Abstract
The present study intends to explore the influence of intensity-modulated radiation therapy on the quality of life for patients with nasopharyngeal carcinoma, which provides a theoretical basis and practical foundation for clinical practice. The present study randomly enrolled 130 cases of patients with nasopharyngeal carcinoma (NPC) in different stages who were admitted in The Second Affiliated Hospital of Fujian Medical University and the First Affiliated Hospital of Chongqing Medical University from September 2007 to August 2012, including 65 cases in IMRT group who received intensity-modulated radiation therapy and 65 cases in CRT group who received conventional radiation therapy. The prescribed dose in the target region of radical radiation therapy was 72 Gy/36 f; the prescribed dose in the target region at high risk was 60–64 Gy/30–32 f; the prescribed dose in the target region at low risk was 50–54 Gy/25–27 f and 2 Gy/f, with conventional fractionated irradiation of 1 f/d and 5 f/w. The data of the quality of life for patients with NPC who received intensity-modulated radiation therapy and conventional radiation therapy were collected and analyzed by filling in the questionnaire survey, including the Quality of Life Questionnaire of Head and Neck 35 (QLQ-H&N35) and Shot Form 36 Health Survey Questionnaire (SF-36). RP, VT, BP, SF, and RE scores in eight fields in SF-36 Scale were declined during the radiation therapy and risen again after radiation therapy, and those measured at 6 months after radiation therapy were higher than those before radiation therapy (all P < 0.05). The scores in IMRT group measured at two and six months after radiation therapy were all higher than those in CRT group (all P < 0.05). The scores of head and neck pain, pararthria, dysphagia, social difficulty, sensory difficulty, difficulty in feeding, xerostomia, cough, sticky saliva, and sensory discomfort during the radiation therapy were lower than those before radiation therapy (all P < 0.05). Except for the scores of sticky saliva and xerostomia, the other scores measured at 6 months after radiation therapy were all lower than those before radiation therapy, and the scores of dysphagia, sticky saliva, and xerostomia in MRT group were lower than those in CRT group (all P < 0.05). Conventional radiation therapy and intensity-modulated radiation therapy can cause a decline the quality of life for the patient with head and neck cancer, but intensity-modulated radiation therapy can improve local tumor control rate and significantly reduce the incidence of adverse reactions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is one of the most frequently malignant tumors in China usually occurs in the southern region that originates in the top and lateral wall of the pharyngonasal cavity, possessing the top incidence of malignant otorhinolaryngologic tumors. It was reported abroad that the 5-year survival rate of NPC patients after radiation therapy was varying from 8 to 62 % [1]. Common clinical symptoms include bloody nasal discharge, nasal obstruction, hearing loss, ear blockage, diplopia, and headache. Since NPC has a good sensitivity to radiation therapy, radiation therapy is the preferred treatment of NPC. Currently, the methods of radiation therapy for NPC include conventional radiation therapy (CRT) and intensity-modulated radiation therapy (IMRT). IMRT is a kind of dimensional conformal radiation therapy that requires for the intensity dose adjustment according to a certain requirement within the radiation field. The beam intensity can be adjusted in allusion to the three-dimensional shape of target region and specific anatomical relationship between the critical organ and target region on the basis of consistency between the radiation field and the shape of target region. The dose distribution within a single radiation field is uneven, while the dose distribution within the gross target volume is more even than that in three-dimensional conformal therapy. It was reported that with the increased clinical application, IMRT technology and its adjusted odd of dose could be converted into a clinical benefit, improve the local control rate, and increase the patient’s life expectancy compared to CRT [2–5]. However, there were few reports whether IMRT could improve the patient’s quality of life compared to CRT, and differences were present in the results [6–8]. This article aims to discuss the influence of IMRT on the quality of life of NPC patients, providing theoretical and practical foundations for its clinical applications.
Materials and Methods
Objects
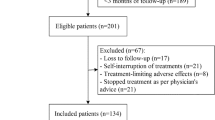
The NPC patients underwent CRT or IMRT and agreed to cooperate with the investigation from September 2007 to August 2012 in our hospital were enrolled in the present study. The inclusion criteria were as follows: (1) patients who were NPC diagnosed by pathological or cytological examination and previously untreated; (2) patients without recurrence or distant metastasis during the follow-up period; (3) patients without other malignant tumor metastasis or invasion to the nasopharynx; (4) patients without other major diseases (cerebral apoplexy, hypertension, heart disease, and diabetes mellitus); (5) patients who were able to answer the questionnaire content independently without a history of mental illness or disturbance of consciousness. A total of 130 NPC patients met with the mentioned conditions, including 65 cases in IMRT group and 65 cases in CRT group. The details are shown in Table 1.
