phospho-prohibitin axis enhances ovarian cancer stemness and chemoresistance via Notch3-PBX1 and β-catenin-ABCG2 signaling. Journal of Biomedical Science, 27(1), 42 https://doi.org/10.1186/s12929-020-00638-x.
Zhang, K., Ying, H., Zhao, R., Chen, Y., & Deng, Q. (2021). Capilliposide from Lysimachia capillipes promotes terminal differentiations and reverses paclitaxel resistance in A2780T cells of human ovarian cancer by regulating Fos/Jun pathway. Chinese Herbal Medicines, 14(1), 111–116. https://doi.org/10.1016/j.chmed.2021.09.009.
Jiang, Y. X., Siu, M. K. Y., Wang, J. J., Leung, T. H. Y., Chan, D. W., Cheung, A. N. Y., Ngan, H. Y. S., & Chan, K. K. L. (2022). PFKFB3 regulates chemoresistance, metastasis and stemness via IAP proteins and the NF-κB signaling pathway in ovarian cancer. Frontiers in Oncology, 12, 748403 https://doi.org/10.3389/fonc.2022.748403.
Muñoz-Galván, S., Felipe-Abrio, B., Verdugo-Sivianes, E. M., Perez, M., Jiménez-García, M. P., Suarez-Martinez, E., Estevez-Garcia, P., & Carnero, A. (2020). Downregulation of MYPT1 increases tumor resistance in ovarian cancer by targeting the Hippo pathway and increasing the stemness. Molecular Cancer, 19(1), 7 https://doi.org/10.1186/s12943-020-1130-z.
Li, X., Wang, J., Wu, W., Gao, H., Liu, N., Zhan, G., Li, L., Han, L. & Guo, X. (2020). Myeloid-derived suppressor cells promote epithelial ovarian cancer cell stemness by inducing the CSF2/p-STAT3 signalling pathway. FEBS Journal, 287(23), 5218–5235. https://doi.org/10.1111/febs.15311.
Wang, S., Li, Z., Zhu, G., Hong, L., Hu, C., Wang, K., Cui, K., & Hao, C. (2021). RNA-binding protein IGF2BP2 enhances circ_0000745 abundancy and promotes aggressiveness and stemness of ovarian cancer cells via the microRNA-3187-3p/ERBB4/PI3K/AKT axis. Journal of Ovarian Research, 14(1), 154 https://doi.org/10.1186/s13048-021-00917-7.
He, M., Wu, H., Jiang, Q., Liu, Y., Han, L., Yan, Y., Wei, B., Liu, F., Deng, X., Chen, H., Zhao, L., Wang, M., Wu, X., Yao, W., Zhao, H., Chen, J. & Wei, M. (2019). Hypoxia-inducible factor-2α directly promotes BCRP expression and mediates the resistance of ovarian cancer stem cells to adriamycin. Molecular Oncology, 13(2), 403–421. https://doi.org/10.1002/1878-0261.12419.
Muralikrishnan, V., Hurley, T. D., & Nephew, K. P. (2020). Targeting aldehyde dehydrogenases to eliminate cancer stem cells in gynecologic malignancies. Cancers, 12, 961.
Kaipio, K., Chen, P., Roering, P., Huhtinen, K., Mikkonen, P., Ostling, P., Lehtinen, L., Mansuri, N., Korpela, T., & Potdar, S., et al. (2020). ALDH1A1-related stemness in high-grade serous ovarian cancer is a negative prognostic indicator but potentially targetable by EGFR/mTOR-PI3K/aurora kinase inhibitors. The Journal of Pathology, 250, 159–169.
Liu, L., Cai, S., Han, C., Banerjee, A., Wu, D., Cui, T., Xie, G., Zhang, J., Zhang, X., & McLaughlin, E., et al. (2020). ALDH1A1 Contributes to PARP inhibitor resistance via enhancing DNA repair in BRCA2(−/−) ovarian cancer cells. Molecular Cancer Therapeutics, 19, 199–210.
