Abstract
The vital participation of Ca2+ in human organ functions such as muscular contractions, heartbeat, brain functionality, skeletal activity, etc, motivated the scientists to thoroughly research the mechanisms of calcium (Ca2+) signalling in distinct human cells. Ca2+, inositol triphosphate (IP3), and adenosine triphosphate (ATP) play important roles in cell signaling and physiological processes. ATP and its derivatives are hypothesized to be important in the pathogenic process that leads to fibrotic illnesses like fibrosis. Fluctuations in Ca2+ and IP3 in a fibroblast cell influence ATP production. To date, no evidence of coupled Ca2+ and IP3 mechanics regulating ATP generation in a fibroblast cell during fibrotic disease has been found. The current work suggests an integrated mechanism for Ca2+ and IP3 dynamics in a fibroblast cell that regulates ATP generation. Simulation has been carried out using the finite element approach. The mechanics of interdependent systems findings vary dramatically from the results of basic independent system mechanics and give fresh information about the two systems’ activities. The numerical results provide new insights into the impacts of disturbances in source influx, the serca pump, and buffers on interdependent Ca2+ and IP3 dynamics and ATP synthesis in a fibroblast cell. According to the findings of this study, fibrotic disorders cannot be attributed solely to disruptions in the processes of calcium signaling mechanics but also to disruptions in IP3 regulation mechanisms affecting the regulation of calcium in the fibroblast cell and ATP release.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ca2+ is an essential signaling ion in many biological processes and activities across various tissues and animals. Ca2+ signaling is crucial for a number of cellular processes in fibroblast cells, including proliferation, migration, myofibroblast differentiation and extracellular matrix (ECM) production. Dysregulation of Ca2+ signaling may contribute to the development of fibrotic diseases [1].
G-protein-coupled receptors (GPCRs) are proteins found on the surface of fibroblast cell [2]. When a neurotransmitter or signal molecule connects to a GPCR, the GPCR’s shape changes. This modification activates a G protein that is linked to a GPCR. This G protein serves as a messenger, allowing the signal to be sent farther. The activated G protein subsequently interacts with a phospholipase C (PLC) effector enzyme. This interaction causes the synthesis of IP3. IP3 serves as a backup messenger [3]. It goes throughout the cell in search of its target, the endoplasmic reticulum (ER), a compartment within the cell that stores calcium ions. IP3 binds to particular receptors on the ER membrane when it enters the ER. This binding leads the ER to release calcium ions that have been held in the cell’s cytoplasm [4, 5]. In fibroblast cells, IP3 has a significant impact in mediating various cellular processes including differentiation, migration cell, proliferation and survival. Specifically, IP3-mediated Ca2+ signaling regulates fibroblast migration and proliferation, which are important processes for wound healing and tissue repair [5].
ATP is a molecule that significantly impacts cellular energy metabolism. ATP has also been linked to the pathogenesis of fibrotic disorders. Fibrosis is a pathological disease characterized by an abnormal accumulation of ECM proteins leading to tissue scarring and dysfunction [6]. In the context of fibrosis and wound healing, the production and degradation of ATP play important roles in cellular processes that influence tissue repair and remodeling. During tissue injury or inflammation, cells often experience increased metabolic demands and stress. This can lead to overproduction of ATP through processes like glycolysis and oxidative phosphorylation in mitochondria. Overproduction of ATP can be influenced by factors such as increased cellular activity, inflammation, and hypoxia [7]. ATP is essential for cell migration and proliferation, which are critical for wound healing and tissue repair [8]. ATP acts as a signaling molecule and can attract immune cells to the site of injury or inflammation, aiding in the resolution of tissue damage. Overproduction of ATP can lead to excessive inflammation and oxidative stress, which can contribute to tissue damage and exacerbate fibrosis [9]. High levels of extracellular ATP can activate purinergic receptors on fibroblasts and other cells, promoting fibrosis by stimulating collagen production and fibroblast differentiation [10]. ATP degradation leads to the production of adenosine, which has vasodilatory and anti-inflammatory properties. Adenosine can promote tissue protection and healing by reducing inflammation and enhancing blood flow to the site of injury [11]. Adenosine can modulate immune responses and promote tissue repair by promoting the differentiation of fibroblasts into myofibroblasts, which are important for wound contraction and matrix deposition. Inefficient ATP degradation can result in the accumulation of ATP in the extracellular space, leading to sustained activation of purinergic receptors and perpetuating inflammation and scarring in multiple organs, including the lung, heart, kidney and liver [10,11,12]. Therefore, a surplus of ATP and inadequate removal of ATP insufficient degradation can leads various illnesses of the fibroblast, including wound healing and fibrosis. As a result, ATP can trigger excitotoxicity, which can harm fibroblasts or even kill them. ATP pathogenic mechanisms and their roles in fibrotic diseases are still unknown. Therefore, it is essential to make models that show the movements of Ca2+ and IP3 affecting the production of ATP.
Modeling keratinocyte-fibroblast interactions during the normal and abnormal wound recovery process is described by Shakti et al. [13]. Droniou et al. [14] investigated a two-dimensional tumor development model with shifting boundaries that were numerically solved. Using the idea of advection-diffusion, Simpson et al. [15] investigated the contributions of directed and random motility in a fibroblast cell migration test induced by an electric field. Michell [16] proposed a link between high intracellular Ca2+ and PIP2 catabolism. Berridge and Irvine [3] discovered IP3 to be a second messenger that mobilizes Ca2+ from the ER. Regarding cellular transmitter release, Fogelson and Zucker [17] proposed the model of presynaptic diffusion of Ca2+ that includes inflow, cytoplasmic binding and surface pumps. Jafri and Keizer [18] examined Ca2+ transport in the cell cytosol and Ca2+ handling by the ER in their study of IP3-induced Ca2+ wave propagation.
Smith et al. [19] developed a reaction-diffusion model describing Ca2+ transport with diffusion, source influx, and buffer mechanisms. The reaction model for calcium buffering has been described in fibroblast cells [20, 21]. Wagner and Keizer [22] studied the effects of fast buffers on Ca2+ transport and fluctuation. Kotwani and Adlakha [23] developed a reaction-diffusion model to study effect of buffer binding affinity, diffusion and source amplitude in fibroblast cells. Kotwani and Adlakha [24] investigated a computational model of calcium distributions with source fluxes, serca, and buffer approximations in a fibroblast cell. Sun et al. [25] constructed a dynamic model for intracellular calcium responses in a fibroblast cell induced by electrical stimulation.