Main Equipments
Accelerator: ClinacEX, 2300C/D medical linear accelerator (Varian, US); TPS: Eclipse treatment planning system (Varian, US); CT simulated positioner: 64-slice spiral CT machine (GE company, US).
Therapy Methods
The radiation therapy with 6 MV X-ray was combined with synchronous chemotherapy in two groups. CRT group: The penetration irradiation was used in the combined field of face and neck. The median dose on the ICRU point of primary gross tumor volume of nasopharynx was 72 Gy/36 f; the dose in tumor target volume at high risk was 60–64 Gy/30–32 f; the dose in tumor target volume at low risk was 50–54 Gy/25–27 f and 2 Gy/f; conventional fractionated irradiation, 1 f/d, 5 f/w. IMRT group: The target dose in tumor volume was expressed as 95 % of the minimal PTV dose (D95 %): primary gross tumor volume of nasopharynx (PGTVnx) = 68.2 Gy/31 f; primary gross tumor volume of neck dissection (PGTVnd) = 66.6 Gy/31 f; primary control tumor volume at high risk (PCTV1) = 62.0 Gy/31 f; primary control tumor volume at low risk (PCTV2) = 52.7 Gy/31 f; primary control tumor volume of neck dissection (PCTVnd) = 52.7 Gy/31 f. The uniformity limit of target dose was D98 > 95 %D95 % and D2 < 110 %D95 %. Vital organs at risk and dose limits: at least one side of the parotid gland Dmean ≤ 25–30 Gy; crystal D2 % < 10 Gy; temporomandibular joint D2 % < 60 Gy; spinal cord D2 % ≤ 45 Gy; brainstem D2 % ≤ 50 Gy; optic nerve and optic chiasma D2 % < 50 Gy; pituitarium D2 % < 60 Gy.
Synchronous Chemotherapy
All patients in stage III and IV and some patients in stage II were given single-agent chemotherapy with 100 mg/m2 cis-platinum within 3 days. The dose was adjusted as AUC = 5.5 or carboplatin. It was given at D1, D21, and D42 after radiation therapy, respectively, with a total of three cycles. The dose of cis-platinum was reduced by 25 % in case of grade 4 of myelosuppression; the chemotherapy was terminated incase of febrile neutropenia or other severe side effects.
Data Collection
All questionnaire surveys were conducted by questionnaire and telephone interview under the guidance of researchers. The patients who were required for reexamination filled the forms themselves. The patients who were not required for reexamination answered the questions in the forms that were filled by the researchers by telephone interview.
Questionnaire
The questionnaire forms included NPC Follow-up Form, Quality of Life Questionnaire Head and Neck 35 (QLQ-H&N35) and SF-36 Scale. The SF-36 Scale with a total of 36 items was used and the following eight items were involved: Physical Functioning (PF), Body Pain (BP), General Health (GH), Role Physical (RP), Vitality (VT), Role Emotional (RE), Social Function (SF), and Mental Health (MH). QLQ-H&N35 was a specific scale of head and neck in combination with the core scale, including 35 items, 7 symptom ratings, and 6 symptom entries of head and neck cancer and adverse reactions. The main contents were involved with pain, sensation, swallowing, eating, speaking, interpersonal communication, sexual life, dental problems, limited mouth opening, xerostomia, cold, sensory discomfort, and sticky saliva. Each item was counted between 1 and 4 points on the basis of 4-level Likert scoring method. The raw score was transformed within 0–100 points by linear conversion in order to achieve the inter-comparison among all fields. The functional level or overall quality of life score was higher and the symptom rating was higher, the symptoms were more obvious.
Statistical Methods
SPSS 15.0 statistical software was used in the present study. The measurement data were expressed with \( \bar{X}\; \pm \;S \). The t test was used for inter-group comparison. The Mann–Whitney U test was used to compare data in various fields between two groups. Wilcoxon signed-rank sum test was used for comparison of datum at each point in time before radiation therapy. P < 0.05 was regarded as statistically significant.
Results
Quality of Life Scores
The RP, VT, BP, SF, and RE scores at 3w in two groups were lower than those before radiation therapy and gradually increased after the end of radiation therapy, which at 6 m were higher than those before radiation therapy (P < 0.05). The scores at 2 and 6 m in IMRT group were higher than those in CRT group. The details are shown in Table 2.
Symptom Scores
The scores of head and neck pain, dysphagia, pararthria, sensory difficulty, difficulty in feeding, social difficulty, xerostomia, sticky saliva, cough, and sensory discomfort after the start of radiation therapy in two groups were lower than those before radiation therapy (P < 0.05), which began to rise at the end of radiation therapy. In addition to xerostomia and sticky saliva, the others at 6 m were higher than those before radiation therapy, and the scores of dysphagia, xerostomia and sticky saliva in IMRT group were lower than those in CRT group (P < 0.05). The details are shown in Table 3.
