Abstract
This randomized, double-blind study evaluated the short-term effects and safety of perioperative retrograde autologous priming (RAP) for cardiopulmonary bypass (CPB) in patients with cardiac replacement surgery to determine if this approach is a better substitute for crystal liquids priming in patients with valvular heart disease. We observed that RAP significantly decreased the actual priming volume, preserved the hematocrit and hemoglobin level during CPB to a certain degree, and decreased lactate accumulation in CPB period. Moreover, RAP lowered the volume of transfusion and dosage blood products. Thus, our results showed that RAP approach effectively improved tissue perfusion and lowered intraoperative Lac levels, by reducing the hemodilution, which safely and reliably improve the microcirculation perfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Valvular heart disease (VHD), which is usually caused by rheumatic fever, is a common heart disease [1]. With the increase of the aging population, more and more senile valvular disease and valvular disease originate from coronary heart disease, which make myocardial infarction more commonly seen [2]. Treatments for valvular heart disease include drug therapy, interventional therapy, and surgeries [3]. Drug treatment can improve the symptoms of mild valvular heart disease, but fail to reverse valve structures that have been damaged during certain pathogenesis of VHD [4]. The long-term clinical effects of interventional therapy still need confirmation. Thus, surgical treatment is widely recognized as the most common, reliable, and effective treatment for VHD [5]. According to the degree and nature of valve damages, heart valve prosthesis or artificial valve replacement are used in surgery.
Cardiopulmonary bypass (CPB), which is a very essential process in patients with valve replacement to reduce blood transfusion, involves the following steps of blood recollection, blood ultrafiltration, and priming liquid reduction [6]. However, serious technical challenges still exist in CPB. Due to the requirement for the transfusion of large amount of stored blood or blood products during complex cardiovascular surgery, lack of blood, immune response after the transfusion, and virus contamination all call for new approaches of blood conservation and improved CPB method with reduced need for allogeneic blood transfusion [7, 8]. Furthermore, the routine primed crystal liquids during CPB inevitably cause severe hemodilution and decreased plasma colloid osmotic pressure, which in turn produce adverse effects on the body [9]. Therefore, large amounts of blood and/or blood products are usually used in cardiac surgery with CPB during perioperative period, so blood protection has always been the focus in cardiology [10]. Thus, new approaches to overcome these problems in CPB are in urgent need.
Retrograde autologous blood priming (RAP) is a new kind of priming technique in patients with CPB to replace the crystal liquid with the patient’s own blood in CPB priming pipe as long as possible [11]. In 1998, Rosengart et al. [12] first proposed the concept of RAP, which is a non-drug blood protection method, to effectively reduce the priming volume, ameliorate the excess hemodilution, improve the hematocrit (Hct) during CPB, and reduce the ratio of patients receiving blood transfusion during operation and the perioperative period. However, controversies about the advantages and disadvantages about RAP remain. Murphy et al. [13] found that RAP application did not reduce allogeneic blood appliance after they performed a 2-year retrospective cohort study, in which 559 cases of coronary artery bypass grafting (CABG) patients with CPB were observed. Hct above 34 in CABG patients may increase the incidence of the postoperative myocardial infarction and severe left ventricular dysfunction [13]. Higher Hct value resulted in increased blood viscosity and harder cardiac work with inevitable damage to the oxygen transport in tissues. Thus, further studies are needed to determine the exact effect and safety of RAP, especially in patients undergoing cardiac valve replacement surgeries.
In this study, we evaluated the short-term effects and safety of perioperative RAP for CPB in patients with cardiac valve replacement surgery to determine whether RAP could reduce perioperative blood transfusion and blood loss and benefit the patients undergoing cardiac surgeries.
Materials and Methods
Patient Population
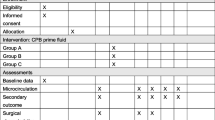
The protocol and consent were approved by an institutional review board or ethics review committee. 240 patients (aged 19–60 years old, pooled from inpatients for 2 years from 2012 to 2014) received cardiac valve replacement surgeries with similar perioperative situations. Written informed consents were received from all participants. The patients were randomized into two groups, the standard priming group (n = 120) and the RAP group (n = 120). The randomization was performed according to a random number sequence generated by computer. Both medical and nursing staff in the ICU and the postoperative wards were blinded from the priming techniques used for the purpose of this study.