Nwani, N. G., Condello, S., Wang, Y., Swetzig, W. M., Barber, E., Hurley, T., & Matei, D. (2019). A novel ALDH1A1 inhibitor targets cells with stem cell characteristics in ovarian cancer. Cancers, 11(4), 502 https://doi.org/10.3390/cancers11040502.
Cui, T., Srivastava, A. K., Han, C., Wu, D., Wani, N., Liu, L., Gao, Z., Qu, M., Zou, N., Zhang, X., Yi, P., Yu, J., Bell, E. H., Yang, S. M., Maloney, D. J., Zheng, Y., Wani, A. A., & Wang, Q. E. (2018). DDB2 represses ovarian cancer cell dedifferentiation by suppressing ALDH1A1. Cell Death & Disease, 9(5), 561 https://doi.org/10.1038/s41419-018-0585-y.
Muralikrishnan, V., Fang, F., Given, T. C., Podicheti, R., Chtcherbinine, M., Metcalfe, T. X., Sriramkumar, S., O’Hagan, H. M., Hurley, T. D., & Nephew, K. P. (2022). A Novel ALDH1A1 inhibitor blocks platinum-induced senescence and stemness in ovarian cancer. Cancers, 14(14), 3437 https://doi.org/10.3390/cancers14143437.
Fang, G. A., Zhi, Y. A., & Hk, A., et al. (2019). Inhibitory effect on ovarian cancer ALDH+ stem-like cells by Disulfiram and Copper treatment through ALDH and ROS modulation. Biomedicine & Pharmacotherapy, 118, 109371–109371.
Guo, F., Yang, Z., Sehouli, J., & Kaufmann, A. M. (2022). Blockade of ALDH in cisplatin-resistant ovarian cancer stem cells in vitro synergistically enhances chemotherapy-induced cell death. Current Oncology, 29(4), 2808–2822. https://doi.org/10.3390/curroncol29040229.
Whitworth, J. M., et al. (2012). The impact of novel retinoids in combination with platinum chemotherapy on ovarian cancer stem cells. Gynecologic Oncology, 125, 226–230.
Kim, D., Choi, B. H., Ryoo, I. G., & Kwak, M. K. (2018). High NRF2 level mediates cancer stem cell-like properties of aldehyde dehydrogenase (ALDH)-high ovarian cancer cells: inhibitory role of all-trans retinoic acid in ALDH/NRF2 signaling. Cell Death & Disease, 9(9), 896 https://doi.org/10.1038/s41419-018-0903-4.
Lee, H., Kwon, O. B., & Lee, J. E., et al. (2021). Repositioning trimebutine maleate as a cancer treatment targeting ovarian cancer stem cells. Cells, 10(4), 918.
Lee H., Kim J. W., Lee D. S., et al. (2020) Combined poziotinib with manidipine treatment suppresses ovarian cancer stem-cell proliferation and stemness. International Journal of Molecular Sciences, 21(19):7379.
Zhang, Q., Wang, J., Qiao, H., Huyan, L., Liu, B., Li, C., Jiang, J., Zhao, F., Wang, H. & Yan, J. (2021). ISG15 is downregulated by KLF12 and implicated in maintenance of cancer stem cell‐like features in cisplatin‐resistant ovarian cancer. Journal of Cellular and Molecular Medicine, 25(9), 4395–4407. https://doi.org/10.1111/jcmm.16503.
Sohn, E. J. (2022). PIK3R3, a regulatory subunit of PI3K, modulates ovarian cancer stem cells and ovarian cancer development and progression by integrative analysis. BMC Cancer, 22(1), 708.
Lokman, N. A., Price, Z. K., & Hawkins, E. K., et al. (2019). 4-Methylumbelliferone inhibits cancer stem cell activation and overcomes chemoresistance in ovarian cancer. Cancers, 11(8), 1187.
Kristen, S., Linah, A. A., & Eavarone, D. A., et al. (2018). Treatment of ovarian cancer by targeting the tumor stem cell-associated carbohydrate antigen, Sialyl-Thomsen-nouveau. Oncotarget, 9(33), 23289.
Shan, L., Song, P., & Zhao, Y., et al. (2022). miR-600 promotes ovarian cancer cells stemness, proliferation and metastasis via targeting KLF9. Journal of Ovarian Research, 15, 52.