Discussion
The patients with head and neck cancer who underwent CRT had seriously affected quality of life, with discomforts of xerostomia, difficulty in opening mouth, and oral mucosal reaction during radiation therapy [9–11]. It was reported that the long-term survived patients underwent CRT had xerostomia, with the incidence of 55–70 % corresponding to moderate and severe xerostomia [12–14]. The optimal therapy was determined by NPC biological behaviors. Due to relatively rapid reproduction, poor differentiation, and high degree of malignancy NPC cells which were more sensitive to radiation, the primary means of treatment for NPC were radiation therapy and chemotherapy [15, 16]. IMRT is intensity-modulated radiation therapy, a three-dimensional conformal radiation therapy, which requires for the intensity dose adjustment according to a certain requirement within the radiation field. It can maximize the radiation dose concentrated within the target area to kill tumor cells. It has been widely used in the treatment of head and neck cancer, which can reduce the dose in the surrounding affected organs and shorten the duration of long-term adverse effects. However, there were still few prospective studies on its impacts on the patient’s quality of life [17, 18]. SF-36 was evolved the Boston Health Research on the basis of medical outcomes study-short form (MOS SF) developed by Stewartse in 1988. It is one of the most popular clinical universal scales, which can be used for both the general population and patients. It is easy to use, but there were lack of relevant entries of head and neck cancer. The Symptom Scale is specific for the quality of life questionnaire for head and neck cancer, including 18 symptom fields and 7 multi-item fields (head and neck pain, dysphagia, pararthria, sensory difficulty, social difficulty, difficulty in feeding, and reduced sexual life) and 11 single-item fields (dental problems, xerostomia, difficulty in opening mouth, cough, sticky saliva, feeling ill, nutrition, nasogastric tube, acesodyne, reduced body mass, and increased body mass).
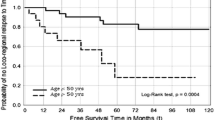
The present study revealed that the RP, VT, BP, SF, and RE scores in eight fields of SF-36 Scale during radiation therapy in two groups were lower than those before radiation therapy and gradually increased after the end of radiation therapy, which at 6 m were higher than those before radiation therapy (P < 0.05). The scores at 2 and 6 m in IMRT group were higher than those in CRT group (P < 0.05). The scores of head and neck pain, dysphagia, pararthria, sensory difficulty, difficulty in feeding, social difficulty, xerostomia, sticky saliva, cough, and sensory discomfort after the start of radiation therapy in two groups were lower than those before radiation therapy (P < 0.05). In addition to xerostomia and sticky saliva, the others at 6 m were higher than those before radiation therapy, and the scores of dysphagia, xerostomia, and sticky saliva in IMRT group were lower than those in CRT group (P < 0.05). Most scores in two scales at 6 m after radiation therapy were increased in two groups, indicating that the quality of life could be improved for IMRT patients. The symptoms of xerostomia and sticky saliva at 6 m were not significantly improved after radiation therapy in two groups, but the scores in IMRT group were higher than those in CRT group. Since IMRT was operated by computer, the radiation dose in the salivary glands could be reduced in high dose of radiation to the tumor target volume to improve the local control rate of tumor, and thus better protecting the function of normal tissues, such as salivary glands, while CRT could not technologically protect the parotid and submandibular glands [19, 20].
In conclusion, CRT and IMRT can cause declined quality of life in patients with head and neck cancer, prolonged time after the end of radiation therapy, and gradual disappearance of adverse reactions, while the local control rate of tumor improved by IMRT and adverse reactions caused by IMRT are much weaker. Therefore, IMRT is worthy of promotion and application in NPC patients. With the improvement of IMRT technology and experience of physician practices, IMRT is expected to improve the survival rate of NPC patients.
References
Stelter, P., & Hurt, E. A. (2014). Pulse-chase epitope labeling to study cellular dynamics of newly synthesized proteins: A novel strategy to characterize NPC biogenesis and ribosome maturation/export[J]. Methods in Cell Biology, 122, 147–163.
Berger, M. L., et al. (2014). A questionnaire to assess the relevance and credibility of observational studies to inform health care decision making: An ISPOR-AMCP-NPC good practice task force report[J]. Value Health, 17(2), 143–156.
Hui, K. F., & Chiang, A. K. (2014). Combination of proteasome and class I HDAC inhibitors induces apoptosis of NPC cells through an HDAC6-independent ER stress-induced mechanism[J]. International Journal of Cancer, 135(12), 2950–2961.