Anesthesia
Anesthesia was performed as previously described [14]. Briefly, general anesthesia was induced with propofol, midazolam. After intubation, anesthesia was maintained with target mean blood pressure (BP) at 70 mmHg before and 60 mmHg after CPB using isoflurane and neuromuscular blockade. Heparin was given to achieve anticoagulation with 300 U/kg before CPB. After CPB, 1 mg protamine sulfate was administered for heparin.
Cardiopulmonary Bypass Management
Standard circuit and cardiopulmonary bypass was managed according to previous studies [15]. In brief, patients were dynamically cooled to 32 °C during CPB after intermittent cold (4 °C) blood cardioplegia was infused. Management of CPB included arterial BPs between 50–80 mmHg, pump flow rates of 2.0–2.4 l/min/m, and alpha-stat pH management. Patients were warmed to 37 °C at the end of CPB. Perfusion equipment and techniques were kept constant throughout the study period.
Retrograde Autologous Priming
The RAP process was completed in 2 min. Blood leaking during the process of cardiac catheterization was salvaged and stored in vacuum blood reservoir, which is not mixed with crystal priming liquid in the venous blood reservoir. During RAP process, the changes in blood pressure were closely observed and RAP liquid return rate was in close control. Aorta road was clamped until the pipeline at pulmonary arterial road to the aortic cannula was completely filled with blood. Replace all liquids in the pipeline with autologous blood from the patients as much as possible. After RAP, the venous drainage was open, with the start of a full cardiopulmonary bypass circuit. Once the mean arterial pressure is less than 60 mmHg during RAP process, a small amount of phenylephrine was given to the patients. If the phenylephrine fails to raise BP, RAP is terminated immediately, with the imitating of CPB circuit. At the end of CPB, the remaining blood was replaced with crystal priming liquid in the pipeline.
Indexes for Detection
Blood gas analyses were measured through arterial and mixed venous blood samples obtained according to the following time points: the induction of anesthesia (T1), before CPB (T2), 10 min after aortic cross-clamp (T3), 10 min after declamping (T4), after CPB (T5), at ICU arrival (T6), and discharge (T7). Perioperative indexes were tested, including, Hct, hemoglobin (Hb), total bilirubin, Lac, direct bilirubin, serum glutamic–oxaloacetic transaminase, blood urea nitrogen, and creatinine. The volume of blood transfusion and blood loss was measured during and 2 h after the operation. The outcomes of patients were evaluated based on waking time, duration of postoperative ventilation, and the length of ICU and hospital stay.
Statistical Analyses
STATA 12.0 was used to determine the statistical significance between samples by one-way analysis of variance (ANOVA) or two-way ANOVA followed by the Dunnett’s test. Data are presented as means ± SEM. p < 0.05 was considered to be statistically significant.
Results
The Representative and Scientifically Sound Sample Population by Successful Randomization
All the patients included in this study underwent the surgeries without complications and were successfully discharged. Characteristics of selected patients, types of surgical procedure, and duration of aortic cross-clamping and CPB are compared and summarized in Table 1. No significant difference of these basic clinical characteristics was observed between the two groups.
RAP Significantly Decreased Actual Priming Volume
The volumes of administered fluids before CPB were not significantly different between the RAP group and standard priming group (p > 0.05, data not shown). The total priming volume of an average person was 1013.5 ± 121.5 ml in the RAP group, which is also not statistically different from that in the standard priming group with the value of 1190.9 ± 100.1 ml (p > 0.05, Table 2). Moreover, crystalloid given until first postoperative day and intraoperative urine output was similar between the two groups (Table 2). However, the average priming volume removed in the RAP group was 620.9 ± 191.3 ml, representing 61.2 ± 18.0 % of the priming volume, which thus resulted in a significantly less actual priming volume of the RAP group than that of the standard priming group (p < 0.05). Thus, RAP significantly decreased the actual priming volume, which may help to ameliorate complications resulting from crystal priming liquids.