Manhas and Pardasani [26] proposed a probable mechanism for Ca2+ fluctuations based on the interaction of the cell’s three Ca2+ stores like mitochondria, cytosol and ER. Manhas and Pardasani [27] created a mathematical model to investigate the IP3 kinetics-based Ca2+ fluctuations in pancreatic acinar. Jha and Adlakha [28] created a two-dimensional unsteady state model of Ca2+ concentration change in neurons. Joshi and Jha [29] analyze the physiological involvement of calbindin-D28k and VGCC in Parkinson’s disease using a mathematical model that incorporates all key factors such as diffusion coefficient and fluxes. Joshi and Jha [30] created a mathematical model based on the Hilfer fractional reaction-diffusion equation to investigate Ca2+ transport in cells. Jha and Adlakha [31] conducted two-dimensional finite element simulations of unsteady state Ca2+ diffusion in neurons with a ER leak and a serca pump. Jha and Adlakha [32] sought to investigate the impact of sodium-Ca2+ exchangers and source geometry on the dynamics of Ca2+ in a neuron cell. Tewari and Pardasani [33] investigated the oscillations in Ca2+ caused by dynamically changing membrane potential, focusing on the sodium pump. Pathak and Adlakha [34] created a two-dimensional model of Ca2+ distribution in myocytes, including excess buffer approximation, diffusion and point source. In a one-dimensional instance, Naik and Pardasani [35] investigated the influence of the serca pump and ryanodine receptor (RyR) on the Ca2+ profile in oocytes. For a one-dimensional unstable state situation, Naik and Pardasani [36] created a finite element model of Ca2+ distribution in oocytes. Naik and Pardasani [37] used a three-dimensional finite element model to investigate the spatiotemporal Ca2+ distribution in oocytes. Kotwani et al. [38] created a two-dimensional unsteady state Ca2+ distribution model in fibroblast cells. Kothiya and Adlakha [39] developed a model to investigate the function of Ca2+ signaling in the production of IP3 and ATP in fibroblast cells. Jha et al. [40] use FEM to investigated the cytosolic Ca2+ concentration distribution in astrocytes in a two-dimensional steady-state situation with excess buffer. Jagtap and Adlakha [41] used finite volume and Crank Nicolson simulations to investigate the advection-diffusion of Ca2+ in a hepatocyte cell. ATP interacts with P2Y purinergic receptors in the cell membrane, activating PLC, which catalyses IP3 synthesis from PIP2. IP3 interacts synergistically with Ca2+ in receptors on the surface of the endoplasmic reticulum (ER) and opens channels that allow Ca2+ ions to be secreted into the cytoplasm. Ca2+ promotes and inhibits its own release. The huge Ca2+ concentration gradient also causes a Ca2+ leak. An ATP-dependent pump returns Ca2+ to the ER. As a result of this cascade, ATP is released into the extracellular space. The study of Stamakis and Mantzaris [42] provides two ideas concerning ATP release: Ca2+-regulated or IP3-regulated ATP synthesis.
Let’s go further into the physiological dynamics of ATP synthesis, concentrating on the interaction between adenosine generation via de novo purine and salvage pathways, as well as the mitochondrial ETC. De Novo Purine Pathway and Adenosine Synthesis: The de novo purine process entails the progressive synthesis of purine bases from simple precursors such as aspartate, carbon dioxide, glutamine, and glycine. The route begins with the creation of the purine ring structure, which is followed by a series of enzymatic activities that result in the production of inosine monophosphate (IMP). This is subsequently converted into adenosine monophosphate (AMP) through a series of reactions, ultimately leading to ATP synthesis during oxidative phosphorylation [43]. Salvage Pathway for Adenosine Production: Cells use the salvage process to recycle purine bases (adenine and guanine) from nucleotides and nucleosides produced during DNA and RNA degradation. This recycling conserves energy and resources by reusing purine components to build new nucleotides. This enzyme catalyzes the cleavage of nucleosides (e.g., adenosine) into their respective purine bases (adenine). Adenine is then converted into adenosine monophosphate (AMP) through the addition of a phosphoribosyl group. AMP can subsequently undergo phosphorylation to form adenosine diphosphate (ADP) and, ultimately, ATP through the process of oxidative phosphorylation in the mitochondria [44]. Mitochondrial Electron Transport Chain (ETC) andATP Synthesis: The mitochondrial ETC is a crucial component of ATP synthesis, occurring within the inner mitochondrial membrane. It involves a series of protein complexes that facilitate electron transport and proton pumping. Electrons obtained from molecules like glucose and fatty acids are shuttled through these complexes, leading to the transfer of electrons along the ETC. As electrons move through the complexes, protons (H+ ions) are pumped across the inner mitochondrial membrane, creating a proton gradient. This enzyme complex, also known as Complex V, is embedded in the membrane and harnesses the proton gradient to synthesize ATP from ADP and inorganic phosphate (Pi) through a process called chemiosmotic coupling. As protons flow back into the mitochondrial matrix through ATP synthase, the energy generated is used to drive ATP synthesis [45].
In mouse fibroblasts, Bryan et al. [46] investigated the dual function of ATP in maintaining volume-regulated chloride channels and in regulating the release of Ca2+. Miyoshi et al. [47] looked at how cells die as they age and what role ATP plays in apoptosis and necrosis caused by hydrogen peroxide. Astrocytic cells were explored by Stamatakis and Mantzaris [42], who investigated the link between Ca2+-regulated and IP3-regulated ATP production mechanisms. Chen et al. [6] demonstrated that ATP activates the P2Y2 receptors in fibroblasts of human cardiac muscle and raises their proliferation via increasing cell cycle progression. It also has the additional effect of increasing the migration of cells. These actions of ATP may assist in modifying the structure of damaged hearts. Kotwal et al. [48] investigated the essential function ATP plays in macrophages as they expedite wound healing and regeneration. One-dimensional mathematical models of T-lymphocyte Ca2+ distribution were constructed by Kumar et al. [49] using a finite element technique. Source inflow, buffers and RyR receptor effects were also acquired for unusual circumstances, and the serca pump effects were found for the temporal case. A one-dimensional fractional reaction-diffusion model for RyR, VGCC and calbindin-D28k was explored by Joshi and Jha [29]. They found analytical answers for Parkinson’s brain physiology. Jagtap and Adlakha [50] used the finite volume method to be looked into the cytosolic Ca2+ distribution in hepatocyte cells. Joshi et al. [51] investigated intracellular calcium dynamics in fibroblasts using an exponential kernel rule.