Chirshev, E., Suzuki, T., & Wang, H., et al. (2021). Let-7i reduces aggressive phenotype and induces BRCAness in ovarian cancer cells. Cancers, 13(18), 4617.
Wu, Y., Wang, T., Xia, L., & Zhang, M. (2021). LncRNA WDFY3-AS2 promotes cisplatin resistance and the cancer stem cell in ovarian cancer by regulating hsa-miR-139-5p/SDC4 axis. Cancer Cell International, 21(1), 284 https://doi.org/10.1186/s12935-021-01993-x.
Cheng, F. H. C., Lin, H. Y., Hwang, T. W., Chen, Y. C., Huang, R. L., Chang, C. B., Yang, W., Lin, R. I., Lin, C. W., Chen, G. C. W., Mai, S. Y., Lin, J. M. J., Chuang, Y. M., Chou, J. L., Kuo, L. W., Li, C., Cheng, A. S. L., Lai, H. C., Wu, S. F., Tsai, J. C. & & Chan, M. W. Y. (2019). E2F6 functions as a competing endogenous RNA, and transcriptional repressor, to promote ovarian cancer stemness. Cancer Science, 110(3), 1085–1095. https://doi.org/10.1111/cas.13920.
Khalil, A. M., Guttman, M., & Huarte, M., et al. (2009). Many human large intergenic noncoding RNAs associate with chromatin-modifying complexes and affect gene expression. Proceedings of the National Academy of Sciences of the United States of America, 106, 11667–11672. https://doi.org/10.1073/pnas.0904715106.
Zhan, F. L., Chen, C. F. & Yao, M. Z. (2020). LncRNA TUG1 facilitates proliferation, invasion and stemness of ovarian cancer cell via miR-186-5p/ZEB1 axis. Cell Biochemistry & Function, 38(8), 1069–1078. https://doi.org/10.1002/cbf.3544.
Shanshan, Yongfang, & Yue, et al. (2018). STON2 negatively modulates stem-like properties in ovarian cancer cells via DNMT1/MUC1 pathway. Journal of Experimental & Clinical Cancer Research: CR, 37, 305.
Piccirillo, S., Reynolds, B. A., Zanetti, N., Lamorte, G., Binda, E., & Broggi, G., et al. (2006). Bone morphogenetic proteins inhibit the tumorigenic potential of human brain tumour-initiating cells. Nature, 444(7120), 761–765. https://doi.org/10.1038/nature05349.
Yan, Y., Li, Z., Xu, X., Chen, C., Wei, W., & Fan, M., et al. (2016). All-trans retinoic acids induce differentiation and sensitize a radioresistant breast cancer cells to chemotherapy. BMC Complementary and Alternative Medicine, 16(1), 1–11. https://doi.org/10.1186/s12906-016-1088-y.
Yang, R., Liu, B., Yang, M., Xu, F., Wu, S., & Zhao, S. (2022). Lumiflavin reduces cisplatin resistance in cancer stem-like cells of OVCAR-3 cell line by inducing differentiation. Frontiers in Oncology, 12, 859275 https://doi.org/10.3389/fonc.2022.859275.
Chang, C., Lee, S. O., Yeh, S., & Chang, T. M. (2014). Androgen receptor (AR) differential roles in hormone-related tumors including prostate, bladder, kidney, lung, breast and liver. Oncogene, 33(25), 3225–3234.
Proverbs-Singh, T., Feldman, J. L., Morris, M. J., Autio, K. A., & Traina, T. A. (2015). Targeting the androgen receptor in prostate and breast cancer: several new agents in development. Endocrine-Related Cancer, 22(3), R87–r106.
Gruessner, C., Gruessner, A., Glaser, K., AbuShahin, N., Zhou, Y., Laughren, C., Wright, H., Pinkerton, S., Yi, X., & Stoffer, J., et al. (2014). Flutamide and biomarkers in women at high risk for ovarian cancer: preclinical and clinical evidence. Cancer Prevention Research, 7(9), 896–905.