Comparison of Hb, Hct, and Lac in Patients at Different Time Points
We further compared hemoglobin (Hb), hematocrit (Hct), and lactate (Lac) in patients from different groups at different time points (Fig. 1). In the RAP group, Hct level after 10 min after cross-clamping to ICU was significantly higher than the standard group (p < 0.05). The Hb level in the RAP group, from 10 min after declamping to after CPB increased significantly compared with the standard group (p < 0.05), indicating that RAP could to a certain degree preserve the Hct and Hb level during CPB. Moreover, the results of Lac showed that the RAP group in 10 min after cross-clamping to discharge were significantly lower than those of the standard group (p < 0.05, Fig. 1), suggesting that RAP could decrease Lac accumulation during CPB procedure.
Serial changes of Hb, Hct, and Lac in patients at different time points during the surgeries. Hb hemoglobin; Hct hematocrit; Lac lactate. The time points are listed as follows: the induction of anesthesia (T1), before CPB (T2), 10 min after aortic cross-clamp (T3), 10 min after declamping (T4), after CPB (T5), at ICU arrival (T6), and discharge (T7). *p < 0.05
RAP Lowers the Volume of Transfusion and Dosage Blood Products
The intraoperative blood loss in RAP group is less than that in the standard group, though not significant (p > 0.05, Table 3). There was also insignificant decrease in the 12 h chest tube drainage. These results indicate that RAP will not significantly improve blood loss and chest drainage, which may not be directly related to RAP procedure. 65 (54.2 %) of 120 patients in the RAP group received transfusion as compared with 115 (95.8 %) of 120 patients in the standard priming group (p < 0.05). Preoperatively, fewer patients in the RAP group received PRBCs than did the standard priming group patients [23 (19.1 %) vs. 106 (88.3 %)] (p < 0.05). The transfusion of freshly frozen plasma and platelets was not significantly different between the two groups (Table 3).
Discussion
Protection of autologous blood is an important task in cardiac surgeries. Preoperative preservation of autologous blood, intraoperative hemodilution, autologous blood transfusion, and postoperative chest reinfusion are important factors for this protection. RAP technology is now of great clinical interest for this purpose [16–18]. A rational choice from various available methods to reduce the occurrence of adverse reactions is an important clinical decision [19].
During the past few decades, CPB priming strategies have changed from whole blood priming to non-blood priming, and then to RAP [2, 20]. Recently, the improvement of CPB technique, equipment, and pipes all aim to reduce the volume of pre-charged liquids, get a satisfactory degree of dilution, and reduce the possible complications resulting from hemodilution [21]. RAP is a way to avoid the excessive hemodilution, to maintain a relatively high level of Hct during and at the end of CPB and thus to reduce the volume of blood transfusion [22, 23]. At present, there is no large-scale study of the influence from application of RAP in CPB during cardiac valve replacement surgery.
In the present study, the RAP group had significantly increased Hct during and after operation, reduced actual priming volume to 382.6 ± 118.3 ml, and mildly reduced blood transfusion volume. There was no significant difference between the two groups of patients in the amount of blood loss. In theory, RAP could reduce hemodilution and relatively increased concentrations of coagulation factors and platelets, which may further reduce the blood loss [24, 25]. However, RAP itself is not a hemostatic measure, and we were not able to show that RAP could effectively reduce blood loss in the study.
The early studies on the safety of RAP showed a reverse correlation of blood viscosity and temperature [26]. Moderate hemodilution during CPB was once thought to increase blood viscosity and lead to bad microcirculatory perfusion [26]. In the RAP group, Hct did not appear to be markedly increased in CPB, along with significantly decreased Lac levels. Ranucci et al. [27] and Salinas et al. [28], respectively, reported that, hemodilution during CPB after surgery was associated with bad prognosis like increased blood Lac level and renal failure. Thus, the maintenance of Hct > 0.25 would help to prevent the increased blood lactic acid level. In this study, RAP group effectively improved tissue perfusion and lowered intraoperative Lac levels, by reducing hemodilution, indicating that RAP is able to reduce hemodilution, as well as improve the microcirculation perfusion safely and reliably.