Glycolysis is a key metabolic pathway that happens in the cytoplasm of cells and acts as the first step in the breakdown of glucose to create ATP. Glycolysis begins with the activation of glucose, a six-carbon sugar. Two molecules of ATP are initially invested to convert glucose into fructose-1,6-bisphosphate. The six-carbon sugar molecule is split into two three-carbon molecules: glyceraldehyde-3-phosphate and dihydroxyacetone phosphate. Only glyceraldehyde-3-phosphate continues through the pathway. Glyceraldehyde-3-phosphate undergoes a series of reactions, leading to the production of two molecules of NADH (a high-energy electron carrier) and four molecules of ATP. However, since two ATP molecules were initially invested, there is a net gain of two ATP molecules per glucose molecule. The final steps of glycolysis convert each glyceraldehyde-3-phosphate into pyruvate, a three-carbon compound. During this process, an additional two molecules of NADH are produced [52]. The Tricarboxylic Acid (TCA) Cycle, often known as the citric acid cycle or Krebs cycle, is a major metabolic system that occurs in eukaryotic cell mitochondria and prokaryotic cell cytoplasm. It is an essential component of respiration in cells and helps to generate energy in the form of ATP. The TCA cycle begins when acetyl coenzyme A (Acetyl-CoA) enters the cycle. Acetyl-CoA is derived from various sources, including the breakdown of carbohydrates, fats, and amino acids. The acetyl group from Acetyl-CoA is combined with a four-carbon compound called oxaloacetate to form citrate. Citrate undergoes a series of enzyme-catalyzed reactions, including isomerization and dehydration, leading to the regeneration of isocitrate. It is further oxidized by the enzyme isocitrate dehydrogenase, resulting in the release of carbon dioxide (CO2) and the formation of α-ketoglutarate. This step also generates reduced nicotinamide adenine dinucleotide (NADH), a carrier molecule that stores high-energy electrons [53]. α-Ketoglutarate is then oxidized by the enzyme α-ketoglutarate dehydrogenase complex, producing another molecule of CO2 and another molecule of NADH. The resulting molecule, succinyl-CoA, also captures high-energy electrons. Succinyl-CoA undergoes a series of reactions that ultimately lead to the formation of succinate. This step releases a molecule of guanosine triphosphate (GTP), which is a molecule similar to ATP and can be readily converted into ATP. Succinate is further oxidized by the enzyme succinate dehydrogenase, which is embedded in the inner mitochondrial membrane and also serves as a part of the ETC. This oxidation generates another molecule of FADH2, another carrier molecule storing high-energy electrons. The oxidation of succinate produces fumarate. This step involves the addition of water to the double bond of succinate. Fumarate is then enzymatically converted to malate. Malate is oxidized by the enzyme malate dehydrogenase, producing another molecule of NADH and regenerating oxaloacetate. Oxaloacetate can then combine with another acetyl group from Acetyl-CoA to restart the cycle. The reduced electron carriers, NADH and FADH2, generated during the TCA cycle, play a crucial role in ATP production. These carriers carry high-energy electrons to the ETC located in the inner mitochondrial membrane. As these electrons move through the ETC, they establish a proton gradient across the membrane, which creates a flow of protons (H+) back into the mitochondrial matrix through ATP synthase [54]. This flow of protons drives the ATP synthase enzyme to synthesize ATP from inorganic phosphate (Pi) & ADP in a process known as oxidative phosphorylation. The coupling of electron transport and proton pumping in the ETC with ATP synthesis is termed chemiosmotic coupling. The exact number of ATP molecules generated from one round of the TCA cycle varies based on factors such as the availability of oxygen and the efficiency of electron transport. However, in total, one round of the TCA cycle can contribute to the production of multiple molecules of ATP [55].
Several researchers have investigated the interdependence Ca2+ and IP3 dynamics in cells, such as hepatocytes [56], myocyte [57], etc. Some one-way feedback models of Ca2+ with other ions like nitric oxide, β-amyloid and dopamine are proposed by Pawar and Pardasani [58,59,60]. The literature contains models of Ca2+ dynamics in fibroblast cells that assume IP3 as a constant. To make the model more realistic, examine the coupling of Ca2+ with other systems’ dynamics.
The role of interdependent Ca2+ and IP3 kinetics a in the control of distinct signalling molecules such as nitric oxide, β-amyloid and ATP in neurons have been studied by Pawar and Pardasani [61,62,63]. Recently, feedback model of NO generation is regulated by Ca2+ and IP3 in fibroblast cells was developed by Kothiya and Adlakha [64]. Singh and Adlakha [65] investigated the influence of source geometry on the system kinetics of calcium and IP3 in myocytes of the heart. Joshi et al. [51] established a model to study the impact of buffer and calcium oscillation in fibroblast cells. The effects of buffer, serca pump and source influx, on coupled calcium and IP3 dynamics with insulin secretion in beta cells have been studied by Vaishali and Adlakha [66]. Kothiya and Adlakha [67] developed a two-way feedback model of the system kinetics model of PLC and Ca2+ incorporating the buffer mechanism, diffusion parameters, source influx, and serca rate in a fibroblast cell.
There has been no attempt to investigate the influence of coupled calcium and IP3 kinetics on the control of ATP synthesis. Given the regulatory functions of IP3, ATP and Ca2+ ions in fibroblasts and cancer-associated fibroblast (CAF), there is a need for knowledge about the effects of IP3 and Ca2+ dynamics on ATP synthesis and the cytoprotective and cytotoxic effects of ATP. In the past, no such theoretical investigation in this area has been recorded. The goal of this study is to look at the regulatory and deregulatory effects of system mechanics of calcium and IP3 in fibroblasts that regulate ATP synthesis. The findings were derived with the use of the FEM. The impact of numerous factors on the paired dynamics of calcium and IP3, as well as their impacts on ATP synthesis, have been investigated. A model is provided here that incorporates a two-way coupling between the Ca2+ and IP3 systems in fibroblast cells to regulate ATP levels. It is simulated to disclose information on changes in ATP synthesis induced by changes in the amounts of Ca2+ and IP3 in fibroblasts. The coupled dynamics of calcium and IP3 with a buffer mechanism and ATP release propose to study the role of constitutive processes like buffer, source influx, association rate, etc., in normal and fibrotic conditions.