Zhu, H., Zhu, X., Zheng, L., Hu, X., Sun, L., & Zhu, X. (2017). The role of the androgen receptor in ovarian cancer carcinogenesis and its clinical implications. Oncotarget, 8(17), 29395–29405.
Jonsson, J. M., Skovbjerg Arildsen, N., Malander, S., Masback, A., Hartman, L., Nilbert, M., & Hedenfalk, I. (2015). Sex steroid hormone receptor expression affects ovarian Cancer survival. Translational Oncology, 8(5), 424–433.
Ling, K., Jiang, L., & Liang, S., et al. (2018). Nanog interaction with the androgen receptor signaling axis induce ovarian cancer stem cell regulation: studies based on the CRISPR/Cas9 system. Journal of Ovarian Research, 11(1), 1–16.
Naujokat, C., Fuchs, D., & Opelz, G. J. (2010). Salinomycin in cancer: a new mission for an old agent. Molecular Medicine Reports, 3(4), 555–559. https://doi.org/10.3892/mmr_00000296.
An, H., Kim, J. Y., Lee, N., Cho, Y., Oh, E., & Seo, J. H. (2015). Salinomycin possesses anti-tumor activity and inhibits breast cancer stem-like cells via an apoptosis-independent pathway. Biochemical and Biophysical Research Communications, 466(4), 696–703. https://doi.org/10.1016/j.bbrc.2015.09.108.
Lee, H. G., Shin, S. J., & Chung, H. W., et al. (2017). Salinomycin reduces stemness and induces apoptosis on human ovarian cancer stem cell. Journal Gynecologic Oncology, 28(2), e14 https://doi.org/10.3802/jgo.2017.28.e14.
Mao, J., Fan, S., & Ma, W., et al. (2014). Roles of Wnt/beta-catenin signaling in the gastric cancer stem cells proliferation and salinomycin treatment. Cell Death & Disease, 5, e1039 https://doi.org/10.1038/cddis.2013.515.
Zou, M., Yin, X., Zhou, X., Niu, X., Wang, Y., & Su, M. (2022). Salinomycin-loaded high-density lipoprotein exerts promising anti-ovarian cancer effects by inhibiting epithelial-mesenchymal transition. International Journal of Nanomedicine, 17, 4059–4071. https://doi.org/10.2147/IJN.S380598.
Lee, Y. J., Kim, S. W., Jung, M. H., Kim, Y. S., Kim, K. S., Suh, D. S., Kim, K. H., Choi, E. H., Kim, J., & Kwon, B. S. (2022). Plasma-activated medium inhibits cancer stem cell-like properties and exhibits a synergistic effect in combination with cisplatin in ovarian cancer. Free Radical Biology & Medicine, 182, 276–288. https://doi.org/10.1016/j.freeradbiomed.2022.03.001.
Coward, J. I., Barve, M. A., Kichenadasse, G., Moore, K. N., Harnett, P. R., Berg, D., Garner, J. S., & Dizon, D. S. (2021). Maximum tolerated dose and anti-tumor activity of intraperitoneal cantrixil (TRX-E-002-1) in patients with persistent or recurrent ovarian cancer, fallopian tube cancer, or primary peritoneal cancer: phase I study results. Cancers, 13(13), 3196 https://doi.org/10.3390/cancers13133196.
Ohsawa, I., Ishikawa, M., & Takahashi, K., et al. (2007). Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nature Medicine, 13, 688–694.
Ohta, S. (2014). Molecular hydrogen as a preventive and therapeutic medical gas: initiation, development and potential of hydrogen medicine. Pharmacology & Therapeutics, 144, 1–11.
Lei, S., Fei, X., & Li, J., et al. (2018). Therapeutic potential of molecular hydrogen in ovarian cancer. Translational Cancer Research, 7(4), 988–995.
Feng, X., Li, L., Wang, L., Luo, S., & Bai, X. (2019). Chromatin target of protein arginine methyltransferase regulates invasion, chemoresistance, and stemness in epithelial ovarian cancer. Bioscience Reports, 39(4), BSR20190016 https://doi.org/10.1042/BSR20190016.