The implementation of the RAP shows poor tolerance for postoperative severe low blood volume in patients, such as elders, low birth weight babies, or those with severe dehydration [29–31]. Thus, preoperative evaluation of general state, preoperative treatments for anemia and dehydration are required to guarantee the smooth application of RAP.
In summary, RAP is an economic, safe, and fast way for autologous blood protection, to reduce hemodilution during CPB, increase Hb and Hct, improve microcirculation perfusion, and decrease the volume of blood transfusion during perioperative care.
References
Zaid, R. R., et al. (2013). Pre- and post-operative diastolic dysfunction in patients with valvular heart disease: Diagnosis and therapeutic implications. Journal of the American College of Cardiology, 62(21), 1922–1930.
Khilji, S. A., & Khan, A. H. (2004). Acute renal failure after cardiopulmonary bypass surgery. Journal of Ayub Medical College, Abbottabad, 16(3), 25–28.
Ekert, H., et al. (2006). Elective administration in infants of low-dose recombinant activated factor VII (rFVIIa) in cardiopulmonary bypass surgery for congenital heart disease does not shorten time to chest closure or reduce blood loss and need for transfusions: A randomized, double-blind, parallel group, placebo-controlled study of rFVIIa and standard haemostatic replacement therapy versus standard haemostatic replacement therapy. Blood Coagulation and Fibrinolysis, 17(5), 389–395.
Song, L., et al. (2011). Effects of peri-operative glucose levels on adverse outcomes in infants receiving open-heart surgery for congenital heart disease with cardiopulmonary bypass. Perfusion, 26(2), 133–139.
Ranieri, V. M., et al. (1999). Time-course of impairment of respiratory mechanics after cardiac surgery and cardiopulmonary bypass. Critical Care Medicine, 27(8), 1454–1460.
Kapoor, P., et al. (2011). Changes in myocardial lactate, pyruvate and lactate–pyruvate ratio during cardiopulmonary bypass for elective adult cardiac surgery: Early indicator of morbidity. Journal of Anaesthesiology Clinical Pharmacology, 27(2), 225–232.
Murai, N., et al. (2005). Venous drainage method for cardiopulmonary bypass in single-access minimally invasive cardiac surgery: Siphon and vacuum-assisted drainage. Journal of Artificial Organs, 8(2), 91–94.
Dogan, R., et al. (2003). Three unusual cases where cardiopulmonary bypass was used in thoracic surgery. Respiration, 70(5), 537–540.
Gruenwald, C. E., et al. (2010). Management and monitoring of anticoagulation for children undergoing cardiopulmonary bypass in cardiac surgery. The Journal of Extra-Corporeal Technology, 42(1), 9–19.
Salis, S., et al. (2008). Cardiopulmonary bypass duration is an independent predictor of morbidity and mortality after cardiac surgery. Journal of Cardiothoracic and Vascular Anesthesia, 22(6), 814–822.
Kearsey, C., et al. (2013). Assessing the effectiveness of retrograde autologous priming of the cardiopulmonary bypass machine in isolated coronary artery bypass grafts. Annals of The Royal College of Surgeons of England, 95(3), 207–210.
Rosengart, T. K., et al. (1998). Retrograde autologous priming for cardiopulmonary bypass: A safe and effective means of decreasing hemodilution and transfusion requirements. Journal of Thoracic and Cardiovascular Surgery, 115(2), 426–438. (discussion pp. 438–439).
Murphy, G. S., et al. (2004). The failure of retrograde autologous priming of the cardiopulmonary bypass circuit to reduce blood use after cardiac surgical procedures. Anesthesia & Analgesia, 98(5), 1201–1207.
Bliacheriene, F., et al. (2012). Anesthesia for cardiac surgery under cardiopulmonary bypass in pregnant patients: Experience with nine cases. International Journal of Obstetric Anesthesia, 21(4), 388–389.
Colangelo, N., et al. (2006). Vacuum-assisted venous drainage in extrathoracic cardiopulmonary bypass management during minimally invasive cardiac surgery. Perfusion, 21(6), 361–365.