Mathematical Formulation
By adding buffer terms to the model of Wagner et al. [68] the Ca2+ transport in fibroblasts in the presence of IP3 is expressed as
In this case, [B]∞ represents the steady-state buffer concentration, while \({[C{a}^{2+}]}_{\infty }\) represents the steady-state Ca2+ ion concentration.The notation Dc denotes the diffusion coefficient of Ca2+. The variable for time is denoted by the letter ‘t’, while the variable for the position is denoted by the letter ‘x’. The symbol K+ represents the rate of buffer association. The influx and outflux terms of equation (1) are given by Keizer et al. [69] as given below,
Where \({J}_{I{P}_{3}R},{J}_{leak}\) and Jserca each represent a different flow associated with the IP3 receptor, the leaking pump and the serca pump, respectively. Vleak and \({V}_{I{P}_{3}R}\) are the flux rate constants for leak and IP3 respectively.The maximum rate and the Michaelis constant for the serca pump are represented by the variables Vleak and \({V}_{I{P}_{3}R}\), respectively.
The definitions of m and h can be found in Keizer and Young’s work [69].
\({K}_{I{P}_{3}},{K}_{Ac}\) and KInh are the dissociation constants of IP3 that activate Ca2+ and inhibit Ca2+ successively. Here, IP3 dynamics in the presence of Ca2+ described by Wagner et al. [68] is used and might be represented in fibroblasts as;
Where [IP3] shows the cytosolic concentration of IP3. DI is IP3 diffusion coefficient. Wagner et al. [68] gives the Ca2+ dependent IP3 release terms as given below;
Where Kproduction represents the Michaelis constant for calcium activation, Jproduction represents the flux term for IP3 production and Vproduction represents the maximal IP3 generation rate. Bugrim et al. [70] and Sims and Allbrittont [71], as noted below, supply the additional flux terms, namely the IP3 degradation by JKin and Jphosphatase.
Where V1, V3 and V2 are the maximum rate constants for low calcium (3-kinase), phosphatase and high calcium (3-kinase) respectively. A variable parameter (λ = 30) estimates the degradation rate [68].
The cell calcium level calculates the \(C{a}_{ER}^{2+}\) via conversation relationship.
Initial Conditions
The following two initial conditions are framed by Brown et al. [72] and Dupont et al. [73] based on the assumption that the cell is initially at rest, having an initial concentration of IP3 and Ca2+.
Boundary Conditions
For Ca2+, the boundary conditions framed by Brown et al. [72] as mentioned below;
where σ represents the source amplitude.
The furthest border from the source is indicated by [74, 75]
Also, for IP3 kinrtics, the boundary circumstances given by Fink et al. [76] and Brown et al. [72] as given below.
Regulation of C a 2+ and I P 3 Dependent A T P
The Ca2+ and IP3 regulated ATP synthesis is given by Stamatakis and Mantzaris [42] as,
Where, β is the maximum synthesis rate and P([Ca2+]) and Q([IP3]) are the ATP release dependent on Ca2+ and IP3 respectively. The Ca2+ and IP3 dependent ATP release can be characterized respectively as given below;
Where a0 and b0 are constants for ATP feedback and \({[C{a}^{2+}]}_{max}\) and \({[I{P}_{3}]}_{max}\) are the cell’s maximum Ca2+ and IP3 values. The finite element and Crank Nicholson procedure followed for the solution are given in Appendix.
Results and Discussion
A quantitative solution of the partial differential equations representing the coupled dynamics of IP3 and Ca2+ was achieved using MATLAB software. Graphs are employed to visually represent the numerical findings generated by solving the equations. Table 1 shows the numerical measurements of the various parameters used in this study. Figure 1 depicts the systematic pathways of calcium and IP_3 dynamics with the regulation of neurotransmitter ATP production.
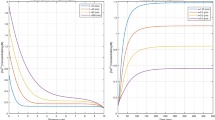
Figure 2 depicts the geographic and temporal distributions of Ca2+ in fibroblast cells at various periods in time and space. Because the source channel delivers many Ca2+ ions into the cell, there may be a high Ca2+ distribution at the source x = 0 μm. The spatial Ca2+ profile lowers from x = 0 μm to x = 10 μm and eventually convergence occurs to the cellular background Ca2+ profile (0.1 μM). Because the source channel opens, the temporal concentration of Ca2+ rises with time in Fig. 2B and the Ca2+ level rises in the cytosol of fibroblast cells due to increasing intracellular Ca2+ concentration coming from the source. The temporal Ca2+ profile achieved equilibrium within 150 ms regardless of the cell’s location.
Figure 3 displays the ATP release which is Ca2+-dependent for the different time points and positions. The impact of Ca2+ concentration on ATP release is significant in situations where Ca2+ is high. The ATP release is also high wherever Ca2+ profile is high in the fibroblast cell. The Ca2+ distribution is generally high near the source. The ATP release is also high at x = 0 μm. In Fig. 2B, it has been seen that Ca2+ concentration gets a steady state in 150 ms. In Fig. 3B, the ATP release achieves a steady state in 150 ms. This implies that the ATP release directly depends on Ca2+ concentration in the cell.
Figure 4 displays the spatiotemporal profile of IP3 profile at various times and places in fibroblasts. In Fig. 4A, the profile of IP3 goes down (x = 0 to x = 10) and ends up at a concentration of 0.16 μM in the cell. The IP3 particles stick together near the IP3 receptor and achieve it’s border value (3 μM at x = 0 μm) for time t = 0, 5, 10, 20, 50, 100 and 1000 ms in the fibroblast cell. In Fig. 4A it is observed that IP3 dynamics is nonlinear initially and approaches a linear behavior after the passage of time reaching a steady state condition. This nonlinearity is due to an imbalance among the various processes of the cell and as these processes achieve equilibrium, the behavior of the profile becomes linear. Figure 4B shows the profile of time of IP3 distribution which increases with time for various places x = 0.25, 0.50, 0.75, 1, 2, 5 & 10 μm synergetically with the increase in Ca2+ with time in Fig. 2B.
Figure 5 displays the Ca2+ distribution at x = 5 μm for [B] = 400 μM under fibrotic conditions in cell. The fluctuation in the temporal profile of Ca2+ is observed for greater buffer levels in the cell at the initial time. This damping fluctuation is due to an imbalance among the various processes of the cell and the buffer binds the Ca2+ ions and lowers the level of Ca2+ concentration in the cell. In Fig. 5A, we found substantial differences in the Ca2+ profiles of normal fibroblasts and CAF, though the behavior of the curves is similar in both cases. The oscillation in the Ca2+ profile in Fig. 5A is due to the substantial imbalances among the regulatory processes that exist up to 20 ms and then achieve equilibrium. Similarly, in Fig. 5B, the synergetic changes in ATP level are observed like those in Fig. 5A. The spatiotemporal Ca2+ concentrations are higher (30%) in the case of cystic fibrosis than in normal fibroblasts [77], As a result, an increased level of Ca2+ concentration is hazardous and can lead to fibrosis [78].