Lee, J. S., Choi, Y. D., Lee, J. H., Nam, J. H., Choi, C., & Lee, M. C., et al. (2006). Expression of cyclooxygenase-2 in epithelial ovarian tumors and its relation to vascular endothelial growth factor and p53 expression. International Journal of Gynecological Cancer, 16(Suppl 1), 247–253.
Wen, Z., Liu, H., Li, M., Li, B., Gao, W., & Shao, Q., et al. (2015). Increased metabolites of 5-lipoxygenase from hypoxic ovarian cancer cells promote tumorassociated macrophage infifiltration. Oncogene, 34, 1241–1252.
Hirst, J., Pathak, H. B., Hyter, S., Pessetto, Z. Y., Ly, T., Graw, S., Koestler, D. C., Krieg, A. J., Roby, K. F. & Godwin, A. K. (2018). Licofelone enhances the efficacy of paclitaxel in ovarian cancer by reversing drug resistance and tumor stem-like properties. Cancer Research, 78(15), 4370–4385. https://doi.org/10.1158/0008-5472.CAN-17-3993.
Nacarelli, T., Fukumoto, T., Zundell, J. A., Fatkhutdinov, N., Jean, S., Cadungog, M. G., Borowsky, M. E., & Zhang, R. (2020). NAMPT Inhibition suppresses cancer stem-like cells associated with therapy-induced senescence in ovarian cancer. Cancer Research, 80(4), 890–900. https://doi.org/10.1158/0008-5472.CAN-19-2830.
Kapur, A., Mehta, P., Simmons, A. D., Ericksen, S. S., Mehta, G., Palecek, S. P., Felder, M., Stenerson, Z., Nayak, A., Dominguez, J. M. A., Patankar, M., & Barroilhet, L. M. (2022). Atovaquone: An inhibitor of oxidative phosphorylation as studied in gynecologic cancers. Cancers, 14(9), 2297 https://doi.org/10.3390/cancers14092297.
Li, X., Liu, Y., & Wang, N., et al. (2019). Synthesis and discovery of 18β-glycyrrhetinic acid derivatives inhibiting cancer stem cell properties in ovarian cancer cells. RSC Advances, 9, 27294–27304.
Lupia, M., & Cavallaro, U. (2017). Ovarian cancer stem cells: still an elusive entity? Molecular Cancer, 16(1), 64.
Sriramkumar, S., Sood, R., Huntington, T. D., Ghobashi, A. H., Vuong, T. T., Metcalfe, T. X., Wang, W., Nephew, K. P., & O’Hagan, H. M. (2022). Platinum-induced mitochondrial OXPHOS contributes to cancer stem cell enrichment in ovarian cancer. Journal of Translational Medicine, 20(1), 246 https://doi.org/10.1186/s12967-022-03447-y.
Zhao, E., Maj, T., & Kryczek, I., et al. (2016). Cancer mediates effector T cell dysfunction by targeting microRNAs and EZH2 via glycolysis restriction. Nature Immunology, 17(1), 95–103.
Wojtowicz, K., Sterzyńska, K., Świerczewska, M., Nowicki, M., Zabel, M., & Januchowski, R. (2021). Piperine targets different drug resistance mechanisms in human ovarian cancer cell lines leading to increased sensitivity to cytotoxic drugs. International Journal of Molecular Sciences, 22(8), 4243 https://doi.org/10.3390/ijms22084243.
Simpkins, F., Hevia-Paez, P., Sun, J., Ullmer, W., Gilbert, C. A., & da Silva, T., et al. (2012). Src inhibition with saracatinib reverses fulvestrant resistance in ERpositive ovarian cancer models in vitro and in vivo. Clinical Cancer Research, 18, 5911–5923.
Hew, K., Miller, P. C., El-Ashry, D., Sun, J., Besser, A., & Ince, T., et al. (2016). MAPK activation predicts poor outcome and the MEK inhibitor, selumetinib, reverses antiestrogen resistance in high-grade serous ovarian cancer. Clinical Cancer Research, 22, 935–947.