Lee, F. K., et al. (2014). Dosimetric difference amongst 3 techniques: TomoTherapy, sliding-window intensity-modulated radiation therapy (IMRT), and RapidArc radiation therapy in the treatment of late-stage nasopharyngeal carcinoma (NPC) [J]. Medical Dosimetry, 39(1), 44–49.
Rosales-Perez, S., et al. (2014). Expression of Epstein–Barr virus-encoded latent membrane protein (LMP-1), p16 and p53 proteins in nonendemic nasopharyngeal carcinoma (NPC): A clinicopathological study[J]. Archives of Medical Research, 45(3), 229–236.
Jansen, J. P., et al. (2014). Indirect treatment comparison/network meta-analysis study questionnaire to assess relevance and credibility to inform health care decision making: an ISPOR-AMCP-NPC good practice task force report[J]. Value Health, 17(2), 157–173.
Chien, J. M., et al. (2014). The mechanism of NPC-14686-induced [Ca(2)(+)]i rises and non-Ca(2) (+)- triggered cell death in MG63 human osteosarcoma cells[J]. Chinese Journal of Physiology, 57(3), 158–166.
Flemming, D., Stelter, P., & Hurt, E. (2014). Utilizing the Dyn2 dimerization-zipper as a tool to probe NPC structure and function[J]. Methods in Cell Biology, 122, 99–115.
Su, S. F., et al. (2013). Analysis of dosimetric factors associated with temporal lobe necrosis (TLN) in patients with nasopharyngeal carcinoma (NPC) after intensity modulated radiation therapy[J]. Journal of Radiation Oncology, 8, 17.
Feng, X., Ching, C. B., & Chen, W. N. (2012). EBV up-regulates cytochrome c through VDAC1 regulations and decreases the release of cytoplasmic Ca2+ in the NPC cell line[J]. Cell Biology International, 36(8), 733–738.
Shimizu, S., et al. (2014). Early results of urethral dose reduction and small safety margin in intensity-modulated radiation therapy (IMRT) for localized prostate cancer using a real-time tumor-tracking radiation therapy (RTRT) system[J]. Journal of Radiation Oncology, 9, 118.
Lee, B., et al. (2014). Radiation therapy-induced secondary cancer risk for breast cancer: 3D conformal therapy versus IMRT versus VMAT[J]. Journal of Radiological Protection, 34(2), 325–331.
Chin, A. L., et al. (2014). Feasibility and limitations of bulk density assignment in MRI for head and neck IMRT treatment planning[J]. Journal of Applied Clinical Medical Physics, 15(5), 4851.
Johnson, D., et al. (2014). A simple model for predicting the signal for a head-mounted transmission chamber system, allowing IMRT in vivo dosimetry without pretreatment linac time[J]. Journal of Applied Clinical Medical Physics, 15(4), 4842.
Olteanu, L. A., et al. (2014). Comparative dosimetry of three-phase adaptive and non-adaptive dose-painting IMRT for head-and-neck cancer[J]. Radiotherapy and Oncology, 111(3), 348–353.
Saenz, D. L., Paliwal, B. R., & Bayouth, J. E. (2014). A dose homogeneity and conformity evaluation between ViewRay and pinnacle-based linear accelerator IMRT treatment plans[J]. Journal of Medical Physics, 39(2), 64–70.
Mukesh, M. B., et al. (2014). Patient reported outcome measures (PROMs) following forward planned field-in field IMRT: Results from the Cambridge Breast IMRT trial[J]. Radiotherapy and Oncology, 111(2), 270–275.
Moteabbed, M., Yock, T. I., & Paganetti, H. (2014). The risk of radiation-induced second cancers in the high to medium dose region: a comparison between passive and scanned proton therapy, IMRT and VMAT for pediatric patients with brain tumors[J]. Physics in Medicine & Biology, 59(12), 2883–2899.
Leicher, B., et al. (2014). Dosimetric comparison of IMRT rectal and anal canal plans generated using an anterior dose avoidance structure[J]. Medical Dosimetry, 39(3), 272–275.
Hirose, Y., et al. (2014). Evaluation of different set-up error corrections on dose-volume metrics in prostate IMRT using CBCT images[J]. Journal of Radiation Research, 55(5), 966–975.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, J., Liu, P., Wang, Q. et al. Influence of Intensity-Modulated Radiation Therapy on the Life Quality of Patients with Nasopharyngeal Carcinoma. Cell Biochem Biophys 73, 731–736 (2015). https://doi.org/10.1007/s12013-015-0638-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0638-0