Figure 6 shows the IP3 dependent ATP release for different times and positions. In Fig. 4A, it was seen that IP3 is highest at x = 0 μm and decreases as we move away from x = 0 μm to x = 10 μm. Similarly in Fig. 6A, we observe that ATP release is highest at x = 0 μm and reduces as it departs from the source. We observed that the behavior of the IP3 profile changed from nonlinear to linear with the increment of time steps. Also from Fig. 6A, it is observed that the nonlinear behavior of IP3-dependent ATP has changed. This is due to an imbalance among the various processes of the cell. The same patterns are observed in Fig. 4B and Fig. 6B for the temporal profile of IP3 and ATP release. The IP3 and ATP release profiles reach steady-state simultaneously at 150 ms.
Figure 7 depicts the spatiotemporal Ca2+-dependent ATP release for the different source amplitude values along with the buffer concentration 5 μM and diffusion coefficient 16 μm2/s under normal and cystic fibrosis conditions. In Fig. 7, it can be seen that the distribution of Ca2+-dependent ATP is higher for greater source amplitude values. In Fig. 7A, the ATP concentration is higher at x = 0 μm, reduces along the spatial axis and converges on 0.1 μM at x = 10 μm. From Fig. 7B, it is clear that the ATP level achieves a steady state at time t = 120 ms. Further, there is a substantial difference in ATP levels between normal and cystic fibrosis patients. The spatiotemporal ATP fluxes are greater in cystic fibrosis patients because the Ca2+ concentration is 30% higher in CF fibroblasts than in normal [77]. The excess ATP is dangerous since it can cause fibrotic diseases [9].
The computation has been carried out for Ca2+ concentration with varying buffer concentration values in the range t = 25 ms to t = 100 ms for ATP release in fibroblast cells. The consequences of buffer concentration on ATP distribution profile in fibroblast cells concerning time for various buffer values, i.e., B = 15, 30, 60, 120 μM, have been displayed in Fig. 8. For t = 25, 50, 75 & 100 ms, we observe that the increase in buffering reduces the ATP concentration in the cell. Thus, in all cases, the fall in ATP is lower for the low buffer and higher for the high buffer. Also, ATP concentration converges to a minimum of 0.1 μM.
Figure 9 depicts the spatial and temporal Ca2+ dependent ATP release under normal and cystic fibrosis for a range of buffer associations rates 5 μM. As seen in Fig. 9, the Ca2+ dependent ATP decreases as the buffer binding rate increases. Higher binding rates bind higher amounts of free calcium, thereby reducing calcium levels in the cell, which signals the ATP system to reduce the production of ATP in the cell. In Fig. 9A, we observe the alteration in the curves’ nonlinear nature. When the association rate of the buffer is high, we observe a fall in ATP production at the source and a steep fall in the ATP production curves near the source from x = 0 to x = 2 μm due to the dominance of calcium-reducing mechanisms weakening the calcium signal feedback to the ATP production system and prompting it to reduce ATP production. But when the buffer association rates are low, the ATP production is higher at the source due to a strong calcium signal caused by a reduction in the dominance of calcium-reducing mechanisms leading to more effect of calcium-elevating mechanisms. There is a substantial difference in ATP levels in normal and CF fibroblasts. Ca2+ dependent ATP is 30% higher in CF fibroblasts than in normal. This process occurs if the rate of association is high.
Error Estimation
The absolute comparative error and its percentage in a fibroblast cell have been estimated and shown in Tables 2 and 3. The model’s accuracy for Ca2+ and IP3 is 99.84019761%, 99.84070305%, 99.84070305 and 99.167848%, 99.18513997%, 99.18514701% for the time (t = 50, 100, 200, 500 & 1000) ms respectively. As a result, the absolute worst-case scenario for the error rate of this model is 0.16%, while 99.84% is the utmost best-case scenario for its accuracy. Because the grid sensitivity is essentially nonexistent, this strongly argues that the solution is not grid-reliant.
Validation
For varied parameters, the profiles of Ca2+ and IP3 levels were produced. For the Ca2+ profile, the amount of buffer was set at 0.0 μM, while the source inflow was set at 2.46 pA. The results of the Ca2+ and IP3 in the current model for t = 50 s are compared with the findings of Pawar and Pardasani [61, 62] & Wagner et al. [68] as depicts in Tables 4 and 5. It appears that the proposed study’s results are very similar to those derived from previous studies.
Stability Analysis
We determined the spectral radius for the stability investigation, and if the radius of the spectrum is equal to or below one, the system is considered stable [79]. In this specific case, the spectral radius was determined to be 0.9853, so it’s <1, indicating that the calculated result is stable.
Conclusion
A model is developed and successfully implemented to explore the consequences of disruptions in coupled IP3 and Ca2+ dynamics on ATP generation in a fibroblast cell.
Disruptions in the interdependent IP3 and Ca2+ levels can be induced by the failure of mechanisms such as buffering and the serca pump. As a result of some disorder in these processes, high amounts of source input, association rate and higher buffer values were investigated. These perturbations significantly impacted Ca2+ and IP3 dynamics regulating ATP generation. For obtaining numerical solutions under various situations, the finite element and Crank Nicholson were used. In light of the unexpected results, the following conclusions are reached:
-
1.
When the source of the inflow is substantial and the serca and buffer are low, the calcium concentration rises, resulting in increased IP3 concentrations in fibroblast cells.
-
2.
High buffer levels cause irregularities because of oscillations in the Ca2+ distributions in fibroblast cells.
-
3.
An rise in Ca2+ concentration results from an increase in IP3 levels, which in turn boosts ATP synthesis.
The fundamental findings described above are supported by biological evidence. In addition, the results of the stability analysis, error analysis, and validation procedures used in the current study suggest that the suggested model is appropriate and effective for the inquiry at hand. Furthermore, the following innovative deductions and inferences drawn from the numerical data are provided:
-
1.
The large volumes of source input result in higher Ca2+ levels, which boosts the ATP release in normal fibroblast and cystic fibrosis fibroblast. These changes in ATP signalling can result in fibrotic disorders like fibrosis [46].
-
2.
The presence of buffers decreases Ca2+ and IP3 levels in normal fibroblast and cystic fibrosis fibroblast and lowers the rate of selective death of fibroblasts. insufficient quantities of EGTA and calmodulin buffers can lead to cystic fibrosis [77].