Hou, X., et al. (2009). Retrograde autologous priming of the cardiopulmonary bypass circuit reduces blood transfusion in small adults: A prospective, randomized trial. European Journal of Anaesthesiology, 26(12), 1061–1066.
Saxena, P., et al. (2003). Intraoperative autologous blood donation and retrograde autologous priming for cardiopulmonary bypass: A safe and effective technique for blood conservation. Annals of Cardiac Anaesthesia, 6(1), 47–51.
Silver, H. (1975). Banked and fresh autologous blood in cardiopulmonary bypass surgery. Transfusion, 15(6), 600–603.
Balachandran, S., et al. (2002). Retrograde autologous priming of the cardiopulmonary bypass circuit reduces blood transfusion after coronary artery surgery. The Annals of Thoracic Surgery, 73(6), 1912–1918.
Welsby, I. J., et al. (2002). The association of complication type with mortality and prolonged stay after cardiac surgery with cardiopulmonary bypass. Anesthesia & Analgesia, 94(5), 1072–1078.
Manrique, A., et al. (2009). The association of renal dysfunction and the use of aprotinin in patients undergoing congenital cardiac surgery requiring cardiopulmonary bypass. Anesthesia & Analgesia, 109(1), 45–52.
Hwang, J., et al. (2011). The effect of retrograde autologous priming of the cardiopulmonary bypass circuit on cerebral oxygenation. Journal of Cardiothoracic and Vascular Anesthesia, 25(6), 995–999.
Huebler, M., et al. (2006). Cardiopulmonary bypass for complex cardiac surgery using bivalirudin anticoagulation in a patient with heparin antibodies. Journal of Cardiac Surgery, 21(3), 286–288.
Murphy, G. S., et al. (2006). Retrograde autologous priming of the cardiopulmonary bypass circuit: Safety and impact on postoperative outcomes. Journal of Cardiothoracic and Vascular Anesthesia, 20(2), 156–161.
Ortega, G. M., et al. (2003). Alteration of vancomycin pharmacokinetics during cardiopulmonary bypass in patients undergoing cardiac surgery. American Journal of Health-System Pharmacy, 60(3), 260–265.
Ling, I. S., et al. (1992). Changes of blood viscosity in patients undergoing cardiac surgery during cardiopulmonary bypass. Ma Zui Xue Za Zhi = Anaesthesiologica Sinica, 30(3), 153–157.
Ranucci, M., et al. (2006). Lowest hematocrit on cardiopulmonary bypass impairs the outcome in coronary surgery: An Italian multicenter study from the National Cardioanesthesia Database. Texas Heart Institute Journal, 33(3), 300–305.
Sanchez, A. S. Salinas, et al. (2000). Adrenal cortex carcinoma with right atrium involvement. Surgery with cardiopulmonary bypass. Actas Urologicas Espanolas, 24(7), 590–593.
Grieco, G., et al. (1996). Evaluating neuroprotective agents for clinical anti-ischemic benefit using neurological and neuropsychological changes after cardiac surgery under cardiopulmonary bypass. Methodological strategies and results of a double-blind, placebo-controlled trial of GM1 ganglioside. Stroke, 27(5), 858–874.
Kato, Y., et al. (1996). Deep hypothermia cardiopulmonary bypass and direct surgery of two large aneurysms at the vertebro-basilar junction. Acta Neurochirurgica (Wien), 138(9), 1057–1066.
Gruenwald, C. E., et al. (2010). Randomized, controlled trial of individualized heparin and protamine management in infants undergoing cardiac surgery with cardiopulmonary bypass. Journal of the American College of Cardiology, 56(22), 1794–1802.
Acknowledgments
This study was supported by the Technological Innovation Talent Special Foundation of Harbin, China (2009RFXXS018) and the Youth Science Foundation of Heilongjiang Province (QC2013C116).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Cheng, M., Li, JQ., Wu, TC. et al. Short-Term Effects and Safety Analysis of Retrograde Autologous Blood Priming for Cardiopulmonary Bypass in Patients with Cardiac Valve Replacement Surgery. Cell Biochem Biophys 73, 441–446 (2015). https://doi.org/10.1007/s12013-015-0661-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0661-1