Simpkins, F., Jang, K., Yoon, H., Hew, K. E., Kim, M., Azzam, D. J., Sun, J., Zhao, D., Ince, T. A., Liu, W., Guo, W., Wei, Z., Zhang, G., Mills, G. B. & Slingerland, J. M. (2018). Dual Src and MEK inhibition decreases ovarian cancer growth and targets tumor initiating stem-like cells. Clinical Cancer Research, 24(19), 4874–4886. https://doi.org/10.1158/1078-0432.CCR-17-3697.
Ma, J., Salamoun, J., & Wipf, P., et al. (2018). Combination of a thioxodihydroquinazolinone with cisplatin eliminates ovarian cancer stem cell-like cells (CSC-LCs) and shows preclinical potential. Oncotarget, 9(5), 6042–6054.
Keita, Togashi, & Masashi, et al. (2018). A Small-molecule Kinase Inhibitor, CEP-1347, Inhibits survivin expression and sensitizes ovarian cancer stem cells to paclitaxel. AntiCancer Research, 38(8), 4535–4542.
Wu, Y. H., Chiu, W. T., Young, M. J., Chang, T. H., Huang, Y. F., & Chou, C. Y. (2015). Solanum incanum extract downregulates aldehyde dehydrogenase 1-mediated stemness and inhibits tumor formation in ovarian cancer cells. Journal Cancer, 6(10), 1011–1019.
Young, M. J., Wu, Y. H., Chiu, W. T., Weng, T. Y., Huang, Y. F., & Chou, C. Y. (2015). All-trans retinoic acid downregulates ALDH1-mediated stemness and inhibits tumour formation in ovarian cancer cells. Carcinogenesis, 36(4), 498–507. https://doi.org/10.1093/carcin/bgv018.
Campos, B., Wan, F., Farhadi, M., Ernst, A., Zeppernick, F., & Tagscherer, K. E., et al. (2010). Differentiation therapy exerts antitumor effects on stem-like glioma cells. Clinical Cancer Research, 16(10), 2715–2728. https://doi.org/10.1158/1078-0432.CCR-09-1800.
Mal, A., Bukhari, A. B., Singh, R. K., Kapoor, A., & Barai, A., et al. (2020). EpCAM-mediated cellular plasticity promotes radiation resistance and metastasis in breast cancer. Frontiers in Cell and Developmental Biology, 8, 597673.
Yang, L., Shi, P., Zhao, G., Xu, J., & Peng, W., et al. (2020). Targeting cancer stem cell pathways for cancer therapy. Signal Transduction and Target Therapy, 5, 8.
Fu, Z., Ma, K., Dong, B., Zhao, C., Che, C., Dong, C., Zhang, R., Wang, H., Wang, X., & Liang, R. (2019). The synergistic antitumor effffect of Huaier combined with 5-Florouracil in human cholangiocarcinoma cells. BMC Complementary and Alternative Medicine, 19, 203 .
Pokhriyal, R., Hariprasad, R., Kumar, L., & Hariprasad, G. (2019). Chemotherapy resistance in advanced ovarian cancer patients. Biomark Cancer, 11, 1179299X19860815 .
Motohara, T., & Katabuchi, H. (2019). Ovarian cancer stemness: Biological and clinical implications for metastasis and chemotherapy resistance. Cancers, 11, 907 .
Patch, A. M., Christie, E. L., Etemadmoghadam, D., Garsed, D. W., George, J., Fereday, S., Nones, K., Cowin, P., Alsop, K., & Bailey, P., et al. (2015). Whole-genome characterization of chemoresistant ovarian cancer. Nature, 521, 489–494.
Lee, H., Kim, J. W., & Kim, D. K., et al. (2020). Calcium channels as novel therapeutic targets for ovarian cancer stem cells. International Journal of Molecular Sciences, 21(7), 2327.
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Contributions
Biqing Chen assumed the responsibility of composing and organizing the initial draft, Jiaqi Liu undertook the responsibility of graphic editing and table structuring.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, B., Liu, J. Advances in ovarian tumor stem cells and therapy. Cell Biochem Biophys (2024). https://doi.org/10.1007/s12013-024-01385-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s12013-024-01385-8