-
3.
When buffer is low, Ca2+ levels rise, increasing ATP release in fibroblasts as well as cystic fibrosis fibroblast. The increase in Ca2+ and IP3 concentrations within the cell promotes the loss of fibroblast cells, which leads to cancer [80].
-
4.
Increased ATP production is risky since it might result in fibrotic diseases. One more novelty of the results is the spatiotemporal ATP production are greater in cystic fibrosis patients because the Ca2+ concentration is 30% higher in CF fibroblasts than in normal fibroblasts [77].
Disruptions in numerous generative processes of IP3 and Ca2+dynamics might result in altered ATP synthesis, leading to various fibrotic diseases. Lowered buffering capacity, impaired buffer association performance, high levels of source inflow, and fluctuations in IP3 levels can induce increases in free Ca2+ levels and ATP generation, which is the cause of cystic fibrosis when there is a discrepancy between adenosine triphosphate production and its metabolism.
The results concur with biological realities. In the current work, the FEM technique is extremely successful. The model proposed sheds light on the underlying processes of Ca2+ and IP3 dynamics that cause an increase in ATP production, which has been identified as a factor causing cytotoxicity and contributing to the development of cystic fibrosis. The findings highlight the challenge of determining the correct constitutive procedure of IP3 and Ca2+ dynamics, crucial in ATP production alterations in fibrosis. Although many questions remain unanswered, the results from studying the relationships between the constitutive processes of IP3 and Ca2+ dynamics and ATP synthesis can pave the way to address the aforementioned challenges.
References
Berridge, M., Lipp, P., & Bootman, M. (1999). Calcium signalling. Current Biology, 9, R157–R159.
Capote, L. A., Perez, R. M., & Lymperopoulos, A. (2015). GPCR signaling and cardiac function. European Journal of Pharmacology, 763, 143–148.
Berridge, M. J., & Irvine, R. F. (1984). Inositol trisphosphate, a novel second messenger in cellular signal transduction. Nature, 312, 315–321.
Bootman, M. D., Fearnley, C., Smyrnias, I., MacDonald, F., & Roderick, H. L. (2009). An update on nuclear calcium signalling. Journal Of Cell Science, 122, 2337–2350.
Bootman, M. D., & Berridge, M. J. (1995). The elemental principles of calcium signaling. Cell, 83, 675–678.
Chen, J.-B., et al. (2012). Adenosine-5-triphosphate up-regulates proliferation of human cardiac fibroblasts. British Journal Of Pharmacology, 166, 1140–1150.
Perera, L. M. B., et al. (2019). The regulation of skin fibrosis in systemic sclerosis by extracellular atp via p2y2 purinergic receptor. Journal Of Investigative Dermatology, 139, 890–899.
Smith, D. G., Mills, W. J., Steen, R. G., & Williams, D. (1999). Levels of high energy phosphate in the dorsal skin of the foot in normal and diabetic adults: the role of 31p magnetic resonance spectroscopy and direct quantification with high pressure liquid chromatography. Foot & Ankle International, 20, 258–262.
Riteau, N., et al. (2010). Extracellular atp is a danger signal activating p2x7 receptor in lung inflammation and fibrosis. American Journal of Respiratory and Critical Care Medicine, 182, 774–783.
Lu, D., Soleymani, S., Madakshire, R., & Insel, P. A. (2012). Atp released from cardiac fibroblasts via connexin hemichannels activates profibrotic p2y2 receptors. The FASEB Journal, 26, 2580.
Pelleg, A. (2021). Extracellular adenosine 5-triphosphate in pulmonary disorders. Biochemical Pharmacology, 187, 114319.
Goncalves, R., et al. (2006). The role of purinergic p2x7 receptors in the inflammation and fibrosis of unilateral ureteral obstruction in mice. Kidney International, 70, 1599–1606.
Menon, S. N., et al. (2012). Modelling the interaction of keratinocytes and fibroblasts during normal and abnormal wound healing processes. Proceedings of the Royal Society B: Biological Sciences, 279, 3329–3338.
Droniou, J., Flegg, J. A., & Remesan, G. C. (2020). Numerical solution of a two dimensional tumour growth model with moving boundary. Journal of Scientific Computing, 85, 1–31.
Simpson, M. J., Lo, K.-Y., & Sun, Y.-S. (2017). Quantifying the roles of random motility and directed motility using advection-diffusion theory for a 3t3 fibroblast cell migration assay stimulated with an electric field. BMC Systems Biology, 11, 1–9.
Michell, R. H. (1975). Inositol phospholipids and cell surface receptor function. Biochimica et Biophysica Acta (BBA)-Reviews on Biomembranes, 415, 81–147.
Fogelson, A. L., & Zucker, R. S. (1985). Presynaptic calcium diffusion from various arrays of single channels. implications for transmitter release and synaptic facilitation. Biophysical Journal, 48, 1003–1017.
Jafri, M., & Keizer, J. (1995). On the roles of calcium diffusion, calcium buffers, and the endoplasmic reticulum in ip3-induced calcium waves. Biophysical Journal, 69, 2139–2153.
Smith, G. D., Wagner, J., & Keizer, J. (1996). Validity of the rapid buffering approximation near a point source of calcium ions. Biophysical Journal, 70, 2527–2539.
Torres, J. J., et al. (2004). Modeling action potential generation and propagation in nrk fibroblasts. American Journal of Physiology-Cell Physiology, 287, C851–C865.
Kusters, J., et al. (2007). Hysteresis and bistability in a realistic cell model for calcium oscillations and action potential firing. Physical Review Letters, 98, 098107.
Wagner, J., & Keizer, J. (1994). Effects of rapid buffers on calcium diffusion and calcium oscillations. Biophysical Journal, 67, 447–456.
Kotwani, M., Adlakha, N., & Mehta, M. (2012). Numerical model to study calcium diffusion in fibroblasts cell for one dimensional unsteady state case. Applied Mathematical Sciences, 6, 5063–5072.
Kotwani, M., & Adlakha, N. (2017). Modeling of endoplasmic reticulum and plasma membrane calcium uptake and release fluxes with excess buffer approximation (eba) in fibroblast cell. International Journal of Computational Materials Science and Engineering, 6, 1750004.
Sun, G.-X., Wang, L.-J., Xiang, C., & Qin, K.-R. (2013). A dynamic model for intracellular calcium response in fibroblasts induced by electrical stimulation. Mathematical Biosciences, 244, 47–57.
Manhas, N., & Pardasani, K. (2014). Modelling mechanism of calcium oscillations in pancreatic acinar cells. Journal of Bioenergetics and Biomembranes, 46, 403–420.
Manhas, N., & Pardasani, K. R. (2014). Mathematical model to study ip3 dynamics dependent calcium oscillations in pancreatic acinar cells. Journal of Medical Imaging and Health Informatics, 4, 874–880.
Jha, A., & Adlakha, N. (2014). Analytical solution of two dimensional unsteady state problem of calcium diffusion in a neuron cell. Journal of Medical Imaging and Health Informatics, 4, 547–553.
Joshi, H., & Jha, B. K. (2020). Fractional-order mathematical model for calcium distribution in nerve cells. Computational and Applied Mathematics, 39, 1–22.
Joshi, H., & Jha, B. K. (2021). Chaos of calcium diffusion in parkinson’s infectious disease model and treatment mechanism via hilfer fractional derivative. Mathematical Modelling and Numerical Simulation with Applications, 1, 84–94.
Jha, A., & Adlakha, N. (2015). Two-dimensional finite element model to study unsteady state calcium diffusion in neuron involving er leak and serca. International Journal of Biomathematics, 8, 1550002.
Jha, A., Adlakha, N., & Jha, B. K. (2016). Finite element model to study effect of sodium-calcium exchangers and source geometry on calcium dynamics in a neuron cell. Journal of Mechanics in Medicine and Biology, 16, 1650018.
Tewari, V., Tewari, S., & Pardasani, K. (2011). A model to study the effect of excess buffers and na+ ions on ca2+ diffusion in neuron cell. International Journal of Bioengineering and Life Sciences, 5, 251–256.
Pathak, K., & Adlakha, N. (2016). Finite element model to study two dimensional unsteady state calcium distribution in cardiac myocytes. Alexandria Journal of Medicine, 52, 261–268.
Naik, P. A., & Pardasani, K. R. (2013). One dimensional finite element method approach to study effect of ryanodine receptor and serca pump on calcium distribution in oocytes. Journal of Multiscale Modelling, 5, 1350007.
Naik, P. A., & Pardasani, K. R. (2015). One dimensional finite element model to study calcium distribution in oocytes in presence of vgcc, ryr and buffers. Journal of Medical Imaging and Health Informatics, 5, 471–476.
Naik, P. A., & Pardasani, K. R. (2019). Three-dimensional finite element model to study effect of ryr calcium channel, er leak and serca pump on calcium distribution in oocyte cell. International Journal of Computational Methods, 16, 1850091.
Kotwani, M., Adlakha, N., & Mehta, M. (2014). Finite element model to study the effect of buffers, source amplitude and source geometry on spatio-temporal calcium distribution in fibroblast cell. Journal of Medical Imaging and Health Informatics, 4, 840–847.
Kothiya, A., & Adlakha, N. (2022). Model of calcium dynamics regulating ip3 and atp production in a fibroblast cell. Advances in Systems Science and Applications, 22, 106–125.
Jha, B. K., Adlakha, N., & Mehta, M. (2014). Two-dimensional finite element model to study calcium distribution in astrocytes in presence of excess buffer. International Journal of Biomathematics, 7, 1450031.
Jagtap, Y., & Adlakha, N. (2018). Simulation of buffered advection diffusion of calcium in a hepatocyte cell. Mathematical Biology and Bioinformatics, 13, 609–619.
Stamatakis, M., & Mantzaris, N. V. (2006). Modeling of atp-mediated signal transduction and wave propagation in astrocytic cellular networks. Journal of Theoretical Biology, 241, 649–668.
Allison, A., Hovi, T., Watts, R. & Webster, A. The role of de novo purine synthesis in lymphocyte transformation. Purine and Pyrimidine Metabolism 207–224 (1977).
Scantland, S., et al. (2014). The adenosine salvage pathway as an alternative to mitochondrial production of atp in maturing mammalian oocytes. Biology of Reproduction, 91, 75–1.
Zhao, R.-Z., Jiang, S., Zhang, L., & Yu, Z.-B. (2019). Mitochondrial electron transport chain, ros generation and uncoupling. International Journal of Molecular Medicine, 44, 3–15.
Bryan, A., Sabanov, V., Thoroed, S., & Doroshenko, P. (2000). Dual role of atp in supporting volume-regulated chloride channels in mouse fibroblasts. Biochimica et Biophysica Acta (BBA)-Biomembranes, 1468, 63–72.
Miyoshi, N., Oubrahim, H., Chock, P. B., & Stadtman, E. R. (2006). Age-dependent cell death and the role of atp in hydrogen peroxide-induced apoptosis and necrosis. Proceedings of the National Academy of Sciences, 103, 1727–1731.
Kotwal, G. J., Sarojini, H., & Chien, S. (2015). Pivotal role of atp in macrophages fast tracking wound repair and regeneration. Wound Repair and Regeneration, 23, 724–727.
Kumar, H., Naik, P. A., & Pardasani, K. R. (2018). Finite element model to study calcium distribution in t lymphocyte involving buffers and ryanodine receptors. Proceedings of the National Academy of Sciences, India Section A: Physical Sciences, 88, 585–590.
Jagtap, Y., & Adlakha, N. (2018). Finite volume simulation of two dimensional calcium dynamics in a hepatocyte cell involving buffers and fluxes. Communications in Mathematical Biology and Neuroscience, 2018, Article–ID.
Joshi, H., Yavuz, M., & Stamova, I. (2023). Analysis of the disturbance effect in intracellular calcium dynamic on fibroblast cells with an exponential kernel law. Bulletin of Biomathematics, 1, 24–39.
Bonora, M., et al. (2012). Atp synthesis and storage. Purinergic Signalling, 8, 343–357.
Nazaret, C., Heiske, M., Thurley, K., & Mazat, J.-P. (2009). Mitochondrial energetic metabolism: a simplified model of tca cycle with atp production. Journal of Theoretical Biology, 258, 455–464.
Cortassa, S., Aon, M. A., Marbán, E., Winslow, R. L., & O’Rourke, B. (2003). An integrated model of cardiac mitochondrial energy metabolism and calcium dynamics. Biophysical Journal, 84, 2734–2755.
Tarasov, A. I., Griffiths, E. J., & Rutter, G. A. (2012). Regulation of atp production by mitochondrial ca2+. Cell Calcium, 52, 28–35.
Jagtap, Y., & Adlakha, N. (2019). Numerical study of one-dimensional buffered advection–diffusion of calcium and ip3 in a hepatocyte cell. Network Modeling Analysis in Health Informatics and Bioinformatics, 8, 1–9.
Singh, N., & Adlakha, N. (2019). A mathematical model for interdependent calcium and inositol 1, 4, 5-trisphosphate in cardiac myocyte. Network Modeling Analysis in Health Informatics and Bioinformatics, 8, 1–15.
Pawar, A., & Pardasani, K. R. (2022). Simulation of disturbances in interdependent calcium and β-amyloid dynamics in the nerve cell. The European Physical Journal Plus, 137, 1–23.
Pawar, A. & Pardasani, K. R. Study of disorders in regulatory spatiotemporal neurodynamics of calcium and nitric oxide. Cognitive Neurodynamics 1–22 (2022).
Pawar, A., & Pardasani, K. R. (2023). Computational model of calcium dynamics-dependent dopamine regulation and dysregulation in a dopaminergic neuron cell. The European Physical Journal Plus, 138, 1–19.
Pawar, A. & Pardasani, K. R. (2022). Effect of disturbances in neuronal calcium and ip3 dynamics on β-amyloid production and degradation. Cognitive Neurodynamics, 17, 239–256.
Pawar, A., & Raj Pardasani, K. (2022). Effects of disorders in interdependent calcium and ip3 dynamics on nitric oxide production in a neuron cell. The European Physical Journal Plus, 137, 1–19.
Pawar, A. & Pardasani, K. R. (2023). Mechanistic insights of neuronal calcium and ip3 signaling system regulating atp release during ischemia in progression of alzheimer’s disease. European Biophysics Journal, 52, 153–173.
Kothiya, A. B. & Adlakha, N. (2023). Cellular nitric oxide synthesis is affected by disorders in the interdependent calcium and ip3 dynamics during cystic fibrosis disease. Journal of Biological Physics, 49, 133–158.
Singh, N. & Adlakha, N. Effect of source geometry on interdependent calcium and inositol 1; 4; 5-trisphosphate dynamics in a cardiac myocyte cell. In Mathematical Modelling and Scientific Computing with Applications: ICMMSC 2018, Indore, India, July 19–21, 75–83, Singapore (Springer, 2020).
Vaishali & Adlakha, N. Disturbances in system dynamics of c a 2+ and ip 3 perturbing insulin secretion in a pancreatic β-cell due to type-2 diabetes. Journal of Bioenergetics and Biomembranes, 55, 151–167 (2023).
Kothiya, A. & Adlakha, N. (2023). Simulation of biochemical dynamics of calcium and plc in fibroblast cell. Journal of Bioenergetics and Biomembranes, 55, 267–287.
Wagner, J., et al. (2004). A wave of ip3 production accompanies the fertilization calcium wave in the egg of the frog, xenopus laevis: theoretical and experimental support. Cell Calcium, 35, 433–447.
Keizer, J., & De Young, G. (1994). Simplification of a realistic model of ip3-induced calcium oscillations. Journal of Theoretical Biology, 166, 431–442.
Bugrim, A., Fontanilla, R., Eutenier, B. B., Keizer, J., & Nuccitelli, R. (2003). Sperm initiate a ca2+ wave in frog eggs that is more similar to ca2+ waves initiated by ip3 than by ca2+. Biophysical Journal, 84, 1580–1590.
Sims, C. E., & Allbritton, N. L. (1998). Metabolism of inositol 1, 4, 5-trisphosphate and inositol 1, 3, 4, 5-tetrakisphosphate by the oocytes of xenopus laevis. Journal of Biological Chemistry, 273, 4052–4058.
Brown, S.-A., Morgan, F., Watras, J., & Loew, L. M. (2008). Analysis of phosphatidylinositol-4, 5-bisphosphate signaling in cerebellar purkinje spines. Biophysical Journal, 95, 1795–1812.
Dupont, G., Swillens, S., Clair, C., Tordjmann, T., & Combettes, L. (2000). Hierarchical organization of calcium signals in hepatocytes: from experiments to models. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research, 1498, 134–152.
Smith, G. D. (1996). Analytical steady-state solution to the rapid buffering approximation near an open calcium channel. Biophysical Journal, 71, 3064–3072.
Tewari, S., & Pardasani, K. (2010). Finite element model to study two dimensional unsteady state cytosolic calcium diffusion in presence of excess buffers. IAENG International Journal of Applied Mathematics, 40, 108–112.
Fink, C. C., et al. (2000). An image-based model of calcium waves in differentiated neuroblastoma cells. Biophysical Journal, 79, 163–183.
Gnegy, M. E., Erickson, R. P., & Markovac, J. (1981). Increased calmodulin in cultured skin fibroblasts from patients with cystic fibrosis. Biochemical Medicine, 26, 294–298.
Shapiro, B. L., Feigal, R. J., Laible, N. J., Biros, M. H., & Warwick, W. J. (1978). Doubling time α-aminoisobutyrate transport and calcium exchange in cultured fibroblasts from cystic fibrosis and control subjects. Clinica Chimica Acta, 82, 125–131.
Öziş, T., Aksan, E., & Özdeş, A. (2003). A finite element approach for solution of burgers’ equation. Applied Mathematics and Computation, 139, 417–428.
Housey, G. M., et al. (1988). Overproduction of protein kinase c causesdisordered growth control in rat fibroblasts. Cell, 52, 343–354.
Author information
Authors and Affiliations
Contributions
We, the writers, contributed equally to this paper regarding problem design, solution, literature review, and result interpretation. MATLAB code is developed by the first author.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The shape function is assumed
Where,
In equation (A3), substitute the nodal conditions, we obtain
Where,
By the equations (A5), we have
Where,
Substituting the values of q(e) & r(e) in equation (A3), we obtained
The partial differential equations (1) and (7) can be written as,
Where
Linearizing IP3 and Ca2+ dynamics yields the quantity of δ, γ, k, η, μ, ζ, γ2, α, β and τ. The equations after calculation and boundary circumstances are as follows.
Where,
We utilize the statistically stable Crank Nicholson Method on the matrices A and B to determine the time derivative using the Finite Element Approach, and the force vector is F. To solve the resultant system of equations, the Gaussian Elimination Method is utilized.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kothiya, A., Adlakha, N. Impact of Interdependent Ca2+ and IP3 Dynamics On ATP Regulation in A Fibroblast Model. Cell Biochem Biophys 81, 795–811 (2023). https://doi.org/10.1007/s12013-023-01177-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-023-01177-6